Abstract
What are the basic functions of the placenta?
Acknowledgments The author would like to thank Dr. İ. İlker Arıkan, Dr. Avni Ozan Tekin, Dr. Fadime Dinçer and Dr. Büşra Aynalı who contributed to this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
What are the basic functions of the placenta?
-
Transfer of gases: flow-limited passive diffusion.
-
Transport of nutrients: Principally glucose (facilitated diffusion), amino acids (active transport), fatty acids (via specific lipoprotein receptors or scavenger receptors), vitamins, and minerals.
-
Waste elimination.
-
Protection; reservoir of blood for fetus.
-
Nutritional: Provides oxygen, glucose, amino acids, and volume (liquid) transfer.
-
Immunological: Protects fetus from pathogens and maternal immune system.
-
Endocrine: Secretes human chorionic gonadotropin (hCG), Human placental lactogen (hPL), progesterone, estradiol, growth factors, cytokines, and other vasoactive mediators.
-
Metabolic: It acts as the respiratory organ and kidneys of the fetus and is responsible for the elimination of carbon dioxide, metabolic acids, and other waste products from the fetus and maintenance of acid–base balance.
How does amniotic fluid volume changes during pregnancy?
-
Normal amniotic fluid volume: gradually ↑, approximately 250 mL (16th gestational week) → 800 mL ~ 38 weeks. Then volume ↓ and after term ↓
-
All amniotic fluid renovates in term fetus at about 3 h
What are the factors contributing to amniotic fluid balance?
-
Amniotic fluid formation: Fetal urine {fluid from the fetal kidneys (hypotonic)} and lung fluid secretions
-
Amniotic fluid absorption: Fetal swallowing, amniotic–chorionic interface, and transport within the intervillous range
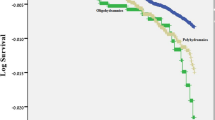
What is the definition of oligohydramnios?
-
Amniotic fluid index (AFI): 5 cm ↓ (standard definition) or 8 cm ↓ (alternative)
-
Deepest pocket <2 cm → oligohydramnios
What is the definition of polyhydramnios?
-
AFI: 25 cm ↑ (standard definition) or 18 cm ↑ (alternative)
-
Deepest pocket ˃ 8 cm → polyhydramnios
What are the fetal and maternal causes of oligohydramnios?
-
Fetal causes
-
Renal agenesis
-
Obstructive uropathy
-
PROM
-
IUGR
-
Post-term pregnancy
-
-
Maternal causes
-
Dehydration, hypovolemia
-
Hypertensive diseases
-
Uteroplacental insufficiency
-
Antiphospholipid syndrome (APS)
-
Idiopathic
-
What are the causes of the first trimester oligohydramnios?
-
Congenital heart anomalies, chromosomal aneuploidy, fetal death, and premature rupture of membranes. It may also be iatrogenic due to CVS. The reason may not be clear.
What are the causes of the second trimester oligohydramnios?
-
Congenital urinary system anomalies, preterm PROM, placental causes, amniochorionic separation, early and severe IUGR, indeterminate group (3%)
What are the causes of the third trimester Oligohydramnios?
-
Preterm PROM, IUGR, ablation placenta, fetal anomalies, iatrogenic (ACE inhibitors or prostaglandin synthesis inhibitors)
What is the incidence rate of the third trimester oligohydramnios?
-
Incidence: 3–5% (late preterm group); (5–11%) 40–42 weeks
Describe the approach to a pregnant woman with oligohydramnios.
-
The gestational week is important.
-
Fetal anatomical evaluation by ultrasound.
-
Fetal biometry is measured.
-
Examination of cervico-vaginal fluid to rule out PROM.
-
Maternal hydration.
-
Amnioinfusion (with informed consent).
-
In isolated and persistent oligohydramnios, if the maternal and fetal conditions are stable, the decision is to deliver at 36–37 weeks of gestation. Close fetal monitoring in preterm cases and betamethasone.
Describe the approach to a pregnant woman with polyhydramnios.
-
Detailed fetal anatomical examination with ultrasound
-
Fetal karyotype analysis?
-
Fetal biometry
-
Signs of fetal infection (hepatosplenomegaly, liver, and intracranial calcifications) or fetal hydrops.
-
MCA Doppler for screening fetal anemia
-
Color or power Doppler examination of the placenta (placental hemangioma)
-
Maternal DM or Pre- or gestational diabetes screening
-
If congenital anomalies and/or IUGR are detected: chromosome analysis or microarray test, serological examination for congenital infections (TORCH)
-
If fetal hydrops is detected: if it is immune etiology, indirect coombs test, TORCH serology, investigation of heart failure findings, approach for other causes
Describe the approach to isolated polyhydramnios.
-
Perinatal mortality is 3–5 times higher than normal amniotic fluid.
-
Fetal movement monitoring and weekly NST.
-
Fetal growth monitoring every 3–4 weeks.
-
AFI monitoring every 2–3 weeks.
-
<32 w: amnioreduction and Indomethacin (4×25 mg orally). >32 w: amnioreduction. After 32 gestational weeks PGI are not used concerning constriction of the ductus arteriosus.
What are the fetal causes of polyhydramnios?
-
Central nervous system: neural tube defects (anencephaly, iniencephaly, encephalocele), sacral teratoma
-
Gastrointestinal system: Esophageal atresia, diaphramatic hernia, duodenal stenosis atresia
-
Respiratory system: Cystic adenomatoid malformation of the lung, chylothorax
-
CVS: Ebstein’s anomaly, atrioventricular valve regurgitation, arrhythmias, TTTS
-
Musculoskeletal system: Skeletal dysplasias, myotonic dystrophy, Pena–Shokeir syndrome, fetal akinesia/hypokinesia syndrome. Polyhydramnios is typically caused by decreased fetal swallowing.
What are the maternal fetal complications of polyhydramnios?
-
Maternal respiratory problems
-
Preeclampsia (mirror syndrome)
-
Preterm birth
-
PPROM
-
Fetal malpresentation
-
Umbilical cord prolapse
-
Ablation placenta
-
Uterine atony
What are the properties of indomethacin used in the treatment of polyhydramnios?
-
Effective in severe symptomatic polyhydramnios
-
It acts by reducing fetal urine production (reduction in AFI in the first 24 h)
-
Used from 26–27 weeks to 32 weeks of gestation
-
25 mg per os every 6 h
-
Long admission is rare, no more than 3 days
-
Fetal echocardiography in long-term use (follow-up for duct us arteriosus closure)
-
Platelet dysfunction could occur so not to be used in cases with Placental abruption.
Which factors increase fetal cardiac output causing high fetal urine production, which is one of the contributing factors in polyhydramnios?
-
Increased urine production may occur in high fetal cardiac output states (e.g., fetal anemia due to alloimmunization, parvovirus infection, fetomaternal hemorrhage, alpha-thalassemia, hemolysis secondary to glucose-6-phosphate dehydrogenase deficiency) or, rarely, from entities such as fetal Bartter syndrome.
Which infections can cause polyhydramnios?
-
Infections that may present with hydramnios:
-
Cytomegalovirus
-
Toxoplasmosis
-
Syphilis
-
Parvovirus
-
Suggested Reading
Beloosesky R, Ross MG. Oligohydramnios. UpToDate (09 Aug 2018). https://www.uptodate.com/contents/oligohydramnios.
Ross MG, Beall MH. Physiology of amniotic fluid volume regulation. UpToDate (30 Mar 2018). https://www.uptodate.com/contents/physiology-of-amniotic-fluid-volume-regulation.
Magann E, Ross MG. Assessment of amniotic fluid volume. UpToDate (26 Apr 2018). https://www.uptodate.com/contents/assessment-of-amniotic-fluid-volume.
Beloosesky R, Ross MG. Polyhydramnios. UpToDate (16 Oct 2018). https://www.uptodate.com/contents/polyhydramnios.
Antepartum fetal surveillance. ACOG Practice Bulletin No. 145. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2014;124(1):182–92. https://doi.org/10.1097/01.AOG.0000451759.90082.7b.
Cunningham F, Leveno KJ, Bloom SL, et al. Amniotic fluid. In: Williams obstetrics. 25th ed. New York: McGraw-Hill; 2018. p. 225–34.
Beloosesky R, Ross MG, Simpson LL, Levine D, Barss VA. Polyhydramnios. UpToDate (May 2019). https://www.uptodate.com/contents/polyhydramnios.
Khan S, Donnelly J. Outcome of pregnancy in women diagnosed with idiopathic polyhydramnios. Aust N Z J Obstet Gynaecol. 2017;57:57.
Donnelly L, Campling G. Functions of the placenta. Anaesth Intensive Care Med. 2016;17:349–53. https://doi.org/10.1016/j.mpaic.2016.04.004.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sel, G. (2020). Amniotic Fluid Anomalies. In: Practical Guide to Oral Exams in Obstetrics and Gynecology . Springer, Cham. https://doi.org/10.1007/978-3-030-29669-8_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-29669-8_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-29668-1
Online ISBN: 978-3-030-29669-8
eBook Packages: MedicineMedicine (R0)