Abstract
Paraphimosis is defined as inability to replace the retracted prepuce. If phimosis is inability to retract the foreskin over the glans, paraphimosis is the reverse of it. The word paraphimosis is derived from two Greek words, ‘para’ (meaning ‘beyond’ or ‘resembling’) and ‘phimosis’ (meaning ‘muzzling’ or ‘restriction’). Occasionally it is also spelt as ‘paraphymosis’, as the Greek word phyma (meaning swelling) refers to the characteristic preputial swelling of this condition [1, 2]. Colloquially it is referred to as ‘nuptial night tragedy’ because it is common among newlywed males who, in exited state, indulge in hasty penetrative intercourse without being aware of their pre-existing phimosis. Scientific literature on paraphimosis is largely anecdotal, most of them being restricted to isolated case series and there are hardly any randomized controlled studies [3–6].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Paraphimosis is defined as inability to replace the retracted prepuce. If phimosis is inability to retract the foreskin over the glans, paraphimosis is the reverse of it. The word paraphimosis is derived from two Greek words, ‘para’ (meaning ‘beyond’ or ‘resembling’) and ‘phimosis’ (meaning ‘muzzling’ or ‘restriction’). Occasionally it is also spelt as ‘paraphymosis’, as the Greek word phyma (meaning swelling) refers to the characteristic preputial swelling of this condition [1, 2]. Colloquially it is referred to as ‘nuptial night tragedy’ because it is common among newlywed males who, in exited state, indulge in hasty penetrative intercourse without being aware of their pre-existing phimosis. Scientific literature on paraphimosis is largely anecdotal, most of them being restricted to isolated case series and there are hardly any randomized controlled studies [3,4,5,6].
History of Paraphimosis
Earliest mention of paraphimosis is found in Sushruta Samhita, an ancient Hindu surgical text written in circa 1200 BCE [7]. The then Sanskrit name of paraphimosis was Avapatika. Sushruta vividly describes it as follows:
When the integuments of prepuce is abnormally and forcibly turned back by such causes as coition under excitation, with a girl (before menstruation and before the rupture of the hymen and consequently with a narrow external orifice of the vagina) or masturbation or pressure or a blow on the penis, or a voluntary retention of a flow of semen or forcible opening of the prepuce, the disease is called Avapatika
He recommended reduction by gentle compression of glans using clarified butter as lubricant. Unlike Egyptians, Hindus of ancient India did not practice routine circumcision. This explains as to why paraphimosis is described in Sushruta Samhita but not in Edwin Smith papyrus.
Among the Greek scholars Aulus Cornelius Celsus (25 BC–50 AD) used the term ‘phymosis’ to mean both phimosis and paraphimosis [8]. He advised hot fomentation as relief. It was the Greek physician Antyllus (circa 100 CE) who first used the term paraphimosis [9]. His writings, copied verbatim into the medical encyclopedia of Oribasius (400 CE), reads as follows:
There are two kinds of phimosis: in one case, sometimes the foreskin covers the glans and cannot be pulled back; in the other case, the foreskin is retracted but cannot be returned over the glans. This second type is specifically called paraphimosis
John Hunter, the great English surgeon and founder of Royal College of Surgeons, held that paraphimosis was a sexually transmitted disease because most of his patients had had associated chancroid, syphilis or gonorrhea. A similar notion had existed ever since the times of the great Galen. Interestingly, none of the ancient surgeons considered paraphimosis as a complication of phimosis.
Pathophysiology
Ability to retract the prepuce over the glans as well as replacing it back depends upon two factors namely the elastic compliance of preputial orifice and the tumescence of glans [10]. When any one or both of them are compromised, difficulty arises in retraction of foreskin as well as restoring it to original position. Thus paraphimosis may occur either as a complication of phimosis (uncommon) or independently in a previously normal prepuce (common). This author prefers to call the former as ‘compound paraphimosis’ , while the later as ‘simple paraphimosis’ [10].
When the preputial orifice is cicatrized and stenosed, it is impossible—even with force—to retract it over a flaccid penis. Thus, penile erection is a pre-requisite of compound paraphimosis. On the other hand, simple paraphimosis results when the compliant foreskin is retracted and negligently left at the coronal sulcus for prolonged period. In both the types, the circumferentially narrow skin of preputial orifice, known as the preputial band or constricting paraphimotic band, is stuck at the corona. The inner layer of prepuce is distal to the band while the outer prepuce is proximal to it. Circumferential compression of the preputial band produces a gentle strangulating effect on the glans and the inner prepuce. As the venous return of the glans is hampered it engorges immediately. Tumescent glans prevents spontaneous return of the retracted prepuce. Prolonged impaction impedes lymphatic drainage of inner prepuce and causes it to swell up. Increased tissue pressure of edema worsens the strangulation effect thereby setting a vicious cycle. Vascular congestion of glans in turn precipitates edema of erectile tissue. The combination of preputial band constriction, preputial edema, glans tumescence and glans edema makes reduction of the retracted prepuce increasingly difficult over time. The pace of events occurs much faster in compound paraphimosis than in the simple paraphimosis [10].
As the outer layer of prepuce and penile shaft are proximal to the strangulating preputial band, they remain remarkably normal for a very long period. Onset of infection and inflammation in the edematous ischemic tissue still worsen the situation. It is theoretically possible that in due course, arterial supply to the glans may be compromised leading to necrosis of the penile tip; however, it seldom appears to happen. Rather more practically, capillary ischemia and venous micro infarcts leads to erosions and micro-ulceration of both the glans and the swollen inner prepuce. Frequently, the preputial band is the first to undergo ischemic ulceration. Extraordinary delay in treatment leads to fibroblast infiltration of the edematous inner prepuce, thereby converting it into rubbery tumor like mass [11].
Classification
In 1864 Thompson [12] described two different types of paraphimosis: (1) Primary paraphimosis is a complication of phimosis wherein the preputial swelling is caused by paraphimosis; (2) Secondary paraphimosis occurs as a complication of preputial edema (due to venereal diseases) wherein the preputial swelling was the cause of paraphimosis. In fact, both of them can be included under the compound paraphimosis described above. Rangarajan and Jayakar [11] classified paraphimosis into acute and chronic based on the time delay of seeking medical help and presence of pain. In fact, simple and compound paraphimosis are equivalent but not identical to that of chronic and acute types respectively. However, as the time of presentation depends not only on biological factors but also on socioeconomic factors, the classification of acute and chronic is scientifically imprecise. Some authors have also classified it as ‘painful’ versus ‘painless’ [13]; others classified it as ‘intact-prepuce paraphimosis’ versus ‘post-circumcision paraphimosis’.
Grading System
Kumar and Javle [1] graded the severity of paraphimosis based on the pathogenic sequence (Table 19.1).
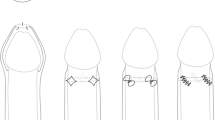
Kumar assumed glanular tumescence to occur at a later stage. In fact, it is the first change to occur in response to gentle strangulation of the glans by the preputial band. Further, Kumar’s grading system does not accomodate gangrene of the glans or chronic fibrosis of the prepuce. The present author has expanded the grading system (Table 19.2) and found it useful in therapeutic decision making (Figs. 19.1 and 19.2).
Epidemiology
Incidence
The exact incidence of paraphimosis in community is not known. Kumar and Javle in 2001 reported 37 patients from India over a period of 63 months and eight patients from UK over a span of 20 months [1]. Rangarajan and Jayakar from South India reported 68 patients between 1997 and 2005 [11]. Cletsoway from California described 13 patients during 1953–57 [14]. Thus, a busy hospital is likely to see 5–6 new cases every year and this trend appears to remain constant irrespective of the geographical location and chronology of time period. Herzog and Alvarez estimated the frequency of paraphimosis among uncircumcised boys to be 0.2% [15]. The present author personally collected 84 cases over a period of 25 years. From these discussions, contrary to popular perception, paraphimosis appears to be a rare disease.
Notwithstanding the forgoing description, high frequency of paraphimosis has also been reported in some series. For example, Kaker et al. from Pakistan reported 45 pediatric cases over a period of 9 months (Feb 2016–Oct 2016) [16]. Similarly, in 2013 Jadhavs from Pune reported 100 patients over a period of 2 years [17]. It is difficult to calculate the actual frequency of paraphimosis from these data because the denominator—the total number of patients seen during the study period—is missing in all these papers. Burstein and Paquin from Canada reported 46 patients between October 2013 and September 2016 [18]. They cite an annual footfall of 84,000 patients in their emergency department. Thus the calculated incidence of paraphimosis is 1 in 5400 emergency admissions.
Sex Predilection
Paraphimosis is exclusively a male disorder. However, the term “female paraphimosis” has also been rarely used imprecisely to mean female urethral prolapse [19] or edema of the clitoral hood [20].
Age Distribution
In pediatric age group paraphimosis has bimodal distribution; [10] the first and larger peak occurs between 3 and 6 years and the second and smaller peak occurs in adolescence (Fig. 19.3). The first peak corresponds to Freud’s phallic phase of personality development during which period children are said to derive pleasure by genital manipulation or massage. The peri-pubertal peak may be explained by the increased frequency of masturbation and sexual misadventures such as self-experimentations [10]. Jadhavs who extended the study to adult population have also noted a similar bimodal presentation [17]. In their study the first peak occurred between 6 and 12 years of age while the second peak occurred during the sexually active age of 21–60 years. It is perplexing as to why adolescents who are more curious of sexual activities are least affected in this study. It is generally agreed that the incidence of compound paraphimosis decreases with increasing age after adolescence while that of simple paraphimosis remains a constant throughout all age groups.
Age distribution of pediatric paraphimosis, (Raveenthiran [10])
Geographic Distribution
Since circumcision is preventive of paraphimosis, one may expect it to be uncommon in countries where routine male circumcision is practiced. Paraphimosis defies this simple logic and it has been reported in large numbers from USA [14] and Islamic countries such as Pakistan [16] where neonatal circumcision is widely practiced for hygiene and religious reasons respectively. Inadequate or incomplete removal of the foreskin is the cause of post-circumcision paraphimosis. Similarly there is no difference in the incidence of paraphimosis between temperate and tropical countries [10].
Etiology
Etiology differs according to the age of patient and the type of paraphimosis. As noted earlier, compound paraphimosis cannot occur in the absence of stiff penile erection. Vigorous sexual acts such as penetrative intercourse [21, 22] and masturbation [23] account for majority of compound paraphimosis. In Rangarajan’s series 63 of the 68 patients (93%) were newlywed and developed this during maiden intercourse [11]. Wining, a form of erotic dancing, wherein the dancers keep rubbing their genitals for several hours has also been described to cause paraphimosis [24]. In a peculiar case, paraphimosis was a corroborative forensic evidence of rape (forced intercourse) [25]. Lichen sclerosis of the prepuce predisposes to paraphimosis by causing phimosis [26].
Simple paraphimosis occurs due to self-retraction by a curious child or parental retraction during bathing [17]. It may also occur in children due to spontaneous nocturnal erection or due to vigorous scratching of genitals as in the case of genital scabies or tinea cruris [10]. Although iatrogenic failure to replace the retracted prepuce following catheterization or cystoscopy is often incriminated in the literature, it is extremely rare accounting for only 5% of all paraphimosis (Table 19.3). Adults may develop simple paraphimosis when they fall asleep after coitus without returning the retracted foreskin.
Rarely swelling of the glans penis and edema of prepuce causes the foreskin to roll back and mimic paraphimosis. They are called pseudo-paraphimosis and their etiology is discussed in the section of differential diagnosis [27]. It is possible that some of the pseudo-paraphimosis are actually secondary paraphimosis (i.e. true paraphimosis precipitated by another unrelated disease). Surprisingly, child abuse has never been reported to cause paraphimosis.
Clinical Features
Clinical features of paraphimosis considerably differ between the two subtypes (Table 19.4). A doughnut-like swelling of the inner prepuce around the corona of glans is characteristic but not unique of paraphimosis; it may also be seen in pseudo-paraphimosis. Contrary to popular perception, paraphimosis—especially the simple variety—is often painless. Children often project the unpleasant glans sensation as pain [10]. Compound paraphimosis which is highly painful usually presents within 24 h while procrastination the rule in simple paraphimosis. In the series of Jadhavs only 4% presented within few hours; 20% presented within 24 h, 68% between 2 and 4 days, 6% between 5 and 6 days and 2% beyond 6 days [17]. The longest reported delay was 25 days! [11]. Social embarrassment associated with the genital tragedy is the principal cause of delay. Senile dementia, lack of proper caretaker, inadequate transport facilities and economic constraints are also responsible for delayed presentation. It is the type of paraphimosis rather than the delay in presentation that is associated with complications such as retention of urine and ischemic ulceration of the glans [10]. This assertion is supported by the fact that those who presented after a delay of 15 days and 25 days were free of voiding problems or penile gangrene [11, 17]. In my personal experience grade-1 lesion is seen in 2% of patients, grade-2 in 72%, grade-3 in 6%, grade-4 in 17% and grade-5b in 2% and grade-5c in 1% [10].
Differential Diagnosis
Occasionally, swelling of the prepuce or the glans causes the foreskin to roll back and mimic paraphimosis. These are better called as secondary paraphimosis or pseudo-paraphimosis [27] and should be considered in the differential diagnosis of true paraphimosis (Fig. 19.4). Glanular hemangioma has been incriminated as the cause of paraphimosis in a 1-year-old boy [28]. Preputio-glanular edema of genital piercing [29], chancroid [30], viral urethritis, syphilitic balanitis of Follmann [31, 32], angioedema, insect- or ant-bite allergy, contact allergy due to topical application of aphrodisiac such as celandine juice [33] and use of auto-erotic devices such as metal rings [34] are known to cause pseudo-paraphimosis. Professional strippers [24] and prostate cancer patients [35], who self-apply penile tourniquet either to sustain erection or to relieve referred pain respectively, are at increased risk of pseudo-paraphimosis. Bizarre etiologies such as plasmodium infection [36] and spinal cord injury (tetraplegia) [37] have been reported; however, they lack satisfactory explanation of pathogenic mechanism. Occasionally, penile paraffinoma (self-injection of substances like paraffin with a mistaken idea of penile augmentation) has been reported to mimic paraphimosis [38]. Coital and non-coital injuries of penis may also result in preputial edema mimicking paraphimosis [39].
Treatment of Paraphimosis
Paraphimosis is a clinical diagnosis and hence laboratory investigations or imaging are unnecessary. Perhaps, for medico-legal reasons, clinical photography is desirable in those who present with ischemic necrosis. The aim of paraphimosis treatment is to restore anatomical normalcy of prepuce by simple manual reduction; [40] when this is impossible, the foreskin is sacrificed to relieve symptoms. Table 19.5 summarizes various therapeutic options available to treat paraphimosis. If the paraphimosis is due to catheterization, removal of the catheter will facilitate reduction.
Anesthesia for Paraphimosis Reduction
Reduction of paraphimosis is a painful procedure and hence requires some form of anesthesia. Topical anesthetics, penile nerve block, procedural sedation, spinal or caudal analgesia and general anesthesia have been used. In a non-randomized study Burstein and Paquin [18] compared paraphimosis reduction using topical LET gel (LET: Lidocaine 4%, Epinephrine 0.1%, Tetracaine 0.5%) versus procedural sedation with ketamine (1–2 mg/kg). They found both of them equally good; however minor adverse events were more frequent with procedural sedation. Topical application of eutectic mixture of 2.5% lidocaine and 2.5% prilocaine (EMLA) has also been reported [41]. Alternatively , Flores and Herring used ultrasound guided dorsal penile nerve block [42]. I prefer penile ring-block using 2% lignocaine in older children and procedural sedation with ketamine or propofol in uncooperative young infants [10].
Simple Manual Reduction Techniques
In thumb-thrusting technique the shaft of penis is held by palmar grasp in the non-dominant hand and the glans is pushed backward using the thumb of dominant hand. The 3-finger (squeeze) technique is similar to thumb-thrusting technique except that the glans is squeezed using the first three fingers of dominant hand while reducing it. Toogood described a 6-finger technique (Fig. 19.5) wherein the preputial doughnut is held between the index and middle fingers of both hands attempting to roll it forward while the glans is simultaneously pushed backward using both the thumbs [2]. Among them, the Toogood’s technique is the most popular method. All these techniques are equally successful in simple paraphimosis especially in stage 1 and 2.
In Keyes’ technique the constricting band of prepuce is still further retracted proximally and the edematous swelling is squeezed before attempting reduction [43]. Wrinkles of the inner prepuce are then smoothened out by applying liberal amount of Vaseline. These maneuvers are believed to facilitate dissipation of edema and reduction of constricting band. Although Keyes recommended lubrication, others found it slippery and messy. I prefer to have firm grip of the preputial doughnut by wrapped a shawl of dry gauze around it.
Adjuvants of Manual Reduction
When simple manual reduction is difficult, it is facilitated by a variety of adjuvant techniques. They can be broadly divided into techniques of dissipating preputial edema and techniques of causing detumescence of the engorged glans. Preputial edema may be dissipated by mechanical, osmotic or enzymatic methods.
-
1.
Mechanical adjuvants
The most popular of all mechanical adjuvants is the puncture technique [44,45,46]. It was originally described by Hamdy-Hastie from Sheffield [44]. Following a spat of priority claims, it was decided to be called as Arbroath-Dundee-Perth technique or simply the ‘needle- or puncture-technique’ [47]. The swollen inner prepuce is punctured at multiple places (usually 6–20) allowing edema fluid to seep out. Frequently, squeezing of edematous prepuce is necessary to expel the fluid. The size of needle used was 21G in Sheffield, 25G in Perth and 26G in Oxford [44,45,46]. Although this technique is invasive, antibiotic prophylaxis is not usually necessary. Critics maintain that it is the manual pressure of squeezing rather than the punctures that is responsible for reduction of edema [48]. It is also said to be ineffective in delayed cases [49].
In Barry’s technique , instead of making punctures, multiple Southey’s needles are inserted into the edematous prepuce and left in situ for the edema fluid to drip [50]. This method has never gained popularity as it is scary to the young patient as well as his caretakers.
In Ganti’s technique , edema can also be reduced by applying constant pressure over the preputial doughnut using a 2-in. wide elastic bandage [51]. The bandage is firmly applied in the distal-to-proximal direction and left in situ for 5–7 min to have the edema reduced. Colorado technique [3] is a modification of Ganti’s method, in which elastic adhesive plaster is used instead of elastic bandage and the duration of compression is 20 min instead of 7 min. As the bandage appears like a headgear of the penis, these methods are also called as turban technique [52]. In some cases, spontaneous reduction of paraphimosis is said to occur with turban technique without the need for further manual reduction.
-
2.
Enzymatic adjuvants : Williams and Nichols [53] first reported the use of hyaluronidase in reducing paraphimosis; Ratliff and Engel popularized it [54, 55]. This enzyme digests the ground substance (hyaluronic acid) and facilitates interstitial dispersion of fluid. About 0.5–1 mL of reconstituted enzyme in normal saline is injected into the edematous preputial doughnut at two or three places and it is gently massaged to reduce edema. Most of the authors used 1:150 dilutions [53,54,55], while Doyle used 1:1000 dilutions [56]. This method enjoyed wide popularity without anyone questioning as to where the fluid would percolate if the preputial band is tightly strangulating proximally. Litzky correctly observed that multiple punctures of the injecting needle rather than hyaluronidase is responsible for reduction of edema [57].
-
3.
Osmotic adjuvants : Several hygroscopic materials have been applied over the glans and preputial doughnut aiming to draw out edema fluid under osmotic gradient. This is the most commonly used method in veterinary practice to reduce paraphimosis in horses and dogs. The lists of hygroscopic agents include gauze soaked in 50% dextrose solution [58] or 20% mannitol [59], paste of glycerin magnesium sulphate [60] and granulated sugar [61, 62]. Although they are obviously less frightening, it is often impractical to tie down the child for 20–30 min for the osmotic reduction to occur.
-
4.
Houghton’s iced glove method [63]: In this technique, a rubber surgical glove is filled with ice cold water and its cuff end is knotted preventing leakage. The affected penis is thrust into the glove by invaginating its thumb. Thus the penis will be inside the glove but without being in actual contact with iced water. In such a position the glove is kept pressed against the pubis until the edema is reduced. It is not known as to whether the low temperature of ice or the compression of gloves that causes the desired effect. Vasospasm induced by ice may reduce venous congestion of glans thereby facilitating reduction. At the same time it is not safe to have vasospasm of penile end artery and risk ischemic gangrene [48]. Further, ice cold temperature is uncomfortable to the patient.
-
5.
EMLA glove technique [41]: Thumb of a surgical rubber glove is cut and filled with EMLA cream. EMLA filled sleeve is then applied to the penis. Osmotic effect of EMLA, compression effect of the rubber sleeve and lubrication effect of the cream probably act additively and cause reduction of edema.
-
6.
Raveenthiran’s aspiration technique [64]: Unlike the aforesaid methods, this technique aims to facilitate simple reduction by reducing tumescence of the glans. This is achieved by thrusting a 20G hypodermic needle into the glans and aspirating blood (Fig. 19.6). It is important that the needle be inserted parallel to urethra to avoid injury. Spontaneous refilling of corporal space while aspiration is prevented by applying a proximal tourniquet. This technique is useful in compound paraphimosis presenting within 48 h.
Instrumental Reduction
Bond vividly described the cause of failures in paraphimosis reduction by drawing analogy of trying to push a rigid glass tube through a slightly smaller-sized India rubber tube [65]. Edges of the rubber tube would buckle inward preventing easy passage of the glass tube; insertion will be made easy if the edges are seized and drawn out. Bond compared the infolding rubber edge with the tight preputial band. Bond’s technique involve pinching the preputial band between the finger nails of both hands and drawing it apart dilating the ring while simultaneously pulling it forward over the glans. Sometimes a second operator is required to push down the glans. Dorsal band traction technique of Turner is a modification of Bond’s method wherein Adson forceps are used instead of finger nails to hold the preputial band [66]. According to the age of patient, either one pair of forceps at 12-o’clock position or two pairs of forceps at 3 and 9-o’clock are used. Skoglund-Chapman’s modification involves using of four Babcock clamps to pinch the preputial band at each quadrant [67]. In all these techniques it is essential to grasp sufficient bulk of tissue to prevent lacerations during reduction. In small children there will insufficient space to apply four Babcock clamps.
Surgical Reduction
When simple or instrumental reduction fails, surgical division of the constricting preputial band brings in success. In fact, small unintended tears of the friable preputial band occurring during forced reduction is actually responsible for many a success of manual techniques. Traditionally the preputial band is incised across at the 12-o’ clock position to avoid bleeding from frenular artery. This Dorsal slit technique often leaves behind an unsightly foreskin necessitating circumcision [68]. Langer-Winthrop’s ventral slitting of preputial band at 6-o’ clock position is intended to avoid this cosmetic disfigurement; [69] it works in flaccid penis but loses its relevance with the onset of erection. Schenck’s preputioplasty involves Heinecke’s principle of horizontally suturing the vertical incision of the preputial band thereby widening it [43]. It is easier said than to do delicate suturing in edematous prepuce.
Circumcision
Emergency circumcision is the last resort when everything else fails. It is generally avoided as sutures tend to cut through the edematous tissue and hence the cosmetic outcome is inferior to elective circumcision. Contrary to this view, Cletsoway and Lewis recommended circumcision as the preferred primary modality of treatment in all cases [14]. Even after successful reduction elective circumcision is recommended by some authors to prevent recurrence. Laceration of preputial band during reduction, underlying phimosis and sloughing (or ulceration) of entangled prepuce are definite indications of elective circumcision.
Comparison of Various Techniques
Most of the literature on paraphimosis are anecdotal and are at the best short series. Personal bias is evident with each author describing a new method. Chance occurrence of treatment success could not be excluded due to extremely small numbers in each series. A systematic review revealed only three out of 33 papers were suitable for analysis. On comparing Houghton’s iced-glove, puncture technique and osmotic reduction by granulated sugar, none of them were found to be superior to each other [4].
Complications
Exact frequency of various complications in paraphimosis is not known. Pathogenic mechanism, cause-effect relationship and optimal treatment of many complications are not well established.
Preputial Lacerations
The commonest complication is perhaps unintended tearing of preputial band during forceful reduction [10]. In fact, success of several manual reductions can be attributed to such incidental lacerations. If the laceration heals spontaneously, it leaves behind a narrow preputial orifice (phimosis) thereby predisposing to further episodes of paraphimosis; if it is severe, it causes grotesque swelling of prepuce. Thus, preputial lacerations invariably necessitate elective circumcision.
Acute Retention of Urine
The cause-effect relationship between acute retention of urine and paraphimosis is not clear. On one hand paraphimosis could be the iatrogenic effect of catheterization for acute retention of urine; on the other hand, tightly strangulating paraphimosis could be the cause of retention. Frequently children present after a delay of several days and they do not suffer any voiding difficulty. From these it appears that a small fraction of compound paraphimosis may present with distended bladder. Reduction of paraphimosis often relieves retention.
Recurrence of Paraphimosis
All paraphimosis patients were previously subjected to elective circumcision even after successful manual reduction. It is logical to assume recurrence of paraphimosis when the underlying causes such as phimosis remain uncorrected [37]. However, in actual practice recurrent paraphimosis is extremely rare. Simple paraphimosis do not recur after successful reduction as the prepuce is normal. Compound paraphimosis, although has the potential to recur, are often irreducible and they end up with emergency circumcision during the first episode. A second episode of paraphimosis definitely calls for circumcision but the same can be avoided with first episode especially if the paraphimosis is of simple type [10].
Gangrene of Glans
Necrosis of the glans may be ischemic [13, 21, 23, 70,71,72] or infective [73]. This is the most feared complication of paraphimosis that is often alluded to in many papers. But a review of literature reveals only seven cases being reported in the world literature over the last two centuries and none of them were in pediatric-adolescent age group (Table 19.6). The youngest was 25 years and five of them (71%) were above 60 years of age. Most of them had had serious co-morbidities such as peripheral vascular disease that could have independently caused glans necrosis. Interestingly, there was no correlation between the occurrence of gangrene and the duration of paraphimosis which ranged from 12 h to 2 weeks. This is corroborated by another report of a patient who presented with healthy glans despite a delay of 25 days [11]. In most of the cases only a part of glans had necrosed. From the foregoing discussion it appears that paraphimosis per se may not be the cause of gangrene; rather it appears to be a precipitator of necrosis in synchrony with another chronic underlying disorder. Except one death, all the other patients have recovered and even the glans morphology had been partially restored.
Urethro-Cutaneous Fistula
Three cases of urethrocutaneous fistula as a complication of neglected paraphimosis have been described in the literature [13, 23, 74]. In all of them fistula was attributed to ischemic necrosis of the ventral glans; but the diagnosis of paraphimosis was not established beyond doubt. Retrospective critical analysis suggests that they could be secondary or pseudoparaphimosis.
Mortality and Outcome
Outcome of paraphimosis is generally excellent. There are only two reports of death in paraphimosis: one was due to chloroform related complication reported in the last century [75] and the other was a 85-year-old man who died of Fournier gangrene complicating paraphimosis [73]. There are no data on the long-term effect of paraphimosis on sexual function.
References
Kumar V, Javle P. Modified puncture technique for reduction of paraphymosis. Ann R Coll Surg Engl. 2001;83:126–7.
Toogood J. On the treatment of paraphymosis. Prov Med Surg J. 1842;3:312–3.
Pohlman GD, Phillips JM, Wilcox DT. Simple method of paraphimosis reduction revisited: point of technique and review of the literature. J Pediatr Urol. 2013;9:104–7.
Mackway-Jones K, Teece S. Best evidence topic reports. Ice, pins, or sugar to reduce paraphimosis. Emerg Med J. 2004;21:77–8.
Chung CH. Emergency management of paraphimosis. Hong Kong J Emerg Med. 2003;10:253–7.
Choe JM. Paraphimosis. Current treatment options. Am Fam Physician. 2000;62:2623–6.
Bhishagratna KL. (Tr) The Sushruta Samhita: an English translation based on original Sanskrit text. Calcutta: Bhaduri publications; 1907.
Hodges FM. Phimosis in antiquity. World J Urol. 1999;17:133–6.
Hodges FM. The history of phimosis from antiquity to the present. In: Denniston GC, Hodges FM, Milos MF, editors. Male and female circumcision medical, legal, and ethical considerations in pediatric practice. New York: Kluwer Academic; 1999. p. 37–62.
Raveenthiran V. On the rationale of paraphimosis treatment based on a new system of classification. Proceedings of 7th annual conference of Indian Association of Pediatric Surgeons (Tamilnadu - Pondicherry chapter), Vellore, 11-12 July 2008.
Rangarajan M, Jayakar SM. Paraphimosis revisited: is chronic paraphimosis a predominantly third world condition? Trop Dr. 2008;38:40–2.
Thompson J. Paraphimosis. Br Med J. 1864;2:363–4.
Hollowood AD, Sibley GN. Non-painful paraphimosis causing partial amputation. Br J Urol. 1997;80:958.
Cletsoway RW, Lewis EL. Treatment of paraphimosis. U S Armed Forces Med J. 1957;8:361–4.
Herzog LW, Alvarez SR. The frequency of foreskin problems in uncircumcised children. Am J Dis Child. 1986;140:254–6.
Kakar M, Rehman M, Shah A. Emergency treatment of paraphimosis by multiple needle puncture technique in children. Pak J Med Health Sci. 2017;11:401–2.
Jadhav SE, Jadhav SS. Clinical study of proportion of predisposing events and causes of paraphimosis. Indian J Appl Res. 2013;3:373–4.
Burstein B, Paquin R. Comparison of outcomes for pediatric paraphimosis reduction using topical anesthetic versus intravenous procedural sedation. Am J Emerg Med. 2017;35:1391–5.
Salim S, Taylor A, Carter C. Female paraphimosis? Management of a large female urethral caruncle, trialling manual reduction. J Obstet Gynaecol. 2014;34:282–3.
Willan RJ. Paraphimosis of the clitoris. Br Med J. 1928;2:1130–1.
Raman SR, Kate V, Ananthakrishnan N. Coital paraphimosis causing penile necrosis. Emerg Med J. 2008;25:454.
Berk DR, Lee R. Paraphimosis in a middle-aged adult after intercourse. Am Fam Physician. 2004;69:807–8.
Sato Y, Takagi S, Uchida K, et al. Long-term follow-up of penile glans necrosis due to paraphimosis. IJU Case Rep. 2019;2:171–3.
Ramdass MJ, Naraynsingh V, Kuruvilla T, Maharaj D. Case report. Paraphimosis due to erotic dancing. Tropical Med Int Health. 2000;5:906–7.
Saini OP, Suman A, Buri S, Saini PK, Mathur PN, Gahlot RK. Paraphimosis – a case report and medicolegal importance. J Indian Acad Forensic Med. 2008;30:82–3.
Roh D, Jin H, You HS, et al. Balanopreputial adhesion and paraphimosis due to lichen sclerosus. Ann Dermatol. 2018;30:384–6.
Ng KL, Mahadevan DT, Htun TH, Razack AH, Dublin N. Pseudoparaphimosis: a hairy affair. Med J Malaysia. 2011;66:268–9.
Yigiter M, Arda IS, Hiçsönmez A. An unusual cause of paraphimosis: hemangioma of the glans penis. J Pediatr Surg. 2008;43:e31–3.
Jones SA, Flynn RJ. An unusual (and somewhat piercing) cause of paraphimosis. Br J Urol. 1996;78:803–4.
Harvey K, Bishop L, Silver D, Jones T. A case of chancroid. Med J Aust. 1977;26:956–7.
Nadimi AE, Carver CM. Syphilis presenting with paraphimosis: painless no longer. J Am Acad Dermatol. 2016;74(5):AB154.
Mainetti C, Scolari F, Lautenschlager S. The clinical spectrum of syphilitic balanitis of Follmann: report of five cases and a review of the literature. J Eur Acad Dermatol Venereol. 2016;30:1810–3.
Farina LA, Alonso MV, Horjales M, Zungri ER. Contact-derived allergic balanoposthitis and paraphimosis through topical application of celandine juice. Actas Urol Esp. 1999;23:554–5.
Low LS, Holmes M. The GEM ring cutter: an effective, simple treatment of penile strangulation caused by metal rings. Urol Case Rep. 2018;19:39–41.
Wimsey S, Thiruchelvam N, Keoghane SR. A key cause of paraphimosis. Int Urol Nephrol. 2006;38:111–3.
Gozal D. Paraphimosis apparently associated with Plasmodium falciparum infection. Trans R Soc Trop Med Hyg. 1991;85:443.
Ghosh S. Recurrent paraphimosis in a tetraplegic patient admitted for inpatient rehabilitation. Turk J Phys Med Rehab. 2014;60(Supp. 1):S78–80.
Downey AP, Osman NI, Mangera A, Inman RD, Reid SV, Chapple CR. Penile Paraffinoma. Eur Urol Focus. 2019;5:894–8.
Verma S. Coital penile trauma with severe paraphimosis. J Eur Acad Dermatol Venereol. 2005;19:134–5.
Vunda A, Lacroix LE, Schneider F, Manzano S, Gervaix A. Reduction of paraphimosis in boys. N Engl J Med. 2013;368:e16 (Video).
Khan A, Riaz A, Rogawski KM. Reduction of paraphimosis in children: the EMLA glove technique. Ann R Coll Surg Engl. 2014;96:168.
Flores S, Herring AA. Ultrasound-guided dorsal penile nerve block for ED paraphimosis reduction. Am J Emerg Med. 2015;33(863):e3–5.
Schenck GF. The treatment of paraphimosis. Am J Surg. 1930;8:329.
Hamdy FC, Hastie KJ. Treatment for paraphimosis: the ‘puncture’ technique. Br J Surg. 1990;77:1186.
Waters TC, Sripathi V. Reduction of paraphimosis. Br J Urol. 1990;66:666.
Reynard JM, Barua JM. Reduction of paraphimosis the simple way - the Dundee technique. BJU Int. 1999;83:859–60.
King PA. Reduction of paraphimosis the simple way - the Dundee technique. BJU Int. 2001;88:305.
Saxena A. Reduction of paraphimosis. Br J Urol. 1992;69:220.
Kamat N. Reduction of paraphimosis the simple way - the Dundee technique. BJU Int. 1999;84:890–1.
Barry CN. A simple method for reduction of paraphimosis. J Urol. 1954;71(4):450.
Ganti SU, Sayegh N, Addonizio JC. Simple method for reduction of paraphimosis. Urology. 1985;25:77.
Olson C. Emergency treatment of paraphimosis. Can Fam Physician. 1998;44:1253–4.
Williams TH, Nichols RK. Method of treating paraphimosis. J Med Assoc Alabama. 1952;21:233–4.
Ratliff RK. Hyaluronidase in the treatment of paraphimosis. J Am Med Assoc. 1954;155:746.
Engel WJ. Hyaluronidase as an aid to correction of paraphimosis: report of a case. Cleve Clin Q. 1954;21:24–6.
Doyle JO. Hyaluronidase in treatment of sequela of paraphimosis. Br Med J. 1954;2:1401.
Litzky GM. Reduction of paraphimosis with hyaluronidase. Urology. 1997;50:160.
Coutts AG. Treatment of paraphimosis. Br J Surg. 1991;78:252.
Anand A, Kapoor S. Mannitol for paraphimosis reduction. Urol Int. 2013;90:106–8.
Kamat N. Reduction of paraphimosis the simple way. BJU Int. 1999;84:890–1.
Kerwat R, Shandall A, Stephenson B. Reduction of paraphimosis with granulated sugar. Br J Urol. 1998;82:755.
Gonzalez Fernandez M, Sousa Escandon MA, Parra Muntaner L. Sugar: treatment of choice in irreducible paraphimosis. Actas Urol Esp. 2001;25:393–5.
Houghton GR. The “iced-glove” method of treatment of paraphimosis. Br J Surg. 1973;60:876–7.
Raveenthiran V. Reduction of paraphimosis: a technique based on pathophysiology. Br J Surg. 1996;83:1247.
Bond CJ. Note on the treatment of paraphimosis. Lancet. 1883;2:1180–1.
Turner CD, Kim HL, Cromie WJ. Dorsal band traction for reduction of paraphimosis. Urology. 1999;54:917–8.
Skoglund RW Jr, Chapman WH. Reduction of paraphimosis. J Urol. 1970;104:137.
Fuenfer MM, Najmaldin A. Emergency reduction of paraphimosis. Eur J Pediatr Surg. 1994;4:370–1.
Langer JC, Winthrop AL. Ventral slit for phimosis and paraphimosis in children. Pediatr Surg Int. 1995;10:209–10.
Palmisano F, Gadda F, Spinelli MG, Montanari E. Glans penis necrosis following paraphimosis: a rare case with brief literature review. Urol Case Rep. 2017;16:57–8.
Williams JC, Morrison PM, Richardson JR. Paraphimosis in elderly men. Am J Emerg Med. 1995;13:351–3.
Sokhal AK, Saini DK, Sankhwar S. Para phimosis leading to glans gangrene - a devastating preventable complication. Balkan Med J. 2017;34:180–1.
Ahmed J, Mallick IH. Paraphimosis leading to Fournier’s Gangrene. J Coll Physicians Surg Pak. 2009;19:203.
Chitale AM, Gulati J, Manekar AA, Thakre SB. A rare case of ventral urethrocutaneous fistula post paraphimosis treatment. Indian. J Appl Res. 2018;8:50–1.
Eddowes A. Reduction of paraphimosis. Br Med J. 1877;2:324.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Raveenthiran, V. (2020). Paraphimosis. In: Normal and Abnormal Prepuce. Springer, Cham. https://doi.org/10.1007/978-3-030-37621-5_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-37621-5_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-37620-8
Online ISBN: 978-3-030-37621-5
eBook Packages: MedicineMedicine (R0)