Abstract
The use of ultrasound guidance has been increasingly recognized as feasible and reliable in performing interventional procedures. In this chapter, we describe the relevant sonoanatomy of the cervical and lumbar spine, as well as technical approaches in performing common interventional spine procedures with ultrasound guidance, including selective cervical spinal nerve root injection, cervical facet joint injection and medial branch block, stellate ganglion block, lumbar facet joint injection and medial branch nerve block, sacroiliac joint injection, and caudal epidural injection.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
While fluoroscopy remains the most frequently used imaging technique employed by interventional spine physicians, the use of ultrasound guidance has been increasingly recognized as both feasible and reliable in performing interventional procedures.
-
Cervical transforaminal epidural injection and selective nerve root injection can be performed safely and effectively with ultrasound guidance.
-
Ultrasound guidance can be utilized for cervical medial branch nerve blocks and facet joint interventions.
-
Ultrasound guidance offers unique advantage in stellate ganglion block.
-
Common lumbosacral interventional procedures, including lumbar facet joint interventions, caudal epidural steroid injection, sacroiliac joint injection, etc., can be performed with ultrasound guidance as well.
Introduction
Low back pain and neck pain of spine origin are extremely common health complaints with an enormous social, psychological, and economic burden [1,2,3]. Interventional spine procedures, though its effectiveness is still being debated, have been utilized for the past several decades, both diagnostically and therapeutically, in the management of spine pain [4, 5]. While fluoroscopy remains the most frequently used imaging technique employed by interventional spine physicians, the use of ultrasound guidance has been increasingly recognized as both feasible and reliable in performing interventional procedures. Several advantages in ultrasound guidance as compared to fluoroscopic guidance have provided the basis for the increasing popularity of such technique among intervention pain physicians. The ability to visualize soft tissue, such as important neural and vascular structures, and the ability to visualize real-time needle advancement make ultrasound guidance appealing to interventional pain physicians. The avoidance of ionizing radiation and the affordability and portability of modern ultrasound machines further add to this appeal. Ultrasonography may be particularly helpful in the cervical area because a multitude of blood vessels and other vital structures are compacted in a small area [6].
Nevertheless, despite progresses in the state-of-art ultrasound scanners, currently the resolution of even the most sophisticated ultrasound units is still not comparable to fluoroscopy; visualization of deep structures with ultrasound as required in performing interventional spine procedures can still be challenging and requires specialized training and considerable experience. In this chapter, we describe the relevant sonoanatomy of the cervical and lumbar spine, as well as technical approaches in performing common interventional spine procedures with ultrasound guidance.
Cervical Transforaminal Epidural Injection (Selective Nerve Root Injection)
Anatomy
The cervical spinal nerve root can be identified as a hypoechoic circle in between the anterior and posterior tubercles of the transverse process at each spinal level. In their early work, Narouze et al. described the technique to identify cervical spinal level with sonography [7]. The cervical spinal level can be identified by the characteristic shape of the transverse process of C7, which has a rudimentary or absent anterior tubercle and a prominent posterior tubercle (Fig. 28.1). The transducer is then moved cranially, the C6 transverse process can be visualized with its characteristic sharp anterior tubercle and a smaller posterior tubercle (Fig. 28.2). From C6 and above, both the anterior and posterior tubercles of the transverse process can be visualized; the cervical spinal nerve root exits the foraminal opening between the anterior and posterior tubercles of the transverse process, which can be easily identified as the “2-humped camel” (Fig. 28.2, C6 level; Fig. 28.3, C5 level).
Short-axis view at C7 level. Patient is placed in a supine position with head turned 45 degrees to the left side. Ultrasound transducer is placed in the right side of the neck at C7 level transversely. CA carotid artery, IJ internal jugular vein, SCM sternocleidomastoid muscle, C7 C7 nerve root, AS anterior scalene muscle, TP transverse process, Arrows brachial plexus, VA vertebral artery, TCt thyrocervical trunk
Short-axis view at C6 level. Patient is placed in a supine position with head turned 45 degrees to the left side. Ultrasound transducer is placed in the right side of the neck at C6 level transversely. CA carotid artery, IJ internal jugular vein, SCM sternocleidomastoid muscle, C6 C6 nerve root, C5 C5 nerve root, AS anterior scalene muscle, AT anterior tubercle, PT posterior tubercle
Short-axis view at C5 level. Patient is placed in a supine position with head turned 45 degrees to the left side. Ultrasound transducer is placed in the right side of the neck at C5 level transversely. CA carotid artery, IJ internal jugular vein, SCM sternocleidomastoid muscle, C5 C5 nerve root, AT anterior tubercle, PT posterior tubercle
Alternatively, the cervical spinal level can be determined by using the vertebral artery as a landmark. The vertebral artery passes anterior and medial to the transverse process of C7, enters through the transverse foramen of C6, and progresses toward the head through the transverse foramen of each cervical vertebrates before it enters the foramen magnum through the posteromedial side of the atlas. The vertebral artery can be visualized as a pulsating round structure anterior and medial to the C7 transverse process. At this level, the thyrocervical trunk, which arises lateral to the vertebral artery from the subclavian artery, can also be seen immediate medial to the C7 transverse process. Using color Doppler can help identify these important vascular structures and avoid inadvertent vascular injury during procedure (Fig. 28.4). The cervical spinal levels can then be determined by moving the transducer cranially until the transverse process of the next cervical level is seen. Doppler imaging can be very helpful in identifying the vertebral artery at the C7 level [8].
Short-axis view at C7 level with color Doppler. Patient is placed in a supine position with head turned 45 degrees to the left side. Ultrasound transducer is placed in the right side of the neck at C5 level transversely. CA carotid artery, IJ internal jugular vein, SCM sternocleidomastoid muscle, C7 C7 nerve root, VA vertebral artery, TCt thyrocervical trunk
Patient Position
Patient is placed in a lateral decubitus position with the side of intervention up. Alternatively, the patient can be placed in a supine position, with the head rotated 30–45 degrees away from the targeted area. An 8–12 Hz linear array transducer is used. The transducer is placed transversely in the lateral neck.
Approach
Once the appropriate spinal level is identified, the transverse axial view is obtained, a 22-gauge, blunt-tip needle is advanced in the posterior-lateral to anterior-medial direction with an in-plane approach under real-time visualization until the needle tip passes the posterior tubercle (Fig. 28.5). Caution should be exercised not to advance the needle into the hypoechoic cervical spinal nerve root. At this point, 2 ml of injectate (local anesthetics only for diagnostic selective nerve root block, dexamethasone 8 mg for transforaminal epidural steroid injection) is injected under direct visualization.
Ultrasound-guided C5 selective nerve root injection. Patient is placed in a supine position with head turned 45 degrees to the left side. Ultrasound transducer is placed in the right side of the neck at C5 level transversely. CA carotid artery, IJ internal jugular vein, SCM sternocleidomastoid muscle, N nerve (C5 nerve root), AT anterior tubercle, PT posterior tubercle, Arrows needle, N C5 nerve root
Outcome Study
In a recent randomized blinded controlled study, ultrasound-guided selective cervical nerve root block was shown to be as effective as the fluoroscopy-guided method in pain relief and functional improvement [9].
Cervical Medial-Branch Intervention and Facet Joint Injections
Anatomy
The zygapophyseal or facet joints are important structures in determining the biomechanical properties of the spinal column and are of clinical relevance. The facet joints are diarthrodial joints formed by the superior articular process of one cervical vertebra articulating with the inferior articular process of the vertebra above at the level of the junction of the lamina and the pedicle. The angulation of the facet joint increases caudally, being about 45 degrees superior to the transverse plane at the upper cervical level to assume a more vertical position at the upper thoracic level [10, 11].
The cervical facet joints are innervated by articular branches derived from the medial branches of the cervical dorsal rami. Bogduk described the anatomy of the cervical dorsal rami [12]. The C4–C8 dorsal rami arise from their respective spinal nerves and pass dorsally over the root of their corresponding transverse process. The medial branches of the cervical dorsal rami curve medially, around the corresponding articular pillars, and have a constant relationship to the bone at the dorsolateral aspect of the articular pillar as they are bound to the periosteum by an investing fascia and held in place by the tendon of the semispinalis capitis muscle.
The cervical articular processes and the facet joints can be identified in a longitudinal view parallel to the long axis of the cervical spine. The alternating hyperechoic cervical articular processes and anechoic facet joints forms the characteristic “saw sign” in this view [13, 14] (Fig. 28.6). The cervical medial branch nerve courses at the lowest point (waist) along the hyper echoic line representing the articular pillar (Fig. 28.7).
Patient Position
Patient is placed in a prone position with forehead supported. The advantage of this approach is using the characteristic bifid C2 spinous process (Fig. 28.8) as a landmark in determining spinal levels and the ease of performing bilateral procedures without repositioning the patient [15].
Approach
The cervical spinal levels can be determined by one of two ways: using the characteristic appearance of C7 transverse process (prominent posterior tubercle and absence of anterior tubercle, adjacent pulsating vertebral artery) or using the characteristic bifid shape of C2 spinous process posteriorly (see Fig. 28.8). Once the appropriate spinal level is identified, the probe is turned 90 degrees to obtain the longitudinal view. A 22-gauge, blunt-tip needle is advanced the caudal to cranial direction into anechoic cervical facet joint in between the hyperechoic articular processes under real-time visualization. At this point, 0.5–1 ml of injectate (local anesthetics only for diagnostic block, 2 mg dexamethasone for steroid injection) is injected under direct visualization.
For medial branch nerve block, the needle tip is placed at the midpoint of the articular process at the corresponding level, which corresponds to the deepest point (waist) of the articular pillar (Fig. 28.9). Although the medial branch nerve can be visualized as a hypoechoic oval structure at the deepest point (waist) of the articular pillar, this nerve may not be clearly visible in many cases due to the small size and limitation of scanner resolution. Fluoroscopy may be superior in this application especially in radiofrequency ablation of the medial nerves as this requires precise needle placement along the targeted nerve [15].
Outcome Study
Obernauer et al. reported a randomized controlled trial with 40 patients randomized to CT or ultrasound-guided facet injections. Ultrasound-guided intra-articular injections showed the same therapeutic effect as CT-guided intra-articular injections and the former resulted in a significant reduction of procedure duration without any exposure to radiation [16].
Stellate Ganglion Block
Anatomy
The stellate ganglion (cervicothoracic ganglion) is a sympathetic ganglion formed by the fusion of the inferior cervical ganglion and the first thoracic ganglion. Stellate ganglion is located at the level of C7, anterior to the transverse process of C7 and the neck of the first rib and superior to the cervical pleura and just below the subclavian artery. For stellate ganglion block, injection is often given near the Chassaignac’s tubercle (anterior tubercle of transverse process of C6) as this is a safer location for intervention. The vertebral artery is projected in the transverse foramen of the cervical vertebrate from the C6 level and up cranially but is exposed at C7 level due to the absence of an anterior tubercle of the transverse process. It is thought that anesthetic spreads along the paravertebral muscles to the stellate ganglion.
Indication
Stellate ganglion block is an established procedure for the diagnosis and treatment of impaired vascular circulation and upper extremity pain including complex regional pain syndrome type I and II and pain from herpes zoster. Left-sided stellate ganglion block has also been used for control of frequent ventricular arrhythmias [17,18,19,20]. Right-sided stellate ganglion block has been shown to reduce hot flushes and night awakenings suffered by breast cancer survivors [21, 22] and women experiencing extreme menopause [23]. Recently, stellate ganglion block has also been shown to be effective against post-traumatic stress syndrome (PTSD) [24, 25].
Patient Position
Patient is placed in a lateral decubitus position with the side of intervention up. Alternatively, the patient can be placed in a supine position, with the head rotated 30–45 degrees away from the targeted area. It is often advantageous to place a roll under the shoulder and place the patient in a semi-lateral position to allow more room posterior to the neck to perform the block. An 8–12 Hz linear array transducer is used. For obese patient, a low-frequency curvilinear probe may be needed. The transducer is placed transversely in the lateral neck.
Approach
It is important to identify the correct cervical spinal level before performing this procedure. To minimize the risk of vertebral artery injury, this procedure is best performed at the C6 level where the vertebral artery is protected in the transverse process, as compared to at C7 level where it is exposed. The cervical spinal level can be identified in the short-axis view based on the characteristic view at C6 and C7 levels as described earlier in this chapter (see Fig. 28.1, Fig. 28.2). At the C6 level, in the short-axis view, the C6 transverse process typically appears with a prominent anterior tubercle and a shorter posterior tubercle. The C6 nerve root exits in between the anterior and posterior tubercles. The longus colli muscle can be seen as an oval structure adjacent to the base of the transverse process and vertebral body. The middle cervical ganglion, which is in continuation with the stellate ganglion via the cervical sympathetic chain, is located anteriorly to longus colli muscle (Fig. 28.10).
Short-axis view at C6 level. The C6 transverse process typically appears with a prominent anterior tubercle and a shorter posterior tubercle. The C6 nerve root exits in between the anterior and posterior tubercles. The longus colli muscle can be seen as an oval structure adjacent to the base of the transverse process and vertebral body. The middle cervical ganglion, which is in continuation with the stellate ganglion via the cervical sympathetic chain, is located anteriorly to the longus colli muscle. CA carotid artery, IJ internal jugular vein, SCM sternocleidomastoid muscle, N nerve (C6 nerve root), AT anterior tubercle, LC longus colli muscle, PT posterior tubercle, TP transverse process
Gofled et al. presented a posterior lateral approach of stellate ganglion block, which has gain popularity among practitioners due to its superior safety [26]. Once a satisfactory short-axis view at C6 level is identified, a 22-gauge, blunt-tip needle is advanced in posterior lateral to anterior medial direction with an in-plane approach under real-time visualization until the needle tip passes the anterior tubercle of C6 and reaches just beneath the prevertebral fascia on the anterior surface of longus colli muscle (Fig. 28.11). Subfascial injection through this approach, even with a volume as little as 5 ml, has been shown to ensure reliable spread of injectate to the stellate ganglion [26].
Ultrasound-guided stellate ganglion block at C6 level. The C6 transverse process typically appears with a prominent anterior tubercle and a shorter posterior tubercle. The C6 nerve root exits in between the anterior and posterior tubercles. The longus colli muscle can be seen as an oval structure adjacent to the base of the transverse process and vertebral body. The middle cervical ganglion, which is in continuation with the stellate ganglion via the cervical sympathetic chain, is located anteriorly to the longus colli muscle. CA carotid artery, IJ internal jugular vein, SCM sternocleidomastoid muscle, AT anterior tubercle, arrows block needle, arrowhead middle cervical ganglion, VB vertebral body of C6
Lumbar Medial Branch and Facet Joint Injections
Anatomy
Similar to cervical facet joints, lumbar facet joints are also diarthrodial joints involving the cartilaginous surfaces of the articular processes of adjacent vertebra. Each lumbar facet joint is innervated by the medial branches of the dorsal rami from the same vertebral level and from the superior vertebral level. Each medial branch nerve crosses the root of the inferior transverse process and then runs in a groove formed by the junction of the corresponding transverse process and superior articular process where it runs under the medial curve of the mamillo-accessory ligament before it innervates the multifidus muscle [27, 28] and divides into the superior and inferior articular branches to supply the facets above and below at each level. The L5 dorsal ramus differs from the other lumbar dorsal rami. It crosses the sacral ala and gives off the medial branch only as it reaches the caudal aspect of the L5-S1 facet joint [27].
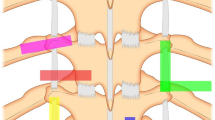
The sonographic anatomy of the lumbar medial branch and facet joints was first described by Greher et al. [29]. A short-axis view through the articular and the transverse process of the lumbar vertebra is obtained. The facet joint space is seen between the inferior articular process and superior articular process (Fig. 28.12). The medial branch nerve may not necessarily be clearly visualized. The junction point between the SAP and the transverse process can be used as the target point for medial branch intervention (Fig. 28.13).
Lumbar facet joint. Patient is placed in a prone position. A curvilinear ultrasound transducer is placed in a transverse plane axis plane. The facet joint space (arrow) is seen between the inferior articular process (IAP) and superior articular process (SAP) of the adjacent vertebrate. SP spinous process, IAP inferior articular process, SAP superior articular process
Lumbar medial branch nerve. Patient is placed in a prone position. A curvilinear ultrasound transducer is placed in a transverse plane axis plane. The junction point between the superior articular process and the transverse process can be used as the target point for medial branch intervention. SP spinous process, TP transverse process, SAP superior articular process
Patient Position
Patient is placed in a prone position. Due to the depth of the relevant structures, a low-frequency curvilinear transducer (2–6 Hz) is best suited for this application. The transducer is first placed in the long axis to identify the sacrum and establishing spinal levels and then rotated to the short-axis view to visualize axial structures.
Approach
First, the correct spinal level needs to be established. The transducer is placed longitudinally in a parasagittal plane over the sacrum. The continuous hyperechoic line represents the dorsal surface of the sacrum. The first interruption to this continuous line cranially represents the L5/S1 interlaminar space (Fig. 28.14). The lamina and interlaminar space alternate as the transducer is moved cranially. Once the correct level is reached, the transducer is rotated by 90 degrees to obtain a transverse view showing the transverse process and the corresponding superior articular process. For medial branch nerve block, a 22-gauge needle is advanced in-plane in a lateral to medial approach under real-time visualization toward the groove at the junction between the base of the superior articular process and the superior border of the transverse process until contacting bone (Fig. 28.15a). The transducer is then rotated to the long-axis view again to confirm the location of the needle tip is at the superior margin of the transverse process (Fig. 28.15b).
Parasagittal view of the sacrum and lumbar spine. The transducer is placed longitudinally in a parasagittal plane over the sacrum. The continuous hyper echoic line represents the dorsal surface of the sacrum. The first interruption to this continuous line cranially represents the L5/S1 interlaminar space. The lamina and interlaminar space alternate as the transducer is moved cranially. Arrows needle accessing the L5/S1 interlaminar space
Lumbar medial branch nerve block. Patient is placed in a prone position. A curvilinear ultrasound transducer is placed in a transverse plane axis plane. A 22-gauge needle is advanced toward the groove at the junction between the base of the superior articular process and the superior border of the transverse process until contacting bone (panel a). The transducer is then rotated to the long-axis view again to confirm the location of the needle tip is at the superior margin of the transverse process (panel b). TP transverse process, SP spinous process, SAP superior articular process, Arrows needle
For lumbar facet joint injection, similar short-axis view is obtained to show the facet joint space between the inferior and superior articular process. A 22-gauge needle is advanced in-plane in a lateral to medial approach under real-time ultrasound visualization toward facet joint space between the inferior and superior articular process (Fig. 28.16a). The transducer is then rotated to the long-axis view again to confirm the location of the needle tip is in the joint space (Fig. 28.16b).
Lumbar facet joint intraarticular injection. Patient is placed in a prone position. A curvilinear ultrasound transducer is placed in a transverse plane axis plane. The facet joint space is seen between the inferior articular process and superior articular process of the adjacent vertebrate. A 22 gauge needle is advanced into the joint space under direct visualization (panel a). The transducer is then rotated to the long-axis view again to confirm the location of the needle tip is in the joint space (panel b). FJ facet joint, TP transverse process, SAP superior articular process, IAP inferior articular process, Arrows needle
Outcome Study
Galiano et al. reported a randomized controlled study comparing ultrasound-guided versus CT-guided lumbar facet joint injection. They were able to visualize the lumbar facet joint in 16 patients out of the 20 patients randomized. There was no difference in benefit detected between the ultrasound-guided versus CT-guided lumbar facet joint injection groups [30]. Due to the depth of the medial branch nerve and facet joints, a low-frequency transducer is often required. As such, the resolution of the sonographic images is relatively low. Visualization of the needle and injectate spread at such depth can be challenging, especially in obese patients. At current time, fluoroscopic guidance is still the preferred technique for performing lumbar facet joint interventions.
Lumbar Selective Nerve Root Injection
Although ultrasound-guided cervical selective nerve root injection is feasible and can achieve similar outcome as fluoroscopic-guided injection, such technique is not amendable at the lumbar level. The depth of the lumbar spinal nerve roots renders the visualization challenging. At this depth, it is also difficult to visualize the needle and injectate spread. Few practitioners perform ultrasound-guided lumbar selective nerve root injections. Real-time fluoroscopy and contrast injection with digital subtraction remains the current standard of care [15].
Caudal Epidural Injection
Anatomy
The S1–S5 sacral vertebrae fuse into the sacrum; the three vestige coccygeal vertebrae fuse into the coccyx. The lower portion of sacrum and coccyx is open at the posterior midline. This bony defect is termed the sacral hiatus and is covered by the sacrococcygeal ligament. The hiatus is bounded laterally by the sacral cornua, and the floor is composed of the posterior aspect of the sacrum. The lumbar epidural space continues as the caudal epidural space, which can be accessed via the sacral hiatus [31, 32]. Chen et al. [33] described the first sonography of the caudal structures relevant to caudal epidural needle placement.
Patient Position
Patient is placed in a prone position, similar to fluoroscopic-guided caudal epidural injections. A linear high-frequency transducer can be used for this application. A low-frequency curvilinear transducer may be needed for obese patients.
Approach
The transducer was first placed transversely at the midline to obtain the sonographic transverse view of the sacral hiatus. The two hyperechoic reversed U-shaped structures are the two bony prominences of sacral cornua. Between the two cornua, there are two hyper echoic band-like structures. The band-like structure on top is the sacrococcygeal ligament. The band-like structure at the bottom is the dorsal bony surface of the sacrum (Fig. 28.17). The transducer is then rotated 90 degrees and rested in between the two sacral cornua to obtain the longitudinal view of the sacral hiatus (Fig. 28.18). A 22-gauge caudal epidural needle is inserted and advanced under the sonographic longitudinal view of the sacral hiatus. A “pop” is usually felt as the sacrococcygeal ligament is penetrated. As the caudal epidural needle pierces through the sacrococcygeal ligament, the portion of the needle inside the caudal epidural space is no longer observed [33]. In a sense, this technique is not a “true” direct visualization, although ultrasound is used to guide the needle placement. Due to the inability to visualize the needle after it enters the sacral canal, it is difficult to assess intravascular injection with this technique. Because of the rich vascularity in the caudal epidural space, confirmation with contrast dye spread under fluoroscopy is recommended to rule out intravascular injection.
Caudal epidural space. The transducer is placed transversely at the midline to obtain the transverse view of the sacral hiatus. The two hyper echoic reversed U-shaped structures are the two bony prominences of sacral cornua. Between the two cornua, there are two hyper echoic band-like structures. The band-like structure on top is the sacrococcygeal ligament. The band-like structure at the bottom is the dorsal bony surface of the sacrum
Sacroiliac Joint Injection
Anatomy
The SI joint is a wedge-shaped diarthrodial joint composed of an inferior cartilaginous joint that contains a joint capsule, synovial lining, and synovial fluid and an upper fibrous articulation [34]. In those cases refractory to conservative treatment, local treatment of the SI joint through intra-articular corticosteroid injection has provided diagnostic value and clinical improvement. Because of its complex anatomical structure, the SI joint injection can be difficult to enter with a needle [35].
Patient Position
Patient is placed in a prone position. A linear transducer (8–12 Hz) is placed transversely at the lower end of the sacrum to obtain a short-axis view. A low-frequency curvilinear transducer may be needed for obese patients.
Approach
The transducer is placed transversely over the lower sacrum at the level of the sacral hiatus. First, identify the lateral edge of the sacrum by slowly moving the transducer laterally. The transducer is then moved cranially following the edge of sacrum until the bony contour of the ileum comes in view. The cleft between the ileum and the lateral sacral edge represents the sacroiliac joint [36, 37]. A 22-gauge needle is then inserted at the medial end of the transducer and advanced from medial to lateral under direct vision in-plane with the US beam until it enters the joint (Fig. 28.19). The major limitation of the approach is the inability to visualize the needle and the injectate once the needle enters below ileum. It is difficult to assess periarticular versus intra-articular injectate spread. In a sense, this technique is not a “true” direct visualization, although ultrasound is used to guide the needle placement.
Sacroiliac joint injection. The transducer is placed transversely over the lower sacrum at the level of the sacral hiatus. First, identify the lateral edge of the sacrum by slowly moving the transducer laterally. The transducer is then moved cranially following the edge of sacrum until the bony contour of the ileum comes in view. The cleft between the ileum and the lateral sacral edge represents the sacroiliac joint. A 22-gauge needle is then inserted at the medial end of the transducer and advanced from medial to lateral under direct vision in-plane with the ultrasound beam until it enters the joint
Outcome Study
Pekkafahli et al. [37] reported a feasibility and effectiveness study of ultrasound-guided intra-articular SI joint injection with fluoroscopic validation in 34 patients with sacroiliitis, 26 patients with bilateral disease, and 8 patients with unilateral disease. The synovial portion of these SI joints was injected under ultrasound guidance, resulting in 46 (76.7%) successful injections and 14 (23.3%) missed injections. The authors noted that successful intra-articular injection rate was 60% for the first 30 injections with improvement to 93.5% in the last 30 injections, suggesting a steep learning curve of this technique.
References
Andersson GB. Epidemiological features of chronic low-back pain. Lancet (London, England). 1999;354(9178):581–5.
Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. 2007;25(2):353–71.
Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12(4):E35–70.
Manchikanti L, Falco FJ, Singh V, Pampati V, Parr AT, Benyamin RM, et al. Utilization of interventional techniques in managing chronic pain in the Medicare population: analysis of growth patterns from 2000 to 2011. Pain Physician. 2012;15(6):E969–82.
Iannuccilli JD, Prince EA, Soares GM. Interventional spine procedures for management of chronic low back pain—a primer. Semin Interv Radiol. 2013;30(3):307–17.
Narouze S. Ultrasonography in pain medicine: a sneak peak at the future. Pain Pract. 2008;8(4):223–5.
Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009;34(4):343–8.
Choi DH, Jung HG, Lee JH, Park JH, Choi YS. Effectiveness of Doppler image of the vertebral artery as an anatomical landmark for identification of ultrasound-guided target level in cervical spine. Asian Spine J. 2015;9(5):683–8.
Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skelet Radiol. 2013;42(1):69–78.
Yoganandan N, Knowles SA, Maiman DJ, Pintar FA. Anatomic study of the morphology of human cervical facet joint. Spine. 2003;28(20):2317–23.
Pal GP, Routal RV. The orientation of the articular facets of the zygapophyseal joints at the cervical and upper thoracic region. J Anat. 2001;198(Pt 4):431–41.
Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine. 1982;7(4):319–30.
Freire V, Grabs D, Lepage-Saucier M, Moser TP. Ultrasound-guided cervical facet joint injections: a viable substitution for fluoroscopy-guided injections? J Ultrasound Med. 2016;35(6):1253–8.
Galiano K, Obwegeser AA, Bodner G, Freund MC, Gruber H, Maurer H, et al. Ultrasound-guided facet joint injections in the middle to lower cervical spine: a CT-controlled sonoanatomic study. Clin J Pain. 2006;22(6):538–43.
Narouze S, Peng PW. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures. Part II: axial structures. Reg Anesth Pain Med. 2010;35(4):386–96.
Obernauer J, Galiano K, Gruber H, Bale R, Obwegeser AA, Schatzer R, et al. Ultrasound-guided versus computed tomography-controlled facet joint injections in the middle and lower cervical spine: a prospective randomized clinical trial. Med Ultrason. 2013;15(1):10–5.
Hayase J, Patel J, Narayan SM, Krummen DE. Percutaneous stellate ganglion block suppressing VT and VF in a patient refractory to VT ablation. J Cardiovasc Electrophysiol. 2013;24(8):926.
Rajesh MC, Deepa KV, Ramdas EK. Stellate ganglion block as rescue therapy in refractory ventricular tachycardia. Anesth Essays Res. 2017;11(1):266–7.
Gadhinglajkar S, Sreedhar R, Unnikrishnan M, Namboodiri N. Electrical storm: role of stellate ganglion blockade and anesthetic implications of left cardiac sympathetic denervation. Indian J Anaesth. 2013;57(4):397–400.
Nademanee K, Taylor R, Bailey WE, Rieders DE, Kosar EM. Treating electrical storm : sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation. 2000;102(7):742–7.
Guirguis M. Stellate ganglion block for the treatment of hot flashes in patients with breast cancer: a literature review. Ochsner J. 2015 Summer;15(2):162–9.
Haest K, Kumar A, Van Calster B, Leunen K, Smeets A, Amant F, et al. Stellate ganglion block for the management of hot flashes and sleep disturbances in breast cancer survivors: an uncontrolled experimental study with 24 weeks of follow-up. Ann Oncol. 2012;23(6):1449–54.
Walega DR, Rubin LH, Banuvar S, Shulman LP, Maki PM. Effects of stellate ganglion block on vasomotor symptoms: findings from a randomized controlled clinical trial in postmenopausal women. Menopause. 2014;21(8):807–14.
Lipov E, Ritchie EC. A review of the use of stellate ganglion block in the treatment of PTSD. Curr Psychiatry Rep. 2015;17(8):599.
Lynch JH, Mulvaney SW, Kim EH, de Leeuw JB, Schroeder MJ, Kane SF. Effect of stellate ganglion block on specific symptom clusters for treatment of post-traumatic stress disorder. Mil Med. 2016;181(9):1135–41.
Gofeld M, Bhatia A, Abbas S, Ganapathy S, Johnson M. Development and validation of a new technique for ultrasound-guided stellate ganglion block. Reg Anesth Pain Med. 2009;34(5):475–9.
Bogduk N. The innervation of the lumbar spine. Spine. 1983;8(3):286–93.
Bogduk N. The lumbar mamillo--accessory ligament. Its anatomical and neurosurgical significance. Spine. 1981;6(2):162–7.
Greher M, Scharbert G, Kamolz LP, Beck H, Gustorff B, Kirchmair L, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004;100(5):1242–8.
Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med. 2007;32(4):317–22.
Sekiguchi M, Yabuki S, Satoh K, Kikuchi S. An anatomic study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain. 2004;20(1):51–4.
Senoglu N, Senoglu M, Oksuz H, Gumusalan Y, Yuksel KZ, Zencirci B, et al. Landmarks of the sacral hiatus for caudal epidural block: an anatomical study. Br J Anaesth. 2005;95(5):692–5.
Chen CP, Tang SF, Hsu TC, Tsai WC, Liu HP, Chen MJ, et al. Ultrasound guidance in caudal epidural needle placement. Anesthesiology. 2004;101(1):181–4.
Kennedy DJ, Shokat M, Visco CJ. Sacroiliac joint and lumbar zygapophysial joint corticosteroid injections. Phys Med Rehabil Clin N Am. 2010;21(4):835–42.
Chen CP, Lew HL, Tsai WC, Hung YT, Hsu CC. Ultrasound-guided injection techniques for the low back and hip joint. Am J Phys Med Rehabil. 2011;90(10):860–7.
Harmon D, O'Sullivan M. Ultrasound-guided sacroiliac joint injection technique. Pain Physician. 2008;11(4):543–7.
Pekkafahli MZ, Kiralp MZ, Basekim CC, Silit E, Mutlu H, Ozturk E, et al. Sacroiliac joint injections performed with sonographic guidance. J Ultrasound Med. 2003;22(6):553–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Zhang, Y., Wu, B., Jin, P. (2020). Ultrasound-Guided Spinal Procedures. In: Mao, J. (eds) Spine Pain Care. Springer, Cham. https://doi.org/10.1007/978-3-030-27447-4_28
Download citation
DOI: https://doi.org/10.1007/978-3-030-27447-4_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-27446-7
Online ISBN: 978-3-030-27447-4
eBook Packages: MedicineMedicine (R0)