Abstract
Polycyclic aromatic hydrocarbons (PAHs) are a large group of chemical contaminants, predominantly produced via fossil fuel combustion. They spread easily worldwide, so they are considered as semipersistent pollutants. Many of them are considered as carcinogenic or mutagenic compounds, for example, interacting directly with DNA. Benzo(a)pyrene (BaP) is the most important and well-known PAH. Living beings are exposed everyday through air, water, plastic stuff and smoke and almost by food intake, because they are highly lipophilic. In human risk assessments, monitoring these compounds, or their products, in environment, biological or food samples has attracted enormous interest. Pets commonly share habitat and routine life with humans. In this chapter, the possibility that pets were good sentinels of human exposure to PAHs is studied in detail. Concentrations of parental PAHs and some metabolites between human and pets have been compared. In the case of dogs, their concentrations and profiles of PAHs are very different to those of humans when compared. Dogs had lesser concentration of parental compounds and higher concentration of their metabolites than humans. Similarly, cats present different concentrations and detection frequencies than humans. Therefore, the scarce data available indicate that dogs and cats seem to have different sources of exposition to PAHs than humans. Although more studies are needed, pets do not seem to be good sentinels for human exposure to PAHs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Benzo(a)pyrene
- Dogs
- Cats
- Semipersistent organic pollutants
- Sentinels
- Carcinogenic chemicals
- Polycyclic aromatic hydrocarbons
- Pets
- Sentinel
- Biomonitoring
1 Introduction
Polycyclic aromatic hydrocarbons or polynuclear aromatic hydrocarbons (PAHs) are a large class of organic compounds (more than a hundred are known) made from carbon and hydrogen, formed by more than two benzene rings fused and organised on linear, angular or cluster structure. According to their molecular weight, they can be classified as low-molecular-weight PAHs (LMW-PAHs, up to three fused rings) or as high-molecular-weight PAHs (HMW-PAHs, minimum of four rings).
Generally, they are colourless, white or yellowish solid at room temperature; have low vapour pressure, high melting and boiling points and low water solubility; and are hence highly lipophilic (WHO 1998). The most harmful and best-known PAH is benzo(a)pyrene (BaP) , but there are many other PAHs of concern (Fig. 4.1) because of their toxicity, human exposure, occurrence in the environment and scope of available information. According to the list of priority pollutants of the United States Environmental Protection Agency (USEPA), there are 16 priority PAHs, because of their occurrence and the fact that they are continuously emitted to the environment (ATSDR 1995). More important are those PAHs that have been identified as mutagenic/teratogenic/carcinogenic by the Joint FAO/WHO Expert Committee on Food Additives (JECFA) (Fig. 4.1). Based on data from oral bioassays conducted in mice with coal tar mixtures, the JECFA calculated margin of exposure values of 25,000 and 10,000 between the BMDL10 value of 100 μg of benzo[a]pyrene/kg bw/day and mean and 95th-percentile intake levels of 4 and 10 ng/kg bw/d, respectively.
According to their origin, PAHs can be classified as pyrolytic (high temperature), petrogenic (high pressure) or biological (synthesised by microorganisms). Besides, they can be disguised between anthropogenic (combustion of fossil fuels, principally) and natural (forest fires, volcanos, fossil fuel formation, vegetal matter decomposition) sources, although the latter have a minimal contribution to the total environment burden.
Granting that they have no utility per se, PAHs are used as intermediaries in different industries, namely, in the manufacture of pharmaceutical products, polyvinyl chloride (PVC) and plasticisers (naphthalene), pigments (acenaphthene, pyrene), dyes (anthracene, fluoranthene) and pesticides (phenanthrene) (WHO 1998). Nevertheless, production, processing and use of fossil fuels principally coal – and, to a lesser extent, oil and natural gas – for industries, heating or transportation in cities, are the main source of emission of these contaminants to the environment (Cabuk et al. 2014; Villar-Vidal et al. 2014). Concerning traffic, petrol-fuelled vehicles can emit greater amounts of fluoranthene and pyrene, whilst diesel-fuelled vehicles emit naphthalene and acenaphthene. In the case of smoking, cooking or burning (of stubble, garbage, tyres or other types of waste), a great variety of different compounds are emitted, including the ones already mentioned.
After being formed, these hydrocarbons are dispersed in the environment according to their molecular weight and climate conditions (Kozak et al. 2003). Thus, the HMW-PAHs can be adsorbed into the organic matter of the soil, water or air, whilst the LMW-PAHs will become a part of the gas phase in the atmosphere (Li et al. 2015). Both can be transported over long distances in several weeks until they are precipitated and/or degraded by solar light or microorganisms in the soil or sediments (Walgraeve et al. 2010). Along the way, they can react with different airborne compounds, namely, sulphur oxides, nitrogen oxides or ozone, resulting in no less toxic combinations (Li et al. 2015; Walgraeve et al. 2010), like nitro-/oxy-PAHs and radicals formation.
2 Sources of Exposure and Health Effects
Humans and other living beings can be exposed to PAHs through inhalation or dermal/mucosa contact or mainly through water and food intake (Boada et al. 2016; Henriquez-Hernandez et al. 2017b; Hernandez et al. 2015, 2017; Luzardo et al. 2013a; Rodríguez-Hernández et al. 2015b, 2016, 2017). Inhalation is an important source in smokers and people who live near or in big cities or industrialised zones, where ten times higher concentrations of PAHs than in rural areas can be found (de la Gala Morales et al. 2015; Srogi 2007). Several authors have described higher concentration of PAHs in winter than in summer because of increased use of domestic heating (de la Gala Morales et al. 2015; Li et al. 2015; Villar-Vidal et al. 2014).
It has also been described that dermal exposure may be relevant, mainly when prolonged or continued contact with products made of petroleum derivatives occurs. Recently, the European Union, through the REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals) regulation, established new restrictions about PAHs in several day-to-day stuffs made of plastics or rubber, which are in direct, prolonged or short-term repetitive contact with human skin or mucosa. These items should not contain more than 10 mg/kg of the sum of benzo(a)pyrene (BaP), benzo(e)pyrene, benzo(a)anthracene, chrysene, benzo(b)fluoranthene, benzo(j)fluoranthene, benzo(k)fluoranthene and dibenzo(a,h)anthracene, or no more than 1 mg/kg of BaP alone (ECHA 2017).
Although parental PAHs are generally inert, once in the organism, PAHs can be metabolised to be eliminated, generally via urine (LMW-PAHs) or faeces (HMW-PAHs). By the way, the process may result in active PAH metabolites (m-PAHs) capable of forming adducts with the DNA (Boada et al. 2016; Ramesh et al. 2004; Rodríguez-Hernández et al. 2015a, Hernandez et al. 2017). The biotransformation process is carried out through a series of enzymes like cytochrome P-450, which catalyses mainly oxidation, reduction and hydrolysis reactions. In vertebrates, the liver is the major contributor in the biotransformation process. However, in other organs there are cytochromes, which are able to perform this function according to the entryway (i.e. lungs, intestine or skin) (Ramesh et al. 2004). In addition, conjugation enzymes such as sulphotransferases, epoxide hydrolase, glutathione transferase and UDP-glycosyltransferase can metabolise PAHs, producing a variety of phenols, catechols, quinones and radical cations. Once they are formed, these compounds may produce adverse effects by means of various mechanisms, such as DNA damage diol-epoxides (that give place to formation of adducts), interaction with membranes and oxidative stress (Li et al. 2015; Sikkema et al. 1994; Zhang et al. 2016). Given that, some PAHs are described as carcinogenic (c-PAHs), namely, human carcinogen BaP (Group 1), whilst others are considered as probably (Group 2A) or possibly carcinogenic (Group 2B) by the International Agency for Research on Cancer (IARC 2005). All these compounds have been described as contributing causes of breast, bladder, lung, skin or gastrointestinal cancers (Alicandro et al. 2016; Boada et al. 2015, 2016; Flesher and Lehner 2016; Korsh et al. 2015).
Often mixtures of hydrocarbons and/or their derivatives (such as nitro-PAH) are more harmful, due in part to synergistic properties. In general terms, the lower the molecular weight, the lower the carcinogenicity potential, but they are more prone to cause acute health effects, such as cardiovascular diseases (thrombosis, haematopoietic effects), dyspnoea, asthma (Al-Daghri et al. 2014), diarrhoea, vomiting, nausea and eye, dermal or bronchial irritation or inflammation (Ramesh et al. 2004). Moreover, it is well known that some PAHs are endocrine disruptors in animals and humans. Neurological, congenital and development problems in the offspring and mothers (Jedrychowski et al. 2013; Neal et al. 2008; Oliveira et al. 2017) or immunosuppressant effects (Bolden et al. 2017; Ramesh et al. 2004) have been reported.
3 Biomonitoring of Polycyclic Aromatic Hydrocarbons
Given the toxicity and environmental prevalence of these compounds, the monitoring of PAHs is a relevant issue, and there is plenty of interest in control and assessment of these substances in food, environmental compartments, living beings and of course humans. Environmental monitoring of these substances is achieved by sampling and analysing samples such as air, water, food or soil (Bucchia et al. 2015; de la Gala Morales et al. 2015; García-Álvarez et al. 2014b; Hernandez et al. 2015; Kakuschke et al. 2010). Specifically, biomonitoring – the monitoring of these compounds in living beings – is usually considered the best approach as it provides a real picture of the exposure of living beings, meaning that it provides an assessment of the whole uptake through all exposure routes (Srogi 2007).
The biomonitoring of human populations may be done either by direct measurement in samples taken from study populations or extrapolating the data from the environmental exposure of other organisms (bioindicators or sentinels). This biomonitoring can be done by directly determining the individual PAHs and/or their metabolites, as well as by determining biomarkers of the effect they produce. In the case of PAHs, it is common to determine the presence of adducts of PAHs with DNA, or the detection of tetrahydroxy-PAHs that can also be measured as an indicator of tissue damage.
For reasons of practicality and ease of collection of samples, it is often considered that urinary metabolites of PAHs are better bioindicators of exposure, being considered the gold standard to determine recent exposure to a single PAH, in particular when multiple routes of exposure have to be taken into account (Jacob and Seidel 2002) or in occupational meaning (Unwin et al. 2006). The main m-PAHs that should be included in biomonitoring studies are 1-hydroxynaphthalene (1-napthol), 2-hydroxynaphthalene (2-naphthol), 1,2-dihydroxynaphthalene, 2-hydroxyfluorene (2-FLUO), 3-hydroxyfluorene (3-FLUO), 9-hydroxyfluorene (9-FLUO), 1-hydroxyphenanthrene, 2-hydroxyphenanthrene, 3-hydroxyphenanthrene, 4-hydroxyphenanthrene, 9-hydroxyphenanthrene, 1-hydroxypyrene (1-PYR) and 3-hydroxybenzo(a)pyrene (3-OHBaP) (Wang et al. 2014a, b). 1-PYR has been linked to dietary exposures, whilst both 1-PYR and 2-naphthol are well correlated with smoking in a non-occupational population (Nethery et al. 2012; Srogi 2007). Urinary 3-OHBaP may be a suitable biomarker to assess BaP genotoxic exposure in humans (Marie-Desvergne et al. 2010; Oliveira et al. 2017). One decisive factor to take into account when determining urinary metabolites is sampling time, due to the high rate of biotransformation of these compounds (Cathey et al. 2018; Grova et al. 2017a, b). Taken together, those results suggest that it is better to use a combination of metabolites, since each metabolite gives an information about a single or few parental PAHs (Castano-Vinyals et al. 2004; Grova et al. 2017b; Hilton et al. 2017; Singh et al. 2008).
Other excretion routes, such as nails, hair, sweat or feathers, amongst others, have been also investigated regarding their content in m-PAHs, as a means of determining long-term exposure to these substances. In fact, some authors have pointed out that these matrices are more appropriate for the determination of HMW-PAHs (Grova et al. 2017b; Marie-Desvergne et al. 2010).
On the other hand, not only for assessing exposure but also the toxicological effect of PAHs, some other authors prefer to determine the amount of PAHs-DNA adducts in peripheral white blood cells, or their binding to plasmatic proteins, especially in occupational studies (Oliveira et al. 2017; Pleil et al. 2010). Other authors correlate the level of oxidative stress induced by PAHs as an indirect indicator of the carcinogenicity of these compounds (Singh et al. 2008). However, these studies of biomarkers have the disadvantage in that the analytical techniques are complex, have low sensitivity and do not allow deriving the global exposure to these compounds.
Finally, some authors consider that the direct measurement of PAHs in blood is the best way to estimate the total body burden and also the most realistic way to estimate exposure (Boada et al. 2015; Pleil et al. 2010). It has the disadvantage in that sampling is invasive, especially taking into account that WHO recommends that biomonitoring studies include mainly children, because it has been estimated that children aged 6–11 are the sector of the population most exposed to these compounds (Singh et al. 2013). In addition, and as we said before, it is possible to evaluate human exposure to PAHs indirectly, using bioindicator species. In these cases also blood is often the easiest sample to take, so comparison with human levels is simpler (Boada et al. 2015; Bucchia et al. 2015; Camacho et al. 2012b, 2014; Camacho et al. 2013b; García-Álvarez et al. 2014a, b; Luzardo et al. 2014).
In this sense, studies of the effects of environmental exposures on vegetables or animals can corroborate or support epidemiological studies in humans or in the environment. In these cases, the levels determined in these easy-to-sample species may reflect the exposure of a group of environmentally related species, rather than the individual exposure. Thus, the use of microbial bioindicators in order to evaluate contamination of some PAHs in agricultural soils (Niepceron et al. 2013) and in the gas and aqueous phases (Cho et al. 2014) has been reported. In the same way, moss, lichens and plants have been used as passive phytomonitors instead of the active samplers and several studies have found promising results. In wildlife, some authors have proposed different species as possible sentinels of exposure. Some invertebrates have been studied. Amphipod (Talitrus saltator) appears to be a good bioindicator of this class of organic compounds in supralittoral zone (Ugolini et al. 2012). The possibility that molluscs are good bioindicators of the contamination of PAHs from the waters or sediments in mudflats of Malaysia (Tavakoly Sany et al. 2014) and mangrove oysters (Crassostrea rhizophorae) (Ramdine et al. 2012) has also been reported. Studies on oil spills such as those occurring on the northern Cantabrian sea and in Guanabara Bay, Brazil, respectively, concluded that barnacles are good indicators for oil spill evolution (Soares-Gomes et al. 2010; Vinas et al. 2009). Other species in the highest levels of the food chain have also been described as efficient indicators of recent pollution. Fuentes-Rios et al. (2005) determined that the cat shark is a good bioindicator for exposure to PAHs on the Chilean Pacific coast, showing good correlation with the concentration of pyrene in water and urinary 1-PYR. On Atlantic eastern coast and Mediterranean sea, several authors (Bucchia et al. 2015; Camacho et al. 2012a, 2013a, 2014, García-Álvarez et al. 2014a) investigated serum levels of PAHs in different populations of sea turtles (Caretta caretta) and bottlenose dolphins (Tursiops truncata) indicating that both species could be good indicators of local and recent pollution in the marine environment.
Since the iconic ‘canary in the cage’ began to be used to detect the presence of toxic gases in the coal mines, pets and other animals in the human immediate environment have been used as sentinels of human exposure to many other chemical classes. In this case, they were used as an early warning system, since the canary is more sensitive to carbon monoxide poisoning than humans and other domestic animals like cats, dogs, pigeons or rabbits. Livestock, including bees, cattle, horses, sheep and goats, can be good bioindicators for outdoor air, whilst pet cats and dogs can share the indoor air, water, food or even household dust. However, daily routine and diet, especially in people who are occupationally exposed, smokers or on some kind of diets, are confounding factors. The different metabolism and elimination capacity amongst the species should be also taken into account as confounding factors.
4 Pet Dogs as Sentinels forHuman Exposure to PAHs
Pet dogs are particularly interesting as sentinels for human exposure to PAH, given that they share the habitat with humans and they respond to toxic assaults similarly than their owners (Backer et al. 2001). As far as we know, there is only one research article that has assessed exposure to PAHs in dogs and humans to date (Ruiz-Suárez et al. 2016). In this study, the authors included blood samples from 87 pet dogs (46 males and 41 females, 0.5–13 years old) visiting the veterinary hospital of the Faculty of Veterinary Medicine of the University of Las Palmas de Gran Canaria (Canary Islands, Spain) for routine care. Only clinically normal animals (negative stool sample, negative result on a heartworm test and no overt disease) were included in the study, after owners’ consent. In parallel, human blood samples from 60 males and 40 females (19–34 years old) were collected from a blood bank during the same period that dogs’ samples were drawn. For logistical reasons the researchers could not get blood from the owners of the same dogs included in the study. Even so it has been estimated that there are about six million domestic dogs in Spain and that more than 40% of Spanish homes have at least one dog, so the authors assumed that a high percentage of these blood donors share habitat with some dog.
In this research work the authors determined 21 PAHs, including the 13 c-PAHs and also 6 common m-PAHs (Table 4.1), by means of solid phase extraction and gas chromatography coupled to tandem triple-quadrupole mass spectrometry. In this research the authors detected the totality of the PAHs and m-PAHs in any of the samples, both in humans and dogs, with the only exception of benzo(a)pyrene, which was not detected in none of the dog plasma samples.
The compounds most frequently detected in both species were phenanthrene, fluorene and fluoranthene and 2-naphthol, which were present in nearly 100% of the samples. The frequencies of detection of the rest of the compounds of this chemical group were highly variable and different between the two species (Table 4.1). The mean values of ∑PAH21 were much lower in dogs than in humans (782.2 vs. 1623.3 ng/g lw, respectively). Regarding the c-PAHs, the authors considered only seven compounds (PAH7, benzo(a)anthracene, chrysene, benzo(a)pyrene, benzo(b)fluoranthene, benzo(k)fluoranthene, dibenzo(a,h)anthracene and indeno(1,2,3-c,d)pyrene), and the mean values were also much lower in dogs than in humans (6.8 vs. 21.9 ng/g lw, respectively). On the opposite, according to the authors’ results, it seems that dogs may have a higher capacity of biotransformation of these compounds, because in parallel to the lower levels of untransformed PAHs, dogs also had higher levels of PAHs metabolites than humans, in whom the relationship was inverse (∑m-PAH = 198.1 and 131.6 ng/g lw in dogs and humans, respectively; p < 0.0001).
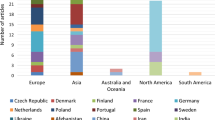
The importance of the employment of sentinel species for the assessment of human exposure to chemicals has been widely demonstrated for many chemical classes, since the sentinel species may reflect the actual human exposure of a given population, much more accurately than the comparison to other remote populations. However, it does not seem to be the case of pet dogs as sentinels of human exposure to PAHs, because the authors of the only study available in this regard found that there were many significant differences between these two species (Fig. 4.2), both in the levels of many parental compounds and in their metabolites. These results suggest that exposure of both species to this contaminant group could be different, but also may be indicating that dogs have a higher capacity to metabolise these compounds than humans. Obviously, to confirm this point, additional research is needed, but these results allowed the authors to hypothesise that the lower levels of PAHs detected in the plasma of dogs could be due to a higher rate of biotransformation and elimination thereof. Furthermore, as shown in Fig. 4.2c, neither the profiles of PAHs contamination were similar between dogs and humans, with a clear predominance of the four-ring compounds in humans and three-ring compounds in dogs. In fact, it is noteworthy that some compounds such as pyrene, which was detected in almost 100% of the human samples, were barely detectable in 17% of samples from dogs, and yet, others such as acenaphthylene or 1-naphthol were much more frequently detected in dog plasma than in human plasma. Thus, in the light of the above, the authors concluded that the pet dogs do not seem to be good sentinels for human exposure to PAHs.
Levels of PAHs in plasma samples. (a) (main body). Box plots of ∑PAH21 in dogs and humans. (a) (inset). Bar graph of ∑PAH7 (carcinogenic PAHs, median and interquartile range) in dogs and humans. (b) Box plots of ∑PAH metabolites in dog and humans. (c) Profile of distribution of PAHs in dogs and humans. The line inside the boxes represents the median, the bottom and top of the boxes are the first and third quartiles of the distribution, and the lines extending vertically from the boxes indicate the variability outside the upper and lower quartiles. (d) profile of contamination by pAHs in humans and dogs
5 Pet Cats as Sentinels for Human Exposure to PAHs
As far as we know, there is no published study that explored the role of domestic cats as sentinels of human exposure to PAHs. However, the cat that lives inside the house is usually considered a good bioindicator, even better than the dog, to assess the exposure of man to the contaminants present in the domestic environment. This is mainly due to their grooming habits, which cause cats to ingest high amounts of household dust, with all the load of contaminants associated with it. Thus, in different publications, it has been indicated that this pet is ideal for evaluating human exposure to different kinds of contaminants. (Bost et al. 2016; Chow et al. 2015; Dirtu et al. 2013; Henriquez-Hernandez et al. 2017a). In addition, other studies have shown that dietary exposure to different contaminants (including PAHs) is different between dogs and cats (Ruiz-Suarez et al. 2015), so although, as we said earlier, dogs do not seem to be good sentinels of human exposure to PAHs, cats present differential facts that could make them suitable for this purpose, so this possibility is worth investigating.
With the purpose of completing the information in this chapter, we decided to shed light on the question whether or not cats would be good sentinels of human exposure to PAHs. For this, we collected venous blood from a total of 25 cats that were recently admitted for routine health check-ups and vaccination in the clinical hospital of the Faculty of Veterinary Medicine of the University of Las Palmas de Gran Canaria. In parallel, blood was collected from 25 volunteers from the same faculty, from amongst the staff and the students of the same, all of them owners of cats (although not from the same cats participating in the study). The serum was obtained, and the PAHs were extracted by solid phase extraction following the procedure described elsewhere (Camacho et al. 2012a). In this work, we included only the 16 priority PAHs for the USEPA, whose analysis was performed by gas chromatography coupled to tandem triple-quadrupole mass spectrometry (Luzardo et al. 2013b). All human volunteers and cat owners provided their written informed consent to participate in this study.
We found only 8 out of the 16 compounds analysed both in humans and cats. In addition, acenaphthylene was also detected in cats, but not in humans. The summary of the results of this study is shown in Table 4.2. As it can be seen, the most frequently detected compounds were acenaphthene, phenanthrene and fluorene, with frequencies of 90% or more in both species. For the rest of the substances, the detection percentage between both species was highly variable. We want to highlight the differences found between cats and humans for chrysene and fluoranthene (percentages of detection of 18.2 vs. 90% and 31.3 vs. 100%, respectively). The median of the ∑16PAHs was similar in both species (1.93 vs. 2.08 ng/mL or 232 vs. 257 ng/g lw, respectively). However, although the total concentrations do not show significant differences between both species, when we focus on carcinogenic compounds for EFSA, the outlook changes radically, since these compounds were practically undetectable in the group of cats, whilst they were present in the group of cat owners (Fig. 4.3). Obviously, this is only a preliminary study, and the conclusions that derive from it should be taken with caution because of the low sample size. However, based on the results obtained, it could not be considered that the cat is the ideal sentinel to assess human exposure to PAHs, although it does seem to be better than dogs in this sense.
Box plot showing the serum levels of sum of all PAHs (panel A) and sum of PAHs 4 (panel B), amongst cats (n = 22) and humans (n = 20). Sum PAHs included all the 16 congeners analysed. Sum of PAHs 4 included only benzo(a)pyrene, benz(a)anthracene, benzo(b)fluoranthene and chrysene. P values were calculated with Mann-Whitney U test. The lines connect the medians, the boxes cover the 25th to 75th percentiles, and the minimal and maximal values are shown by the ends of the bars. Abbreviations: ns, non-significant. ∗∗, p = 0.003
6 Conclusions
Based on the scarce existing bibliography and limitations of the study, it can be concluded that pet dogs and cats are not good sentinels of human exposure to PAHs. The analyses of parental compounds and metabolites in serum and their concentrations and contamination profiles are not comparable between species. These results could indicate that different sources of exposure, such as smoking, occupational setting or food intake, in humans exist. In the analysis of PAH metabolites, higher levels in dogs suggest that they metabolise them more effectively than humans. Despite sharing a home and in some cases diet with humans, pets differ greatly from humans to consider them good sentinels for PAHs exposure.
References
Al-Daghri NM, Alokail MS, Abd-Alrahman SH, Draz HM (2014) Polycyclic aromatic hydrocarbon distribution in serum of Saudi children using HPLC-FLD: marker elevations in children with asthma. Environ Sci Pollut Res Int 21:12085–12090
Alicandro G, Rota M, Boffetta P, La Vecchia C (2016) Occupational exposure to polycyclic aromatic hydrocarbons and lymphatic and hematopoietic neoplasms: a systematic review and meta-analysis of cohort studies. Arch Toxicol 90:2643–2656
ATSDR (1995) Toxicological profile for polycyclic aromatic hydrocarbons (PAHs). Toxic Substances Portal 24 Feb 2018. ATSDR, USA
Backer LC, Grindem CB, Corbett WT, Cullins L, Hunter JL (2001) Pet dogs as sentinels for environmental contamination. Sci Total Environ 274:161–169
Boada LD, Henriquez-Hernandez LA, Navarro P, Zumbado M, Almeida-Gonzalez M, Camacho M et al (2015) Exposure to polycyclic aromatic hydrocarbons (PAHs) and bladder cancer: evaluation from a gene-environment perspective in a hospital-based case-control study in the Canary Islands (Spain). Int J Occup Environ Health 21:23–30
Boada LD, Henriquez-Hernandez LA, Luzardo OP (2016) The impact of red and processed meat consumption on cancer and other health outcomes: epidemiological evidences. Food Chem Toxicol 92:236–244
Bolden AL, Rochester JR, Schultz K, Kwiatkowski CF (2017) Polycyclic aromatic hydrocarbons and female reproductive health: a scoping review. Reprod Toxicol 73:61–74
Bost PC, Strynar MJ, Reiner JL, Zweigenbaum JA, Secoura PL, Lindstrom AB et al (2016) U.S. domestic cats as sentinels for perfluoroalkyl substances: possible linkages with housing, obesity, and disease. Environ Res 151:145–153
Bucchia M, Camacho M, Santos MR, Boada LD, Roncada P, Mateo R et al (2015) Plasma levels of pollutants are much higher in loggerhead turtle populations from the Adriatic Sea than in those from open waters (Eastern Atlantic Ocean). Sci Total Environ 523:161–169
Cabuk H, Kilic MS, Oren M (2014) Biomonitoring of polycyclic aromatic hydrocarbons in urban and industrial environments of the Western Black Sea region, Turkey. Environ Monit Assess 186:1515–1524
Camacho M, Boada LD, Oros J, Calabuig P, Zumbado M, Luzardo OP (2012a) Comparative study of polycyclic aromatic hydrocarbons (PAHs) in plasma of Eastern Atlantic juvenile and adult nesting loggerhead sea turtles (Caretta caretta). Mar Pollut Bull 64:1974–1980
Camacho M, Boada LD, Orós J, Calabuig P, Zumbado M, Luzardo OP (2012b) Comparative study of polycyclic aromatic hydrocarbons (PAHs) in plasma of Eastern Atlantic juvenile and adult nesting loggerhead sea turtles (Caretta caretta). Mar Pollut Bull 64:1974–1980
Camacho M, Calabuig P, Luzardo OP, Boada LD, Zumbado M, Oros J (2013a) Crude oil as a stranding cause among loggerhead sea turtles (Caretta caretta) in the Canary Islands, Spain (1998-2011). J Wildl Dis 49:637–640
Camacho M, Luzardo OP, Boada LD, Lopez Jurado LF, Medina M, Zumbado M et al (2013b) Potential adverse health effects of persistent organic pollutants on sea turtles: evidences from a cross-sectional study on Cape Verde loggerhead sea turtles. Sci Total Environ 458-460C:283–289
Camacho M, Boada LD, Oros J, Lopez P, Zumbado M, Almeida-Gonzalez M et al (2014) Monitoring organic and inorganic pollutants in juvenile live sea turtles: results from a study of Chelonia mydas and Eretmochelys imbricata in Cape Verde. Sci Total Environ 481C:303–310
Castano-Vinyals G, D’Errico A, Malats N, Kogevinas M (2004) Biomarkers of exposure to polycyclic aromatic hydrocarbons from environmental air pollution. Occup Environ Med 61:e12
Cathey A, Ferguson KK, McElrath TF, Cantonwine DE, Pace G, Alshawabkeh A et al (2018) Distribution and predictors of urinary polycyclic aromatic hydrocarbon metabolites in two pregnancy cohort studies. Environ Pollut 232:556–562
Cho JH, Lee DY, Lim WK, Shin HJ (2014) A recombinant Escherichia coli biosensor for detecting polycyclic aromatic hydrocarbons in gas and aqueous phases. Prep Biochem Biotechnol 44:849–860
Chow K, Hearn LK, Zuber M, Beatty JA, Mueller JF, Barrs VR (2015) Evaluation of polybrominated diphenyl ethers (PBDEs) in matched cat sera and house dust samples: investigation of a potential link between PBDEs and spontaneous feline hyperthyroidism. Environ Res 136:173–179
de la Gala Morales M, Holgado FR, Marin MR, Blazquez LC, Gil EP (2015) Ambient air levels and health risk assessment of benzo(a)pyrene in atmospheric particulate matter samples from low-polluted areas: application of an optimized microwave extraction and HPLC-FL methodology. Environ Sci Pollut Res Int 22:5340–5349
Dirtu AC, Niessen SJ, Jorens PG, Covaci A (2013) Organohalogenated contaminants in domestic cats’ plasma in relation to spontaneous acromegaly and type 2 diabetes mellitus: a clue for endocrine disruption in humans? Environ Int 57-58:60–67
ECHA (2017) Draft guideline on the scope of restriction entry 50 of annex XV to REACH: polycyclic organic hydrocarbons in articles supplied to the general public. ECHA documents. European Chemicals Agency, Finland
EPA. United States Environmental Protection Agency, Office of Enviromental Information, Emergency planning and community right-to-know act - Section 313: Guidance for reporting toxic chemicals: polycyclic aromatic compounds category. EPA.260-B-01-03. 2001.
Flesher JW, Lehner AF (2016) Structure, function and carcinogenicity of metabolites of methylated and non-methylated polycyclic aromatic hydrocarbons: a comprehensive review. Toxicol Mech Methods 26:151–179
Fuentes-Rios D, Orrego R, Rudolph A, Mendoza G, Gavilan JF, Barra R (2005) EROD activity and biliary fluorescence in Schroederichthys chilensis (Guichenot 1848): biomarkers of PAH exposure in coastal environments of the South Pacific Ocean. Chemosphere 61:192–199
García-Álvarez N, Boada LD, Fernández A, Zumbado M, Arbelo M, Sierra E et al (2014a) Assessment of the levels of polycyclic aromatic hydrocarbons and organochlorine contaminants in bottlenose dolphins (Tursiops truncatus) from the Eastern Atlantic Ocean. Mar Environ Res 100:48–56
García-Álvarez N, Martín V, Fernández A, Almunia J, Xuriach A, Arbelo M et al (2014b) Levels and profiles of POPs (organochlorine pesticides, PCBs, and PAHs) in free-ranging common bottlenose dolphins of the Canary Islands, Spain. Sci Total Environ 493:22–31
Grova N, Antignac JP, Hardy EM, Monteau F, Pouponneau K, Le Bizec B et al (2017a) Identification of new tetrahydroxylated metabolites of Polycyclic Aromatic Hydrocarbons in hair as biomarkers of exposure and signature of DNA adduct levels. Anal Chim Acta 995:65–76
Grova N, Fays F, Hardy EM, Appenzeller BMR (2017b) New insights into urine-based assessment of polycyclic aromatic hydrocarbon-exposure from a rat model: identification of relevant metabolites and influence of elimination kinetics. Environ Pollut 228:484–495
Henriquez-Hernandez LA, Carreton E, Camacho M, Montoya-Alonso JA, Boada LD, Bernal Martin V et al (2017a) Potential role of pet cats as a sentinel species for human exposure to flame retardants. Front Vet Sci 4:79
Henriquez-Hernandez LA, Montero D, Camacho M, Gines R, Boada LD, Ramirez Bordon B et al (2017b) Comparative analysis of selected semi-persistent and emerging pollutants in wild-caught fish and aquaculture associated fish using Bogue (Boops boops) as sentinel species. Sci Total Environ 581-582:199–208
Hernandez AR, Boada LD, Almeida-Gonzalez M, Mendoza Z, Ruiz-Suarez N, Valeron PF et al (2015) An estimation of the carcinogenic risk associated with the intake of multiple relevant carcinogens found in meat and charcuterie products. Sci Total Environ 514:33–41
Hernández AR, Boada LD, Mendoza Z, Ruiz-Suárez N, Valerón PF, Camacho M et al (2017) Consumption of organic meat does not diminish the carcinogenic potential associated with the intake of persistent organic pollutants (POPs). Environ Sci Pollut Res Int 24:4261–4273
Hilton DC, Trinidad DA, Hubbard K, Li Z, Sjodin A (2017) Measurement of urinary Benzo[a]pyrene tetrols and their relationship to other polycyclic aromatic hydrocarbon metabolites and cotinine in humans. Chemosphere 189:365–372
IARC (2005) Some non-heterocyclic polycyclic aromatic hydrocarbons and some related exposures, IARC monographs on the evaluation of carcinogenic risks to humans, vol 92. World Health Organization – International Agency for Research on Cancer, Lyon, France
Jacob J, Seidel A (2002) Biomonitoring of polycyclic aromatic hydrocarbons in human urine. J Chromatogr B Analyt Technol Biomed Life Sci 778:31–47
Jedrychowski WA, Perera FP, Tang D, Rauh V, Majewska R, Mroz E et al (2013) The relationship between prenatal exposure to airborne polycyclic aromatic hydrocarbons (PAHs) and PAH-DNA adducts in cord blood. J Expo Sci Environ Epidemiol 23:371–377
Kakuschke A, Valentine-Thon E, Griesel S, Gandrass J, Perez Luzardo O, Dominguez Boada L et al (2010) First health and pollution study on harbor seals (Phoca vitulina) living in the German Elbe estuary. Mar Pollut Bull 60:2079–2086
Korsh J, Shen A, Aliano K, Davenport T (2015) Polycyclic aromatic hydrocarbons and breast cancer: a review of the literature. Breast Care (Basel) 10:316–318
Kozak IO, Kozak M, Fekete J, Sharma VK (2003) Concentration of polycyclic aromatic hydrocarbons (PAHs) in moss (Hypnum cupressiforme) from Hungary. J Environ Sci Health A Tox Hazard Subst Environ Eng 38:2613–2619
Li W, Wang C, Shen H, Su S, Shen G, Huang Y et al (2015) Concentrations and origins of nitro-polycyclic aromatic hydrocarbons and oxy-polycyclic aromatic hydrocarbons in ambient air in urban and rural areas in northern China. Environ Pollut 197:156–164
Luzardo OP, Rodríguez-Hernández A, Quesada-Tacoronte Y, Ruiz-Suárez N, Almeida-González M, Henríquez-Hernández LA et al (2013a) Influence of the method of production of eggs on the daily intake of polycyclic aromatic hydrocarbons and organochlorine contaminants: an independent study in the Canary Islands (Spain). Food Chem Toxicol 60:455–462
Luzardo OP, Ruiz-Suarez N, Almeida-Gonzalez M, Henriquez-Hernandez LA, Zumbado M, Boada LD (2013b) Multi-residue method for the determination of 57 persistent organic pollutants in human milk and colostrum using a QuEChERS-based extraction procedure. Anal Bioanal Chem 405:9523–9536
Luzardo OP, Ruiz-Suárez N, Henríquez-Hernández LA, Valerón PF, Camacho M, Zumbado M et al (2014) Assessment of the exposure to organochlorine pesticides, PCBs and PAHs in six species of predatory birds of the Canary Islands, Spain. Sci Total Environ 472:146–153
Marie-Desvergne C, Maitre A, Bouchard M, Ravanat JL, Viau C (2010) Evaluation of DNA adducts, DNA and RNA oxidative lesions, and 3-hydroxybenzo(a)pyrene as biomarkers of DNA damage in lung following intravenous injection of the parent compound in rats. Chem Res Toxicol 23:1207–1214
Neal MS, Zhu J, Foster WG (2008) Quantification of benzo[a]pyrene and other PAHs in the serum and follicular fluid of smokers versus non-smokers. Reprod Toxicol 25:100–106
Nethery E, Wheeler AJ, Fisher M, Sjodin A, Li Z, Romanoff LC et al (2012) Urinary polycyclic aromatic hydrocarbons as a biomarker of exposure to PAHs in air: a pilot study among pregnant women. J Expo Sci Environ Epidemiol 22:70–81
Niepceron M, Martin-Laurent F, Crampon M, Portet-Koltalo F, Akpa-Vinceslas M, Legras M et al (2013) GammaProteobacteria as a potential bioindicator of a multiple contamination by polycyclic aromatic hydrocarbons (PAHs) in agricultural soils. Environ Pollut 180:199–205
Oliveira M, Slezakova K, Alves MJ, Fernandes A, Teixeira JP, Delerue-Matos C et al (2017) Polycyclic aromatic hydrocarbons at fire stations: firefighters’ exposure monitoring and biomonitoring, and assessment of the contribution to total internal dose. J Hazard Mater 323:184–194
Pleil JD, Stiegel MA, Sobus JR, Tabucchi S, Ghio AJ, Madden MC (2010) Cumulative exposure assessment for trace-level polycyclic aromatic hydrocarbons (PAHs) using human blood and plasma analysis. J Chromatogr B Analyt Technol Biomed Life Sci 878:1753–1760
Ramdine G, Fichet D, Louis M, Lemoine S (2012) Polycyclic aromatic hydrocarbons (PAHs) in surface sediment and oysters (Crassostrea rhizophorae) from mangrove of Guadeloupe: levels, bioavailability, and effects. Ecotoxicol Environ Saf 79:80–89
Ramesh A, Walker SA, Hood DB, Guillen MD, Schneider K, Weyand EH (2004) Bioavailability and risk assessment of orally ingested polycyclic aromatic hydrocarbons. Int J Toxicol 23:301–333
Rodríguez-Hernández A, Boada LD, Almeida-González M, Mendoza Z, Ruiz-Suárez N, Valerón PF et al (2015a) An estimation of the carcinogenic risk associated with the intake of multiple relevant carcinogens found in meat and charcuterie products. Sci Total Environ 514:33–41
Rodríguez-Hernández A, Camacho M, Boada LD, Ruiz-Suárez N, Almeida-González M, Henríquez-Hernández LA et al (2015b) Daily intake of anthropogenic pollutants through yogurt consumption in the Spanish population. J Appl Anim Res 43:373–383
Rodriguez-Hernandez A, Camacho M, Henriquez-Hernandez LA, Boada LD, Ruiz-Suarez N, Valeron PF et al (2016) Assessment of human health hazards associated with the dietary exposure to organic and inorganic contaminants through the consumption of fishery products in Spain. Sci Total Environ 557-558:808–818
Rodríguez-Hernández A, Camacho M, Henriquez-Hernandez LA, Boada LD, Valeron PF, Zaccaroni A et al (2017) Comparative study of the intake of toxic persistent and semi persistent pollutants through the consumption of fish and seafood from two modes of production (wild-caught and farmed). Sci Total Environ 575:919–931
Ruiz-Suarez N, Camacho M, Boada LD, Henriquez-Hernandez LA, Rial C, Valeron PF et al (2015) The assessment of daily dietary intake reveals the existence of a different pattern of bioaccumulation of chlorinated pollutants between domestic dogs and cats. Sci Total Environ 530-531:45–52
Ruiz-Suárez N, Rial C, Boada LD, Henríquez-Hernández LA, Valeron PF, Camacho M et al (2016) Are pet dogs good sentinels of human exposure to environmental polycyclic aromatic hydrocarbons, organochlorine pesticides and polychlorinated biphenyls? J Appl Anim Res 44:143–155
Sikkema J, de Bont JA, Poolman B (1994) Interactions of cyclic hydrocarbons with biological membranes. J Biol Chem 269:8022–8028
Singh VK, Patel DK, Ram S, Mathur N, Siddiqui MK, Behari JR (2008) Blood levels of polycyclic aromatic hydrocarbons in children of Lucknow, India. Arch Environ Contam Toxicol 54:348–354
Singh SP, Aggarwal AD, Oberoi SS, Aggarwal KK, Thind AS, Bhullar DS et al (2013) Study of poisoning trends in north India--a perspective in relation to world statistics. J Forensic Legal Med 20:14–18
Soares-Gomes A, Neves RL, Aucelio R, Van Der Ven PH, Pitombo FB, Mendes CL et al (2010) Changes and variations of polycyclic aromatic hydrocarbon concentrations in fish, barnacles and crabs following an oil spill in a mangrove of Guanabara Bay, Southeast Brazil. Mar Pollut Bull 60:1359–1363
Srogi K (2007) Monitoring of environmental exposure to polycyclic aromatic hydrocarbons: a review. Environ Chem Lett 5:169–195
Tavakoly Sany SB, Hashim R, Rezayi M, Salleh A, Rahman MA, Safari O et al (2014) Human health risk of polycyclic aromatic hydrocarbons from consumption of blood cockle and exposure to contaminated sediments and water along the Klang Strait, Malaysia. Mar Pollut Bull 84:268–279
Ugolini A, Perra G, Focardi S, Somigli S, Martellini T, Cincinelli A (2012) Sandhopper Talitrus saltator (Montagu) as a bioindicator of contamination by polycyclic aromatic hydrocarbons. Bull Environ Contam Toxicol 89:1272–1276
Unwin J, Cocker J, Scobbie E, Chambers H (2006) An assessment of occupational exposure to polycyclic aromatic hydrocarbons in the UK. Ann Occup Hyg 50:395–403
Villar-Vidal M, Lertxundi A, Martinez Lopez de Dicastillo MD, Alvarez JI, Santa Marina L, Ayerdi M et al (2014) Air Polycyclic Aromatic Hydrocarbons (PAHs) associated with PM2.5 in a North Cantabric coast urban environment. Chemosphere 99:233–238
Vinas L, Franco MA, Soriano JA, Gonzalez JJ, Ortiz L, Bayona JM et al (2009) Accumulation trends of petroleum hydrocarbons in commercial shellfish from the Galician coast (NW Spain) affected by the Prestige oil spill. Chemosphere 75:534–541
Walgraeve C, Demeestere K, Dewulf J, Zimmermann R, Van Langenhove H (2010) Oxygenated polycyclic aromatic hydrocarbons in atmospheric particulate matter: molecular characterization and occurrence. Atmos Environ 44:1831–1846
Wang Y, Fan R, Dong Y, Zhang W, Sheng G, Fu J (2014a) Urinary monohydroxylated metabolites of polycyclic aromatic hydrocarbons in children living in city and rural residences in Southern China. Environ Technol 35:2973–2981
Wang Y, Zhang W, Fan R, Sheng G, Fu J (2014b) Biological monitoring of environmental exposure to polycyclic aromatic hydrocarbons in subjects living in the area of recycling electronic garbage, in Southern China. Environ Sci Pollut Res Int 21:9161–9168
WHO (1998) Selected non-heterocyclic polycyclic aromatic hydrocarbons. World Health Organization & International Programme on Chemical Safety. World Health Organization, Geneva
Zhang Y, Dong S, Wang H, Tao S, Kiyama R (2016) Biological impact of environmental polycyclic aromatic hydrocarbons (ePAHs) as endocrine disruptors. Environ Pollut 213:809–824
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rial-Berriel, C., Henríquez-Hernández, L.A., Luzardo, O.P. (2020). Role of Pet Dogs and Cats as Sentinels of Human Exposure to Polycyclic Aromatic Hydrocarbons. In: Pastorinho, M., Sousa, A. (eds) Pets as Sentinels, Forecasters and Promoters of Human Health. Springer, Cham. https://doi.org/10.1007/978-3-030-30734-9_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-30734-9_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-30733-2
Online ISBN: 978-3-030-30734-9
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)