Abstract
Many diagnostic imaging techniques—with and without ionizing radiations—such as panoramic radiography, plain radiographs, tomography, computed tomography (CT), and magnetic resonance imaging (MRI), have been proposed for the assessment of TMJ pathologies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
Panoramic (orthopantomogram—DPT: dental panoramic tomography) and plain radiographs may allow a good screening for gross degenerative or traumatic bony changes, but they give limited information because of the anatomy of the region, superimpositions of overlapping structures, and geometric distortion.
-
Conventional tomography and computed tomography (CT) overcome these diagnostic difficulties and they should be adopted for specific evaluation of TMJ osseous changes (i.e., fractures), identification of intra-articular calcifications (i.e., pseudogout arthritis), and for all conditions in which a large view of the maxilla is required with multiplanar and 3D reconstructions (i.e., craniofacial malformations).
-
Cone beam CT (CBCT) offers some advantages over multidetector computed tomography (MDCT), namely image accuracy, X-ray beam limitation, fast acquisition time, if a head and neck CT study is not required.
-
TMJ ultrasound has by now gained widespread acceptance in rheumatology and as a guiding tool in interventional procedures. Ultrasounds are becoming more common in preliminary evaluation of anterior disc dislocations but their capacity and capability of detecting medial, lateral, and posterior dislocations are yet to be confirmed.
Many diagnostic imaging techniques—with and without ionizing radiations—such as panoramic radiography , plain radiographs , tomography , computed tomography (CT), and magnetic resonance imaging (MRI), have been proposed for the assessment of TMJ pathologies.
Over the last 20 years, the study of the temporomandibular joint (TMJ) has mainly moved from radiographic and tomographic imaging to CT and MRI; however, general agreement about TMJ instrumental diagnosis still has to be reached.
While panoramic and plain radiographs allow the detection of gross degenerative or traumatic bony changes, they are often limited due to anatomy of the region, overlapping structures, and geometric distortion. Conventional tomography and the introduction of CT imaging helped overcome these diagnostic difficulties, but they do not have the potential to investigate discal and capsuloligamentous components of TMJ. This is why the advent of MRI marked an important step in the diagnostic evaluation of TMJ disorders.
Nevertheless, CT remains the first choice for specific evaluation of TMJ osseous changes (fractures, post-surgical evaluations), for intra-articular calcifications (synovial chondromatosis or metabolic arthritis), and for all conditions in which a large view of the maxillomandibular complex is required with multiplanar and 3D reconstructions (craniofacial malformations, hyperplasia of coronoid and styloid processes, tumors) (Honda et al. 2006; Huntjens et al. 2008; Farronato et al. 2010; Venturin et al. 2010; Meng et al. 2012; Ferreira et al. 2016).
CT can be performed as multislice computerized tomography (MSCT) or as cone beam computerized tomography (CBCT) . Cone beam CT (CBCT) was introduced as an alternative to MSCT and is now considered appropriate for a wide range of craniofacial indications. CBCT offers some advantages over MSCT , namely image accuracy, X-ray beam limitation, and fast acquisition time. European guidelines, which have been developed thanks to the SEDENTEXCT project, concluded that CBCT can be considered as an alternative to MSCT, as the radiation dose from CBCT is lower (Holdroyd and Gulson 2009; Radiation Protection 2011). As a consequence, in the last decade, the use of CBCT has increased in various dental specialties for the investigation of maxillofacial structures and this is why CBCT has emerged as a cost- and dose-effective imaging modality for the diagnostic assessment of the TMJ.
2.1 Radiographic Imaging
Several methods are available with conventional extra-oral X-ray equipment. Radiographic examination of the TMJ is possible with orthopantomograms, with/without planigraphy (TMJ-specific programs) and plain radiography.
In the past years, radiographic examination of the temporomandibular joint (TMJ) together with linear tomography were the only imaging modalities to investigate TMJ structures (cortical and trabecular architecture of bony structures) and structural changes (extent and progression of osseous changes) (Crow et al. 2005; Ferreira et al. 2016). Moreover, radiographic investigation of TMJ would provide some functional relations between the condyle , the articular tubercle, and the fossa (Ferreira et al. 2016). CBCT has widely replaced radiographic examination of the TMJ as it can overcome the diagnostic difficulties caused by the superimposition of contiguous anatomical structures. Nevertheless one should bear in mind that the effective dose for a TMJ CBCT may be 20–40 times the effective dose of TMJ radiography, depending on the irradiated volume (Holdroyd and Gulson 2009).
2.1.1 Orthopantomograms With or Without Planigraphy
Panoramic radiography can capture an overview of the maxillomandibular complex, it requires a low patient radiation dose and is quite easy to perform. This procedure may be a useful screening tool for differential diagnosis of odontogenic conditions which may mimic TMJ symptoms, and it can highlight gross bony changes in the condyle (as for arthritis in children), in articular morphology (i.e., asymmetries, condylar changes in size and shape) (Fig. 2.1a, b), and intra-articular calcification (Fig. 2.2a, b) (Crow et al. 2005; Ferreira et al. 2016).
Image formation in orthopantomograms follows the basic principles of linear tomography: the X-ray beam is emitted obliquely along the long axis of the condyle in a non-parallel manner, and causes superimpositions and variations in size of structures. It has to be considered that the medial condylar surface maintains a more posterior horizontal rotation with respect to the rear surface, as the condyle is angled between 15° and 33° in a sagittal plane (Fig. 2.3a–c). Moreover, in panoramic radiography, image formation also depends on the position of the TMJ within the image layer, because only a part of the condyle falls within the image layer and is visualized without distortions (Ladeira et al. 2015). Furthermore, projective overlapping (Fig. 2.4) of different anatomical structures can occur, especially in the region of the fossa and of the tubercle and this makes them often difficult to examine correctly, with the risk of inaccurate diagnosis (Crow et al. 2005; Mawani et al. 2005; Hintze et al. 2009; Ferreira et al. 2016). Therefore, it is generally agreed that the diagnostic pathology TMJ should not be solely based upon panoramic radiography (Hintze et al. 2009).
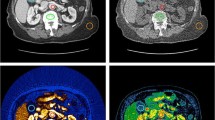
In (a) (Axial SE T1 image) and (b) (Coronal SE T2 image) give an understanding of how the medial and lateral pole project onto different points of the panoramic X-ray. In (c) the lateral pole is seen in the antero-inferior region of the condyle (*), whereas the medial pole lies in the postero-superior part (✕)
In addition to panoramic view, any modern device for panoramic radiography will include specific programs to obtain an anatomical overview of the TMJ (planigraphy Fig. 2.5a, b). Depending on the different available algorithms, multiple projections for each joint can be obtained on the same film, such as two projections in the sagittal plane (an open mouth and a closed mouth, respectively), documenting the relationship of the condyle in the articular fossa in maximum habitual intercuspation and at the end of excursion in maximum mouth opening. Following this procedure, images can be obtained without major projective overlapping and with a good visualization of the surrounding anatomical structures, such as the styloid process, the mastoid process, and the zygomatic arch. This method is useful to obtain an initial functional evaluation and any basic assessment regarding condyle size, presence of displaced fractures, or ankylosis (Epstein et al. 2001; Hintze et al. 2009; Ferreira et al. 2016).
2.1.2 Plain Radiography
Similarly to panoramic radiography , plain radiographs provide a global anatomical assessment of the condyle, the fossa, and the articular tubercle, but fail to provide an accurate evaluation of the TMJ, because of limitations due to structure superimposition and sometimes due to artifacts (for instance, those determined by patient movement) (Barghan et al. 2012).
The literature about this approach is quite outdated; however, in the past years, projections have been set to evaluate TMJ, for instance, using oblique lateral transcranial and Towne projections (Fig. 2.6a–c), but most authors would agree that projections used to evaluate TMJ disorders (i.e., transcranial, transpharyngeal, and transmaxillary) are not reliable from a diagnosis point of view (Lindvall et al. 1976). Furthermore, positioning of the patient can be complex, especially in the case of trauma . Nevertheless this imaging method is widely available and it can be useful for identifying coarse bone changes and displaced fractures of the condylar head and neck (Hintze et al. 2009; Ferreira et al. 2016; Caruso et al. 2017). Often this projection will not be carried out correctly, and the patient will need further assessment by means of a CT scan (Fig. 2.7a–c).
2.2 Tomography
Tomography used to be the most accurate imaging technique for TMJ evaluation. In most cases it was performed as lateral tomograms in the sagittal plane, although some authors reported that frontal tomograms could be useful as well (Fig. 2.8a–c) (Hintze et al. 2009).
This approach however proved limited in its reliability, and this imaging modality ended up being replaced by CBCT due to its higher accuracy in depicting condylar bony erosion (Honey et al. 2007).
2.3 Computed Tomography (CT)
2.3.1 Multislice Computed Tomography (MSCT)
Multislice computed tomography (MSCT) consists in a rotating gantry with an X-ray source and digital X-ray detectors, which are located directly opposite the X-ray source. During a CT scan, the patient lies on a bed that slowly moves through the gantry while the X-ray tube rotates around the patient (Fig. 2.9a, b). The radiation emitted is a narrow fan-shaped X-ray beam and it is typically emitted at 80–150 mA and 120 kVp (kilovoltage peak ) for the maxillofacial region. The emitted radiation passes through the patient and is picked up by the detector as transmitted radiation . The collected data are transmitted to a computer, and a tissue density map in Hounsfield Units (HU) is obtained. Data are represented by numbers in a matrix of pixel (usually 512 × 512 pixels). The fundamental picture element is the pixel, and every pixel is attributed a tissue density in HU . Every slice is divided in voxel (volumetric picture element), whose base has the pixel dimensions, while the voxel height is the thickness of the slice as set by the radiologist. The thickness of the tissue represented in each image slice can vary depending on the CT machine being used, but it usually ranges from less than 1 mm to a few millimeters. The simultaneous movement of patient and gantry allows to thoroughly cover a volume of interest. Image slices can either be displayed individually or stacked together by the computer to generate a multiplanar and 3D image of the explored volume.
2.3.2 Cone Beam Computed Tomography (CBCT)
In its early days, computed tomography of the TMJ was exclusively performed as multislice computed tomography (MSCT). However, in the years that followed the introduction of CBCT, an increased use of this imaging modality for evaluation of the jaws and the TMJ has been observed. This is because of some essential differences between CBCT and MSCT (Palconet et al. 2012; Ferreira et al. 2016; Caruso et al. 2017):
-
CBCT uses a three-dimensional cone-shaped X-ray beam instead of the collimated fan beam used in MSCT (Fig. 2.10). The patient’s head keeps still during the synchronous movement of both the X-ray tube and detector, and the patient may be either in orthostatic position or sitting. The tube detector system performs only one 360° (or 270°, sometimes 180°) rotation around the head of the patient with a constant beam angle. The acquisition lasts from 5 to 70 s depending on the amplitude of the region under examination.
-
A relevant difference between CBCT and MSCT is the choice of the field of view (FOV). In MSCT the FOV is substantially fixed due to the fan beam angle, achieved by adjustment of collimation. In CBCT the FOV is a cylindrical or spherical volume, because the cone-beam X-ray is coupled with a 2D extended digital array providing a wide area detector. A collimator restricts the beam to match the sensor size in order to focus on the anatomical region of interest. Thus CBCT has its FOV as a flexible volume and most CBCT units will scan small regions of a few centimeters; however, others can scan the entire craniofacial complex as well (Honda et al. 2006; Honey et al. 2007; Barghan et al. 2012). The best imaging quality is achieved using small FOVs (allowing to optimize spatial resolution depending on hardware and software with fixed matrix), this also leads to a significant decrease of radiation dose, proportional to the FOV voxel size. According to some authors the best imaging quality is obtained for 6- or 9-in. FOV with a significant decrease of radiation dose, proportional to the FOV voxel size (Librizzi et al. 2011). Depending on patient size, both TMJs can be evaluated with one 9-in. acquisition, while a 6-in. FOV needs 2 scans, hence doubling the exposition. The acquisition of two 6-in. FOV TMJ scans would allow the best image quality and detect small erosions , with a still limited X-ray exposition, compared to the 9- and 12-in. FOV. Small size FOVs allow good quality image with the same matrix. Matrix width is usually fixed (due to computation limits) and small FOVs allow to optimize spatial resolution depending on hardware and software.
-
As in CBCT the FOV is volumetric, the voxel is always isotropic (meaning that the voxel is a perfect cube, with the slice thickness equal to the base and the height of the pixel) and its side ranges from 0.075 to 0.400 mm per side. Image acquisition is performed during the X-ray tube movement at certain fixed degree intervals, producing single projection images, known as basis images. Basis images are similar to lateral teleradiography, each slightly offset from the other. Basis projection images are referred to as the projection data and are reconstructed into a 3D data set. As the voxel is isotropic, CBCT multiplanar reconstructions have high accuracy and are performed in orthogonal planes (axial, coronal, sagittal) or curvilinear planes. Panoramic images can be obtained and cross-sectional images perpendicular to the curve of the dental arch can be obtained. Additional dedicated software can be used to perform curved reconstructions along some complex anatomical structures, such as the mandibular nerve (Honey et al. 2007; Koyama et al. 2007).
-
Exposure parameters are also different in CBCT and in MSCT, being the milliampere (mA) setting very low (1–15 mA), while the peak kilovoltage (kVp) usually ranges from 85 to 120 kVp. Thus the absorbed dose is reduced and a significant reduction of artifacts is reached, especially those determined by X-ray beam hardening (e.g., as in the case of prostheses) (Honey et al. 2007; Barghan et al. 2012).
-
Because of the reduced milliamperage and FOV characteristics, the X-ray dose may be substantially smaller compared to MSCT for TMJ evaluation. Several studies confirm the reduced dose in CBCT and some authors focus on CBCT evaluation of the TMJ compared to MSCT examination: MSCT exhibited higher organ doses for all organs except the salivary glands and lymphatic nodes, with a 20% higher effective dose than CBCT (Hashimoto et al. 2003, 2007; Kadesjö et al. 2015). For bilateral TMJ evaluation, some authors suggested that the estimated effective dose using the optimized exposure parameters would be 92 mSv for a bilateral CBCT examination and 124 mSv for a MSCT; nonetheless, owing to the large range of reported effective doses and large technical differences between the CBCT models, dose comparison between CBCT and MSCT for TMJ diagnostics may be complex (Kadesjö et al. 2015). Existing data suggest that the most important issue to account for is dose optimization (i.e., suitable FOVs and optimized exposure parameters for various diagnostic tasks), rather than the choice of CT modality. The importance of dose exposure should not be overlooked also considering radio-sensitivity of organs and glands in the neck and head district. For instance, recent studies assessed absorbed ionizing radiation by thyroid gland using CBCT , reporting an average of phantom surface radiation dose at the thyroid gland of 0.48 mGy (Setti da Rocha et al. 2017). For dose reduction reasons CBCT operates at much lower mA setting than MDCT resulting in more quantum noise (inconsistent distribution of signal) resulting in grainier images. Increasing radiation dose (mA) reduces noise and may improve spatial resolution. Use of smaller voxel needs an increased amount of radiation to maintain good image quality.
-
No significant difference was found between CBCT and MSCT in detecting osseous abnormalities, erosion, and osteophytes (Honda et al. 2006; Zain-Alabdeen and Alsadhan 2012). On the other hand, it should be considered that, from a biological standpoint, CBCT is a quite expensive method when compared to conventional tomography and radiographs (the absorbed dose is 20–30 higher than the dose delivered during conventional radiography) (Holdroyd and Gulson 2009). Thus, some common and easy doubt may be solved by conventional tomography and radiographs.
In summary, CBCT has an acceptable accuracy for diagnosing osseous TMJ abnormalities with fairly high sensitivity and appears to be cost- and dose-effective. In most studies, high specificity is reported and the diagnostic accuracy of CBCT seems to be comparable with CT for TMJ diagnostics. CBCT was found to be better than conventional radiographic examinations as well as MRI in assessing the TMJ. However, it should be emphasized that the diagnostic information obtained is limited to the morphology of the osseous joint components, cortical bone integrity, and subcortical bone destruction/production. For evaluation of soft-tissue abnormalities, MRI is mandatory (Larheim et al. 2015).
2.4 Ultrasound (US)
TMJ ultrasound has by now gained widespread acceptance because of its acknowledged role in rheumatology and most importantly because of its importance as a guiding tool in interventional procedures (Levorova et al. 2015). US is becoming more common in preliminary evaluation of disc dislocations as it is easily available in most healthcare institutions, is non-invasive, and is readily carried out (Klatkiewicz et al. 2018). Encouraging results currently come from metanalyses reporting sensitivity and specificity between 70% and 85%, with better results in case of anterior disc displacement with reduction in maximum opening (Melis et al. 2007; Li et al. 2012; Dong et al. 2015; Klatkiewicz et al. 2018).
It is yet to be defined US capability of detecting medial, lateral, and posterior dislocations, and this is why further studies are needed and should be carried out with more accurate study procedures so as to assess US effective diagnostic accuracy in all disc dislocations (Li et al. 2012). Metanalyses reach then the conclusion that MRI is fundamental in case of any US finding that could potentially modify the therapeutic approach, or in case of disagreement between a clinical positive finding and a negative US (Li et al. 2012).
One more aspect which is to be standardized is the TMJ method of evaluation, as it is easy to understand that not only a static assessment is needed (closed and open mouth, in coronal, oblique, and axial planes), but also a dynamic orthostatic evaluation during the whole articular excursion (Klatkiewicz et al. 2018).
US oblique–coronal views are taken along the longitudinal axis of the condyle and ramus, whereas axial views are taken along an axis perpendicular to the previous one. These views will show the same anatomical structures that can be seen in a coronal MRI even though they are less comprehensive.
References
Barghan S, Tetradis S, Mallya S. Application of cone beam computed tomography for assessment of the temporomandibular joints. Aust Dent J. 2012;57:109–18. https://doi.org/10.1111/j.1834-7819.2011.01663.x.
Caruso S, Storti E, Nota A, Ehsani S, Gatto R. Temporomandibular joint anatomy assessed by CBCT images. Biomed Res Int. 2017;2017:1–10. https://doi.org/10.1155/2017/2916953.
Crow HC, Parks E, Campbell JH, Stucki DS, Daggy J. The utility of panoramic radiography in temporomandibular joint assessment. Dentomaxillofac Radiol. 2005;34:91–5. https://doi.org/10.1259/dmfr/24863557.
Dong Y, He S, Zhu L, Dong TY, Pan SS, Tang LJ, Zhu ZF. The diagnostic value of high resolution ultrasonography for the detection of anterior disc displacement of the temporomandibular joint: a meta-analysis employing the HSROC statistical model. Int J Oral Maxillofac Surg. 2015;44:852–8.
Epstein JB, Caldwell J, Black G. The utility of panoramic imaging of the temporomandibular joint in patients with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:236–9. https://doi.org/10.1067/moe.2001.114158.
Farronato G, Garagiola U, Carletti V, Cressoni P, Mercatali L, Farronato D. Change in condylar and mandibular morphology in juvenile idiopathic arthritis: cone beam volumetric imaging. Minerva Stomatol. 2010;59:519–34.
Ferreira LA, Grossmann E, Januzzi E, de Paula MV, Carvalho AC. Diagnosis of temporomandibular joint disorders: indication of imaging exams. Braz J Otorhinolaryngol. 2016;82:341–52. https://doi.org/10.1016/j.bjorl.2015.06.010.
Hashimoto K, Arai Y, Iwai K, Araki M, Kawashima S, Terakado M. A comparison of a new limited cone beam computed tomography machine for dental use with a multidetector row helical CT machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:371–7. https://doi.org/10.1067/moe.2003.120.
Hashimoto K, Kawashima S, Kameoka S, Akiyama Y, Honjoya T, Ejima KI, Sawada K. Comparison of image validity between cone beam computed tomography for dental use and multidetector row helical computed tomography. Dentomaxillofac Radiol. 2007;36:465–71. https://doi.org/10.1259/dmfr/22818643.
Hintze H, Wiese M, Wenzel A. Comparison of three radiographic methods for detection of morphological temporomandibular joint changes: panoramic, scanographic and tomographic examination. Dentomaxillofac Radiol. 2009;38:134–40. https://doi.org/10.1259/dmfr/31066378.
Holdroyd JR, Gulson AD. The radiation protection implication of the use of cone beam computed tomography (CBCT) in dentistry - what you need to know. Oxfordshire: Health Protection Agency; 2009. Available at www.bsdmfr.org.uk/wp-content/uploads/2014/12/hpaguidance.pdf.
Honda K, Larheim TA, Maruhashi K, Matsumoto K, Iwai K. Osseous abnormalities of the mandibular condyle: diagnostic reliability of cone beam computed tomography compared with helical computed tomography based on an autopsy material. Dentomaxillofac Radiol. 2006;35:152–7. https://doi.org/10.1259/dmfr/15831361.
Honey BO, Scarfe WC, Hilgers MJ, Klueber K, Silveira A, Haskell B, Farman A. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofac Orthop. 2007;132:429–38. https://doi.org/10.1016/j.ajodo.2005.10.032.
Huntjens E, Kiss G, Wouters C, Carels C. Condylar asymmetry in children with juvenile idiopathic arthritis assessed by cone-beam computed tomography. Eur J Orthod. 2008;30:545–51. https://doi.org/10.1093/ejo/cjn056.
Kadesjö N, Benchimol D, Falahat B, Näsström K, Shi XQ. Evaluation of the effective dose of cone beam CT and multislice CT for temporomandibular joint examinations at optimized exposure levels. Dentomaxillofac Radiol. 2015;44:20150041. https://doi.org/10.1259/dmfr.20150041.
Klatkiewicz T, Gawriołek K, Pobudek Radzikowska M, Czajka-Jakubowska A. Ultrasonography in the diagnosis of temporomandibular disorders: a meta-analysis. Med Sci Monit. 2018;24:812–7. https://doi.org/10.12659/MSM.908810.
Koyama J, Nishiyama H, Hayashi T. Follow-up study of condylar bony changes using helical computed tomography in patients with temporomandibular disorder. Dentomaxillofac Radiol. 2007;36:472–7. https://doi.org/10.1259/dmfr/28078357.
Ladeira DBS, Da Cruz AD, De Almeida SM. Digital panoramic radiography for diagnosis of the temporomandibular joint: CBCT as the gold standard. Original Research Imaginology. Braz Oral Res. 2015;29:1–7. https://doi.org/10.1590/1807-3107BOR-2015.
Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44:20140235. https://doi.org/10.1259/dmfr.20140235.
Levorova J, Machon V, Hirjak D, Foltan R. Ultrasound-guided injection into the lower joint space of the temporomandibular joint. Int J Oral Maxillofac Surg. 2015;44:491–2. https://doi.org/10.1016/j.ijom.2014.12.013.
Li C, Su N, Yang X, Yang X, Shi Z, Li L. Ultrasonography for detection of disc displacement of temporomandibular joint: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2012;70:1300–9. https://doi.org/10.1016/j.joms.2012.01.003.
Librizzi ZT, Tadinada AS, Valiyaparambil JV, Lurie AG, Mallya SM. Cone-beam computed tomography to detect erosions of the temporomandibular joint: effect of field of view and voxel size on diagnostic efficacy and effective dose. Am J Orthod Dentofac Orthop. 2011;140:e25–30.
Lindvall AM, Helkimo E, Hollender L, Carlsson GE. Radiographic examination of the temporomandibular joint. Dentomaxillofac Radiol. 1976;5:24–32.
Mawani F, Lam EW, Heo G, McKee I, Raboud DW, Major PW. Condylar shape analysis using panoramic radiography units and conventional tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:341–8. https://doi.org/10.1016/j.tripleo.2004.07.011.
Melis M, Secci S, Ceneviz C. Use of ultrasonography for the diagnosis of temporomandibular joint disorders: a review. Am J Dent. 2007;20:73–8.
Meng Q, Chen S, Long X, Cheng Y, Deng M, Cai H. The clinical and radiographic characteristics of condylar osteochondroma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:e66–74. https://doi.org/10.1016/j.oooo.2012.01.016.
Palconet G, Ludlow JB, Tyndall DA, Lim PF. Correlating cone beam computed tomography results with temporomandibular joint pain of osteoarthritic origin. Dentomaxillofac Radiol. 2012;41:126–30. https://doi.org/10.1259/dmfr/60489374.
Radiation protection: Cone Beam CT for Dental and Maxillofacial Radiology - Evidence Based Guidelines. Energy Protection Radiation n. 172. Directorate General for Energy, Unit D4-Radiation Protection. Euratom, Seventh Framework. Luxembourg: European Commission. 2011; ISSN 1681-6803. Available at http://www.sedentexct.eu/content/guidelines-cbct-dental-and-maxillofacial-radiology.htm.
Setti da Rocha ASP, de Mello Aguiar G, Tulio AP, Ditzel AS, Filipov D. Evaluation of thyroid radiation dose using cone beam computed tomography. Radiat Prot Dosim. 2017;175:368–72. https://doi.org/10.1093/rpd/ncw360.
Venturin JS, Shintaku WH, Shigeta Y, Ogawa T, Le B, Clark GT. Temporomandibular joint condylar abnormality: evaluation, treatment planning, and surgical approach. J Oral Maxillofac Surg. 2010;68:1189–96. https://doi.org/10.1016/j.joms.2009.08.002.
Zain-Alabdeen E, Alsadhan R. A comparative study of accuracy of detection of surface osseous changes in the temporomandibular joint using multidetector CT and cone beam CT. Dentomaxillofac Radiol. 2012;41:185–91. https://doi.org/10.1259/dmfr/24985971.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Luberto, L., Garberoglio, S., Carnazza, G. (2020). Other TMJ Imaging Modalities. In: Robba, T., Tanteri, C., Tanteri, G. (eds) MRI of the Temporomandibular Joint. Springer, Cham. https://doi.org/10.1007/978-3-030-25421-6_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-25421-6_2
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-25420-9
Online ISBN: 978-3-030-25421-6
eBook Packages: MedicineMedicine (R0)