Abstract
Post-intensive care syndrome (PICS) is defined as newly recognized or worsening impairment in one or more of the following domains after critical illness: cognitive function, mental health, and physical function. These impairments frequently persist and can impact health-related quality of life after critical illness. In this chapter, we provide an illustrative case, and then we detail the clinical manifestations, diagnosis, and prevention and management strategies related to PICS. Last, we explore controversial aspects of PICS management that require further study.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Case Presentation
A 60 year-old man with a history of tobacco use and diabetes mellitus was admitted to the hospital with community acquired pneumonia. His course was complicated by hypoxemic respiratory failure requiring 5 days of mechanical ventilation in the Intensive Care Unit (ICU). After 13 days in the hospital, including 5 days of delirium, he was discharged to a skilled care facility. Upon returning home to live with his wife several weeks later, he described a frequent fear that his breathing will worsen and that he may have to return to the hospital. He kept a bag of his possessions ready for an emergency return to the hospital. His wife reported that his thinking “isn’t quite the same” as prior to the acute illness. He slept on the first floor as he had difficulty climbing the flight of stairs to his bedroom. He also reported developing depression secondary to his dependence on others’ for his activities of daily living and his inability to return to work as an accountant.
Question
Which features are characteristic of the Post-Intensive Care Syndrome?
Answer
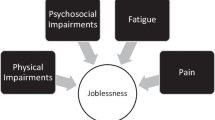
The Post-Intensive Care Syndrome (PICS) describes a constellation of symptoms, which includes impairment in neuropsychological and physical well being that occurs following an episode of critical illness [1, 2].
This recently recognized entity lies at the core of critical care survivorship, and is common, with new impairment in one or more PICS domains occurring in 64% and 56% of survivors 3 and 12 months after hospital discharge, respectively [3]. Patients who have experienced shock, respiratory failure, and prolonged sedation and mechanical ventilation are most at risk for development of PICS. Furthermore, pre-existing impairment in one or more of these domains may worsen after critical illness, a fact that warrants obtaining a history that captures physical function, mental health and cognitive function pre-illness. A longitudinal, coordinated effort is required to mitigate the risk of PICS development and rehabilitate new or more severe impairments (Table 109.1).
Principles of Management
Diagnosis
Survivors of critical i llness are at risk for PICS development, in particular those who experience shock and respiratory failure requiring mechanical ventilation. Risk factors associated with long-term physical and/or neuropsychological impairment include sepsis, acute respiratory distress syndrome (ARDS) , multi-system organ failure, prolonged ICU length of stay, duration of delirium, and glucose dysregulation [2, 7,8,9,10,11]. Corticosteroids have been implicated in ICU-acquired weakness, yet appear to have a protective effect in terms of PTSD [12].
Physical and neuropsychological impairment should be screened for at the time of hospital discharge to guide the procurement of post-acute care services (Table 109.2). Physical impairment is common following critical illness, can be measured using a standardized scale, and frequently contributes to the need for skilled care or acute rehabilitation facility placement. Several validated options exist to examine functional status, and specific areas of functional abilities, clinically. Cognitive impairment is an under-recognized consequence of critical illness. In a prospective study of survivors of shock and respiratory failure, Pandharipande et al. revealed that 40% of survivors performed at a level consistent with moderate traumatic brain injury at 3 months, 26% performed at a level consistent with mild Alzheimer’s disease, and these impairments frequently persisted [10]. Given its prevalence, providers should screen for cognitive impairment in ICU survivors w ith suspected PICS. A number of validated screening tools exist to identify cognitive impairment, including the Mini Mental Status Exam, the Mini-Cog, and the Montreal Cognitive Assessment (MoCA) . As a simple, highly sensitive, and validated test, the MoCA is arguably the best screening tool to detect mild cognitive impairment in ICU survivors [4]. Psychiatric illness seen in PICS manifests as symptoms of anxiety, depression, or post-traumatic stress disorder (PTSD ) [16].
Prevention and Rehabilitation
A growing body of literature supports the use of the “ABCDEF” bundle as a potential means to mitigate the risk of PICS [17]. The components of the ABCDE bundle include the coordination of sedation minimization and standardized ventilator weaning [18], delirium monitoring, prevention, and management, and early occupational and physical therapy [19]. When coupled with family engagement and empowerment, the bundle is transformed to the ABCDEF bundle. The benefits of an ABCDE bundle include reduced duration of delirium, reduced incidence of ventilator-associated events, increased ventilator-free days, and improved functional outcomes at discharge with increased likelihood of return to functional independence [18,19,20,21,22].
Components of the ABCDEF Bundle
A Recommended Strategy to Mitigate the Risk of Post-intensive Care Syndrome
Assess, Prevent , and Manage Pain
-
Daily asse ssment with validated scales, such as the behavioral pain scale
-
Prevention and management with goal-directed treatment for pain
Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT)
-
Daily safety screen
-
Daily sedation interruption and/or minimization of sedation use to target
-
Use of sedation scales in goal-directed delivery of medications
-
Daily ventilator weaning attempt
Choice of Analgesia and Sedation
-
Choice of agent and delivery modality, continuous versus intermittent
Delirium: Assess, Prevent, and Manage
-
Daily assessment in all ICU patients
-
Avoidance or minimization of medications that exacerbated delirium
-
Active management with non-pharmacologic and appropriate pharmacologic treatment to facilitate patient safety
Early Mobility and Exercise
-
Daily exercise regimens, including ambulation as tolerated
Family Engagement and Empowerment
-
Engage and communicate with families on rounds as active participants in patient care
-
Facilitate family participation with care tasks in the ICU (e.g. cleaning, feeding)
To complemen t the ABCDEF bundle, an effective strategy to reduce psychological distress in survivors is the use of an ICU diary [23]. The ICU diary has been shown to reduce post-ICU PTSD symptoms. Used widely throughout Europe (www.icu-diary.org), and more recently in several centers in the United States, an ICU diary is a notebook within which physicians, nurses, family members, and patient visitors can record, in patient-friendly language, information about the patient’s hospital course and messages from friends and family. The ICU diary may also include pictures of the patient during the course of their illness. Post-discharge, patients review the content of the diary with a health care provider as a strategy to fill gaps in their memory regarding the hospitalization and to realign delusional memories with an accurate depiction of the illness narrative. Beyond the positive effect that the ICU diary can have on the patient’s psychological condition, its use is now recommended in family-centered care guidelines [24] as it also appears beneficial to family members [25]. Because it is increasingly recognized that family members of survivors also experience lasting psychological effects, known as Post-Intensive Care Syndrome-Family (PICS-F) [1], the ability to mitigate long-term psycho logical distres s in caregivers is an important one.
Evidence Contour
Effective strategies for use in the ICU and post-discharge are urgently needed to reduce the burden of PICS.
ICU Follow Up Clinic
While conceptually appe aling, the benefits of an ICU follow-up clinic have yet to be demonstrated [26]. Following discharge from the ICU, primary care physicians were historically responsible for all follow-up care. Increasingly, however, ICU follow-up clinics staffed by pulmonary and critical care specialists are being established to screen for and address symptoms related to PICS. These specialized clinics employ a multidisciplinary approach with extensive care coordination between physical and occupational therapists, psychologist and psychiatrists, physical medicine and rehabilitation physicians, pulmonary physicians and neurologists. Given the resources required to staff such a clinic, systematic research is required to identify the optimal staffing structure and processes that lead to better patient-centered outcomes.
In the absence of compelling data regarding the optimal approach to longitudinally follow survivors after critical illness, the following “best practice” principles can be applied. First, to address the informational needs of survivors and their caregivers [27], it is critical to increase awareness of PICS so as to inform providers of the anticipated challenges faced by many patients after a critical illness. Second, this knowledge should facilitate discussions between health care providers and the patient and their family regarding what they may encounter following discharge from an ICU. The patient described in the above case may have followed up in an intensive care follow-up clinic or with his primary care physician. Regardless, during clinic visits, a manual to guide and chart the progress made during recovery should be developed and consultations placed with experts to attend to the symptoms and impairments identified (e.g., physical and occupational therapy, psychologists and/or psychiatrists, sleep disturbances, etc.) (Table 109.1).
Peer support, either alone o r in concert with a post-ICU clinic, has emerged as a novel solution with potential benefit [28, 29]. Conceptually, drawn from its utility in other conditions, peer support for survivors of critical illness is the “process of providing empathy, offering advice, and sharing stories between Intensive Care Unit survivors. It is founded on the principles that both taking and giving support can be healing, if done with mutual respect” [28]. Through the Society of Critical Care Medicine’s Thrive initiative, launched in 2015, an international collaborative of post-ICU clinics and peer support programs have been implemented to identify best pr actices for these novel models of care delivery [30].
Cognitive and Physical Rehabilitation
The potential for cognitive and physical rehabilitation as a means to improve the lives of survivors of critical illness exists, yet requires further study. In a small randomized trial of ICU survivors with cognitive or physical impairment at discharge, subjects randomized to receive cognitive and physical rehabilitation in their homes experienced improved executive function at three month follow-up compared to control subjects [31]. More proximally, cognitive rehabilitation initiated in the ICU appears to be feasible [32]. In addition to timely referral to rehabilitation experts, strategies during the ICU stay and beyond should consider incorporating cognitive exercise, given the potential for neural plasticity, and coping and compensation strategies (e.g. memory aids) as means to potentially prevent and remediate neuropsychological impairment. Last, given the relationship between physical and cognitive function [33, 34], physical therapy has the potential to be the most effective means to preserve cognitive function and/or rehabilitate cognitive impairment.
Because long-term impairment may be challenging to effectively rehabilitate, urgent investigation is also needed to understand how ICU practice can impact long-term health. For example, traditional ventilator strategies in ARDS protocolize oxygenation targets far below normal levels. Because hypoxemia has been associated with long-term cognitive impairment [8], it is plausible that targeting normoxemia in ARDS could result in improved long-term outcomes [35]. Through careful design of future clinical trials, the opportunity exists to better understand the long-term effects of critical care interventions so as to optimize both short- an d long-term outcomes and reduce the burden of PICS.
References
Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–9.
Mikkelsen ME, Netzer G, Iwashyna TJ. Post-intensive care syndrome (PICS) and post-intensive care syndrome—family (PICS-F). In: UpToDate, Basow DS, editors. UpToDate. Waltham;2014.
Marra A, Pandharipande PP, Girard TD, et al. Co-occurrence of post-intensive care syndrome problems among 406 survivors of critical illness. Crit Care Med. 2018;46(9):1393–401.
Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Weiss DS, Marmar CR, Wilson JP, et al. The impact of event scale-revised. In: Assessing Psychological Trauma and PTSD: a practitioner’s handbook. New York: Guilford Press; 1997. p. 399–411.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94.
Mikkelsen ME, Christie JD, Lanken PN, et al. The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med. 2012;185(12):1307–15.
Hopkins RO, Suchyta MR, Snow GL, et al. Blood glucose dysregulation and cognitive outcome in ARDS survivors. Brain Inj. 2010;24(12):1478.
Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–16.
Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, Jones RN. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–9.
Schelling G, Stoll C, Kapfhammer HP, et al. The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder and health-related quality of life in survivors. Crit Care Med. 1999;27(12):2678–83.
Katz S. Assessing self-maintenance: activities of daily living, mobility and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–6.
Kleyweg RP, van der Meche FG, Schmitz PI. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barre syndrome. Muscle Nerve. 1991;14:1103–9.
Bohannon RW. Reference values for the Timed Up and Go Test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29(2):64–8.
Jackson JC, Pandharipande PP, Girard TD, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369–79.
Pandharipande P, Banerjee A, McGrane S, Ely EW. Liberation and animation for ventilated ICU patients: the ABCDE bundle for the back-end of critical care. Crit Care. 2010;14(3):157.
Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet. 2008;371(9607):126–34.
Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized, controlled trial. Lancet. 2009;373:1874–82.
Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42(5):1024–36.
Klompas M, Anderson D, Trick W, et al. The preventability of ventilator-associated events: the CDC Prevention Epicenters’ Wake Up and Breathe Collaborative. Am J Respir Crit Care Med. 2015;191:292–301. Epub Nov 4
Calvo-Ayala E, Khan BA, Farber MO, et al. Interventions to improve the physical function of ICU survivors: a systematic review. Chest. 2013;144(5):1469–80.
Mehlhorn J, Freytag A, Schmidt K, et al. Rehabilitation interventions for postintensive care syndrome: a systematic review. Crit Care Med. 2014;42(5):1263–71.
Davidson J, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103–28.
Garrouste-Orgeas M, Coquet I, Perier A, et al. Impact of an intensive care unit diary on psychological distress in patients and relatives. Crit Care Med. 2012;40:2033–40.
Jensen JF, Thomsen T, Overgaard D, et al. Impact of follow-up consultations for ICU survivors on post-ICU syndrome: a systematic review and meta-analysis. Intensive Care Med. 2015;41:763–75.
Lee CM, Herridge MS, Matte A, et al. Education and support needs during recovery in acute respiratory distress syndrome. Crit Care. 2009;13:R153.
Mikkelsen ME, Jackson C, Hopkins RO, et al. Peer support as a novel strategy to mitigate post intensive care syndrome. AACN Adv Crit Care. 2016;27(2):221–9.
Haines KJB, Beesley SJ, Hopkins R, et al. Peer support in critical care: a systematic review. Crit Care Med. 2018;46(9):1522–31.
McPeake J, Hirshberg E, Christie L, et al. Models of peer support to remediate post-intensive care syndrome: a report developed by the SCCM international peer support collaborative (THRIVE). Crit Care Med. 2019;47(1):e21–e27.
Jackson JC, Ely EW, et al. Cognitive and physical rehabilitation of intensive care unit survivors: results of the RETURN randomized controlled pilot investigation. Crit Care Med. 2012;40(4):1088–197.
Brummel NE, Girard TD, Ely EW, et al. Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: the Activity and Cognitive Therapy in ICU (ACT-ICU) trial. Intensive Care Med. 2014;40(3):370–9.
Hopkins RO, Suchyta MR, Farrer TJ, Needham D. Improving post-intensive care unit neuropsychiatric outcomes: understanding cognitive effects of physical activity. Am J Respir Crit Care Med. 2012;186(12):1220–8.
Cohen D, Anderson B, Christie JD, et al. Cognitive function, mental health, and health-related quality of life after lung transplantation. Ann Am Thorac Soc. 2014;11(4):522–30.
Mikkelsen ME, Anderson B, Christie JD, et al. Can we optimize long-term outcomes in acute respiratory distress syndrome by targeting normoxemia? Ann Am Thorac Soc. 2014;11(4):613–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Maley, J.H., Mikkelsen, M.E. (2020). The Post-Intensive Care Syndrome. In: Hyzy, R.C., McSparron, J. (eds) Evidence-Based Critical Care. Springer, Cham. https://doi.org/10.1007/978-3-030-26710-0_109
Download citation
DOI: https://doi.org/10.1007/978-3-030-26710-0_109
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-26709-4
Online ISBN: 978-3-030-26710-0
eBook Packages: MedicineMedicine (R0)