Abstract
Independent organizations, supported by research, have recommended a standard of intensivist-led intensive care unit (ICU) staffing model given the association with improved ICU and hospital mortality (Hassan, Crit Care Nurs Q 41(1):47–59, 2018; Barrett et al., Utilization of Intensive Care Services, 2011: Statistical Brief #185. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD), Agency for Healthcare Research and Quality (US), 2016). However, this model can prove to be difficult to achieve due to a multitude of reasons such as financial resources and the limited availability of board-certified intensivists. In order to fill this need, Tele-ICU has been put forward as a potential solution to this lack of availability of certified intensive care providers. Tele-ICU is defined as networks of audiovisual communication and data systems to link hospital ICUs to intensivists and other critical care professionals at remote locations (Breslow et al., Crit Care Med 32(1):31–8, 2004). They can be designed to be one of three different models: centralized, decentralized, or hybrid. Each model comes with its own advantages and disadvantages, and the selection of which can depend greatly on geography, resource availability, and patient characteristics.
Telemedicine as an entity has been known for around 50 years; however it has experienced a slow evolution due to technologic constraints, regulatory issues, and lack of reimbursement. The initial concept of Tele-ICU was described by Grundy and colleagues in 1982 and fully implemented by the Sentara Hospital System in Norfolk, Virginia, in 2000 (Chen et al., J Intensive Care Med 33(7):383–93, 2018). The time period from 2003 to 2013 saw a rapid growth in the number of Tele-ICU systems, increased from 16 to 213, representing an increase of 61% per year but has slowed down over more recent years (Chen et al., J Intensive Care Med 33(7):383–93, 2018).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tele-ICU
- Telemedicine
- Intensivists
- ICU
- Centralized
- Decentralized
- Hybrid model
- Intensivist staffing
- Technology in medicine
- Rural medicine
Introduction
The US healthcare system is the most expensive in the world, and critical care services represent a significant fraction of this expense [4]. ICU services consume an estimated 10% of hospital costs at over $81 billion dollars annually [4]. Inpatient admissions requiring ICU stay cost approximately $61,800 on average, about 2.5 times more than a stay without ICU care [5]. Given the increased scrutiny of healthcare resources, newer methods are needed to improve the efficiency of care for patients in the ICU.
Care of critically ill patients by intensivists has shown to improve both ICU length of stay and mortality [6]. The Society of Critical Care Medicine recommends that an intensivist, usually unit-based, have the authority to intervene and directly care for critically ill patients in urgent and emergency situations [7]. The demand for critical care services in the United States is anticipated to increase due to aging of the population and the 35% shortfall of intensivists that is anticipated by 2030 [6].
ICU staffing models have been a subject of much debate. A systematic review and meta-analysis of 52 composite studies by Wilcox showed that access to intensivists and high-intensity staffing models are associated with reductions in ICU and in-hospital mortality [2]. However, around-the-clock staffing models still remain controversial as within the high-intensity staffing cohort, the same systematic review reported no survival benefit for continuous around-the-clock coverage versus daytime-only coverage [2]. These findings were also shown by Kerlin et al. in a systematic review and meta-analysis where nighttime intensivist staffing was not associated with reduced ICU patient mortality [8]. Realistically, it may be difficult for many hospitals to even have high-intensity daytime coverage due to lack of patient volume, lack of financial resources, and/or availability of intensivists. This disparity is magnified when focused on rural medicine. Rural populations are more likely to be underserved due to access to critical care services. Mohr et al. found that in Iowa, a state in the Midwest United States with a large rural population, most ICUs did not meet the Leapfrog standard for ICU staffing. This standard requires daytime coverage by board-certified intensivists and overnight access to an intensivist by telephone. It also requires a minimum 5-minute bedside response by a non-critical care physician, advanced practice provider, or specially trained nurse [9].
Tele-ICU is one of the ways the medical community hopes to solve the imbalance in supply and demand. It is defined as the provision of care to critically ill patients by healthcare professionals located remotely [10]. Tele-ICU services are meant to leverage, not replace, the need for bedside clinical expertise in the diagnosis, treatment, and assessment of various critical illnesses while allowing fewer intensivists to provide care to a larger number of critically ill patients. Modern telemedicine primarily occurs in centers that house intensivists, advanced practice providers, and nurses who either provide continuous around-the-clock coverage or during evening and weekend hours exclusively. They have the ability to access all patient data such as medical records, laboratory tests, and radiographic studies. Concurrently, they have the ability to remotely monitor vital signs and facilitate communication with bedside clinicians and other providers via computerized audiovisual approaches [11]. Additionally, Tele-ICU also requires a communication network to be established between the physical ICUs and the Tele-ICU monitoring center. These monitoring centers are typically located in areas with higher than average population densities of intensivists.
Models of Tele-ICU
There are three main models upon which Tele-ICU systems are designed: centralized, decentralized, and hybrid. Overall, there is much more literature available describing centralized models and review articles that describe implementation of a Tele-ICU system do so from the point of view of a centralized model [11].
Centralized Model
A centralized system is often referred to as a continuous high-intensity or active system. It is described as a team of healthcare care providers at a discrete site monitoring and intervening on a large population of critically ill patients. This closely resembles a hub-and-spoke model and offers clinicians the ability to integrate large amounts of data from within a hospital system as well as from different hospital systems. It often provides computer-generated alerts, notifications, and clinical decision support algorithms [1]. It also provides the ability to highlight individual patients by acuity and to intervene on one patient at time while simultaneously monitoring a large patient population. Understandably, this more advanced system comes with associated higher costs and requires centralized location of the Tele-ICU team (see Fig. 8.1).
Decentralized Model
A decentralized system allows a remote intensivist to virtually visit one patient at a time from a remote location that can be anywhere the intensivist chooses. There is no established central monitoring facility, and monitoring is done from the providers’ computer or laptop. It typically involves computers, tablets, and smart phones equipped with camera, speakers, and microphones located at sites of convenience for the physician [12]. The provider in this model communicates directly with an ICU team member who is at the bedside. This model provides much more limited information and lower-level intensity of interventions as compared to a centralized system, leading it to be referred to as a point-to-point passive system (see Table 8.1). This allows healthcare systems to provide intensive care at much lower costs. However, it is a reactive consultative model, without the ability to integrate different data streams.
Hybrid Model
The hybrid model is one that combines features of both the centralized and decentralized models. This model is not utilized as frequently and, thus, is not as well studied in regard to outcomes and effectiveness in comparison to centralized and decentralized systems. It resembles a centralized model; however the intensivists are separate entities that combine as a single virtual practice.
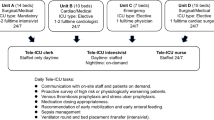
Staffing for Tele-ICU
Staffing may vary greatly depending on the Tele-ICU model being implemented with centralized models having more intense requirements. Additionally, the care model being used can have a significant impact on staffing needs. A continuous care model implies around-the-clock monitoring in real time that allows for monitoring of all ICU patients. A scheduled care model is also a type of care model used where dedicated times are previously identified for physician rounding and is typically set for 6 to 8 hours after a daytime ICU team has ended their shift. There is a reactive staffing model, where Tele-ICU staff respond on an as-needed basis such as for unstable patients, new admissions, or requests for ICU consultation [1, 12].
The centralized facility must be staffed by intensivists, nurses/advanced practice providers (APPs), and clerical assistants. This is independent of staffing at the ICU being monitored. The number of staff at each monitoring center depends on the total number of ICUs being covered as well as patients being monitored. Currently, recommendations suggest 60 to 125 patients for each intensivist, 30 to 40 for each nurse, and 50 to 125 for each clerical assistant [13].
Additional factors that can impact hours include academic versus community settings, availability of residents in-house, and hours of intensivist staffing at the bedside. Most centralized monitoring centers will provide continuous nursing and physician coverage 12 to 19 hours a day during the week and 24 hours a day on the weekends. The nurses and clerical assistants typically cover 12-hour shifts, while intensivists work in shifts of 9 to 12 hours. Most intensivists maintain bedside clinical responsibilities as well when not scheduled to provide Tele-ICU service, while some intensivists choose to work Tele-ICU full time [3].
The intensivists’ responsibilities can be categorized as routine and unscheduled. Routine responsibilities include evaluation of all new ICU admissions and monitoring of existing patients. Unscheduled responsibilities include responding to emergencies and identifying emerging problems [13]. As such, Tele-ICU physician engagement can be classified as high level or low level. High-level involvement includes emergency interventions such as direction of cardiopulmonary resuscitation, guidance for invasive airway management, and adjustment to other life-sustaining interventions. Low-level engagement of Tele-ICU intensivists includes non-emergent interventions such as reviewing results of blood tests ordered and electrolyte replacement. A low-level model would typically focus on emergency interventions and some minor interventions only; it typically would not include changes or modifications to existing therapies [1].
Financial Considerations
Every Tele-ICU program requires a well-developed financial business plan that can be significantly different for a centralized vs decentralized model. Areas of potential savings to a hospital system include decreased length of stay (LOS), decreased time on mechanical ventilation, and ICU triage 24 hours a day, among other indirect potential benefits.
The impact of Tele-ICU on overall ICU costs varies in the literature. Two previous studies reported detailed financial information that reported contradictory results as to whether Tele-ICU improved costs and clinical outcomes [14, 15]. Yoo et al. performed a cost-effective analysis of Tele-ICU systems and concluded that the current application of a centralized Tele-ICU is cost-effective under most circumstances [3]. However, this may have some variation based on severity of patient illness. A 2010 study on the cost-effectiveness of Tele-ICU across six intensive care units in a large healthcare system showed that the cohort of patients with lower disease severity had increased expense per patient and was not effective [15]. Patients with higher disease severity, however, showed decreased hospital mortality without increasing costs significantly. The authors showed that for this sub-group of patients, costs increased by $2895 per patient after Tele-ICU implementation which was not statistically significant while decreasing hospital mortality by 11.4% [15].
For rural hospitals, the importance of high ICU bed utilization is paramount as underutilization can represent a significant financial burden on a healthcare system. The primary aim of such hospitals is often to maintain an ICU at nearly full capacity with appropriate patients. Being part of a Tele-ICU program may allow a rural hospital to potentially retain patients who might have otherwise been transferred to a larger, higher-acuity facility. However, this purported benefit was not consistent with the findings of Pannu et al. who noted that inter-hospital transfers actually increased post-implementation of a Tele-ICU program and were attributed primarily to transfers from less specialized ICUs. There was no relation to illness severity [16].
Tele-ICUs have mostly been unable to charge for intensivist services that they provide, so their costs can only be recouped through improved efficiency. However there have been significant efforts made to address this issue by the American Telemedicine Association. Breslow and colleagues showed that reductions in the patients’ average length of stay (LOS) translated to a 24.6% decrease in cost per case, and this resulted in a $3.1 million benefit to the hospital over the 6-month study period [17]. A financial analysis of Tele-ICU at the University of Pennsylvania showed similar results with a decrease in ICU and hospital LOS leading to an estimated reduction in costs of up to $3.8 million dollars per year [18]. The most detailed financial analysis to date was performed by the Massachusetts Technology Collaborative in conjunction with the New England Healthcare Institute [19]. In this analysis, the University of Massachusetts Memorial Medical Center (UMMMC) implemented a Tele-ICU within its medical center and placed the technology into two smaller community ICUs. The change most affecting the financial results was the reduction in LOS, which decreased by approximately 20% [19]. The actual financial effects of a Tele-ICU are, however, difficult to measure because accounting systems are designed to measure direct billing and reimbursement rather than actual costs or indirect savings. Despite the paucity of financial analyses that have been conducted and completed, a number of healthcare systems have and continue to make large investments in Tele-ICUs which is likely due to the potential of a well-implemented Tele-ICU system to impact positive change on a healthcare system in terms of costs and quality of care.
Barriers to Implementation
There are five commonly cited barriers to adoption of a Tele-ICU system: high capital and operating costs, unproven return on investment, clinician resistance, lack of interoperability with EMR systems, and lack of documented outcomes [19]. It is estimated that establishing a Tele-ICU system can cost from 6 to 8 million dollars in upfront capital costs. On the other end, it can cost a single facility approximately $300,000–500,000 dollars to acquire and install the Tele-ICU technology required to allow monitoring by an established service. Also, reports suggest that it costs approximately 1–3 million dollars per year to maintain a command center [19]. The annual contracting fee to a command center for subscribing hospitals can vary from $23,000 to $40,000 per year [19]. Additionally, there are limited research findings available for hospitals to help guide the decision on whether or not to adopt a Tele-ICU program. Research that is available is mostly applicable to the particular ICU setting and hospital system in which they were studied [19].
Outcomes from Utilization of Tele-ICU
According to a consensus statement from the Critical Care Societies Collaborative, Tele-ICU outcomes should be evaluated from the perspective of the provider, patient, and healthcare system (see Fig. 8.2) [20].
Tele-ICU outcomes. (Venkataraman and Ramakrishnan [21])
Provider-Centered Outcomes
Tele-ICU can positively impact several important provider-centered outcomes. A systematic review of staff acceptance of Tele-ICU services found that it was viewed favorably by physicians and nurses. Nursing surveys report improved satisfaction from having access to an intensivist when needed [21]. Residents reported that Tele-ICU improved patient care and benefited their training specifically with regard to ventilator management, management of unstable patients, code supervision, and recognition of respiratory failure [22]. Romig and colleagues evaluated the impact of a nocturnal telemedicine service on staff satisfaction and perceptions of quality care. They found that nurses exposed to Tele-ICU responded more favorably than nurses who were not. Specifically, they reported a positive impact on communication with other healthcare workers, psychological working condition, and educational experience [23]. This likely translates to increased job satisfaction and decreased turnover. The bedside intensivist also benefits through decreased number of overnight shifts, increased sleep quality, and lower rates of burnout [6].
Patient-Centered Outcomes
Several studies have attempted to address the impact Tele-ICU has on patient care. A great example of this can be seen with the impact of Tele-ICU on various best practices in the ICU such as stress ulcer prophylaxis, DVT prophylaxis, and adherence to VAP bundle. These practices are generally well accepted as favorably affecting ICU outcomes, yet there remains difficulty in achieving high rates of compliance. This was demonstrated by Lilly et al. who studied a large group of ICU patients and found generally low compliance rates [24]. The same investigators then conducted a pre-/post-Tele-ICU intervention study and reported an improved compliance rate with several common ICU best practices (see Table 8.2). In this study, they found that many potential complications were significantly reduced and ultimately would result in decreased patient morbidity and improved outcomes. This was verified due to the fact that they associated this improvement in best practice implementation with reduced adjusted odds of mortality and reduced hospital length of stay [10]. Youn demonstrated a Tele-ICU program-enhanced compliance with three ventilator bundle components, specifically head of bed elevation, deep venous thrombosis prophylaxis, and stress ulcer prophylaxis [25].
System-Centered Outcomes
Cost-effectiveness and reimbursement are two of the primary system-centered outcomes that have been studied.
Breslow et all showed that an effective Tele-ICU program can reduce ICU costs per patient by up to 25% [17]. This was attributed to increasing the number of ICU admissions per month as the average length of stay decreased after Tele-ICU implementation. This however is in direct contrast to the findings of Franzini et al. who concluded that average daily costs increased after implementation of a Tele-ICU system [15]. There is no definitive answer yet as to the economic viability of a Tele-ICU system, and future studies are needed.
Hospitals are currently unable to bill directly for Tele-ICU services that are provided as noted previously in this chapter. Telemedicine services outside of the ICU have been able to overcome some of the obstacles and can be easily reimbursed; however this has not trickled down to critical care. Given the uncertainties regarding the financial benefits of Tele-ICU, any progress on this front is unlikely to be seen for some time.
Conclusion
The use of telemedicine to provide intensive care coverage to underserved areas is a burgeoning field of medicine that can provide improved care and outcomes for patients. It offers a way to supplement and elevate traditional bedside care and allow healthcare systems to face the challenges of an ever-changing healthcare environment. While research is ongoing, there is a fair amount of evidence to suggest that when implemented appropriately, it can improve access to timely and quality critical care. There is still considerable room for advancement in terms of reimbursement for services provided and determining the optimal model to best service the needs of a healthcare system. However, the potential benefits and implications in helping to reduce morbidity, mortality, and healthcare costs are too significant to ignore, and further studies are required.
References
Hassan E. Tele-ICU and patient safety considerations. Crit Care Nurs Q. 2018;41(1):47–59.
Barrett M L, et al. Utilization of Intensive Care Services, 2011: Statistical Brief #185. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD), Agency for Healthcare Research and Quality (US); 2006.
Breslow MJ, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: an alternative paradigm for intensivist staffing. Crit Care Med. 2004;32(1):31–8.
Chen J, et al. Clinical and economic outcomes of telemedicine programs in the intensive care unit: a systematic review and meta-analysis. J Intensive Care Med. 2018;33(7):383–93.
Fortis S, et al. A health system-based critical care program with a novel tele-ICU: implementation, cost, and structure details. J Am Coll Surg. 2014;219(4):676–83.
Franzini L, et al. Costs and cost-effectiveness of a telemedicine intensive care unit program in 6 intensive care units in a large health care system. J Crit Care. 2011;26(3):329.e321–6.
Kahn JM, et al. Adoption of ICU telemedicine in the United States. Crit Care Med. 2014;42(2):362–8.
Kerlin MP, et al. An official American Thoracic Society systematic review: the effect of nighttime intensivist staffing on mortality and length of stay among intensive care unit patients. Am J Respir Crit Care Med. 2017;195(3):383–93.
Kohl BA, et al. The effect of ICU telemedicine on mortality and length of stay. J Telemed Telecare. 2012;18(5):282–6.
Lilly CM, et al. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011;305(21):2175–83.
Mohr NM, et al. Characterizing critical care physician staffing in rural America: a description of Iowa intensive care unit staffing. J Crit Care. 2014;29(2):194–8.
Pannu J, et al. Impact of telemedicine monitoring of community ICUs on Interhospital transfers. Crit Care Med. 2017;45(8):1344–51.
Reynolds HN, Bander JJ. Options for tele-intensive care unit design: centralized versus decentralized and other considerations: it is not just a “another black sedan”. Crit Care Clin. 2015;31(2):335–50.
Ries M. Tele-ICU: a new paradigm in critical care. Int Anesthesiol Clin. 2009;47(1):153–70.
Rogove H. How to develop a tele-ICU model? Crit Care Nurs Q. 2012;35(4):357–63.
Scurlock C, D’Ambrosio C. Telemedicine in the intensive care unit: state of the art. Crit Care Clin. 2015;31(2):187–95.
Wallace DJ, et al. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366(22):2093–101.
Yoo BK, et al. Economic evaluation of telemedicine for patients in ICUs. Crit Care Med. 2016;44(2):265–74.
The New England Healthcare Institute Massachusetts Technology Collaborative. Critical Care, Critical Choices: The Case for Tele-ICUs in Intensive Care. 2010. Available at: http://www.nehi.net/writable/publication_files/file/teleicu_critical_care_critical_choices.pdf.
Kahn JM, et al. The research agenda in ICU telemedicine: a statement from the critical care societies collaborative. Chest. 2011;140(1):230–8.
Venkataraman R, Ramakrishnan N. Outcomes related to telemedicine in the intensive care unit: what we know and would like to know. Crit Care Clin. 2015;31(2):225–37.
Mora A, Faiz SA, Kelly T, et al. Resident perception of the educational and patient care value from remote telemonitoring in a medical intensive care unit. Chest. 2007;132(4):443a.
Lilly CM, et al. Benchmark data from more than 240,000 adults that reflect the current practice of critical care in the United States. Chest. 2011;140(5):1232–42.
Romig MC, et al. Perceived benefit of a telemedicine consultative service in a highly staffed intensive care unit. J Crit Care. 2012;27(4):426.e429–16.
Youn BA. ICU process improvement: using telemedicine to enhance compliance and documentation for the ventilator bundle. Chest. 2006;130:226S.
Disclosures
Neither ZK or SLT have any disclosures to report
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kalarikkal, Z., Thompson, S.L. (2020). Tele-ICU. In: Hidalgo, J., Pérez-Fernández, J., Rodríguez-Vega, G. (eds) Critical Care Administration. Springer, Cham. https://doi.org/10.1007/978-3-030-33808-4_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-33808-4_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-33807-7
Online ISBN: 978-3-030-33808-4
eBook Packages: MedicineMedicine (R0)