Abstract
McArdle disease is a glycogen storage myopathy which is caused by mutations in the PYGM gene with resultant myophosphorylase deficiency. Patients with McArdle disease typically present with exercise intolerance and recurrent rhabdomyolysis. These patients may also manifest fixed proximal limb weakness and persistent CK elevation. Muscle biopsy is useful to differentiate McArdle disease from other metabolic myopathies, such as other glycogen storage myopathies, lipid storage myopathies, and mitochondrial myopathies, to direct genetic testing. Here we present a patient with McArdle disease who was initially misdiagnosed with inflammatory myopathy and was unnecessarily exposed to immunosuppressive therapies. A correct diagnosis was achieved by a muscle biopsy, which led to appropriate management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
History
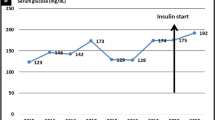
A 51-year-old Hispanic woman started to run 2–3 miles a day and 5 days a week when she was in high school. At the end of high school, the running became difficult as she would develop intense leg muscle pain, cramps, and fatigue which required frequent rest. She also noticed dark-color urine several times triggered by running at age 20s and 30s. She stopped running regularly at late 30s. She usually developed annoying muscle pain, cramps, and fatigue in the legs shortly after running. She had to slow down or stop for a few minutes to get the symptoms relieved. She also developed mild difficulty climbing stairs and uncomfortable heaviness feeling in her arms when carrying grocery bags at age 40s. She saw a local neurologist who found persistently elevated serum creatine kinase (CK) level in a range of 300s to 5,000s U/L. In one occasion, CK went up to 21,000 U/L when she had tea-color urine after jogging for 2 miles. She underwent a left quadriceps muscle biopsy with no definitive diagnosis. She was suspected to have an inflammatory myopathy. She had been treated with Prednisone, methotrexate, and Cytoxan for 2–1/2 years with no improvement. Her muscle pain and cramps as well as the degree of CK elevation correlated with her physical activity but not the treatment. She discontinued all the immunosuppressive agents 3 years prior to the presentation with no change of her symptoms of exercise intolerance. Her leg weakness, however, had been slowly progressed. She came to our clinic for a second opinion. Her birth history and developmental history were unremarkable. Her past medical history was significant for hypothyroidism, for which she took levothyroxine. Her family history was negative for a muscle disease. There was no consanguinity in her parents. She did not drink alcohol, smoke cigarettes, or abuse illicit drugs.
Physical Examination
General examination was unremarkable. Neurologic examination showed intact cranial nerve functions with no facial, ocular, or bulbar weakness. Motor examination revealed normal muscle tone and bulk, and mild weakness in the hip flexors (MRC 4/5). She could get up from a chair without using her hands to push but with difficulty. Sensation and coordination were normal. Deep tendon reflexes were 2+ throughout. Toes were downgoing bilaterally. Her gait was normal, including heel, toe, and tandem walking.
Investigations
Serum CK level was mildly elevated at 830 U/L. CBC, comprehensive metabolic panel, TSH, and free T4 were all normal. Plasma lactate and pyruvate levels as well as acylcarnitine profile were also unremarkable. Nerve conduction study (NCS) was normal. Electromyography (EMG) showed a non-irritable myopathy with myopathic motor unit potentials seen in the proximal limb muscles and paraspinal muscles. Her prior muscle biopsy slides were reviewed, which showed very tiny specimen with remarkable freezing artefact, precluding adequate interpretation. There was no obvious inflammation. A right quadriceps muscle biopsy was performed.
Muscle Biopsy Findings
The right quadriceps muscle biopsy (Fig. 13.1) showed a vacuolar myopathy with many fibers containing subsarcolemmal vacuoles or blebs. These vacuoles were not red rimmed or autophagic with no acid phosphatase reactivity. Electron microscopy (EM) showed striking subsarcolemmal accumulations of glycogen granules, corresponding to the blebs seen under light microscopy. There were very few scattered polygonal atrophic fibers but no myofiber necrosis, degeneration, or regeneration. The findings are typical for a glycogen storage myopathy .
Additional Investigation After the Muscle Biopsy Diagnosis
A part of the patient’s muscle biopsy tissue was sent for myoglobinuria panel (biochemical analysis of enzyme activities involved in muscle energy metabolism, the deficiencies in which could cause recurrent rhabdomyolysis). It showed a reproducible and profound deficiency in myophosphorylase activity.
Final Diagnosis
Glycogen Storage Disease Type V (McArdle Disease)
Patient Follow-up
The test results were discussed with the patient . Due to the long distance, she preferred to be managed by her local physicians. She was recommended to obtain the PYGM gene test and genetic counseling. She was instructed to receive physical therapy, modify her exercise and diet, and take nutritional supplements.
Discussion
McArdle disease, also known as glycogen storage disease type V , is an autosomal recessive metabolic myopathy caused by mutations in the PYGM gene which encodes the muscle isoenzyme of glycogen phosphorylase (myophosphorylase) [1]. Myophosphorylase is one of the key enzymes involved in converting glycogen to glucose 1-phosphate (glycogenolysis) which enters the glycolytic pathways to produce the energy molecule ATP to support muscle activity. Deficiency in myophosphorylase causes abnormal glycogen accumulation and impaired energy metabolism in skeletal muscle.
Among the metabolic myopathies that are caused by the defects in carbohydrate metabolism, McArdle disease is the most common with an estimated prevalence of 1:100,000 in Dallas-Fort Worth of Texas [2] and 1:167,000 in Spain [3]. The usual symptom onset is in the first or second decade of life but it can vary. The clinical presentation of McArdle disease is heterogeneous. The majority of patients present with exercise intolerance, and they start to notice muscle symptoms when they become athletic at school ages. The common symptoms include myalgia, cramps, and fatigue in exercising muscles, which are usually developed a few minutes after isometric (e.g., carrying weights) or sustained aerobic exercise (e.g., jogging). The symptoms may improve after a brief rest or reducing the exercise intensity (second wind phenomenon). Recurrent rhabdomyolysis occurs in approximately 50% of the patients. These episodes may cause acute renal failure. Fixed proximal limb weakness can be detected in 11% of the patients, mostly in those above 40 years of age [3, 4].
The diagnosis of McArdle disease is often delayed due to the rarity and underrecognition of the disease. It can be misdiagnosed with inflammatory myopathy as seen in our case because of the persistent CK elevation and fixed proximal limb weakness. Misdiagnosis causes diagnostic delay in McArdle disease [5]. Making a correct diagnosis of McArdle disease at an early stage of the disease is important because patients can be managed appropriately to avoid unnecessary exposure to the side effects of immunosuppressive therapies.
Diagnostic evaluation of McArdle disease mainly includes serum CK, NCS/EMG, muscle biopsy, and gene test. Forearm non-ischemic test and cycle and walking test to detect the heart rate response to the second wind phenomenon may also be used to screen for McArdle disease [6, 7]. As exercise intolerance with an early age at onset is a common feature of metabolic myopathies which also include mitochondrial myopathies and lipid storage myopathies, one may also check serum lactate, pyruvate, carnitines, acylcarnitine profile, and urine organic acids during the initial evaluation. Resting serum CK is usually persistently elevated in McArdle disease. The CK elevation is mild or moderate at baseline and severe during the episodes of rhabdomyolysis. EMG may show myopathic changes but can be normal. Muscle biopsy is useful in evaluating a patient with a suspected metabolic myopathy. It can differentiate a glycogen storage myopathy from a lipid storage myopathy or a mitochondrial myopathy, as these individual metabolic myopathies have distinct pathological features. It can also rule out other chronic myopathies which can cause exercise intolerance and muscle weakness such as muscular dystrophy. The phosphorylase stain allows histochemical analysis of the myophosphorylase activity in muscle fibers to detect myophosphorylase deficiency. Myophosphorylase activity can also be measured by biochemical analysis using biopsied muscle tissue, and the diagnosis of McArdle disease can be established when the myophosphorylase enzyme activity is deficient. The PYGM gene test identifies specific mutations causing myophosphorylase deficiency. So far, 147 pathological mutations of the PYGM gene have been identified [8]. There is no genotype-phenotype correlation [9,10,11,12,13,14]. Some neurologists prefer genetic testing first; if negative, proceed with a muscle biopsy.
Muscle pathology of McArdle disease features the presence of subsarcolemmal vacuoles or blebs . These vacuoles are filled with glycogen granules, which may be striking on PAS stain (Fig. 13.2). Unlike lysosomal glycogen storage disease (e.g., Pompe disease), these vacuoles are not autophagic with no reactivity to acid phosphatase (see Fig. 13.2). EM allows ultrastructural visualization of glycogen granules accumulated in the subsarcolemmal areas corresponding to the blebs seen under light microscopy (see Fig. 13.1) [15]. Phosphorylase reactivity is completely absent in muscle fibers but often retain in the wall of blood vessels (see Fig. 13.2) as blood vessel smooth muscle contains a different phosphorylase isoenzyme. The finding is specific to McArdle disease as long as the biopsied muscle tissue contains endogenous glycogen. A positive control should be used to avoid false-negative results of the phosphorylase stain. Muscle fiber type proportion or size is not altered [16].
Muscle biopsy from another patient, a 14-year-old female, with a history of rhabdomyolysis and muscle pain. (a), H&E shows subtle subsarcolemmal vacuoles in an otherwise unremarkable muscle (arrows). These vacuoles are negative for acid phosphatase stain (b, arrows), but contain PAS-positive granules (c, arrows) that are diastase digestible. Phosphorylase reactivity is completely absent in myofibers but retained in the wall of blood vessels (d, arrows). (This figure is provided by Dr. Chunyu Cai)
Management of patients with McArdle disease consists of aerobic training, exercise and dietary modifications, and nutritional supplementation. The goal is to reduce exercise intolerance and to avoid rhabdomyolysis. Aerobic training is beneficial as it can improve fitness by improving cardiorespiratory capacity and increasing delivery of blood-born fuels without adverse events in patients with McArdle disease [17,18,19,20]. Intense isometric exercise (e.g., weight lifting) or maximal aerobic exercise (e.g., running, strenuous swimming, or cycling) should be avoided. As McArdle disease is caused by the defect in the breakdown of glycogen to generate glucose for glycolysis, rich carbohydrate diet (65% carbohydrates) and taking carbohydrates (glucose, fructose, or sucrose) right before exercise have been shown beneficial to reduce exercise intolerance [21,22,23]. Combining aerobic exercise training and carbohydrates ingestion before exercise has been advocated [24, 25]. Low-dose creatine monohydrate also appears beneficial [26,27,28]. Large-scale, double-blinded, and placebo-controlled studies are needed to confirm the efficacy of nutritional and pharmacological treatments. Such studies may be difficult to do because the disease is rare. Genetic counseling should be provided to every patient. These patients should also be instructed to recognize myoglobinuria (pigmenturia). They should go to a local emergency department when pigmenturia occurs to obtain acute treatment (intravenous hydration, etc.) to avoid acute renal failure.
Pearls
Clinical Pearls
-
1.
The clinical hallmark feature of McArdle disease is exercise intolerance with recurrent rhabdomyolysis triggered by strenuous exercise. The main differential diagnosis is the other metabolic myopathies such as lipid storage myopathies, mitochondrial myopathies, and other glycogen storage myopathies.
-
2.
Patients with McArdle disease may manifest fixed proximal limb weakness especially after age 40 years, persistent CK elevation, and myopathic changes on EMG.
-
3.
Recognition and early diagnosis of McArdle disease is important for initiating appropriate management and avoiding wrong diagnosis and treatment.
-
4.
Diagnostic evaluation of McArdle disease mainly includes serum CK, NCS/EMG, muscle biopsy, and gene test.
-
5.
Muscle biopsy is useful as it can differentiate McArdle disease from other glycogen storage myopathies, lipid storage myopathies, and mitochondrial myopathies to direct subsequent genetic testing. Myophosphorylase activity can be assessed by histochemical and biochemical analyses using muscle biopsy tissue. The diagnosis of McArdle disease can be established if myophosphorylase activity is absent.
-
6.
The PYGM gene test identifies specific mutations in patients with McArdle disease. There is no genotype-phenotype correlation.
-
7.
The current management of patients with McArdle disease consists of aerobic exercise training, dietary modifications, nutritional supplementation, and acute treatment of rhabdomyolysis when it occurs. Genetic counselling should be provided to every patient.
Pathology Pearls
-
1.
Muscle pathology of McArdle disease features the presence of subsarcolemmal vacuoles or blebs filled with excessive glycogen granules. These vacuoles are not autophagic with no reactivity to acid phosphatase. These vacuoles contain excessive PAS-positive granules that are diastase digestible.
-
2.
EM study is essential, which allows ultrastructural confirmation of subsarcolemmal accumulation of glycogen granules.
-
3.
Phosphorylase stain shows complete absence of reactivity in muscle fibers, but the reactivity often retains in the wall of intramuscular blood vessels. The finding is specific to McArdle disease as long as the biopsied muscle tissue contains endogenous glycogen. A positive control should be used to avoid false-negative results.
References
Schmid R, Mahler R. Chronic progressive myopathy with myoglobinuria: demonstration of a glycogenolytic defect in the muscle. J Clin Invest. 1959;38:2044–58.
Haller RG. Treatment of McArdle disease. Arch Neurol. 2000;57(7):923–4.
Lucia A, Ruiz JR, Santalla A, Nogales-Gadea G, Rubio JC, Garcia-Consuegra I, et al. Genotypic and phenotypic features of McArdle disease: insights from the Spanish national registry. J Neurol Neurosurg Psychiatry. 2012;83(3):322–8.
Nadaj-Pakleza AA, Vincitorio CM, Laforet P, Eymard B, Dion E, Teijeira S, et al. Permanent muscle weakness in McArdle disease. Muscle Nerve. 2009;40(3):350–7.
Scalco RS, Morrow JM, Booth S, Chatfield S, Godfrey R, Quinlivan R. Misdiagnosis is an important factor for diagnostic delay in McArdle disease. Neuromuscul Disord. 2017;27(9):852–5.
Vissing J, Haller RG. A diagnostic cycle test for McArdle’s disease. Ann Neurol. 2003;54(4):539–42.
Buckley JP, Quinlivan RM, Sim J, Eston RG, Short DS. Heart rate and perceived muscle pain responses to a functional walking test in McArdle disease. J Sports Sci. 2014;32(16):1561–9.
Nogales-Gadea G, Brull A, Santalla A, Andreu AL, Arenas J, Martin MA, et al. McArdle disease: update of reported mutations and polymorphisms in the PYGM gene. Hum Mutat. 2015;36(7):669–78.
Aquaron R, Berge-Lefranc JL, Pellissier JF, Montfort MF, Mayan M, Figarella-Branger D, et al. Molecular characterization of myophosphorylase deficiency (McArdle disease) in 34 patients from Southern France: identification of 10 new mutations. Absence of genotype-phenotype correlation. Neuromuscul Disord. 2007;17(3):235–41.
Bruno C, Cassandrini D, Martinuzzi A, Toscano A, Moggio M, Morandi L, et al. McArdle disease: the mutation spectrum of PYGM in a large Italian cohort. Hum Mutat. 2006;27(7):718.
Deschauer M, Morgenroth A, Joshi PR, Glaser D, Chinnery PF, Aasly J, et al. Analysis of spectrum and frequencies of mutations in McArdle disease. Identification of 13 novel mutations. J Neurol. 2007;254(6):797–802.
Martin MA, Rubio JC, Buchbinder J, Fernandez-Hojas R, del Hoyo P, Teijeira S, et al. Molecular heterogeneity of myophosphorylase deficiency (McArdle’s disease): a genotype-phenotype correlation study. Ann Neurol. 2001;50(5):574–81.
Vieitez I, Teijeira S, Fernandez JM, San Millan B, Miranda S, Ortolano S, et al. Molecular and clinical study of McArdle’s disease in a cohort of 123 European patients. Identification of 20 novel mutations. Neuromuscul Disord. 2011;21(12):817–23.
Santalla A, Nogales-Gadea G, Encinar AB, Vieitez I, Gonzalez-Quintana A, Serrano-Lorenzo P, et al. Genotypic and phenotypic features of all Spanish patients with McArdle disease: a 2016 update. BMC Genomics. 2017;18(Suppl 8):819.
Dubowitz V, Sewry CA, Oldfors A. Metablic myopathies I: glycogenoses and lysosomal myopathies. In: Muscle biopsy: a practical approach. 4th ed. Oxford: Saunders Elsevier; 2013. p. 423–45.
Henning F, Cunninghame CA, Martin MA, Rubio JC, Arenas J, Lucia A, et al. Muscle fiber type proportion and size is not altered in mcardle disease. Muscle Nerve. 2017;55(6):916–8.
Haller RG, Wyrick P, Taivassalo T, Vissing J. Aerobic conditioning: an effective therapy in McArdle’s disease. Ann Neurol. 2006;59(6):922–8.
Mate-Munoz JL, Moran M, Perez M, Chamorro-Vina C, Gomez-Gallego F, Santiago C, et al. Favorable responses to acute and chronic exercise in McArdle patients. Clin J Sport Med. 2007;17(4):297–303.
Quinlivan R, Vissing J, Hilton-Jones D, Buckley J. Physical training for McArdle disease. Cochrane Database Syst Rev. 2011;12:CD007931.
Ollivier K, Hogrel JY, Gomez-Merino D, Romero NB, Laforet P, Eymard B, et al. Exercise tolerance and daily life in McArdle’s disease. Muscle Nerve. 2005;31(5):637–41.
Andersen ST, Vissing J. Carbohydrate- and protein-rich diets in McArdle disease: effects on exercise capacity. J Neurol Neurosurg Psychiatry. 2008;79(12):1359–63.
Perez M, Mate-Munoz JL, Foster C, Rubio JC, Andreu AL, Martin MA, et al. Exercise capacity in a child with McArdle disease. J Child Neurol. 2007;22(7):880–2.
Vissing J, Haller RG. The effect of oral sucrose on exercise tolerance in patients with McArdle’s disease. N Engl J Med. 2003;349(26):2503–9.
Amato AA. Sweet success—a treatment for McArdle’s disease. N Engl J Med. 2003;349(26):2481–2.
Nogales-Gadea G, Santalla A, Ballester-Lopez A, Arenas J, Martin MA, Godfrey R, et al. Exercise and preexercise nutrition as treatment for McArdle disease. Med Sci Sports Exerc. 2016;48(4):673–9.
Quinlivan R, Beynon RJ, Martinuzzi A. Pharmacological and nutritional treatment for McArdle disease (Glycogen Storage Disease type V). Cochrane Database Syst Rev. 2008;2:CD003458.
Vorgerd M, Grehl T, Jager M, Muller K, Freitag G, Patzold T, et al. Creatine therapy in myophosphorylase deficiency (McArdle disease): a placebo-controlled crossover trial. Arch Neurol. 2000;57(7):956–63.
Vorgerd M, Zange J, Kley R, Grehl T, Husing A, Jager M, et al. Effect of high-dose creatine therapy on symptoms of exercise intolerance in McArdle disease: double-blind, placebo-controlled crossover study. Arch Neurol. 2002;59(1):97–101.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Zhou, L. (2020). A 51-Year-Old Woman with Long-Standing Exercise Intolerance. In: Zhou, L., Burns, D., Cai, C. (eds) A Case-Based Guide to Neuromuscular Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-25682-1_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-25682-1_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-25681-4
Online ISBN: 978-3-030-25682-1
eBook Packages: MedicineMedicine (R0)