Abstract
Class III antiarrhythmic drugs (AADs) predominantly block outward-repolarizing potassium currents and prolong cardiac action potential duration (APD) and refractoriness at concentrations at which they do not affect the sodium channels and, therefore, intracardiac conduction velocity is not significantly affected. The prolongation of the APD and refractoriness, combined with the maintenance of normal conduction velocity, leads to an increase in the wavelength of the cardiac impulse, defined as the distance travelled by the depolarization wave during the functional refractory period, closes the excitable gap in the reentrant circuit and suppresses reentry. Class III AADs include: amiodarone, dofetilide, dronedarone, ibutilide and sotalol.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Class III antiarrhythmic drugs (AADs) predominantly block outward-repolarizing potassium currents and prolong cardiac action potential duration (APD) and refractoriness at concentrations at which they do not affect the sodium channels and, therefore, intracardiac conduction velocity is not significantly affected [1]. The prolongation of the APD and refractoriness, combined with the maintenance of normal conduction velocity, leads to an increase in the wavelength of the cardiac impulse, defined as the distance travelled by the depolarization wave during the functional refractory period, closes the excitable gap in the reentrant circuit and suppresses reentry (Fig. 3.1). Class III AADs include: amiodarone, dofetilide, dronedarone, ibutilide and sotalol.
Class III antiarrhythmic drugs (AADs). (a) Class III AADs prolong the cardiac action potential duration (APD) and refractoriness (ERP) and under certain circumstances can induce early depolarizations that induce a polymorphic ventricular tachycardia (torsades de pointes). (b) Many class III AADs prolong the APD at slow but not at normal or fast heart rates, i.e., they exhibit reverse use-dependence. (c) Class III AADs prolong the APD/ERP, do not modify the conduction velocity (CV) and increase the wavelength of the cardiac impulse (WL), defined as the distance travelled by the depolarization wave during the functional refractory period. As a consequence, they close the excitable gap in the reentrant circuit and they can prevent or abolish reentry. Because the APD/ERP is longer than the conduction time around a reentrant circuit, class III AADs can prevent or abolish impulse reentry
However, class III AADs present several disadvantages. First, some of them exhibit reverse-use dependence, i.e. the prolongation of the APD increases at normal or at slower heart rates (during bradycardia or after a long diastolic interval) but declines as heart rate is increased (i.e., during tachyarrhythmias), which limits their antiarrhythmic efficacy (Fig. 3.1). Second, they produce an excessive and sometimes inhomogeneous prolongation of the ventricular APD (QT interval), which increases the transmural dispersion of cardiac repolarization and can induce early afterdepolarizations (Fig. 3.1) that can trigger the development of polymorphic ventricular tachycardias called torsades de pointes (TdP) . The risk of ventricular proarrhythmia is a serious limitation of class III AADs. Third, these drugs produce an acquired long QT syndrome and they should be avoided in combination with other QT-prolonging drugs. Table 3.1 summarizes the main QT-prolonging drugs and the risk factors that predispose to TdP.
In this chapter, we review the electrophysiological and pharmacological properties, adverse effects and clinical indications of amiodarone, dofetilide, dronedarone, ibutilide and sotalol. Their pharmacokinetic properties, adverse effects, doses and clinical indications are summarized in Tables 3.2, 3.3, 3.4, 3.5, 3.6, 3.7, and 3.8.
Amiodarone
Amiodarone is a iodinated benzofuran derivative that exhibits a “wide-spectrum” of antiarrhythmic properties. It blocks inwardly depolarizing Na+ (INa) and L-type Ca2+ (ICaL) currents and several outward repolarizing K+ currents, including the transient (Ito), the inward rectifier (IK1), the ultrarapid (IKur), rapid (IKr), and slow (IKs) components of the delayed rectifier and the acetylcholine-activated (IKAch) [2,3,4,5]. Amiodarone inhibits the INa by blocking the inactivated state of sodium channels with a fast diastolic recovery from block. This effect is accentuated in depolarized tissues (voltage-dependent block) and at fast rates (rate-dependent block), but it is almost nonexistent at slow heart rates. In fact, amiodarone reduces cardiac excitability and conduction velocity and prolongs the QRS and H-V intervals at fast rates. Additionally, amiodarone noncompetitively antagonizes α- and β-adrenoceptors (class II effect) [2,3,4,5,6], inhibits both the conversion of thyroxine (T4) to triiodothyronine (T3) and the entry of T3 and T4 into cells [7], and produces a vasodilator effect mediated via the blockade of ICaL and β-adrenergic receptors. The blockade of ICaL and β-adrenergic receptors explains why amiodarone produces bradycardia and atrio-ventricular (AV) block. Thus, amiodarone exhibits class I, III and IV antiarrhythmic actions of the Vaughan Williams classification.
Electrophysiological Actions
The acute and chronic electrophysiological effects of amiodarone in humans are very different [2, 5, 6, 8, 9]. After intravenous administration, the main effect is the lengthening of AV nodal refractoriness and intranodal conduction (with prolongation of the PR and A-H intervals) possibly related to the blockade of ICaL and the non-competitive β-adrenergic antagonism. However, the drug produces minimal effects on the APD and refractoriness of the atrial and ventricular muscle, by pass tracts, or His-Purkinje system and there is almost no effect on the QRS, H-V and QTc intervals or the monophasic action potentials [1,2,3, 5, 6]. Thus, the class III action of the drug is not observed.
However, long-term treatment with oral amiodarone prolongs the APD and refractoriness in all cardiac tissues, including bypass tracts, without affecting the resting membrane potential. Interestingly, amiodarone lengthens the APD preferentially in cardiac tissues with the shortest APD (His bundle, atrial muscle and ventricular epicardium and endocardium), with lesser effects, or even a shortening at slow rates, in Purkinje fibres and M cells [1,2,3, 5, 6]. Thus, in contrast to other class I and III AADs, amiodarone produces a homogeneous prolongation of the APD (QT interval) and reduces transmural dispersion of repolarization across the ventricular wall and the possible re-entry of cardiac impulses. Additionally, amiodarone prolongs the APD at all driving rates, i.e., it does not produce reverse use-dependence. Furthermore, despite amiodarone prolongs the ventricular APD, the risk of TdP is less than with other AADs, possibly because it blocks both the ICaL and β-adrenoceptors, does not produce reverse use-dependence and produces a more homogenous recovery of ventricular repolarization reducing the transmural dispersion of repolarization. In chronic treatments and at fast driving rates, amiodarone blocks the INa (prolongs the QRS complex) and decreases cardiac excitability and conduction velocity and increases the VF threshold. Desethylamiodarone (DEA), the main active metabolite, has relatively greater effects on the INa and contributes to the antiarrhythmic efficacy of amiodarone [3]. On the ECG, amiodarone prolongs the RR, PR, A-H, H-V, QRS, JT and QT intervals (occasionally it can produce U waves). Oral amiodarone was more effective than IV amiodarone in lengthening the anterograde effective refractory period of the accessory AV pathway.
In the sinoatrial node and other cardiac pacemaker cells, amiodarone decreases the slope of phase 4 depolarization (pacemaker potential) and the rate of spontaneous excitation and suppresses the slow action potentials (abnormal automaticity) elicited in abnormally depolarized cardiac cells as well as the early afterdepolarizations generated in Purkinje fibres and M cells [2,3,4,5]. In the AV node, amiodarone slows intranodal conduction and increases refractoriness and, therefore, reduces the ventricular rate in patients with supraventirulcar arrhythmias. In patients with AF, amiodarone prolongs the refractory periods both in the atria and in the pulmonary veins, slows AV nodal conduction and, in experimental models, it prevents atrial remodelling [10]. The effects of oral amiodarone on sinoatrial and AV nodal function are maximal within 2 weeks, whereas the effects on VT and ventricular refractoriness appear gradually, becoming maximal at ≥10 weeks.
Hemodynamic Effects
Amiodarone is a peripheral and coronary vasodilator. After oral administration, amiodarone slows sinus rate (15–20%) and prolongs the PR and QT intervals but does not depress the left ventricular ejection fraction (LVEF). Indeed, the LVEF may increase slightly even in patients with reduced LVEF, possibly because its vasodilator effect reduces LV afterload. However, after IV administration amiodarone decreases heart rate, systemic vascular resistances, blood pressure and contractile force; thus, it should be given cautiously to patients with depressed LVEF because of the risk of bradycardia and hypotension [5, 6].
Pharmacokinetics (Table 3.2)
After oral administration, amiodarone presents a slow, variable and incomplete absorption (bioavailability of 35–65%) and peak plasma levels are reached after 3–8 h [11]. Food increases its oral bioavailability and reduces gastrointestinal adverse effects [12]. The onset of action after oral administration occurs after 2–3 days (1–2 h after IV administration) [9]. Amiodarone is highly protein bound (99%) and extensively distributed (Vd 70 L/kg). It accumulates in the heart (cardiac levels are 10–50 times higher than in plasma), adipose tissue, liver, lungs and skin, crosses the placenta and is found in breast milk. This wide tissular distribution explains why even when the onset of drug action occurs after 2–3 days, steady-state plasma levels are reached after several months unless large loading doses are used, and why the drug effects persist for weeks or months after drug discontinuation [9, 11]. Amiodarone is extensively metabolized in the liver by CYP450 3A4 and 2C8, leading to various active metabolites. DEA also accumulates in almost all tissues and exhibits electrophysiologic effects quite similar to those of amiodarone. Both amiodarone and DEA are excreted primarily via the hepatic-biliary route undergoing some enterohepatic recirculation, so that doses do not need to be reduced in patients with renal disease. Amiodarone is eliminated very slowly. There is an initial 50% reduction in plasma levels 3–10 days after drug discontinuation which probably represents drug elimination from well-perfused tissues, followed by a terminal elimination half-life (t) of 53 days (range 26–107 days). The therapeutic plasma levels are between 1.0 and 2.5 mg/mL [6]. Amiodarone and DEA are not dialyzable.
Adverse Effects (Table 3.3)
They are reported in up to 75% of patients treated with amiodarone for more than 2 years, leading to drug discontinuation in 18–37% of patients. Some side effects may be potentially fatal [9, 13, 14]. Adverse effects are more common on chronic therapy and at high doses, but they still occur even at dosages ≤200 mg/day. Cardiac side effects include symptomatic bradycardia (especially in the elderly), AV block, conduction disturbances, worsening heart failure (HF) and QT prolongation [9, 13, 14]. However, the risk of TdP is very uncommon (<0.5%) [15], probably because of its class II and IV properties, but may occur in patients with hypokalemia or bradycardia, or those receiving QT-prolonging drugs. Phlebitis and hypotension are observed when administered IV.
Adverse extracardiac effects are gastrointestinal (nausea, vomiting, constipation, anorexia), ocular (almost all patients develop asymptomatic corneal microdeposits; rare: optic neuritis and atrophy with visual loss), neurological (proximal muscle weakness, fatigue, peripheral neuropathy, headache, ataxia, tremors, impaired memory, sleep disturbances), cutaneous (rash, photosensitivity, alopecia, blue-gray skin discoloration), hyperthyroidism or hypothyroidism and hepatotoxicity (elevated transaminase levels, hepatitis, cirrhosis and fatal hepatic necrosis) [6, 9, 13,14,15,16,17]. Amiodarone can increase creatinine plasma levels due to partial inhibition of the tubular organic cationic transporter system, rather than a decline in renal function. In fact, the drug does not affect the glomerular filtration rate (GFR), renal blood flow, and Na+ or K+ excretion. Most of these adverse effects are reversible after dose reduction or drug discontinuation, but because of its long half-life, some of them may persist for many months (skin discoloration slowly reverses after 18 months but may not disappear). Neurological and gastrointestinal adverse effects are common during loading doses and usually improve with lower maintenance doses.
Pulmonary toxicity (interstitial pneumonitis, pulmonary fibrosis) occurs in 1–15% of patients receiving doses ≥400 mg/day. Pulmonary function tests show a restrictive pattern with reduced forced vital capacity and diffusing capacity, and chest computed tomography can reveal evidence of fibrosis and diffuse ground glass confluent opacities. Advanced age, high cumulative dose (>400 mg/day), duration of therapy (>6 months), reduced predrug diffusion capacity and preexisting pulmonary disease are risk factors for the development of pulmonary toxicity [14, 18, 19]. Pulmonary toxicity can be fatal in about 10% of patients [13]. Treatment includes drug discontinuation and administration of glucocorticoids [9].
Amiodarone inhibits the peripheral conversion of T4 to T3, producing a slight increase in T4, reverse T3 and thyroid-stimulating hormone (TSH), and a slight decrease in T3 levels. Hypothyroidism appears in 2–6% during the first year of treatment (TSH >10 mU/L) particularly in areas with high dietary iodine intake [7, 20]. Drug discontinuation and/or levothyroxine are the main treatments for amiodarone-induced hypothyroidism. Hyperthyroidism (TSH < 0.35 mU/L) appears in 0.9% of patients and predominates in areas with iodine deficiency [21]. Because it may precipitate cardiac arrhythmias, hyperthyroidism should be excluded if recurrence of arrhythmias appears during amiodarone therapy [7]. Even if amiodarone is discontinued, thyrotoxicosis persists for up to 8 months. Type 1 amiodarone-induced thyrotoxicosis (AIT) occurs in patients with an underlying thyroid pathology and is treated with high doses of thionamides (eg, methimazole or propylthiouracil) to block thyroid hormone synthesis, adding potassium perchlorate to block iodide uptake by the thyroid and deplete intrathyroidal iodine stores. Type 2 AIT is a result of a destructive thyroiditis that results in excess release of preformed T4 and T3 into the circulation and is treated with glucocorticoids. Total thyroidectomy is the only measure that consistently allows continued use of amiodarone. Therefore, thyroid function tests should be performed every 3 months for the first year and every 6–12 months unless thyroid dysfunction appeared.
Because adverse effects are usually dose-related their incidence can be reduced by using very low doses (100–200 mg daily) [9, 14]. Additionally, it is recommended to examine before and periodically during treatment the ECG, chest x-ray, skin, peripheral nerves, thyroid, hepatic, visual and pulmonary function (including carbon monoxide diffusion capacity testing) [9].
Amiodarone and DEA cross the placenta and are detected in breast milk. Amiodarone is associated with severe adverse fetal effects (neurodevelopmental abnormalities, preterm birth, fetal growth restriction and fetal neonatal hypo-/hyper-thyroidism and bradycardia) [22, 23]. Therefore, amiodarone is not recommended in women who are, or may become, pregnant (Pregnancy category X) and in nursing mothers [11]. Oral amiodarone may be considered for ongoing management in pregnant patients when treatment of highly symptomatic patients is required and other therapies are ineffective or contraindicated [24,25,26,27,28,29].
Drug Interactions
Amiodarone and DEA inhibit CYP450 isoenzymes (CYP1A1/2, 3A4, 2C9 y 2D6) and some transporters [P-glycoprotein (P-gp) and organic cation transporter 2 (OCT2)]. Additionally, amiodarone is a substrate for CYP3A4 [11]. Therefore, amiodarone has the potential for multiple interactions with other drugs that are summarized in Table 3.4.
Contraindications and Cautions
See Table 3.3.
Dosage and Administration
See Table 3.5.
Indications
Amiodarone is indicated for a wide spectrum of supraventricular [atrial fibrillation (AF) or flutter (Af), atrial tachycardia, AV nodal reentrant tachycardia and AV reentrant tachycardia] and ventricular tachyarrhythmias [ventricular tachycardia (VT) and fibrillation (VF)] in patients with structural heart disease (coronary artery disease, LV hypertrophy, HF or LV dysfunction, hypertrophic cardiomyopathy), being the drug of choice when other AADs are ineffective, not tolerated or contraindicated [24,25,26,27,28,29]. Furthermore, because amiodarone produces less negative inotropic effects or hypotension than β-blockers, diltiazem or verapamil, it is preferred in critically ill patients or in those with hemodynamic instability. However, amiodarone presents several disadvantages, including its slow onset of action after oral administration, so that it should be administered IV or at loading doses to achieve effects rapidly, its long half-life, and its poor safety profile and multiple drug interactions. Because of long-term amiodarone therapy is associated with cardiac and extracardiac adverse effects, it remains as a second-line treatment in patients who are suitable for other AADs or in young patients [9, 24,25,26,27,28,29].
-
1.
Atrial fibrillation/flutter (Table 3.6). Amiodarone is used for the maintenance of sinus rhythm (SR) conversion of AF/Af to SR and ventricular rate control. Amiodarone is the most effective drug for the maintenance of SR in patients with recurrent symptomatic AF/Af [15, 30,31,32,33]. It is superior to class I AADs and sotalol and the drug of choice in patients with structural heart disease and the only AAD recommended in patients with congestive HF or significant aortic stenosis [24, 27, 30, 34, 35]. Amiodarone is superior to sotalol or propafenone for maintenance of SR after cardioversion [30] and in a substudy of the AFFIRM trial, amiodarone was superior to both sotalol and a mixture of class I drugs. In the SAFE-T trial, amiodarone was superior to sotalol, but both drugs had similar efficacy in the subgroup of patients with ischemic heart disease [35].
Amiodarone is also effective for the conversion of AF/Af to SR. However, most data derived from use in patients with AF, while few data are available for patients with Af [24, 27]. Although it has the disadvantage that conversion is often delayed beyond 6 h, amiodarone also slows ventricular rates and it has no risk of postconversion ventricular arrhythmias. For the acute conversion of AF, IV amiodarone is as effective as IV propafenone [36] and both amiodarone and flecainide appear more effective than sotalol in restoring SR [37,38,39]. Pretreatment with amiodarone can facilitate DC cardioversion and prevent AF recurrences; in relapses to AF after successful cardioversion, repeating DC cardioversion after prophylactic amiodarone can improve the efficacy of DC cardioversion to maintain the SR and prevent the recurrences [37, 40]. Furthermore, amiodarone should be considered to achieve rhythm control and maintain SR in patients with hypertrophic cardiomyopathy and recurrent symptomatic AF [24, 27, 41].
Short-term oral amiodarone treatment following ablation for paroxysmal or persistent AF did not reduce the recurrence of AF/Af at the 6-month follow-up but prolonged time to first documented recurrence and more than halved arrhythmia-related hospitalization and cardioversion rates within the blanking period [42]. Administered before cardiothoracic surgery or postoperatively, amiodarone (alone or in combination with β-blockers) decreased the incidence of post-operative AF (POAF) and hospital stay compared to β-blocker therapy [43,44,45,46] and was effective in converting POAF to SR [47, 48].
Amiodarone can be useful for rate control in patients whose heart rate cannot be controlled with combination therapy (e.g. β-blockers or verapamil/diltiazem combined with digoxin) or when these drugs are contraindicated or poorly tolerated [24, 27]. Intravenous amiodarone slows the ventricular rate (10–12 bpm after 8–12 h) [34, 49].
Amiodarone prolongs the anterograde refractory period of the accessory pathway and can be used both for rate control and to achieve conversion in patients with pre-excitation and AF, although urgent electrical cardioversion is often necessary. IV amiodarone is not recommended in these patients, because case reports of accelerated ventricular rhythms and VF [50].
-
2.
Supraventricular tachycardias (SVT) (Table 3.7). Evidence for amiodarone for the ongoing management of SVT is limited [26, 29]. IV amiodarone may be considered for acute treatment in hemodynamically stable patients and for ongoing treatment, but because of its safety profile, oral amiodarone is a second-line agent recommended when catheter ablation or other AADs are ineffective or contraindicated (i.e. in patients with structural heart disease) [26, 29].
-
3.
Ventricular arrhythmias (Table 3.8). Amiodarone is recommended for the treatment and prophylaxis of life-threatening recurrent ventricular arrhythmias (VT and/or VF) and life-threatening recurrent hemodynamically unstable VT not responding to other AADs, particularly in patients with structural heart disease (i.e. HF, myocardial infarction-MI, hypertension, or cardiomyopathies) or after cardiac surgery when other AADs are not tolerated or contraindicated [25, 28, 51,52,53]. However, there is modest evidence from randomized controlled trials supporting its use and nowadays it has been replaced by the implantable cardioverter-defibrillator (ICD) therapy. Doses of amiodarone should be as low as possible and restricted to selected patients with refractory ventricular arrhythmias and in young patients it should be reserved as a bridge to more definitive treatment options such as catheter ablation.
Amiodarone is more effective than sotalol and presents a lower risk of ventricular proarrhythmia, but chronic therapy (18–24 months) and high doses of amiodarone (>400 mg/day) increase the risk of adverse effects that require drug discontinuation [9, 51, 54]. Therefore, doses of amiodarone should be as low as possible and restricted to selected patients with refractory ventricular arrhythmias. Chronic treatment in young patients should be reserved as a bridge to more definitive treatment options such as catheter ablation [28].
Several studies compared IV amiodarone with other AADs (lidocaine, procainamide or bretylium) for the prophylaxis and treatment of VF and recurrent, hemodynamically destabilizing VT when they can no longer be controlled by successive electrical cardioversion or defibrillation [28, 55,56,57,58,59]. Administered during incessant VT, amiodarone produced a gradual slowing of the VT cycle length, with eventual termination of the arrhythmia [60]. However, these trials showed that IV amiodarone was moderately effective during a 24–48 h period against VT and VF and the arrhythmia frequently recurred. Furthermore, in a retrospective study, IV amiodarone produced an acute termination of sustained monomorphic VT only in 29% of patients [61]. Very recently the PROCAMIO study compared for the first time in a randomized design IV procainamide and amiodarone for the treatment of the acute episode of sustained monomorphic well-tolerated VT. Procainamide therapy was associated with less major cardiac adverse events and a higher proportion of tachycardia termination within 40 min [62].
In patients with sustained VT or VF and cardiac arrest several placebo-controlled trials and meta-analysis found that amiodarone decreased the recurrences and improved symptoms and survival, but when compared with ICD therapy there was a significant reduction (28%) in the relative risk of death with the ICD that was due almost entirely to a 50% reduction in arrhythmic death [63,64,65,66]. Therefore, in these patients amiodarone has been replaced by ICD. However, in the ICD era amiodarone (plus β-blockade) may still be used in ICD-treated patients to decrease the frequency of shocks from VT/VF episodes or to control supraventricular tachyarrhythmias elicited by device therapy [64, 66]. When amiodarone is added to an ICD, the defibrillation threshold is usually increased and reprogramming prior to discharge from hospital may be necessary. Amiodarone is also indicated to improve symptoms in patients with DCM with an ICD who experience recurrent appropriate shocks in spite of optimal device programming and in patients with arrhythmogenic right ventricular cardiomyopathy and presenting frequent premature ventricular beats (PVBs) or non-sustained VT who are intolerant or have contraindications to β-blockers [25, 28].
The ARREST and ALIVE trials , analyzed the effects of IV amiodarone in hemodynamically destabilizing refractory VT/VF, VT when they can no longer be controlled by successive electrical cardioversion or defibrillation. In patients with out-of-hospital cardiac arrest due to refractory VT or VF after 3 direct-current shocks, those who received amiodarone were more likely than those who received placebo or lidocaine to have a return of spontaneous circulation and to survive to be admitted to the hospital [55, 57]. However, neither amiodarone nor lidocaine result in a significantly higher rate of survival to hospital discharge or favourable neurologic outcome at discharge. Thus, amiodarone may be useful for resuscitating some cardiac arrest victims.
A meta-analysis evaluated the effectiveness of amiodarone for primary or secondary prevention in sudden cardiac death (SCD) compared with placebo, no intervention or any other AAD in patients at high risk (primary prevention) or who have recovered from a cardiac arrest or a syncope due to VT and/or VF (secondary prevention) [51, 67]. There was low-to-moderate quality evidence that amiodarone reduced SCD, cardiac and all-cause mortality when compared to placebo or no intervention for primary prevention, but its effects were superior to other AADs. However, it was uncertain if amiodarone reduced or increased SCD and mortality for secondary prevention because the quality of the evidence was very low.
The CASCADE study evaluated AAD therapy in survivors of out-of-hospital VF not associated with a Q-wave MI who were at especially high-risk of recurrence of VF. All patients received an ICD in addition to randomized therapy [68]. The risk of the primary outcome, a composite of cardiac death, sustained VT/VF, or syncopal ICD shock, was significantly reduced by amiodarone. Patients on amiodarone were less likely to receive ICD shocks and syncope followed by a shock from a defibrillator was less common in patients treated with amiodarone. These results suggested a benefit of amiodarone over class I AADs. However, it is uncertain whether the observed benefit is due to the harmful effect of conventional AAD therapy and/or a beneficial effect of amiodarone, or most likely, their combination.
Intravenous amiodarone is the preferred AAD for incessant VT or frequent symptomatic VT episodes and severe LV dysfunction because in contrast to many other AADs it does not increase mortality. Two placebo-controlled studies analyzed the effects of amiodarone on the risk of resuscitated VF or arrhythmic death among survivors of MI treated with β-blockers at baseline reaching contradictory results. In the EMIAT trial, amiodarone did not modify all-cause mortality and cardiac mortality as compared with placebo [69]. Conversely, in the CAMIAT trial, amiodarone reduced the incidence of VF or arrhythmic death among survivors of acute MI with frequent or repetitive frequent or repetitive ventricular premature depolarisations. Similarly, several major trials in patients with a history of HF and LV dysfunction, arrived at conflicting results [70]. The GESICA trial suggested low-dose amiodarone improved survival, decreased hospital admissions for congestive HF, and improved functional class in patients with HF independently of the presence of complex ventricular arrhythmias [71]. However, in the STAT-CHF trial recruiting patients with HF (LVEF ≤40%) and ≥ 10 PVBs/h, amiodarone as compared to placebo was effective in suppressing ventricular arrhythmias, slowed heart rate and increased LVEF by 42% at 2 years, but it did not reduce the incidence of SCD or prolong survival among patients with HF, except for a trend toward reduced mortality among those with nonischemic cardiomyopathy [72]. In the SCD-HeFT study, recruiting patients with New York Heart Association (NYHA) class II-III (LVEF≤35%), amiodarone had no favorable effect on survival, whereas ICD therapy reduced overall mortality by 23% [73]. In a meta-analysis of 13 trials recruiting patients with recent MI or congestive HF, prophylactic amiodarone reduced the rate of arrhythmic/sudden death (29%), but it only displayed a modest reduction (13%) on total mortality [53]. The treatment benefit was uniform across the congestive HF and post–MI trial patients and was independent of major prognostic variables, such as LV function. Furthermore, a contemporary study in patients with post-acute MI with HF and/or LV systolic dysfunction from VALIANT trial, amiodarone use was associated with an excess in early and late all-cause and cardiovascular mortality [74]. Thus, further studies are needed to define the role of amiodarone in post-MI patients with HF and/or LV systolic dysfunction.
Dofetilide
Dofetilide is a methanesulfonamide drug not available in Europe. It selectively blocks the IKr and unlike most other AADs has minimal effects on other ion channels [75]. As a consequence, dofetilide prolongs dose-dependently the APD and refractoriness of atrial and ventricular myocardium (but the effect is more prominent in the atria) and accessory pathways, without slowing intracardiac conduction. Like ibutilide and sotalol, dofetilide exhibits the phenomenon of reverse use-dependence, so that the prolongation of APD and refractoriness diminished as the heart rate increases, while at slow heart rates the prolongation of the APD and the risk of early afterdepolarizations (proarrhythmia) increases [75]. It prolongs the QT and JT intervals but has no effect on heart rate, intracardiac conduction (no changes in the PR, QRS, A-H and H-V intervals) or significant hemodynamic effects and appears to be hemodynamically safe in patients with HF or a prior MI. Drug potency is affected by extracellular potassium concentration, and hypokalemia and hyperkalemia increases and decreases drug potency, respectively [76].
Pharmacokinetics (Table 3.2)
Dofetilide is well absorbed (bioavailability 92–95%) and peak plasma levels are reached within 2–3 h. It binds to plasma proteins (60–70%) and 80% of the dose is excreted in urine (80% as unchanged dofetilide) and the remaining 20% as inactive or minimally active metabolites. Its t½ is 7–13 hours [11, 75, 77].
Adverse Effects (Table 3.3)
The most significant adverse effect of dofetilide is QT prolongation–related TdP. Rates of TdP ranged from 1% to ~3% in the DIAMOND trials [78]. The risk of TdP is highest at the time of drug initiation (80% within the first 3 days of therapy), in women, patients with severe HF, recent MI, hypokalemia, prolonged baseline QT or after conversion from AF to SR. The risk can be reduced maintaining normal serum potassium and magnesium levels, and following the manufacturer’s algorithm in patients with renal disease, bradycardia, or baseline QT interval. To minimize the risk of proarrhythmia, patients initiated or re-initiated on dofetilide should be placed for a minimum of 3 days in a facility that can provide calculations of creatinine clearance, continuous ECG monitoring, and cardiac resuscitation. Other adverse effects include headache, chest pain, dizziness, respiratory tract infection, dyspnea, insomnia, rash, flu-like syndrome, nausea and diarrhea. There are no well-controlled studies that have been done in pregnant women (Pregnancy Category: C).
Drug Interactions
Dofetilide does not inhibit or induce any CYP450 enzyme isoforms. Avoid its combinations with drugs that prolong the QT interval, other antiarrhythmic agents or potent CYP3A4 inhibitors (cimetidine, dolutegravir, grapefruit juice, HIV protease inhibitors, macrolide antibiotics, verapamil, prochlorperazine) that increase its plasma levels [11, 77].
Contraindications and Cautions
See Table 3.3.
Dosage and Administration
See Table 3.5.
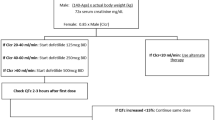
Dofetilide therapy should be initiated in-hospital under continuous ECG monitoring because of the risk of excessive QT prolongation, periodic calculation of creatinine clearance (CrCl) and expert personnel for the treatment of ventricular arrhythmias [24, 26, 28]. Dosage adjustments are determined by QTc changes and CrCl. Renal function and QTc should be monitored every 3 months. The drug is contraindicated if the baseline QTc >440 m or the CrCl <20 mL/min. If 2–3 h after the first dose of dofetilide the QTc increased by >15% compared with baseline or the QTc is >500 ms (550 ms in patients with ventricular conduction abnormalities), subsequent dosing should be reduced by 50%. At 2–3 h after each subsequent dose, determine QTc and if at any time after the second dose the QTc is >500 ms (550 ms in patients with ventricular conduction abnormalities), dofetilide should be discontinued [24, 26, 28].
Indications
Dofetilide is indicated for the acute conversion of recent-onset AF/Af (≤7 days) and the maintenance of SR (Table 3.6) [24, 27, 79, 80]. Dofetilide can be used in patients with structural heart disease or coronary artery disease. In the SAFIRE-D study, 70% of the pharmacological conversions occurred within 24 h and 91% within 36 h [80]. Furthermore, dofetilide appears safe and effective in preventing AF in patients refractory to other AADs undergoing catheter ablation [81]. Between 40% and 60% of patients on dofetilide remained in SR at 1 year (25% on placebo). Dofetilide is not associated with an increased mortality risk in patients with AF/Af [32].
Dofetilide restores and maintains SR in patients with congestive heart failure or recent MI and left ventricular dysfunction [82,83,84]. In patients with AF/Af and significant LV dysfunction, the DIAMOND studies showed that dofetilide was superior to placebo for the restoration and maintenance of SR and even when it had no effect on all-cause mortality, restoration and maintenance of SR was associated with significant reduction in mortality. Additionally, dofetilide reduced the risk for either all-cause or HF rehospitalization. Thus, dofetilide is an alternative to amiodarone in patients with AF/Af and LV dysfunction. In patients with AF/Af, severe LV dysfunction and recent MI, dofetilide did not affect all-cause or cardiac mortality, or total arrhythmic deaths. Thus, unlike flecainide and propafenone, dofetilide can be used in patients with structural heart disease or coronary artery disease.
Oral dofetilide may be reasonable in: (a) patients with AVRT and/or pre-excited AF who are not candidates for, or prefer not to undergo, catheter ablation [26]. In patients with paroxysmal supraventricular tachycardia (PSVT) dofetilide and propafenone were equally effective in preventing recurrences or decreasing the frequency of PSVT compared with placebo [85]. (b) For prevention of recurrent atrial tachycardia or Af in adult congenital heart disease patients, the long-term efficacy of the drug (defined by either complete suppression or partial improvement of symptoms) ranges from 70% to 85% [86, 87].
Dofetilide decreases the VF threshold in patients undergoing defibrillation testing prior to ICD implantation, suppresses the inducibility of VT and decreases the frequency of ICD shocks. It is as effective as sotalol in preventing the induction of sustained VT, but is significantly better tolerated during the acute phase [88] and in patients with an ICD and ventricular arrhythmias, dofetilide decreases the frequency of VT/VF and ICD shocks even when other ADDs, including amiodarone, are ineffective [89].
However, dofetilide is not frequently used because therapy must be started in an inpatient setting for 3 days and the risk of proarrhythmia. Thus, it should be reserved under ECG monitoring for highly symptomatic patients, in patients with depressed LVEF, who are not candidates for catheter ablation and/or when other AADs are ineffective or contraindicated.
Dronedarone
Dronedarone is a noniodinated benzofuran derivative with a structure similar to that of amiodarone. The lack of the iodine moiety minimizes the risk of thyroid toxicity, and the addition of a methyl-sulfonyl group decreases its lipophilicity and tissular distribution which is expected to reduce organ toxicity due to tissular accumulation and to shorten its half-life [90]. Like amiodarone, dronedarone blocks Na+, Ca2+ (ICaL) and several K+ currents (Ito, IKur, IKr, IKs, IK1 and IKAch) and produces a non- competitive inhibition of α- and β-adrenergic receptors and a vasodilator effect mediated via the ICaL blockade and activation of the NO pathway [90,91,93]. Dronedarone and amiodarone exhibit similar effects on the ICaL, IKr and IKs, but dronedarone is a more potent blocker of INa and IKAch and exhibits more potent non-competitive antiadrenergic effects than amiodarone.
Electrophysiological Actions
Dronedarone prolongs the APD and refractoriness in all cardiac tissues, an effect independent of the rate of stimulation, and reduces transmural dispersion of repolarization. It slows heart rate and AV nodal conduction and prolongs the RR, PR, QT, JT and A-H intervals on the ECG with no change in H-V and QRS intervals [91, 92]. Dronedarone decreases blood pressure, myocardial contractility and slightly increases the defibrillation threshold. Dronedarone has little effect on cardiac performance except in patients with compromised LVEF and should not be used in those with clinical signs of HF.
Pharmacokinetics (Table 3.2)
Dronedarone is rapidly and well absorbed after oral administration (70–90%), but it undergoes extensive first-pass metabolism, so that oral bioavailability is ~5% (15% when administered with a high-fat meal) [11, 90]. Dronedarone is extensively metabolized in the liver via CYP3A4 (and CYP2D6) to an active N-debutyl metabolite. Peak plasma levels of dronedarone and its metabolite are reached within 3–6 h and steady-state plasma levels within 4–8 days. Dronedarone and its active metabolite bind to plasma proteins (>98%) and are widely distributed (Vd 20 L/kg), crossing the blood–brain and placental barriers. Dronedarone presents a lower Vd (tissular accumulation) and a shorter a t½ (13–19 h) than amiodarone and 85% of the drug being excreted in feces. Dronedarone and its metabolite are completely eliminated from the body within 2 weeks after the end of treatment. Drug pharmacokinetics is not influenced by age, gender, weight, or renal function, but dose adjustments are recommended in patients with severe hepatic dysfunction [11, 90].
Adverse Effects (Table 3.3)
The most frequent are gastrointestinal (diarrhea, nausea, abdominal pain, vomiting, dyspepsia), abnormal liver function tests, asthenia, bradycardia, and QT prolongation. Uncommon adverse effects include: headache, rash and photosensitivity. Dronedarone increases serum creatinine levels due to partial inhibition of the tubular organic cationic transporter system, but the drug does not affect the GFR [94]. Sinus bradycardia is less frequent than with amiodarone and TdP have not been reported.
The ANDROMEDA trial which randomized patients with LV systolic dysfunction (LVEF 35%) and NYHA class III or IV symptoms within the prior month was prematurely discontinued because of increased mortality in the dronedarone group related to the worsening of HF [95]. In the PALLAS trial, dronedarone also increased rates of HF, stroke, and death from cardiovascular causes in patients with permanent AF who were at risk for major vascular events [96]. Thus, dronedarone should not be used in patients with recently decompensated HF or with permanent AF.
Dronedarone may cause fetal harm and it is contraindicated in women who are, or may become, pregnant (Pregnancy category X); it is not known whether dronedarone is excreted in human milk.
Drug Interactions
Dronedarone is a moderate inhibitor of CYP3A4 and CYP2D6, and a potent inhibitor of P-gp and is metabolized by CYP3A4, so that it can present many drug interactions [11].
Coadministration of dronedarone with β-blockers, verapamil, or diltiazem increases their depressant effects on sino-atrial and AV nodes. Because diltiazem and verapamil are weak CYP3A4 inhibitors, in patients treated with dronedarone, diltiazem and verapamil should be initiated at low doses and dose uptitration should be done after ECG assessment. Class I or III antiarrhythmics increase the risk of proarrhythmia and should be discontinued before the administration of dronedarone. Dronedarone increases the plasma levels of digoxin (a P-gp substrate) and the risk of bradycardia and AV block. In the PALLAS trial, the use of digoxin was associated with an increased risk of arrhythmia or sudden death in dronedarone-treated patients [96]. Thus, the dose of digoxin should be halved and ECG and digoxin plasma levels carefully monitored.
Dronedarone is primarily metabolized by CYP3A4. Potent CYP3A4 inhibitors [azole antifungals (itraconazole, pozaconazole, voriconazole), cimetidine, cyclosporine, macrolides (clarithromycin, telithromycin), nefazodone, ritonavir, grapefruit juice] and inducers (carbamazepine, phenobarbital, phenytoin, rifampin, St John’s Wort) significantly increase and decrease, respectively, exposure of dronedarone and should be administered with caution or avoided [90, 92]. Reduce the dose of dronedarone when coadministered with moderate CYP3A4 inhibitors (diltiazem, erythromycin, verapamil). Dronedarone can increase the exposure of statins that are substrates of CYP3A4 and/or P-gp (atorvastatin, lovastatin, simvastatin) and the risk of myopathy; thus, the dose of lovastatin and simvastatin should be limited to 20 mg/day and 10 mg/day, respectively. Dronedarone may increase the plasma levels of immunosupressants (tacrolimus, sirolimus, everolimus, cyclosporine); monitor their plasma concentrations, and adjust doses as appropriate [11]. Unlike amiodarone, dronedarone does not modify the INR, but it increases the exposure of dabigatran and this combination should be avoided. Avoid the combination of dronedarone with QT-prolonging drugs.
Contraindications and Cautions
See Table 3.3.
Dosage and Administration
See Table 3.5.
Indications
Dronedarone is approved for the maintenance of SR after successful cardioversion in clinically stable adult patients with paroxysmal or persistent AF [97,98,99], but it is less effective than amiodarone [32, 100, 101]. In patients with paroxysmal or persistent AF or Af with additional risk factors for death, the ATHENA trial showed that dronedarone significantly reduced the composite outcome of first hospitalization due to cardiovascular events or death as compared with placebo [102]. Additionally, dronedarone decreased the mean ventricular rate during the recurrence of AF [98, 99]. In a short-term study, amiodarone was significantly more effective than dronedarone at preventing recurrence of AF, but was associated with significantly more adverse thyroid, neurological, ocular, and dermatological adverse effects [103].
Ibutilide
Ibutilide is a methanesulfonamide derivative that prolongs cardiac repolarization through the inhibition of the IKr and the activation of the late inward sodium current (INaL) during the plateau phase of the cardiac action potential [104].
Electrophysiologic Actions
Like other class III agents, ibutilide prolongs APD and refractoriness of the atrial and ventricular myocardium, AV node, His-Purkinje system, and accessory pathways, prolongs the QT and JT intervals and produces a mild slowing of the sinus rate, but it has no effect on the PR, A-H, QRS and H-V intervals [105,106,107]. The prolongation of QT interval is related to the dose, rate of infusion and heart rate. Indeed, the prolongation of APD and refractoriness becomes less pronounced at higher tachycardia rates, i.e. ibutilide exhibits reverse use dependence. Ibutilide has no significant hemodynamic effects or negative inotropic effects and can be used safely in patients with structural heart disease and prior MI. It can lower the energy threshold required for VF.
Pharmacokinetics (Table 3.2)
Ibutilide is administered IV. It binds to plasma proteins (40%), presents a large Vd (11 L/kg) and is extensively metabolized in the liver; one hydroxy metabolite has weak class III effects. Ibutilide is renally excreted and its t½ presents a marked interpatient variability (2–12 h) [107]. The pharmacokinetics of ibutilide is independent of dose, age and LV function.
Adverse Effects (Table 3.3)
The most serious adverse effect is a dose-dependent QT prolongation that returns to normal values 2–4 h after stopping the IV infusion [104,105,106]. TdP can occur in up to 4% of patients during or shortly after the infusion period (within the first 4–6 h of dosing) and the risk increases in patients with LVEF <20% [108]. Non-sustained monomorphic VT may occur in ~5% and proarrhythmia requiring cardioversion occurred in ~2% of treated patients [109, 110]. To reduce the risk of proarrhythmia, high doses of ibutilide and rapid infusion rates should be avoided; IV pretreatment with magnesium sulfate reduces the incidence of ventricular arrhythmias, including TdP [111, 112]. Therefore, patients receiving ibutilide should undergo continuous ECG monitoring during administration and for at least 4 hours after completion of dosing. Other noncardiac adverse effects are headache, bradycardia, hypotension, palpitations and nausea [11, 109]. The safety of ibutilide during pregnancy has not been well studied, and its use during pregnancy should be restricted to patients in whom no safer alternative exists (pregnancy category: C).
Drug Interactions (Table 3.4)
Class I or class III AADs should not be given concurrently with ibutilide (or within 4 h after infusion); other antiarrhythmics should be withheld prior to conversion with ibutilide.
Contraindications and Cautions
See Table 3.3.
Dosage and Administration
See Table 3.5.
Because of the risk for ventricular proarrhythmia, ibutilide should be initiated in-hospital on continuous ECG monitoring by personnel trained in identification and treatment of ventricular arrhythmias during the drug administration and for 6–8 h thereafter and with resuscitation facilities available. The infusion should be stopped if the QTc is >500 ms or conversion to SR occurs. Although dose adjustment is not necessary in patients with hepatic or renal impairment, patients with liver disease may metabolize ibutilide more slowly and require longer postinfusion monitoring [107].
Indications
Intravenous ibutilide is indicated for the rapid conversion of recent-onset AF/Af (≤ 7 days) to SR, but it is more effective for the conversion of Af (Table 3.6) [105,106,107, 110, 113,114,115]. In AF or Af, a single dose of ibutilide successfully converted 53% patients; an additional 22% patients is converted with the second dose, which resulted in an overall conversion rate of 75% [116]. The mean termination time was 27 min after the start of the infusion. Ibutilide was more effective than amiodarone, procainamide or sotalol in converting recent-onset Af to SR; however, ibutilide and amiodarone are equally effective in converting recent-onset AF to SR [33, 105, 106, 108, 113, 117]. In patients with persistent AF/Af the efficacy was 44% and 49%, respectively. Ibutilide is safe and effective for the rapid conversion of AF and Af after cardiac surgery (conversion rate 57% at the dose of 1 mg) [115]. Ibutilide also facilitates electrical cardioversion in patients with AF refractory to prior electrical cardioversions and prevent recurrent AF [24, 27]. All 50 patients receiving ibutilide before electrical cardioversion achieved SR while only 36 of 50 who did not receive the drug. The 14 patients who did not respond to electrical cardioversion were successfully cardioverted when a second attempt was made after ibutilide pretreatment [108]. However, because of the risk of proarrhythmia, ibutilide should not be used in patients with frequent short episodes of paroxysmal AF because even if the drug is effective to terminate the arrhythmia it is not useful for long-term prevention. The effectiveness of ibutilide for treatment of focal AT is unclear [26, 105, 106].
Furthermore, ibutilide prolongs accessory pathway refractoriness and can temporarily slow ventricular rate during pre-excited AF and may be used for the pharmacologic cardioversion of micro-reentrant AT [118] and AV reentrant tachycardia [119].
Sotalol
Sotalol is a non-selective β1-adrenoceptor blocker without intrinsic sympathomimetic activity that, in addition, inhibits the K+ current IKr, i.e., it is a mixed class II and class III AAD [11, 120, 121].
Electrophysiological Actions
Sotalol is a racemic mixture of dextro- and levo-isomers. Both isomers have comparable class III activity, but l-sotalol is responsible for the β-blocking activity [121, 122]. The β-blocking effects appear at low oral doses (half-maximal at 80 mg/day), while the class III effects are observed at doses >160 mg/day. Sotalol dose-dependently prolongs atrial and ventricular APD and refractoriness, slows heart rate, decreases AV nodal conduction, increases AV nodal refractoriness and prolongs the RR, PR, A-H and QT intervals of the ECG, but does not modify the QRS and H-V intervals. It also slows conduction along any bypass tract in both directions. The prolongation of the APD is greater at slower rates (reverse use-dependence) and under these conditions, sotalol may cause early afterdepolarizations triggering TdP. Unlike amiodarone, sotalol appears to reduce the defibrillation threshold [26].
Hemodynamics. Sotalol exerts a direct negative inotropic effect through its β-blocker activity, but it may indirectly increase Ca2+ entry and cardiac contractility by prolonging repolarization, particularly at slow heart rates. However, in patients with reduced LVEF, sotalol can decrease the cardiac index, increase filling pressures and precipitate overt HF [120, 121]. Therefore, it must be used cautiously in patients with LV dysfunction or HF and should be avoided in patients with LVEF <20%, although is well tolerated in those with normal cardiac function. In 415 patients with AF/Af and PSVT, new or worsening HF occurred in 1.2% of patients, but in these studies patients with NYHA classes III-IV were excluded.
Pharmacokinetics (Table 3.2)
Sotalol is completely absorbed (oral bioavalability 90–100%), reaching peak plasma concentrations within 2.5–4 h and steady-sate plasma levels in 2–3 days. It does not bind to plasma proteins, is not metabolized in the liver and is excreted unchanged primarily by the kidneys. Its t½ is 7–18 h. The dose must be reduced in the elderly and in patients with renal impairment [11, 120].
Adverse Effects (Table 3.3)
They are those commonly seen with other β-blockers, including bradycardia and AV block, asthenia, fatigue, hypotension, dizziness and cardiac ischemia after abrupt discontinuation. Proarrhythmia is the most serious adverse effect. TdP appears in 0.3% of patients treated with ≤240 mg/day, in 4.4% of those treated with 480 mg/day, in ~1.3% of patients when the QTc <500 ms and in 3.4–5.6% when the QTc is between 500–550 ms. In the PAFAC trial TdP appear in 1% of patients [123]. Proarrhytmia was probably the cause of the increased mortality observed with d-sotalol in patients with LV dysfunction post-MI [32, 124]. The risk of TdP increases in females, at high doses (>320 mg/day) and in patients with bradycardia, baseline QTc intervals >450 ms, electrolyte disturbances (hypokalemia and hypomagnesaemia), severe LV failure, treated with QT-prolonging drugs or with congenital long-QT syndrome.
Sotalol crosses the placenta and is present in breast milk (Pregnancy category B). β-blockers are commonly used in pregnant women with cardiovascular conditions and are associated with intrauterine growth retardation [23].
Drug interactions (Table 3.4)
Sotalol should be used with caution or avoided in patients treated with QT-prolonging drugs and additive effects are expected if co-administered with other β-blockers. Class IA, IC and III AADs are not recommended as concomitant therapy with sotalol. Coadministration with digoxin can increase the risk of bradycardia and AVB and coadministration with diltiazem or verapamil may increase the risk of hypotension, bradycardia, or AVB. In diabetic patients sotalol may mask symptoms of hypoglycemia (tachycardia, tremor) or worsen hyperglycemia; so, the doses of insulin or antidiabetic drugs may require adjustment. β2-receptor agonists should be administered at higher dosages in patients treated with sotalol. Antacids containing aluminum hydroxide and magnesium hydroxide given 2 h or less before sotalol may reduce its bioavailability.
Contraindications and Cautions
See Table 3.3.
Dosage and Administration
See Table 3.5.
Patients initiated or reinitiated on sotalol should be placed in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring for a minimum of 3 days [24,25,26,27,28]. The starting oral dose is 80 mg bid in patients with a QT <450 ms and a CrCl >60 mL/min. Doses may be increased in increments of 80 mg/day every 2–3 days to reach steady-state levels (maximum dose of 160 mg bid) provided the QTc interval <500 ms. Higher doses (480–640 mg/day) are used in patients with refractory life-threatening ventricular arrhythmias. Because sotalol can cause TdP or severe bradycardia, it may be considered to initiate the treatment in-hospital, particularly in patients in whom sinus bradycardia may cause syncope or when the conversion of AF/Af to SR prolong the QT interval. The use of high doses of sotalol requires careful ECG monitoring, especially in patients with impaired renal function.
In patients with ventricular arrhythmias and a CrCl between 30 and 59 mL/min sotalol must be administered od; with a CrCl between 10 and 29 mL/min the dose should be administered every 36–48 h, and with a CrCl <10 mL/min the dose should be individualized.
In patients with AF/Af and renal impairment (CrCl <60 mL/min) sotalol should be administered bid; if the CrCl is between 40 and 59 mL/min sotalol should be administered od; if the CrCl <40 mL/min sotalol is contraindicated.
Indications
Sotalol is approved for the:
-
1.
Maintenance of SR following cardioversion of recurrent AF/Af (Table 3.6). For the maintenance of SR sotalol is as effective as flecainide or propafenone, but it can be administered to patients with structural heart disease or coronary artery disease where class IC drugs are contraindicated and without an additional agent to slow AV-nodal conduction [26, 33]. However, sotalol is less effective than amiodarone. In patients with persistent AF amiodarone and sotalol were equally efficacious in converting AF to SR but amiodarone was superior for maintaining SR; however, both drugs had similar efficacy in patients with ischemic heart disease [125]. Furthermore, in the CTAF trial, after a mean of 16 months of follow-up 65% of patients treated with amiodarone and 37% of patients treated with sotalol or propafanone remained free of AF recurrence [30]. Similarly, in a large meta-analysis, efficacy of sotalol is similar to that of most AADs other than amiodarone [32]. Thus, sotalol can replace amiodarone when adverse effects are expected.
Pretreatment with sotalol can facilitate DC cardioversion and prevent recurrent AF and in relapses to AF after successful cardioversion, repeating DC cardioversion after sotalol facilitates the successful cardioversion (Table 3.6). Sotalol is also effective to decrease the incidence of POAF and to control ventricular rate during AF/Af [43, 126].
-
2.
Supraventricular tachycardias. Sotalol may be reasonable for ongoing management in patients with SVT who are not candidates for, or prefer not to undergo, catheter ablation (Table 3.7) [26, 127]. Additionally, sotalol slows the ventricular response to atrial tachyarrhythmias and offers an effective alternative to DC cardioversion in adults and adolescents with congenital heart disease and hemodynamically stable atrial tachyarrhythmias [128]. One study randomized patients with reentrant SVT (AVNRT or AVRT) or other atrial tachyarrhythmias (eg, AF, Af, AT) to sotalol (80–160 mg bid) or placebo and found significant reductions in recurrence risk, including for patients with reentrant SVT, with no proarrhythmic adverse effects [127]. However, because of the potential for proarrhythmia, sotalol should be reserved for patients with SVT who are not candidates for, or prefer not to undergo, catheter ablation and for whom other AADs are ineffective or cannot be prescribed.
-
3.
Treatment of life-threatening sustained ventricular arrhythmias and acute conversion of hemodynamically stable monomorphic sustained VT (Table 3.8). In patients with hemodynamically stable VT, sotalol was superior to lidocaine for the acute termination of sustained VT [129]. In patients with life-threatening arrhythmias (sustained VT/VF) which were also inducible by programmed electrical stimulation (PES), the ESVEM trial showed that sotalol was significantly more efficacious at decreasing death and ventricular arrhythmias than other six class I AADs [130]. In patients who had received an ICD for secondary prevention of serious malignant ventricular arrhythmias, the combination of amiodarone with a β-blocker prevented shocks better than the β-blocker alone, although sotalol alone tended to reduce ICD shocks [131]. However, in another placebo-controlled study in patients with ICD, sotalol reduced the risk of death from any cause or the delivery of a first shock for any reason by 48% whether or not ventricular function was depressed. Sotalol also prevented the occurrence of shocks in response to supraventricular arrhythmias [132]. Two studies that compared the efficacy of metoprolol and sotalol yielded contradictory results. In one trial, sotalol was less effective than metoprolol for reducing recurrence of ventricular arrhythmia events; however, this study did not include inappropriate shocks that were a prominent feature in the previous studies [133]. In another trial, metoprolol was as efficacious as sotalol in preventing VT/VF recurrences in patients with an ICD [134]. In patients with sustained VT/VF and a ICD, sotalol reduced the recurrences in comparison to no AAD treatment and the frequency of ICD discharges, but it did not improve survival [135].
Because of its proarrhythmic risk, the use of sotalol is not recommended in patients with less severe arrhythmias (non-sustained VT or supraventricular tachyarrhythmias), even if symptomatic. Sotalol can be used safely in patients with coronary artery disease, but it should also be avoided in patients with severe HF (NYHA functional class III or IV). Although specific studies in treating atrial arrhythmias after MI have not been conducted, the administration of sotalol started 5–15 days after the MI did not increase rate after a 12 month follow-up [136].
References
Tamargo J, Delpón E. Pharmacologic bases of antiarrhythmic therapy. Chapter 54. In: Zipes DP, Jalife J, Stevenson WG, editors. Cardiac electrophysiology. 8th ed. Estados Unidos: Elsevier; 2017. p. 513–24.
Singh BN. Antiarrhythmic actions of amiodarone: a profile of a paradoxical agent. Am J Cardiol. 1996;78:41–53.
Kodama I, Kamiya K, Toyama J. Cellular electropharmacology of amiodarone. Cardiovasc Res. 1997;35:13–29.
Tamargo J. Happy 50th anniversary of amiodarone (1969–2019). Int J Cardiol. 2019;293:115–6.
Vamos M, Hohnloser SH. Amiodarone and dronedarone: an update. Trends Cardiovasc Med. 2016;26:597–602.
Connolly SJ. Evidence-based analysis of amiodarone efficacy and safety. Circulation. 1999;100:2025–34.
Harjai KJ, Licata AA. Effects of amiodarone on thyroid function. Ann Intern Med. 1997;126:63–73.
Wellens HJJ, Brugada P, Abdollah H, Dassen WR. A comparison of the electrophysiologic effects of intravenous and oral amiodarone in the same patient. Circulation. 1984;69:120–4.
Epstein AE, Olshansky B, Naccarelli GV, Kennedy JI Jr, Murphy EJ, Goldschlager N. Practical management guide for clinicians who treat patients with amiodarone. Am J Med. 2016;129:468–75.
Shinagawa K, Shiroshita-Takeshita A, Schram G, Nattel S. Effects of antiarrhythmic drugs on fibrillation in the remodeled atrium: insights into the mechanism of the superior efficacy of amiodarone. Circulation. 2003;107:1440–6.
Tamargo J, Caballero R, Delpón E. Chapter 8.1: Cardiovascular drugs—from A to Z. In: Kaski JC, Kjeldsen K, editors. The ESC handbook on cardiovascular pharmacotherapy. 2nd ed. Oxford: Oxford University Press; 2019. p. 413–812.
Meng X, Mojaverian P, Doedee M, Lin E, Weinryb I, Chiang ST, et al. Bioavailability of amiodarone tablets administered with and without food in healthy subjects. Am J Cardiol. 2001;87:432–5.
Vorperian VR, Havighurst TC, Miller S, January CT. Adverse effects of low dose amiodarone: a meta-analysis. J Am Coll Cardiol. 1997;30:791–8.
Ruzieh M, Moroi MK, Aboujamous NM, Ghahramani M, Naccarelli GV, Mandrola J, et al. Meta-analysis comparing the relative risk of adverse events for amiodarone versus placebo. Am J Cardiol. 2019. pii: S0002-9149(19)31046-X.
Zimetbaum P. Amiodarone for atrial fibrillation. N Engl J Med. 2007;356:935–41.
Passman RS, Bennett CL, Purpura JM, Kapur R, Johnson LN, Raisch DW, et al. Amiodarone-associated optic neuropathy: a critical review. Am J Med. 2012;125:447–53.
Orr CF, Ahlskog JE. Frequency, characteristics, and risk factors for amiodarone neurotoxicity. Arch Neurol. 2009;66:865–9.
Papiris SA, Triantafillidou C, Kolilekas L, Markoulaki D, Manali ED. Amiodarone: review of pulmonary effects and toxicity. Drug Saf. 2010;33:539–58.
Colby R, Geyer H. Amiodarone-induced pulmonary toxicity. JAAPA. 2017;30:23–6.
Elnaggar MN, Jbeili K, Nik-Hussin N, Kozhippally M, Pappachan JM. Amiodarone-induced thyroid dysfunction: a clinical update. Exp Clin Endocrinol Diabetes. 2018;126:333–41.
Cohen-Lehman J, Dahl P, Danzi S, Klein I. Effects of amiodarone therapy on thyroid function. Nat Rev Endocrinol. 2010;6:34.
Bartalena L, Bogazzi F, Braverman LE, Braverman LE. Effects of amiodarone administration during pregnancy on neonatal thyroid function and subsequent neurodevelopment. J Endocrinol Investig. 2001;24:116–30.
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cıfkova R, De Bonis M, et al. ESC Scientific Document Group. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39:3165–241.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. ACC/AHA Task Force Members. 2014 AHA/ACC/HRS Guideline for the management of patients with atrial fibrillation: Executive Summary. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071–4.
Priori S, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2015;36:2793–867.
Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, et al. 2015 ACC/AHA/HRS Guideline for the management of adult patients with supraventricular tachycardia: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016;67:1575–623.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS: The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC Endorsed by the European Stroke Organisation (ESO). Eur Heart J. 2016;37:2893–962.
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Heart Rhythm. 2018;15:e773-e189.
Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, et al.; ESC Scientific Document Group. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2019. pii: ehz467. https://doi.org/10.1093/eurheartj/ehz467.
Roy D, Talajic M, Dorian P, Connolly S, Eisenberg MJ, Green M, et al. Amiodarone to prevent recurrence of atrial fibrillation. Canadian Trial of Atrial Fibrillation Investigators. N Engl J Med. 2000;342:913–20.
AFFIRM First Antiarrhythmic Drug Substudy Investigators. Maintenance of sinus rhythm in patients with atrial fibrillation: an AFFIRM substudy of the first antiarrhythmic drug. J Am Coll Cardiol. 2003;42(1):20–9.
Lafuente-Lafuente C, Valembois L, Bergmann JF, Belmin J. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst Rev. 2015;3:CD005049.
Miller MR, McNamara RL, Segal JB, Kim N, Robinson KA, Goodman SN, et al. Efficacy of agents for pharmacologic conversion of atrial fibrillation and subsequent maintenance of sinus rhythm: a meta-analysis of clinical trials. J Fam Pract. 2000;49:1033–46.
Chevalier P, Durand-Dubief A, Burri H, Cucherat M, Kirkorian G, Touboul P. Amiodarone versus placebo and class Ic drugs for cardioversion of recent-onset atrial fibrillation: a meta-analysis. J Am Coll Cardiol. 2003;41:255–62.
Singh SN, Tang XC, Reda D, Singh BN. Systematic electrocardioversion for atrial fibrillation and role of antiarrhythmic drugs: a substudy of the SAFE-T trial. Heart Rhythm. 2009;6:152–5.
Kochiadakis GE, Igoumenidis NE, Parthenakis FI, Chlouverakis GI, Vardas PE. Amiodarone versus propafenone for conversion of chronic atrial fibrillation: results of a randomized, controlled study. J Am Coll Cardiol. 1999;33:966–71.
Singh BN, Singh SN, Reda DJ, Tang XC, Lopez B, Harris CL, et al. Amiodarone versus sotalol for atrial fibrillation. N Engl J Med. 2005;352:1861–72.
Vijayalakshmi K, Whittaker VJ, Sutton A, Campbell P, Wright RA, Hall JA, et al. A randomized trial of prophylactic antiarrhythmic agents (amiodarone and sotalol) in patients with atrial fibrillation for whom direct current cardioversion is planned. Am Heart J. 2006;151:863.e1–6.
Reisinger J, Gatterer E, Heinze G, Wiesinger K, Zeindlhofer E, Gattermeier M, et al. Prospective comparison of flecainide versus sotalol for immediate cardioversion of atrial fibrillation. Am J Cardiol. 1998;81:1450–4.
Channer KS, Birchall A, Steeds RP, Walters SJ, Yeo WW, West JN, et al. A randomized placebo-controlled trial of pre-treatment and short- or long-term maintenance therapy with amiodarone supporting DC cardioversion for persistent atrial fibrillation. Eur Heart J. 2004;25:144–50.
Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35:2733–79.
Darkner S, Chen X, Hansen J, Pehrson S, Johannessen A, Nielsen JB, et al. Recurrence of arrhythmia following short-term oral AMIOdarone after CATheter ablation for atrial fibrillation: a double-blind, randomized, placebo-controlled study (AMIO-CAT trial). Eur Heart J. 2014;35:3356–64.
Arsenault KA, Yusuf AM, Crystal E, Healey JS, Morillo CA, Nair GM, et al. Interventions for preventing post-operative atrial fibrillation in patients undergoing heart surgery. Cochrane Database Syst Rev. 2013;1:CD003611.
Burgess DC, Kilborn MJ, Keech AC. Interventions for prevention of postoperative atrial fibrillation and its complications after cardiac surgery: a meta-analysis. Eur Heart J. 2006;27:2846–57.
Zhu J, Wang C, Gao D, Zhang C, Zhang Y, Lu Y, Gao Y. Meta-analysis of amiodarone versus beta-blocker as a prophylactic therapy against atrial fibrillation following cardiac surgery. Intern Med J. 2012;42:1078–87.
Chatterjee S, Sardar P, Mukherjee D, Lichstein E, Aikat S. Timing and route of amiodarone for prevention of postoperative atrial fibrillation after cardiac surgery: a network regression meta-analysis. Pacing Clin Electrophysiol. 2013;36:1017–23.
Kowey PR, Levine JH, Herre JM, Pacifico A, Lindsay BD, Plumb VJ, et al. Randomized double-blind comparison of intravenous amiodarone and bretylium in the treatment of patients with recurrent, hemodynamically destabilizing ventricular tachycardia or fibrillation. The Intravenous Amiodarone Multicenter Investigators Group. Circulation. 1995;92:3255–63.
Heldal M, Atar D. Pharmacological conversion of recent-onset atrial fibrillation: a systematic review. Scand Cardiovasc J Suppl. 2013;47:2–10.
Letelier LM, Udol K, Ena J, Weaver B, Guyatt GH. Effectiveness of amiodarone for conversion of atrial fibrillation to sinus rhythm: a meta-analysis. Arch Intern Med. 2003;163:777–85.
Simonian SM, Lotfipour S, Wall C, Langdorf MI. Challenging the superiority of amiodarone for rate control in Wolff-Parkinson-White and atrial fibrillation. Intern Emerg Med. 2010;5:421–6.
Claro JC, Candia R, Rada G, Baraona F, Larrondo F, Letelier LM. Amiodarone versus other pharmacological interventions for prevention of sudden cardiac death. Cochrane Database Syst Rev. 2015;12:CD008093.
Bunch TJ, Mahapatra S, Murdock D, Molden J, Weiss JP, May HT, et al. Ranolazine reduces ventricular tachycardia burden and ICD shocks in patients with drug-refractory ICD shocks. Pacing Clin Electrophysiol. 2011;34:1600–6.
Amiodarone Trials Meta-Analysis Investigators (ATMAI). The effect of prophylactic amiodarone on mortality after acute myocardial infarction and in congestive heart failure: meta-analysis of individual data from 6500 patients in randomized trials. Lancet. 1997;350:1417–24.
Connolly SJ, Dorian P, Roberts RS, Gent M, Bailin S, Fain ES, et al. Comparison of beta-blockers, amiodarone plus beta-blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC Study: a randomized trial. JAMA. 2006;295:165–71.
Kudenchuk PJ, Cobb LA, Copass MK, Cummins RO, Doherty AM, Fahrenbruch CE, et al. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med. 1999;341:871–8.
Kudenchuk PJ, Brown SP, Daya M, Rea T, Nichol G, Morrison LJ, et al. Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N Engl J Med. 2016;374:1711–22.
Dorian P, Cass D, Schwartz B, Cooper R, Gelaznikas R, Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med. 2002;346:884–90.
Levine JH, Massumi A, Scheinman MM, Winkle RA, Platia EV, Chilson DA, et al. Intravenous amiodarone for recurrent sustained hypotensive ventricular tachyarrhythmias. Intravenous Amiodarone Multicenter Trial Group. J Am Coll Cardiol. 1996;27:67–75.
Somberg JC, Bailin SJ, Haffajee CI, Paladino WP, Kerin NZ, Bridges D, et al. Intravenous lidocaine versus intravenous amiodarone (in a new aqueous formulation) for incessant ventricular tachycardia. Am J Cardiol. 2002;90:853–9.
Scheinman MM, Levine JH, Cannom DS, Friehling T, Kopelman HA, Chilson DA, et al. Dose-ranging study of intravenous amiodarone in patients with life-threatening ventricular tachyarrhythmias. The Intravenous Amiodarone Multicenter Investigators Group. Circulation. 1995;92:3264–72.
Marill KA, deSouza IS, Nishijima DK, Stair TO, Setnik GS, Ruskin JN. Amiodarone is poorly effective for the acute termination of ventricular tachycardia. Ann Emerg Med. 2006;47:217–24.
Ortiz M, Martin A, Arribas F, Coll-Vinent B, Del Arco C, Peinado R, et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. Eur Heart J. 2017;38:1329–35.
AVID Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med. 1997;337:1576–83.
Connolly SJ, Hallstrom AP, Cappato R, Schron EB, Kuck KH, Zipes DP, et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg. Canadian Implantable Defibrillator Study. Eur Heart J. 2000;21:2071–8.
Bokhari F, Newman D, Greene M, Korley V, Mangat I, Dorian P. Long-term comparison of the implantable cardioverter defibrillator versus amiodarone: eleven-year follow-up of a subset of patients in the Canadian Implantable Defibrillator Study (CIDS). Circulation. 2004;110:112–6.
Steinberg JS, Martins J, Sadanandan S, Goldner B, Menchavez E, Domanski M, et al. Antiarrhythmic drug use in the implantable defibrillator arm of the Antiarrhythmics Versus Implantable Defibrillators (AVID) Study. Am Heart J. 2001;142:520–9.
Farre J, Romero J, Rubio JM, Ayala R, Castro-Dorticós J. Amiodarone and “primary” prevention of sudden death: critical review of a decade of clinical trials. Am J Cardiol. 1999;83:55D–63D.
CASCADE Investigators. Cardiac arrest in Seattle: conventional versus amiodarone drug evaluation. Am J Cardiol. 1991;67:578–84.
Julian DG, Camm AJ, Frangin G, Julian DG, Frangin GA, Schwartz PJ. Randomized trial of effect of amiodarone on mortality in patients with left ventricular dysfunction after recent myocardial infarction (EMIAT). Lancet. 1997;347:667–74.
Cairns JA, Connolly SJ, Roberts R, Gent M. Randomised trial of outcome after myocardial infarction in patients with frequent or repetitive ventricular premature depolarisations: CAMIAT. Canadian Amiodarone Myocardial Infarction Arrhythmia Trial Investigators. Lancet. 1997;349:675–82.
Doval HC, Nul DR, Grancelli HO, Perrone SV, Bortman GR, Curiel R. Randomised trial of low-dose amiodarone in severe congestive heart failure. Grupo de Estudio de la Sobrevida en la Insuficiencia Cardiaca en Argentina (GESICA). Lancet. 1994;344:493–8.
Singh SN, Fletcher RD, Fisher SG, Singh BN, Lewis HD, Deedwania PC, et al. Amiodarone in patients with congestive heart failure and asymptomatic ventricular arrhythmia. Survival Trial of Antiarrhythmic Therapy in Congestive Heart Failure. N Engl J Med. 1995;333:77–82.
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–37.
Thomas KL, Al-Khatib SM, Lokhnygina Y, Solomon SD, Kober L, McMurray JJ, et al. Amiodarone use after acute myocardial infarction complicated by heart failure and/or left ventricular dysfunction may be associated with excess mortality. Am Heart J. 2008;155:87–93.
Mounsey JP, DiMarco JP. Cardiovascular drugs. Dofetilide. Circulation. 2000;102:2665–270.
Yang T, Roden DM. Extracellular potassium modulation of drug block of IKr. Implications for torsade de pointes and reverse usedependence. Circulation. 1996;93:407–11.
McClellan KJ, Markham A. Dofetilide: a review of its use in atrial fibrillation and atrial flutter. Drugs. 1999;58:1043–59.
Pedersen HS, Elming H, Seibaek M, Burchardt H, Brendorp B, Torp-Pedersen C, et al. Risk factors and predictors of torsade de pointes ventricular tachycardia in patients with left ventricular systolic dysfunction receiving dofetilide. Am J Cardiol. 2007;100:876–80.
Falk RH, Pollak A, Singh SN, Friedrich T. Intravenous dofetilide, a class III antiarrhythmic agent, for the termination of sustained atrial fibrillation or flutter. Intravenous Dofetilide Investigators. J Am Coll Cardiol. 1997;29:385–90.
Singh S, Zoble RG, Yellen L, Brodsky MA, Feld GK, Berk M, et al. Efficacy and safety of oral dofetilide in converting to and maintaining sinus rhythm in patients with chronic atrial fibrillation or atrial flutter: the symptomatic atrial fibrillation investigative research on dofetilide (SAFIRE-D) study. Circulation. 2000;102:2385–90.
Shamiss Y, Khaykin Y, Oosthuizen R, Tunney D, Sarak B, Beardsall M, et al. Dofetilide is safe and effective in preventing atrial fibrillation recurrences in patients accepted for catheter ablation. Europace. 2009;11:1448–55.
Torp-Pedersen C, Moller M, Bloch-Thomsen PE, Køber L, Sandøe E, Egstrup K, et al. Dofetilide in patients with congestive heart failure and left ventricular dysfunction. Danish Investigations of Arrhythmia and Mortality on Dofetilide Study Group. N Engl J Med. 1999;341:857–65.
Kober L, Bloch Thomsen PE, Moller M, Torp-Pedersen C, Carlsen J, Sandøe E, et al. Effect of dofetilide in patients with recent myocardial infarction and left ventricular dysfunction: a randomised trial. Lancet. 2000;356:2052–8.
Pedersen OD, Bagger H, Keller N, Marchant B, Køber L, Torp-Pedersen C. Efficacy of dofetilide in the treatment of atrial fibrillation-flutter in patients with reduced left ventricular function: a Danish investigations of arrhythmia and mortality on dofetilide (diamond) substudy. Circulation. 2001;104:292–6.
Tendera M, Wnuk-Wojnar AM, Kulakowski P, Malolepszy J, Kozlowski JW, Krzeminska-Pakula M, et al. Efficacy and safety of dofetilide in the prevention of symptomatic episodes of paroxysmal supraventricular tachycardia: a 6-month double-blind comparison with propafenone and placebo. Am Heart J. 2001;142:93–8.
Wells R, Khairy P, Harris L, Anderson CC, Balaji S. Dofetilide for atrial arrhythmias in congenital heart disease: a multicenter study. Pacing Clin Electrophysiol. 2009;32:1313–8.
Tanel RE, Walsh EP, Lulu JA, Saul JP. Sotalol for refractory arrhythmias in pediatric and young adult patients: initial efficacy and long-term outcome. Am Heart J. 1995;130:791–7.
Boriani G, Lubinski A, Capucci A, Niederle R, Kornacewicz-Jack Z, Wnuk-Wojnar AM, et al. Ventricular Arrhythmias Dofetilide Investigators. A multicentre, double-blind randomized crossover comparative study on the efficacy and safety of dofetilide vs sotalol in patients with inducible sustained ventricular tachycardia and ischaemic heart disease. Eur Heart J. 2001;22:2180–91.
Baquero GA, Banchs JE, Depalma S, Young SK, Penny-Peterson ED, Samii SM, et al. Dofetilide reduces the frequency of ventricular arrhythmias and implantable cardioverter defibrillator therapies. J Cardiovasc Electrophysiol. 2012;23:296–301.
Schweizer PA, Becker R, Katus HA, Thomas D. Dronedarone: current evidence for its safety and efficacy in the management of atrial fibrillation. Drug Des Devel Ther. 2011;5:27–39.
Patel C, Yan GX, Kowey PR. Dronedarone. Circulation. 2009;120:636–44.
Tamargo J, López-Farré A, Caballero R, Delpón E. Dronedarone. Drugs Today (Barc). 2011;47:109–33.
Kathofer S, Thomas D, Karle CA. The novel antiarrhythmic drug dronedarone: comparison with amiodarone. Cardiovasc Drug Rev. 2005;23:217–30.
Tschuppert Y, Buclin T, Rothuizen LE, Decosterd LA, Galleyrand J, Gaud C, Biollaz J. Effect of dronedarone on renal function in healthy subjects. Br J Clin Pharmacol. 2007;64:785–91.
Køber L, Torp-Pedersen C, McMurray JJ, Gøtzsche O, Lévy S, Crijns H, et al. Dronedarone Study Group. Increased mortality after dronedarone therapy for severe heart failure. N Engl J Med. 2008;358:2678–87.
Connolly SJ, Camm AJ, Halperin JL, Joyner C, Alings M, Amerena J, et al. Dronedarone in high-risk permanent atrial fibrillation. N Engl J Med. 2011;365:2268–76.
Davy JM, Herold M, Hoglund C, Timmermans A, Alings A, Radzik D, et al. Dronedarone for the control of ventricular rate in permanent atrial fibrillation: the Efficacy and safety of dRonedArone for the cOntrol of ventricular rate during atrial fibrillation (ERATO) study. Am Heart J. 2008;156:527.e1–9.
Singh BN, Connolly SJ, Crijns HJ, Roy D, Kowey PR, Capucci A, et al. Dronedarone for maintenance of sinus rhythm in atrial fibrillation or flutter. N Engl J Med. 2007;357:987–99.
Khan MH, Rochlani Y, Aronow WS. Efficacy and safety of dronedarone in the treatment of patients with atrial fibrillation. Expert Opin Drug Saf. 2017;16:1407–12.
Piccini JP, Hasselblad V, Peterson ED, Washam JB, Califf RM, Kong DF. Comparative efficacy of dronedarone and amiodarone for the maintenance of sinus rhythm in patients with atrial fibrillation. J Am Coll Cardiol. 2009;54:1089–95.
Vamos M, Hohnloser SH. Amiodarone and dronedarone: an update. Trends Cardiovasc Med. 2016;26:597–602.
Hohnloser SH, Crijns HJ, van Eickels M, Gaudin C, Page RL, Torp-Pedersen C, et al. Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med. 2009;360:668–78.
Le Heuzey JY, De Ferrari GM, Radzik D, Santini M, Zhu J, Davy JM. A short-term, randomized, double-blind, parallelgroup study to evaluate the efficacy and safety of dronedarone versus amiodarone in patients with persistent atrial fibrillation: the DIONYSOS study. J Cardiovasc Electrophysiol. 2010;21:597–605.
Naccarelli GV, Lee KS, Gibson JK, VanderLugt J. Electrophysiology and pharmacology of ibutilide. Am J Cardiol. 1996;78:12–6.
Stambler BS, Beckman KJ, Kadish AH, Camm JA, Ellenbogen KA, Perry KT, et al. Acute hemodynamic effects of intravenous ibutilide in patients with or without reduced left ventricular function. Am J Cardiol. 1997;80:458–63.
Stambler BS, Wood MA, Ellenbogen KA. Antiarrhythmic actions of intravenous ibutilide compared with procainamide during human atrial flutter and fibrillation: electrophysiological determinants of enhanced conversion efficacy. Circulation. 1997;96:4298–306.
Murray KT. Ibutilide. Circulation. 1998;97:493–7.
Oral H, Souza JJ, Michaud GF, Knight BP, Goyal R, Strickberger SA, et al. Facilitating transthoracic cardioversion of atrial fibrillation with ibutilide pretreatment. N Engl J Med. 1999;340:1849–54.
Kowey PR, VanderLugt JT, Luderer JT. Safety and risk/benefit analysis of ibutilide for acute conversion of atrial fibrillation/flutter. Am J Cardiol. 1996;78:46–52.
Nair M, George LK, Koshy SK. Safety and efficacy of ibutilide in cardioversion of atrial flutter and fibrillation. J Am Board Fam Med. 2011;24:86–92.
Patsilinakos S, Christou A, Kafkas N, Nikolaou N, Antonatos D, Katsanos S, et al. Effect of high doses of magnesium on converting ibutilide to a safe and more effective agent. Am J Cardiol. 2010;106:673–6.
Tercius AJ, Kluger J, Coleman CI, White CM. Intravenous magnesium sulfate enhances the ability of intravenous ibutilide to successfully convert atrial fibrillation or flutter. Pacing Clin Electrophysiol. 2007;30:1331–5.
Kafkas NV, Patsilinakos SP, Mertzanos GA, Papageorgiou KI, Chaveles JI, Dagadaki OK, et al. Conversion efficacy of intravenous ibutilide compared with intravenous amiodarone in patients with recent-onset atrial fibrillation and atrial flutter. Int J Cardiol. 2007;118:321–5.
Volgman AS, Carberry PA, Stambler B, Lewis WR, Dunn GH, Perry KT, et al. Conversion efficacy and safety of intravenous ibutilide compared with intravenous procainamide in patients with atrial flutter or fibrillation. J Am Coll Cardiol. 1998;31:1414–9.
VanderLugt JT, Mattioni T, Denker S, Torchiana D, Ahern T, Wakefield LK, et al. Efficacy and safety of ibutilide fumarate for the conversion of atrial arrhythmias after cardiac surgery. Circulation. 1999;100:369–75.
Andò G, Di Rosa S, Rizzo F, Carerj S, Bramanti O, Giannetto M, et al. Ibutilide for cardioversion of atrial flutter: efficacy of a single dose in recent-onset arrhythmias. Minerva Cardioangiol. 2004;52:37–42.
Bernard EO, Schmid ER, Schmidlin D, Scharf C, Candinas R, Germann R. Ibutilide versus amiodarone in atrial fibrillation: a double-blinded, randomized study. Crit Care Med. 2003;31:1031–4.
Eidher U, Freihoff F, Kaltenbrunner W, Steinbach K. Efficacy and safety of ibutilide for the conversion of monomorphic atrial tachycardia. Pacing Clin Electrophysiol. 2006;29:358–62.
Glatter KA, Dorostkar PC, Yang Y, Lee RJ, Van Hare GF, Keung E, et al. Electrophysiological effects of ibutilide in patients with accessory pathways. Circulation. 2001;104:1933–9.
Hohnloser SH, Woosley RL. Sotalol. N Engl J Med. 1994;331:31–8.
Manoach M, Tribulova N. Sotalol: the mechanism of its antiarrhythmic-defibrillating effect. Cardiovasc Drug Rev. 2001;19:172–82.
Kato R, Ikeda N, Yabek SM, Kannan R, Singh BN. Electrophysiologic effects of the levo- and dextrorotatory isomers of sotalol in isolated cardiac muscle and their in vivo pharmacokinetics. J Am Coll Cardiol. 1986;7:116–25.
Fetsch T, Bauer P, Engberding R, Koch HP, Lukl J, Meinertz T, et al. Prevention of atrial fibrillation after cardioversion: results of the PAFAC trial. Eur Heart J. 2004;25:1385–94.
Waldo AL, Camm AJ, deRuyter H, Friedman PL, MacNeil DJ, Pauls JF, et al. Effect of d-sotalol on mortality in patients with left ventricular dysfunction after recent and remote myocardial infarction. The SWORD Investigators. Survival with oral d-sotalol. Lancet. 1996;348:7–12.
Singh BN, Singh SN, Reda DJ, Tang XC, Lopez B, Harris CL, et al. Amiodarone versus sotalol for atrial fibrillation. N Engl J Med. 2005;352:1861–72.
Kerin NZ, Jacob S. The efficacy of sotalol in preventing postoperative atrial fibrillation: a meta-analysis. Am J Med. 2011;124:875.e1–9.
Wanless RS, Anderson K, Joy M, Joseph SP. Multicenter comparative study of the efficacy and safety of sotalol in the prophylactic treatment of patients with paroxysmal supraventricular tachyarrhythmias. Am Heart J. 1997;133:441–6.
Rao SO, Boramanand NK, Burton DA, Perry JC. Atrial tachycardias in young adults and adolescents with congenital heart disease: conversion using single dose oral sotalol. Int J Cardiol. 2009;136:253–7.
Ho DS, Zecchin RP, Richards DA, Uther JB, Ross DL. Double-blind trial of lignocaine versus sotalol for acute termination of spontaneous sustained ventricular tachycardia. Lancet. 1994;344:18–23.
Mason JW. A comparison of seven antiarrhythmic drugs in patients with ventricular tachyarrhythmias. Electrophysiologic Study versus Electrocardiographic Monitoring Investigators. N Engl J Med. 1993;329:452–8.
Connolly SJ, Dorian P, Roberts RS, Gent M, Bailin S, Fain ES, et al. Comparison of beta-blockers, amiodarone plus beta-blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC Study: a randomized trial. JAMA. 2006;295:165–71.
Pacifico A, Hohnloser SH, Williams JH, Tao B, Saksena S, Henry PD, et al. Prevention of implantable defibrillator shocks by treatment with sotalol. d,l-Sotalol Implantable Cardioverter-Defibrillator Study Group. N Engl J Med. 1999;340:1855–62.
Seidl K, Hauer B, Schwick NG, Zahn R, Senges J. Comparison of metoprolol and sotalol in preventing ventricular tachyarrhythmias after the implantation of a cardioverter/defibrillator. Am J Cardiol. 1998;82:744–8.
Kettering K, Mewis C, Dornberger V, Vonthein R, Bosch RF, Seipel L, et al. Efficacy of metoprolol and sotalol in the prevention of recurrences of sustained ventricular tachyarrhythmias in patients with an implantable cardioverter defibrillator. Pacing Clin Electrophysiol. 2002;25:1571–6.
Kühlkamp V, Mewis C, Mermi J, Bosch RF, Seipel L. Suppression of sustained ventricular tachyarrhythmias: a comparison of d,l-sotalol with no antiarrhythmic drug treatment. J Am Coll Cardiol. 1999;33:46–52.
Julian DG, Prescott RJ, Jackson FS, Szekely P. Controlled trial of sotalol for one year after myocardial infarction. Lancet. 1982;1:1142–7.
Acknowledgments
This work was supported by grants from the Institute of Health Carlos III (PI16/00398 and CB16/11/00303), MINECO (SAF2017-88116-P) and Comunidad de Madrid [ITACA-CM (S2017/BMD-3738)].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tamargo, J., Caballero, R., Delpón, E. (2020). Class III Antiarrhythmic Drugs. In: Martínez-Rubio, A., Tamargo, J., Dan, G . (eds) Antiarrhythmic Drugs. Current Cardiovascular Therapy. Springer, Cham. https://doi.org/10.1007/978-3-030-34893-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-34893-9_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-34891-5
Online ISBN: 978-3-030-34893-9
eBook Packages: MedicineMedicine (R0)