Abstract
Smart components highly integrated and miniaturized facilitate the development of wearable devices to support home monitoring of patients with chronic diseases and that should be interoperable with existing electronic health records. Objective: This study aimed to systematize current evidence of how interoperability is considered during the development of new applications to gather patients’ information in their home environments. Methods: A systematic review was performed based on a search of the literature. Results: A total of 37 articles were retrieved from the 4141 articles that result from the initial search. Conclusion: From the 4141 initial references only 81 references explicitly mentioned interoperability issues and, within these 81 references, only eight reported end-to-end solutions that can be integrated and usable in care service provision.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Background
During the last two decades, there was a considerable increase in the capacity to develop and manufacture systems that employ smart components highly integrated and miniaturized [1]. Because of this remarkable development, ubiquitous computing is nowadays part of our everyday and social life and impacts our surrounding environments.
According to the vision of Weiser [2], ubiquitous computing aims the enhancement of the computer use by bringing computing devices into everyday life (e.g. integration of computing power and sensing features into anything, including everyday objects like white goods, toys or furniture), making them available throughout the physical environment in such a way that the users would not notice their presence. In turn, ubiquitous communication comprises multiple technologies to allow the interaction among multiple devices anytime and anywhere.
Pervasive health has emerged as a specialization of eHealth and deals with the application of ubiquitous computing [3, 4] for health and wellness management, aiming to make health care more seamlessly to our everyday life [5]. Pervasive health can contribute, with different roles, to personalize health and wellness services promoting an evolution from a medical approach to individual-centric operational models, in which the individual becomes an active partner in the care process [5].
Health care services are highly mobile in nature [6] and involve multiple locations (e.g. clinics, outpatients’ services or patients’ homes), particularly when dealing with older adults and their respective major diseases [7]: cardiovascular disease, hypertension, stroke, diabetes, cancer, chronic obstructive pulmonary disease, musculoskeletal conditions, mental health conditions or visual impairment and blindness. Therefore, the pervasive health landscape includes mobile health (mHealth) application. For that smartphones are fairly robust, truly pervasive and accessible - they are accessible to over 90% of the global population [1] - and they provide ubiquitous user interfaces and have the ability to collect, store and communicate information [1]. Furthermore, an interesting feature of smartphone devices is the availability of short-distance wireless data transmission, such as Bluetooth [6]. This enables the smartphone applications to work with a wide range of hardware devices (e.g. glucose meters, pulse oximeter or thermometers) from different vendors.
Meeting the specific individual needs, namely providing care services at individuals’ home together with intelligent applications, is one of the main strategies to guarantee independent living of older people [8]. Considering this context, important goals are to promote personal assistance (e.g. medication reminder) and distance support (e.g. telerehabilitation programs) or to provide the caregiver with accurate and up-to-date information in order to be delivered the right care at the right time (e.g. continuous monitoring of physiological parameters or behaviors, emotions and activities), which can contribute to the overall effort to provide personalized and affordable access to essential services with efficacy and efficiency [9,10,11]. Therefore, a typical pervasive health application consists in monitoring health conditions or the progress of some chronic diseases.
For monitoring applications, sensors are required to collect relevant physiological data. A wide range of sensors, including pressure and thermal sensors, might be used to measure blood pressure, body temperature, blood glucose, heart sound, heart rate, respiration, respiratory rate, blood oxygen saturation or perspiration. Some sensors are non-invasive, but various biological signals require invasive sensors such as electrodes. Non-invasive wearable and textile devices present a considerable potential, and, for instance, they allow measuring physiological parameters through the use of techniques such as infrared or optical sensing [12].
In health care delivery, there is significant amount of information available, so the problem is less the volume and more the value that is created with the available information. Major difficulties are related to the aggregation of information from different sources, with different formats and meanings, as well as the lack of tools to identify, within all the available information, the one that is relevant for each particular situation and to make it useful rather than just being visible [13].
The information is no longer stored and exclusively managed by the Electronic Health Records (EHR) of the health care institutions [14,15,16,17]. Although EHR are adequate for the presentation of information from patients, collected and aggregated in local healthcare information systems, the reality is that the provision of health care is not restricted to an institution or even to a single care provision system. All caregivers need comprehensive, up-to-date, safe and congruent information from the patient, immediately accessible at the place of care, to ensure the highest levels of clinical quality. For instance, when considering the home monitoring of a patient with a chronic disease (e.g. diabetes, heart failure or chronic obstructive pulmonary disease), the resulting monitoring information should be distributed within an information network ranging from clinicians, social care network, and family members to the patients themselves. These requirements promote the emergence of new technological approaches such as Personal Health Record (PHR) [18] that aimed at electronic management of information between the patients and their formal and informal health care providers, and that might contribute to the availability of the patients’ clinical information that is collected throughout their lives [13].
However, the implementation of this vision is bounded by a set of problems: for instance, clinical information is blocked in healthcare information systems silos, generated and stored in different systems that either do not communicate with one another or are unable to synthesize information to make it meaningful and usable. Therefore, interoperability must be ensured, in terms of communications protocols and semantic normalization, between a wide range of information sources and eHealth applications. Hence, efforts carried out by international institutions such as the Continua Health Alliance, the Health Care Information and Management Systems Society (HIMSS), the National Institute of Standards and Technology (NIST) and the Integrating the Healthcare Enterprise (IHE), have been crucial to overcome interoperability difficulties and to promote a homogeneous eHealth ecosystem [19].
According to the European Commission [20], interoperability is a key precondition for ensuring more and better coordination and integration in health care delivery, which includes health information sharing.
The need to ensure technological and semantic interoperability in the European context is reinforced, with a set of objectives such as: defining guidelines for the type of data to be included in patient summaries, developing standards and specifications (e.g. for technological and semantic interoperability) and the promotion of systems for testing and certifying the interoperability of solutions. The Commission therefore proposes a greater effort in the development and validation of specifications and components. This effort should be extended to the pervasive health developments [21, 22].
There are also two other dimensions of interoperability mentioned in the European Commission’s report [20], which should be stated, given the importance they are assumed to have in achieving the objectives of the health services. These are organizational and legal interoperability. Organizational interoperability is directly related to the integration of processes (and conditions of information sharing between organizations) in order not to compromise collaborative work. Concerning the legal framework, there are a number of legal issues related to the issue of interoperability, such as those relating to data protection rules for patients and citizens, as well as regulatory issues (e.g. lack of definition of the roles of the various actors in the system) around mHealth applications, which offer more possibilities for self-administration of care.
Given this background, the main purpose of the systematic review reported in the present article was to explore if interoperability is a real concern when developing concrete pervasive solutions (e.g. telehealth, mHealth or ambient assisted living applications) to gather patients’ information, both clinical and contextual information.
2 Methods
The purpose of this systematic review was to identify and analyse in more detail articles related to home monitoring, which reveal an explicit concern with interoperability requirements. The general goals of this systematic review, that extends the results present in [23] were to identify, within the selected references, how interoperability is addressed in the solutions being proposed, how they are validated and if there is effective technological and semantic interoperability. The goal of this analysis was to assess if, in addition to allowing information sharing, the solutions proposed are able to produce meaningful and contextualized information that can be integrated into EHR, that is, if the information they collect is qualified to be integrated and usable in the care service provision. Moreover, if this is the case, it is important to identify the healthcare interoperability standards that are most commonly used.
2.1 Study Design
Considered the aforementioned purposes, the systematic review of the present study was informed by the following research question: Is there an explicit concern related to interoperability during the development of new eHealth applications to gather patients’ information in their home environments?
Within references selected as expressing an effective concern related to interoperability, some sub-questions were raised:
-
What are the target users being considered?
-
What interoperability solutions are being proposed?
-
What healthcare interoperability standards are being used?
-
Which methods are being used to validate the proposed interoperability implementations?
To achieve these goals, initially, a systematic review of literature published between 2011 and 2017 was performed.
Exclusively the references that had the keywords “interoperability” or “interoperable” in title or abstract were considered for further assessment and classification, being excluded the first group of references.
Subsequently, the references included for analysis were assessed and some more were excluded reflecting specified criteria, which is described below. The remaining references were then categorized according to the degree of significance to answer the questions posed within this research, that is to say, the option was to analyse in greater depth the references that proposed solutions in which it was assumed as relevant that the information produced could be integrated into the health care service provision.
The methods used to conduct this systematic review of literature as well as the subsequent categorization of search results is described in the following subsections.
2.2 Data Sources and Searches
The research was carried out using the Scopus, Web of Science and IEEE Xplore Digital Library databases, in the publications titles, abstracts and keywords.
The keywords used in the search, simultaneously, were: “monitoring” and “pervasive health”, since these are the topics around which it is important to evaluate the centrality of the interoperability issue. Pervasive health is seen as a contribution to a more personalized model of care allowing individuals to be more actively involved in their care process. A classic pervasive health care application is home monitoring of health conditions, particularly patients with chronic diseases. However, it is important to note that pervasive health is more than monitoring applications as it can also include preventive applications (e.g. elderly people to live independently) [24].
The remaining keywords were: “mobile health”, “mhealth” and “ambient assisted living”. These keywords were combined so that at least one of them corresponded to the subject of the search.
2.3 Inclusion and Exclusion Criteria
References with no author, no abstract, not written in English, duplicates and editorials were excluded. References selected for review were all written in English and all who had a date of publication between 2011 and 2017. Then, all the references that did not explicitly mention the “interoperability” or “interoperable” keywords in tittle and/or in abstract were also rejected.
Subsequently, within the references’ full texts revised, those that corresponded to items out of ambit of this systematic review were also excluded. Then, in the group of references within the scope of this systematic review, were also identified and excluded those references that corresponded to categories to be rejected in view of the objectives of this analysis, specifically: overviews, political perspectives, position papers, reviews and systematic reviews.
Then, the remaining references were clustered in ascending order of importance for this study: connection between devices; intermediate components between the devices and the client applications for handling the storage and sharing of the information being gathered (e.g. architectures, gateways, middleware or data hubs); intermediate components but incorporating medical devices specificities; and end-to-end solutions.
2.4 Study Selection
After the first screening, one author assessed all titles for relevance. Those clearly not meeting the inclusion criteria were removed.
Afterwards, the abstracts of the retrieved articles were assessed against the inclusion and exclusion criteria, by two authors. Any disagreements were discussed with a third reviewer and resolved by consensus. Abstracts were then subject to a first classification and grouping.
Finally, the references that were selected by the superior interest for this study were gathered and analysed in more detail. Two authors, according to the outlines criteria, then assessed again these full texts thought to be of relevance, and any divergences were also discussed with a third reviewer and agreed by consensus.
3 Results
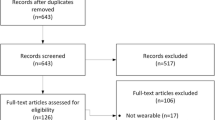
This systematic review followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [25], as described in Fig. 1.

(extended from [23]).
PRISMA flowchart
After the initial database search, 4141 references were considered for the next phase. Then, 4060 of these references were rejected because they did not explicitly mention “interoperability” or “interoperable” in the tittle and/or in the abstract.
Afterwards, by reviewing these 81 references’ full-texts, 44 were excluded: the first 30 references grouped and classified are articles assumed as out of the scope of this study; other cluster (n = 14) are references that, although within the ambit of the present analysis, were also excluded because they correspond to position papers (n = 5), systematic reviews (n = 3), reviews (n = 1), overviews (n = 2) and political standpoints (n = 3).
The remaining 37 references were first clustered in ascending order of importance for this study.
3.1 Characteristics of the Studies
The purpose of the 37 references selected for this systematic review is presented in Table 1. The studies were categorized according to different aspects of interoperability:
-
Sensors aggregation: four references [26,27,28,29] describe solutions providing communication protocols to network a large number of sensors.
-
Data aggregation: 23 references report solutions to aggregate data from various sources to provide it in an integrated way to client applications [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52]. These articles, though being related to health care applications, they do not allude to interoperability standards used in health care, inhibiting the information that is produced from being integrated into the health care service provision. However, what is described in the type of solutions proposed in three references [31, 33, 39], explicitly refer the use of health care standards, considering the specificity of medical devices (e.g. the already established ISO/IEEE 11073 standards-based Continua personal health ecosystem - X73 protocol [33]).
-
End-to-end solutions: ten references [53,54,55,56,57,58,59,60,61,62] propose interoperability solutions to ensure that the information produced could be integrated into the health care provision.
Moreover, Fig. 2 presents the temporal distribution of the selected studies.
3.2 Target Users
Among the included articles, 19 report studies aiming to develop solutions to support elderly people in their residential environment [29, 31, 33,34,35,36, 38,39,40,41, 43, 45,46,47, 49, 51, 52, 55, 58], four articles report studies targeting patients with chronic conditions (i.e. diabetes [56], cardiovascular diseases [60, 62] and cancer [54]) and the remainder articles do not refer the target users or refer that the target users are patients, without specifying their pathologies.
3.3 Interoperability
The main problem being addressed here is the lack of interoperability among different levels of available technologies which restricts a wider deployment among intermediate and end-users [39], therefore the demand for interoperability among devices is emphasized as most commercially available devices include their own software and communication protocols, which cause serious problems and hinder the application of a standard [33]. Therefore, the shortfalls of dominating insulated available products are highlighted [31].
Concerning the type of interoperability computational support, different solutions’ designations are reported although they pursue the same objective, which is the aggregation of data from multiple sources to provide them in an integrated way to client applications, namely: architectures [36,37,38, 43, 44, 46], gateways [38, 41, 44, 45], middleware [32, 35] or data hub [43].
To address interoperability, the references reported different communication protocols, including Bluetooth Health Device Profile (HDP) [39] and Open Services Gateway initiative (OSGi), a framework for modular systems that simplifies building, deploying, and managing complex applications. OSGi is complemented with the X73 standard data model, which allowed, for instance, the modelling of the information being gathered [33] so that the information resulting from different ambient assisted living systems might be integrated [31].
Next, it will be referred the ten articles (within the 81 references assessed for inclusion) that have been highlighted by this systematic review. These ten articles correspond to end-to-end solutions and they report an effective concern related to the interoperability issue, proposing concrete solutions to ensure that the information produced could be integrated into the health care provision, as summarized in Table 2.
Considering these references [53,54,55,56,57,58,59,60,61,62], which were subject to a depth analysis, in all the solutions reported the focus is on guaranteeing integration of information, being reported in every case that the resulting information is ready to be integrated in the health care service provision. However, concerning this issue, in some cases more details are given than others.
The integration of information from existing eHealth applications to provide integrated data analysis is a central concern [57]. In particular the demand to ensure interoperability of various Personal Health Devices (PHDs) and EHR for continuous monitoring and self-management of patients with chronic diseases [53,54,55,56, 58,59,60]. The need to provide sensor data in proven standard form is denoted, as the existing coding systems do not appear to be sufficient to encode the data resulting from a variety of sensors [55]. Thus, current solutions are considered to lack interoperability and obstruct the establishment of a remote patient monitoring solution market [58]. Three references are particularly focused on the need to find more advanced solutions to guarantee interconnection with the EHR as well as to improve, optimize and reduce the time in care in particular pathologies, specifically diabetes [56], cancer [54] and stroke [60].
In order to address interoperability, the reported solutions include, for instance: an application, the self-management mobile PHR that communicates with PHDs (e.g. blood pressure monitor or pulse oximeter) that have implemented standard protocols so that stored vital signs are converted to HL7 and are transmitted to PHR [59]; a PHR service, interconnected with mHealth applications that use clinical information from the EHR system from a tertiary hospital to provide services to support patients with chronic diseases, such as diabetes patients [56]; an architectural approach to integrate Home-Centred Health-Enabling Technology into Regional Health Information Systems; and a centralized registration of placeholder-documents and a decentralized data storage at patients’ home, using the Systematic Nomenclature for Contexts, Analysis methods and Problems in Health Enabling Technologies (SNOCAP-HET), which is a nomenclature to describe the context of sensor-based measurements in health-enabling technologies [55].
3.4 Interoperability Standards
Regarding the healthcare interoperability standards applied in the proposed solutions, the choice of HL7 was made in most of the solutions in which standardized solutions are reported [53, 55, 58, 59, 61, 62]. X73 Standard Data Model was used in four cases [31, 33, 58, 59] and X73 with HL7 V2.6 was used in two cases [58, 59]. Other standards were stated such as: Bluetooth Health Device Profile [39], Continuity of Care Document (CCD) and Continuity of Care Record (CCR) [59], the standards based on Continua Personal Health ecosystem [31], openEHR [62], LOINC [62], SNOMED-CT [62], DICOM [62], CEN/ISO 13606, which has been designed to support the semantic interoperability of the communications between EHR [60], and FHIR [61, 62].
3.5 Validation
Finally, concerning the methods used to validate the proposed interoperability solutions (Table 3), in one of the cases the evaluation was carried out by meaningful use [53], in another case, after laboratory tested, it was adopted as a routine in two hospitals, having also been investigated its usability and acceptance within professionals using the system [54], and in other cases the options were the proof of concept [38, 58], prototype [28, 29, 33, 37, 44, 46, 57], simulation [48, 50, 60, 62], case study [35, 42], scenarios implementation [30], and clinical trial [59]. In the remaining cases, the validation methods were not reported.
As an example, a clinical trial was carried out to evaluate the transmission error rate for the measured vital signs transmitted from PHD to an mHealth application and from this to PHR Systems [59]. Another case was the technological platform that was tested with clinician staff, researchers, electronic support staff and actors playing patients role, having been defined several scenarios to test the technological structure, being stated that, after this phase, the platform would be tested with patients suffering from clinical suspicion of stroke [60].
4 Conclusion
Considering the target users of the applications being reported, surprisingly in most articles the specifications are quite vague (i.e. elderly or patients, in general). Only four articles do specifically refer which are the target users (i.e. patients suffering from diabetes, cardiovascular diseases or cancer).
A central challenge for healthcare applications is how to handle the complexity and variability caused by the specificities of the healthcare processes. Deeper analyses of the healthcare process reveal the intricacy and the changeability of the clinical information and, therefore, the difficulties in dealing with information interoperability. The vague description of the target users and the respective health conditions precludes that additional elicitations of requirements are needed, which will increase the costs and the density of the resulting implementations.
The design and implementation of pervasive health applications has not yet reached its potential in terms of impact it can have on health care provision, and interoperability is assumed as being an essential requirement. In this respect, the included articles reporting end-to-end solutions aimed to turn possible PHD connected in conjunction with institutional EHR systems. For that, the studies propose interoperability platforms able to gather and distribute the clinical information [53,54,55, 57, 58, 60], or applications able to guarantee a common understanding between PHD and EHRs, using a diversity of standards (e.g. HL7, CEN/ISO 13606 or X73). In all the solutions reported the focus is on guaranteeing integration of information, being stated in every case that the resulting information is ready to be integrated in the health care service provision, although in only half of the cases the details concerning this issue, are given more objectively. The integration of information from pervasive health applications to provide integrated data analysis should be a concern. Current solutions lacking interoperability might obstruct the establishment of a remote patient monitoring solution market.
In terms of the validation of the solutions being proposed, only one study [59] included a clinical trial. However, evidence-based medicine is supported on statistical significance and the new developments must be conveniently evaluated in real world conditions. It is necessary to go behind studies aiming the design, development and evaluation of prototypes (i.e. proof-of-concept).
The results of the systematic review presented in this article show that interoperability is not the major concern of a significant number of current technological developments related to pervasive health. Indeed, it should be emphasized that of the 4141 initial references only 81 references explicitly mentioned the issue of interoperability. Moreover, within these 81 references assessed for inclusion, only ten corresponded to end-to-end solutions, since the information produced could be integrated into the health care service provision, where interoperability was considered an effective concern. Finally, within these ten references only three refer standards specifically related to semantic interoperability, used in a system whose validation is not yet reported.
Therefore, large-scale collaboration among technology developers, companies, policy makers, patient’s organizations and health professionals are essential for pervasive health surpass the interoperability challenge.
References
Cook, D.J., Das, S.K.: Pervasive computing at scale: transforming the state of the art. Pervasive Mob. Comput. 8(1), 22–35 (2012)
Weiser, M.: Hot topics: ubiquitous computing. IEEE Comput. 26(10), 71–72 (1993)
Cook, D.J., Augusto, J.C., Jakkula, V.R.: Ambient intelligence, applications, and opportunities. Pervasive Mob. Comput. 5(4), 277–298 (2009)
Connelly, K., et al.: The future of pervasive health. IEEE Pervasive Comput. 16(1), 16–20 (2017)
Korhonen, I., Barddram, J.: Guest editorial introduction to the special section on pervasive healthcare. IEEE Trans. Inf. Technol. Biomed. 8(3), 229 (2004)
Mosa, A., Yoo, I., Sheets, L.: A systematic review of healthcare applications for smartphones. BMC Med. Inform. Decis. Mak. 12(1), 67 (2012)
Heath, I.: Never had it so good? BMJ 336(7650), 950–951 (2008)
Kleinberger, T., Becker, M., Ras, E., Holzinger, A., Müller, P.: Ambient intelligence in assisted living: enable elderly people to handle future interfaces. In: Stephanidis, C. (ed.) UAHCI 2007. LNCS, vol. 4555, pp. 103–112. Springer, Heidelberg (2007). https://doi.org/10.1007/978-3-540-73281-5_11
Kapoor, A.: New frontiers in machine learning for predictive user modeling. In: Human-Centric Interfaces for Ambient Intelligence. Academic Press, Oxford (2010)
Mirarmandehi, N.: An asynchronous dynamic bayesian network for activity recognition in an Ambient Intelligent environment. In: Pervasive Computing and Applications (ICPCA) (2010)
Queirós, A., Carvalho, S., Pavão, J., Rocha, N.: AAL information based services and care integration. In: Healthinf 2013 - Proceedings of the International Conference on Health Informatics. SciTePress (2013)
Rashidi, P., Mihailidis, A.: A survey on ambient-assisted living tools for older adults. IEEE J. Biomed. Health Inform. 17(3), 579–590 (2013)
Halevy, A.: Game-changing interoperability for healthcare: bringing semantically harmonized clinical information into provider workflows from disparate health information technologies. In: 8th International Conference and Expo on Emerging Technologies for a Smarter World, CEWIT 2011 (2011). https://doi.org/10.1109/cewit.2011.6135863
Emery, D., Heyes, B.J., Cowan, A.M.: Telecare delivery of health and social care information. Health Inform. J. 8(1), 29–33 (2002)
Eysenbach, G.: What is e-health? J. Med. Internet Res. 3(2), E20 (2001). https://doi.org/10.2196/jmir.3.2.e20 [Medline: 11720962]
Kvedar, J., Coye, M.J., Everett, W.: Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff. (Millwood) 33(2), 194–199 (2014). https://doi.org/10.1377/hlthaff.2013.0992 [Medline: 24493760]
Rossi, M.A., Mazzeo, M., Mercurio, G., Verbicaro, R.: Holistic health: predicting our data future (from inter-operability among systems to co-operability among people). Int. J. Med. Inform. 82(4), e14–e28 (2013). https://doi.org/10.1016/j.ijmedinf.2012.09.003 [Medline: 23122923]
Krukowski, A., et al.: Personal health record. In: Voros, N.S., Antonopoulos, C.P. (eds.) Cyberphysical Systems for Epilepsy and Related Brain Disorders, pp. 205–238. Springer, Cham (2015). https://doi.org/10.1007/978-3-319-20049-1_11
Aragüés, A., et al.: Trends and challenges of the emerging technologies toward interoperability and standardization in e-Health communications. IEEE Commun. Mag. 49(11), 182–188 (2011). https://doi.org/10.1109/MCOM.2011.6069727
European Commission Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions: eHealth Action Plan 2012–2020 - Innovative healthcare for the 21st century. European Commission, Brussels (2012). https://ec.europa.eu/digital-single-market/en/news/ehealth-action-plan-2012-2020-innovative-healthcare-21st-century. Accessed 06 June 2018
Kuziemsky, C.E., Peyton, L.A.: framework for understanding process interoperability and health information technology. Health Policy Technol. 5(2), 196–203 (2016). https://doi.org/10.1016/j.hlpt.2016.02.007
Perlin, J.B.: Health information technology interoperability and use for better care and evidence. JAMA – J. Am. Med. Assoc. 316(16), 1667–1668 (2016). https://doi.org/10.1001/jama.2016.12337
Dias, A., Martins, A., Queirós, A., Pacheco, R.N.: Interoperability in pervasive health: is it tackled as a priority? In: Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies – HEALTHINF, vol. 5, pp. 57–65 (2018). ISBN 978-989-758-281-3. https://doi.org/10.5220/0006545400570065
Queirós, A., et al.: Pervasive health and regulatory frameworks. In: Verdier, C., Bienkiewicz, M., Fred, A., Gamboa, H., Elias, D. (eds.) BIOSTEC 2015, Proceedings of the International Joint Conference on Biomedical Engineering Systems and Technologies, vol. 5, pp. 494–501 (2015). https://doi.org/10.5220/0005249204940501
Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G.: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6(7), e1000097 (2009). https://doi.org/10.1371/journal.pmed.1000097
Grossi, F., Bianchi, V., Losardo, A., Matrella, G., De Munari, I., Ciampolini, P.: A flexible framework for ambient assisted living applications. In: IASTED International Conference on Assistive Technologies Proceedings, AT 2012, pp. 817–824 (2012). https://doi.org/10.2316/p.2012.766-007
Escobar, R., Akopian, D., Boppana, R.: A sensor data format incorporating battery charge information for smartphone-based mHealth applications. In: SPIE - The International Society for Optical Engineering Proceedings, vol. 9411 (2015). https://doi.org/10.1117/12.2083758
Elsaadi, R., Shafik, M.: Deployment of assisted living technology using intelligent body sensors platform for elderly people health monitoring. Adv. Transdisc. Eng. 3, 219–224 (2016). https://doi.org/10.3233/978-1-61499-668-2-219
Palma, L., Pernini, L., Belli, A., Valenti, S., Maurizi, L., Pierleoni, P.: IPv6 WSN solution for integration and interoperation between smart home and AAL systems. In: SAS 2016 - Sensors Applications Symposium Proceedings, pp. 171–175 (2016). https://doi.org/10.1109/sas.2016.7479840
Su, C., Wu, C.: JADE implemented mobile multi-agent based, distributed information platform for pervasive health care monitoring. Appl. Soft Comput. J. 11(1), 315–325 (2011). https://doi.org/10.1016/j.asoc.2009.11.022
Norgall, T., Wichert, R.: Towards interoperability and integration of personal health and AAL ecosystems. Stud. Health Technol. Inform. 177, 272–282 (2012). https://doi.org/10.3233/978-1-61499-069-7-272
Carr, D., O’Grady, M.J., O’Hare, G.M.P., Collier, R.: SIXTH: a middleware for supporting ubiquitous sensing in personal health monitoring (2013). https://doi.org/10.1007/978-3-642-37893-5_47_e
Damas, M., Pomares, H., Gonzalez, S., Olivares, A., Rojas, I.: Ambient assisted living devices interoperability based on OSGi and the X73 standard. Telemed. e-Health 19(1), 54–60 (2013). https://doi.org/10.1089/tmj.2012.0052
Ferreira, L., Ambrósio, P.: Towards an interoperable health-assistive environment: the eHealthCom platform. In: IEEE-EMBS International Conference on Biomedical and Health Informatics Proceedings: Global Grand Challenge of Health Informatics, BHI 2012, pp. 930–932 (2012). https://doi.org/10.1109/bhi.2012.6211740
Kilintzis, V., Moulos, I., Koutkias, V., Maglaveras, N.: Exploiting the universAAL platform for the design and development of a physical activity monitoring application. In: ACM International Conference Proceeding Series (2013). https://doi.org/10.1145/2504335.2504351
Norgall, T., Wichert, R.: Personalized use of ICT-from telemonitoring to ambient assisted living. Stud. Health Technol. Inform. 187, 145–151 (2013). https://doi.org/10.3233/978-1-61499-256-1-145
Ruiz-Zafra, Á., Benghazi, K., Noguera, M., Garrido, J.L.: Zappa: an open mobile platform to build cloud-based m-Health systems. In: van Berlo, A., Hallenborg, K., Rodríguez, J., Tapia, D., Novais, P. (eds.) Ambient Intelligence - Software and Applications. AISC, vol. 219, pp. 87–94. Springer, Heidelberg (2013). https://doi.org/10.1007/978-3-319-00566-9_12
Costa, A., Novais, P., Simoes, R.: An AAL collaborative system: the AAL4ALL and a mobile assistant case study. In: Camarinha-Matos, L.M., Afsarmanesh, H. (eds.) PRO-VE 2014. IAICT, vol. 434, pp. 699–709. Springer, Heidelberg (2014). https://doi.org/10.1007/978-3-662-44745-1_69
Pereira, R., Barros, C., Pereira, S., Mendes, P.M., Silva, C.A.: A middleware for intelligent environments in ambient assisted living. In: Annual International Conference of the IEEE Engineering in Medicine and Biology Society, IEEE Engineering in Medicine and Biology Society. Annual Conference, pp. 5924–5927 (2014). https://doi.org/10.1109/embc.2014.6944977
Rossi, L., et al.: Interoperability issues among smart home technological frameworks. In: MESA 2014 – 10th IEEE/ASME International Conference on Mechatronic and Embedded Systems and Applications, Conference Proceedings (2014). https://doi.org/10.1109/mesa.2014.6935626
Denkovski, D., Atanasovski, V., Gavrilovska, L.: Device gateway design for ambient assisted living. In: Atanasovski, V., Leon-Garcia, A. (eds.) FABULOUS 2015. LNICST, vol. 159, pp. 100–107. Springer, Cham (2015). https://doi.org/10.1007/978-3-319-27072-2_13
Pradilla, J., Palau, C., Esteve, M.: SOSLITE: lightweight sensor observation service (SOS) for the internet of things (IOT). In: 2015 ITU Kaleidoscope: Trust in the Information Society (K-2015), Barcelona, pp. 1–7 (2015). https://doi.org/10.1109/kaleidoscope.2015.7383625
Woznowski, P., et al.: A multi-modal sensor infrastructure for healthcare in a residential environment. In: 2015 IEEE International Conference on Communication Workshop Proceedings, ICCW 2015, pp. 271–277 (2015). https://doi.org/10.1109/iccw.2015.7247190
Ding, F., Song, A., Tong, E., Li, J.: A smart gateway architecture for improving efficiency of home network applications. J. Sens. 216, 10 p. (2016). https://doi.org/10.1155/2016/2197237
Smirek, L., Zimmermann, G., Beigl, M.: Just a smart home or your smart home - a framework for personalized user interfaces based on eclipse smart home and universal remote console. Procedia Comput. Sci. 58, 107–116 (2016). https://doi.org/10.1016/j.procs.2016.09.018
Xiao, B., Kanter, T., Rahmani, R.: Logical interactions for heterogeneous IoT entities via virtual world mirrors in support of ambient assisted living. J. Ambient Intell. Smart Environ. 8(5), 565–580 (2016). https://doi.org/10.3233/AIS-160398
Frontoni, E., Pollini, R., Russo, P., Zingaretti, P., Cerri, G.: HDOMO: smart sensor integration for an active and independent longevity of the elderly. Sensors 17(11), 2610 (2017)
Xu, B., Xu, L., Cai, H., Jiang, L., Luo, Y., Gu, Y.: The design of an m-Health monitoring system based on a cloud computing platform. Enterp. Inf. Syst. 11(1), 17–36 (2017)
Costa, A., Julián, V., Novais, P.: Advances and trends for the development of ambient-assisted living platforms. Expert Syst. 34(2), e12163 (2017)
Garcés, L., Nakagawa, E.Y.: A process to establish, model and validate missions of systems-of-systems in reference architectures. In: the Symposium on Applied Computing Proceedings, pp. 1765–1772. ACM (2017)
Yacchirema, D.C., Palau, C.E., Esteve, M.: Enable IoT interoperability in ambient assisted living: Active and healthy aging scenarios. In: Proceedings of 2017 14th IEEE Annual Consumer Communications & Networking Conference (CCNC), pp. 53–58. IEEE (2017)
Zgheib, R., De Nicola, A., Villani, M.L., Conchon, E., Bastide, R.: A flexible architecture for cognitive sensing of activities in ambient assisted living. In: Proceedings of Enabling Technologies: Infrastructure for Collaborative Enterprises (WETICE), pp. 284–289. IEEE (2017)
Lee, D., Bae, S., Song, J.H., Yi, B., Kim, I.K.: Improving chronic disease management with mobile health platform. In: Annual International Conference of the IEEE Engineering in Medicine and Biology Society Proceedings, EMBS, pp. 2275–2278 (2013). https://doi.org/10.1109/embc.2013.6609991
Galligioni, E., et al.: Integrating mHealth in oncology: experience in the province of trento. J. Med. Internet Res. 17(5), e114 (2015). https://doi.org/10.2196/jmir.3743
Gietzelt, M., et al.: Home-centered health-enabling technologies and regional health information systems an integration approach based on international standards. Methods Inf. Med. 53(3), 160–166 (2014). https://doi.org/10.3414/ME13-02-0008
Jung, E., Kim, J., Chung, K., Park, D.K.: Mobile healthcare application with EMR interoperability for diabetes patients. Clust. Comput. 17(3), 871–880 (2014). https://doi.org/10.1007/s10586-013-0315-2
Alberts, R., Fogwill, T., Botra, A., Cretty, M.: An integrative ICT platform for eHealth. In: 2014 IST-Africa Conference and Exhibition Proceedings, IST-Africa 2014 (2014). https://doi.org/10.1109/istafrica.2014.6880650
Mihaylov, M., Mihovska, A., Kyriazakos, S., Prasad, R.: Interoperable eHealth platform for personalized smart services. In: 2015 IEEE International Conference on Communication Workshop Proceedings, ICCW 2015, pp. 240–245 (2015). https://doi.org/10.1109/iccw.2015.7247185
Park, H.S., Cho, H., Kim, H.S.: Development of a multi-agent m-health application based on various protocols for chronic disease self-management. J. Med. Syst. 40(1), 36 (2016). https://doi.org/10.1007/s10916-015-0401-5
Torres Zenteno, A.H., et al.: Mobile platform for treatment of stroke: a case study of tele-assistance. Health Inform. J. 22(3), 676–690 (2016). https://doi.org/10.1177/1460458215572925
Aliakbarpoor, Y., Comai, S., Pozzi, G.: Designing a HL7 compatible personal health record for mobile devices. In: 2017 IEEE 3rd International Forum Research and Technologies for Society and Industry (RTSI) Proceedings, pp. 1–6. IEEE (2017)
Roehrs, A., da Costa, C.A., da Rosa Righi, R.: OmniPHR: a distributed architecture model to integrate personal health records. J. Biomed. Inform. 71, 70–81 (2016)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this paper
Cite this paper
Dias, A., Martins, A.I., Queirós, A., Rocha, N.P. (2019). Interoperability in Pervasive Health: A Systematic Review. In: Cliquet Jr., A., et al. Biomedical Engineering Systems and Technologies. BIOSTEC 2018. Communications in Computer and Information Science, vol 1024. Springer, Cham. https://doi.org/10.1007/978-3-030-29196-9_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-29196-9_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-29195-2
Online ISBN: 978-3-030-29196-9
eBook Packages: Computer ScienceComputer Science (R0)