Abstract
Many types of neurologic injury are known to affect the cardiovascular system. Both rhythm and pump function can be dramatically affected. In this chapter, we review the cardiovascular changes that can be seen after neurologic injury and the specific neurologic diseases most commonly associated with those changes. This chapter covers hypertension, cardiomyopathy, shock, arrhythmias, and myocardial ischemia. These neurocardiogenic changes are important to diagnose, understand, and manage in order to simultaneously optimize neurologic recovery and cardiovascular function. Recognition of these neurocardiovascular connections can help neurointensivists and cardiologists best understand the underlying driving forces behind hemodynamic instabilities that can be seen in patients after acute neurologic injury.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The heart-brain connection has been documented for centuries, and a variety of neurologic emergencies are known causes of disruption of the cardiovascular system [1,2,3]. While the main focus of this book has been to provide guidance on the triage and management of neurologic disease, it would be remiss to ignore the cardiovascular impact that neurologic disease can have and how management of the cardiovascular system is imperative in preventing further neurologic decline. Here we describe some of the cardiac complications that one might encounter in the emergency department or after admission to the neurocritical care unit (NCCU) that require management in the setting of various neurologic diseases.
Hypertension
Hypertension is the etiology, or at the very least a contributing factor, underlying multiple neurologic conditions, including hypertensive urgency, posterior reversible encephalopathy syndrome (PRES), ischemic stroke, and intracranial hemorrhage. In the NCCU, a provider will be faced with the need to manipulate blood pressure in different ways to reduce secondary injury. Many of these interventions can and should be initiated in the emergency department immediately upon identifying the diagnosis.
Hypertensive encephalopathy and the PRES spectrum are the most notable of neurologic diseases directly caused by hypertension. Hypertensive encephalopathy occurs when severe hypertension induces headache, nausea, visual disturbances, confusion, seizures, and ultimately coma. PRES is a manifestation of accelerated hypertension in which encephalopathy can be accompanied by focal symptoms and MRI hyperintensities that are typically posterior and symmetric, though this can vary. In extreme cases, small amounts of subarachnoid hemorrhage can occur. These imaging findings are thought to be due to an alteration in the permeability of blood vessels, leading to edema, but these changes most often normalize over the course of several weeks [4]. PRES can also be found in eclampsia, which manifests with seizures in addition to the above findings. Treatment of hypertensive encephalopathy is typically performed using antihypertensive agents. Target blood pressure (BP) is either 20% reduction per day or systolic blood pressure (SBP) <140 mm Hg, generally via intravenous medications (calcium channel or beta-blockers) followed by oral agents once stable. In eclampsia, continuous magnesium sulfate is the mainstay of treatment in addition to BP control.
One of the major causes of intraparenchymal hemorrhage is hypertension. A patient presenting with hypertension and hemorrhage location in deeper brain regions such as the basal ganglia, brainstem, and cerebellum tends to suggest a hypertensive etiology [4]. Regardless of intraparenchymal hemorrhage etiology, BP control post-hemorrhage is vital to reducing the risk of hematoma expansion. This BP control can be difficult to manage, and there has been some controversy regarding the optimal target SBP goal, with the ATACH II and INTERACT-2 trials showing no difference in death or disability with aggressive BP lowering measures. However, SBP goal <140 is generally viewed as safe and is thus an adopted target for many centers, with liberalization of that goal to SBP < 160 after hemorrhage stability is confirmed [5]. Initial BP lowering is recommended via intravenous antihypertensive medications, followed by the addition of oral agents. In some patients, BP can be difficult to manage on an oral regimen, ultimately requiring multiple agents. It is important for these patients to be closely followed as they exit the acute period as there is a risk of developing hypotension while on these medications as their post-hemorrhage hypertension resolves.
More broadly, intracranial hemorrhage, including epidural hemorrhage, subdural hemorrhage, subarachnoid hemorrhage, and intraventricular hemorrhage of any etiology, is recommended to be treated in the same manner with SBP goal <140 until hemorrhage is confirmed stable after which liberalizing to <160 is often acceptable.
Ischemic stroke can be caused by hypertension as well, though a majority of these strokes tend to be smaller in size compared to their embolic counterparts. Hypertension management becomes more relevant after an ischemic stroke of any etiology occurs. For 24 hours after ischemic stroke, BP should be allowed to autoregulate up to SBP 220 (unless the patient has other active medical problems such as myocardial infarction that often require SBP < 140, or the patient has received thrombolysis, anticoagulation, or thrombectomy in which case SBP < 185 is often used as an upper limit). After this time period, the BP should be brought down by 20% per day to normotension. The exception to this rule is when a patient has evidence of a pressure-dependent exam, meaning that at higher BPs symptoms improve and at lower BPs symptoms worsen, suggesting a relative perfusion deficit with at-risk penumbral tissue. In this instance, close BP monitoring in the intensive care unit (ICU), while maintaining BP in a range that provides the best clinical exam, is crucial. Often IV fluids and vasopressors are considered to maintain this perfusion as needed, though the evidence behind this practice is Class IIb [6].
Traumatic spinal cord injury is another neurologic disease for which blood pressure management is key. Adequate perfusion must be maintained after blunt force injury to the spinal cord. While the data are limited, general practice guidelines suggest maintaining a mean arterial pressure (MAP) goal of 85–90 for 7 days [7]. This often requires vasopressors given the vasoplegia that occurs post-injury. In particular, norepinephrine is often the vasopressor of choice given it is less likely to exacerbate any bradycardia that may already exist. Spinal cord injury itself induces multiple hemodynamic changes both acutely and chronically. Acutely, both spinal shock and neurogenic shock can be observed [8], the latter of which will be discussed in the shock section below.
Autonomic dysfunction is very common after spinal cord injury, usually above T6 and more common in those who suffer American Spinal Injury Association (ASIA) A grade injuries. Hypertension, tachycardia, or bradycardia can be seen along with a host of other manifestations including diaphoresis and spasms. Left untreated, such symptoms can lead to PRES, seizures, intracranial hemorrhage, myocardial infarction, and even death [8]. However, autonomic dysfunction is not limited to spinal cord injury alone. It can be seen in many severe manifestations of brain injury including traumatic brain injury, hypoxic-ischemic injury, infectious or autoimmune encephalitis, and many others. Autonomic dysfunction can be difficult to treat as it manifests as paroxysmal events, which can sometimes be characterized by different autonomic changes. Intravenous management of these episodes often relies upon opiates, benzodiazepines, and antihypertensive medications. Oral treatment options for dysautonomia are extensive and best chosen based upon the predominant symptoms and triggers. For those with mainly BP and heart rate manifestations, beta-blockers, such as propranolol, and alpha-blockers, like clonidine, are commonly used.
Cardiomyopathy
While both electrical and structural abnormalities of the heart have been noted after brain injury, probably none is more famous than Takotsubo cardiomyopathy, the subject of “Voodoo Death” documented in 1942 [1, 2]. Takotsubo cardiomyopathy is also referred to as stress-induced cardiomyopathy or more recently as neurogenic stress cardiomyopathy [9]. The classic abnormality is apical hypo- or akinesis with intact contraction at the base, leading to a ballooning pattern from which its namesake is derived [10]. However, both mid-ventricular and basilar hypokinetic patterns have been described [11,12,13]. The cardinal rule of neurogenic cardiomyopathy is that there is complete functional recovery in most cases. The exception is very severe cardiomyopathy with such poor ejection fraction as to cause cardiogenic shock and sometimes death.
Neurogenic cardiomyopathy has been reported after nearly all acute brain injuries, including ischemic stroke, seizures, intraparenchymal hemorrhage, infection, traumatic brain injury, and, most commonly, subarachnoid hemorrhage [14,15,16,17,18]. In fact, neurogenic cardiomyopathy has been reported in up to 30% of subarachnoid hemorrhage cases [9, 12]. Patients who develop neurogenic cardiomyopathy as a complication of their acute brain injury have significantly higher mortality than those without [19]. Pathophysiologically, it is thought that there is a catecholamine surge at the time of neurologic injury that leads to contraction band necrosis and early calcifications [2, 12, 19,20,21,22].
Early diagnosis of neurogenic cardiomyopathy is important for initiating proactive treatment to prevent complications and speed recovery. It can sometimes be clinically difficult to differentiate from primary ischemic cardiomyopathy, and there have been multiple investigations into the utility of various biomarkers [23, 24]. Troponins are highly sensitive for cardiac dysfunction and should be trended, but alone can mislead a provider into thinking a patient is suffering from a myocardial infarction. Transthoracic echocardiograms are needed to assess bi-ventricular dysfunction and the presence of left ventricular outflow tract (LVOT) obstruction and characterize the pattern of hypokinesis. Concurrent measurements of N-terminal prohormone of brain natriuretic peptide (NT-proBNP) and creatine kinase-muscle/brain (CK-MB) have been found to be more specific in assessing cardiomyopathy and differentiating it from cardiac ischemia. In particular, high ratios of NT-proBNP/ejection fraction and NT-proBNP/CK-MB were found to be most accurate in predicting neurogenic stress cardiomyopathy [23, 24]. This is thought to be related to the high levels of BNP released in the catecholamine surge that induces neurogenic stress cardiomyopathy.
The mainstay of treatment for neurogenic stress cardiomyopathy is supportive care [12, 20]. Because it is a reversible injury in most without hemodynamic instability, diuretics and afterload reduction are important in both optimizing cardiac output and reducing pulmonary edema. If there is no LVOT obstruction, then often beta-blockers and/or angiotensin-converting enzyme (ACE) inhibitors are initiated until functional recovery is documented, though some encourage continuing beta-blockers indefinitely [12, 20, 25]. Short interval repeat transthoracic echocardiogram is recommended, as functional recovery is typically within 1–4 weeks. Approximately 10% of patients develop cardiogenic shock, which may be related to the severity of ventricular dysfunction or the presence of LVOT obstruction [25]. The management of cardiogenic shock is discussed in section entitled “Shock”. Of note, in rare cases, LV thrombus formation is a complication of reduced ejection fraction, and anticoagulation should be considered if evidence that the source of hemorrhage, like an aneurysm, is obliterated.
Shock
Cardiogenic Shock
In the majority of patients suffering cardiogenic shock after neurologic injury, neurogenic stress cardiomyopathy is the cause. However, pre-existing cardiac dysfunction can be exacerbated in the setting of acute neurologic injury. Diagnostically, transthoracic echocardiogram is needed to assess bi-ventricular function. Other ancillary tests include pulmonary artery catheterization, the measurement of central venous pressures, and more recently, advanced hemodynamic monitoring using arterial pressure waveform–based cardiac output measurements. Measures of filling pressures and systemic vascular resistance can assist with guiding therapy, though these and the above tests have unclear benefit with regard to patient outcomes.
Treatment of cardiogenic shock depends on whether LVOT obstruction exists. If there is no LVOT obstruction, then cautious fluid resuscitation (if pulmonary congestion is minimal) should be used. This is usually followed by inotropic therapy with dobutamine or dopamine. However, before initiating these therapies, the clinician must first evaluate for LVOT obstruction and heart failure with preserved ejection fraction since these medications can worsen cardiogenic shock if these abnormalities are present [25]. Milrinone and, outside the US, levosimendan have been shown to be promising inotropic therapies as well and can be used as concomitant therapy [12, 14, 20, 26]. Vasopressors may also be necessary in persistently hypotensive patients refractory to the above therapies. Norepinephrine, with both vasopressor and inotropic effects, is often the first-line agent in this scenario. Phenylephrine may be helpful in LVOT obstruction cases by increasing afterload and improving hemodynamics but should be used with close monitoring as the vasoconstrictive properties could be harmful. Vasodilator therapy, such as nitroprusside, is reserved for those with evidence of severe hypertension, acute mitral regurgitation, or acute aortic regurgitation. In most cases, the primary neurologic injury precludes the use of mechanical circulatory support, such as intra-aortic balloon pumps, ventricular assist devices and extra-corporeal membrane oxygenation, due to the risk of hemorrhage. However, if a patient has refractory hypotension and LV dysfunction with a neurologic injury that does not preclude full anticoagulation, then these forms of mechanical support should be considered. More recently, the requirement for anticoagulation in intra-aortic balloon pumps has been called into question, and they have been used successfully without anticoagulation in small case series [27, 28], so this mechanical modality without anticoagulation is also a consideration on a case-by-case basis.
Septic Shock
While septic shock is less common in the NCCU than in the Medical Intensive Care Unit, it can be seen either related to the patient’s primary neurologic injury, as is the case in bacterial meningitis or endocarditis, or as a complication of a patient’s admission to the ICU (e.g., pneumonia from mechanical ventilation, central line–related infections). In general, sepsis is a leading cause of death in hospitalized patients [29]. There has been a concerted push for early identification and treatment to reduce the mortality and morbidity of this disease, with new international guidelines published in 2016 [30]. For the diagnosis of sepsis, routine cultures (including aerobic and anaerobic blood, urine, sputum, etc.) should be collected without delay, preferably before starting antimicrobial therapy as cultures can sterilize within minutes to hours after treatment administration. Repeat cultures should be completed prior to antimicrobial changes. Establishing urgent vascular access is imperative to care, including the use of intraosseous access if necessary as it is fast and reliable. Intravenous antimicrobials should be started as soon as possible after recognition of sepsis and septic shock. This is because each hour delay in administration of appropriate antimicrobials is associated with a measurable increase in mortality [29]. Broad-spectrum therapy is recommended to cover all likely pathogens. For many infections, a 7–10-day duration of antimicrobial treatment is sufficient with longer courses reserved for special circumstances. More recently, procalcitonin levels are being used in some institutions both for the diagnosis of bacterial infections and to support shortening the duration of antibiotic therapy [30]. Aggressive fluid resuscitation with crystalloids using an initial infusion of 30 cc/kg is recommended, with volume status reassessment thereafter. If a patient is felt to be euvolemic but remains hypotensive, then vasopressors should be initiated. Norepinephrine is the first-choice vasopressor for septic shock. The addition of vasopressin or epinephrine to either augment MAP goals or decrease norepinephrine dosage is also recommended. Dopamine is only to be used in a select group of patients at low risk for tachyarrhythmias and bradycardia. Dobutamine can be used in patients who show persistent hypoperfusion despite adequate fluid resuscitation and vasopressor agents. Milrinone and levosimendan, where available, can also be considered, though dobutamine is considered the first-line inotrope for septic shock. The use of corticosteroids in sepsis is controversial and generally not recommended, but in refractory cases of septic shock, there is new evidence to suggest that intravenous hydrocortisone plus fludrocortisone confer some benefit [31, 32]. If the source of sepsis is pulmonary with associated evidence of acute respiratory distress syndrome (ARDS), then low-volume ventilation and other maneuvers should be used as needed for proper ARDS management.
Neurogenic Shock
Neurogenic shock is hypotension, and sometimes also bradycardia, due to loss of sympathetic tone leading to vasodilation and increased vagal tone [8]. A majority of cases are related to cervical and high thoracic spinal cord injury, though it can rarely be seen after severe brain injury. This type of shock is different than the above shock types. Normally in shock, the sympathetic nervous system triggers multiple compensatory mechanisms including vasoconstriction, tachycardia, and hyperventilation to shunt blood away from the extremities and toward vital organs. In neurogenic shock, these compensatory mechanisms are impaired. Diagnostically, patients will have clinical evidence of vasodilation, such as warm peripheries and slower heart rates that are unique from other forms of shock. Dopamine is often used as first-line therapy, with the addition of phenylephrine or other vasopressors as needed [8]. Newly available angiotensin II analogs are mechanistically promising in treating hypotension but have yet to be evaluated in neurogenic shock. Atropine can be administered for slowed heart rate. Neurogenic shock usually resolves over the course of 1–6 weeks post-injury [8].
Hemorrhagic Shock
Hemorrhagic shock is never due to primary neurologic injury and is rarely seen in the setting of neurosurgical procedures during which some inadvertent vascular access, such as into the venous sinuses, results in massive blood loss, which without proper transfusions can be fatal. Outside of this infrequent circumstance, hemorrhagic shock after acute brain injury is secondary to either a common preceding event (e.g., a patient on anticoagulation who has an intracranial hemorrhage in addition to other systemic hemorrhage) or a complication of hospitalization (e.g., stress ulcer). Frequent hemoglobin monitoring and assessment of coagulation abnormalities are crucial for diagnosis. Imaging, including endoscopy, is vital to identifying any hemorrhage source. Volume resuscitation is the cornerstone to treating hemorrhagic shock. Crystalloid fluid can be used immediately for volume resuscitation as it is readily available, but ultimately replacement with blood products is preferred as soon as possible. If needed, a massive transfusion protocol should be activated, with the patient being resuscitated with 1:1:1 (red blood cells to platelets to fresh frozen plasma) blood products as suggested by new guidelines [33]. Large bore intravenous catheters (preferably 14 or 16 gauge), intraosseous access, or sheath introducers (e.g., Cordis) are preferred for rapid infusion. The number one priority is to control the source of bleeding whether via surgical or endovascular means. If a coagulopathy is diagnosed, then factor replacement and/or cryoprecipitate should be considered.
Myocardial Infarction
STEMI
ST segment elevations after primary neurologic injury are common, but ST-elevation myocardial infarctions (STEMIs) are not. ST elevations are often due to neurogenic stress cardiomyopathy, demand ischemia, and rarely aortic dissections [15, 23]. ST elevations from coronary artery ischemia that is concurrent with acute brain injury are rare though possible in cases such as hypercoagulable states, cocaine use, and aortic dissection. EKG, troponin, and BNP should be immediately checked [23]. If a bedside echocardiogram is readily available without delaying treatment decisions, it may help to assess for regional wall motion abnormalities. As with all circumstances in which STEMI is suspected, the hospital procedure for activating the catheterization lab team should be initiated in a time-sensitive manner. However, the concurrent acute neurologic injury may limit treatment options (and perhaps even anticoagulation during the procedure). Primary myocardial infarction treatment often necessitates stent treatment that requires dual antiplatelet therapy, which is often contraindicated in certain acute neurologic injuries such as intracranial hemorrhage or large cerebral infarction. Similarly, coronary artery bypass grafting (CABG) requires significant anticoagulation while on cardiopulmonary bypass during the procedure; risks and benefits should be weighed on a case-by-case basis.
NSTEMI
Non-ST-elevation myocardial infarction (NSTEMI) similarly is an uncommon presentation associated with neurologic disease, but more common than STEMI. NSTEMI evaluation is similar to the STEMI evaluation described above. The classic “MONA” pneumonic (morphine, oxygen, nitrate, aspirin) for initial treatment is recommended for all patients with angina symptoms in which there are no contraindications [34]. Unfortunately, while anticoagulation and antiplatelet therapy are mainstays of NSTEMI treatment they are often contraindicated in acute neurologic injury. Other treatments, such as beta-blockers and statins, are generally recommended if LV function is not acutely compromised and there are no contraindications from a neurologic standpoint [34]. Once antiplatelet agents are considered safe from a neurologic injury perspective, they should be initiated as soon as possible.
EKG Abnormalities and Arrhythmias
EKG Abnormalities
EKG abnormalities are seen in many, if not most, cases of severe acute neurologic injury. Almost all types of abnormalities have been reported [2, 16, 21, 35]. As already discussed, ST changes are quite common, either as elevations, depressions, or T-wave inversions. Heart block is also commonly seen. While first-degree heart block is the most common manifestation, type II Mobitz I and Mobitz II heart blocks can be seen and rarely type III [35]. Asystolic pauses, though rare, can also be seen post injury. “Cerebral T-waves” are a unique EKG abnormality that has been found after brain injury [2]. These are diffuse, inverted T waves that are very large and deep (Fig. 4.1). U waves, which appear after a T wave and typically are too subtle to detect on a normal EKG, have been reported to be prominent after some cases of acute neurologic injury. Finally, QT prolongation is also frequently seen after neurologic injury [2, 16, 21, 35]. Thus, one must be cautious in monitoring the use of QT-prolonging medications and the potential for developing torsades de pointes. EKG monitoring, sometimes daily if abnormalities are found, along with telemetry monitoring is important for diagnosis. Treatment goals include avoiding any medications that could exacerbate the EKG abnormalities observed and maintaining potassium and magnesium levels within high normal range. First-line treatment for torsades is continuous magnesium infusion. If significant abnormalities are found including high-degree heart block or prolonged asystolic pauses, then urgent consultation to cardiology may be warranted with consideration for pacemaker placement.
Arrhythmias
By far, the most common arrhythmia observed after neurologic injury is atrial fibrillation. Often atrial fibrillation is either a previously known diagnosis or a new diagnosis that can sometimes be the etiology of acute neurologic injury, such as ischemic stroke or anticoagulation-related hemorrhage. If atrial fibrillation is a new diagnosis, then it should be documented and addressed, especially in the setting of ischemic stroke; in these cases, this diagnosis will likely dictate ultimate medical management since the presence of atrial fibrillation increases ischemic stroke risk five-fold [36]. Atrial fibrillation can also result from the acute stress of neurologic injury or neurosurgery [36]. Diagnosis of atrial fibrillation is usually made using telemetry monitoring and should be confirmed with a 12-lead EKG. Initiation of anticoagulation is based upon the CHA2DS2-VASc score (≥2) balanced with bleeding risk (for which there are scores such as HAS-BLED; however, the utility of such scoring systems is controversial). The timing of anticoagulation initiation after an acute neurologic injury is based on each individual patient situation. The choice of long-term anticoagulant agent should also be patient-specific, and options include both warfarin and direct oral anticoagulant agents (e.g., apixaban, rivaroxaban, dabigatran, edoxaban). If a patient with atrial fibrillation develops rapid ventricular response, then intravenous beta-blockers or calcium channel blockers can be used as intravenous pushes and/or infusions as needed. In unstable patients, chemical or electrical cardioversion can be considered, but there is a risk that any residual cardiac thrombus may embolize.
Almost all forms of tachy- and brady-arrhythmias have been reported after neurologic injury and can be life-threatening. As already mentioned, torsades de pointes, third-degree heart block, and asystolic pauses can occur [2, 16, 21, 35]. Sustained monomorphic ventricular tachycardia can also be seen, especially in the setting of large intracranial hemorrhage. Cushing response is a classical triad that presents as hypertension, bradycardia, and hypoventilation. This triad is a marker of elevated intracranial pressure and, practically speaking, when all signs are present, is almost exclusively seen during active acute herniation. Immediate hyperosmolar therapy administration and consideration for surgical decompression is warranted in these cases. Direct treatment of the life-threatening arrhythmia should follow Advanced Cardiovascular Life Support (ACLS) guidelines.
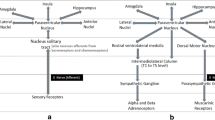
The pathophysiology behind EKG abnormalities and arrhythmias is due to multiple anatomic nodes of the “brain-heart connection.” The insula and brainstem are the most well-described hubs for such alterations [19, 22, 37]. The insular cortex has been long reported to be associated with arrhythmias, and even the presence of a laterality has been described (although controversial) [19, 38]; classically, the laterality is thought to be a sympathetic drive originating from right insular cortex activation and a parasympathetic drive originating from the left insular cortex. Brainstem compression can lead to any arrhythmia type, though based on Cushing phenomenon, thought to be more commonly presenting with bradycardia [22, 37].
Cardiac Arrest
Cardiac arrest can cause significant neurologic injury; the prognosis, evaluation, and management of neurologic recovery after cardiac arrest will be in part discussed in the “Therapeutic Hypothermia in Neurocritical Care” chapter. Neurologic injury that causes cardiac arrest is much less frequent, though it includes a broad range of pathologies such as intraparenchymal/intraventricular hemorrhage and seizures. Serious arrhythmias or extreme cardiomyopathy are the most likely modes by which cardiac arrest can occur. ACLS algorithms should be followed.
Pharmacology
Table 4.1 summarizes the major continuous infusions mentioned throughout the chapter used to treat patients with cardiac dysfunction induced after neurologic injury. The list provides classes of drugs and common dose ranges used clinically.
References
Cannon WB. “Voodoo” death. Am Anthropol. Wiley/Blackwell (10.1111). 1942;44(2):169–81.
Samuels MA. The brain-heart connection. Circulation. 2007;116(1):77–84.
Finsterer J, Wahbi K. CNS-disease affecting the heart: brain-heart disorders. J Neurol Sci Elsevier BV. 2014;345(1):8–14.
Ropper AH, Samuels MA, Klein JP. Adams and Victor’s: principles of neurology. New York: McGraw-Hill; 2014. p. 778–884.
Hemphill JC, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. American Heart Association, Inc. 2015;46(7):2032–60.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. American Heart Association, Inc. 2018;49(3):e46–99.
Ryken T, Hurlbert R, Hadley M, Aarabi B, Dhall S, Gelb D, et al. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery. 2013;72:84–92.
Biering-Sørensen F, Biering-Sørensen T, Liu N, Malmqvist L, Wecht JM, Krassioukov A. Alterations in cardiac autonomic control in spinal cord injury. Auton Neurosci Basic Clin. 2018;209:4–18.
Kilbourn KJ, Levy S, Staff I, Kureshi I, McCullough L. Clinical characteristics and outcomes of neurogenic stress cadiomyopathy in aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. Elsevier BV;. 2013;115(7):909–14.
Sato H, Tateishi H, Uchida T. Takotsubo-type left ventricular dysfunction due to multivessel coronary spasm. In: Kodama K, Haze K, Hori M, editors. Clinical aspects of myocardial injury: from ischemia to heart failure. Kagakuhyoronsha Publishing Co, Tokyo, Japan; 1990. p. 56–64.
Pelliccia F, Kaski JC, Crea F, Camici PG. Pathophysiology of takotsubo syndrome. Circulation. 2017;135(24):2426–41.
Kerro A, Woods T, Chang JJ. Neurogenic stunned myocardium in subarachnoid hemorrhage. J Crit Care. Elsevier Inc.; 2017;38:27–34.
Maréchaux S, Fornes P, Petit S, Poisson C, Thevenin D, Le Tourneau T, et al. Pathology of inverted takotsubo cardiomyopathy. Cardiovasc Pathol. 2008;17(4):241–3.
Cheah CF, Kofler M, Schiefecker AJ, Beer R, Klug G, Pfausler B, et al. Takotsubo cardiomyopathy in traumatic brain injury. Neurocrit Care. 2017;26(2):284–91.
Murthy SB, Shah S, Venkatasubba Rao CP, Suarez JI, Bershad EM. Clinical characteristics of myocardial stunning in acute stroke. J Clin Neurosci. Elsevier Ltd.; 2014;21(8):1279–82.
Krishnamoorthy V, Burkhard Mackensen G, Gibbons EF, Vavilala MS. Cardiac dysfunction after neurologic injury what do we know and where are we going? Chest. Elsevier Inc.; 2016;149(5):1325–31.
Sajeev J, Koshy A, Rajakariar K, Gordon G. Takotsubo cardiomyopathy and transient global amnesia: a shared aetiology. BMJ Case Rep. 2017;2017:10–2.
Nasr DM, Tomasini S, Prasad A, Rabinstein AA. Acute brain diseases as triggers for stress cardiomyopathy: clinical characteristics and outcomes. Neurocrit Care. Springer US;. 2017;27(3):356–61.
Mazzeo AT, Micalizzi A, Mascia L, Scicolone A, Siracusano L. Brain-heart crosstalk: the many faces of stress-related cardiomyopathy syndromes in anaesthesia and intensive care. Br J Anaesth. The Author(s);. 2014;112(5):803–15.
Goldfinger JZ, Nair A, Sealove BA. Brain-heart interaction in takotsubo cardiomyopathy. Heart Fail Clin. Elsevier Inc.; 2013;9(2):217–23.
Koppikar S, Baranchuk A, Guzmán JC, Review MCA. Stroke and ventricular arrhythmias. Int J Cardiol. Elsevier Ireland Ltd.; 2013;168(2):653–9.
Grunsfeld A, Fletcher JJ, Nathan BR. Cardiopulmonary complications of brain injury. Curr Neurol Neurosci Rep. 2005;5(6):488–93.
Budnik M, Kochanowski J, Piatkowski R, Wojtera K, Peller M, Gaska M, et al. Simple markers can distinguish takotsubo cardiomyopathy from ST segment elevation myocardial infarction. Int J Cardiol. Elsevier Ireland Ltd.; 2016;219:417–20.
Gopalakrishnan P, Zaidi R, Sardar MR. Takotsubo cardiomyopathy: pathophysiology and role of cardiac biomarkers in differential diagnosis. World J Cardiol. 2017;9(9):723–30.
Reeder G, Prasad A. Management and prognosis of stress (takotsubo) cardiomyopathy. In: Melin J, editor. Waltham, MA: UpToDate Inc.; 2018.
Mrozek S, Srairi M, Marhar F, Delmas C, Gaussiat F, Abaziou T, et al. Successful treatment of inverted Takotsubo cardiomyopathy after severe traumatic brain injury with milrinone after dobutamine failure. Hear Lung J Acute Crit Care. Elsevier Inc.; 2016;45(5):406–8.
Morris NA, Manning N, Marshall RS, Connolly ES, Claassen J, Agarwal S, et al. Transcranial Doppler waveforms during intra-aortic balloon pump counterpulsation for vasospasm detection after subarachnoid hemorrhage. Neurosurgery. 2018;83(3):416–21.
Al-Mufti F, Morris N, Lahiri S, Roth W, Witsch J, Machado I, et al. Use of intra-aortic- balloon pump counterpulsation in patients with symptomatic vasospasm following subarachnoid hemorrhage and neurogenic stress cardiomyopathy. J Vasc Interv Neurol. 2016;9(1):28–34.
Howell MD, Davis AM. Management of sepsis and septic shock. JAMA. 2017;317(8):847–8.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017;45:486–552.
Venkatesh B, Finfer S, Cohen J, Rajbhandari D, Arabi Y, Bellomo R, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med. 2018;378(9):797–808.
Annane D, Renault A, Brun-Buisson C, Megarbane B, Quenot J-P, Siami S, et al. Hydrocortisone plus fludrocortisone for adults with septic shock. N Engl J Med. 2018;378(9):809–18.
Colwell C, Moreira M, Grayzel J. Initial management of moderate to severe hemorrhage in the adult trauma patient. In: Melin J, editor. Waltham, MA: UpToDate Inc.; 2018.
Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. American Heart Association, Inc.;. 2014;130(25):e344–426.
Katsanos AH, Korantzopoulos P, Tsivgoulis G, Kyritsis AP, Kosmidou M, Giannopoulos S. Electrocardiographic abnormalities and cardiac arrhythmias in structural brain lesions. Int J Cardiol. Elsevier Ireland Ltd.; 2013;167(2):328–34.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, et al. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on practice guidelines and the heart rhythm society. Circulation. 2014;2014:199–267.
Tahsili-Fahadan P, Geocadin RG. Heart-brain axis: effects of neurologic injury on cardiovascular function. Circ Res. 2017;120(3):559–72.
Nagai M, Hoshide S, Kario K. The insular cortex and cardiovascular system: a new insight into the brain-heart axis. J Am Soc Hypertens. Elsevier Ltd.; 2010;4(4):174–82.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kim, J.A., Izzy, S. (2020). Cardiac Complications in Neurocritical Care Patients. In: Nelson, S., Nyquist, P. (eds) Neurointensive Care Unit. Current Clinical Neurology. Humana, Cham. https://doi.org/10.1007/978-3-030-36548-6_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-36548-6_4
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-36547-9
Online ISBN: 978-3-030-36548-6
eBook Packages: MedicineMedicine (R0)