Abstract
Given the success of frontline treatments and the ability to salvage the majority of Hodgkin lymphoma (HL) patients after disease progression or recurrence, the short-term overall survival of HL is high. However, this survival comes at a cost to patients in the form of late effects, which can alter both the length and quality of survivorship. To reduce downstream late-effect risk while preserving excellent disease control, modifications have been made in frontline therapy, including changes in indications for radiation, reduction in radiation dose and field among those receiving treatment, risk stratification to determine need for either dose reduction or dose escalation to optimize outcomes, and incorporation of novel agents, initially in the salvage setting and more recently in frontline therapy.
To guide patients and their families, alongside their providers, we describe the process of developing robust and nimble decision models to enhance and optimize the difficult decisions that affect acute and long-term outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Treatment Choices and Individualized Care
Hodgkin lymphoma (HL) is one of the best curable cancers, particularly when presenting as early-stage disease [1,2,3]. Although outcomes differ by age, cure rates exceed 80–85% across most stages and ages. Despite these overall excellent outcomes, there is no clear consensus regarding treatment recommendations across age groups, and individual patients, with regard to several treatment options, including which chemotherapy regimen to use, the optimal number of chemotherapy cycles, and the role of sequential adjunctive radiation therapy (RT) [1, 2, 4,5,6,7,8,9,10,11,13]. Furthermore, choices and debate over therapeutic options have further expanded to include if and how to integrate and use early/interim positron emission tomography (PET) therapy to guide treatment (i.e., response-adapted therapy), as well as the optimum integration of novel therapeutics into frontline therapy [6, 14,15,16,17].
2 Treatment-Related Late Effects and Associated Human Cost
Critically, because the majority of newly diagnosed HL patients are young (median age 35 years) [18], curing disease can come at considerable “human cost,” including treatment-related toxicities and late effects (LE) (e.g., secondary malignant neoplasms [SMN], cardiovascular disease [CVD]) and potential loss of young lives. The incidence of CVD and SMN rises exponentially >20–30 years after treatment. Results from analyses led by Dutch investigators and others have shown that the risk of SMNs do not appear to differ or be significantly lower over consecutive time periods [19,20,21]. Both Ng et al. [15] and Castellino et al. [18] have highlighted increased mortality among long-term HL survivors, although both of these studies reflect the impact of historical treatment approaches, including extended field radiotherapy.
Additionally, cost-per-death analyses also have shown that HL has the second highest cost per death or lost productivity cost, behind only malignant melanoma [22]. Further, productivity analyses of cancer mortality have shown HL to be the second most costly cancer in terms of lost lifetime earnings [23]. In addition to economic consequences, HL survivors also experience significantly compromised health-related quality of life (HRQL) due to LEs [24].
3 Risk, Impact, and Variability of Treatment-Related Late Effects
The risk of SMN depends on many clinical factors (e.g., age at exposure, sex, stage) as well as several treatment-related factors (e.g., chemotherapy [type and number of cycles] and RT [dose and field]). A recent Dutch analysis highlighted the impact of radiation dose and field, sex, and smoking on the risk of breast, lung, and other cancers [19]. Studies have investigated the impact of age and sex on the development of solid cancers after treatment for HL [25] and the impact of sex and type of treatment (i.e., anthracycline chemotherapy ± radiation) on the incidence of major cardiac disease [26, 27]. However, it is not possible to use current population-level findings to reliably predict outcomes of alternative therapies for specific, individual patients and hence contribute to fully informed decision-making.
4 Paucity of Harmonized Data to Guide Providers and Patients Towards Individualized Treatment Choices
Helping clinicians assess and navigate alternative HL treatment options for individual patients poses substantial challenges. First, ideal information is not available. Often, empirical data for contemporary therapies is limited to relatively short-term follow-up with differences in initial risk and response criteria driving therapy and limited information about the risk and severity of treatment-related LEs. While follow-up data from previous treatment eras offer insights [28], treatment changes and improvements over time limit the relevance of existing information. Second, the benefits and risks of different therapies depend in part on individual characteristics, such as patient age and sex, among other factors. A recent HL position paper by Travis and Ng et al. recommended development of comprehensive risk prediction models for LEs to customize treatment strategies [29].
There is a need to harmonize individual patient data across age groups from recent trials and existing datasets while establishing a data repository that facilitates incorporation of future data. The past 15 years have seen publications of several clinical trials involving many pediatric and adult HL patients with early-stage and advanced-stage disease [3, 30]. However, each study examined a slightly different HL question and most used different treatments. The result was a range of distinct findings and hence a wide range of therapeutic choices (Table 14.1).
Over the past 10 years, most HL studies worldwide have integrated PET-response-adapted designs, an approach that directs the type and/or amount of therapy based on PET scan results (positive vs. negative) early during the patient’s treatment course, usually after two chemotherapy cycles [16, 33]. These PET-response-adapted data have significantly expanded the range of treatments that providers and patients must consider in assessing treatment options for individual HL patients.
Taken together, there remains a multitude of unanswered questions, especially for individual HL patients, as exemplified by the index case example above, including: (1) What is the efficacy of alternative treatments, and how do individual patient and disease characteristics influence efficacy? (2) What is the HRQL impact of each treatment option? (3) What are the incidence and severity of LEs (absolute risk for different SMNs and/or CVD), and how do these outcomes depend on treatment, individual patient characteristics, and disease characteristics? (4) How does “real-world” HL data inform treatment decisions in light of patient preferences?
5 Disease Classification and Prognostication
In adults, “early-stage” HL is often subdivided into two categories designated “favorable” and “unfavorable,” with the distinction made on the basis of clinical factors and blood test results [3]. However, there are several different classifications that have been developed and studied over the past 20 years in prospective HL clinical studies. The criteria used by the German Hodgkin Study Group (GHSG) and the European Organization for Research and Treatment of Cancer (EORTC) differ with regard to several factors, such as number of nodal groups. Furthermore, the “nodal maps” differ, reflecting differences between GHSG and EORTC clinical studies [14, 15, 34, 35]. In addition, clinical studies conducted in North America have utilized different criteria to delineate early-stage disease, and some HL clinical trials have not separated early-stage patients into different groups [4, 5]. These staging definition differences can influence the treatment patients receive and their outcomes. Advanced disease has generally been classified as Ann Arbor stage III and IV, but clinical trials have often included patients with high-risk stage II disease, such as those with B-symptoms, involvement at multiple sites, and/or bulky disease. The inclusion criteria have often varied on a study-by-study basis, leading to substantial patient heterogeneity across HL studies.
Pediatric oncology research groups in the United States and across the world have used different criteria than adult groups use to categorize HL patients [10, 36]. While both pediatric and adult groups rely on the Ann Arbor classification system for staging, risk stratification has varied within these risk groups. For example, some adult studies classify patients with stage IIB disease with bulk as having early-stage disease, while pediatric trials currently designate patients as having advanced-stage disease based on inferior outcomes. Similarly, application of adult criteria would classify pediatric patients with stage IIIA disease as having advanced disease even though these patients have had superior outcomes compared to other pediatric subgroups (e.g., stage IIIB, IVA, IVB). Some pediatric trials do not include these patients in advanced-stage studies, but, rather, designate them to be at “intermediate” risk.
Prognosis in adult advanced-stage HL as defined by the International Prognostic Index (IPS) in 1998 includes measurements of albumin, hemoglobin, sex, ages >45 years, stage IV, and the presence of leukocytosis or lymphocytosis [37]. HL patients with higher IPS scores had inferior treatment outcomes and were thus identified as potentially requiring more intensive therapy. The British Columbia Cancer Agency (BCCA) conducted an updated analysis of the IPS that showed that the utility of the IPS was altered [38]. In this analysis, the 5-year freedom from progression (FFP) ranged from 62% to 88% and 5-year OS ranged from 67% to 98% with a much narrower range of outcomes for patients ages <65 years (FFP ranging from 70% to 88% and 5-year OS ranging from 73% to 98%). Furthermore, in a multivariate regression analysis, which controlled for all IPS factors, only age and hemoglobin level retained independent significance.
Notably, no new and more comprehensive prognostic models have been developed for HL (early stage or advanced stage) in more than 20 years. Because age is an integral component of the original IPS, attempts have been made to develop and validate a child-specific prognostic score, known as CHIPS (Childhood Hodgkin International Prognostic Score) [39]. The original testing found that several factors were independent predictors of event-free survival (EFS), including stage IV, large mediastinal mass, low albumin, and fever. Further validation in other cohorts of children and adolescents with advanced disease is underway.
6 Simulation Modeling
Statistical and simulation modeling offers a rigorous approach to systematically and explicitly incorporate assumptions and information based on multiple data sources to explore how alternative treatments affect outcomes of interest, including LEs, survival, and quality-adjusted survival. Collectively, harmonization of independent patient data from large, international prospective studies and prominent cancer registries, along with development of common data standards, will establish robust “patient-specific” disease progression and LE probabilities that may be harnessed for dynamic decision-making tools with the expectation of ultimately improving outcomes across pediatric and adult HL.
Decision models have proved useful in connection with other diseases when treatment options involve trade-offs, and the risks and benefits can vary substantially, depending on patient characteristics. Here, we review the models developed to evaluate measures to either help prevent or treat two conditions: (1) lung cancer and (2) diffuse large B-cell lymphoma (DLBCL).
6.1 Low-Dose CT Scan for Lung Cancer
The National Lung Screening Trial (NLST) demonstrated that for patients at high risk for lung cancer mortality, low-dose computed tomography (LDCT) reduces lung cancer mortality by 20 percent compared to screening by conventional chest X-ray [40]. Cost-effectiveness analysis revealed that compared to no screening, LDCT accrues 0.02 quality adjusted life years (QALYs) per person screened at an incremental cost of $1631 [41]. The corresponding cost-effectiveness ratio suggesting an outlay of $81,000 per QALY gained represents “good value” relative to contemporary benchmarks for the United States [42].
Nonetheless, there remains the possibility that more narrowly targeted selection of the population to be screened would accrue even greater benefits and, hence, achieve a more favorable cost-effectiveness ratio. Kovalchik et al. [43] reported that after ranking the NLST population by estimated lung cancer mortality risk, screening prevented one lung cancer death for every 5276 individuals in the lowest-risk quintile, but that it achieved the same benefit for every 161 screened among the highest-risk quintile. The risk function developed by Kovalchik et al. therefore offers an approach for reducing the amount of screening needed to achieve the same mortality reduction.
Kumar et al. [44] investigated the efficiency of targeting individuals at even higher risk for lung cancer mortality than the NLST population as a whole. Using a different risk model than Kovalchik et al., Kumar et al. reported similar efficiency gains for reducing lung cancer mortality. Screening top decile individuals yielded a nearly eightfold gain in averted deaths per person screened, compared to screening of individuals in the bottom decile. Assessment using other outcome measures yielded less impressive efficiency gains. For life years gained, the benefit per person screened was 3.6 times greater for top mortality risk decile individuals, compared to the bottom decile. For quality-adjusted life year gains (QALYs), the corresponding ratio was 2.4. Finally, the cost-effectiveness of screening improved across the risk deciles by an even smaller relative margin, from $75,000 per QALY gained in the lowest-risk decile to $53,000 per QALY gained in the highest-risk decile, a ratio of approximately 1.4.
The broad range of efficiency gains for different outcome measures illustrates both the strengths and limitations of risk targeting. When the targeting criterion—lung cancer mortality risk, in this case—matches the outcome measure, targeting vastly improves efficiency. On the other hand, when the outcome measure is less tightly related to the targeting measure, potential efficiency gains can decrease. Kumar et al. note, for example, that in the NLST cohort, higher-risk individuals were older, had greater smoking exposure, and were more likely to have a preexisting diagnosis of chronic obstructive pulmonary disease [44]. Because the characteristics making these individuals “high risk” also reduce life expectancy, targeting is less effective at maximizing life year gains. Likewise, mortality risk is inversely associated with future quality of life and positively associated with higher future care costs. Those factors further mitigate the efficiency gains from mortality risk targeting measured in terms of QALY gains and cost-effectiveness.
6.2 Diffuse Large B-Cell Lymphoma (DLBCL)
Because there are multiple treatments for patients with DLBCL, and because treatments vary in terms of their intensity and side effects, an accurate prognosis is crucial to identifying a course of care that appropriately accounts for a patient’s risks and benefits.
In recent decades, clinicians have relied on the International Prognostic Index (IPI) to characterize risk [45]. The IPI produces a risk score ranging from 0 to 5 based on a series of dichotomized risk factors, including age (less than 60 vs. 60 or older), number of extranodal sites (0–1 vs. 2 or more), Ann Arbor stage (I or II vs. III or IV), lactate dehydrogenase levels (not elevated vs. elevated), and Eastern Cooperative Oncology Group performance status (2 or less vs. greater than 2). Incorporation of additional prognostic characteristics has improved the prognostic accuracy of the IPI, but limitations remain, including the dichotomous characterization of inputs and the tool’s semi-qualitative characterization of risk that does not specify probabilities for key outcomes such as mortality.
To address these limitations, Biccler et al. [45] developed a model to predict overall survival and event-free survival as a function of both categorical characteristics (e.g., sex, Ann Arbor stage, presence or absence of B symptoms, among others) and continuous values (e.g., log leukocyte count, hemoglobin level, among others). The prediction reflects a weighted average of statistical models, with weights selected to maximize prediction accuracy.
The authors have made the model available on the Internet (https://lymphomapredictor.org/). The results show overall survival (compared to background survival) and event-free survival, both of which are projected over a period of five years. Because this model incorporates fine-grained individual characteristics and reports outcome probabilities over time, it represents a substantial improvement over earlier prognostic tools. Nonetheless, it has two key limitations. First, its projections are limited to a period of five years. That limitation reflects the extent of the follow-up in the population data used to build the model. Second, the model does not describe how alternative treatments influence outcomes. While clinicians and patients may infer that higher risks warrant more intensive treatment, the model does not quantify the resulting trade-offs.
Altogether, trade-offs, in the form of adverse events and resource costs, are common. Typically, these downside impacts do not depend on the size of the potential benefit. The size of the potential benefit, and hence the magnitude of the net benefit, often depends on how big the baseline risk is. As a result, targeting individuals at highest risk for disease or severe outcomes often increases efficiency. The effectiveness of this strategy depends on the strength of the association between the risk stratification measure and the benefit measure. Prognostic risk models can help clinicians and patients weigh treatment alternatives, but these models can be limited by their time horizon and the extent to which they incorporate the impact of alternative therapies.
7 Decision Models in Hodgkin Lymphoma (HL)
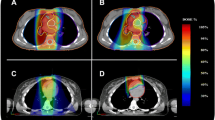
Given the varying treatment approaches and their trade-offs relative to disease control and LE risks and the impact of individual patient characteristics, such as gender and age at the time of exposure, there has been considerable interest in the development of decision models for newly diagnosed HL. Our initial model of early-stage HL utilized published, group-level data from recent clinical trials to estimate simulated short-term and long-term outcomes [46]. We began with the development of a detailed disease map (Fig. 14.1), which highlights the health states through which a patient can move once diagnosed with HL. Based on best available information, we estimated the probability of transitioning from one health state to the next and the HRQL of each health state in the form of utility weights.
Utility Weight Simulation Model: The State Transition Diagram. The bubbles represent individual health states. The value within each bubble is the utility weight (or health-related quality of life impact) of that health state. The arrows represent transition pathways between states. Scaling each year of survival by that year’s utility weight (specified for each health state in the figure) and then summing the quality-adjusted years yields quality-adjusted survival
To test the model, we created two hypothetical cases that differed with regard to gender, disease location, and extent of disease. We then compared the projected outcomes (life expectancy and QALYs) for each patient for each of two treatment modalities—chemotherapy alone and combined modality therapy [46]. Sensitivity analyses explored the impact on projected clinical outcomes of age at diagnosis and the assumed incidence and severity of late effects. The purpose of this initial model was not to identify which modality might be definitively superior to the other, but, rather, to illustrate that treatment recommendations should reflect patient factors, disease characteristics, and the outcome preferences of the patient and his/her provider.
Decision models such as these can also be adapted as new information becomes available. For example, consider the use of early PET-based response. In the figure below, we have added the PET-adapted response as a new health state (that is, rapid early response or slow early response) (Fig. 14.2). Because addition of this new health state requires revision of the probabilities downstream, such as risk of relapse, the revised decision model can be run to estimate updated clinical outcomes.
The State Transition Diagram—therapeutic-response enhanced model. Individuals in State A can proceed to States B or C2. The transition rates depend on whether the patient experiences a rapid or slow response to initial therapy—i.e., whether the individual progresses from substate A-i to A-ii, or to A-iii
To extend this one step further, one could utilize this type of model as patients transition from one phase of care to another, namely, from active treatment to active surveillance or active surveillance to survivorship. By incorporating emerging information, patients and their providers can refine ongoing care needs and clarify areas of likely risk and uncertainty.
The development of these types of dynamic decision models requires individual patient data from large numbers of patients to account for differences across patients in terms of their demographic characteristics and disease factors. Moreover, model development depends on identifying data projecting the impact of contemporary treatment on short- and long-term outcomes, including toxicity, death, relapse, and LEs. Data must also be updated, as additional information becomes available (e.g., from new trials, or from further follow-up of existing trials) and as new therapies are introduced.
Critical to the implementation and dissemination of these tools is an understanding of how patients, caregivers, and providers would use such models in the real world, what concerns they have, what kind of decision support they need, and what outcomes they are interested in. As noted, our first version of the model estimated life expectancy and QALYs, but these outcomes can be modified to reflect what is salient and/or accessible to different stakeholders.
8 Conclusion
Given the success of frontline treatments and the ability to salvage the majority of HL patients after disease progression or recurrence, the overall survival of HL is high. However, this survival comes at a cost to patients in the form of LEs, which can alter both the length and quality of survivorship. To reduce downstream LE risk, modifications have been made in frontline therapy, including: changes in indications for radiation, reduction in radiation dose and field among those receiving treatment, risk stratification to determine need for either dose reduction or dose escalation to optimize outcomes, and incorporation of novel agents, initially in the salvage setting and more recently in frontline therapy.
Through data sharing and international collaboration, including across pediatric and adult specialties, we can create robust and nimble decision models to guide our patients and their families, alongside their providers, to enhance and optimize the difficult decisions that affect acute and long-term outcomes.
References
Giulino-Roth L et al (2015) Current approaches in the management of low risk Hodgkin lymphoma in children and adolescents. Br J Haematol 169(5):647–660
Armitage JO (2010) Early-stage Hodgkin’s lymphoma. N Engl J Med 363(7):653–662
Evens AM, Hutchings M, Diehl V (2008) Treatment of Hodgkin lymphoma: the past, present, and future. Nat Clin Pract Oncol 5(9):543–556
Meyer RM et al (2005) Randomized comparison of ABVD chemotherapy with a strategy that includes radiation therapy in patients with limited-stage Hodgkin’s lymphoma: National Cancer Institute of Canada Clinical Trials Group and the Eastern Cooperative Oncology Group. J Clin Oncol 23(21):4634–4642
Meyer RM et al (2012) ABVD alone versus radiation-based therapy in limited-stage Hodgkin’s lymphoma. N Engl J Med 366(5):399–408
Radford J et al (2015) Results of a trial of PET-directed therapy for early-stage Hodgkin’s lymphoma. N Engl J Med 372(17):1598–1607
Percival ME, Hoppe RT, Advani RH (2014) Bulky mediastinal classical Hodgkin lymphoma in young women. Oncology (Williston Park) 28(3):253-6–258-60. C3
Crump M et al (2015) Evidence-based focused review of the role of radiation therapy in the treatment of early-stage Hodgkin lymphoma. Blood 125(11):1708–1716
Hay AE et al (2013) An individual patient-data comparison of combined modality therapy and ABVD alone for patients with limited-stage Hodgkin lymphoma. Ann Oncol 24(12):3065–3069
Wolden SL et al (2012) Long-term results of CCG 5942: a randomized comparison of chemotherapy with and without radiotherapy for children with Hodgkin’s lymphoma—a report from the Children’s Oncology Group. J Clin Oncol 30(26):3174–3180
Nachman JB et al (2002) Randomized comparison of low-dose involved-field radiotherapy and no radiotherapy for children with Hodgkin’s disease who achieve a complete response to chemotherapy. J Clin Oncol 20(18):3765–3771
Straus DJ et al (2004) Results of a prospective randomized clinical trial of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) followed by radiation therapy (RT) versus ABVD alone for stages I, II, and IIIA nonbulky Hodgkin disease. Blood 104(12):3483–3489
Laskar S et al (2004) Consolidation radiation after complete remission in Hodgkin’s disease following six cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine chemotherapy: is there a need? J Clin Oncol 22(1):62–68
Raemaekers JM et al (2014) Omitting radiotherapy in early positron emission tomography-negative stage I/II Hodgkin lymphoma is associated with an increased risk of early relapse: Clinical results of the preplanned interim analysis of the randomized EORTC/LYSA/FIL H10 trial. J Clin Oncol 32(12):1188–1194
Andre MP et al (2017) Early positron emission tomography response-adapted treatment in stage I and II Hodgkin lymphoma: final results of the randomized EORTC/LYSA/FIL H10 trial. J Clin Oncol 35(16):1786–1794. https://doi.org/10.1200/JCO.2016.68.6394
Evens AM, Kostakoglu L (2014) The role of FDG-PET in defining prognosis of Hodgkin lymphoma for early-stage disease. Blood 124(23):3356–3364
Olszewski AJ, Shrestha R, Castillo JJ (2015) Treatment selection and outcomes in early-stage classical Hodgkin lymphoma: analysis of the National Cancer Data Base. J Clin Oncol 33(6):625–633
Available from https://seer.cancer.gov/csr/1975_2015/.
Schaapveld M et al (2015) Second cancer risk up to 40 after treatment for Hodgkin’s lymphoma. N Engl J Med 373(26):2499–2511
Aleman BM et al (2007) Late cardiotoxicity after treatment for Hodgkin lymphoma. Blood 109(5):1878–1886
van Leeuwen FE, Ng AK (2016) Long-term risk of second malignancy and cardiovascular disease after Hodgkin lymphoma treatment. Hematology Am Soc Hematol Educ Program 2016(1):323–330
Hanly P, Soerjomataram I, Sharp L (2015) Measuring the societal burden of cancer: the cost of lost productivity due to premature cancer-related mortality in Europe. Int J Cancer 136(4):E136–E145
Bradley CJ et al (2008) Productivity costs of cancer mortality in the United States: 2000–2020. J Natl Cancer Inst 100(24):1763–1770
Linendoll N et al (2016) Health-related quality of life in Hodgkin lymphoma: a systematic review. Health Qual Life Outcomes 14(1):114
Hodgson DC et al (2007) Long-term solid cancer risk among 5-year survivors of Hodgkin’s lymphoma. J Clin Oncol 25(12):1489–1497
Myrehaug S et al (2008) Cardiac morbidity following modern treatment for Hodgkin lymphoma: supra-additive cardiotoxicity of doxorubicin and radiation therapy. Leuk Lymphoma 49(8):1486–1493
Myrehaug S et al (2010) A population-based study of cardiac morbidity among Hodgkin lymphoma patients with preexisting heart disease. Blood 116(13):2237–2240
Castellino SM et al (2011) Morbidity and mortality in long-term survivors of Hodgkin lymphoma: a report from the Childhood Cancer Survivor Study. Blood 117(6):1806–1816
Travis LB et al (2012) Second malignant neoplasms and cardiovascular disease following radiotherapy. J Natl Cancer Inst 104(5):357–370
Diefenbach CS et al (2017) Hodgkin lymphoma: current status and clinical trial recommendations. J Natl Cancer Inst 109:4
Straus DJ et al (2018) CALGB 50604: risk-adapted treatment of nonbulky early-stage Hodgkin lymphoma based on interim PET. Blood 132(10):1013–1021
Johnson P et al (2016) Adapted treatment guided by interim PET-CT scan in advanced Hodgkin’s lymphoma. N Engl J Med 374(25):2419–2429
Coyle M, Kostakoglu L, Evens AM (2016) The evolving role of response-adapted PET imaging in Hodgkin lymphoma. Ther Adv Hematol 7(2):108–125
von Tresckow B et al (2012) Dose-intensification in early unfavorable Hodgkin’s lymphoma: final analysis of the German Hodgkin Study Group HD14 trial. J Clin Oncol 30(9):907–913
Engert A et al (2010) Reduced treatment intensity in patients with early-stage Hodgkin’s lymphoma. N Engl J Med 363(7):640–652
Keller FG et al (2018) Results of the AHOD0431 trial of response adapted therapy and a salvage strategy for limited stage, classical Hodgkin lymphoma: a report from the Children’s Oncology Group. Cancer 124(15):3210–3219
Hasenclever D, Diehl V (1998) A prognostic score for advanced Hodgkin’s disease. International Prognostic Factors Project on Advanced Hodgkin’s Disease. N Engl J Med 339(21):1506–1514
Moccia AA et al (2012) International Prognostic Score in advanced-stage Hodgkin’s lymphoma: altered utility in the modern era. J Clin Oncol 30(27):3383–3388
Schwartz CL et al (2017) Childhood Hodgkin International Prognostic Score (CHIPS) Predicts event-free survival in Hodgkin lymphoma: a report from the Children’s Oncology Group. Pediatr Blood Cancer 64:4
Aberle DR et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365(5):395–409
Black WC et al (2014) Cost-effectiveness of CT screening in the National lung screening trial. N Engl J Med 371(19):1793–1802
Neumann PJ, Cohen JT, Weinstein MC (2014) Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med 371(9):796–797
Kovalchik SA et al (2013) Targeting of low-dose CT screening according to the risk of lung-cancer death. N Engl J Med 369(3):245–254
Kumar V et al (2018) Risk-targeted lung cancer screening: a cost-effectiveness analysis. Ann Intern Med 168(3):161–169
Biccler J et al (2018) Simplicity at the cost of predictive accuracy in diffuse large B-cell lymphoma: a critical assessment of the R-IPI, IPI, and NCCN-IPI. Cancer Med 7(1):114–122
Parsons SK et al (2018) Early-stage Hodgkin lymphoma in the modern era: simulation modelling to delineate long-term patient outcomes. Br J Haematol 182(2):212–221
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Parsons, S.K., Cohen, J.T., Evens, A.M. (2020). Optimizing Decision Making in Hodgkin Lymphoma. In: Engert, A., Younes, A. (eds) Hodgkin Lymphoma. Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-32482-7_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-32482-7_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32481-0
Online ISBN: 978-3-030-32482-7
eBook Packages: MedicineMedicine (R0)