Abstract
In recent years, pediatricians have been increasingly treating insulin resistance with drugs such as metformin to improve cardiovascular risk. However, some randomized controlled trials in adolescents reported that metformin has no effect on insulin resistance and its associated cardiovascular risk factors. This raises questions about the concept of insulin resistance as a treatment target. Furthermore, some shortcomings of the definition and measurement of insulin resistance in children and adolescents have to be kept in mind. There is currently no accurate, reliable, reproducible, and easily applicable method of measurement of insulin resistance. Fasting insulin as an index of insulin resistance or insulin resistance indices such as homeostasis model assessment (HOMA) may be applicable in epidemiological studies using large populations of children and/or well-defined cohorts, but not at the individual level. Even if a uniformly reliable insulin assay became available, separate normative values specific to sex, ethnic group, and pubertal stage would be needed. Additionally, there are very limited longitudinal data in childhood regarding whether insulin resistance itself predicts the development of cardiovascular diseases and type 2 diabetes mellitus better than body mass index (BMI) or classic cardiovascular risk factors alone. In conclusion, the presence of obesity or associated cardiovascular risk factors should be treated with lifestyle intervention and/or drugs that secondarily improve insulin resistance without a focus on insulin resistance as a primary treatment target.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
As in adulthood, obesity in childhood contributes to an increased prevalence of cardiovascular risk factors, such as hypertension, hypertriglyceridemia, low high-density lipoprotein (HDL) cholesterol, and impaired glucose metabolism [1,2,3,4,5] (see Table 17.1). The clustering of these risk factors is summarized in the definition of metabolic syndrome (MetS), which is associated with atherosclerosis and cardiovascular diseases leading to increased morbidity and mortality [6,7,8,9,10,11,12].
Insulin resistance is regarded as the key mechanism in MetS linking obesity to cardiovascular risk factors [6, 13] and type 2 diabetes mellitus (T2D), in both adults and children [14,15,16]. Confirmatory factor analysis of adult data suggests one pathophysiological mechanism underlying all cardiovascular risk factors summarized in the definition of MetS is insulin resistance [17, 18]. Other diseases linked to insulin resistance are polycystic ovarian syndrome (PCOS) [19] and nonalcoholic fatty liver disease (NAFLD), which are also associated with MetS [20].
Recently, based on this observation, pediatricians have increasingly been treating insulin resistance using lifestyle interventions and drugs, such as metformin [21]. Indeed, some studies in adolescents demonstrated a positive effect of metformin on insulin resistance and associated cardiovascular risk factors [22, 23]. However, other randomized controlled trials have reported no effect [24, 25]. Therefore, before basing treatment recommendations on the concept of insulin resistance itself, some shortcomings of its definitions and its measurement in children and adolescents have to be kept in mind, which will be discussed in the following.
Definition of Insulin Resistance
Insulin resistance is defined as the decreased tissue response to insulin-mediated cellular actions. Therefore, insulin resistance means an impairment of insulin action leading to reduced whole-body glucose uptake in response to physiological insulin levels [14]. This is manifested by decreased insulin-stimulated glucose uptake in skeletal muscle and adipose tissue and impaired suppression of hepatic glucose output through glycogenolysis. Insulin resistance results in compensatory increase in insulin secretion. The resulting hyperinsulinemia overcomes the insulin resistance for a while and keeps blood glucose in the normal range. However, when relative β(beta)-cell insufficiency (i.e., insulin secretion insufficient for the level of hyperglycemia) also sets in, overt diabetes develops. Furthermore, insulin resistance is associated with deterioration in fat metabolism [26, 27].
Underlying Mechanism of Insulin Resistance
The mechanisms of insulin resistance involve defects in insulin signaling, skeletal muscle and adipose triglyceride and fatty acid metabolism, glucose uptake, and glucose metabolism, among others. Adipose tissue cytokines, such as adiponectin and leptin, and other obesity genes may be involved too [28]. In humans, euglycemic hyperinsulinemic clamp studies have shown that insulin resistance is determined primarily by the response of skeletal muscle, with more than 75% of infused glucose taken up by muscle and only 2–3% by adipose tissue [29]. Independent of the relation between total body fat and insulin resistance, increased abdominal visceral adipose tissue in obese youth is associated with lower insulin sensitivity and higher acute insulin response [30].
Clinical Picture of Insulin Resistance
Insulin resistance is frequently associated with the presence of acanthosis nigricans, as well as the occurrence of cardiovascular risk factors summarized in the definition of MetS. Acanthosis nigricans is a condition of the skin presenting as pigmentation along with verrucous hypertrophy [31]. A typical clinical presentation of insulin resistance is mild hypertriglyceridemia combined with low HDL cholesterol levels and increased blood pressure [26, 32]. However, these clinical features cannot define or quantify insulin resistance [14].
Measurement of Insulin Resistance
There is an ongoing discussion about how insulin resistance in childhood is best assessed. Standards for measurements of insulin resistance in children have not been established so far [14]. This is due, in part, to the use of a variety of techniques to measure insulin sensitivity, lack of sufficient cohort sizes to establish normative distributions for insulin sensitivity, and lack of adequate longitudinal studies to relate definitions of insulin resistance to long-term outcomes.
The euglycemic hyperinsulinemic clamp is the “gold standard” for measuring insulin sensitivity [14]. The frequently sampled intravenous glucose tolerance test (FSIVGTT) and steady-state plasma glucose (SSPG) methods are also valid measurements [14]. However, each of these methods is time consuming and costly, requires IV infusions and frequent blood sampling in a research setting, and is burdensome for participants. Therefore, these techniques are useful for research but not for clinical practice.
Clinicians prefer simple tools, such as fasting glucose. However, fasting glucose showed only a weak correlation to continuously measured blood glucose and insulin resistance [33]. Impaired glucose tolerance (IGT) demonstrated a better association with continuously measured blood glucose and insulin resistance [33]. However, the reproducibility of pathological glucose levels in oral glucose tolerance tests is low, therefore limiting its value on an individual level [32, 34, 35]. It has been suggested that hemoglobin A1c (HbA1c) may be a better parameter to describe insulin resistance, since it demonstrates the best correlation to continuous glucose measurements [33]. However, there are no studies in childhood proving the relationship between insulin resistance and HbA1c. Likely, all parameters—such as fasting glucose, glucose in oral glucose tolerance tests, and HbA1c levels—that depend on the measurement of glucose without linking to simultaneous insulin concentrations will fail to describe insulin resistance since there is a narrow range of fasting glucose even among obese children with insulin resistance due to compensatory increased insulin secretion that maintains euglycemia until β(beta)-cell decompensation occurs [21]. Thus, glucose-based measures are more reflective of β(beta)-cell function.
Fasting insulin levels are also not a reliable tool for individual assessment of insulin resistance [14, 36]. The accuracy of fasting insulin as a measure of insulin sensitivity has been compared through correlation analyses with the euglycemic hyperinsulinemic clamp, FSIVGTT, and SSPG and found to be disappointingly poor [37,38,39]. The value of fasting insulin is limited by great intra- and interindividual variability [36]. Insulin secretion is pulsatile and normal values change physiologically based on pubertal stage [40], making them difficult to interpret in adolescents. Furthermore, the insulin assay itself can be a source of error; testing of aliquots of a common sample assayed in different laboratories has shown disparate results [41]. Sample processing can also introduce error, as insulin levels decrease rapidly if the sample is not frozen [36]. In conclusion, fasting insulin is an unreliable clinical measure of insulin resistance in an individual child and should not be used for decision making in daily practice [14].
The homeostasis model assessment (HOMA)
and the quantitative insulin-sensitivity check index (QUICKI)
are alternative diagnostic tests for insulin resistance that need only a simultaneous fasting determination of glucose and insulin [42, 43]. Both indices use a mathematical formula that adjusts for individual variability in insulin and glucose secretion and clearance. Although the goal of these methods was to improve the accuracy of fasting insulin as a measure of insulin resistance by the addition of fasting glucose, it is now agreed that they yield similar results to fasting insulin alone. For instance, HOMA, the most widely used of the surrogate measures in children, is highly correlated with fasting insulin (r = 0.95) in children [37]. These high correlations can be attributed to the narrow range of fasting glucose, even among insulin-resistant children [21, 37]. In contrast, there is a 53-fold variation in fasting insulin in children with and without insulin resistance [37]. Therefore, on an individual level HOMA and QUICKI have the same problems of reliability as described above for fasting insulin levels.
A further less-intensive method, the measurement of insulin during the oral glucose tolerance test (OGTT), offers the advantage of a smaller number of blood samples. Based on these measurements, indices such as ISI Cederholm
are calculated [44]. Good correlations were reported in adult studies comparing OGTT-based indices with the euglycemic hyperinsulinemic clamp [45]. However, the correlation in children is less clear. First reports in a small group of obese children reported only moderate correlations [46]. Finally, this index, as well as other indices such as HOMA, cannot distinguish between peripheral and hepatic insulin resistance [36].
Using the calculation of HOMA and QUICKI as models, a formula using fat metabolism has been suggested to describe insulin resistance [26, 27]. Instead of glucose, free fatty acids (FFAs) were used for the mathematical calculation of insulin resistance. While these calculations correlated well with cardiovascular risk factors [26, 27], the same problems seen for HOMA and QUICKI were also true for these calculations, since the great majority of variability is accounted for by the insulin levels, while the FFA levels differ to a lesser degree between insulin-resistant and nonresistant humans.
In summary, an accurate assessment of insulin resistance requires an invasive and impractical test (e.g., the hyperinsulinemic euglycemic clamp technique). The Insulin Resistance in Children Consensus Conference Group stated that there is no justification for screening children for insulin resistance by HOMA, QUICKI, fasting insulin, or other indices [14]. However, having a uniform internationally accepted definition of insulin resistance that can be measured under clinical conditions would be very helpful for the description of populations in different research studies.
Influence Factors on Insulin Resistance
The two most important biological conditions associated with insulin resistance in childhood besides obesity are ethnicity and puberty [14]. In studies of adult twins, approximately half of the variance in insulin sensitivity and secretion can be attributed to genetic factors [47]. Healthy children with a family history of type 2 diabetes mellitus are more insulin resistant, with an impaired balance between insulin sensitivity and secretion [48]. Using a variety of methods, studies show that non-Hispanic black, Hispanic, Pima Indian, and Asian children are less insulin sensitive than non-Hispanic white children [49, 50]. The insulin resistance in minority ethnic groups is manifested as lower insulin-stimulated glucose uptake, concomitant with hyperinsulinemia, evidence of increased insulin secretion from the β(beta)-cell and decreased insulin clearance [49, 50].
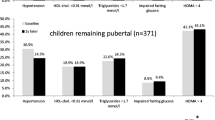
Pubertal stage has been identified as an additional major influence factor on insulin resistance. Puberty onset is characterized by a physiological ~30% reduction of insulin sensitivity that is reversed when puberty is complete [51,52,53,54]. Furthermore, impaired glucose tolerance and impaired fasting glucose are also more frequent in pubertal obese adolescents compared to prepubertal children [55] and normalize at the end of puberty [56]. In a longitudinal study in 253 overweight Hispanic youths, insulin resistance increased in both sexes in early puberty with a recovery in late puberty [57]. In non-Hispanic white children, the same changes of insulin resistance during puberty have been reported [58]. Pinhas-Hamiel and colleagues reported an increase of insulin levels during puberty [59]. A rise of insulin resistance has been reported already before puberty when adrenarche starts [60, 61]. Moreover, it has been reported that insulin resistance increases during puberty in obese children more than in normal-weight children [62,63,64]. Furthermore, it is well-known that glucose metabolism frequently deteriorates during puberty in children suffering from type 1 diabetes mellitus and improves at the end of puberty [65].
The reasons for changes of insulin resistance during puberty are not yet well-understood. The increase in growth hormone, sex hormone, and insulin-like growth factor-1 (IGF-1) that occurs during puberty is thought to be the cause of this form of insulin resistance [66]. Furthermore, puberty has an effect on the fat oxidation rates during exercise in both overweight and normal-weight girls resulting in increased insulin resistance [67]. A temporal relationship between insulin resistance and the pubertal decrease in physical activity in peripubertal Hispanic and non-Hispanic black females has been reported [68]. Furthermore, concentrations of sex hormones, adipocytokines, and inflammatory cytokines change dramatically during pubertal development, making an influence on insulin resistance probable [69, 70]: Adiponectin concentrations had been negatively correlated to many cardiovascular risk factors and decrease with onset of puberty in males [71]. An association between insulin resistance and leptin has also been reported [72]. Sex hormone binding globulin levels also predict insulin resistance and cardiovascular risk factors during puberty [73]. However, the observed relationships between various adipocytokines and insulin resistance during puberty were weak in longitudinal studies, suggesting additional important influences [69].
Interestingly, puberty is also influenced by insulin resistance. In mouse models, an interaction between insulin and leptin signaling was reported during the peripubertal period in the neurons responsible for pubertal development [74]. Furthermore, a study in obese children reported advanced onset of puberty after metformin therapy—a drug that decreases insulin resistance [75]. Therefore, there seems to be a bidirectional interaction between insulin resistance and puberty.
The compensatory increase in insulin secretion during puberty may be blunted in non-Hispanic and Hispanic youths, thus increasing their risk for T2D around the time of puberty [21, 76,77,78]. This points toward genetic factors modulating both insulin resistance and insulin secretion [78, 79].
Furthermore, other factors influencing insulin resistance have been identified in children. Hormones secreted by the muscle, such as irisin, are also related to insulin resistance [80]. A chronic inflammatory process is also likely involved in the relationship between obesity and insulin resistance, since inflammation increases insulin resistance through different pathways [81]. A disturbed secretion of adipocytokines and inflammatory markers could be observed especially in mesenteric fat [72, 81]. Therefore, it is not surprising that some studies in children and adolescents reported a stronger correlation between waist circumference and insulin resistance than the correlation between body mass index (BMI) and insulin resistance [82,83,84,85].
Normal Values for Insulin Resistance
There are currently no internationally accepted normal values for insulin concentrations in children analyzed by age, sex, pubertal stage, and genetic background available. This lack of normal values makes it difficult even for research measurements using rigorous approaches—such as euglycemic hyperinsulinemic clamp, the frequently sampled IV glucose tolerance test, and steady-state plasma glucose—to define at which exact cut point insulin resistance starts. Normal values for HOMA have been reported [40], but the proposed cutoffs are not adjusted for pubertal stage. Normal values for insulin adapted to pubertal stage have been proposed (for example, definition of insulin resistance by fasting insulin: ≥15 mU/l prepubertal, ≥30 mU/l pubertal, ≥20 mU/l late/postpubertal) [77]. However, studies validating these proposed cutoffs are missing.
Insulin Resistance as an Independent Cardiovascular Risk Factor
Classical cardiovascular risk factors—such as hypertension, dyslipidemia, and impaired glucose tolerance—are related to morbidity and mortality of obesity [15, 86]. Even though they are all based at least in part on insulin resistance, the use of insulin resistance itself as a treatment goal, rather than management of classical cardiovascular risk factors, is only meaningful if insulin resistance is itself related to morbidity and mortality.
An independent effect of insulin resistance on cardiovascular risk in children has been suggested. Fasting insulin levels in 6- to 9-year-old children predicted their blood pressure at age 9–15 years [87]; and in 5- to 9-year-old Pima Indian children, fasting insulin was associated with the level of weight gain during the subsequent 9 years of childhood [88]. The Bogalusa Heart Study has shown a strong relationship over an 8-year period between persistently high fasting insulin levels and the development of cardiovascular risk factors in children and young adults [89]. In studies of insulin resistance in childhood that used the euglycemic insulin clamp, an important independent association of both body fatness and insulin resistance with increased cardiovascular risk factors was shown, as well as an interaction between body fatness and insulin resistance, so that the presence of both was associated with a level of cardiovascular risk greater than that expected with either fatness or insulin resistance alone [90]. However, none of these studies prove that insulin resistance itself, and not the associated classical cardiovascular risk factors, is related to morbidity and mortality.
Indeed, the role of insulin in the development of cardiovascular morbidity remains controversial. Several lines of evidence suggest insulin may directly promote cardiovascular pathology. Insulin stimulates mitogen-activated protein kinase, mitogenesis, and plasminogen activator inhibitor-1 within vascular smooth muscle cells [91] and stimulates endothelin-1 production, with subsequent vascular smooth muscle growth [92]. Insulin stimulates ras-p21 in vascular smooth muscle, which promotes increased effects of other growth factors, such as platelet-derived growth factor [93]. The vascular endothelial cell insulin receptor knockout mouse has lower blood pressure and endothelin-1 levels than its wild-type counterpart [94].
Conversely, other lines of evidence suggest that insulin may be antiatherogenic: Insulin inhibits the inflammatory transcription factor nuclear factor-κ(kappa)B [95] and decreases tumor necrosis factor-α(alpha) [96]. As with other hormone-receptor interactions, the duration and amplitude of insulin effects may play a role, because chronic hyperstimulation by excessive ligand may lead to alternative cellular responses (e.g., cortisol) or tachyphylaxis (e.g., opioids), which would alter hormone action.
Furthermore, not all patients with insulin resistance develop MetS [97]. Therefore, in addition to obesity, other metabolic and pathological factors (inflammatory factors, adipocytokines, cortisol, oxidative stress, vascular factors, heredity, and lifestyle factors) are operative in this process [17].
Studies Treating Insulin Resistance
There are several studies in childhood demonstrating an improvement of insulin resistance by lifestyle intervention, weight loss, and increased physical activity [98,99,100]. However, all these studies are based on indices, such as HOMA, and not on the gold standard euglycemic hyperinsulinemic clamp or other rigorous measures of insulin sensitivity.
Some studies demonstrated a positive effect of metformin on insulin resistance and the associated cardiovascular risk factors [14, 22, 23]. However, other randomized controlled trails reported no effect [24, 25]. This may be explained by the fact that children in the untreated control group move from mid- to late puberty as the age ranges of these studies suggest. This change of pubertal status is associated with an improvement of cardiovascular risk factors (see above) [101].
Arguments for Using Insulin Resistance as Treatment Goal
There are some important arguments for using insulin resistance as a treatment goal (see Fig. 17.1). First, all cardiovascular risk factors determining morbidity and mortality in obesity are related to insulin resistance; it is clear that insulin-resistant obese children have significantly greater cardiovascular risk profiles, including the metabolic syndrome [17, 90]. Initial observations suggest a relationship between insulin resistance and arterial stiffness in youth [102, 103]. A role for insulin resistance in the early abnormalities of vascular smooth muscle is proposed based on the observation that circulating biomarkers of endothelial dysfunction (intercellular adhesion molecule and E-selectin) are highest, whereas the antiatherogenic adipocytokine adiponectin is lowest among the most insulin-resistant youths [104]. Furthermore, insulin resistance is a risk factor for prediabetes and type 2 diabetes in adults [14].
Improving insulin resistance leads to normalization of all cardiovascular risk factors [98, 105] and diabetes risk. Weight loss and increased physical activity improve insulin resistance [6, 105,106,107,108,109,110,111,112,113,114,115,116]. These changes in insulin resistance paralleled the changes in cardiovascular risk factors during puberty [63, 101, 117] in both non-Hispanic whites [101] and Afro-Caribbean girls [118].
Arguments Against Using Insulin Resistance as Treatment Goal
Even if the concept of insulin resistance and its association with cardiovascular risk factors is convincing, there are several shortcomings in the definition and measurement of insulin resistance that make it impossible to use insulin resistance as treatment goal in the clinical setting (see Fig. 17.1). Furthermore, there is a lack of evidence in childhood that insulin resistance has a higher cardiovascular risk than the sum of the classical cardiovascular risk factors, such as hypertension, dyslipidemia, and impaired glucose tolerance. Additionally, the degree of insulin resistance is not stable in adolescents and there are no approved drugs for this indication available for children.
Problem of Measurements
Today there is no availability of an accurate, reliable, reproducible, and easily applicable method of measurement of insulin resistance [14]. It is impractical to use any methods requiring multiple samples because of the complexity, time, and cost of testing. Fasting insulin as an index of insulin resistance or insulin resistance indices such as HOMA or Matsuda may be applicable in epidemiological studies using large populations of children and/or a well-defined cohort, but not on the individual level [14].
Problem of Cutoffs
Even if a uniformly reliable insulin assay became available, separate standards would need to be developed by sex, ethnic group, and pubertal stage [14, 101]. Without such specific cutoffs, treatment goals based on insulin resistance cannot be determined. However, the use of cutoff points for insulin resistance in the absence of longitudinal outcome studies represents a major concern, since this implies that values above the specified thresholds are associated with excess risk—although the rationale for the different cutoff points has never been delineated in children and adolescents [12]. Moreover, the artificial dichotomization of continuous variables, such as insulin resistance, seems debatable since dichotomization leads to an unnecessary loss of information [119]. In fact, insulin resistance is not even linear, which opens up the issue of how risk might be weighted more appropriately.
Indeed, the use of rigid cutoff points, such as in the definition of MetS for cardiovascular risk factors and insulin resistance, reduces its prognostic value in both adults and children. Mente and colleagues reported an underestimation of myocardial infarction in adults using the dichotomous variable MetS instead of the continuous variables, blood pressure or lipids [120]. Fadini et al., as well as Baldassare and colleagues, reported no increased risk in MetS compared to the sum of its individual components based on carotid intima-media thickness (cIMT) measurements. CIMT is a noninvasive, reliable, and predictive marker for early atherosclerotic changes [121, 122]. We have recently reported that the sum of the individual components of the different MetS definitions was superior to predict presence of increased cIMT in obese adolescents compared to the all-or-nothing variable: occurrence of MetS [123]. Furthermore, adding the MetS indicator to the individual components added no additional information to prediction of increased cIMT [123, 124].
Problem of Predictive Value
There are very limited longitudinal data on whether insulin resistance in childhood predicts the development of impaired glucose tolerance (IGT) and type 2 diabetes mellitus later in life [14]. A recent longitudinal study has shown that obese adolescents progressing to IGT manifest primary defects in β(beta)-cell function that are aggravated by a progressive increase in insulin resistance [125]. However, another study reported a low predictive value of impaired glucose tolerance for later type 2 diabetes in the next 3–5 years in adolescents. Furthermore, the high reversion rate (66% to 75%) to normal glucose tolerance in youth contrasts to a conversion rate of 30% from impaired glucose tolerance to type 2 diabetes in 5 years in adults [126, 127]. These findings may be attributed, at least in part, to the fact that many adolescents in the longitudinal studies move from mid- to late or postpuberty [35, 56]. Moreover, there also seems to be a genetic contribution, since in Sweden impaired fasting glucose is more frequent than in mid-European countries and conversion to type 2 diabetes more frequent [128, 129].
There are no studies that directly measure in vivo insulin resistance and its relationship to atherosclerotic abnormalities in children. Furthermore, studies reported that insulin resistance measured by HOMA was not a better predictor of increased cIMT than BMI alone [130]. Accordingly, some studies reported that cardiovascular risk factors correlated stronger to degree of overweight than insulin resistance [1, 131]. Obese children and adults without cardiovascular risk factors have been classified as metabolic healthy obese [82, 132, 133]. A total of 6–40% of obese adults [134, 135] and 6–36% of obese children [82,83,84,85] are metabolically healthy. However, longitudinal studies have demonstrated that even obese children without cardiovascular risk factors can switch to an unhealthy metabolic state without change in their weight status [1, 101]. Also in adults, the status of metabolic healthy—characterized by the absence of insulin resistance and cardiovascular risk factors—is not a steady state [136], questioning the whole concept of metabolic healthy since there is no evidence for decreased mortality [83,84,85].
While autopsy studies have shown that the extent of early atherosclerosis of the aorta and coronary arteries is directly associated with levels of lipids, blood pressure, and obesity in childhood and adolescence, this evidence is lacking for insulin resistance [137, 138]. In conclusion, up to now no outcome study in childhood has proven an increased mortality or morbidity due to insulin resistance [12, 139].
Problem of Approved Drugs
Even though metformin improves insulin resistance in several studies in children [14, 22, 23], no consistent metabolic effect or change in cardiovascular risk factors has been demonstrated and it has to be stressed that metformin has not been approved for the treatment of children with insulin resistance.
Summary
The reported prevalences of hypertension, dyslipidemia, and disturbed glucose metabolism in obese children and adolescents underline the necessity for screening, since most of these disorders are asymptomatic but related to later cardiovascular disease. Indications for treatment, including antihypertensive and lipid- or glucose-lowering drugs and bariatric surgery, should be based on weighing of the cardiovascular risk factors themselves, keeping in mind the pubertal stage, rather than on one single variable, such as insulin resistance. Since puberty and genetics influence insulin resistance, it is questionable to use definitions of insulin resistance in adolescents not accounting for pubertal stage and ethnic background. Furthermore, we do not currently have feasible and reliable measurements of insulin resistance that can be used in clinical practice; surrogate measures, such as fasting insulin, are poor estimates of insulin sensitivity [14]. There is also a lack of validated cutoffs to define insulin resistance in children. Because of these limitations, there is no justification for treating insulin resistance in children, though insulin resistance is associated with cardiovascular risk factor, MetS, prediabetes, type 2 diabetes, as well as polycystic ovarian syndrome and fatty liver disease [14]. Therefore, the mere presence of these abnormalities should call for intervention to treat the associated obesity by lifestyle intervention, surgery, or medications to reduce weight or improve insulin sensitivity without a need to measure insulin resistance [14].
Future research should aim at the following:
-
1.
How to best measure insulin sensitivity in children and adolescents
-
2.
Standardization of insulin measurements
-
3.
Identification of strong surrogate biomarkers of insulin resistance
-
4.
The potential role of both lifestyle intervention and medications in the prevention and treatment of insulin resistance
Having a uniform internationally accepted definition of insulin resistance for children and adolescents adjusted by sex, ethnic background, and pubertal stage would be very helpful for the description of populations in different studies. What is probably needed is not a dichotomous definition of insulin resistance but a more complex weighted scoring system that takes into account the magnitude of all of the risk factors, their interaction, and other important patient-specific characteristics [17].
References
I’Allemand D, Wiegand S, Reinehr T, Muller J, Wabitsch M, Widhalm K, et al. Cardiovascular risk in 26,008 European overweight children as established by a multicenter database. Obesity (Silver Spring). 2008;16(7):1672–9.
Csabi G, Torok K, Jeges S, Molnar D. Presence of metabolic cardiovascular syndrome in obese children. Eur J Pediatr. 2000;159(1–2):91–4.
Chu NF, Rimm EB, Wang DJ, Liou HS, Shieh SM. Clustering of cardiovascular disease risk factors among obese schoolchildren: the Taipei Children Heart Study. Am J Clin Nutr. 1998;67(6):1141–6.
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6 Pt 1):1175–82.
Han JC, Lawlor DA, Kimm SY. Childhood obesity. Lancet. 2010;375(9727):1737–48.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365(9468):1415–28.
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683–9.
Reaven GM. Insulin resistance and compensatory hyperinsulinemia: role in hypertension, dyslipidemia, and coronary heart disease. Am Heart J. 1991;121(4 Pt 2):1283–8.
Grundy SM. Obesity, metabolic syndrome, and coronary atherosclerosis. Circulation. 2002;105(23):2696–8.
Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485–93.
Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med. 2016;374(25):2430–40.
Reinehr T, de Sousa G, Toschke AM, Andler W. Comparison of metabolic syndrome prevalence using eight different definitions: a critical approach. Arch Dis Child. 2007;92(12):1067–72.
Vukovic R, Milenkovic T, Mitrovic K, Todorovic S, Plavsic L, Vukovic A, et al. Preserved insulin sensitivity predicts metabolically healthy obese phenotype in children and adolescents. Eur J Pediatr. 2015;174(12):1649–55.
Levy-Marchal C, Arslanian S, Cutfield W, Sinaiko A, Druet C, Marcovecchio ML, et al. Insulin resistance in children: consensus, perspective, and future directions. J Clin Endocrinol Metab. 2010;95(12):5189–98.
Reaven GM. Pathophysiology of insulin resistance in human disease. Physiol Rev. 1995;75(3):473–86.
Ten S, Maclaren N. Insulin resistance syndrome in children. J Clin Endocrinol Metab. 2004;89(6):2526–39.
Steinberger J, Daniels SR, Eckel RH, Hayman L, Lustig RH, McCrindle B, et al. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2009;119(4):628–47.
Pladevall M, Singal B, Williams LK, Brotons C, Guyer H, Sadurni J, et al. A single factor underlies the metabolic syndrome: a confirmatory factor analysis. Diabetes Care. 2006;29(1):113–22.
Lass N, Kleber M, Winkel K, Wunsch R, Reinehr T. Effect of lifestyle intervention on features of polycystic ovarian syndrome, metabolic syndrome, and intima-media thickness in obese adolescent girls. J Clin Endocrinol Metab. 2011;96(11):3533–40.
Fishbein MH, Miner M, Mogren C, Chalekson J. The spectrum of fatty liver in obese children and the relationship of serum aminotransferases to severity of steatosis. J Pediatr Gastroenterol Nutr. 2003;36(1):54–61.
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362–74.
Kendall D, Vail A, Amin R, Barrett T, Dimitri P, Ivison F, et al. Metformin in obese children and adolescents: the MOCA trial. J Clin Endocrinol Metab. 2013;98(1):322–9.
Freemark M, Bursey D. The effects of metformin on body mass index and glucose tolerance in obese adolescents with fasting hyperinsulinemia and a family history of type 2 diabetes. Pediatrics. 2001;107(4):E55.
Rynders C, Weltman A, Delgiorno C, Balagopal P, Damaso L, Killen K, et al. Lifestyle intervention improves fitness independent of metformin in obese adolescents. Med Sci Sports Exerc. 2012;44(5):786–92.
Wiegand S, l’Allemand D, Hubel H, Krude H, Burmann M, Martus P, et al. Metformin and placebo therapy both improve weight management and fasting insulin in obese insulin-resistant adolescents: a prospective, placebo-controlled, randomized study. Eur J Endocrinol. 2010;163(4):585–92.
Reinehr T, Kiess W, Andler W. Insulin sensitivity indices of glucose and free fatty acid metabolism in obese children and adolescents in relation to serum lipids. Metabolism. 2005;54(3):397–402.
Hershkop K, Besor O, Santoro N, Pierpont B, Caprio S, Weiss R. Adipose insulin resistance in obese adolescents across the spectrum of glucose tolerance. J Clin Endocrinol Metab. 2016;101(6):2423–31.
Bastian W. Genes with linkage or association with type 2 diabetes mellitus. J Pediatr Endocrinol Metab. 2002;15(Suppl 1):471–84.
DeFronzo RA, Ferrannini E. The pathogenesis of non-insulin-dependent diabetes: an update. Medicine (Baltimore). 1982;61(3):125–40.
Bacha F, Saad R, Gungor N, Janosky J, Arslanian SA. Obesity, regional fat distribution, and syndrome X in obese black versus white adolescents: race differential in diabetogenic and atherogenic risk factors. J Clin Endocrinol Metab. 2003;88(6):2534–40.
Burke JP, Hale DE, Hazuda HP, Stern MP. A quantitative scale of acanthosis nigricans. Diabetes Care. 1999;22(10):1655–9.
Reinehr T. Metabolic syndrome in children and adolescents: a critical approach considering the interaction between pubertal stage and insulin resistance. Curr Diab Rep. 2016;16(1):8.
Chan CL, Pyle L, Newnes L, Nadeau KJ, Zeitler PS, Kelsey MM. Continuous glucose monitoring and its relationship to hemoglobin A1c and oral glucose tolerance testing in obese and prediabetic youth. J Clin Endocrinol Metab. 2015;100(3):902–10.
Libman IM, Barinas-Mitchell E, Bartucci A, Robertson R, Arslanian S. Reproducibility of the oral glucose tolerance test in overweight children. J Clin Endocrinol Metab. 2008;93(11):4231–7.
Kleber M, Desousa G, Papcke S, Wabitsch M, Reinehr T. Impaired glucose tolerance in obese white children and adolescents: three to five year follow-up in untreated patients. Exp Clin Endocrinol Diabetes. 2011;119(3):172–6.
Wallace TM, Matthews DR. The assessment of insulin resistance in man. Diabet Med. 2002 Jul;19(7):527–34.
Schwartz B, Jacobs DR Jr, Moran A, Steinberger J, Hong CP, Sinaiko AR. Measurement of insulin sensitivity in children: comparison between the euglycemic-hyperinsulinemic clamp and surrogate measures. Diabetes Care. 2008;31(4):783–8.
Gungor N, Saad R, Janosky J, Arslanian S. Validation of surrogate estimates of insulin sensitivity and insulin secretion in children and adolescents. J Pediatr. 2004;144(1):47–55.
Brandou F, Brun JF, Mercier J. Limited accuracy of surrogates of insulin resistance during puberty in obese and lean children at risk for altered glucoregulation. J Clin Endocrinol Metab. 2005;90(2):761–7.
Allard P, Delvin EE, Paradis G, Hanley JA, O’Loughlin J, Lavallee C, et al. Distribution of fasting plasma insulin, free fatty acids, and glucose concentrations and of homeostasis model assessment of insulin resistance in a representative sample of Quebec children and adolescents. Clin Chem. 2003;49(4):644–9.
Marcovina S, Bowsher RR, Miller WG, Staten M, Myers G, Caudill SP, et al. Standardization of insulin immunoassays: report of the American Diabetes Association Workgroup. Clin Chem. 2007;53(4):711–6.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Hrebicek J, Janout V, Malincikova J, Horakova D, Cizek L. Detection of insulin resistance by simple quantitative insulin sensitivity check index QUICKI for epidemiological assessment and prevention. J Clin Endocrinol Metab. 2002;87(1):144–7.
Penesova A, Radikova Z. Comparison of insulin sensitivity indices calculated from standard 3-sampled and frequently sampled oral glucose tolerance test. Endocr Regul. 2004;38(4):167–71.
Stumvoll M, Mitrakou A, Pimenta W, Jenssen T, Yki-Jarvinen H, Van HT, et al. Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care. 2000;23(3):295–301.
Yeckel CW, Weiss R, Dziura J, Taksali SE, Dufour S, Burgert TS, et al. Validation of insulin sensitivity indices from oral glucose tolerance test parameters in obese children and adolescents. J Clin Endocrinol Metab. 2004;89(3):1096–101.
Poulsen P, Levin K, Petersen I, Christensen K, Beck-Nielsen H, Vaag A. Heritability of insulin secretion, peripheral and hepatic insulin action, and intracellular glucose partitioning in young and old Danish twins. Diabetes. 2005;54(1):275–83.
Arslanian SA, Bacha F, Saad R, Gungor N. Family history of type 2 diabetes is associated with decreased insulin sensitivity and an impaired balance between insulin sensitivity and insulin secretion in white youth. Diabetes Care. 2005;28(1):115–9.
Goran MI, Bergman RN, Cruz ML, Watanabe R. Insulin resistance and associated compensatory responses in african-american and Hispanic children. Diabetes Care. 2002;25(12):2184–90.
Whincup PH, Gilg JA, Papacosta O, Seymour C, Miller GJ, Alberti KG, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ. 2002;324(7338):635.
Goran MI, Gower BA. Longitudinal study on pubertal insulin resistance. Diabetes. 2001;50(11):2444–50.
Yin J, Li M, Xu L, Wang Y, Cheng H, Zhao X, et al. Insulin resistance determined by Homeostasis Model Assessment (HOMA) and associations with metabolic syndrome among Chinese children and teenagers. Diabetol Metab Syndr. 2013;5(1):71.
Hannon TS, Janosky J, Arslanian SA. Longitudinal study of physiologic insulin resistance and metabolic changes of puberty. Pediatr Res. 2006;60(6):759–63.
Goran MI, Shaibi GQ, Weigensberg MJ, Davis JN, Cruz ML. Deterioration of insulin sensitivity and beta-cell function in overweight Hispanic children during pubertal transition: a longitudinal assessment. Int J Pediatr Obes. 2006;1(3):139–45.
Reinehr T, Wabitsch M, Kleber M, de Sousa G, Denzer C, Toschke AM. Parental diabetes, pubertal stage, and extreme obesity are the main risk factors for prediabetes in children and adolescents: a simple risk score to identify children at risk for prediabetes. Pediatr Diabetes. 2009;10(6):395–400.
Kleber M, Lass N, Papcke S, Wabitsch M, Reinehr T. One-year follow-up of untreated obese white children and adolescents with impaired glucose tolerance: high conversion rate to normal glucose tolerance. Diabet Med. 2010;27(5):516–21.
Kelly LA, Lane CJ, Weigensberg MJ, Toledo-Corral CM, Goran MI. Pubertal changes of insulin sensitivity, acute insulin response, and beta-cell function in overweight Latino youth. J Pediatr. 2011;158(3):442–6.
Brufani C, Tozzi A, Fintini D, Ciampalini P, Grossi A, Fiori R, et al. Sexual dimorphism of body composition and insulin sensitivity across pubertal development in obese Caucasian subjects. Eur J Endocrinol. 2009;160(5):769–75.
Pinhas-Hamiel O, Lerner-Geva L, Copperman NM, Jacobson MS. Lipid and insulin levels in obese children: changes with age and puberty. Obesity (Silver Spring). 2007;15(11):2825–31.
Raab J, Haupt F, Kordonouri O, Scholz M, Wosch A, Ried C, et al. Continuous rise of insulin resistance before and after the onset of puberty in children at increased risk for type 1 diabetes – a cross-sectional analysis. Diabetes Metab Res Rev. 2013;29(8):631–5.
Jeffery AN, Metcalf BS, Hosking J, Streeter AJ, Voss LD, Wilkin TJ. Age before stage: insulin resistance rises before the onset of puberty: a 9-year longitudinal study (EarlyBird 26). Diabetes Care. 2012 Mar;35(3):536–41.
Pilia S, Casini MR, Foschini ML, Minerba L, Musiu MC, Marras V, et al. The effect of puberty on insulin resistance in obese children. J Endocrinol Invest. 2009;32(5):401–5.
Xu L, Li M, Yin J, Cheng H, Yu M, Zhao X, et al. Change of body composition and adipokines and their relationship with insulin resistance across pubertal development in obese and nonobese Chinese children: the BCAMS Study. Int J Endocrinol. 2012;2012:389108.
Pilia S, Casini MR, Foschini ML, Minerba L, Musiu MC, Marras V, et al. The effect of puberty on insulin resistance in obese children. J Endocrinol Invest. 2009 May;32(5):401–5.
Hainan E. Diabetes and puberty. Am J Nurs. 2014 Oct;114(10):12.
Moran A, Jacobs DR Jr, Steinberger J, Cohen P, Hong CP, Prineas R, et al. Association between the insulin resistance of puberty and the insulin-like growth factor-I/growth hormone axis. J Clin Endocrinol Metab. 2002 Oct;87(10):4817–20.
Chu L, Riddell MC, Schneiderman JE, McCrindle BW, Hamilton JK. The effect of puberty on fat oxidation rates during exercise in overweight and normal-weight girls. J Appl Physiol. 2014;116(1):76–82.
Spruijt-Metz D, Belcher BR, Hsu YW, McClain AD, Chou CP, Nguyen-Rodriguez S, et al. Temporal relationship between insulin sensitivity and the pubertal decline in physical activity in peripubertal Hispanic and African American females. Diabetes Care. 2013 Nov;36(11):3739–45.
Kayser BD, Toledo-Corral CM, Alderete TL, Weigensberg MJ, Goran MI. Temporal relationships between adipocytokines and diabetes risk in Hispanic adolescents with obesity. Obesity (Silver Spring). 2015;23(7):1479–85.
Agirbasli M, Agaoglu NB, Orak N, Caglioz H, Ocek T, Poci N, et al. Sex hormones and metabolic syndrome in children and adolescents. Metabolism. 2009;58(9):1256–62.
Jurimae J, Gruodyte R, Saar M, Cicchella A, Stefanelli C, Passariello C, et al. Plasma visfatin and adiponectin concentrations in physically active adolescent girls: relationships with insulin sensitivity and body composition variables. J Pediatr Endocrinol Metab. 2011;24(7–8):419–25.
Koerner A, Kratzsch J, Kiess W. Adipocytokines: leptin--the classical, resistin--the controversial, adiponectin--the promising, and more to come. Best Pract Res Clin Endocrinol Metab. 2005;19(4):525–46.
Sorensen K, Aksglaede L, Munch-Andersen T, Aachmann-Andersen NJ, Petersen JH, Hilsted L, et al. Sex hormone-binding globulin levels predict insulin sensitivity, disposition index, and cardiovascular risk during puberty. Diabetes Care. 2009;32(5):909–14.
Qiu X, Dao H, Wang M, Heston A, Garcia KM, Sangal A, et al. Insulin and leptin signaling interact in the mouse Kiss1 neuron during the peripubertal period. PLoS One. 2015;10(5):e0121974.
Astiz S, Gonzalez-Bulnes A, Astiz I, Barbero A, Perez-Solana ML, Garcia-Real I. Advanced onset of puberty after metformin therapy in swine with thrifty genotype. Exp Physiol. 2014;99(9):1241–52.
Adam TC, Hasson RE, Lane CJ, Davis JN, Weigensberg MJ, Spruijt-Metz D, et al. Fasting indicators of insulin sensitivity: effects of ethnicity and pubertal status. Diabetes Care. 2011;34(4):994–9.
Viner RM, Segal TY, Lichtarowicz-Krynska E, Hindmarsh P. Prevalence of the insulin resistance syndrome in obesity. Arch Dis Child. 2005 Jan;90(1):10–4.
Dowling AR, Nedorezov LB, Qiu X, Marino JS, Hill JW. Genetic factors modulate the impact of pubertal androgen excess on insulin sensitivity and fertility. PLoS One. 2013;8(11):e79849.
Reinehr T, Toschke AM. Onset of puberty and cardiovascular risk factors in untreated obese children and adolescents: a 1-year follow-up study. Arch Pediatr Adolesc Med. 2009;163(8):709–15.
Reinehr T, Elfers C, Lass N, Roth CL. Irisin and its relation to insulin resistance and puberty in obese children: a longitudinal analysis. J Clin Endocrinol Metab. 2015;100(5):2123–30.
Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006;17(1):4–12.
Prince RL, Kuk JL, Ambler KA, Dhaliwal J, Ball GD. Predictors of metabolically healthy obesity in children. Diabetes Care. 2014;37(5):1462–8.
Bokor S, Frelut ML, Vania A, Hadjiathanasiou CG, Anastasakou M, Malecka-Tendera E, et al. Prevalence of metabolic syndrome in European obese children. Int J Pediatr Obes. 2008;3(Suppl 2):3–8.
Cruz ML, Weigensberg MJ, Huang TT, Ball G, Shaibi GQ, Goran MI. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J Clin Endocrinol Metab. 2004;89(1):108–13.
Shaibi GQ, Goran MI. Examining metabolic syndrome definitions in overweight Hispanic youth: a focus on insulin resistance. J Pediatr. 2008;152(2):171–6.
Ruige JB, Assendelft WJ, Dekker JM, Kostense PJ, Heine RJ, Bouter LM. Insulin and risk of cardiovascular disease: a meta-analysis. Circulation. 1998;97(10):996–1001.
Taittonen L, Uhari M, Nuutinen M, Turtinen J, Pokka T, Akerblom HK. Insulin and blood pressure among healthy children. Cardiovascular risk in young Finns. Am J Hypertens. 1996;9(3):194–9.
Odeleye OE, de Courten M, Pettitt DJ, Ravussin E. Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children. Diabetes. 1997;46(8):1341–5.
Bao W, Srinivasan SR, Berenson GS. Persistent elevation of plasma insulin levels is associated with increased cardiovascular risk in children and young adults. The Bogalusa Heart Study. Circulation. 1996;93(1):54–9.
Sinaiko AR, Steinberger J, Moran A, Prineas RJ, Vessby B, Basu S, et al. Relation of body mass index and insulin resistance to cardiovascular risk factors, inflammatory factors, and oxidative stress during adolescence. Circulation. 2005;111(15):1985–91.
Begum N, Song Y, Rienzie J, Ragolia L. Vascular smooth muscle cell growth and insulin regulation of mitogen-activated protein kinase in hypertension. Am J Physiol. 1998;275(1 Pt 1):C42–9.
Nagai M, Kamide K, Rakugi H, Takiuchi S, Imai M, Kida I, et al. Role of endothelin-1 induced by insulin in the regulation of vascular cell growth. Am J Hypertens. 2003;16(3):223–8.
Goalstone ML, Natarajan R, Standley PR, Walsh MF, Leitner JW, Carel K, et al. Insulin potentiates platelet-derived growth factor action in vascular smooth muscle cells. Endocrinology. 1998;139(10):4067–72.
Vicent D, Ilany J, Kondo T, Naruse K, Fisher SJ, Kisanuki YY, et al. The role of endothelial insulin signaling in the regulation of vascular tone and insulin resistance. J Clin Invest. 2003;111(9):1373–80.
Dandona P, Aljada A, Mohanty P, Ghanim H, Hamouda W, Assian E, et al. Insulin inhibits intranuclear nuclear factor kappaB and stimulates IkappaB in mononuclear cells in obese subjects: evidence for an anti-inflammatory effect? J Clin Endocrinol Metab. 2001;86(7):3257–65.
Fraker DL, Merino MJ, Norton JA. Reversal of the toxic effects of cachectin by concurrent insulin administration. Am J Physiol. 1989;256(6 Pt 1):E725–31.
Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003;163(4):427–36.
Reinehr T, Lass N, Toschke C, Rothermel J, Lanzinger S, Holl RW. Which amount of BMI-SDS reduction is necessary to improve cardiovascular risk factors in overweight children? J Clin Endocrinol Metab. 2016;101(8):3171–9.
Savoye M, Nowicka P, Shaw M, Yu S, Dziura J, Chavent G, et al. Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics. 2011;127(3):402–10.
Oude LH, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;1:CD001872.
Reinehr T, Wolters B, Knop C, Lass N, Holl RW. Strong effect of pubertal status on metabolic health in obese children: a longitudinal study. J Clin Endocrinol Metab. 2015;100(1):301–8.
Gungor N, Thompson T, Sutton-Tyrrell K, Janosky J, Arslanian S. Early signs of cardiovascular disease in youth with obesity and type 2 diabetes. Diabetes Care. 2005;28(5):1219–21.
Reinehr T, Wunsch R. Intima media thickness-related risk factors in childhood obesity. Int J Pediatr Obes. 2011;6(Suppl 1):46–52.
Lee S, Gungor N, Bacha F, Arslanian S. Insulin resistance: link to the components of the metabolic syndrome and biomarkers of endothelial dysfunction in youth. Diabetes Care. 2007;30(8):2091–7.
Reinehr T, Kiess W, Kapellen T, Andler W. Insulin sensitivity among obese children and adolescents, according to degree of weight loss. Pediatrics. 2004;114(6):1569–73.
Reinehr T, de Sousa G, Andler W. Longitudinal analyses among overweight, insulin resistance, and cardiovascular risk factors in children. Obes Res. 2005;13(10):1824–33.
Reinehr T, de Sousa G, Toschke AM, Andler W. Long-term follow-up of cardiovascular disease risk factors in children after an obesity intervention. Am J Clin Nutr. 2006;84(3):490–6.
Sung RY, Yu CW, Chang SK, Mo SW, Woo KS, Lam CW. Effects of dietary intervention and strength training on blood lipid level in obese children. Arch Dis Child. 2002;86(6):407–10.
Reinehr T, Andler W. Changes in the atherogenic risk factor profile according to degree of weight loss. Arch Dis Child. 2004;89(5):419–22.
Coppen AM, Risser JA, Vash PD. Metabolic syndrome resolution in children and adolescents after 10 weeks of weight loss. J Cardiometab Syndr. 2008;3(4):205–10.
Reinehr T, Kleber M, Toschke AM. Lifestyle intervention in obese children is associated with a decrease of the metabolic syndrome prevalence. Atherosclerosis. 2009;207(1):174–80.
Savoye M, Shaw M, Dziura J, Tamborlane WV, Rose P, Guandalini C, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA. 2007;297(24):2697–704.
Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002;347(19):1483–92.
Uusitupa M, Laakso M, Sarlund H, Majander H, Takala J, Penttila I. Long term effects of a very low calorie diet on metabolic control and cardiovascular risk factors in the treatment of obese non-insulin-dependent diabetics. Int J Obes (Lond). 1989;13(Suppl 2):163–4.
Skov AR, Toubro S, Ronn B, Holm L, Astrup A. Randomized trial on protein vs carbohydrate in ad libitum fat reduced diet for the treatment of obesity. Int J Obes Relat Metab Disord. 1999;23(5):528–36.
Inoue DS, De Mello MT, Foschini D, Lira FS, De Piano GA, Da Silveira Campos RM, et al. Linear and undulating periodized strength plus aerobic training promote similar benefits and lead to improvement of insulin resistance on obese adolescents. J Diabetes Complications. 2015;29(2):258–64.
Tobisch B, Blatniczky L, Barkai L. Cardiometabolic risk factors and insulin resistance in obese children and adolescents: relation to puberty. Pediatr Obes. 2015;10(1):37–44.
Boyne MS, Thame M, Osmond C, Fraser RA, Gabay L, Taylor-Bryan C, et al. The effect of earlier puberty on cardiometabolic risk factors in Afro-Caribbean children. J Pediatr Endocrinol Metab. 2014;27(5–6):453–60.
Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med. 2006;25(1):127–41.
Mente A, Yusuf S, Islam S, McQueen MJ, Tanomsup S, Onen CL, et al. Metabolic syndrome and risk of acute myocardial infarction a case-control study of 26,903 subjects from 52 countries. J Am Coll Cardiol. 2010;55(21):2390–8.
Baldassarre D, Werba JP, Castelnuovo S, Frigerio B, Amato M, Ravani A, et al. The metabolic syndrome predicts carotid intima-media thickness no better than the sum of individual risk factors in a lipid clinic population. Atherosclerosis. 2010;210(1):214–9.
Fadini GP, Coracina A, Inchiostro S, Tiengo A, Avogaro A, de Kreutzenberg SV. A stepwise approach to assess the impact of clustering cardiometabolic risk factors on carotid intima-media thickness: the metabolic syndrome no-more-than-additive. Eur J Cardiovasc Prev Rehabil. 2008;15(2):190–6.
Reinehr T, Wunsch R, Putter C, Scherag A. Relationship between carotid intima-media thickness and metabolic syndrome in adolescents. J Pediatr. 2013;163(2):327–32.
Reinehr T, Wunsch R, de Sousa G, Toschke AM. Relationship between metabolic syndrome definitions for children and adolescents and intima-media thickness. Atherosclerosis. 2008;199(1):193–200.
Cali AM, Man CD, Cobelli C, Dziura J, Seyal A, Shaw M, et al. Primary defects in beta-cell function further exacerbated by worsening of insulin resistance mark the development of impaired glucose tolerance in obese adolescents. Diabetes Care. 2009;32(3):456–61.
Rasmussen SS, Glumer C, Sandbaek A, Lauritzen T, Borch-Johnsen K. Progression from impaired fasting glucose and impaired glucose tolerance to diabetes in a high-risk screening programme in general practice: the ADDITION Study, Denmark. Diabetologia. 2007;50(2):293–7.
Rasmussen SS, Glumer C, Sandbaek A, Lauritzen T, Borch-Johnsen K. Determinants of progression from impaired fasting glucose and impaired glucose tolerance to diabetes in a high-risk screened population: 3 year follow-up in the ADDITION study, Denmark. Diabetologia. 2008;51(2):249–57.
Hagman E, Reinehr T, Kowalski J, Ekbom A, Marcus C, Holl RW. Impaired fasting glucose prevalence in two nationwide cohorts of obese children and adolescents. Int J Obes (Lond). 2014;38(1):40–5.
Hagman E, Danielsson P, Brandt L, Ekbom A, Marcus C. Association between impaired fasting glycaemia in pediatric obesity and type 2 diabetes in young adulthood. Nutr Diabetes. 2016;6(8):e227.
Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation. 2010 Oct 19;122(16):1604–11.
Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373(14):1307–17.
Bluher M. Are there still healthy obese patients? Curr Opin Endocrinol Diabetes Obes. 2012;19(5):341–6.
Bluher M. The distinction of metabolically ‘healthy’ from ‘unhealthy’ obese individuals. Curr Opin Lipidol. 2010;21(1):38–43.
Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Targher G, et al. Prevalence of insulin resistance in metabolic disorders: the Bruneck Study. Diabetes. 1998;47(10):1643–9.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med. 2008;168(15):1617–24.
Mongraw-Chaffin M, Foster MC, Kalyani RR, Vaidya D, Burke GL, Woodward M, et al. Obesity severity and duration are associated with incident metabolic syndrome: evidence against metabolically healthy obesity from the Multi-Ethnic Study of Atherosclerosis. J Clin Endocrinol Metab. 2016;101(11):4117–24.
McGill HC Jr, McMahan CA, Zieske AW, Tracy RE, Malcom GT, Herderick EE, et al. Association of Coronary Heart Disease Risk Factors with microscopic qualities of coronary atherosclerosis in youth. Circulation. 2000;102(4):374–9.
McGill HC Jr, McMahan CA, Herderick EE, Tracy RE, Malcom GT, Zieske AW, et al. Effects of coronary heart disease risk factors on atherosclerosis of selected regions of the aorta and right coronary artery. PDAY Research Group. Pathobiological Determinants of Atherosclerosis in Youth. Arterioscler Thromb Vasc Biol. 2000;20(3):836–45.
Brambilla P, Lissau I, Flodmark CE, Moreno LA, Widhalm K, Wabitsch M, et al. Metabolic risk-factor clustering estimation in children: to draw a line across pediatric metabolic syndrome. Int J Obes (Lond). 2007;31(4):591–600.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Reinehr, T. (2020). Is Insulin Resistance a Treatment Target?. In: Zeitler, P., Nadeau, K. (eds) Insulin Resistance. Contemporary Endocrinology. Humana, Cham. https://doi.org/10.1007/978-3-030-25057-7_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-25057-7_17
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-25055-3
Online ISBN: 978-3-030-25057-7
eBook Packages: MedicineMedicine (R0)