Abstract
Herpes simplex virus (HSV) can present as a variety of ocular diseases. Keratitis, including epithelial and stromal, is a leading cause of infectious corneal blindness, particularly in developed countries. Most humans are infected with HSV-1 in early childhood and maintain latent infection throughout their lifetime. While majority remain asymptomatic, some can reactivate and also experience recurrences. Recent epidemiological studies show that the incidence and prevalence of ocular HSV are on the rise. This chapter reviews the clinical disease, traditional and evolving medical and surgical therapeutic options, and future directions in prevention strategies, including development of vaccination.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ocular herpes simplex
- Herpes simplex keratitis
- Recurrent herpes simplex keratitis
- Dendritic keratitis
- Stromal keratitis
- Inflammation
- High-risk corneal graft
Disease Entity
Ocular viral infections range from benign to malignant and are caused by various DNA and RNA viruses. Of these, the DNA virus, herpes simplex virus (HSV), causes significant ocular morbidity as it affects nearly every ocular tissue by both infectious and immune pathogenic mechanisms [1].
Epidemiology
HSV is the most common infectious cause of corneal blindness in the developed world. The global incidence of ocular HSV is estimated to be 1,000,000 new cases and 9,000,000 recurrent episodes each year [2]. The annual incidence of ocular HSV infections has recently been estimated at 11.8 per 100,000 people in the United States [3] and 13.2 per 100,000 in France [4]. Extrapolation of epidemiological data to the total US population in 2011 yielded an estimate of 64,499 new and recurrent cases annually. Comparison of the recent data to the reported incidence of 8.4 per 100,000 and prevalence of 149 cases per 100,000 in the early 1980s suggests an upward trend in both incidence and prevalence of ocular HSV [5].
The mean age for the first occurrence of ocular HSV -1 in the United States is 37.4 years, with autopsy studies on the trigeminal ganglia showing that >90% of the population is infected with latent HSV-1 by 60 years of age. Reported seroprevalence rates of HSV-1 in the United States, Germany, and Tanzania are >50%, >75%, and>90%, respectively, and are related to age and socioeconomic status. While 30% of children and 70–80% of adolescents in lower socioeconomic class are seropositive, the overall seroprevalence of HSV-1 in adolescents in the United States is about 30% [6]. While HSV-1 is shown to be responsible for most ocular herpes simplex infections, HSV-2 is the usual cause of neonatal HSV infection [7]. Recent studies indicate a changing epidemiology with 30% increase in HSV-2 seroprevalence in the United States over the past 3–4 decades. The incidence of neonatal HSV ranges from 5.8 to 11.5 per 100,000 live births in the United States, with 13–20% of neonates with HSV having ocular manifestations [8]. Of these, dendritic epithelial keratitis is the most common, with the incidence in the United States being 63%. The reported incidence of blepharoconjunctivitis, stromal keratitis, and uveitis is 54%, 16%, and 4%, respectively [5], while in the French study, the incidence rates were 56% dendritic keratitis, 10% geographic keratitis, and 30% stromal keratitis [4].
Economic Burden
In the United States, it is estimated that 500,000 people have ocular HSV, requiring between 4 and 6 ophthalmologist visits, leading to the total treatment cost of $ 17.7million and a loss of 444,000 work days annually [9].
Etiology
Herpes simplex virus belongs to the alpha subgroup of the Herpesviridae family which is characterized by a double-stranded linear DNA genome encased within an icosahedral viral protein capsid surrounded by a lipid bilayer envelope. The herpes viral genome can also survive without the viral capsid which allows it to lie quiescent and establish latency – a feature unique to herpes viruses. HSV-1 and HSV-2 have different virus-specific antigens. HSV-1 preferentially affects the oropharynx, while HSV-2 colonizes the genital tract. Both HSV-1 and HSV-2 can cause ocular herpetic disease although HSV-1 is more common.
Pathophysiology
The transmission of HSV is by direct contact with the saliva and/or genital secretions of infected individuals and is more common in periods of asymptomatic shedding.
At the time of initial acquisition, the virus replicates in the skin, cornea, or mucosal surfaces of the orofacial region. It then travels via the trigeminal nerve axons in a retrograde fashion and becomes latent in the trigeminal nerve ganglion. In order to establish latency, the viral genome is circularized to form an episomal DNA element packed in histones. In this state of latency, the virus employs various immune-evasive mechanisms and can exist for a variable amount of time before reactivation. One such mechanism is induction of intracellular accumulation of CD1d molecules in antigen-presenting cells. This helps the infected cells to evade recognition by natural killer T cells. HSV-1 has several other mechanisms by which it downregulates various immunologic cells and cytokines. Viral reactivation is believed to occur in response to various stimuli that induce HSV lytic gene expression, virion replication in the ganglia, and linearization of the DNA. The various environmental and systemic stressors that trigger reactivation are emotional stress, fever, UV light, menstruation, and hormonal changes. In vitro studies have shown that during periods of cellular stress, there is transient interruption of protein synthesis. This in turn affects the activity of mTOR kinase activity and causes mRNA translation in the neuron harboring the viral episome leading to viral replication. It can then travel back down any branch of the trigeminal ganglion. Recurrences tend to occur at sites with high distribution of sensory receptors such as cornea, lips, and oral mucosa. Reactivation in the ophthalmic division causes recurrent corneal disease [10].
Risk Factors
A majority of the adult population above 60 years of age is serologically positive for HSV-1. A study by Kaufman et al. showed HSV-1 DNA shedding in the tears and saliva of 98% of subjects, at least once in a 30-day study [11]. The detection of HSV-1 DNA on the corneal surface is, therefore, very common. Despite this frequent shedding of HSV-1 DNA in humans, the incidence of HSV-1 ocular disease is very low. Various factors that determine viral reactivation and disease recurrence include genetic makeup of the host, genetic makeup of the virus, and immune status of the host. Genetic factors in the host include the presence of the apoE ε4 genotype. Viral factors include virulence, antigenic differences, and viral load.
Host factors include underlying immune insufficiencies, inherited and acquired, and local tissue health. Immunocompromised individuals, for example, organ transplant recipients or patients with diabetes mellitus or HIV, experience more severe disease and more frequent recurrences. CD8+ T cells produce interferons and related factors and inhibit viral activation in the infected neurons. In periods of immune deficiency, the activity of CD8+ T cells is reduced leading to viral replication. Several case reports have shown that patients infected with measles have altered T cell function and are more likely to develop HSV. HIV patients have been shown to have a higher recurrence rate compared to immune-competent individuals. Atopic conditions also lead to altered cell mediated immunity, and such patients are susceptible to HSV infections. It has been shown that severe atopy has 2.6 greater odds of developing ocular HSV [12]. These patients tend to have bilateral, severe disease and are less responsive to treatment. Although the HEDS trial concluded that age does not affect the recurrences, other retrospective studies have shown that children have more severe disease with more recurrences, with the recurrence rate within first year of an episode being 45–50% as compared to 18% in adults. Likelihood of bilateral HSV keratitis is also more in children.
Further, corneal health is an important factor that determines the susceptibility to HSV factors. Trauma, postsurgical inflammation, and medications have been implicated in increased risks of HSV keratitis. Topical anti-glaucoma drops, particularly prostaglandin analogs, have been shown to cause recurrences of HSV keratitis and blepharitis [13]. Corticosteroids, topical, intravitreal, and/or systemic, all alter the immune response and predispose to HSV epithelial keratitis. A few case reports have also shown HSV epithelial keratitis after intravitreal anti-VEGF injections. A recent case report shows HSV keratitis following botulinum toxin injection for epiphora. Laser procedures including laser photokeratectomy, laser-assisted in situ keratomileusis (LASIK), laser iridotomy, and laser trabeculoplasty have also been strongly implicated as a risk factor for HSV. This may be due to trauma to the corneal nerves from the laser or inflammation. Several reports have shown viral reactivation after cataract surgery, penetrating keratoplasty, and deep anterior lamellar keratoplasty. Following PKP, recurrence can occur due to reactivation from the trigeminal ganglion.
Clinical Disease
Ocular herpetic disease may be primary neonatal, primary, or recurrent. Primary disease is the infectious disease of the nonimmune host. Recurrent disease occurs in the previously immune host, with or without a known history of herpes, and may be either infectious, immune, or both [6, 14] (Fig. 6.1).
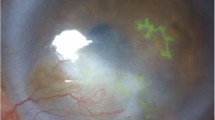
Clinical involvement in ocular herpes simplex keratitis. Slit lamp photography. (a) Scleritis and episcleritis showing superficial and deep focal injection. (b) Epithelial keratitis showing dendritic lesion with fluorescein staining of ulcer bed. (c) Epithelial and stromal keratitis showing rose bengal staining of ulcer edges with underlying stromal haze. (d) Acute stromal interstitial keratitis with focal corneal edema and haze. (e) Stromal keratitis showing peripheral corneal neovascularization with stromal edema. (f) Immune stromal keratitis showing circular haze. (g) Endotheliitis showing keratic precipitates and stromal edema. (h) Iritis showing iris inflammation. (i) Iris atrophy with transillumination defects
Primary Ocular Herpes
Acute Neonatal Ocular HSV
Neonatal HSV is rare and affects about 1 in 10, 000 infants, with 80% of the infection caused by HSV-2. Most exposure occurs during passage through the infected birth canal, while about 5% occurs in utero. Clinical manifestations include local disease involving the skin, eye, or oral mucosa, CNS infection, or disseminated disease with visceral organ involvement. The CNS and disseminated infections have very high mortality rates, 6% and 31%, respectively [15]. Ocular involvement mostly presents as conjunctivitis and ulcerative epithelial keratitis with punctate, dendritic, or serpiginous epitheliopathy. Stromal involvement is very rare and suggestive of intrauterine infection. Long-term ocular complications include cataracts, necrotizing chorioretinitis, and optic neuropathy. Strabismus and opsoclonus can develop due to CNS infection and subsequent damage [16].
Primary Ocular HSV (POHSV)
Primary ocular HSV (POHSV) is the first HSV infection of the nonimmune host with less than 4% presenting as overt disease. Clinically, overt disease begins about 1 week after exposure to an infected carrier and typically manifests itself as a vesicular periocular dermatitis or blepharitis, follicular conjunctivitis, keratitis, iritis, and a nonsuppurative preauricular adenopathy. The skin eruption remains fairly localized to the periocular area in the immunocompetent host and is a self-limited disease that resolves without scarring. A study conducted at the Moorfields Hospital on patients with primary ocular HSV reported that 84% of patients had conjunctivitis, 38% blepharitis, 15% epithelial dendritic keratitis, and 2% disciform keratitis. While POHSV is generally unilateral, 19% of these patients had bilateral disease which tends to be seen in children or patients with underlying atopic diseases.
Recurrent Ocular HSV
Blepharoconjunctivitis
HSV blepharitis presents with vesicular rash on the eyelids and along the lid margins. These lesions shed viruses for a few days and heal in about a week. Conjunctivitis is generally follicular and may be pseudomembranous.
Episcleritis and Scleritis
While HSV episcleritis is generally an infectious process, HSV scleritis is either an infection or an immune process and presents as a focal or diffuse deeply injected red eye that is hypersensitive to palpation. In review studies of deep sectoral scleritis, the majority of patients have tested positive for HSV and responded to treatment with acyclovir and steroids.
Keratitis
Corneal HSV can involve the epithelium, stroma, or endothelium; and the disease process, underlying pathophysiology and clinical picture, differs in each [17, 18].
-
Epithelial keratitis
Infectious epithelial keratitis presents with redness, decreased vision, and photophobia. In dendritic keratitis, the cornea shows ulceration in a dendritic pattern with linear branches ending in terminal bulbs. The edges have active virus and stain with rose bengal (RB) stain; the center is devoid of active virus and does not stain with RB, instead picking up fluorescein stain. As the dendritic ulcer progresses when left untreated or in patients with compromised immunity and poor healing, it can lose its dendritic shape and spread out. It is then called geographic ulcer. The edges retain active virus and stain with RB. Neurotrophic or metaherpetic ulcers develop due to damage of the corneal subbasal nerve plexus by HSV. Decreased corneal sensation is seen in about 80% cases of epithelial keratitis. This damage to nerves leads to chronic ocular surface disease and epitheliopathy as corneal nerves produce trophic factors for corneal epithelium. Secondary inflammation produces further damage to nerves and epithelium and sets up a vicious cycle. This presents as irregular epithelium with punctate keratopathy that progresses to interpalpebral epithelial defect (PED) with thick rolled edges. However, unlike dendritic or geographic ulcers, the edges do not contain virus and do not stain with RB stain. This PED does not heal easily due to underlying damage to corneal nerves and can progress and cause stromal thinning and possible corneal melt and perforation [19, 20].
-
Stromal keratitis
Stromal keratitis presents often with eye pain and blurred vision. The stromal involvement in HSV can either be due to direct viral invasion or due to immune reaction to the antigens in the stroma.
Immune stromal keratitis may present many years following initial HSV infection. The risk of developing stromal keratitis has been reported to be 21% within 2 years of the initial episode of infectious epithelial keratitis. Stromal inflammation in HSV keratitis is due to the activation of CD4 cells from HSV-specific cells, cytokine activation, and autoimmune reaction due to HSV antigen binding to host autoantigens. These CD4 cells initiate an immune destructive response and the stroma is infiltrated by inflammatory cells including neutrophils. Depending on the extent of inflammation, these antigen-antibody complex-mediated herpetic stromal keratitis can present in various forms. Limbal vasculitis is sectoral and presents as areas of focal hyperemia and edema and resolves over time without scarring. Wessely immune rings precipitate in the anterior to mid-stroma and may have a hazy edema within the ring and exhibit neovascularization. Interstitial keratitis (IK) is characterized by necrotic, blotchy, cheesy-white stromal infiltrates. Neovascularization, stromal scarring, and stromal edema develop subsequently. Hence without proper treatment, stromal keratitis is vision threatening and recurrence is common. In the Herpetic Eye Disease Study, 18% of patients diagnosed with HSV-1 ocular disease experienced a recurrence involving the stroma with stromal keratitis representing 44% of all recurrences. Furthermore, a history of stromal keratitis is a significant risk factor for future recurrences [18, 21].
-
Endotheliitis
HSV endotheliitis can be both an infectious or immune-mediated process and may present in linear, disciform, or diffuse patterns [6]. Linear endotheliitis manifests as a line of keratic precipitates (KP) that extends from the limbus toward the center with edema of the peripheral stroma and epithelium. Disciform keratitis is a focal area of stromal edema without necrosis. The endothelium develops an inflammatory response to viral antigens, characterized by deposition of focal KP. The underlying endothelium decompensates and manifests as focal disc-shaped edema, hence the name disciform. Diffuse endotheliitis represents a more diffuse severe form of endothelial inflammation with KP over the entire cornea, diffuse edema, anterior chamber inflammation, and trabecular meshwork inflammation leading to elevated intraocular pressure.
Iridocyclitis
HSV iridocyclitis is the most common presentation of herpetic uveitis and is responsible for about 9% of all cases of nontraumatic iritis. It generally presents as unilateral anterior uveitis with non-granulomatous fine KP. Focal areas of iris inflammation result in sectoral iris atrophy.
Acute Retinal Necrosis
ARN is a syndrome characterized by retinal vasculitis, necrosis, vitritis, papillitis, and uveitis. It has been thought to be caused by herpes viruses, most commonly VZV followed by HSV-1. In immunocompromised patients, ARN may present in association with HSV-1 keratitis. In the acute viral phase, viral particles in the retina invoke an intense inflammatory response with retinal vasculitis and necrosis. In the late cicatricial phase, contractile membranes form in the vitreous and on surface of the necrotic retina causing retinal detachments in the majority of patients within 3 months [22].
Diagnosis
Diagnosis of ocular HSV is mostly made based on clinical impression only. However, objective tests are available to confirm the diagnosis in cases of neonatal infections and difficult cases.
Laboratory Approaches
-
1.
Microscopic examination of skin, conjunctival, or corneal scrapings (Tzanck smear) or tissue obtained at keratoplasty after staining with Geimsa or Papanicolaou. Herpetic infections are characterized by multinucleated epithelial cells with ballooning degeneration and a mixed mononuclear and polymorphonuclear leukocyte (PMN) reaction. Intranuclear eosinophilic viral inclusion bodies of Lipschutz also called Cowdry A inclusions are seen in the epithelial cells.
-
2.
Detection of HSV antigens by direct fluorescent antibody (DFA) or enzyme-linked immunosorbent assay (ELISA) test. DFA is rapid and has high specificity; however, it requires an ultraviolet microscope. Also, topical fluorescein prior to specimen collection can lower the yield. Immunologic ELISA diagnostic kits are available commercially; they however have been shown to have low sensitivity [23].
-
3.
Detection of HSV DNA by polymerase chain reaction (PCR) [24].PCR has been used to detect HSV in the tear film and corneas of patients and is more sensitive and specific compared to cell cultures. PCR has further been used to identify HSV DNA in iridocorneal endothelial and in Posner-Schlossman syndromes. Commercially available kits are based on the amplification and simultaneous detection of a specific region of the HSV-1 and HSV-2 genome using real-time PCR.
-
4.
Viral culture. The recovery rate from acutely infected ulcers is about 70% if the specimen is taken within 2–3 days of the appearance of the lesion. Although isolation of HSV-1 by cell culture has excellent specificity, the use is limited by low sensitivity and length of time need for positive results. Cultures obtained after corneal rose bengal staining may be falsely negative due to virucidal effects of the stain [25].
-
5.
Serology. This has a limited role as HSV infections are generally due to reactivation of a latent infection. However, it is useful in certain circumstances. As IgM does not cross the placental barrier, finding IgM in a newborn is diagnostic of intrauterine infection. Serology may also be useful in patients with atypical disease. Serial titers tested 1 month apart can be informative. Quantitative documentation of a fourfold rise in either IgM or IgG strongly supports a diagnosis.
Imaging
In addition, newer imaging modalities such as in vivo confocal microscopy and anterior segment OCT can help to assess inflammation, corneal nerve damage, and corneal scarring. In vivo confocal microscopy studies in HSV keratitis have shown decreased superficial epithelial cells with increase in cell size and squamous metaplasia with a decrease in subbasal corneal nerve density correlating with decreased corneal sensation seen clinically. Immune dendritic cells (DC) are increased in both epithelial and endothelial layers. Interestingly, endothelial cell density is decreased in cases of endotheliitis as well as in cases of epithelial and stromal keratitis with decreased corneal nerve density. Moreover, these changes of decreased corneal nerve and endothelial cell density have been shown in contralateral unaffected eyes as well suggesting a potential bilateral involvement in clinically unilateral disease. Studies have also studied changes in DC corneal nerve and endothelial cell density during the therapeutic phase to help guide treatment [20, 26, 27].
Antiviral Susceptibility Testing
This may have a role in the diagnosis of ocular HSV, specifically in recurrent and treatment nonresponsive cases. Acyclovir resistance mediated by mutations in thymidine kinase may be as high as 6.4% in immunocompetent patients. These patients are also immune to other thymidine kinase-dependent drugs such as valacyclovir, ganciclovir, and famciclovir. In such cases, foscarnet, cidofovir, and trifluridine can be good alternatives [28].
Differential Diagnosis
Differential diagnosis of HSV keratitis includes other infectious etiologies such as viral and acanthamoeba and noninfectious etiologies such as contact lens overwear, neurotrophic keratitis, and Thygeson’s superficial punctate keratitis. HSV interstitial keratitis includes other viral, bacterial, or fungal etiologies as well as immune-mediated conditions such as sarcoidosis, Cogan’s syndrome. HSV endotheliitis includes other viral etiologies, corneal graft failure, inflammatory conditions such as Fuchs heterochromic iridocyclitis, and Posner-Schlossman syndrome.
Treatment
Medical Treatment
The mainstay of treatment is antiviral therapy in topical or oral form or both [18, 29].
The topical antiviral drugs approved by the US Food and Drug Administration (FDA) are trifluridine (TFT) solution and ganciclovir gel. Although topical acyclovir is not approved in the United States, it is widely used outside. Aqueous humor concentrations are adequate with both topical TFT and acyclovir. While TFT penetration doubles in presence of corneal epithelial defect, topical acyclovir achieves adequate levels even in intact corneal epithelium. While there are no clinical trials directly comparing topical ganciclovir gel to trifluridine solution, several clinical trials have compared each to topical acyclovir ointment and have concluded that efficacy of the three agents are similar [30]. While both TFT and ganciclovir are considered safe, prolonged topical TFT causes toxic epitheliopathy, allergic conjunctivitis, and punctal stenosis.
There are three oral antiviral agents that demonstrate activity against HSV infections and have favorable safety profile – acyclovir (ACV), valacyclovir (VCV), or famciclovir. Clinically, all three have been shown to have equal efficacy. The therapeutic dose of ACV is 400 mg orally 5×/day, for 7–10 days [31]. VCV and famciclovir require less frequent dosing (VCV 500 mg 2×/day or famciclovir 250 mg 2×/day for the same time period as acyclovir) but are more expensive. VCV is hydrolyzed back into ACV but has five times the bioavailability, and famciclovir has a longer intracellular half-life than ACV. Oral antiviral agents should be used with caution in elderly patients (>65 years old) and those with renal impairment, as all three oral antiviral agents have the potential to cause nephrotoxicity. All three oral antivirals are designated Pregnancy Category B as the use of oral valganciclovir, foscarnet, and cidofovir is limited by a poor safety profile [32].
Primary Ocular HSV
Although POHSV can resolve spontaneously, specific antiviral therapy results in earlier resolution. ACV is the most commonly used drug with dosage altered according to age of patients. For children less than 8 years of age, oral acyclovir, available as a suspension of 200 mg/5 ml, is administered at a dosage of 20 mg/kg every 8 hours. Post-pubertal children are treated at the same dose as adults – ACV 400 mg 5×/day. Alternatively, VCV 500 mg twice daily or famciclovir 125–250 mg three times daily can be used [33]. Herpes simplex keratoconjunctivitis is treated with topical TFT 5×/day until resolution. For ocular and mucocutaneous HSV infections in the immunocompromised host, therapy consists of IV acyclovir at 5 mg/kg every 8 hours for 7–14 days [30].
Acute Neonatal Ocular HSV
Pregnant females with frequent recurrences of genital herpes should receive suppressive acyclovir therapy beginning at 36 weeks gestation. In women with active lesions at the onset of labor, caesarean section should be done to prevent infection [34]. Neonates delivered through an infected birth canal should be screened between 24 and 48 hours of age with viral cultures of eyes, nasopharynx, mouth, and rectum and if positive, they should be treated with acyclovir even if asymptomatic. An emergency pediatric or infectious disease consultation should be obtained. Treatment is with high-dose intravenous acyclovir (60 mg/kg per day in three divided doses) for 3 weeks, with adjustments made for infants with renal or hepatic insufficiency. Infants with disease localized to the skin, eyes, and mucous membranes can be treated for 2 weeks if the CSF PCR reaction assay is negative for HSV DNA. Decreasing the acyclovir dosage or administering granulocyte colony-stimulating factor should be considered if the absolute neutrophil count falls and remains below 500/mm3 for a prolonged period [35].
Recurrent Ocular HSV
Blepharitis, Dacryoadenitis, and Conjunctivitis
ACV 400 mg orally 5×/day or TFT 5×/day for 10 days or until the lesions have scabbed.
Keratitis
-
Epithelial keratitis: Mainstay of treatment is antiviral therapy, either topical with TFT or ganciclovir gel for 7–10 days or oral antivirals in therapeutic doses; there is no reported benefit of combining oral and topical therapy. Debridement alone is not as effective. Topical antibiotic is added when active ulceration is present and corticosteroids are contraindicated in these cases [17, 32].
-
Neurotrophic keratitis: Antiviral therapy has a limited role. Treatment of meibomian gland dysfunction and copious lubrication is needed in early stages of NK to prevent epithelial breakdown. In case of epithelial defect, autologous serum tears, cord blood serum, and platelet-rich plasma have all shown efficacy in healing of ulcers. In addition, bandage contact lenses, scleral lenses, and amniotic membrane Prokera™ amniolens may be used to promote epithelial healing. More recently, recombinant human nerve growth factor (cenegermin) has shown promise in moderate to severe NK. Surgical interventions are reserved for nonhealing ulcers or progressive corneal melts and perforations [19].
-
Stromal keratitis: As stromal keratitis is an immune-mediated process. The mainstay of treatment is topical corticosteroids with antivirals for at least 10 weeks in cases of stromal keratitis without ulceration. In case of epithelial ulceration, corticosteroids are held or limited in strength or frequency until the epithelium heals, and topical antibiotic drops are added.
-
Uncontrolled inflammation itself may interfere with healing. The above guidelines were established based on the HEDS study, a double-blind, randomized clinical trial that compared prednisolone with TFT versus placebo with TFT [21]. Only 26% of the patients in the prednisolone group failed treatment as compared to 73% in the placebo group. Further, the study showed that the minimum recommended treatment period is 10 weeks. There was no added benefit of oral antivirals to the treatment regimen with topical antivirals and prednisolone. However, given poor corneal concentration and unfavorable safety profile of the topical antivirals currently available in the United States, oral antivirals in the therapeutic dose were used [17].
-
Endotheliitis: The recommended treatment for HSV endothelial keratitis includes a topical corticosteroid in conjunction with an oral antiviral agent similar to stromal keratitis; however, the mean healing time for endotheliitis is less compared to stromal keratitis; hence the treatment is recommended for 3 weeks [17, 21].
Iridocyclitis
Mild iritis is treated with cycloplegics, while more severe disease requires topical steroids with slow taper. Oral antivirals in the prophylactic dose are often recommended as well.
Acute Retinal Necrosis (ARN)
ARN is a serious disease with very poor prognosis as retinal detachments often develop in the necrotic thinning retina. Prompt hospitalization with intravenous antiviral therapy and oral steroids is needed. Intravitreal injection of antiviral medication may also be performed.
Surgical Treatment
Surgical treatment is required acutely for progressive ulceration with corneal melting and perforation, severe neurotrophic keratitis, and visual rehabilitation in case of corneal scarring. In case of progressive thinning, tissue adhesive glue or ocular surface reconstruction with amniotic membrane or conjunctival and pedicle grafts may be needed. These procedures are indicated to provide tectonic support to the cornea. In case of advanced NK, adjunctive lateral tarsorraphy is often very helpful. In further progression, therapeutic keratoplasty may be indicated [36]. A novel surgical technique has been proposed recently for restoring corneal sensation in case of neurotrophic damage. This corneal neurotization involves grafting sural nerve to the ophthalmic division of the trigeminal nerve and has shown improvement in corneal sensation in 3–6 months.
Surgical options for optical reasons depend on the extent of scarring and degree of visual impairment. For partial-thickness scars, deep anterior lamellar keratoplasty (DALK) can be performed. In case of full-thickness scars, penetrating keratoplasty may be performed when the disease is quiescent. A comparison of DALK and PKP in herpetic infections has shown lower rejection, recurrence, and failure rates in DALK, although most studies have been retrospective with small sample sizes [37]. The Boston keratoprosthesis may be indicated in cases that cannot sustain a PKP [38, 39].
A major challenge in corneal transplantation in herpetic keratitis is poor graft survival. The reasons are manifold. Grafts done in case of active inflammation have less than 25% chance of survival at 1 year. Corneal neovascularization in the graft with subsequent graft rejection and failure is a common complication [40]. This occurs due to deep corneal neovascularization in stromal keratitis and also release of VEGF by viral antigens in the residual scar. Corneal hypesthesia further reduces chances of graft survival. Recurrence rate of HSV keratitis in patients without oral antiviral prophylaxis was reported at 32% at 4 months, 39–46% at 1 year, and 27–50% at 2 years after transplantation [41]. A recent review of randomized controlled trials to assess the efficacy of oral antivirals after corneal transplantation in ocular HSV showed that oral acyclovir reduces HSK recurrence by about 23 cases less per 100 grafts and graft failure by 13 fewer cases per 100 cases [42].
Thus, four major factors are key to long-term survival of keratoplasty in herpetic eyes: (1) waiting till the eye is quiescent; (2) intensive postoperative topical steroids to suppress inflammation and neovascularization; (3) removing the scar in its entirety and adjunctive lateral tarsorraphy; and (4) oral antivirals, e.g., ACV 400 mg po bid for 12–18 months (or longer as needed) as prophylaxis against recurrence of infection in the graft. The recurrence rate of HSV keratitis following penetrating keratoplasty decreases with increased length of oral acyclovir treatment resulting in reported recurrence rates of 0% at 16 months and 5% at 2 years. Further, it appears reasonable following keratoplasty to continue prophylaxis with oral antivirals for as long as the patient remains on topical corticosteroids.
Prognosis
A major factor contributing to the prognosis of ocular HSV is the high recurrence rate. The HEDS study estimated the cumulative probability of recurrence in any type of ocular HSV to be 32% at 1 year [43]. While a previous history of epithelial keratitis does not significantly increase the risk of epithelial keratitis, a history of stromal keratitis increases the rate of recurrence by tenfold [43]. Leisegang et al. reported recurrence rates of 9.6% at 1 year, 36% at 5 years, and 63.2% at 20 years after an initial episode [44]. The rate of recurrence increases significantly with the number of previous episodes; patients with one recurrence following an initial episode had a recurrence rate up to 38% at 1 year and 67% by 5 years. The relative risk of recurrence is 1.41 in 2–3 previous episodes and 2.09 with more than 4 previous episodes. A more recent study of recurrence rates reports 27% at 1 year, 50% at 5 years, 57% at 10 years, and 63% at 20 years [3].
Prophylaxis
Inhibition of reactivation and preventing recurrent infection is one of the most important aspects in the management of ocular HSV to prevent vision-threatening complications. The HEDS study was the first landmark clinical trial to establish the efficacy of systemic antiviral therapy to decrease recurrences in ocular HSV. It showed that oral prophylaxis with 400 mg of acyclovir 2×/day over a period of 12–18 months significantly decreased the recurrence rate (p < 0.05). Further, in patients with a history of HSK, the rate of recurrence decreased from 28% in the placebo group to 14% in the treatment group [21]. Further, there was no role for adding prophylactic dose of systemic antivirals in patients with epithelial keratitis being treated with topical antivirals to reduce rates of iritis and stromal keratitis. However, as the number of recurrences has been shown to be an important predictor of the recurrence rates, two or more episodes of epithelial keratitis per year warrants oral prophylactic therapy. In terms of the oral antiviral agent used, studies have showed that efficacy and safety profiles of acyclovir 400 mg 2×/day is similar to valacyclovir 500 mg/day and either may be used.
Further, as HSV patients undergoing laser and surgical procedures are at an increased risk of reactivation, they should be protected with prophylactic oral antiviral therapy starting at least 24 hours pre-op and continuing for about 2 weeks. Similarly, patients undergoing laser refractive surgeries, collagen cross-linking, and cataract are at risk of reactivation and must be protected with oral prophylactic dose in the peri- and postoperative period. Oral prophylactic therapy has shown to be critical in the graft survival after corneal transplantation. Acyclovir 800 mg 3–5×/day initially for about 3 months and then tapered to 400 mg 2×/day or valacyclovir 500 mg 2–3×/day for 3 months and then tapered to 250 mg 2×/day for up to 30 months has shown dramatically reduced rates of HSV recurrence after PKP [42]. It is recommended to continue oral prophylactic therapy till the patient remains on a topical corticosteroid.
Prevention
There is much ongoing research for development of an HSV vaccine to prevent primary infection and recurrence. Epitope-based vaccines, recombinant viral vaccine vectors, and DNA vaccines show promise. HSV envelope glycoproteins are ideal immunogens as these are the targets for antibody production in HSV infection. One such subunit vaccine based on glycoprotein gD has been developed and studied for primary prevention of genital HSV [45]. The clinical trial in phase III has shown that this subunit vaccine was effective in preventing HSV-1 infection with an efficacy of 58% [46]. So far, there has been no vaccine for prevention of primary ocular infection as most systemic vaccines fail to induce local ocular immune responses. There has been some research to develop strategies to reduce local shedding in tears of asymptomatic carriers. A study demonstrated that topical ophthalmic administration of human CD 8 T cells epitope-based vaccine to latently infected rabbits reduced the spontaneous viral shedding in tears [47].
There is also emphasis on developing vaccines for the prevention of HSV reactivation. CD 8 T cells mount an immunological response to combat viral reactivation in the trigeminal ganglion. A recent animal study demonstrated that a HSV envelope glycoprotein epitope-based vaccine was associated with mobilization of antiviral CD 8 T cells into the cornea and trigeminal ganglia, thus protecting against ocular HSV [48]. Heat-inactivated HSV-1 vaccine can boost CD 8 T cell response in the latently infected ganglia in hope to inhibit reactivation. A small clinical trial in humans showed a significant reduction in ocular HSV recurrence rate after administration of heat-inactivated HSV-1 vaccine subcutaneously [49]. However, one major risk of this approach is conversion of a non-virulent strain to an active virulent strain through mutation. Thus, the development of an effective and safe vaccine to prevent HSV warrants prospective, randomized, controlled, and long-term clinical trials.
References
Whitley RJ, Roizman B. Herpes simplex virus infections. Lancet. 2001;357(9267):1513–8.
Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol. 2012;57(5):448–62.
Young RC, Hodge DO, Liesegang TJ, Baratz KH. Incidence, recurrence, and outcomes of herpes simplex virus eye disease in Olmsted County, Minnesota, 1976–2007: the effect of oral antiviral prophylaxis. Arch Ophthalmol. 2010;128(9):1178–83.
Labetoulle M, Auquier P, Conrad H, et al. Incidence of herpes simplex virus keratitis in France. Ophthalmology. 2005;112(5):888–95.
Liesegang TJ, Melton LJ 3rd, Daly PJ, Ilstrup DM. Epidemiology of ocular herpes simplex. Incidence in Rochester, Minn, 1950 through 1982. Arch Ophthalmol. 1989;107(8):1155–9.
Rowe AM, St Leger AJ, Jeon S, Dhaliwal DK, Knickelbein JE, Hendricks RL. Herpes keratitis. Prog Retin Eye Res. 2013;32:88–101.
Looker KJ, Magaret AS, May MT, et al. First estimates of the global and regional incidence of neonatal herpes infection. Lancet Glob Health. 2017;5(3):e300–9.
Chong EM, Wilhelmus KR, Matoba AY, Jones DB, Coats DK, Paysse EA. Herpes simplex virus keratitis in children. Am J Ophthalmol. 2004;138(3):474–5.
Lairson DR, Begley CE, Reynolds TF, Wilhelmus KR. Prevention of herpes simplex virus eye disease: a cost-effectiveness analysis. Arch Ophthalmol. 2003;121(1):108–12.
Toma HS, Murina AT, Areaux RG Jr, et al. Ocular HSV-1 latency, reactivation and recurrent disease. Semin Ophthalmol. 2008;23(4):249–73.
Kaufman HE, Azcuy AM, Varnell ED, Sloop GD, Thompson HW, Hill JM. HSV-1 DNA in tears and saliva of normal adults. Invest Ophthalmol Vis Sci. 2005;46(1):241–7.
Borkar DS, Gonzales JA, Tham VM, et al. Association between atopy and herpetic eye disease: results from the pacific ocular inflammation study. JAMA Ophthalmol. 2014;132(3):326–31.
Kothari MT, Mehta BK, Asher NS, Kothari KJ. Recurrence of bilateral herpes simplex virus keratitis following bimatoprost use. Indian J Ophthalmol. 2006;54(1):47–8.
Green LK, Pavan-Langston D. Herpes simplex ocular inflammatory disease. Int Ophthalmol Clin. 2006;46(2):27–37.
Kimberlin DW, Whitley RJ. Neonatal herpes: what have we learned? Semin Pediatr Infect Dis. 2005;16:7–16.
Silva RA, Berrocal AM, Moshfeghi DM, Blumenkranz MS, Sanislo S, Davis JL. Herpes simplex virus type 2 mediated acute retinal necrosis in a pediatric population: case series and review. Graefes Arch Clin Exp Ophthalmol. 2013;251(2):559–66.
Khan BF, Pavan-Langston D. Clinical manifestations and treatment modalities in herpes simplex virus of the ocular anterior segment. Int Ophthalmol Clin. 2004;44(3):103–33.
Kalezic T, Mazen M, Kuklinski E, Asbell P. Herpetic eye disease study: lessons learned. Curr Opin Ophthalmol. 2018;29(4):340–6.
Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107–31.
Hamrah P, Sahin A, Dastjerdi MH, et al. Cellular changes of the corneal epithelium and stroma in herpes simplex keratitis: an in vivo confocal microscopy study. Ophthalmology. 2012;119(9):1791–7.
Acyclovir for the prevention of recurrent herpes simplex virus eye disease. Herpetic Eye Disease Study Group. N Engl J Med. 1998;339(5):300–6.
Miserocchi E, Iuliano L, Fogliato G, et al. Bilateral acute retinal necrosis: clinical features and outcomes in a multicenter study. Ocul Immunol Inflamm. 2018:1–9.
Satpathy G, Behera HS, Sharma A, et al. A 20-year experience of ocular herpes virus detection using immunofluorescence and polymerase chain reaction. Clin Exp Optom. 2018;101(5):648–51.
Tei M, Nishida K, Kinoshita S. Polymerase chain reaction detection of herpes simplex virus in tear fluid from atypical herpetic epithelial keratitis after penetrating keratoplasty. Am J Ophthalmol. 1996;122(5):732–5.
Athmanathan S, Bandlapally S, Rao GN. Comparison of the sensitivity of a 24 h-shell vial assay, and conventional tube culture, in the isolation of herpes simplex virus - 1 from corneal scrapings. BMC Clin Pathol. 2002;2(1):1.
Moein HR, Kheirkhah A, Muller RT, Cruzat AC, Pavan-Langston D, Hamrah P. Corneal nerve regeneration after herpes simplex keratitis: a longitudinal in vivo confocal microscopy study. Ocul Surf. 2018;16(2):218–25.
Muller RT, Pourmirzaie R, Pavan-Langston D, et al. In vivo confocal microscopy demonstrates bilateral loss of endothelial cells in unilateral herpes simplex keratitis. Invest Ophthalmol Vis Sci. 2015;56(8):4899–906.
Shiraki K. Antiviral drugs against alphaherpesvirus. Adv Exp Med Biol. 2018;1045:103–22.
https://www.aao.org/clinical-statement/herpes-simplex-virus-keratitis-treatment-guideline.
Klysik K, Pietraszek A, Karewicz A, Nowakowska M. Acyclovir in the treatment of herpes viruses – a review. Curr Med Chem. 2018.
Lee SY, Pavan-Langston D. Role of acyclovir in the treatment of herpes simplex virus keratitis. Int Ophthalmol Clin. 1994;34(3):9–18.
Roozbahani M, Hammersmith KM. Management of herpes simplex virus epithelial keratitis. Curr Opin Ophthalmol. 2018;29(4):360–4.
Liu S, Pavan-Langston D, Colby KA. Pediatric herpes simplex of the anterior segment: characteristics, treatment, and outcomes. Ophthalmology. 2012;119(10):2003–8.
Sheffield JS, Hollier LM, Hill JB, Stuart GS, Wendel GD. Acyclovir prophylaxis to prevent herpes simplex virus recurrence at delivery: a systematic review. Obstet Gynecol. 2003;102(6):1396–403.
Harris JB, Holmes AP. Neonatal herpes simplex viral infections and acyclovir: an update. J Pediatr Pharmacol Ther. 2017;22(2):88–93.
Tuli S, Gray M, Shah A. Surgical management of herpetic keratitis. Curr Opin Ophthalmol. 2018;29(4):347–54.
Li J, Ma H, Zhao Z, et al. Deep anterior lamellar keratoplasty using precut anterior lamellar cap for herpes simplex keratitis: a long-term follow-up study. Br J Ophthalmol. 2014;98(4):448–53.
Brown CR, Wagoner MD, Welder JD, et al. Boston keratoprosthesis type 1 for herpes simplex and herpes zoster keratopathy. Cornea. 2014;33(8):801–5.
Khan BF, Harissi-Dagher M, Pavan-Langston D, Aquavella JV, Dohlman CH. The Boston keratoprosthesis in herpetic keratitis. Arch Ophthalmol. 2007;125(6):745–9.
Kuffova L, Knickelbein JE, Yu T, et al. High-risk corneal graft rejection in the setting of previous corneal herpes simplex virus (HSV)-1 infection. Invest Ophthalmol Vis Sci. 2016;57(4):1578–87.
Epstein RJ, Seedor JA, Dreizen NG, et al. Penetrating keratoplasty for herpes simplex keratitis and keratoconus. Allograft rejection and survival. Ophthalmology. 1987;94(8):935–44.
Bhatt UK, Abdul Karim MN, Prydal JI, Maharajan SV, Fares U. Oral antivirals for preventing recurrent herpes simplex keratitis in people with corneal grafts. Cochrane Database Syst Rev. 2016;(11):CD007824.
Predictors of recurrent herpes simplex virus keratitis. Herpetic Eye Disease Study Group. Cornea. 2001;20(2):123–8.
Liesegang TJ. Epidemiology of ocular herpes simplex. Natural history in Rochester, Minn, 1950 through 1982. Arch Ophthalmol. 1989;107(8):1160–5.
Bettahi I, Nesburn AB, Yoon S, et al. Protective immunity against ocular herpes infection and disease induced by highly immunogenic self-adjuvanting glycoprotein D lipopeptide vaccines. Invest Ophthalmol Vis Sci. 2007;48(10):4643–53.
Belshe RB, Leone PA, Bernstein DI, et al. Efficacy results of a trial of a herpes simplex vaccine. N Engl J Med. 2012;366(1):34–43.
Khan AA, Srivastava R, Chentoufi AA, et al. Therapeutic immunization with a mixture of herpes simplex virus 1 glycoprotein D-derived “asymptomatic” human CD8+ T-cell epitopes decreases spontaneous ocular shedding in latently infected HLA transgenic rabbits: association with low frequency of local PD-1+ TIM-3+ CD8+ exhausted T cells. J Virol. 2015;89(13):6619–32.
Khan AA, Srivastava R, Vahed H, et al. Human asymptomatic epitope peptide/CXCL10-based prime/pull vaccine induces herpes simplex virus-specific gamma interferon-positive CD107(+) CD8(+) T cells that infiltrate the corneas and trigeminal ganglia of humanized HLA transgenic rabbits and protect against ocular herpes challenge. J Virol. 2018;92(16).
Pivetti-Pezzi P, Accorinti M, Colabelli-Gisoldi RA, Pirraglia MP, Sirianni MC. Herpes simplex virus vaccine in recurrent herpetic ocular infection. Cornea. 1999;18(1):47–51.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Aggarwal, S., Pavan-Langston, D. (2020). Ocular Herpes Simplex. In: Colby, K., Dana, R. (eds) Foundations of Corneal Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-25335-6_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-25335-6_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-25334-9
Online ISBN: 978-3-030-25335-6
eBook Packages: MedicineMedicine (R0)