Abstract
Infectious agents, and especially viruses, can induce severe forms of acute and chronic lymphocytic myocarditis which may progress to heart failure. The diagnosis of infectious myocarditis in endomyocardial biopsies (EMB) is guided by the detection of viral RNA and DNA using molecular tools such as quantitative (RT-) polymerase chain reaction and in situ hybridization in association with acute and chronic cardiac inflammation. Enteroviruses, parvovirus B19 (B19V), and herpesviruses, i.e., Epstein–Barr virus (EBV), human herpesvirus-6 (HHV6), are most often detected in EMB of patients with myocarditis and dilated cardiomyopathy. Meanwhile it is known that the outcome and course of myocarditis are influenced by genetic host factors as well as by the viral pathogenicity which considerably differs in the various infections. A considerable portion of our knowledge about the etiopathogenetic mechanisms in viral heart disease is derived from animal studies. By investigation of immunocompetent and gene-targeted mice valuable new insights into host and virus factors relevant for the control of cardiac viral infection and inflammation were gained which are reviewed in this paper.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
5.1 Introduction
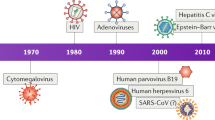
In endomyocardial biopsies of patients with acute and chronic forms of myocarditis a variety of RNA and DNA viruses have been detected by molecular biological techniques such as in situ hybridization and nested or quantitative (RT)-PCR. Besides enteroviruses (EV), including coxsackieviruses of group B (CVB), parvovirus B19 (B19V), human herpesvirus-6 (HHV6), and Epstein–Barr virus (EBV) were found in a significant number of patients with myocarditis [1,2,3,4,5]. In addition, genomes of other virus infections including adenoviruses (ADV), influenza viruses, HIV, human herpesvirus type 1 (HSV1), and human cytomegalovirus (CMV) were amplified by (RT-) PCR in inflamed hearts [6, 7]. However, whereas the aetiopathogenetic role of enteroviruses and especially of CVB in the induction and progression of acute myocarditis to postviral cardiomyopathy was substantially confirmed by observations in CVB3-infected mice, it is rather unclear by which mechanisms herpesviruses, adenoviruses, or parvovirus B19 might contribute to cardiac damage and inflammation.
In order to improve the knowledge about the pathophysiology of viral myocarditis diverse animal models of DNA and RNA virus infections have been established. By investigation of infected immunocompetent as well as gene-targeted mice valuable new insights into virus pathogenicity and the host immune response were gained. It is important to note that considerable differences in the outcome and course of myocarditis in dependency of virus-induced pathogenicity and genetic factors of the host are present in these animal models (Fig. 5.1; for review see [8]). Thus, it is highly probable that also the different course of myocarditis in humans is determined by individual immune reactions on infection of specific cardiac cell types by the various RNA and DNA viruses. By means of light and electron microscopic in situ hybridization experiments it was possible to allocate specific virus infections to particular cardiac cell types in the human heart as well as in murine hearts [9, 10]. Coxsackieviruses belonging to the enteroviruses were found to infect primarily cardiomyocytes and due to extensive virus replication a rapid cytolysis of these cells occurs [11]. The consecutive antiviral immune response which involves NK cells, macrophages, and CD4+ and CD8+ T lymphocytes aims to eliminate CVB from the myocardium and is successful in most humans but some patients develop a chronic myocarditis on the basis of viral genome persistence [9]. At later stages of the disease, the virus-induced cytolysis may also trigger autoimmune reactions which are primed by the release of specific cellular antigens from necrotic myocytes such as to beta1-adrenergic receptors [12], myosin, or M2 muscarinic receptors which have also been observed in some animal models of myocarditis [13]. Further studies are needed to address the contribution of autoimmune reactions in comparison to those induced by persistent virus infections in the outcome of viral heart disease.
Heart tissue sections of a susceptible ABY/SnJ obtained 2 weeks after infection with coxsackievirus B3 (CVB3) reveal massive calcification (Kossa staining) in areas of necrotic myocytes (HE) and ongoing inflammation as detected by MAC-3+ macrophages and CD3+ T lymphocytes (a). CVB3 replication in myocytes during acute infection as detected by radioactive in situ hybridization, cardiac damage, and inflammation is extensive in susceptible ABY/SnJ (H-2b) mice compared to resistant C57BL/6 (H-2b) mice which do not get a chronic myocarditis (b)
In contrast to enteroviruses, all other viruses often detected in the human heart cannot infect myocytes, e.g., due to absence of the correspondent viral receptors. Instead, some cardiotropic viruses infect exclusively endothelial cells as we have shown by radioactive in situ hybridization for B19V. This virus was exclusively found in endothelial cells of children and adult patients with myocarditis (Fig. 5.2). On the other hand herpesviruses including HHV6 and EBV which also do not infect cardiomyocytes were detected in cardiac inflammatory cells (macrophages, T or B lymphocytes) in patients with myocarditis (Fig. 5.2). Thus, numerous cardiotropic viruses do not damage the heart via cytolysis of cardiomyocytes but most likely via expression of cardiotoxic chemokines and cytokines from infected endothelial or immune cells, contributing to further attraction of potentially harmful immune cells into the heart. It is known that, e.g., HHV6 may induce the expression of the pro-inflammatory cytokine IL-6 which is decisive for the invasion of T cells into infected organs [14]. In order to delineate the differences of the cellular and molecular mechanisms in acute and chronic myocarditis induced by different viral triggers various animal models are discussed in the following chapters.
Radioactive in situ hybridization demonstrates the localization of viral genomes in different cardiac cell types in patients with acute myocarditis (virus genomes are indicated by black silver grains). Coxsackieviruses infect mainly cardiomyocytes, whereas parvovirus B19 DNA is exclusively found in endothelial cells. Nucleic acids of Epstein–Barr virus and human herpesvirus-6 are present in interstitial immune cells (T cells, B cells, macrophages) but not in cardiomyocytes
5.2 Murine Models of Coxsackievirus Myocarditis
The murine model of CVB3 myocarditis is by far the most thoroughly investigated animal model of viral myocarditis as genetically diverse mouse strains perfectly reflect the different course of enteroviral myocarditis in patients (Fig. 5.1) [15]. The induction of enteroviral myocarditis is mediated by the entry of the virus into the cardiomyocytes via internalization using the transmembrane receptor CAR (coxsackievirus and adenovirus receptor) (CAR) and the deflecting protein decay accelerating factor (DAF) as a coreceptor. CVB are able to lyse myocytes in vitro and in vivo very quickly due to pronounced viral replication as shown in Fig. 5.1 [10, 11]. In CVB3-infected mice myocytolysis due to virus replication was proven by electron microscopic in situ hybridization studies, demonstrating replicative RNA intermediates in close spatial association with vacuoles within myocytes [10]. Transgenic mice which express a replication-competent but not infectious full-length CVB3 cDNA reveal severe loss of myocytes and scarring, indicating that expression of viral proteins mediates cardiac dysfunction [16].
A decisive molecular mechanism by which enteroviruses contribute to the pathogenesis of myocarditis was described by Badorff et al. [17], demonstrating that CVB3 cleaves dystrophin via the viral proteinase 2A resulting in the disruption of cytoskeleton in myocytes. More recently, the intracellular protein degradation systems comprising the ubiquitin-proteasome and lysosome pathways have been identified as crucial factors of virus infectivity. Luo et al. [18] demonstrated that treatment of cells with proteasome inhibitors significantly decreased virus titers and prevented virus-induced cell death. Moreover, the virus-induced pro-inflammatory cytokine and chemokine production was found to be prevented by ONX 0914, an immunoproteasome-specific inhibitor [19].
As a consequence of viral replication in myocytes, the innate immune response is triggered. Pro-inflammatory cytokines such as interleukin-1 (IL-1), IL-6, tumor necrosis factor (TNFα), and interferons (type I and II) are released from resident cardiac cells, which consecutively activate macrophages. Also, the NLRP3 activity was enhanced during early stage of CVB3 infection, as evidenced by increased gene expression and/or secretion of IL-1β and caspase-1. NLRP3 and its upstream serine/threonine-protein kinase receptor-interacting protein 1/3 are degraded via the proteolytic activity of virus-encoded proteinases, thus counteracting the host defense response against CVB3 [20]. When IL-1ß in CVB3-infected mice is depleted, a reduction of cardiac inflammation and fibrosis is noted during the acute but also during the chronic phase of myocarditis in presence of persistent virus infection [21].
A major impact for the course of the disease emerged to be the type I interferon system. CVB3-infected type I-IFNR-deficient mice died within 2–4 days post infection [22]. In mice deficient for IFN-beta a downregulation of IFN-stimulated gene targets as well as increased cardiomyocyte injury was noted [23]. A disease-phase dependent role of interferon (IFN) regulatory factor 7 (IRF7) was suggested to robust IFN-beta induction in acute CVB3 myocarditis [24]. Various TLRs which are expressed on immune cells, comprising natural killer (NK) cells, dendritic cells (DCs), and macrophages have been implicated to be involved in the early immune response against enteroviruses. During acute CVB3-induced myocarditis Tlr2, Tlr3, Tlr6, Tlr7, and Tlr9 displayed by far the highest increase of mRNA expression during acute disease [24]. CVB3-infected TLR3-knockout (ko) mice developed a severe ongoing myocarditis underlining the view that TLR3 plays a central role in the effective control of the infection [25]. TLR3 signaling in DCs and in other cells was found to be relevant for the activation and polarization of the CD4+ T lymphocyte response toward a Th1 profile and, consequently for a better outcome of CVB3 infection [26]. Monocytes, macrophages, dendritic cells express the colony-stimulating factor 1 receptor (CSF-1R). CSF-1R signaling screws mature monocytes into a pro-inflammatory state. Silencing the CSF-1 axis by siCSF-1 inverted virus-mediated immunopathology as reflected by lower troponin T levels, a reduction of accumulating myeloid cells in heart tissue and improved cardiac function [27].
Following the activation of the innate immunity, the adaptive immune response evolves around 6 days post infection (pi) (Fig. 5.1). As shown in CVB3-infected beta-2 microglobulin- [28] and CD8-deficient mice [29] the severity of disease was magnified, demonstrating protective effects of CD8+ T cells in the propagation of viral myocarditis. Dependent on the genetic background, susceptible animals such as A/J, ABY/SnJ, ASW/J, SWR/J, Balb/c develop a chronic myocarditis which may last for several months [15]. The failure to resolve viral RNA from the heart can be deleterious and results in ongoing myocarditis [15]. However, when the virus is completely cleared as observed in C57BL/6 mice 2 weeks pi, the downregulation of the inflammation in the heart occurs which is mediated by the production of anti-inflammatory cytokines such as transforming growth factor beta (TGFβ) and IL-10 by regulatory T cells and alternatively activated (M2) macrophages [30]. Adoptive Treg transfer in the inflammatory phase of CVB3 myocarditis was found to protect the heart against inflammatory damage and fibrosis via modulation of monocyte subsets [31]. Susceptible mice revealing chronic inflammation were found to have a delayed IFN-γ secretion and a highly diminished IL-10 production [32]. Findings in IL-10-deleted mice confirmed the regulatory role of IL-10 in the outcome of CVB3 myocarditis [32]. Recently, Li et al. [33] showed that the protection of female mice to excessive cardiac damage in the coxsackieviral mouse model is attributed to a larger presence of M2 macrophages in comparison to male mice. The consequences of chronic inflammation following CVB3 infection are cardiac fibrosis with remodeling of the extracellular matrix (EMC), which may finally result in dilated cardiomyopathy and heart failure. Important regulators of the ECM are matrix metalloproteinases (MMPs) which can degrade the different components in the interstitium. MMP-2, MMP-9, and MMP-12 transcription was increased during acute myocarditis, the tissue inhibitors of metalloproteinases-3 (TIMP-3) and TIMP-4 expression were found to be downregulated, indicating that cardiac remodeling is at least partially mediated via activation of MMPs [34]. Another protein that has been described to be involved in inflammatory responses and in the maintenance or reconfiguration of tissue integrity is osteopontin (OPN). In contrast to resistant C57BL/6 and OPN gene-deficient mice, transcription levels of matrix metalloproteinase-3, TIMP1, urokinase-type plasminogen activator (uPA), and transforming growth factor (TGF) beta1 were elevated in susceptible mice, and as a consequence, procollagen-1 mRNA expression and fibrosis were considerably enhanced but could be successfully treated with a vitamin D analog [35]. In addition to OPN [21] also connective tissue growth factor (CTGF), a member of the CCN protein family was found to be associated with the development of fibrosis in ongoing enteroviral myocarditis. CTGF which is known to be basically mediated by TGF-β was found to be extensively upregulated in CVB3-infected susceptible mice [36]. Interestingly, the matricellular protein Cyr61, another CCN protein was found not only to be linked with tissue repair but also to function as a modulator of immune cell migration as shown in a murine model of autoimmune myocarditis. The CCN1-driven modulation of immune cell migration is mimicked in part by cyclic RGD peptides which might offer a therapeutic option for the treatment of inflammatory heart diseases [37].
5.3 Murine Models of Encephalomyocarditis Virus Myocarditis
Encephalomyocarditis virus (EMCV) is another single-stranded picornavirus of the Enterovirus genus which has been studied to evaluate pathogenetic mechanisms in enteroviral myocarditis. Similar to CVB, EMCV was found to induce a necrotic myocarditis in mice but was also detected in the heart of young Rhesus macaques [38]. Whether transmission of EMCV to humans occurs is unclear. However, in 2009 EMCV was obviously isolated in two patients with fever, nausea, headache, and dyspnea supporting a role for EMCV in human infection and febrile illness [39].
In order to identify molecular mechanisms in EMCV myocarditis, mice lacking functional TLR3 were investigated. Correspondent to findings in CVB3-infected TLR3 ko mice [25], EMCV-infected TLR3 ko mice were found to be unable to control the proliferation of EMCV, subsequently resulting in increased cytopathogenic effects in cardiac myocytes and early death. The findings in this study implicate the importance of TLR3 signaling and antiviral effects of TNF-alpha and IL-6 in the very early stages of the heart disease [40]. On the other hand, it is well known that inflammatory cytokines including TNF-alpha may accelerate the pathology of EMCV-myocarditis and negatively influence the cardiac function [41]. Most recently, depletion of CD103+ conventional dendritic cell (cDC) was found to abrogate antigen-specific CD8+ T cell proliferative expansion, transforming subclinical cardiac injury to overt heart failure [42].
5.4 Murine Models of Reovirus Myocarditis
Reoviruses which are enteric non-enveloped viruses with a double-stranded RNA genome have been widely used as model systems to study viral pathogenesis in the central nervous system, liver, and heart. The morphology of reovirus-induced myocarditis is generally characterized by mild inflammatory infiltrates but extensive myocardial necrosis. Comparable to findings in coxsackievirus infections, also, reovirus was found to induce a myocarditis in severe combined immunodeficient (SCID) mice, illustrating that reovirus myocarditis is primarily not an immune-mediated disease [43]. Correspondent to observations in CVB3 myocarditis [15) the extent of viral RNA synthesis during replication but not generation of infectious virus was found to be a determinant of reovirus-induced acute myocarditis [44].
Differences in the tropism and virulence have been linked to sensitivity of type I interferons [45]. The retinoic acid inducible gene I (RIG-I) and the RIG-I adaptor were found to be necessary for the activation of antiviral transcription factors including interferon regulatory factor 3 (IRF-3) and NF-κB [46]. The spontaneous activation of a mitochondrial antiviral signaling (MAVS) pathway in cardiac myocytes but not cardiac fibroblasts or skeletal muscle cells was found to determine high basal interferon-β expression in the heart [47].
5.5 Animal Models of Parvovirus Myocarditis
Human parvovirus B19 (B19V), the only human pathogenic parvovirus, is the causative agent of a wide spectrum of human diseases, including fifth disease (erythema infectiosum), hydrops fetalis in pregnant women, and transient aplastic crisis in patients. Numerous reports demonstrating the presence of B19V in the heart of patients with acute and chronic myocarditis further suggest that this virus may be associated with inflammatory heart disease. Our current understanding about the mechanisms by which B19V regulates disease progression is rather limited, also due to the lack of adequate animal models as infection of mice with B19V does not induce myocarditis. Interestingly, immunization of BALB/c mice with B19V VP1-unique region was found to result in dilated cardiomyopathy with cardiac fibrosis and progressive dilatation of left ventricle [48]. Recently, it was shown that parvovirus B19V non-structural protein-1 (NS-1) induced apoptotic bodies may elicit inflammation and degeneration in murine hearts [49]. Also, parvovirus B19-induced vascular damage in the heart was demonstrated to be associated with elevated circulating endothelial microparticles (EMPs) as detected in transgenic B19V-NS1-mice [50].
5.6 Murine Models of Herpesvirus Myocarditis
Epstein–Barr virus has been observed in the hearts of up to 8% of the patients with inflammatory heart disease [1]. The processes explaining cardiac inflammation and injury in EBV infection are uncertain mainly due to the absence of suitable animal models [51]. One animal model which might mimic in some aspects human EBV infection is infection of mice with the murine gamma herpesvirus MHV-68. Both viruses can induce a latent infection of B cells [52]. With regard to myocardial infection MHV-68 seems to replicate in the heart of immunocompetent mice showing a maximum replication between 5 and 10 days. Myocardial necrosis and focal inflammation, consisting mainly of T lymphocytes, occur after 10–12 days and 33–35 days, respectively. B- and T-cell deficient B6-(Rag1)™ mice revealed high myocardial viral loads but no myocardial necrosis, indicating that viral replication is not sufficient to explain myocardial damage. However, in this model it is still unclear which cells are infected in the heart and which molecular mechanisms lead to myocardial necrosis in BALB/c mice but not in C57BL/6 [52].
The evolvement of myocarditis has also been reported in mice infected with another herpesvirus, the murine cytomegalovirus (MCMV) [53]. The hearts of MCMV-infected BALB/c mice were found to be more susceptible than those of C57BL/6 for cardiac infiltration, which mainly consist of CD8+ and CD4+ T cells, macrophages, B cells, and neutrophils. In this model MCMV titres in the heart were low and replicative virus could not be isolated beyond the first week pi. Correspondent to human infection with cytomegalovirus (HCMV), also in cardiac MHV-68 and MCMV infection the direct lysis of myocytes due to virus replication in vivo was not proven [53]. In another study of MCMV-induced myocarditis in BALB/c mice it was shown that myocarditis-related pathological changes and increase in viral load were greatest at day 8 p.i., corresponding with peak cytokine transcription of TNF-alpha, IL-6, and IFN-γ, as well as of IL-10 mRNA transcripts [54]. Interestingly, treatment of MCMV-infected mice with IFNA6, A9, and B inhibited acute myocarditis, and IFNA6 was even found to reduce chronic cardiac inflammation, supporting the hypothesis that acute MCMV myocarditis does not reflect virus load but rather the immunomodulatory responses to this infection [55].
5.7 Molecular Diagnosis in Patients
Myocarditis in humans—a frequent cause of dilated cardiomyopathy and sudden cardiac death—typically results from cardiotropic viral infection followed by active inflammatory destruction of the myocardium. Advances in molecular detection of viruses by endomyocardial biopsy have improved our ability to diagnose and understand the pathophysiological mechanisms of this elusive disease, which have been summarized in 2013 by Klingel and Pankuweit [56]. Here, we present a condensed and updated summary of this review.
The diagnosis of virus-associated myocarditis was clearly facilitated by the introduction of endomyocardial biopsy techniques by Sakakibara and Konno in 1962 [57] in addition to the development of polymerase chain reaction (PCR) by Mullis et al. in 1982 [58]. The combination of both methods allowed for the first time the detection of viral genomes directly within the affected myocardial tissue in a patient with suspected myocarditis. A wide range of different PCR assays have been developed, which are suitable to identify different cardiac RNA and/or DNA viruses with a higher sensitivity in comparison to standard immunohistochemical methods used for the detection of viral proteins (for review [56, 59,60,61,62]).
By these molecular approaches enteroviruses have been identified as highly relevant pathogenic agents in myocarditis [63,64,65,66,67,68,69,70,71]. Moreover, the presence of genomes from adenoviruses (ADV), parvovirus B19 (B19V) [72], herpesviruses (human herpesvirus 6 (HHV6), cytomegalovirus (CMV), Epstein–Barr virus (EBV), herpes simplex virus type 1 (HSV1) [73], chlamydia pneumoniae [74], Borrelia burgdorferi [75, 76], as well as other infectious agents [77] was reported in patients with inflammatory heart disease.
One of the major problems associated with the analysis of cardiotropic agents by PCR is the fact that this technique only allows the detection of viral genomes without differentiating potentially infected cardiac cell types. In addition, active replication of the virus is generally not investigated by PCR [9]. Thus, in order to substantiate the etiopathogenetic role of an infectious agent, PCR must be carefully evaluated in the context of clinical, and histological and immunohistochemical findings of endomyocardial biopsies.
To overcome this diagnostic gap the in situ hybridization technique was established, which is capable to attribute viral sequences to specific cells types in the heart as illustrated in Fig. 5.2 and Table 5.1. Also, as shown for coxsackieviruses in situ hybridization allows the detection viral plus-strand RNA as well as the replicative minus-strand RNA intermediates, which are of particular interest for the diagnosis of active myocardial infections [9, 65,66,67, 78].
Starting from 2002, fluorescence-based real-time PCR assays were established for the evaluation of the viral load in the heart. Regarding the quantification of B19V genomes, real-time PCR assays have been developed for the use of the LightCycler system [79], fluorescence resonance energy transfer probes [80] as well as for the ABI Prism system [81, 82].
5.8 Prevalence of Cardiotropic Viruses in Endomyocardial Biopsies Assessed by Molecular Tools
Viral genomes were identified in a varying subset of patients with acute and chronic myocarditis and DCM, but the impact of these viral genomes on cardiac function and clinical outcome is still controversial [83]. The overall prevalence of cardiotropic viruses amplified by (RT-) PCR in endomyocardial biopsies of these patients differs widely: enteroviral genomes were detected in 3–53%, cytomegalovirus DNA in 3–40%, and adenoviruses in 3–23% in the myocardium of patients with inflammatory heart disease. In addition to the previous summaries [56, 59], the wide range of results that have been obtained by different molecular methods were summarized as follows with regard to the most prevalent cardiotropic viruses such as HHV6, EBV, and B19V.
5.9 Prevalence of Parvovirus B19 Genomes in Patients with Myocarditis and DCM
Investigations in adult patients with inflammatory heart diseases revealed a prevalence of B19V DNA in 19.5% of patients with myocarditis, 23% in patients with DCMi, and 16% in patients with DCM [84]. Prevalences for PVB19 genomes detected in patients with myocarditis or DCM ranged from 11–56% in patients with myocarditis and 10–51% in patients with DCM. As reported for enteroviruses also persistence of B19V in patients with LV dysfunction was found to be associated with a progressive impairment of LVEF [2]. In contrast to enteroviruses, spontaneous virus elimination of B19V was observed in only 22% of patients. These results suggest that persisting cardiac viral infections may constitute a major cause of progressive LV dysfunction in patients with past myocarditis or DCM. Interestingly, it was shown in 24 patients presented with acute onset of angina pectoris and ST-segment elevations or T-wave inversion mimicking acute myocardial infarction, that histological analysis excluded mostly active or borderline myocarditis, but B19V, EV, and ADV genomes were detected in the myocardium of 12, three, and two patients, respectively [85]. Here, virus genomes were found in 71% of patients with normal coronary anatomy, clinically mimicking acute myocardial infarction, an observation which was first published in a patient with lethal myocarditis by Bültmann et al. [86]. In this female patient with clinical signs of myocardial infarction and histopathological fulminant myocarditis in situ hybridization studies of the autopsy heart revealed the presence of B19V genomes exclusively in endothelial cells of the smaller intramyocardial vessels. Immunohistochemical stainings exhibited marked expression of E-selectin on endothelial cells, a finding indicative of endothelial dysfunction. These processes are likely to lead to disturbances in the coronary microcirculation and may explain the observation that many patients with B19V-associated myocarditis present with the clinical signs that are typical of ischemic heart disease.
However, the causal relationship of B19V infections to cardiac disease has been questioned, mainly because epidemiological data demonstrated a lifelong persistence of B19V genomes in various organs, apart from the heart [87, 88] and the fact, that B19V DNA was also detected in heart tissue from patients without clinical manifestations of inflammatory cardiomyopathy [89,90,91].
Nevertheless, parvovirus replication in myocardial endothelial cells was substantiated by the detection of B19V RNA replicative intermediates in the myocardium only in acutely inflamed hearts, whereas viral RNA was not detected in chronic dilated cardiomyopathy without inflammation or in control hearts [4]. On the basis of these data, it was suggested that viral loads of more than 500 genome equivalents per microgram isolated nucleic acid in endomyocardial biopsies are the clinically relevant threshold for the maintenance of myocardial inflammation.
In a recent publication with human samples, it was shown that endothelial derived microparticles were significantly different in B19V+ compared to B19V− patients and human controls, with an increase of apoptotic but not activated endothelial microparticles [50]. Other microparticles such as platelet-, leukocyte-, and monocyte-derived microparticles showed less specific patterns, indicating that differences in the subtypes of microparticles can be attributed to specific myocardial virus infections.
However, the molecular mechanisms responsible for a possible reactivation of B19V, the influence of the immune system triggering B19V replication and immune-independent viral pathogenesis in uninflamed hearts are the remaining gaps in our understanding of B19V pathogenicity in heart diseases [4].
5.10 Prevalence of Epstein–Barr Virus and Human Herpesvirus 6 and in Patients with Myocarditis and DCM
In immunocompetent patients, herpesviruses including EBV and HHV6 infections rarely induce cardiac symptoms. For example, EBV-linked acute pericarditis or myocarditis is only reported in some immunocompetent patients [92,93,94]. Also, HHV6-induced myocarditis has been published in a low number of patients, but sometimes with a fatal outcome [95, 96]. Investigation of autopsy material showed diffuse myocarditis with a granulocytic and monocytic infiltrate, necrotizing arteritis of the coronary arteries, and fulminant hepatitis with microvesicular steatosis and necrosis together with the detection of HHV6 genome in heart, liver, lung, and spleen [95]. In the larger series of patients with inflammatory heart diseases analyses for HHV6 and EBV were always included. Prevalences for HHV6 genomes detected in patients with myocarditis or DCM ranged from 8 to 20% and for EBV genomes from 0 to 8%. Nevertheless, the pathophysiological mechanisms of herpesviruses in acute myocarditis and especially the possible relevance of HHV-6 reactivation for the development of chronic cardiomyopathies remain to be assessed.
5.11 Prevalence of Influenza Virus RNA in Patients with Myocarditis and DCM
Last but not least several cases of acute myocarditis especially in juvenile patients have been reported in association with pandemic H1N1 influenza virus infections. Genomes of Influenza A/H1N1 virus were detected by RT-PCR analysis in blood as well as in myocardial tissue in patients with a lethal influenzavirus infection, however virus replication was not observed in heart muscle cells [6]. Nevertheless, fulminant myocarditis caused by H1N1 infection seems to be a rare but severe and often lethal complication not only in children [97, 98].
5.12 Prevalence of Double or Multiple Infections
In larger series of patients with myocarditis and dilated cardiomyopathy investigated by Kühl et al. [99] and Kandolf et al. [100] it has been shown that the detection of two or more cardiotropic viruses by PCR in the myocardium is rather common. In a series of 245 patients with DCM multiple infections were found in 27.3% of patients. Most often, HHV6 + B19V (10.6% of cases) and B19V + EV (3.7% of cases) genomes were amplified in parallel by PCR [99]. Comparably, in a published study of 3219 patients with cardiac dysfunction and suspected myocarditis, in 11.6% of the patients HHV6 and B19V genomes were concurrently detected in the heart [100]. However, there are no data available, whether clinical symptoms or cardiac histopathology differ in patients with multiple infections or whether prognosis in those patients is worse or different when compared to patients with only one virus type in the heart.
5.13 Diagnostic Implications
There is convincing evidence from animal models and investigations in humans that viral infections may induce a significant damage of the myocardium through direct virus-mediated injury of cardiomyocytes and secondary immune reactions, finally leading to chronic myocarditis and dilated cardiomyopathy. In addition, viral endomyocardial infections have also been reported as an independent predictor of graft loss in pediatric cardiac transplant recipients [101].
As a consequence from the investigations performed over more than 20 years the position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases with regard to “Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis” was initiated [102]. There it is stated that the endomyocardial biopsy is the “gold standard” to diagnose myocarditis and should be performed early in the course of the disease to optimize diagnostic accuracy and reduce sampling error especially in focal myocarditis. Endomyocardial biopsy confirms the diagnosis of myocarditis and identifies the underlying etiology and the type of inflammation, which imply different treatments and prognosis [103,104,105,106]. Multiple specimens should be taken and immediately fixed in 10% buffered formalin at room temperature for light microscopy; additional 1–2 samples should be snap frozen in liquid nitrogen and stored at −80 °C or stored in RNA later tubes at room temperature for viral PCR [102, 103]. To increase the diagnostic sensitivity of myocarditis, immunohistochemistry is mandatory for the identification and characterization of the inflammatory infiltrate [102, 106, 107]. In addition to routine stainings (hematoxylin/eosin, Giemsa, Masson trichrome), immunohistochemistry is required to demonstrate infiltrating cells by applying antibodies specific for T and B lymphocytes, macrophages, major histocompatibility class 1 and class 2 antigens. Diagnosis of myocarditis in EMB requires ≥14 leucocytes/mm2 in the interstitium [102].
The diagnostic contribution of EMB is significantly enhanced by molecular analysis with DNA/RNA extraction and (RT-) PCR amplification of viral genomes [102, 105, 107]. In this context it is worthy to note that patients with enterovirus myocarditis must not be treated by an immunosuppressive therapy comprising corticosteroids. In order to exclude systemic infection, peripheral blood should be investigated in parallel with EMB [102, 107]; quantification of virus load and determination of virus replication may add diagnostic value [4, 102]. For the detection of cardiotropic viruses total DNA and RNA should be extracted from the heart tissue samples. Primer pairs specific for enteroviruses, parvovirus B19 (B19V), cytomegalovirus (CMV), influenzaviruses (A, B), human herpesvirus-6 (HHV6) and Epstein–Barr virus (EBV) should be used to perform polymerase chain reaction (RT-) PCR, including quantitative real-time PCR in case of PVB19. These investigations are required to investigate, e.g., the success of an antiviral therapy.
Last but not least, as an innovative approach, next-generation sequencing was recently evaluated for detecting potential pathogens of acute myocarditis from sera [108]. In this small investigation virus-derived sequences were identified in seven of 17 cases, and the presence of viruses was confirmed by PCR or antigen testing in four patients. So far, the relationship between sequencing results and myocarditis remains to be clarified, but a NGS-based approach may have the potential to detect different viral pathogens and contribute to the clarification of the etiology of acute myocarditis.
References
Kindermann I, Kindermann M, Kandolf R, Klingel K, Bültmann B, Müller T, et al. Predictors of outcome in patients with suspected myocarditis. Circulation. 2008;118(6):639–48.
Kühl U, Pauschinger M, Seeberg B, Lassner D, Noutsias M, Poller W, Schultheiss HP. Viral persistence in the myocardium is associated with progressive cardiac dysfunction. Circulation. 2005;112(13):1965–70.
Trachtenberg BH, Hare JM. Inflammatory cardiomyopathic syndromes. Circ Res. 2017;121(7):803–18.
Bock CT, Klingel K, Kandolf R. Human parvovirus B19-associated myocarditis. N Engl J Med. 2010;362(13):1248–9.
Ruppert V, Meyer T, Balbach A, Richter A, Müller HH, Maisch B, Pankuweit S, German Heart Failure Network. Genotype-specific effects on left ventricular function in parvovirus B19-positive patients with dilated cardiomyopathy. J Med Virol. 2011;83(10):1818–25.
Gdynia G, Schnitzler P, Brunner E, Kandolf R, Bläker H, Daum E, Schnabel P, Schirmacher P, Roth W. Sudden death of an immunocompetent young adult caused by novel (swine origin) influenza A/H1N1-associated myocarditis. Virchows Arch. 2011;458(3):371–6.
Barbaro G. HIV-associated myocarditis. Heart Fail Clin. 2005;1(3):439–48. Review.
Esfandiarei M, McManus BM. Molecular biology and pathogenesis of viral myocarditis. Annu Rev Pathol. 2008;3:127–55. Review.
Klingel K, Sauter M, Bock CT, Szalay G, Schnorr JJ, Kandolf R. Molecular pathology of inflammatory cardiomyopathy. Med Microbiol Immunol. 2004;193(2–3):101–7.
Klingel K, Rieger P, Mall G, Selinka HC, Huber M, Kandolf R. Visualization of enteroviral replication in myocardial tissue by ultrastructural in situ hybridization: identification of target cells and cytopathic effects. Lab Investig. 1998;78(10):1227–37.
McManus BM, Chow LH, Wilson JE, Anderson DR, Gulizia JM, Gauntt CJ, Klingel KE, Beisel KW, Kandolf R. Direct myocardial injury by enterovirus: a central role in the evolution of murine myocarditis. Clin Immunol Immunopathol. 1993;68(2):159–69.
Jahns R, Boivin V, Hein L, Triebel S, Angermann CE, Ertl G, Lohse MJ. Direct evidence for a beta1-adrenergic receptor-directed autoimmune attack as a cause of idiopathic dilated cardiomyopathy. J Clin Invest. 2004;113(10):1419–29.
Caforio AL, Tona F, Bottaro S, Vinci A, Dequal G, Daliento L, Thiene G, Iliceto S. Clinical implications of anti-heart autoantibodies in myocarditis and dilated cardiomyopathy. Autoimmunity. 2008;41(1):35–45. Review.
Ogata M, Satou T, Kawano R, Takakura S, Goto K, Ikewaki J, Kohno K, Ikebe T, Ando T, Miyazaki Y, Ohtsuka E, Saburi Y, Saikawa T, Kadota J. Correlations of HHV-6 viral load and plasma IL-6 concentration with HHV-6 encephalitis in allogeneic stem cell transplant recipients. Bone Marrow Transplant. 2010;45(1):129–36.
Klingel K, Hohenadl C, Canu A, Albrecht M, Seemann M, Mall G, Kandolf R. Ongoing enterovirus-induced myocarditis is associated with persistent heart muscle infection: quantitative analysis of virus replication, tissue damage, and inflammation. Proc Natl Acad Sci U S A. 1992;89(1):314–8.
Wessely R, Klingel K, Santana LF, Dalton N, Hongo M, Jonathan Lederer W, Kandolf R, Knowlton KU. Transgenic expression of replication-restricted enteroviral genomes in heart muscle induces defective excitation-contraction coupling and dilated cardiomyopathy. J Clin Invest. 1998;102(7):1444–53.
Badorff C, Lee GH, Lamphear BJ, et al. Enteroviral protease 2A cleaves dystrophin: evidence of cytoskeletal disruption in an acquired cardiomyopathy. Nat Med. 1999;5(3):320–6.
Luo H, Zhang J, Cheung C, Suarez A, McManus BM, Yang D. Proteasome inhibition reduces coxsackievirus B3 replication in murine cardiomyocytes. Am J Pathol. 2003;163(2):381–5.
Althof N, Goetzke CC, Kespohl M, Voss K, Heuser A, Pinkert S, Kaya Z, Klingel K, Beling A. The immunoproteasome-specific inhibitor ONX 0914 reverses susceptibility to acute viral myocarditis. EMBO Mol Med. 2018;10(2):200–18.
Wang C, Fung G, Deng H, Jagdeo J, Mohamud Y, Xue YC, Jan E, Hirota JA, Luo H. NLRP3 deficiency exacerbates enterovirus infection in mice. FASEB J. 2019;33(1):942–52.
Kraft L, Erdenesuk T, Sauter M, Tschöpe C, Klingel K. Blocking the IL-1β signalling pathway prevents chronic viral myocarditis and cardiac remodeling. Basic Res Cardiol. 2019;114(2):11–27.
Wessely R, Klingel K, Knowlton KU, Kandolf R. Cardioselective infection with coxsackievirus B3 requires intact type I interferon signaling: implications for mortality and early viral replication. Circulation. 2001;103(5):756–61.
Deonarain R, Cerullo D, Fuse K, Liu PP, Fish EN. Protective role for interferon-beta in coxsackievirus B3 infection. Circulation. 2004;110(23):3540–3.
Becher PM, Hinrichs S, Fluschnik N, Hennigs JK, Klingel K, Blankenberg S, Westermann D, Lindner D. Role of toll-like receptors and interferon regulatory factors in different experimental heart failure models of diverse etiology: IRF7 as novel cardiovascular stress-inducible factor. PLoS One. 2018;13(3):e0193844.
Weinzierl AO, Szalay G, Wolburg H, Sauter M, Rammensee HG, Kandolf R, Stevanović S, Klingel K. Effective chemokine secretion by dendritic cells and expansion of cross-presenting CD4-/CD8+ dendritic cells define a protective phenotype in the mouse model of coxsackievirus myocarditis. J Virol. 2008;82(16):8149–60.
Sesti-Costa R, Françozo MCS, Silva GK, Proenca-Modena JL, Silva JS. TLR3 is required for survival following Coxsackievirus B3 infection by driving T lymphocyte activation and polarization: the role of dendritic cells. PLoS One. 2017;12(10):e0185819.
Meyer IS, Goetzke CC, Kespohl M, Sauter M, Heuser A, Eckstein V, Vornlocher HP, Anderson DG, Haas J, Meder B, Katus HA, Klingel K, Beling A, Leuschner F. Silencing the CSF-1 axis using nanoparticle encapsulated siRNA mitigates viral and autoimmune myocarditis. Front Immunol. 2018;9:2303.
Klingel K, Schnorr JJ, Sauter M, Szalay G, Kandolf R. Beta2-microglobulin-associated regulation of interferon-gamma and virus-specific immunoglobulin G confer resistance against the development of chronic coxsackievirus myocarditis. Am J Pathol. 2003;162(5):1709–20.
Opavsky MA, Penninger J, Aitken K, Wen WH, Dawood F, Mak T, Liu P. Susceptibility to myocarditis is dependent on the response of alphabeta T lymphocytes to coxsackieviral infection. Circ Res. 1999;85(6):551–8.
Frisancho-Kiss S, Coronado MJ, Frisancho JA, Lau VM, Rose NR, Klein SL, Fairweather D. Gonadectomy of male BALB/c mice increases Tim-3(+) alternatively activated M2 macrophages, Tim-3(+) T cells, Th2 cells and Treg in the heart during acute coxsackievirus-induced myocarditis. Brain Behav Immun. 2009;23(5):649–57.
Pappritz K, Savvatis K, Miteva K, Kerim B, Dong F, Fechner H, Müller I, Brandt C, Lopez B, González A, Ravassa S, Klingel K, Diez J, Reinke P, Volk HD, Van Linthout S, Tschöpe C. Immunomodulation by adoptive regulatory T-cell transfer improves Coxsackievirus B3-induced myocarditis. FASEB J. 2018;32(11):6066–78. https://doi.org/10.1096/fj.201701408R.
Szalay G, Sauter M, Hald J, Weinzierl A, Kandolf R, Klingel K. Sustained nitric oxide synthesis contributes to immunopathology in ongoing myocarditis attributable to interleukin-10 disorders. Am J Pathol. 2006;169(6):2085–93.
Li K, Xu W, Guo Q, Jiang Z, Wang P, Yue Y, Xiong S. Differential macrophage polarization in male and female BALB/c mice infected with coxsackievirus B3 defines susceptibility to viral myocarditis. Circ Res. 2009;105(4):353–64.
Cheung C, Luo H, Yanagawa B, Leong HS, Samarasekera D, Lai JC, Suarez A, Zhang J, McManus BM. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in coxsackievirus-induced myocarditis. Cardiovasc Pathol. 2006;15(2):63–74.
Szalay G, Sauter M, Haberland M, Zuegel U, Steinmeyer A, Kandolf R, Klingel K. Osteopontin: a fibrosis-related marker molecule in cardiac remodeling of enterovirus myocarditis in the susceptible host. Circ Res. 2009;104(7):851–9.
Lang C, Sauter M, Szalay G, Racchi G, Grassi G, Rainaldi G, Mercatanti A, Lang F, Kandolf R, Klingel K. Connective tissue growth factor: a crucial cytokine-mediating cardiac fibrosis in ongoing enterovirus myocarditis. J Mol Med (Berl). 2008;86(1):49–60.
Rother M, Krohn S, Kania G, Vanhoutte D, Eisenreich A, Wang X, Westermann D, Savvatis K, Dannemann N, Skurk C, Hilfiker-Kleiner D, Cathomen T, Fechner H, Rauch U, Schultheiss HP, Heymans S, Eriksson U, Scheibenbogen C, Poller W. Matricellular signaling molecule CCN1 attenuates experimental autoimmune myocarditis by acting as a novel immune cell migration modulator. Circulation. 2010;122(25):2688–98.
Masek-Hammerman K, Miller AD, Lin KC, Mackey J, Weissenböck H, Gierbolini L, Burgos A, Perez H, Mansfield KG. Epizootic myocarditis associated with encephalomyocarditis virus in a group of rhesus macaques (Macacamulatta). Vet Pathol. 2012;49(2):386–92.
Oberste MS, Gotuzzo E, Blair P, Nix WA, Ksiazek TG, Comer JA, Rollin P, Goldsmith CS, Olson J, Kochel TJ. Human febrile illness caused by encephalomyocarditis virus infection, Peru. Emerg Infect Dis. 2009;15(4):640–6.
Hardarson HS, Baker JS, Yang Z, Purevjav E, Huang CH, Alexopoulou L, Li N, Flavell RA, Bowles NE, Vallejo JG. Toll-like receptor 3 is an essential component of the innate stress response in virus-induced cardiac injury. Am J Physiol Heart Circ Physiol. 2007;292(1):H251–8.
Yamada T, Matsumori A, Sasayama S. Therapeutic effect of anti-tumor necrosis factor-alpha antibody on the murine model of viral myocarditis induced by encephalomyocarditis virus. Circulation. 1994;89(2):846–51.
Clemente-Casares X, Hosseinzadeh S, Barbu I, Dick SA, Macklin JA, Wang Y, Momen A, Kantores C, Aronoff L, Farno M, Lucas TM, Avery J, Zarrin-Khat D, Elsaesser HJ, Razani B, Lavine KJ, Husain M, Brooks DG, Robbins CS, Cybulsky M, Epelman S. A CD103(+) Conventional Dendritic Cell Surveillance System Prevents Development of Overt Heart Failure during Subclinical Viral Myocarditis. Immunity. 2017;47(5):974–989.e8.
Sherry B, Li XY, Tyler KL, Cullen JM, Virgin HW 4th. Lymphocytes protect against and are not required for reovirus-induced myocarditis. J Virol. 1993;67(10):6119–24.
Sherry B, Baty CJ, Blum MA. Reovirus-induced acute myocarditis in mice correlates with viral RNA synthesis rather than generation of infectious virus in cardiac myocytes. J Virol. 1996;70(10):6709–15.
Sherry B, Torres J, Blum MA. Reovirus induction of and sensitivity to beta interferon in cardiac myocyte cultures correlate with induction of myocarditis and are determined by viral core proteins. J Virol. 1998;72(2):1314–23.
Holm GH, Zurney J, Tumilasci V, Leveille S, Danthi P, Hiscott J, Sherry B, Dermody TS. Retinoic acid-inducible gene-I and interferon-beta promoter stimulator-1 augment proapoptotic responses following mammalian reovirus infection via interferon regulatory factor-3. J Biol Chem. 2007;282(30):21953–61.
Rivera-Serrano EE, DeAngelis N, Sherry B. Spontaneous activation of a MAVS-dependent antiviral signaling pathway determines high basal interferon-β expression in cardiac myocytes. J Mol Cell Cardiol. 2017;111:102–13.
Bogomolovas J, Šimoliūnas E, Rinkūnaitė I, Smalinskaitė L, Podkopajev A, Bironaitė D, Weis CA, Marx A, Bukelskienė V, Gretz N, Grabauskienė V, Labeit D, Labeit S. A novel murine model of parvovirus associated dilated cardiomyopathy induced by immunization with VP1-unique region of parvovirus B19. Biomed Res Int. 2016;2016:1627184.
Puttaraksa K, Pirttinen H, Karvonen K, Nykky J, Naides SJ, Gilbert L. Parvovirus B19V non-structural protein NS1 induces dsDNA autoantibodies and end organ damage in non-autoimmune mice. J Infect Dis. 2019;219(9):1418–29.
Bachelier K, Biehl S, Schwarz V, Kindermann I, Kandolf R, Sauter M, Ukena C, Yilmaz A, Sliwa K, Bock CT, Klingel K, Böhm M. Parvovirus B19-induced vascular damage in the heart is associated with elevated circulating endothelial microparticles. PLoS One. 2017;12(5):e0176311.
Kawai C. From myocarditis to cardiomyopathy: mechanisms of inflammation and cell death: learning from the past for the future. Circulation. 1999;99(8):1091–100. Review.
Häusler M, Sellhaus B, Scheithauer S, Gaida B, Kuropka S, Siepmann K, Panek A, Berg W, Teubner A, Ritter K, Kleines M. Myocarditis in newborn wild-type BALB/c mice infected with the murine gamma herpesvirus MHV-68. Cardiovasc Res. 2007;76(2):323–30.
Lenzo JC, Fairweather D, Cull V, Shellam GR, James Lawson CM. Characterisation of murine cytomegalovirus myocarditis: cellular infiltration of the heart and virus persistence. J Mol Cell Cardiol. 2002;34(6):629–40.
Ritter JT, Tang-Feldman YJ, Lochhead GR, Estrada M, Lochhead S, Yu C, Ashton-Sager A, Tuteja D, Leutenegger C, Pomeroy C. In vivo characterization of cytokine profiles and viral load during murine cytomegalovirus-induced acute myocarditis. Cardiovasc Pathol. 2010;19(2):83–93.
Cull VS, Bartlett EJ, James CM. Type I interferon gene therapy protects against cytomegalovirus-induced myocarditis. Immunology. 2002;106(3):428–37.
Pankuweit S, Klingel K. Viral myocarditis: from experimental models to molecular diagnosis in patients. Heart Fail Rev. 2013;18(6):683–702.
Sakakibara S, Konno S. Endomyocardial biopsy. Jpn Heart J. 1962;3:537–43.
Saiki RK, Scharf S, Faloona F, Mullis KB, Horn GT, Ehrlich HA, Arnheim N. Enzymatic amplification of β3-globin genomic sequences and restriction site analysis for diagnosis of sickle cell anemia. Science. 1985;230:1350–13541.
Pankuweit S, Portig I, Eckhardt H, Crombach M, Hufnagel G, Maisch B. Prevalence of viral genome in endomyocardial biopsies from patients with inflammatory heart muscle disease. Herz. 2000;25(3):221–6.
Jackson DP, Lewis FA, Taylor GR, Boylston AW, Quirke P. Tissue extraction of DNA and RNA and analysis by polymerase chain reaction. J Clin Pathol. 1990;43:499–504.
Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156–9.
Maniatis T, Fritsch EF, Sambrook J. Molecular cloning: a laboratory manual. New York: Cold Spring Harbor Laboratory; 1992.
Rotbart HA. Enzymatic RNA amplification of enteroviruses. J Clin Microbiol. 1990;28:438–42.
Martin AB, Webber S, Fricker J, Jaffe R, Demmler G, Kearney D, Zhang YH, Bodurtha J, Gelb B, Ni J. Acute myocarditis: rapid diagnosis in children. Circulation. 1994;90:330–9.
Kandolf R, Ameis D, Kirschner P, Canu A, Hofschneider PH. In situ detection of enteroviral genomes in myocardial cells by nucleic acid hybridization: an approach to the diagnosis of viral heart disease. Proc Natl Acad Sci U S A. 1987;84:6272–6.
Klingel K, Stephan S, Sauter M, Zell R, McManus BM, Bültmann B, Kandolf R. Pathogenesis of murine enterovirus myocarditis: virus dissemination and immune target cells. J Virol. 1996;70:8888–95.
Klump WM, Bergmann I, Müller BC, Ameis D, Kandolf R. Complete nucleotide sequence of infectious coxsackievirus B3 cDNA: two initial 5’ uridine residues are regained during plus-strand RNA synthesis. J Virol. 1990;64:1573–83.
Archard L, Khan M, Soteriou BA, Zhang H, Why HJ, Robinson NM, Richardson PJ. Characterisation of coxsackie B virus RNA in myocardium from patients with dilated cardiomyopathy by nucleotide sequencing of reverse transcription-nested polymerase chain reaction products. Hum Pathol. 1998;29:578–84.
Chapman NM, Tracy S, Gauntt CJ, Fortmüller U. Molecular detection and identification of enteroviruses using enzymatic amplification and nucleic acid hybridisation. J Clin Microbiol. 1990;28:843–50.
Grasso M, Arbustini E, Silini E, Diegoli M, Percivalle E, Ratti G, Bramerio M, Gavazzi A, Vigano M, Milanesi G. Search for Coxsackievirus B3 RNA in idiopathic dilated cardiomyopathy using gene amplification by polymerase chain reaction. Am J Cardiol. 1992;69:658–64.
Tracy S, Chapman NM, McManus BM, Pallansch MA, Beck MA, Carstens J. A molecular and serologic evaluation of enteroviral involvement in human myocarditis. J Mol Cell Cardiol. 1990;22:403–14.
Schowengerdt K, Ni J, Denfield S, Gajarski RJ, Bowles NE, Rosenthal G, Kearney DL, Price JK, Rogers BB, Schauer GM, Chinnock RE, Towbin JA. Association of parvovirus B19 genome in children with myocarditis and cardiac allograft rejection. Diagnosis using the polymerase chain reaction. Circulation. 1997;96:3549–54.
Piiparinen H, Vaheri A. Genotyping of herpes simplex viruses by polymerase chain reaction. Arch Virol. 1991;119:541–8.
Weiss SM, Roblin PM, Gaydos CA, Cummings P, Patton DL, Schulhoff N, Shani J, Frankel R, Penney K, Quinn TC, Hammerschlag MR, Schachter J. Failure to detect chlamydia pneumoniae in coronary atheromas of patients undergoing atherectomy. J Infect Dis. 1996;173:957–62.
Goodman JL, Jurkovic P, Kramber JM, Johnson RC. Molecular detection of persistent Borrelia burgdorferi in the urine of patients with active Lyme disease. Infect Immunol. 1991;59:269–78.
Stanek G, Klein J, Bitnner R, Glogar D. Isolation of Borrelia burgdorferi from the myocardium of a patient with longstanding cardiomyopathy. N Engl J Med. 1990;322:249–52.
Nakhleh RE, Copenhaver CM, Werdin K. Lack of evidence for involvement of Epstein-Barr virus in the development of ‘Quilty’ lesion of transplanted hearts: an in situ hybridization study. J Heart Lung Transplant. 1991;10:504–7.
Kandolf R, Hofschneider PH. Molecular cloning of the genome of a cardiotropic coxsackie B3 virus: full-length reverse-transcribed recombinant cDNA generates infectious virus in mammalian cells. Proc Natl Acad Sci U S A. 1985;82:4818–22.
Manaresi E, Gallinella G, Zuffi E, Bonvicini F, Zerbini M, Musiani M. Diagnosis and quantitative evaluation of parvovirus B19 infections by real-time PCR in the clinical laboratory. J Med Virol. 2002;67:275–81.
Harder TC, Hufnagel M, Zahn K, Beutel K, Schmitt H-J, Ullmann U, Rautenberg P. New LightCycler PCR for rapid and sensitive quantification of parvovirus B19 DNA guides therapeutic decision-making in relapsing infections. J Clin Microbiol. 2001;39:4413–9.
Aberham C, Pendl C, Gross P, Zerlauth G, Gessner M. A quantitative, internally controlled real-time PCR assay for the detection of parvovirus B19 DNA. J Virol Methods. 2001;92:183–91.
Gruber F, Falkner FG, Dorner F, Hammerle T. Quantitation of viral DNA by real-time PCR applying duplex amplification, internal standardization, and two-color fluorescence detection. Appl Environ Microbiol. 2001;67:2837–9.
Yajima T, Knowlton KU. Viral myocarditis: from the perspective of the virus. Circulation. 2009;119:2615–24.
Pankuweit S, Moll R, Baantrup U, Portig I, Hufnagel G, Maisch B. Prevalence of the parvovirus B19 genome in endomyocardial biopsy specimens. Hum Pathol. 2003;34:497–500.
Kühl U, Pauschinger M, Bock T, Klingel K, Schwimmbeck CP, Seeberg B, Krautwurm L, Poller W, Schultheiss HP, Kandolf R. Parvovirus B19 infection mimicking acute myocardial infarction. Circulation. 2003;108(8):945–50.
Bültmann BD, Klingel K, Sotlar K, Bock CT, Baba HA, Sauter M, Kandolf R. Fatal parvovirus B19-associated myocarditis clinically mimicking ischemic heart disease: an endothelial cell-mediated disease. Hum Pathol. 2003;34:92–5.
Kuethe F, Lindner J, Matschke K, Wenzel JJ, Norja P, Ploetze K, Schaal S, Kamvissi V, Bornstein SR, Schwanebeck U, Modrow S. Prevalence of parvovirus B19 and human bocavirus DNA in the heart of patients with no evidence of dilated cardiomyopathy or myocarditis. Clin Infect Dis. 2009;49:1660–6.
Lotze U, Egerer R, Glück B, Zell R, Sigusch H, Erhardt C, Heim A, Kandolf R, Bock T, Wutzler P, Figulla HR. Low level myocardial parvovirus B19 persistence is a frequent finding in patients with heart disease but unrelated to ongoing myocardial injury. J Med Virol. 2010;82:1449–57.
Corcioli F, Zakrzewska K, Rinieri A, Fanci R, Innocenti M, Civinini R, De Giorgi V, Di Lollo S, Azzi A. Tissue persistence of parvovirus B19 genotypes in asymptomatic persons. J Med Virol. 2008;80:2005–11.
Schenk T, Enders M, Pollak S, Hahn R, Huzly D. High prevalence of human parvovirus B19 DNA in myocardial autopsy samples from subjects without myocarditis or dilative cardiomyopathy. J Clin Microbiol. 2009;47:106–10.
Stewart GC, Lopez-Molina J, Gottumukkala RV, Rosner GF, Anello MS, Hecht JL, Winters GL, Padera RF, Baughman KL, Lipes MA. Myocardial parvovirus B19 persistence: lack of association with clinicopathologic phenotype in adults with heart failure. Circ Heart Fail. 2011;4(1):71–8.
Richter J, Quintanilla-Martinez L, Bienemann K, Zeus T, Germing U, Sander O, Kandolf R, Häussinger D, Klingel K. An unusual presentation of a common infection. Infection. 2013;41(2):565–9.
Zafrir B, Aviv A, Reichman N, Flatau E. Epstein-Barr virus associated pericarditis and pericardial effusion: case report and diagnostic aspects. Eur J Intern Med. 2005;16:528–30.
Roubille F, Gahide G, Moore-Morris T, Granier M, Davy JM, Vernhet H, Piot C. Epstein Barr virus (EBV) and acute myopericarditis in an immunocompetent patient: first demonstrated case and discussion. Intern Med. 2008;47(7):627–9.
Chang YL, Parker ME, Nuovo G, Miller JB. Human herpesvirus 6–related fulminant myocarditis and hepatitis in an immunocompetent adult with fatal outcome. Hum Pathol. 2009;40(5):740–5.
Leveque N, Boulagnon C, Brasselet C, Lesaffre F, Boutolleau D, Metz D, Fornes P, Andreoletti L. A fatal case of human herpesvirus 6 chronic myocarditis in an immunocompetent adult. J Clin Virol. 2011;52(2):142–5.
Bratincsák A, El-Said HG, Bradley JS, Shayan K, Grossfeld PD, Cannavino CR. Fulminant myocarditis associated with pandemic H1N1 influenza A virus in children. J Am Coll Cardiol. 2010;55:928–9.
Liao YC, Hsieh YC, Chang WC, Huang JL, Ting CT, Wu TJ. Fulminant myocarditis in an adult with 2009 pandemic influenza A (H1N1 influenza) infection. J Chin Med Assoc. 2011;74(3):130–3.
Kuhl U, Pauschinger M, Noutsias M, Seeberg B, Bock T, Lassner D, Poller W, Kandolf R, Schultheiss HP. High prevalence of viral genomes and multiple viral infections in the myocardium of adults with idiopathic left ventricular dysfunction. Circulation. 2005;111:887–93.
Kandolf R, Bültmann B, Klingel K, Bock CT. Molecular mechanisms and consequences of cardiac viral infections. Pathologe. 2008;29(Suppl 2):112–7.
Moulik M, Breinholt JP, Dreyer WJ, Kearney DL, Price JF, Clunie SK, Moffett BS, Kim JJ, Rossano JW, Jefferies JL, Bowles KR, O’Brian Smith E, Bowles NE, Denfield SW, Towbin JA. Viral endomyocardial infection is an independent predictor and potentially treatable risk factor for graft loss and coronary vasculopathy in pediatric cardiac transplant recipients. J Am Coll Cardiol. 2010;56(7):582–92.
Caforio A, Pankuweit S, Charron P, Cooper L, Basso C, Felix S, Fu M, Gimeno R, Helio T, Heymans S, Jahns R, McKenna WJ, Klingel K, Linhart A, Maisch B, Mogensen J, Monserrat L, Pinto Y, Ristic A, Schultheiss HP, Seggewiss H, Tavazzi L, Yilmaz A, Elliott P. Current state of knowledge on aetiology, diagnosis, management and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636–48.
Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, Martin I, Nordet P. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation. 1996;93:841–2.
Leone O, Veinot JP, Angelini A, Baandrup UT, Basso C, Berry G, Bruneval P, Burke M, Butany J, Calabrese F, d’Amati G, Edwards WD, Fallon JT, Fishbein MC, Gallagher PJ, Halushka MK, McManus B, Pucci A, Rodriguez ER, Saffitz JE, Sheppard MN, Steenbergen C, Stone JR, Tan C, Thiene G, van der Wal AC, Winters GL. 2011 consensus statement on endomyocardial biopsy from the Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology. Cardiovasc Pathol. 2012;21:245–74.
Kindermann I, Barth C, Mahfoud F, Ukena C, Lenski M, Yilmaz A, Klingel K, Kandolf R, Sechtem U, Cooper LT, Bohm M. Update on myocarditis. J Am Coll Cardiol. 2012;59:779–92.
Sagar S, Liu PP, Cooper LT. Myocarditis. Lancet. 2012;379:738–47.
Dennert R, Crijns HJ, Heymans S. Acute viral myocarditis. Eur Heart J. 2008;29:2073–82.
Takeuchi S, Kawada JI, Okuno Y, Horiba K, Suzuki T, Torii Y, Yasuda K, Numaguchi A, Kato T, Takahashi Y, Ito Y. Identification of potential pathogenic viruses in patients with acute myocarditis using next-generation sequencing. J Med Virol. 2018;90(12):1814–21.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pankuweit, S., Klingel, K. (2020). Viral Myocarditis: From Experimental Models to Diagnosis in Patients. In: Caforio, A. (eds) Myocarditis. Springer, Cham. https://doi.org/10.1007/978-3-030-35276-9_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-35276-9_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-35275-2
Online ISBN: 978-3-030-35276-9
eBook Packages: MedicineMedicine (R0)