Abstract
Cardiac resynchronization therapy (CRT) can be delivered by either a CRT pacemaker (CRT-P) or a CRT defibrillator (CRT-D). No randomized control trial has ever been powered to compare the two device types; therefore cardiology society guidelines provide limited recommendations on choice of device. In this chapter we review the evidence for selecting a CRT-P or a CRT-D in individual patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Cardiac resynchronization therapy (CRT) can be delivered through CRT pacemaker devices (CRP-P) or CRTs with a defibrillator component (CRT-P). Most patients with heart failure who qualify for a CRT device also have an overlapping indication for primary prophylaxis against sudden arrhythmic death with an implantable cardioverter-defibrillator (ICD) [1, 2]. Therefore, clinicians must frequently decide whether an individual patient should receive a CRT-P or a CRT-D.
A recent survey of 11,088 patients undergoing CRT implantation conducted in Europe by the European Society of Cardiology (ESC) showed that 70% of patients were implanted with a CRT-D device and 30% with a CRT-P [3]. However, when analyzing individual countries, the percentage of CRT-P ranged from 2% to 88% [4].
International Guideline Recommendations
There is limited specific advice in international guidelines regarding the choice of device type. The ESC European Heart Rhythm Association (EHRA) guidelines suggest implanting a CRT-D in patients with a life expectancy >1 year, NYHA functional class II, ischemic heart disease, and no major comorbidities [5]. They recommend selecting a CRT-P in patients with advanced heart failure, severe renal insufficiency or dialysis, and other major comorbidities including frailty and cachexia. The 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death recommend implanting a CRT-D for prevention of sudden cardiac death (SCD) in heart failure patients in NYHA class II if their QRS is ≥130 ms, with LBBB and a LVEF ≤30% [2]. Another ESC association guideline—the Heart Failure Association (HFA) —states that, if the primary reason for implanting a CRT is to improve prognosis, most evidence lies with CRT-D for patients with NYHA functional class II and with CRT-P for patients in NYHA functional classes III to IV. If the primary reason for implanting the device is relief from symptoms, HFA guidelines propose that the clinician chooses between a CRT-P and a CRT-D, as he/she considers appropriate [1].
The Canadian Cardiac Society (CCS) guidelines suggest that a CRT-P be considered in patients who are not candidates for ICD therapy, such as those with a limited life expectancy because of significant comorbidities [6]. The NICE guidelines specific to the United Kingdom provide specific guidance on whether to implant a CRT-P or a CRT-D depending on NYHA class, QRS duration, and morphology, but do not consider the patient characteristics addressed by the EHRA guidelines [7]. The 2018 heart failure guidelines from Australia state that when CRT is indicated in most cases, a CRT-D is preferred, although, in patients with nonischemic heart failure, a CRT-P device may provide adequate protection. Furthermore, they state that—in patients who do not wish to have the potential for defibrillation, where the left ventricle is likely to improve, in the very elderly, or in those who retain a poorer prognosis but remain symptomatic—it would be reasonable to consider a CRT-P over a CRT-D [8]. American Cardiology Society recommendations relating to CRT are found in the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines for the management of heart failure (2013), which were harmonized with the ACCF/AHA/Heart Rhythm Society (HRS) 2012 focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. Neither of these guidelines provide advice on choice of device type [9,10,11]. Furthermore, since publication of the 2013 guidelines, several focused updates of heart failure have been published by ACC/AHA/Heart Failure Society of America (HFSA). These updates do not propose changes to CRT recommendations, nor do they provide advice on choice of CRT device type [12, 13].
The Evidence for Implanting CRT-D
The recommendation for implanting a defibrillator in patients with symptomatic heart failure and reduced ejection fraction was based on the results of two large trials: the Multicenter Automatic Defibrillator Implantation Trial II (MADIT II) and the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) [14, 15]. In MADIT II 1232 patients with prior myocardial infraction and LVEF ≤30% were randomly assigned in a 3:2 ratio to receive an ICD or optimal medical therapy (OMT) . [15] In the SCD-HeFT 2521 patients with NYHA class II or II heart failure and an LVEF ≤35% were randomized to OMT, OMT and amiodarone, and OMT and ICD. Both these trials showed significantly improved survival in the patient group implanted with a defibrillator. ICDs are therefore recommended as prophylactic therapy for patients with symptomatic heart failure if their left ventricular ejection fraction is ≤35% [2]. A logical extrapolation would therefore be that in the patient group with a wide QRS qualifying for CRT, the preferred choice would be a CRT-D.
The Evidence for Implanting a CRT-P vs. a CRT-D
The Evidence for CRT-P Alone
One of the pivotal CRT trials, CARE HF, randomized 813 patients to OMT with or without CRT. This trial convincingly demonstrated a reduction in total mortality with CRT compared with optimal medical therapy in eligible patients [16]. In the extended follow-up dataset, CRT-P was associated with a reduction in sudden cardiac death closely correlated to LV reverse remodeling [17, 18]. In addition, the REVERSE study that randomized 610 patients with mild heart failure to active or inactive CRT therapy demonstrated that significant reverse LV remodeling was associated with a reduction in ventricular tachycardia (VT). [19]. Furthermore, in the MADIT-CRT trial where 1820 patients with EF ≤30% and QRS >130 ms with mild heart failure were randomized to CRT-D or ICD, reverse remodeling was also associated with a significant reduction in the risk of subsequent life-threatening VT [20].
Therefore, the question remains: Does the addition of a defibrillator offer additional protection to these patients receiving a CRT device? Furthermore, if CRT-D patients need their device replaced, should they perhaps receive a CRT-P instead? This is an important question to answer, as the addition of the defibrillator component is not without potential adverse procedural complications including the risk of inappropriate shocks [21, 22]. In the follow-up analysis of the MADIT II trial (ICD vs. OMT) [15], the investigators found that 11.5% of the 719 patients receiving an ICD experienced an inappropriate shock [21]. The most common trigger for these shocks was atrial fibrillation . Noteworthily, these patients had higher mortality rates than those who did not receive inappropriate shocks (hazard ratio 2.29, p = 0.025). Another retrospective cohort study compared inappropriate shocks in 85 patients implanted with a CRT-D with 100 patients implanted with an ICD device with a follow-up period of 21 ± 13 months [23]. In this study 18 patients experienced inappropriate shocks. However, there was significantly lower rate of inappropriate shock in the CRT-D group vs. the ICD group. Again, atrial fibrillation and atrial flutter were the strongest predictors of inappropriate shocks. The authors therefore suggest that CRT, by reducing the atrial fibrillation burden in these patients, is responsible for lower rate of inappropriate shocks compared with the ICD patients.
One might also assume that implanting an ICD lead with its increased size and rigidity would lead to more periprocedural complications than implanting only the right and left ventricular CRT pacing leads. However, the evidence is conflicting. A 2013 Danish cohort study of 5918 patients with cardiac implantable electronic devices found that implantation of a CRT-D compared with a CRT-P was associated with a higher risk of complications, primarily due to lead-related re-interventions (CRT-D 4.7 vs. 2.3% CRT-P, P = 0.001) [22]. Another study looking at 1-year outcomes of 402 CRT-P and CRT-D implantations found that CRT-D patients had higher incidences of loss of capture (CRT-D 9.2% vs. 3.5% CRT-P, P = 0.01). However, in this study there were no significant differences in infections rates, rehospitalization rates, and mortality rates between the two groups [24]. Furthermore, the ESC CRT Survey II (11,088 patients) and a recent multicenter European cohort study (3008 patients) with CRT-P and CRT-D implantations found similar periprocedural complication rates between both CRT-P and CRT-D recipients [4, 25]. The CRT Survey II also reported similar adverse event rates during hospitalization and similar length of stay between the two groups [4]. This could reflect increased international implantation experience or possibly a choice for CRT-P in patients deemed at higher risk for complications. Although the periprocedural complications were the same in the European cohort study of 3008 patients, they did find significant differences between the groups in late complications in this study during a mean follow-up of 41.4 ± 29 months. The significantly higher rate of complications in the CRT-D group was particularly evident for device-related infections [25].
In addition, one must remember that in a substantial portion of patients who receive a CRT-D or ICD, the device never fires [26]. Furthermore, the defibrillator device has a higher cost than a device with only a pacemaker component and requires a more intensive follow-up program [27].
Direct Comparisons of CRT- P vs. CRT-D
No adequately powered, randomized clinical trial has compared the effect of CRT-P vs. CRT-D on long-term clinical outcomes in eligible patients. Only one head-to-head study of CRT-D vs. CRT-P has ever been published. However, this study (COMPANION) with 1520 patients was not designed to compare different CRT devices; rather, it focused on the overall concept of CRT versus optimal medical therapy . The study had three arms: OMT alone, OMT + CRT-P, or OMT with CRT-D. It established the benefit of a CRT over medical therapy in eligible patients, but was underpowered to compare any difference between the two device arms. Although total mortality was only reduced compared with medical therapy in the CRT-D arm, the CRT-P and CRT-D curves largely overlapped one another [28].
The majority of comparisons of CRT-P vs. CRT-D have been retrospective cohort studies, and these have suggested that the benefit for a CRT-D over a CRT-P may be limited to those patients with ischemic heart failure etiology. A study from a high-volume single center, comparing the mortality rates of 693 patients implanted with a CRT-P vs. 429 implanted with a CRT-D, found CRT-D to be associated with a 30% risk reduction in all-cause mortality compared with a CRT-P. However, such a mortality benefit was not observed for patients with nonischemic cardiomyopathy [27]. Another observational study of 5307 consecutive patients with CRT-P vs. CRT-D again only found improved survival in the patients with ischemic heart failure with a CRT-D. In the patients with nonischemic heart failure there was no mortality benefit from a CRT-D vs. a CRT-P [29]. In a UK cohort study of 551 patients implanted with a CRT-D versus 999 with a CRT-P, CRT-D was associated with lower mortality, heart failure hospitalizations, and hospitalizations for major acute coronary events (MACE) after stratifying for heart failure etiology; this lower mortality rate was only evident for the patients with ischemic heart failure etiology [30].
The only recent RCT of defibrillator over standard care, the DANISH study, randomized 556 patients with heart failure of nonischemic etiology with an LVEF ≤35% to either receive an ICD or usual clinical care. Despite the rate of sudden cardiac death being half in the ICD group (4.3%) compared with the control group (8.2%), this trial showed no significant difference in overall survival benefit between the two groups. There was, however, an age interaction suggesting that the benefits of ICD in patients with nonischemic etiology were limited to the younger patients (<68 years of age) [31]. In both the ICD and the control group 58% of the patients received a CRT device, and these results were independent of whether or not the patients received a CRT. Therefore, this study enabled the direct comparison of 323 CRT-P patients versus 322 CRT-D patients with ischemic heart failure etiology. The DANISH study suggests that in patients >68 years of age with heart failure due to nonischemic etiology, the increased mortality rate is not due to sudden cardiac death but rather to another mode of death for which an ICD does not improve mortality rates.
This futility of the defibrillator in patients ≥75 years of age is further supported by a study examining 775 consecutive patients undergoing CRT implantations [32]. Of the 177 patients that fulfilled the inclusion criteria, 80 were implanted with a CRT-P and 97 with a CRT-D. After 26 ± 19 months, 35% of patients had died with no significant difference between the two groups, 35% in the CRT-P and 35% in the CRT-D group (p = 0.994).
In the French CeRtiTuDe registry, 1705 recipients of either a CRT-P or a CRT-D were followed rigorously for adjudicated causes of death over 2 years [33]. Patients with CRT-P compared with CRT-D were older (mean age 76 years), were less often male, had more symptoms of heart failure, and less often had ischemic etiology, and more patients had atrial fibrillation and other comorbidities. Although in CeRtiTuDe mortality was double in the CRT-P vs. the CRT-D group, this increased mortality rate was due to non-sudden cardiac death in the CRT-P group, thereby suggesting that the patients that are routinely selected for a CRT-P would not benefit from a CRT-D.
A large single-center study published in 2016 showed results similar to the CeRtiTuDe registry, namely, that despite being younger and fitter, recipients of CRT-D systems did not have a clear mortality benefit over those that received CRT-P systems [34]. In short, CRT reduces but probably does not completely abolish the risk of sudden cardiac death . The likely mechanism is related to reverse remodeling following successful resynchronization [20].
Which Patients Are Getting Which Device Type?
The percentage of CRT-P vs. CRT-D varies greatly in different regions and countries as shown in Figs. 6.1 and 6.2 [4, 35]. In Europe the percentage of C RT-P devices ranged from as low as 2% to as high as 88%. The variation could not be explained simply by the country’s economic status, so clearly other factors are motivating physicians to make choices between CRT-P and CRT-D. In a cross-sectional study from the United States, looking at 311,086 CRT implantations, they found that 86.1% were CRT-Ds [36].
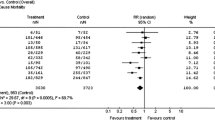
In the CRT Survey II, the CRT-P recipients were older, more commonly had NYHA functional class III–IV symptoms, were more often female, had higher NT-pro BNP levels, and more frequently had comorbidities and additional conduction tissue disease. On the other hand, patients implanted with a CRT-D device were more likely to have ischemic heart failure etiology. A large meta-analysis in patients with CRT-P vs. CRT-D comprising 44 studies and 18,874 patients found that CRT-P recipients were older, were more often female, and had higher NYHA class, with more atrial fibrillation and less ischemic heart disease. This study found an unadjusted mortality rate that was twofold higher in the patients with CRT-P with SCD representing a third of the excess mortality [37], thereby suggesting that patients with higher NYHA class and more comorbidities are being selected for CRT-P over CRT-D.
Furthermore, an analysis of data from patients >75 years of age evaluated 405 patients with a CRT-D and 107 patients with a CRT- P and found that the increased mortality of the CRT-P groups was lost when adjusting for the baseline differences between the groups. These variables included age (the CRT-P groups were older (83 years vs. 81 years, P < 0.001)) and more extensive comorbidities (Charlson index = 5 [3–6] vs. 4 [3–5], P = 0.007) [38].
How Should We Proceed?
Perhaps providing implanters with a scoring system for patient selection would assist in appropriate patient selection. A risk score called the Goldenberg risk score has been proposed to identify patients with a limited survival benefit from a CRT-D, who may therefore be implanted with a CRT-P rather than a CRT-D. This risk score includes five clinical risk factors including NYHA class >2, atrial fibrillation, QRS duration >120 ms, age >70 years, and blood urea nitrogen >26 mg/dl. In a retrospective observational cohort study of 638 patients, it was found that patients with a low score of 0–2 had a decreased mortality rate compared with a CRT-P in the first 4 years of follow-up (CRT-D 11.3 vs. CRT-P 24.7%, P = 0.041). Although this effect attenuated with longer follow-up duration (CRT-D 21.2 vs. CRT-P 32.7%, P = 0.078), no significant benefit of a CRT-D was found in those with a risk score ≥3. Such risk scores may prove useful in informing the selection of the most appropriate type of CRT device in the individual patient [39].
However, in order to properly resolve the P vs. D question, we would require a large, randomized controlled trial directly comparing the two types of CRT devices on long-term clinical outcomes. Such an ambitious trial would necessarily have to include sufficient numbers of patients to permit evaluation of the outcomes in the various clinical subgroups. Fortunately, the RESET-CRT trial is underway in Germany (ClinicalTrials.gov number NCT03494933). In this study, 2030 patients with both ischemic and nonischemic HF etiology will be randomized to a CRT-P or CRT-D with the following inclusion criteria: >18 years of age, symptomatic heart failure (NYHA class II–IV), LVEF ≤35%, on OMT, and with a class I or IIa indication for a CRT device. Patients with a previous VT episode and those with a I or IIa indication for secondary prevention of sudden cardiac death and VT with an ICD are excluded. The primary endpoint of this study is all-cause mortality. Hopefully, the results of such a trial will shed more light on this important and clinically relevant issue.
Conclusion
Faced with many competing causes of death in patients with heart failure and left ventricular dysfunction, the selection of patients who might benefit from a CRT-D is challenging. We should estimate clinically whether the patient is expected to survive at least 1 year with good functional status before implanting a CRT-D. Furthermore, the likelihood of sudden cardiac death should be evaluated and outweigh the potential adverse events associated with the device. However, a CRT-P might also provide adequate protection from the increased mortality risk that these patients face, and they might not require the defibrillator component. This important question can only be adequately addressed by a large RCT comparing both devices in sufficient subgroups of eligible patients with heart failure and left ventricular systolic dysfunction.
References
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975.
Authors/Task Force M, Priori SG, Blomstrom-Lundqvist C, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Europace. 2015;17:1601–87.
Dickstein K, Normand C, Auricchio A, et al. CRT survey II: a European Society of Cardiology survey of cardiac resynchronisation therapy in 11 088 patients-who is doing what to whom and how? Eur J Heart Fail. 2018;20(6):1039–51.
Normand CLC, Bogale N, et al. Cardiac resynchronization therapy pacemaker or cardiac resynchronization therapy defibrillator: what determines the choice?—findings from the ESC CRT survey II. Europace. 2019;21(6):918–27.
Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013;34:2281–329.
Ezekowitz JA, O’Meara E, McDonald MA, et al. 2017 Comprehensive update of the Canadian Cardiovascular Society Guidelines for the Management of Heart Failure. Can J Cardiol. 2017;33:1342–433.
NICE. Implantable cardioverter defibrillators and cardiac resynchronisation therapy for arrhythmias and heart failure (review of TA95 and TA120). guidance.nice.org.uk/ta314: NICE, 2014.
Group NCHFGW, Atherton JJ, Sindone A, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: guidelines for the prevention, detection, and management of heart failure in Australia 2018. Heart Lung Circ. 2018;27:1123–208.
Normand C, Linde C, Singh J, Dickstein K. Indications for cardiac resynchronization therapy: a comparison of the major international guidelines. JACC Heart Fail. 2018;6:308–16.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:1810–52.
Tracy CM, Epstein AE, Darbar D, et al. 2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. [corrected]. Circulation. 2012;126:1784–800.
Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2016;68:1476–88.
Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Card Fail. 2017;23:628–51.
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–37.
Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–83.
Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–49.
Ghio S, Freemantle N, Scelsi L, et al. Long-term left ventricular reverse remodelling with cardiac resynchronization therapy: results from the CARE-HF trial. Eur J Heart Fail. 2009;11:480–8.
Cleland JG, Daubert JC, Erdmann E, et al. Longer-term effects of cardiac resynchronization therapy on mortality in heart failure [the CArdiac REsynchronization-Heart Failure (CARE-HF) trial extension phase]. Eur Heart J. 2006;27:1928–32.
Gold MR, Linde C, Abraham WT, Gardiwal A, Daubert JC. The impact of cardiac resynchronization therapy on the incidence of ventricular arrhythmias in mild heart failure. Heart Rhythm. 2011;8:679–84.
Barsheshet A, Wang PJ, Moss AJ, et al. Reverse remodeling and the risk of ventricular tachyarrhythmias in the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy). J Am Coll Cardiol. 2011;57:2416–23.
Daubert JP, Zareba W, Cannom DS, et al. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008;51:1357–65.
Kirkfeldt RE, Johansen JB, Nohr EA, Jorgensen OD, Nielsen JC. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35:1186–94.
Chen Z, Kotecha T, Crichton S, et al. Lower incidence of inappropriate shock therapy in patients with combined cardiac resynchronisation therapy defibrillators (CRT-D) compared with patients with non-CRT defibrillators (ICDs). Int J Clin Pract. 2013;67:733–9.
Schuchert A, Muto C, Maounis T, et al. Lead complications, device infections, and clinical outcomes in the first year after implantation of cardiac resynchronization therapy-defibrillator and cardiac resynchronization therapy-pacemaker. Europace. 2013;15:71–6.
Barra S, Providencia R, Boveda S, et al. Device complications with addition of defibrillation to cardiac resynchronisation therapy for primary prevention. Heart. 2018;104:1529–35.
Stevenson LW, Desai AS. Selecting patients for discussion of the ICD as primary prevention for sudden death in heart failure. J Card Fail. 2006;12:407–12.
Kutyifa V, Geller L, Bogyi P, et al. Effect of cardiac resynchronization therapy with implantable cardioverter defibrillator versus cardiac resynchronization therapy with pacemaker on mortality in heart failure patients: results of a high-volume, single-centre experience. Eur J Heart Fail. 2014;16:1323–30.
Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140–50.
Barra S, Boveda S, Providencia R, et al. Adding defibrillation therapy to cardiac resynchronization on the basis of the myocardial substrate. J Am Coll Cardiol. 2017;69:1669–78.
Leyva F, Zegard A, Umar F, et al. Long-term clinical outcomes of cardiac resynchronization therapy with or without defibrillation: impact of the aetiology of cardiomyopathy. Europace. 2018;20:1804–12.
Kober L, Thune JJ, Nielsen JC, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med. 2016;375:1221–30.
Doring M, Ebert M, Dagres N, et al. Cardiac resynchronization therapy in the ageing population – with or without an implantable defibrillator? Int J Cardiol. 2018;263:48–53.
Marijon E, Leclercq C, Narayanan K, et al. Causes-of-death analysis of patients with cardiac resynchronization therapy: an analysis of the CeRtiTuDe cohort study. Eur Heart J. 2015;36:2767–76.
Drozd M, Gierula J, Lowry JE, et al. Cardiac resynchronization therapy outcomes in patients with chronic heart failure: cardiac resynchronization therapy with pacemaker versus cardiac resynchronization therapy with defibrillator. J Cardiovasc Med. 2017;18:962–7.
Bastian D, Ebrahim IO, Chen JY et al. Real-world geographic variations in the use of cardiac implantable electronic devices-The PANORAMA 2 observational cohort study. Pacing Clin Electrophysiol (PACE). 2018;41(8):978–89.
Lindvall C, Chatterjee NA, Chang Y, et al. National trends in the use of cardiac resynchronization therapy with or without implantable cardioverter-defibrillator. Circulation. 2016;133:273–81.
Barra S, Providencia R, Duehmke R, et al. Cause-of-death analysis in patients with cardiac resynchronization therapy with or without a defibrillator: a systematic review and proportional meta-analysis. Europace. 2018;20:481–91.
Munir MB, Althouse AD, Rijal S, et al. Clinical characteristics and outcomes of older cardiac resynchronization therapy recipients using a pacemaker versus a defibrillator. J Cardiovasc Electrophysiol. 2016;27:730–4.
Barra S, Looi KL, Gajendragadkar PR, Khan FZ, Virdee M, Agarwal S. Applicability of a risk score for prediction of the long-term benefit of the implantable cardioverter defibrillator in patients receiving cardiac resynchronization therapy. Europace. 2016;18:1187–93.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Normand, C., Dickstein, K. (2019). CRT Devices in Heart Failure: Does the Patient Need a Pacemaker or Defibrillator?. In: Steinberg, J., Epstein, A. (eds) Clinical Controversies in Device Therapy for Cardiac Arrhythmias . Springer, Cham. https://doi.org/10.1007/978-3-030-22882-8_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-22882-8_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-22881-1
Online ISBN: 978-3-030-22882-8
eBook Packages: MedicineMedicine (R0)