Abstract
As we start the third decade of the third millennium AD, children with Hodgkin lymphoma (HL) continue to be treated differently from adults. The primary driving force for this divergence over the last 15–20 years has been a desire to reduce the burden of treatment with particular reference to late effects. That reduction is being achieved primarily by limiting the amount of radiotherapy required to maintain excellent EFS rates. Titration of therapeutic aggressiveness by the use of PET/CT response assessment scans has been instrumental in achieving this goal. Children and adolescents with early-stage lymphocyte predominant (NLP) HL are treated on, or according to, dedicated clinical trials employing surgery alone in select situations, and low dose NHL-like therapy, often without radiotherapy. The use of combination anti-CD 20 antibody therapy is also increasing in this pediatric population. Management of teenagers and young adults (TYA) straddles between the pediatric and adult approaches depending on the treating institution. Awareness of the specific needs of this age group is escalating and several “pediatric” trials have been extended to include young adults. International harmonization of prognostic factors, risk categorization, and response assessment remains a challenge. The treatment of pediatric and adolescent refractory disease and relapse, however, converges with the adult approach. Trials using anti-CD30 antibody alone or in combination with PD-1 inhibitors and other checkpoint inhibitors are ongoing currently as a bridge to transplant. The debate regarding which sort of stem cell “transplant,” when, and after what continues. It is gratifying that advances in treating pediatric HL continue, and we are confident that the future will bring more.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hodgkin (cHL)
- Late effects
- Radiotherapy
- PET/CT
- NLPHL
- Teenagers and Young adults (TYA)
- Harmonisation
- Antibody therapy
- Trials
- Transplant
1 Introduction
1.1 Comparison of Pediatric/Adolescent Vs. Adult HL
Pediatric/young adult Hodgkin lymphoma (HL) is one of the few childhood malignancies that shares aspects of its biology and natural history with an adult cancer. Historically, children were thought to have a worse prognosis than adults due to antiquated treatment approaches that were initially designed to mitigate toxicities in children. It is now clear that effective therapy provides similar or even superior outcomes in children/young adults. A comparison of the demographics of clinical presentations of pediatric/adolescent HL compared with adult HL is presented in Table 15.1. The first of the bimodal incidence peaks in HL occurs in teenagers and young adults (15–25-year age group). HL represents less than 5% of malignancies in children under the age of 15 years. In contrast, it represents 16–20% of malignancies in adolescents, making it the most common malignancy of this age group.
Childhood HL is biologically indistinguishable from HL of young and middle-aged adults other than the relative incidence of specific disease histologies (Table 15.1). Mixed cellularity (MC) and nodular lymphocyte predominant (nLP) HL are the common types of HL in the preadolescent child; adolescents and young adults are most frequently (85%) afflicted with nodular sclerosing (NS) HL [3]. Only a third of children will have advanced disease; approximately 25% will have B symptoms. The incidence of HL with adverse features increases with age. Although there were no discernable differences in clinical presentation, response to therapy, or long-term outcome for adolescents (16–21 years) vs. young adults (22–45 years) treated similarly for HL [4], the treatment of children/adolescents and adults has diverged over the years primarily due to concerns about the late adverse effects of therapy.
1.2 Classical Pediatric Hodgkin Lymphoma (PHL)
1.2.1 Overall Strategies
The adverse consequences of therapy have driven the pediatric treatment paradigm of care. Clinical trials for pediatric and adolescent HL have been designed to both reduce long-term organ injury and increase efficacy. Pediatric oncologists responded first to developmental issues in the young child and later to the long-term treatment consequences in all young survivors in the design of treatment approaches. Recognition of musculoskeletal hypoplasia in young children with HL treated with high-dose radiation such as shortened sitting height, thin necks, and narrow shoulders and chest [5,6,7,8] precipitated the development of pediatric-specific regimens for HL. Combined-modality treatments, even for low-stage disease, allowed for the reduction of radiation dose [9] and field size, thus sparing normal structures (Fig. 15.1). This strategy for care was extended to older children and adolescents when hypothyroidism [11, 12], secondary cancers, and valvular and atherosclerotic heart disease [13, 14] were also found to be attributable to high-dose radiation.
CT-based planning images depicting a historic mantle RT, compared to standard involved field radiation treatment (IFRT) and involved-node RT (INRT) for a patient with stage I disease involving the mediastinum. The postchemotherapy volume of initially involved paratracheal nodes is depicted in dark red and the cardiac silhouette is also evident. (a–c) Demonstration of the reduction in dose to breast, lung, heart, and thyroid for the female patient shown in (a) from Mantle 36Gy to IFRT 21Gy to INRT 21Gy. From Hodgson et al. [10]
Low-dose radiation of 15–25 Gy has been the standard in childhood and adolescent HL for decades. This reduced the potential for long-term risk without adversely impacting event-free survival. A convergence of treatment approaches for adults and children/adolescents may be emerging as recent adult trials have begun to address these issues and reduce radiation doses. With overall survival over 90%, the quality of survival becomes paramount.
Early response to therapy was recognized [15, 16] as highly predictive of outcome. In Europe and the United States, response-based, risk-adapted approach to treating HL [17] allows therapy to be tailored to each individual, within the context of clinical trials. Dose-dense regimens [17] used are similar to those used by adult groups [18, 19], but the pediatric algorithms use the enhanced efficacy to support reduction of therapy.
1.2.2 Low-Risk (Early Favorable) Disease
Although there have been differing definitions of low-risk disease (Table 15.2), risk-adapted approaches aim to define a cohort of patients that is curable with minimal therapy. Treatment group allocation, risk stratification, and response assessment vary according to each study group (Table 15.2), but all treatment groups define low risk based on stage and bulky disease. Children and adolescents with NLPHL are increasingly being treated with surgery alone or using low-dose regimens separate from those used for the treatment of classical HL.
In the decade following the introduction of MOPP, secondary leukemia and sterility emerged as significant concerns [24,25,26,27]. During the 1980s, alkylator exposure and leukemia risk were reduced by alternating MOPP and ABVD [28, 29]. The goal was to avoid reaching thresholds of toxicity for any specific agent. The Pediatric Oncology Group (POG) compared four cycles of MOPP/ABVD plus 25.5 Gy to six cycles of chemotherapy alone without detecting differences in efficacy [15]. However, the profound sensitivity of the testes to procarbazine continued to cause sterility in boys, even with only two cycles of procarbazine-containing chemotherapy [30]. Although early attempts to avoid procarbazine were unsuccessful [31], more recent regimens have achieved this goal [17].
ABVD is used routinely in adults [32], but also has not been standard of care in children. Successful regimens have been devised by the German Paediatric Oncology Hodgkin’s Group (GPOH) [33] using OEPA (vincristine, etoposide, prednisone, and doxorubicin) in males (Table 15.3), by the French Society of Pediatric Oncology [36] using EBVP (etoposide, bleomycin, vincristine, prednisone), by Donaldson et al. [42] using VAMP (vincristine, doxorubicin, methotrexate, and prednisone), and by the Children’s Oncology Group (COG) using ABVE (doxorubicin, bleomycin, vincristine, etoposide) [43] and ABV-PC [41] all avoiding the use of procarbazine. With these approaches, EFS of 88–92% can be achieved without significant radiation or alkylator toxicity. Patients treated on these newer regimens receive less than 200 mg/m2 of doxorubicin plus or minus 20–25 Gy of involved-field radiation.
The traditional approach of most pediatric HL treatment groups has been to use combined-modality therapy. Currently, these study groups are involved in evaluating methods to define low-risk patients who may be cured without radiotherapy, i.e., with chemotherapy alone. However, patients with early-stage HL treated with chemotherapy alone most frequently relapse in the initially involved lymph node(s) [44]. Therefore, an effort has also been made to reduce the radiation field size by including only the initially involved lymph node(s)—so-called involved node-radiation (INRT) [45]. The complexity of defining the field for INRT has led to the development of an alternative approach termed “involved-site radiation therapy” (ISRT) [46,47,48]. This is a modification of IFRT, recommended for patients who when optimal pre-chemotherapy imaging (PET-CT in a position similar to what will be used at the time of radiation therapy) is not available that would be necessary for INRT treatment planning. Because the delineation of the area of involvement is less precise, a somewhat larger treatment volume is treated than with INRT, but less than traditionally used with IFRT. Other radiation techniques that are contemporary and reduce the treatment volume include intensity-modulated radiation therapy, deep inspiration breath holding (to reduce the volumes of the lung and heart that might be exposed), and protons [49].
Nachman et al. showed an increased relapse rate in patients who did not receive radiation despite achieving CR at the end of chemotherapy [34, 35]. Late-response evaluation may not have identified the optimal cohort for reduction of radiation. Early response may better define the profoundly chemotherapy-sensitive patient who does not need radiation. Based on the excellent outcomes of low-risk HL patients achieving CR after two cycles of chemotherapy [15], recent trials in the COG, the St. Jude/DFCI/Stanford Consortium, and the EuroNet PHL group [50, 51], have examined early response to determine who does or does not require radiation post-chemotherapy.
The prognostic importance of early chemotherapy response rather than end of chemotherapy response has led to the use of early response assessment (after 6–9 weeks) to titrate individual therapy and dose-dense regimens to maximize the early response rates. The St. Jude/DFCI/Stanford Consortium has reported 2-year EFS of 90.8% in early-responding, low-risk patients with either classical or nodular lymphocyte-predominant HL treated with 4 cycles of VAMP without radiation [51]. The most recent COG study (AHOD0431) found that early assessment by PET after one cycle is a predictor of recurrence [41, 52]. The current EuroNet PHL-C1 classical HL trial is evaluating PET activity after two intensive cycles of OEPA (cumulative dose of anthracycline is 160 mg/m2) to predict who does not require radiotherapy [53]. All such reductions in treatment may increase the risk of relapse; hence, adverse outcomes such as the need for high-dose salvage therapy (e.g., stem cell transplant or high-dose radiation) must be closely monitored.
1.2.3 Intermediate- and High-Risk (Advanced, Unfavorable) Disease
For children with advanced-stage disease, improving efficacy while limiting long-term toxicity is even more challenging. The approach in pediatric HL has been to increase the number of agents so as to limit cumulative doses of individual agents. Regimens used in the 1980–1990s alternated MOPP/ABVD [29, 54] or used the hybrid COPP/ABV [34] to avoid the cumulative doses of doxorubicin (300–400 mg/m2) and bleomycin (120–160 mg/m2) associated with six to eight cycles of the four-drug ABVD regimen [28, 32].
Minimalistic dose regimens in combined-modality protocols, such as VEPA (Table 15.4), that eliminated traditional alkylating agents were not successful and resulted in a 70 and 49% 5-year EFS for stage III and IV HD, respectively [61].
It has been known for decades that outcome in HL is optimized by chemotherapeutic dose intensity. Only recently has this knowledge been considered a clue to improving outcome [62,63,64]. ABVE-PC was developed by the COG (by adding prednisolone and cyclophosphamide to ABVE) for the treatment of advanced HL and dose density was increased by the use of 3-week cycles [17]. This regimen is similar to dose-dense regimens such as Stanford V and BEACOPP, developed simultaneously in the adult groups [18, 19]. BEACOPP and escalated BEACOPP are dose-intensive regimens with improved efficacy compared to COPP/ABVD. Instead of further cumulative dose escalation, the COG and EuroNet PHL take advantage of dose-dense delivery to limit cumulative cytotoxic therapy. Such dose-intensive regimens also limit the cumulative dose of agents delivered to the early responders. The GPOH-HD/EuroNet PHL group has substituted dacarbazine for procarbazine, resulting in excellent long-term results [40].
ABVE-PC is the backbone for all COG trials. This dose-dense approach allows for the elimination of procarbazine and the limitation of the doxorubicin and etoposide dose. The first such study (POG 9425) resulted in 5-year EFS of 84% and 5-year overall survival (OS) of 95% for advanced HL. Early responders (after three cycles of ABVE-PC) on this study proceeded directly to receive 21 Gy regional RT. Others received two more cycles (total five ABVE-PC in 15 weeks) prior to 21 Gy RT This backbone was used in AHOD0031 to evaluate a response-based vs. standard approach to therapy for intermediate-risk disease and to study augmentation of therapy for high-risk patients with a slow early response to therapy [65].
Low-dose, involved-site radiation remains a relevant modality of therapy in high-risk disease. The multicenter trial GPOH-HD95 used OPPA/COPP for girls and OEPA/COPP for boys with radiation dose determined by end of chemotherapy response. For the intermediate- and higher-risk groups (TG2 and TG4), outcome was significantly better for those receiving radiation therapy (TG2, 0.78 vs. 0.92; TG 2 + 3, 0.79 vs. 0.91) [33, 38]. The Children’s Cancer Group also noted improved outcome for patients treated with radiation, despite CR at the end of chemotherapy [34, 35]. Kelly et al. [66] reported excellent results using a modified approach to BEACOPP that reduced doses of chemotherapy for girls and for boys with a rapid response. Nonetheless, this regimen is not being used currently because cumulative doses of chemotherapy remain high.
Recent trials in both the COG and in Europe addressed early-response-directed approaches to limit the need for radiation. AHOD0031 for intermediate-risk HL used the dose-dense ABVE-PC regimen to support and evaluate the concept of an early-response-based algorithm [60]. This study showed that rapid early response (RER) could identify a cohort comprising 45% of patients who did not benefit from radiation. However, in a subset analysis from this study of patients with anemia and bulky limited-stage disease, the EFS was 89.3% for rapid early responder or complete remission patients who received IFRT, compared with 77.9% for patients who did not receive IFRT (P = 0.019) [67]. For patients who had a slow early response (SER), a marginal benefit from augmented chemotherapy was observed. The high-risk study (AHOD-0831) limited radiation fields for rapid early responders while augmenting therapy for slow early responders; outcomes were similar to POG9425 but used less radiation for RER and less doxorubicin for SER [E].
Adult patients with high risk randomized to ABVD vs. brentuximab with AVD have been reported to have a reduced risk of progression, death, or non-complete response [68], resulting in approval in the United States for this indication. However, it is not clear that this approach has an advantage in the setting of pediatric regimens that have had greater efficacy than ABVC. COG has a randomized, ongoing study comparing standard ABVE-PC to ABrVE-PC (Harker-Murray et al.), and the St. Jude Consortium is similarly evaluating the use of brentuximab with their backbone therapy.
1.2.4 Future Considerations in Classical Pediatric and Adolescent HL
Progress has been made in the treatment of children with HL with all stages of disease and risk factors, but several issues remain to be resolved. Response to chemotherapy may define both the total amount of chemotherapy required and the need for radiotherapy (RT). For early-stage patients, the balance between chemotherapy dose and radiation exposure continues to be explored. Restriction of RT to initially involved lymph nodes (involved-node irradiation or involved-site irradiation) rather than chains (or regions) of nodes may affect the balance of risk. For high-risk disease, dose-dense chemotherapy improves efficacy and supports tailoring of therapy to the patient’s response. RT is clearly effective in enhancing the local control of PHL, but has a dose-dependent toxicity profile favoring a limited volume/dose approach. Ongoing studies are needed to assess the role of RT for initial bulky disease, to residual postchemotherapy disease (particularly if it is PET negative), and to involved organs. Carefully designed and sequential evidence-based studies are needed to continue to improve efficacy while limiting toxicity.
1.3 Nodular Lymphocyte-Predominant HL (NLPHL)
An indolent, peripheral, NHL-like disease, NLPHL was recognized in the early 1990s as a clinicopathologically distinct form of HL [69]. Unlike classical HL, NLPHL is a CD20-positive, CD30- and CD15-negative, B cell lymphoma that is not associated with EBV genomic integration. There is a distinct male predominance (ratio 2–3:1) with nearly 90% of pediatric patients having early-stage disease (IA/IIA). A higher percentage (10–20%) of children have NLPHL [3] compared to adults (3–8%) [70], and although >50% of pediatric and adolescent cases are under the age of 14 years [71], the incidence peaks between 14 and 18 years. Peripheral lymphadenopathy is the most common presentation involving the axilla, cervical, and inguinal regions, often present for months or years. Rarely is advanced or central disease seen.
Adults with early-stage NLPHL are treated with involved-field radiotherapy, standard cHL therapy, or combined-modality therapy. Children have, until 2005 and the start of NLPHL-specific clinical trials, received standard pediatric cHL therapy with combined-modality chemoradiotherapy [72], which is excessively toxic.
Morbidity, even mortality, secondary to repeated courses of intensive therapy to eradicate this indolent, usually nonfatal disease has resulted in a drive to reduce the intensity of therapy to avoid late effects [71].
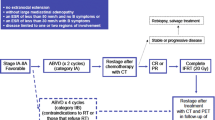
Children with fully resected early-stage nLPHD have been cured without the need for any chemoradiotherapy [73,74,75,76], but the specific situations in which this strategy is appropriate are currently under investigation. Two nonrandomized clinical trials, EuroNetPHL-LP1 and COG’s AHOD03P1, have looked at reducing the toxicity of upfront therapy for early-stage disease (stage I and II) [73, 74]. As salvage therapy is effective for late or even multiple relapses which generally recur at the original site of disease with no stage upgrade, OS is expected to remain near to 100% [77]. The EuroNetPHL-LP1 used surgical resection alone or low-dose anthracycline-free CVP chemotherapy for non-resectable disease, and COG’s AHOD03P1 used AVPC (equivalent to CHOP) with selective radiotherapy. Excellent EFS rates of 60–75% with no or low-dose chemotherapy have been obtained and only 10% of COG patients received RT, maintaining 100% OS [78].
Because of transformation rates of approximately 5% to aggressive B-NHL [79] in adults, usually diffuse large B cell lymphoma [80], concerns regarding reduced therapy that could potentially allow persistence of the CD20 clone and increased transformation rates remain. In theory, the addition of rituximab would help to specifically eradicate the CD20 clone and reduce transformation rates. However, transformation rates in children are not known but appear extremely low.
Rituximab has been studied in adults for use in this and all other CD20-positive lymphomas [81]. The pediatric community have traditionally been wary about using rituximab in young children because of impact on immune status/memory. As early-stage NLPHL is viewed as a highly curable disease with minimal chemotherapy or surgery alone, the use of rituximab has been reserved for treating more aggressive, advanced, or relapsed disease. Assessing the impact of adjuvant rituximab therapy on EFS and transformation rates in children within a randomized clinical trial has been the unattainable aim of clinicians for well over a decade. The reluctance of the pediatric community to use rituximab in this and other CD20+ lymphomas is abating.
Current proposed clinical trials using low-dose NHL-like therapy including anti-CD20 therapy are focused on the natural history, establishing risk categories, variant histologies, and transformation rates, with biological substudies looking at specific molecular characteristics.
1.4 Recurrence, Relapse, and Salvage in PHL
1.4.1 Introduction
Relapsed and refractory classical Hodgkin lymphoma (HL) remains a clinical and therapeutic challenge. Approximately 10% of patients with early-stage and up to 30% with advanced-stage disease relapse after first-line chemotherapy.
Cure can still be achieved in a substantial proportion of patients with recurrent disease, but there is no uniform approach to salvage therapy. The optimal salvage treatment has not been defined in children and adolescents as there are no randomized trials defining the “best” salvage chemotherapy regimen or comparing standard-dose chemotherapy (SDCT) vs. high-dose chemotherapy and autologous stem cell transplant (HDCT/ASCT), which is often considered the standard of care in adult practice. Pediatric practice adopts a more individualized risk-stratified and response-adapted approach to salvage treatment with both non-transplant (SDCT plus radiotherapy) and transplant (SDCT plus HDCT/ASCT) salvage.
At the point of relapse, a full disease reassessment including histologic confirmation is mandatory and then an analysis of pre-salvage risk factors is undertaken. All patients have a common starting point with re-induction SDCT and this is followed by consolidation treatment. The choice of consolidation treatment is guided by risk stratification based on prognostic factors as well as an assessment of chemosensitivity which is commonly done after two cycles of SDCT and includes FDG-PET response. Achieving a complete metabolic remission on FDG-PET prior to consolidation has been shown to be highly prognostic in the relapse setting and is considered to be a major goal of re-induction SDCT [82]. Consolidation after SDCT will be radiotherapy only in “low-risk” relapse or HDCT/ASCT in “standard-risk” relapse, and these two strategies will be appropriate for the vast majority of relapse/progressive HL. A small number of patients are refractory to SDCT and do not achieve a CR with two or more lines of SDCT and these are “high-risk” patients [82]. Consolidation in these high-risk patients may be either conventional HDCT/ASCT possibly with post-HDCT consolidation RT or maintenance-targeted therapy such as brentuximab vedotin, or alternative experimental approaches may be applied including novel agents such as checkpoint inhibitors or allogeneic transplantation.
1.4.2 Standard-Dose Salvage Chemotherapy Regimens
After recurrence is noted, the first step is reinduction with a SDCT salvage regimen. There is no “best” chemotherapy regimen at salvage, and there are no randomized studies comparing standard-dose chemotherapy regimens. The choice of regimen should take account of primary therapy, use of non-cross-resistant drugs, and cumulative drug toxicities. The aim of salvage therapy is to obtain cytoreduction and to demonstrate chemosensitivity which is done most accurately now with FDG-PET as first-line treatment. It also facilitates collection of peripheral stem cells for ASCT. Salvage regimes can be divided into intensive conventional regimensFootnote 1 (mini-BEAM), cisplatin-based regimensFootnote 2 (ESHAP, DHAP [ESHAP, DHAP, APPE, DECAL]), ifosfamide-based regimensFootnote 3(EPIC, IEP, ICE, IV), or othersFootnote 4 (GV, IGEV). The COG uses IV as its standard regimen because of efficacy and with the intent of avoiding etoposide-induced secondary malignancy after stem cell transplantation [83]. In Europe, alternating IEP/ABVD was used in the EuroNet-PHL-R1 trial but more recently the IGEV regimen has been widely adopted. The decision to continue salvage therapy with RT consolidation vs. HDCT/ASCT is based on assessment of predictive factors.
1.4.3 Prognostic Factors at Relapse in Pediatric HL: Standard-Dose Chemoradiotherapy Vs. High-Dose Chemotherapy/Stem Cell Transplantation
Prognostic factors at relapse may be used to allocate patients to a risk-stratified salvage approach. This is in contrast to adult practice where consolidation with HDCT/ASCT is considered standard of care. There are currently no universally accepted prognostic criteria in children (or adults) defining individualized salvage treatment plans. Factors which are prognostically important include time to relapse, prior treatment in first line, stage/disease burden at relapse, and response to salvage chemotherapy. In children, low-risk patients may be salvaged with RT consolidation only, while standard-risk patients are salvaged with HDCT. The cut point between low- and standard-risk patients is not universally defined. In Europe, low-risk patients salvaged with SDCT plus RT only include those with early relapse after up to 4 cycles of chemotherapy and late relapse after up to 6 cycles with all of the following: nodal relapse, no prior RT (or relapse only outside prior RT fields), consolidation RT that has acceptable toxicity (i.e., no excessive RT fields), and chemotherapy-responsive disease. All other patients have intensification with HDCT/ASCT.
Time to relapse from end of first-line treatment is the most important pretreatment risk factor and highly significant for OS and EFS in pediatric studies [84,85,86] and dominated all other prognostic factors in multivariate analysis of the ST-HD-86 trial, the largest prospective pediatric relapse trial published to date [87], with DFS of 41, 55, and 86% for those with refractory disease, early relapse, and late relapse, respectively. This study showed that salvage can be risk adapted because subgroups with markedly better or worse prognosis can be defined. Stage IV and extranodal disease were also associated with lower OS.
A recent French experience [88] found the only relevant prognostic factors to be time to relapse and chemoresistance with primary progressive HL having an EFS <40% compared with approximately 80% in late relapse and chemosensitivity (CR or PR >70%) to salvage associated with a DFS of 77% vs. 10% with poor response (p < 0.0001). Chemosensitivity to SDCT and disease status at transplantation are also predictive of outcome. In one study, 5-year FFS was 35% for patients with chemosensitive disease vs. 9% with chemoresistant disease [84]. Another group found 68% OS and 59% FFS at 5 years in chemosensitive patients vs. 18% and 0% in chemoresistant patients [85]. Several particularly adverse factors have been noted. Chemoresistant patients had 5-year FFS of 0% with HDCT/ASCT [85]. Adolescents with B symptoms at recurrence had poor OS even after HDCT/ASCT (11-year OS 27% with B symptoms vs. 60% without) [89]. No difference in OS or FFS between age subgroups or in comparison with adult cohorts has been reported by several studies [84, 85, 90]. Of note, many of these studies did not incorporate FDG-PET response assessment which is now well recognized as the most important prognostic factor, which may overcome the significance of some factors as is the case in first-line treatment [91].
1.4.4 Role of Radiotherapy in Relapsed Hodgkin Lymphoma
Radiotherapy has an important role in salvage, but must be individualized based on previous radiation exposure, in or out of field recurrence, stage at recurrence, and the toxicities of total treatment burden [92]. Increasing numbers of patients are RT naïve at relapse as the use of RT is increasingly restricted in first-line treatment and RT fields are also becoming highly restricted in some first-line trials to FDG-PET-positive residua. Therefore, at relapse many patients have never received RT, and some other patients may relapse in prior disease sites that have never received RT because they received focal targeted RT only. Salvage with RT alone is generally not recommended, but integration of RT in salvage is relevant in two contexts:
-
1.
As consolidation treatment in low-risk group patients after SDCT.
-
2.
In selected patients as consolidation after HDCT/ASCT
1.4.5 High-Dose Chemotherapy and Autologous Stem Cell Transplant
COG protocols have studied HDCT/ASCT and immunomodulatory therapy in all patients except the lowest-risk group (late relapse without bulky disease or B symptom in those initially treated for IA/IIA disease with minimal systemic therapy) [93]. In Europe, HDCT/ASCT has a recognized role in salvage for those with higher-risk features, namely, all primary progressive HL and early relapse after 6 cycles of first-line chemotherapy, all relapse with poor response to reinduction, and finally those patients in whom RT consolidation is either not feasible (advanced-stage relapse) or too toxic (extensive RT fields required or re-irradiation of prior irradiated sites). Patients without high-risk features and who achieve a complete FDG-PET-defined response after two cycles of SDCT may receive only consolidation SDCT plus RT.
There are no studies that define the most effective HDCT. BEAM and CVB (cyclophosphamide, etoposide, carmustine) are commonly used. TBI-containing regimens confer no benefit and are associated with increased toxicity and late effects. Transplant-related mortality is down to 0–2% in some series. A higher TRM rate has been associated with history of atopy, thoracic irradiation, multiple chemotherapy regimens, and multiple relapses.
Series with HDCT/ASCT in pediatric and adolescent patients are small and report EFS rates of 31–67% [84, 85, 90, 94]; outcome for children is similar to adults with HDCT/ASCT [84, 90]. Studies that evaluate survival benefit rather than event-free survival after disease recurrence often rely on transplant after second or later recurrence to achieve good OS [85, 95]. Patients with primary progressive disease and those resistant to salvage regimens remain a huge challenge. SDCT with radiotherapy will not afford a chance of cure, but even HDCT/ASCT is inadequate therapy for most such patients. New approaches to such patients, such as use of post-HDCT consolidation maintenance-targeted treatment, were tested in the Aethera trial with up to 16 cycles of brentuximab vedotin or post-HDCT radiotherapy which is also an option to minimize further relapse. Allogeneic SCT or immunomodulatory therapy may prove beneficial [93].
Long-term follow-up is required post-HDCT for detection of late relapse and development of second cancers, which have been reported at a rate of 5–10% at 5 years and substantially higher at 20 years or more in some series. Thirty-eight percent of deaths occurred 4–12 years after ASCT; 85% of relapses occur within 2 years of ASCT [86].
1.4.6 High-Dose Chemotherapy and Allogeneic Stem Cell Transplantation
The role of allogeneic transplant in relapsed HL remains unknown. The poor outcome with HDCT/ASCT in chemotherapy poor responders to salvage and those who remain FDG-PET positive after salvage has resulted in exploration of alloSCT. Allogeneic transplantation is not recommended as the initial transplant approach outside of a clinical trial setting [96] due to the high non-relapse mortality (NRM) rate, mainly caused by graft vs. host disease and infection. Reduced intensity conditioning (RIC) ameliorates the NRM while maintaining theoretical graft vs. lymphoma effect. Allogeneic-SCT may be an option for relapse post-HDCT/ASCT and for patients with refractory advanced-stage HL and chemoresistant disease at salvage.
Children and adolescents allografted for HL had an OS of 45% and PFS of 30% at 5 years [97]. All were heavily pretreated, almost half with HDCT/ASCT. Those with chemosensitive disease and good performance status achieved 3-year OS of 83% and PFS of 60%. NRM was 21 ± 4% in both the RIC and myeloablative conditioning groups. RIC was associated with a significantly higher relapse risk compared to myeloablative conditioning. Graft vs. host disease did not affect relapse rate.
Although studies based on registry data are useful, prospective trials are required to gain a better understanding of the role of allogeneic transplantation. The indications, optimal time point, conditioning regimen, and GVHD prophylaxis still need to be better defined. With the advent of newer immunotherapy agents, including checkpoint inhibitors, the role of alloSCT globally in HL is under review and the numbers of such transplants are declining globally.
1.4.7 Brentuximab Vedotin and Checkpoint Inhibitors
In recent years there have been two early-phase pediatric trials investigating novel agents in children. The first is the phase I/II pediatric trial (ClinicalTrials.gov number NCT01492088) investigating single-agent brentuximab vedotin in R/R HL and anaplastic large cell lymphoma [98]. The recommended phase II dose was 1.8 mg/kg as in adults and the ORR was 47% (CR rate 33%, PR rate 12%) in HL patients and toxicity was manageable. This compares with the pivotal phase II study in adults where the ORR was 75% (CR rate 34%) [99]. The second is the ongoing risk-stratified and response-adapted phase II salvage trial in first R/R HL of nivolumab plus brentuximab vedotin followed by bendamustine plus brentuximab vedotin in poor initial responders in first R/R HL in children and young adults (Checkmate 744 trial, AHOD1721; NCT02927769) [100]. The preliminary results of this study are recently presented showing 64% of patients achieved a CMR after brentuximab vedotin plus nivolumab. Of those inadequate responders that switched to second-line brentuximab vedotin plus bendamustine, all achieved a CMR after 2 cycles of this intensification. The overall CMR rate with either first or second salvage in this trial was 86%, demonstrating that only a small number of patients cannot achieve a CMR pre-HDCT with these combinations.
Treatments that block the interaction between programmed death-1 (PD-1) and its ligands have shown high levels of activity in adults with HL. The anti-PD-1 antibody nivolumab induced objective responses in 20 of 23 adult patients (87%) with relapsed HL [101]. Another anti-PD-1 antibody, pembrolizumab, produced an objective response rate of 65% in 31 heavily pretreated adult patients with Hodgkin lymphoma who relapsed after receiving brentuximab vedotin [102]. These agents may be used as a bridge to transplant, as post-HDCT maintenance brentuximab vedotin, or as alternatives to conventional SDCT. These novel agents when used as a single agent achieve CR rates of 19–33%, but in combination achieve higher CR rates as in the Checkmate trial [100]. An interesting combination is brentuximab vedotin plus bendamustine [103] which achieves CR rates in excess of 75% which means that most patients can achieve a CR prior to HDCT making the use of alloSCT which is often used in patients that cannot achieve a CR less appealing.
1.5 Late Effects
Long-term adverse sequelae of greatest concern in children treated for HL (particularly with regimens including high-dose radiation) include impairment of muscle and bone development [5] and injury to the lungs [104], heart [105], thyroid gland [11, 12], and reproductive organs [106]. Cardiovascular dysfunction, pulmonary fibrosis, and secondary malignancies significantly compromise the quality and length of life in survivors [107].
1.5.1 Cardiac Toxicities
High-dose (>30 Gy) radiation to the mediastinum has been associated with significant long-term effects in patients with HL. Stanford investigators reported that the actuarial risk of developing cardiac disease necessitating pericardiectomy was 4% at 17 years in a series of long-term survivors of childhood HL who had received high-dose radiation [14]. Screening echocardiogram, exercise stress test, and resting and 24-h ECG identified numerous clinically significant cardiac abnormalities in HL patients who had mediastinal irradiation at a median age of 16.5 years (range, 6.4–25 years). Significant valvular defects were detected in 42%, autonomic dysfunction in 57%, persistent tachycardia in 31%, and reduced hemodynamic response to exercise in 27% of patients [108]. With the introduction of techniques that reduce the radiation dosage to the heart, rates of radiation-associated cardiac injury have declined dramatically.
Mediastinal irradiation given for HL may further predispose patients with PHL to anthracycline-related myocardiopathy [14, 109]. Cardiac dysfunction after anthracycline therapy itself is notable, with the highest risk in those receiving high cumulative doses or in young children who may be affected by an adverse effect on cardiac myocyte growth [14, 109]. Fortunately, most pHL patients are adolescents and current pHL regimens doses are significantly lower than those used in adult ABVD regimens.
1.5.2 Pulmonary Toxicities
Chronic pneumonitis and pulmonary fibrosis should be rare in the current era of treatment for primary HL (Fig. 15.1). Predisposing therapies include thoracic radiation and bleomycin chemotherapy [104, 105]. The bleomycin in ABVD can cause both acute pulmonary compromise and late pulmonary fibrosis and can be augmented by the fibrosis that can be associated with pulmonary radiation. Asymptomatic pulmonary dysfunction that improves over time has been observed after contemporary combined-modality treatment.
1.5.3 Thyroid Toxicities
Thyroid sequelae are common after RT for PHL. Hypothyroidism, hyperthyroidism, thyroid nodules, and thyroid cancer have been observed in long-term survivors [11, 12]. Of these, hypothyroidism, particularly compensated hypothyroidism, defined as thyroid-stimulating hormone (TSH) elevation in the presence of a normal thyroxine (T4) level, is the most common thyroid abnormality. The primary risk factor for hypothyroidism is higher cumulative radiation dosage; the influence of age remains controversial [11, 12]. As many as 78% of patients treated with radiation dosages greater than 26 Gy demonstrate thyroid dysfunction, as indicated by elevated TSH levels [11].
1.5.4 Secondary Malignancies
The overall cumulative risk of developing a subsequent malignancy after treatment for PHL has been reported to range from 7% to 10% at 15 years from diagnosis and rises to 16–28% by 20 years (Table 15.5) [116]; these data are based on patients treated in earlier decades. The most common secondary malignancies historically included both secondary acute myeloid leukemia (MDS/secondary AML) and solid tumors. However, leukemias are now infrequent due to changes in chemotherapy. Female breast cancer is a particular concern but is likely to be less common with current radiation doses and techniques, since it is associated with RT fields that include breast tissue (especially mantle fields) and higher radiation doses (Fig. 15.1).
1.6 Summary/Future Directions
Tremendous strides have been made in treating children with HL, both in terms of cure and reduction of toxicity. Devising new strategies to treat children with HL is problematic because of the overall success of current treatment regimens. However, grouping patients into different risk categories, using response-based therapy and newer imaging techniques, allows investigators to construct protocols intended to diminish therapy-induced toxicity for patients with favorable prognoses. These protocols also aim to improve efficacy of treatment for patients with intermediate and unfavorable prognoses. Unfortunately, the ability to conduct clinical trials, where the difference in survival between treatment arms is likely to be small, is compromised by the large patient numbers required to detect such differences. If a reduction in treatment toxicity is the intended goal of a new regimen, then many years of follow-up are necessary to prove efficacy. For patients with refractory, or multiple relapsed disease, phase II studies investigating the use of monoclonal anti-CD30 and anti-PD-1 antibodies alone and in combination, and with other checkpoint inhibitors, in children and adolescents are ongoing internationally. The importance of investigators working together throughout the world to share data and new treatment approaches in order to cure children with HL safely is clear.
Notes
- 1.
Mini-BEAM; BCNU, etoposide, cytarabine, melphalan
- 2.
ESHAP, etoposide, methylprednisolone, cytarabine, cisplatin; DHAP, dexamethasone, cytarabine, cisplatin; APPE, cytarabine, cisplatin, prednisone, etoposide; DECAL, cytarabine, cisplatin, prednisone, etoposide, asparaginase
- 3.
EPIC, etoposide, vincristine epirubicin, prednisolone; IEP, ifosfamide, etoposide, prednisolone; ICE, ifosfamide, carboplatin, etoposide; IV, ifosfamide, vinorelbine
- 4.
GV gemcitabine, vinorelbine; IGEV, ifosfamide, gemcitabine, vinorelbine, prednisolone
References
Rubin P, Williams JP, Devesa SS, Travis LB, Constine LS (2010) Cancer genesis across the age spectrum: associations with tissue development, maintenance, and senescence. Semin Radiat Oncol 20:3–11
Punnett A, Tsang RW, Hodgson DC (2010) Hodgkin lymphoma across the age spectrum: epidemiology, therapy, and late effects. Semin Radiat Oncol 20:30–44
Hochberg J, Waxman IM, Kelly KM, Morris E, Cairo MS (2009) Adolescent non-Hodgkin lymphoma and Hodgkin lymphoma: state of the science. Br J Haematol 144:24–40
Foltz LM, Song KW, Connors JM (2006) Hodgkin’s lymphoma in adolescents. J Clin Oncol 24:2520–2526
Donaldson SS, Kaplan HS (1982) Complications of treatment of Hodgkin’s disease in children. Cancer Treat Rep 66:977–989
Mauch PM, Weinstein H, Botnick L, Belli J, Cassady JR (1983) An evaluation of long-term survival and treatment complications in children with Hodgkin’s disease. Cancer 51:925–932
Merchant TE, Nguyen L, Nguyen D, Wu S, Hudson MM, Kaste SC (2004) Differential attenuation of clavicle growth after asymmetric mantle radiotherapy. Int J Radiat Oncol Biol Phys 59:556–561
Probert JC, Parker BR, Kaplan HS (1973) Growth retardation in children after megavoltage irradiation of the spine. Cancer 32:634–639
Donaldson SS, Glatstein E, Rosenberg SA, Kaplan HS (1976) Pediatric Hodgkin’s disease. II. Results of therapy. Cancer 37:2436–2447
Hodgson DC, Hudson MM, Constine LS (2007) Pediatric Hodgkin lymphoma: maximizing efficacy and minimizing toxicity. Semin Radiat Oncol 17:230–242
Constine LS, Donaldson SS, McDougall IR, Cox RS, Link MP, Kaplan HS (1984) Thyroid dysfunction after radiotherapy in children with Hodgkin’s disease. Cancer 53:878–883
Sklar C, Whitton J, Mertens A, Stovall M, Green D, Marina N et al (2000) Abnormalities of the thyroid in survivors of Hodgkin’s disease: data from the childhood cancer survivor study. J Clin Endocrinol Metab 85:3227–3232
Adams MJ, Hardenbergh PH, Constine LS, Lipshultz SE (2003) Radiation-associated cardiovascular disease. Crit Rev Oncol Hematol 45:55–75
Hancock SL, Donaldson SS, Hoppe RT (1993) Cardiac disease following treatment of Hodgkin’s disease in children and adolescents. J Clin Oncol 11:1208–1215
Kung FH, Schwartz CL, Ferree CR, London WB, Ternberg JL, Behm FG et al (2006) POG 8625: a randomized trial comparing chemotherapy with chemoradiotherapy for children and adolescents with stages I, IIA, IIIA1 Hodgkin disease: a report from the Children’s oncology group. J Pediatr Hematol Oncol 28:362–368
Weiner MA, Leventhal B, Brecher ML, Marcus RB, Cantor A, Gieser PW et al (1997) Randomized study of intensive MOPP-ABVD with or without low-dose total-nodal radiation therapy in the treatment of stages IIB, IIIA2, IIIB, and IV Hodgkin’s disease in pediatric patients: a pediatric oncology group study. J Clin Oncol 15:2769–2779
Schwartz CL, Constine LS, Villaluna D, London WB, Hutchison RE, Sposto R et al (2009) A risk-adapted, response-based approach using ABVE-PC for children and adolescents with intermediate- and high-risk Hodgkin lymphoma: the results of P9425. Blood 114:2051–2059
Diehl V, Franklin J, Pfreundschuh M, Lathan B, Paulus U, Hasenclever D et al (2003) Standard and increased-dose BEACOPP chemotherapy compared with COPP-ABVD for advanced Hodgkin’s disease. N Engl J Med 348:2386–2395
Horning SJ, Hoppe RT, Breslin S, Bartlett NL, Brown BW, Rosenberg SA, Stanford V (2002) Radiotherapy for locally extensive and advanced Hodgkin’s disease: mature results of a prospective clinical trial. J Clin Oncol 20:630–637
Mauz-Körholz C, Metzger ML, Kelly KM, Schwartz CL, Castellanos ME, Dieckmann K, Kluge R, Körholz D (2015) Pediatric Hodgkin lymphoma. J Clin Oncol 33(27):2975–2985
Keller FG, Castellino SM, Chen L, Pei Q, Voss SD, McCarten KM et al (2018) Results of the AHOD0431 trial of response adapted therapy and a salvage strategy for limited stage, classical Hodgkin lymphoma: a report from the Children’s Oncology Group. Cancer 124:3210–3219
Friedman DL, Chen L, Wolden S, Buxton A, McCarten K, FitzGerald TJ et al (2014) Dose-intensive response-based chemotherapy and radiation therapy for children and adolescents with newly diagnosed intermediate-risk Hodgkin lymphoma: a report from the Children’s Oncology Group Study AHOD0031. J Clin Oncol 32:3651–3658
Mauz-Korholz C. Second International Inter-Group Study for Classical Hodgkin Lymphoma in Children and Adolescents. ClinicalTrials.gov Identifier: NCT02684708. https://clinicaltrials.gov/ct2/show/NCT02684708
Kaldor JM, Day NE, Clarke EA, Van Leeuwen FE, Henry-Amar M, Fiorentino MV et al (1990) Leukemia following Hodgkin’s disease. N Engl J Med 322:7–13
Mackie EJ, Radford M, Shalet SM (1996) Gonadal function following chemotherapy for childhood Hodgkin’s disease. Med Pediatr Oncol 27:74–78
Ortin TT, Shostak CA, Donaldson SS (1990) Gonadal status and reproductive function following treatment for Hodgkin’s disease in childhood: the Stanford experience. Int J Radiat Oncol Biol Phys 19:873–880
van den Berg H, Furstner F, van den Bos C, Behrendt H (2004) Decreasing the number of MOPP courses reduces gonadal damage in survivors of childhood Hodgkin disease. Pediatr Blood Cancer 42:210–215
Canellos GP, Anderson JR, Propert KJ, Nissen N, Cooper MR, Henderson ES et al (1992) Chemotherapy of advanced Hodgkin’s disease with MOPP, ABVD, or MOPP alternating with ABVD. N Engl J Med 327:1478–1484
Hunger SP, Link MP, Donaldson SS (1994) ABVD/MOPP and low-dose involved-field radiotherapy in pediatric Hodgkin’s disease: the Stanford experience. J Clin Oncol 12:2160–2166
Bramswig JH, Heimes U, Heiermann E, Schlegel W, Nieschlag E, Schellong G (1990) The effects of different cumulative doses of chemotherapy on testicular function. Results in 75 patients treated for Hodgkin’s disease during childhood or adolescence. Cancer 65:1298–1302
Schellong G, Hornig I, Bramswig J, Bokkerink JP, Steinhoff A, Ludwig R et al (1988) Significance of procarbazine in the chemotherapy of Hodgkin’s disease--a report of the cooperative therapy study DAL-HD-85. Klin Padiatr 200:205–213
Bonadonna G (1982) Santoro a. ABVD chemotherapy in the treatment of Hodgkin’s disease. Cancer Treat Rev 9:21–35
Dorffel W, Luders H, Ruhl U, Albrecht M, Marciniak H, Parwaresch R et al (2003) Preliminary results of the multicenter trial GPOH-HD 95 for the treatment of Hodgkin’s disease in children and adolescents: analysis and outlook. Klin Padiatr 215:139–145
Nachman JB, Sposto R, Herzog P, Gilchrist GS, Wolden SL, Thomson J et al (2002) Randomized comparison of low-dose involved-field radiotherapy and no radiotherapy for children with Hodgkin’s disease who achieve a complete response to chemotherapy. J Clin Oncol 20:3765–3771
Wolden SL, Chen L, Kelly KM, Herzog P, Gilchrist GS, Thomson J et al (2012) Long-term results of CCG 5942: a randomized comparison of chemotherapy with and without radiotherapy for children with Hodgkin’s lymphoma--a report from the Children’s oncology group. J Clin Oncol 30:3174–3180
Landman-Parker J, Pacquement H, Leblanc T, Habrand JL, Terrier-Lacombe MJ, Bertrand Y et al (2000) Localized childhood Hodgkin’s disease: response-adapted chemotherapy with etoposide, bleomycin, vinblastine, and prednisone before low-dose radiation therapy-results of the French Society of Pediatric Oncology Study MDH90. J Clin Oncol 18:1500–1507
Ruhl U, Albrecht M, Dieckmann K, Luders H, Marciniak H, Schellenberg D et al (2001) Response-adapted radiotherapy in the treatment of pediatric Hodgkin’s disease: an interim report at 5 years of the German GPOH-HD 95 trial. Int J Radiat Oncol Biol Phys 51:1209–1218
Dorffel W, Ruhl U, Luders H, Claviez A, Albrecht M, Bokkerink J et al (2013) Treatment of children and adolescents with Hodgkin lymphoma without radiotherapy for patients in complete remission after chemotherapy: final results of the multinational trial GPOH-HD95. J Clin Oncol 31:1562–1568
Schellong G (1996) Treatment of children and adolescents with Hodgkin’s disease: the experience of the German-Austrian Paediatric study group. Baillieres Clin Haematol 9:619–634
Mauz-Korholz C, Hasenclever D, Dorffel W, Ruschke K, Pelz T, Voigt A et al (2010) Procarbazine-free OEPA-COPDAC chemotherapy in boys and standard OPPA-COPP in girls have comparable effectiveness in pediatric Hodgkin’s lymphoma: the GPOH-HD-2002 study. J Clin Oncol 28:3680–3686
Keller FG, Nachman J, Constine L et al (2010) A phase III study for the treatment of children and adolescents with newly diagnosed low risk Hodgkin lymphoma (HL). ASH Annual Meeting. Blood 116(21):767
Donaldson SS, Hudson MM, Lamborn KR, Link MP, Kun L, Billett AL et al (2002) VAMP and low-dose, involved-field radiation for children and adolescents with favorable, early-stage Hodgkin’s disease: results of a prospective clinical trial. J Clin Oncol 20:3081–3087
Tebbi CKMN, Schwartz C, Williams J (2001) Response dependent treatment of stages IA, IIA, and IIIA1 micro Hodgkin’s disease with ABVE and low dose involved field irradiation with or without dexrazoxane. Leuk Lymphoma 42:100
Shahidi M, Kamangari N, Ashley S, Cunningham D, Horwich A (2006) Site of relapse after chemotherapy alone for stage I and II Hodgkin’s disease. Radiother Oncol 78:1–5
Girinsky T, van der Maazen R, Specht L, Aleman B, Poortmans P, Lievens Y et al (2006) Involved-node radiotherapy (INRT) in patients with early Hodgkin lymphoma: concepts and guidelines. Radiother Oncol 79:270–277
Specht L, Yahalom J, Illidge T, Berthelsen AK, Constine LS, Eich HT et al (2014) Modern radiation therapy for Hodgkin lymphoma: field and dose guidelines from the international lymphoma radiation oncology group (ILROG). Int J Radiat Oncol Biol Phys 89:854–862
Terezakis SA, Metzger ML, Hodgson DC, Schwartz CL, Advani R, Flowers CR et al (2014) ACR appropriateness criteria pediatric Hodgkin lymphoma. Pediatr Blood Cancer 61:1305–1312
Hodgson DC, Dieckmann K, Terezakis S, Constine L, International Lymphoma Radiation Oncology G (2015) Implementation of contemporary radiation therapy planning concepts for pediatric Hodgkin lymphoma: Guidelines from the International Lymphoma Radiation Oncology Group. Pract Radiat Oncol 5:85–92
Hoppe BS, Flampouri S, Su Z, Latif N, Dang NH, Lynch J et al (2012) Effective dose reduction to cardiac structures using protons compared with 3DCRT and IMRT in mediastinal Hodgkin lymphoma. Int J Radiat Oncol Biol Phys 84:449–455
Korholz D, Claviez A, Hasenclever D, Kluge R, Hirsch W, Kamprad F et al (2004) The concept of the GPOH-HD 2003 therapy study for pediatric Hodgkin’s disease: evolution in the tradition of the DAL/GPOH studies. Klin Padiatr 216:150–156
Metzger ML, Weinstein HJ, Hudson MM, Billett AL, Larsen EC, Friedmann A et al (2012) Association between radiotherapy vs no radiotherapy based on early response to VAMP chemotherapy and survival among children with favorable-risk Hodgkin lymphoma. JAMA 307:2609–2616
Kelly KM, Hodgson D, Appel B, Chen L, Cole PD, Horton T et al (2013) Children’s oncology Group’s 2013 blueprint for research: Hodgkin lymphoma. Pediatr Blood Cancer 60:972–978
Korholz D, Kluge R, Wickmann L, Hirsch W, Luders H, Lotz I et al (2003) Importance of F18-fluorodeoxy-D-2-glucose positron emission tomography (FDG-PET) for staging and therapy control of Hodgkin’s lymphoma in childhood and adolescence – consequences for the GPOH-HD 2003 protocol. Onkologie 26:489–493
Weiner MA, Leventhal BG, Marcus R, Brecher M, Ternberg J, Behm FG et al (1991) Intensive chemotherapy and low-dose radiotherapy for the treatment of advanced-stage Hodgkin’s disease in pediatric patients: a pediatric oncology group study. J Clin Oncol 9:1591–1598
Oberlin O, Leverger G, Pacquement H, Raquin MA, Chompret A, Habrand JL et al (1992) Low-dose radiation therapy and reduced chemotherapy in childhood Hodgkin’s disease: the experience of the French Society of Pediatric Oncology. J Clin Oncol 10:1602–1608
Vecchi V, Pileri S, Burnelli R, Bontempi N, Comelli A, Testi AM et al (1993) Treatment of pediatric Hodgkin disease tailored to stage, mediastinal mass, and age. An Italian (AIEOP) multicenter study on 215 patients. Cancer 72:2049–2057
Shankar AG, Ashley S, Radford M, Barrett A, Wright D, Pinkerton CR (1997) Does histology influence outcome in childhood Hodgkin’s disease? Results from the United Kingdom Children’s Cancer Study Group. J Clin Oncol 15:2622–2630
Hudson MM, Krasin M, Link MP, Donaldson SS, Billups C, Merchant TE et al (2004) Risk-adapted, combined-modality therapy with VAMP/COP and response-based, involved-field radiation for unfavorable pediatric Hodgkin’s disease. J Clin Oncol 22:4541–4550
Atra A, Higgs E, Capra M, Elsworth A, Imeson J, Radford M et al (2002) ChlVPP chemotherapy in children with stage IV Hodgkin’s disease: results of the UKCCSG HD 8201 and HD 9201 studies. Br J Haematol 119:647–651
Friedman DL, Wolden S, Constine LS, et al AHOD0031: a phase III study of dose-intensive therapy for intermediate risk Hodgkin lymphoma: a report from the Children’s Oncology Group 2010. p. 766
Friedmann AM, Hudson MM, Weinstein HJ, Donaldson SS, Kun L, Tarbell NJ et al (2002) Treatment of unfavorable childhood Hodgkin’s disease with VEPA and low-dose, involved-field radiation. J Clin Oncol 20:3088–3094
Carde P, MacKintosh FR, Rosenberg SA (1983) A dose and time response analysis of the treatment of Hodgkin’s disease with MOPP chemotherapy. J Clin Oncol 1:146–153
De Vita VT Jr, Hubbard SM, Longo DL (1990) Treatment of Hodgkin’s disease. J Natl Cancer Inst Monogr 10:19–28
van Rijswijk RE, Haanen C, Dekker AW, de Meijer AJ, Verbeek J (1989) Dose intensity of MOPP chemotherapy and survival in Hodgkin’s disease. J Clin Oncol 7:1776–1782
Kelly KM, Cole PD, Chen L, Roberts KB, Hodgson DC, McCarten K, et al. Phase III Study of Response Adapted Therapy for the Treatment of Children with Newly Diagnosed Very High Risk Hodgkin Lymphoma (Stages IIIB/IVB) (AHOD0831): A Report from the Children’s Oncology Group. 57th ASH Annual Meeting 2015. p. 3927
Kelly KM, Hutchinson RJ, Sposto R, Weiner MA, Lones MA, Perkins SL et al (2002) Feasibility of upfront dose-intensive chemotherapy in children with advanced-stage Hodgkin’s lymphoma: preliminary results from the Children's cancer group study CCG-59704. Ann Oncol 13(Suppl 1):107–111
Charpentier AM, Friedman DL, Wolden S, Schwartz C, Gill B, Sykes J et al (2016) Predictive factor analysis of response-adapted radiation therapy for chemotherapy-sensitive pediatric Hodgkin lymphoma: analysis of the Children’s oncology group AHOD 0031 trial. Int J Radiat Oncol Biol Phys 96:943–950
Connors JM, Jurczak W, Straus DJ, Ansell SM, Kim WS, Gallamini A et al (2018) Brentuximab Vedotin with chemotherapy for stage III or IV Hodgkin’s lymphoma. N Engl J Med 378:331–344
Mason DY, Banks PM, Chan J, Cleary ML, Delsol G, de Wolf Peeters C et al (1994) Nodular lymphocyte predominance Hodgkin’s disease. A distinct clinicopathological entity. Am J Surg Pathol 18:526–530
Diehl V, Sextro M, Franklin J, Hansmann ML, Harris N, Jaffe E et al (1999) Clinical presentation, course, and prognostic factors in lymphocyte-predominant Hodgkin’s disease and lymphocyte-rich classical Hodgkin’s disease: report from the European task force on lymphoma project on lymphocyte-predominant Hodgkin’s disease. J Clin Oncol 17:776–783
Shankar A, Hall GW, Gorde-Grosjean S, Hasenclever D, Leblanc T, Hayward J et al (2012) Treatment outcome after low intensity chemotherapy [CVP] in children and adolescents with early stage nodular lymphocyte predominant Hodgkin’s lymphoma – an Anglo-French collaborative report. Eur J Cancer 48:1700–1706
Sandoval C, Venkateswaran L, Billups C, Slim M, Jayabose S, Hudson MM (2002) Lymphocyte-predominant Hodgkin disease in children. J Pediatr Hematol Oncol 24:269–273
Mauz-Korholz C, Gorde-Grosjean S, Hasenclever D, Shankar A, Dorffel W, Wallace WH et al (2007) Resection alone in 58 children with limited stage, lymphocyte-predominant Hodgkin lymphoma-experience from the European network group on pediatric Hodgkin lymphoma. Cancer 110:179–185
Appel B, Ehrlich P, Chen L, et al. Treatment of pediatric stage IA lymphocyte-predominant Hodgkin lymphoma with surgical resection alone: a report from the Children’s Oncology Group. ASCO Annual Meeting 2012. p. 9524
Murphy SB, Morgan ER, Katzenstein HM, Kletzel M (2003) Results of little or no treatment for lymphocyte-predominant Hodgkin disease in children and adolescents. J Pediatr Hematol Oncol 25:684–687
Pellegrino B, Terrier-Lacombe MJ, Oberlin O, Leblanc T, Perel Y, Bertrand Y et al (2003) Lymphocyte-predominant Hodgkin’s lymphoma in children: therapeutic abstention after initial lymph node resection--a study of the French Society of Pediatric Oncology. J Clin Oncol 21:2948–2952
Hall GW, Katzilakis N, Pinkerton CR, Nicolin G, Ashley S, McCarthy K et al (2007) Outcome of children with nodular lymphocyte predominant Hodgkin lymphoma – a Children’s cancer and Leukaemia group report. Br J Haematol 138:761–768
Appel B, Chen L, Hutchinson RJ, Hodgson D, Ehrlich P, Constine L et al (2014) Treatment of pediatric lymphocyte predominant Hodgkin lymphoma (LPHL): a report from the Children’s Oncology Group. Klin Padiatr 226:10
Biasoli I, Stamatoullas A, Meignin V, Delmer A, Reman O, Morschhauser F et al (2010) Nodular, lymphocyte-predominant Hodgkin lymphoma: a long-term study and analysis of transformation to diffuse large B-cell lymphoma in a cohort of 164 patients from the adult lymphoma study group. Cancer 116:631–639
Wickert RS, Weisenburger DD, Tierens A, Greiner TC, Chan WC (1995) Clonal relationship between lymphocytic predominance Hodgkin’s disease and concurrent or subsequent large-cell lymphoma of B lineage. Blood 86:2312–2320
Advani RH, Horning SJ, Hoppe RT, Daadi S, Allen J, Natkunam Y et al (2014) Mature results of a phase II study of rituximab therapy for nodular lymphocyte-predominant Hodgkin lymphoma. J Clin Oncol 32:912–918
Moskowitz CH, Matasar MJ, Zelenetz AD, Nimer SD, Gerecitano J, Hamlin P et al (2012) Normalization of pre-ASCT, FDG-PET imaging with second-line, non-cross-resistant, chemotherapy programs improves event-free survival in patients with Hodgkin lymphoma. Blood 119:1665–1670
Bhatia S, Robison LL, Francisco L, Carter A, Liu Y, Grant M et al (2005) Late mortality in survivors of autologous hematopoietic-cell transplantation: report from the bone marrow transplant survivor study. Blood 105:4215–4222
Baker KS, Gordon BG, Gross TG, Abromowitch MA, Lyden ER, Lynch JC et al (1999) Autologous hematopoietic stem-cell transplantation for relapsed or refractory Hodgkin’s disease in children and adolescents. J Clin Oncol 17:825–831
Claviez A, Sureda A, Schmitz N (2008) Haematopoietic SCT for children and adolescents with relapsed and refractory Hodgkin’s lymphoma. Bone Marrow Transplant 42(Suppl 2):S16–S24
Lieskovsky YE, Donaldson SS, Torres MA, Wong RM, Amylon MD, Link MP et al (2004) High-dose therapy and autologous hematopoietic stem-cell transplantation for recurrent or refractory pediatric Hodgkin’s disease: results and prognostic indices. J Clin Oncol 22:4532–4540
Schellong G, Dorffel W, Claviez A, Korholz D, Mann G, Scheel-Walter HG et al (2005) Salvage therapy of progressive and recurrent Hodgkin’s disease: results from a multicenter study of the pediatric DAL/GPOH-HD Study Group. J Clin Oncol 23:6181–6189
Gorde-Grosjean S, Oberlin O, Leblanc T, Pacquement H, Donadieu J, Lambilliotte A et al (2012) Outcome of children and adolescents with recurrent/refractory classical Hodgkin lymphoma, a study from the Societe Francaise de Lutte contre le cancer des Enfants et des adolescents (SFCE). Br J Haematol 158:649–656
Akhtar S, El Weshi A, Rahal M, Abdelsalam M, Al Husseini H, Maghfoor I (2010) High-dose chemotherapy and autologous stem cell transplant in adolescent patients with relapsed or refractory Hodgkin’s lymphoma. Bone Marrow Transplant 45:476–482
Williams CD, Goldstone AH, Pearce R, Green S, Armitage JO, Carella A et al (1993) Autologous bone marrow transplantation for pediatric Hodgkin’s disease: a case-matched comparison with adult patients by the European bone marrow transplant group lymphoma registry. J Clin Oncol 11:2243–2249
Moskowitz AJ, Schoder H, Gavane S, Thoren KL, Fleisher M, Yahalom J et al (2017) Prognostic significance of baseline metabolic tumor volume in relapsed and refractory Hodgkin lymphoma. Blood 130:2196–2203
Constine LS, Yahalom J, Ng AK, Hodgson DC, Wirth A, Milgrom SA et al (2018) The role of radiation therapy in patients with relapsed or refractory Hodgkin lymphoma: Guidelines From the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 100:1100–1118
Chen AR, Hutchison R, Hess A et al (2007) Clinical outcomes of patients with recurrent/refractory Hodgkin disease receiving cyclosporine, interferon-V and interleukin-2 immunotherapy to induce autoreactivity after autologous stem cell transplantation with BEAM: a COG study. Blood 110:1896
Frankovich J, Donaldson SS, Lee Y, Wong RM, Amylon M, Verneris MR (2001) High-dose therapy and autologous hematopoietic cell transplantation in children with primary refractory and relapsed Hodgkin’s disease: atopy predicts idiopathic diffuse lung injury syndromes. Biol Blood Marrow Transplant 7:49–57
Stoneham S, Ashley S, Pinkerton CR, Wallace WH, Shankar AG, United Kingdom Children’s Cancer Study G (2004) Outcome after autologous hemopoietic stem cell transplantation in relapsed or refractory childhood Hodgkin disease. J Pediatr Hematol Oncol 26:740–745
Bradley MB, Cairo MS (2008) Stem cell transplantation for pediatric lymphoma: past, present and future. Bone Marrow Transplant 41:149–158
Claviez A, Canals C, Dierickx D, Stein J, Badell I, Pession A et al (2009) Allogeneic hematopoietic stem cell transplantation in children and adolescents with recurrent and refractory Hodgkin lymphoma: an analysis of the European Group for Blood and Marrow Transplantation. Blood 114:2060–2067
Locatelli F, Mauz-Koerholz C, Neville K, Llort A, Beishuizen A, Daw S et al (2018) Brentuximab vedotin for paediatric relapsed or refractory Hodgkin’s lymphoma and anaplastic large-cell lymphoma: a multicentre, open-label, phase 1/2 study. Lancet Haematol 5:e450–ee61
Younes A, Gopal AK, Smith SE, Ansell SM, Rosenblatt JD, Savage KJ et al (2012) Results of a pivotal phase II study of brentuximab vedotin for patients with relapsed or refractory Hodgkin’s lymphoma. J Clin Oncol 30:2183–2189
Harker-Murray P, Leblanc T, Mascarin M, Mauz-Körholz C, Michel G, Cooper S et al (2018) Response-adapted therapy with Nivolumab and Brentuximab Vedotin (BV), followed by BV and Bendamustine for suboptimal response, in children, adolescents, and young adults with standard-risk relapsed/refractory classical Hodgkin lymphoma. 60th ASH Annual Meeting. Blood:927
Ansell SM, Lesokhin AM, Borrello I, Halwani A, Scott EC, Gutierrez M et al (2015) PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med 372:311–319
Armand P, Shipp MA, Ribrag V, Michot JM, Zinzani PL, Kuruvilla J et al (2016) Programmed Death-1 blockade with Pembrolizumab in patients with classical Hodgkin lymphoma after Brentuximab Vedotin failure. J Clin Oncol 34:3733–3739
LaCasce AS, Bociek RG, Sawas A, Caimi P, Agura E, Matous J et al (2018) Brentuximab vedotin plus bendamustine: a highly active first salvage regimen for relapsed or refractory Hodgkin lymphoma. Blood 132:40–48
Marina NM, Greenwald CA, Fairclough DL, Thompson EI, Wilimas JA, Mackert PW et al (1995) Serial pulmonary function studies in children treated for newly diagnosed Hodgkin’s disease with mantle radiotherapy plus cycles of cyclophosphamide, vincristine, and procarbazine alternating with cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine. Cancer 75:1706–1711
Mefferd JM, Donaldson SS, Link MP (1989) Pediatric Hodgkin’s disease: pulmonary, cardiac, and thyroid function following combined modality therapy. Int J Radiat Oncol Biol Phys 16:679–685
Green DM, Hall B (1988) Pregnancy outcome following treatment during childhood or adolescence for Hodgkin’s disease. Pediatr Hematol Oncol 5:269–277
Hudson MM, Poquette CA, Lee J, Greenwald CA, Shah A, Luo X et al (1998) Increased mortality after successful treatment for Hodgkin’s disease. J Clin Oncol 16:3592–3600
Adams MJ, Lipsitz SR, Colan SD, Tarbell NJ, Treves ST, Diller L et al (2004) Cardiovascular status in long-term survivors of Hodgkin’s disease treated with chest radiotherapy. J Clin Oncol 22:3139–3148
Green DM, Hyland A, Chung CS, Zevon MA, Hall BC (1999) Cancer and cardiac mortality among 15-year survivors of cancer diagnosed during childhood or adolescence. J Clin Oncol 17:3207–3215
Wolden SL, Lamborn KR, Cleary SF, Tate DJ, Donaldson SS (1998) Second cancers following pediatric Hodgkin’s disease. J Clin Oncol 16:536–544
Sankila R, Garwicz S, Olsen JH, Dollner H, Hertz H, Kreuger A et al (1996) Risk of subsequent malignant neoplasms among 1,641 Hodgkin’s disease patients diagnosed in childhood and adolescence: a population-based cohort study in the five Nordic countries. Association of the Nordic Cancer Registries and the Nordic Society of Pediatric Hematology and Oncology. J Clin Oncol 14:1442–1446
Holmqvist AS, Chen Y, Berano Teh J, Sun C, Birch JM, van den Bos C et al (2019) Risk of solid subsequent malignant neoplasms after childhood Hodgkin lymphoma-identification of high-risk populations to guide surveillance: a report from the late effects study group. Cancer 125(8):1373–1383
Green DM, Hyland A, Barcos MP, Reynolds JA, Lee RJ, Hall BC et al (2000) Second malignant neoplasms after treatment for Hodgkin’s disease in childhood or adolescence. J Clin Oncol 18:1492–1499
Bhatia S, Robison LL, Oberlin O, Greenberg M, Bunin G, Fossati-Bellani F et al (1996) Breast cancer and other second neoplasms after childhood Hodgkin’s disease. N Engl J Med 334:745–751
Metayer C, Lynch CF, Clarke EA, Glimelius B, Storm H, Pukkala E et al (2000) Second cancers among long-term survivors of Hodgkin’s disease diagnosed in childhood and adolescence. J Clin Oncol 18:2435–2443
Constine LS, Tarbell N, Hudson MM, Schwartz C, Fisher SG, Muhs AG et al (2008) Subsequent malignancies in children treated for Hodgkin’s disease: associations with gender and radiation dose. Int J Radiat Oncol Biol Phys 72:24–33
Acknowledgments
Thanks to Laura Finger, Rochester, for her help with the final draft and references of the third edition 2019.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hall, G.W., Schwartz, C., Daw, S., Constine, L.S. (2020). Pediatric Hodgkin Lymphoma. In: Engert, A., Younes, A. (eds) Hodgkin Lymphoma. Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-32482-7_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-32482-7_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32481-0
Online ISBN: 978-3-030-32482-7
eBook Packages: MedicineMedicine (R0)