Abstract
Introduction: In the past two decades, there have been a number of studies that test preventive intervention strategies for young people at imminent and elevated clinical risk for psychosis. We review these studies, integrate their findings, and lay out a framework for future clinical trials.
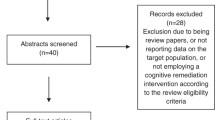
Methods: We used keywords relevant to risk for psychosis and schizophrenia to search in PubMed for randomized clinical trials (RCTs) in clinical or ultra-high-risk (CHR/UHR) cohorts, reviewing references to find earlier studies cited, and PubMed to identify later studies that referenced them. Studies are described with respect to interventions tested and treatment outcomes.
Results: For RCTs in CHR/UHR cohorts, interventions have included pharmacological strategies, such as second-generation antipsychotics (SGA), omega-3 polyunsaturated fatty acids (PUFA), lithium, and modulators of N-methyl-D-aspartate-type (NMDA) receptors; psychological strategies of cognitive behavioral therapy (CBT), family therapy, and cognitive remediation (CR); and combinations of these. Outcome measures include psychosis onset, clinical symptoms, function, and cognition.
Discussion: Overall, among pharmacological strategies, only omega-3 polyunsaturated fatty acids showed efficacy in preventing psychosis onset in initial study, whereas second-generation antipsychotics have led to significant side effects and high dropout. Meta-analysis shows that cognitive behavioral therapy holds promise as a treatment, but it remains unclear to what extent this reflects nonspecific effects of clinician contact. In initial studies, cognitive remediation is effective for improving cognitive deficits such as in processing speed, with concurrent improvement in function. Many promising strategies await study, including exercise and neurostimulation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Schizophrenia
- Psychosis
- Clinical high risk
- Ultra-high risk
- Treatment
- Intervention
- Randomized clinical trials
- Cognitive remediation
- Cognitive behavioral therapy
Introduction
Schizophrenia is a neurodevelopmental disorder characterized by psychosis (e.g., delusions, hallucinations, and disorganized communication), negative symptoms (motivational deficits and decreased emotional experience/expression), cognitive deficits (e.g., processing speed and verbal memory), and impairment in social and academic/vocational function. As schizophrenia is associated with significant morbidity and cost, for both patients and their families [1,2,3], and is as yet refractory to cure, there has been an effort to identify at-risk individuals before the onset of psychosis and provide preventive intervention to improve outcomes [4, 5].
Psychosis onset in schizophrenia is typically preceded by a prodromal stage, characterized first by social withdrawal and nonspecific affective symptoms of anxiety and depression, and then the emergence of psychotic-like symptoms such as unusual thought content, suspiciousness, perceptual disturbances, and subtle disturbance in language [5,6,7]. This prodromal period typically has its onset between the ages of 12 and 35 [8] and can last from months to years [9,10,11,12,13].
Research into the putative schizophrenia prodrome began in the early- to mid-1990s as researchers sought to gain insight into schizophrenia before psychosis onset [9,10,11, 14]. This work inspired the development of criteria to identify individuals during a putative prodromal state, comprising the clinical or ultra-high-risk (CHR/UHR) syndrome for psychosis [15]. The main goals of clinical psychosis risk research have been early identification and intervention to prevent psychosis onset and improve clinical and functional outcome. Over the past two decades, there has been a significant increase in the number of early detection and intervention programs worldwide and several efforts to design and test preventive intervention strategies.
The main operationalized criteria to identify the CHR/UHR syndrome is the presence of clinically significant attenuated or subthreshold psychotic symptoms in the absence of any prior threshold psychosis, which cannot be attributable to medical illness or exposure to drugs of abuse. These criteria were first described in the Comprehensive Assessment of At-Risk Mental States (CAARMS) [16]. There is a second and very similar measure that has been used in North America, the Structured Interview for Prodromal Syndromes (SIPS)/Scale of Prodromal Symptoms (SOPS) [17], adapted from the positive and negative syndrome scale (PANSS) [18]. These two measures have overall agreement in the identification of CHR/UHR [19]. Individuals identified as at CHR/UHR for psychosis typically meet criteria for the Attenuated Positive Symptom Syndrome (APSS), though a few also (or exclusively) meet criteria for Brief Intermittent Psychotic Syndrome (BIPS), and/or Genetic Risk and Decline (GRD), comprised of familial risk or schizotypy in the context of a significant decline in function.
In developing preventive interventions for CHR/UHR individuals, investigators have focused on positive symptoms as a primary outcome measure (e.g., psychosis onset and/or the proxy of worsening positive symptoms over a shorter timeframe). Other outcome measures in studies have included improvement in negative symptoms, cognition, and function.
Approaches for Intervention to Prevent Psychosis
Treatment for the putative prodrome is still a nascent field, with no evidence base for intervention yet established. The first manuscripts describing studies of preventive intervention for CHR/UHR individuals were published in 2002, including an open-label trial of risperidone to assess efficacy and safety [20] and two larger RCTs of cognitive behavioral therapy (CBT), one alone [21,22,23] and the other in combination with risperidone (Table 14.1) [24]. An RCT of olanzapine vs. placebo in CHR/UHR individuals was published in the following year [25], suggesting efficacy in psychosis prevention but at the cost of significant weight gain. The rationale for testing antipsychotics was that their efficacy in treating threshold psychosis might extend to earlier, more attenuated, or subthreshold psychotic symptoms. A similar rationale existed for CBT, with the additional advantage of not having problematic adverse effects such as weight gain and akathisia, but its efficacy has been less clear. The combination of CBT with risperidone showed both efficacy and safety in an RCT in CHR individuals [24], as compared with treatment as usual (TAU), though has not yet been replicated (see Table 14.1). In the ensuing years, other preventive interventions have been tested, including pharmacological strategies, such as omega fatty acids, lithium, and D-serine; psychological approaches, including additional CBT studies, cognitive remediation, and family therapy; and studies that combine both pharmacological and psychological strategies.
Pharmacological Interventions
Antipsychotics
Antipsychotic medications are an established effective treatment for acute psychosis [26]. Antipsychotics are based on the dopamine model of psychosis and inhibit dopamine activity at D2-type dopamine receptors [27,28,29]. Second-generation antipsychotics (SGA) have typically been tested in CHR/UHR cohorts, as serious adverse effects like tardive dyskinesia are far less common than for first-generation antipsychotics (FGA) [30, 31].
One of the first studies examining the efficacy and tolerability of antipsychotics in a CHR/UHR sample was an open-label trial of risperidone [20]. The mean dose of risperidone was 1.04 mg/day (SD = 0.12). The primary outcome, symptom severity, was assessed using the Child Behavior Checklist (CBCL) [32] in a CHR/UHR sample (n = 5; mean age = 15.6; SD = 0.8) and the PANSS in a first episode psychosis (FEP) sample (n = 11; mean age = 23.9; SD = 5.5). In the CHR/UHR sample, follow-up was at 12 weeks, and thought disorder (t = −5.9; p = 0.01) and attention symptoms (t = −40.6; p = 0.0001) decreased significantly from baseline, as did average CBCL scores (t = −3.6; p = 0.04). Although the sample was small, there was no placebo group, and the CBCL was used (as opposed to a more psychosis-specific measure, like the PANSS), this study encouraged the development of RCTs to more rigorously evaluate the promise of antipsychotic medications in CHR/UHR.
Risperidone RCTs conducted since Cannon’s open-label trial have combined the medication with CBT (see the section “Interventions Combining Psychological and Pharmacological Strategies” and Table 14.1) [33, 34]. Other open-label pilot studies have evaluated antipsychotics such as aripiprazole [35] and perospirone [36]. In an 8-week aripiprazole (5–30 mg/day) trial (n = 15), SOPS scores significantly improved from baseline (p < 0.001), but more than half of the participants experienced akathisia (n = 8). No participants transitioned to psychosis. In a preliminary open-label trial of perospirone for 26 weeks (n = 11), the mean changes of total SOPS score from baseline were significant in the CHR/UHR sample (p < 0.05). No adverse effects were noted, and none of the participants developed psychosis.
The largest antipsychotic monotherapy RCT to date aimed to evaluate the efficacy and safety of olanzapine in decreasing positive symptoms severity and potentially preventing psychosis onset (see Table 14.1) [37,38,39,40]. In a double-blind placebo-controlled RCT conducted at the Prevention through Risk Identification Management and Education (PRIME) clinic, 60 CHR/UHR participants were randomized to olanzapine 5–15 mg/day (n = 31) or placebo (n = 31) for 1 year, with psychosocial treatment held constant [37,38,39,40]. Participants who did not develop psychosis were followed for 1 year, whereas those who transitioned stopped the study drug and were able to participate in an open-label trial of olanzapine 5–20 mg/day. The researchers used the presence of psychotic symptoms (POPS) criteria in the SIPS/SOPS to determine the primary outcome of psychosis onset. Secondary efficacy measures included prodromal symptoms, schizophrenia symptoms, and functioning, changes in which were assessed using the SOPS, PANSS, Clinical Global Impression (CGI) Severity of Illness Scale [41], Montgomery-Asberg Depression Rating Scale (MADRS) [42], Young Mania Rating Scale (YMRS) [43], and Global Assessment of Functioning (GAF) scale [44].
The authors found a trend difference in psychosis onset between groups (16.1% for olanzapine and 37.9% for placebo; p = 0.08) in intent-to-treat analysis and a nonsignificant decrease in positive symptoms at follow-up as compared to baseline (SOPS positive symptom score change from baseline = 0.31) in the olanzapine group. Low acceptability of the study medication was reflected in high dropout rates (45%) and dramatic weight gain in the olanzapine treatment arm (8.8 (SD 9.1) kg vs. 0.3 (SD 4.2) kg).
Omega-3 Polyunsaturated Fatty Acids
Another strategy was to test neuroprotective agents for preventive intervention in a CHR/UHR cohort. Omega-3 polyunsaturated fatty acid (PUFA) acts as an anti-inflammatory agent and antioxidant and is thought to counteract the proinflammatory reactions and oxidative stress associated with symptoms of schizophrenia [45]. RCTs of PUFA in schizophrenia have had mixed results, though some studies suggest it may be effective earlier in the course of the disorder. Therefore, an RCT of omega-3 fatty acids was completed in a cohort of CHR/UHR individuals (see Table 14.1) [46]. In this 12-month double-blinded RCT of 81 CHR/UHR individuals, administration of four capsules of omega-3 PUFA supplements (1.2-g/d) was given daily for 12 weeks, as compared to placebo, and was associated with a lower rate of transition to psychosis at 12 months (4.9% vs. 27.5%; p = 0.007), as well as improvement in positive symptoms (p = 0.01), negative symptoms (p = 0.02), and general symptoms (p = 0.01), and improved functioning (p = 0.002), assessed at 1, 2, 3, 6, and then 12 months, as compared to placebo. The primary outcome was measured using the severity thresholds on the PANSS, and the secondary outcomes were measured by the PANSS, MADRS, and GAF. Dropout was low at 6%. Of note, the difference in psychosis onset between the two treatment arms persisted for up to 7 years, suggesting lasting neuroprotective effects of PUFA [47]. However, despite this early promise, the results of this study have yet to be replicated.
A subsequent study of PUFA vs. placebo in the context of comprehensive care, including evidence-based psychosocial treatment, was inconclusive in that low conversion rates (11.2% for control vs. 11.5% for PUFA) were found for the two groups [48]. In this multicenter RCT, 304 patients were given a daily dose of 1.4 g of omega-3 PUFA or placebo, along with cognitive behavioral case management (CBCM) for 6 months. The outcomes were measured using the Brief Psychiatric Rating Scale (BPRS; [49]), Scale for the Assessment of Negative Symptoms (SANS), MADRS, YMRS, Social and Occupational Functioning Assessment Scale (SOFAS ; [50]), and the Global Functioning Scale (GFS) [51]. While only a handful of studies that directly examine the efficacy of omega-3 PUFA in delaying onset of psychosis exist as of now, further study is indicated (see Table 14.1).
Modulators of NMDA Receptors
Amphetamines can elicit psychotic-like symptoms [52, 53]. But phencyclidine (PCP) and ketamine, N-methyl-D-aspartate-type (NMDA) receptor antagonists, have been found to elicit both psychotic-like and negative symptoms, as well as cognitive deficits, similar to those seen in schizophrenia [54]. Given the wide range of symptoms (positive, negative, and cognitive) associated with schizophrenia, medications that target the glutamatergic pathway via NMDA receptors provide an alternative for treating negative symptoms and neurocognitive deficits that are resistant to dopamine-receptor antagonist antipsychotics [55, 56].
As of now, there is no clear evidence base for treatment of negative symptoms or cognitive deficits in schizophrenia. Recent findings from clinical trials using compounds targeting NMDA receptor sites, such as glycine, D-serine, D-cycloserine, and high-affinity glycine transport inhibitors, show promise in alleviating not only positive symptoms but more notably in negative symptoms, especially early in the course of psychotic illness, without significant side effects [55,56,57,58,59,60,61].
The first clinical study on the efficacy of glycine in CHR/UHR patients was a two-part study, first using an 8-week open-label design and subsequently followed by a 12-week double-blind, placebo-controlled pilot study [62]. Subjects were outpatients ages 14–35; the Criteria of Prodromal Syndromes (COPS) and a minimum Scale of Prodromal Symptoms (SOPS) score of 20 were used to determine eligibility. Glycine dosage started at 0.2 g/kg once daily, ending at 0.4 g/kg twice daily, for both pilot studies. There were large and significant effect sizes in the open-label phase for changes in SOPS scores (total –1.39, positive –1.10, negative –0.74, disorganized –1.05, general –1.12). Effect sizes in the second phase were less pronounced and were not significant for the glycine group (total –0.71, positive –0.82, negative –0.60, disorganized –0.15, general –0.74). No specific concerns for treatment-emergent adverse events were found using the Systematic Assessment For Treatment Emergent Events (SAFTEE), and there were no significant endpoint changes in vital signs and weight. While the strength of these findings is bolstered by having a representative cohort group of risk syndrome patients (who were adolescents with poor function, 70–75% male, and with a baseline SOPS total score in the high 30s), both studies had very small sample sizes (pilot 1: n = 10, pilot 2: n = 4 each for glycine and placebo groups) that led to a lack of statistical power (see Table 14.1).
The first study to assess the efficacy of D-serine in CHR/UHR individuals showed markedly improved negative symptoms [63]. Forty-four participants (with assessable data from 15 D-serine and 20 placebo treatment assignments) participated in a double-blind, placebo-controlled, multicenter, parallel-group RCT. Inclusion criteria were similar to the previous Woods et al. study [62], with a minimum severity score of 20 for the total SOPS score and age range of 13–35. D-serine dosage was set at 60 mg/kg per day, divided into two 30 mg/kg oral doses, which was taken daily for 16 weeks. Assessments took place weekly for the first 6 weeks and then biweekly thereafter. The primary outcome was the SOPS score for negative symptoms, for which D-serine led to a 35.7% reduction, which was significant versus placebo (F 1231 = 4.4, p = 0.03 d = 0.68). Secondary measures such as MATRICS consensus cognitive battery (MCCB) scores did not show significant differences from placebo. The reduction of negative symptoms in this D-serine trial is promising, but requires further replication (see Table 14.1).
Other Pharmacological Interventions
Antidepressants, mood stabilizers, and nonsteroidal anti-inflammatory drugs have also been explored as alternative pharmacological intervention strategies for CHR/UHR, primarily in three pilot studies.
In a naturalistic (non-randomized) study, participants ascertained as CHR/UHR using the SOPS were prescribed one of two types of medications, antidepressants (n = 20) or SGAs (n = 28) [64]. Onset of psychosis was the primary outcome measure: there were 12 cases of psychosis onset in the total sample of 48 (25%), all of whom had been prescribed SGAs. However, 11 of these 12 were nonadherent to the prescribed SGA medication, which suggests the prescription of SGAs was a marker of symptom severity. The high noncompliance rate shows that SGAs are not an acceptable treatment for CHR youths themselves. The study is inconclusive as to the efficacy of antidepressants as there was no randomization to a comparison treatment, such that an RCT of antidepressants in CHR/UHR individuals remains warranted.
Lithium has known neuroprotective properties [65, 66] and so has also been studied as a potential treatment in CHR/UHR patients, in a longitudinal MRI/MRS pilot study of low-dose lithium (n = 21) [67]. Eleven CHR/UHR participants in the experimental group received low-dose lithium, and 10 CHR/UHR participants in the comparison group received treatment as usual (TAU). Primary outcome measures were proton magnetic resonance spectroscopy (1H-MRS) and hippocampal T2 relaxation time (HT2RT) measures. Changes in metabolite concentrations were not significant, but HT2RT was significantly less in the experimental condition compared to control group (p = 0.018), suggesting that low-dose lithium may protect the hippocampus in CHR/UHR.
Inflammation and oxidative stress are potentially important in the development of prodromal and psychotic symptoms [68, 69], and trials with anti-inflammatory drugs are therefore indicated. According to clinicaltrials.gov, there has been an RCT of aspirin 1000 mg/day vs. placebo, with a plan to test inflammation markers and genetic samples. However, results of this RCT have not yet been published.
Psychological Approaches
Cognitive Behavioral Therapy (CBT)
CBT for psychosis emerged consequent to observed partial effectiveness of antipsychotics, challenges for patients in adhering to antipsychotic medication regimens, symptom relapse despite medication adherence, and the limited scope of symptoms that antipsychotics target [70]. In contrast, CBT for psychosis offers a side effect-free, structured, flexible, and time-limited intervention [71]. The cognitive model of psychosis centers around the impairing impact of negative appraisal of psychotic symptoms [72]. For instance, negative appraisals of symptoms and oneself are linked with depressed mood [73] and persistence of delusions in schizophrenia populations. Since its inception, CBT for psychosis has been extended to CHR/UHR and is a growing field of study. To date, there are four CBT monotherapy RCTs in CHR/UHR, which have assessed efficacy of CBT for psychosis in reducing psychosis onset and decreasing positive symptoms.
The earliest CHR/UHR psychological intervention study was a single-blind RCT of CBT vs. mental state monitoring with individuals at high risk for psychosis from the early detection and intervention evaluation (EDIE) program [22]. The primary aim of the intervention was to determine if CBT could significantly reduce the rate of transition to psychosis as compared with TAU in help-seeking CHR/UHR individuals. Transition to psychosis was operationalized in three ways: PANSS-defined psychosis scores, meeting DSM-IV criteria for a psychotic disorder, and/or the prescription of antipsychotic medication. Sixty high-risk participants were randomly assigned to the TAU control group (monitoring only; n = 23) or the experimental group (up to 26 CBT sessions plus monitoring; n = 37) for 6 months. Randomization was stratified by gender and family history of psychosis. In this 3-year study, there were monthly follow-ups in the first year and then follow-ups every 6 months for the next 2 years, with PANSS used to measure symptoms. Low attrition rates (14%) suggest that both conditions were tolerable (see Table 14.1).
At 1-year follow-up, the researchers reported a significant main effect of CBT for PANSS-defined transition (p = 0.03) and antipsychotic prescription (p = 0.01). At 3-year follow-up, the main effect of CBT was not significant (p = 0.24). Taken together, the results of this study were inconclusive. Certain elements of the monitoring component in both conditions incorporated case management, rendering it difficult to identify CBT-specific aspects of intervention as the main ingredient of psychosis prevention. Furthermore, the authors’ conclusion that the 6-month CBT treatment was effective in reducing transition to psychosis over a 12-month period is based on a post-hoc exclusion of two participants because they were discovered to meet criteria for psychosis after randomization into the experimental group. In addition, the small sample size and broad operationalization of conversion to psychosis make interpretation of the results less clear. Depending on the criteria used to determine transition to psychosis, transition rates ranged from 14% to 20% in the experimental group and 22% to 35% in the control group. Although this study had limitations, it did offer the promise of using nonpharmacological interventions to treat attenuated psychosis symptoms and prevent psychosis onset, spurring a movement in CBT RCT research.
The second study was a single-blind 6-month trial of CBT vs. supportive therapy that entailed monitoring at 6, 12, and 18 months [74]. Ascertainment methods differed from the previous CBT study, as the SIPS/SOPS was also used to measure the severity of attenuated positive symptoms over time. Randomization was stratified by gender and prodromal symptom severity, and participants were assigned to either a 20-session CBT treatment (n = 27) or supportive therapy treatment (n = 24). Supportive therapy did not include CBT techniques and was considered treatment as usual (TAU). The SIPS/SOPS was also used to determine conversion to psychosis.
The sample size was modest (n = 51), and there was a high dropout rate (25%; see Table 14.1). Additionally, only 5% of the sample developed psychosis. Further, only 60% of the participants completed the 18-month follow-up. SOPS positive symptoms significantly decreased over time in both groups (p < 0.001), without any significant difference in improvement between them. Raters were blind and treatment fidelity was high (91% of the treatment tapes were rated correctly). This RCT suggests that there are nonspecific factors in psychotherapy that may offer benefit to patients. Alternatively, in the absence of a comparison “follow-along” group, it is unclear if the low conversion rate was due to ascertainment of participants for this RCT or nonspecific effects of clinician contact. Overall, it is difficult to draw conclusions about the efficacy of CBT from this study.
A third single-blind multisite RCT evaluated 26-session CBT plus mental state monitoring vs. mental state monitoring only [75]. Both conditions were in addition to TAU, which was routine clinical care that varied by treatment site; therefore, randomization was stratified by site. CAARMS scores were a primary outcome measure and were ascertained at baseline and then at 6, 12, 18, and 24 months. Rater blinding was moderately successful (22.2% of the participants had treatments that featured blind breaks). Although this RCT was the first CBT study with a large sample (n = 288), there were no significant differences in conversion to psychosis between the experimental (n = 144) and comparison (n = 144) groups. However, there was a within-group effect in that frequency and intensity of psychotic experiences were significantly reduced in the experimental group (p = 0.02; see Table 14.1).
A fourth RCT, the Dutch Early Detection and Intervention Evaluation (EDIE-NL), implemented a single-blind multisite intervention comparing 26-session CBT plus TAU (n = 97) vs. TAU (n = 104) with 18-month follow-up [76]. Randomization was stratified by site and assessors were blinded. The primary outcome for the CHR participants (n = 201) was transition to psychosis, as measured by the CAARMS at baseline, and then at 2, 4, 6, 12, 15, and 18 months. Treatment fidelity is challenging to gauge, as therapy sessions were not recorded, but the authors did report therapists’ competency ratings on the Revised Cognitive Therapy Scale. This study is the most promising in terms of efficacy in preventing psychosis onset: significantly fewer (χ2 (1) = 5.575, P = 0.03) CHR/UHR participants in the experimental group (n = 10) transitioned to psychosis than in the comparison group (n = 22) (see Table 14.1) [76].
The CHR/UHR CBT studies to date have had particularly low conversion rates, suggesting potential methodological concerns (e.g., ascertainment of healthier individuals at lower risk), or perhaps the influence of a nonspecific efficacious element in psychological treatment. Future RCT studies could parse out this question by including a follow-along group.
Family-Focused Therapy
Most treatments for CHR/UHR focus on the individual. However, family dynamics also play a role in the prodrome and FEP [77, 78]. Families play a role in help-seeking and treatment, as well as in social and role functioning. Family-focused therapy adapted for CHR/UHR (FFT-CHR) is a psychosocial intervention that aims to address the individual in the context of his or her family. Thus far, there has been one RCT of family therapy in CHR/UHR. This 6-month multisite RCT (n = 129) used the SIPS/SOPS to ascertain CHR/UHR status and compared 18 sessions of FFT-CHR to 3 sessions of general family psychoeducation [79, 80]. Both treatment assignments were in addition to TAU, which included concurrent antipsychotic, antidepressant, psychostimulant, anxiolytic, and mood stabilizer medication use. FFT-CHR involved 1-hour family sessions that focused on psychoeducation, communication enhancement training, and problem-solving. The intervention mirrored CBT in the assignment of homework between therapy sessions. Independent evaluators were blinded.
The primary outcome measures in this FFT-CHR RCT were SOPS positive and negative symptoms. Attenuated positive symptoms improved more in the experimental than in the control group (F[1,97]=5.49, P = 0.02). Negative symptoms improved for both groups, but improvement was not significantly related to treatment group assignment. Transition to psychosis using SIPS/SOPS criteria and psychosocial functioning was also an outcome measure. Twenty-seven participants dropped out (20.9% attrition). Six of 102 (5.9%) participants who completed baseline and 6-month follow-up developed psychosis. Psychosocial functioning was measured using GAF and GFS Role and GFS Social. Global and role functioning changes were found to be age dependent. Participants between the ages of 16 and 19 in the experimental group showed relatively more improvement than in the comparison group, whereas participants over 19 years of age improved more in the comparison group. Improvement in social function was independent of treatment assignment (see Table 14.1).
Overall, relatively high attrition rates suggest that the intervention may require modification before it is implemented more widely. Furthermore, it would be useful to compare family intervention to individual therapy with respect to efficacy. As with the CBT studies, low transition rates suggest the need for a follow-along group to rule out nonspecific benefits of a therapeutic setting or ascertainment effects. The authors also argued that the short duration of the study may have had an impact on rates of psychosis onset. Overall, this study is promising and FFT-CHR warrants further study.
Cognitive Remediation
Cognitive deficits exist in clinical high-risk patients, typically around a half standard deviation below the norm [81]. These deficits have been associated with both functional impairment and also risk for psychosis. Slowing of processing speed is a predictor of psychosis outcome [82], as is verbal memory impairment [81, 83]. Hence, there has been an effort to test cognitive remediation (CR) in these domains in CHR/UHR patients to improve function and prevent psychosis onset. Early open-label trials suggested that CR might improve the prognosis of CHR/UHR individuals by addressing some of the cognitive deficits present in both people with schizophrenia and those at CHR. One such study found that CR may have greater efficacy in CHR/UHR in improving long-term memory and function, as compared to individuals with schizophrenia. Training CR regimens like Lumosity and Socialville may enhance processing speed and role functioning in CHR/UHR individuals [84]. In open-label studies, Posit Science Brain Fitness Training, a training program focused on remediating auditory processing deficits, has also shown some promise in improving processing in CHR/UHR individuals [85].
Thus far, there has been one study of CR as part of a combined intervention and three RCTs of CR alone in CHR/UHR patients. In the combined intervention, CR was part of a combined treatment intervention that included CBT, skills training, CR, and psychoeducational multifamily groups [86]. The first CR RCT used computer-assisted cognitive remediation (CACR), developed by Captain’s Log® software, which was previously shown to have efficacy in schizophrenia [87]. A second RCT used auditory-based processing tasks as part of a neuroadaptive cognitive training program to improve verbal memory in CHR/UHR individuals [88]. The most recent, and possibly the most promising, trial used neurofeedback during a processing speed task (PST) program to remediate processing speed deficits in CHR/UHR individuals with the aim of improving their long-term social functioning [89]. Each of these is reviewed in more detail in the following paragraphs (see the section “Integrated Psychological Treatments” for more detail about the combined intervention).
In the first CR RCT study, 32 adolescents were randomly assigned to either train with computer-assisted cognitive remediation (CACR) or to play a nontargeted computer game. Only 12 of the participants were considered to be at CHR; the rest had a psychotic disorder. After 8 weeks of training, participants in the CACR group showed significant improvements specifically in visuospatial abilities, but not in other domains [87]. However, it was not clear if this improved performance could be accounted for by increased psychological support, practice effects, activities at the day clinic, or other nonspecific factors, all of which can be clarified in future research. Of note, there were low rates of attrition (12.5%) in the study and high ratings of acceptability (mean of 4.3/5 on motivation rating survey) for the CACR, which makes this training regimen a potentially promising one (see Table 14.1).
In a double-blind RCT targeting verbal and working memory deficits in (n = 83) CHR/UHR individuals, auditory-based processing tasks were used in a CR treatment intervention [88]. This study used neuroadaptive cognitive training with neuroplasticity-based software created by Posit Science Corporation, which aimed to improve accuracy of perception of and response to verbal targets [88]. Outcomes included changes in neurocognitive functioning, measured using the MATRICS, and changes in symptoms as assessed in clinical interviews. All healthy volunteers received the neuroadaptive cognitive training, while CHR/UHR subjects were randomly assigned to neuroadaptive cognitive training, or to a commercially available computer game. Individuals assigned to the neuroadaptive cognitive training significantly improved their verbal memory, as compared to those assigned to the commercially available computer games. However, attrition rates were high (42%), which may have been due to the amount of work involved, which included training at home for an hour each day, 5 days a week, for 8 weeks, a training that was repetitive and entailed tone discrimination [90]. While this study was promising with respect to remediating verbal learning and memory deficits in CHR/UHR, the high attrition rate highlights the importance of creating engaging tasks to make them more acceptable for memory deficits in individuals at CHR/UHR (see Table 14.1).
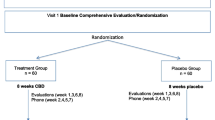
Processing speed deficits are associated with social impairment in CHR/UHR individuals [91]. In an RCT, a novel CR program called processing speed task (PST) was compared to nonspecific computer games, with respect to its efficacy in improving processing speed and concurrent social impairment in CHR/UHR individuals (n = 62) [89]. The intervention was administered for 2 months, and evaluations of cognition were done before the intervention, immediately after the intervention, and 2 months after the completion of the intervention. Of note, PST uses pupillometry as a form of biofeedback that allows the task to personalize the training module for each participant, making it more engaging. The program tracks pupil dilation to appropriately adjust the difficulty level of the practice session. Because pupil dilation increases with activation of the sympathetic nervous system, the task is programmed to decrease difficulty level when dilation surpasses a given threshold (indicating that the person is becoming less engaged in the task) and decreasing the difficulty if the pupils are constricted beyond threshold [92]. This led to fewer errors throughout the intervention, which enhances self-efficacy in participants, according to proponents of errorless learning [93]. As hypothesized, a robust relationship between processing speed (as defined by WAIS-III) and social functioning (as defined by SAS-SR) was found in CHR/UHR individuals, and both improved in tandem with treatment, with enhanced social functioning evident even 2 months beyond end of treatment. The treatment was acceptable to participants, with only 10% dropout, likely because PST was specifically designed to simulate a computer game, with fantasy contexts that increase intrinsic motivation [94]. Given its acceptability and efficacy for both cognition and function, this is particularly a promising treatment that warrants more study (see Table 14.1).
Future studies of CR in CHR/UHR cohorts can explore whether other forms of neurofeedback can be incorporated into CR and if CR would be an important component of a treatment package.
Integrated Psychological Treatments
Prior to the use of CR as an isolated intervention in an RCT, CR was used as part of an integrative psychological intervention (IPI) that included individual CBT, modified social skills training, and multifamily psychoeducation (see Table 14.1) [86]. The CR involved computerized tasks that were based on cognitive tasks used in COGPACK software (Marker Software, 1992) to address thought and perception deficits. During each session, patients repeatedly practiced exercises targeting attention, memory, and executive functioning. Task progression to more difficult levels was based on performance errors [86]. Compared to the participants (n = 65) who received only supportive counseling, participants who also received the IPI (n = 63) had lower rates of psychosis transition, an effect that remained throughout the 2 years of the study. By the end of the treatment phase, 2 of 63 patients in the IPI group and 11 of 65 patients in the supportive counseling group had transitioned to psychosis, with an additional 2 transitions in each of the treatment groups during the posttreatment period [86]. The role of the individual components of the IPI is not clear and bears further study to identify active ingredients.
Interventions Combining Psychological and Pharmacological Strategies
Across the board, in studies combining psychological and pharmacological strategies, the effects of medication versus nonpharmacological intervention are confounded. However, aggregate treatment is promising for preventing psychosis onset, as well as reducing symptoms and improving function.
A landmark single-blind 12-month RCT combining psychological and pharmacological strategies compared 6 months of specific preventive intervention (SPI; n = 31), with needs-based intervention (NBI; n = 28) [24]. NBI involved supportive psychotherapy, case management, and psychoeducation, with potential concurrent antidepressant or benzodiazepine use. SPI was comprised of NBI in addition to low-dose risperidone (mean dose = 1.3 mg/day) and CBT. Follow-up occurred at 6 months and 12 months. Attenuated positive symptoms were the primary outcome, as measured by the Brief Psychiatric Rating Scale (BPRS). Functioning and mood symptoms were secondary outcomes, assessed by the GAF and Hamilton Rating Scales for Depression and Anxiety (HRSD). Treatment adherence for risperidone was an issue, with 14 participants in the SPI group (45%) adhering to the medication regimen.
Another early integrated treatment RCT examined transition to psychosis in individuals diagnosed with schizotypal disorder (n = 79) [95]. The intervention lasted for 2 years. The integrated treatment included a multidisciplinary treatment team conducting a modified assertive community treatment model, social skills training, and patient and family psychoeducation. The standard treatment consisted of treatment at a community mental health center with a physician, nurse, and, in some cases, also a social worker. Antipsychotic medication treatment differed between participants as it remained the decision of the psychiatrist responsible for treatment. Transitions to psychotic disorder was the primary outcome as measured by the SCAN 2.0, the Scale for the Assessment of Positive Symptoms (SAPS), and Scale for Assessment of Negative Symptoms (SANS). Secondary outcome measures were psychotic, negative, and disorganized symptoms based on SAPS and SANS interviews.
Thirty-six integrated-treatment patients and 29 standard-treatment patients participated in the 2-year follow-up conducted by independent assessors who were psychiatrists, psychologists, or psychiatry residents. Of this group, nine participants (25.0%) randomized to integrated treatment and 14 participants (48.3%) randomized to standard treatment converted to psychosis. A multivariate analysis found that male sex was a significant risk factor for transition (relative risk = 4.47 (CI = 1.3–15.33), but integrated treatment reduced the risk (relative risk = 0.36 (CI = 0.16–0.85). Previous work has suggested that cannabis use can be a risk factor for developing psychosis [96], but a univariate analysis in this study indicated that the use of cannabis at least monthly at baseline did not predict transition to psychosis (relative risk = 1.80 (CI 0.66–4.88), P = 0.2).
An open-label, randomized parallel-group study with a 2-year observation period put putatively prodromal participants (n = 124) in one of two conditions; both conditions involved needs-focused interventions which included psychoeducation, crisis intervention, family counseling, and assistance with education or work-related difficulties according to individual need [97]. In the experimental condition (n = 65), participants were also given a second-generation antipsychotic, amisulpride, ranging in dosage from 50 to 800 mg (daily mean = 118.7 mg) and increased if attenuated or brief limited intermittent positive symptoms were present (mean dose at endpoint = 169.5 mg). At baseline and at 12-week follow-up, participants were given a basic and positive psychotic spectrum symptoms score (ERI–BAPPSS) split into two subscores: one for the assessment of threshold psychotic symptoms and attenuated positive symptoms (ERI-PPS) and one for basic symptoms (ERI-BS). Participants were also assessed with the positive, negative, and general psychopathology subscales of the PANSS, as well as the MADRS, GAF, Extrapyramidal Symptom Rating Scale (ESRS), and UKU Side Effect Rating Scale (UKU).
At the 12-week follow-up, the 58 combined protocol participants and 44 control participants who remained were analyzed. The combined treatment produced a significantly superior effect on ERI–BAPPSS scores (F (1,98) = 7.49, P < 0.01), with significant improvement observed in both groups (amisulpride, t = 6.88, d.f. = 57, P < 0.001; controls t = 2.87, d.f. = 43, P < 0.01), ERI–PPS scores (F (1,98) = 7.42, P < 0.001; amisulpride, t = 7.35, d.f. = 57, P < 0.001; controls t = 2.57, d.f. = 43, P < 0.05), and ERI–BS scores (F (1,98) = 6.30, P < 0.05; amisulpride, t = 6.88, d.f. = 57, P < 0.001; controls, t = 2.87, d.f. = 43, P < 0.01). A significant effect of treatment with amisulpride also emerged regarding the PANSS positive subscale (PANSS–P) score (F (1,98) = 7.83, P < 0.01); paired t-tests revealed a significant decrease of baseline scores only in the group with amisulpride (t = 5.50, d.f. = 57, P < 0.001). Analysis of PANSS negative subscale (PANSS–N) scores by ANCOVA also yielded a significantly better effect of amisulpride (F (1,98) = 4.85, P < 0.05). Within-group comparisons revealed a significant effect only for amisulpride (t = 4.56, d.f. = 57, P < 0.001). A superior effect for amisulpride was also observed for GAF scores (F (1,98) = 5.70, P < 0.05), and paired t-tests showed a significant change in the amisulpride group only (t = 4.56, d.f. = 56, P < 0.001). No significant difference between groups emerged regarding MADRS scores. General psychopathology improved significantly in the amisulpride group (F (1,98) = 4.63, P < 0.05; amisulpride: t = 5.02, d.f. = 57, P < 0.001; controls, t = 2.11, d.f. = 43, P < 0.05). The strongest effects were observed for attenuated and brief limited intermittent positive symptoms. Remission occurred more than twice as often in the amisulpride group.
An RCT randomized CHR/UHR participants into three groups: one received CBT, consisting of stress management, strategies for dealing with depression/negative symptoms, positive symptoms, and other comorbid conditions, in conjunction with risperidone (2 mg if tolerated); another group received CBT with a placebo medication; and the third received supportive therapy, providing them with emotional support and problem-solving skills and a placebo medication [98]. There was also a follow-along group not randomized for treatment but simply monitored. The primary outcome measure was transition to psychosis (criteria defined a priori), assessed using the CAARMS. Secondary outcome measures were psychiatric symptoms, psychosocial functioning, and quality of life which were assessed respectively using the CAARMS, Brief Psychiatric Rating Scale (BPRS), SANS, Hamilton Depression Rating Scale (HDRS), GAF, and Quality of Life Scale (QLS).
At 6-month follow-up, 2 of the 43 subjects (4.7%) in the CBT and risperidone group, 4 of the 44 subjects (9.1%) in the CBT and placebo group, and 2 of 28 subjects (7.1%) in the supportive therapy and placebo group had transitioned to a psychotic disorder. These were not significant differences (log-rank test, p = 0.92). In the monitoring group, 4 of 78 (5.1%) developed psychosis, also not significantly different from the randomized groups (log-rank test, p = 0.93). All three randomized groups and the monitoring group showed significant improvement in BPRS total, BPRS psychotic subscale, and HDRS scores. All groups except the combined CBT and risperidone significantly increased in functioning. The supportive therapy and placebo group and the monitoring group showed significant improvement in total negative symptoms. Only the monitoring group showed significant increases in QLS scores. Poor adherence was prevalent in this study: 23 participants in the CBT and risperidone group (53.5%) had poor adherence (less than 50% of doses taken), 18 (41.9%) had partial adherence (50–89% of doses taken), and only 2 (4.7%) had full adherence to risperidone (≥ 90% of doses taken). Of the two subjects in the CBT and risperidone group who were known to have developed psychosis by the 6-month assessment, both belonged to the <50% adherence group. However, this was not statistically significant (log-rank test, P = 0.57). There were no significant differences in symptoms or level of functioning between the groups, although there was a trend for those who were poorly adherent to show greater improvement in functioning and quality of life (GAF, P = 0.095; QLS, P = 0.089).
At a 12-month follow-up [98], seven participants in the CBT and risperidone group, seven in the CBT and placebo group, six in the supportive therapy and placebo group, and five in the monitoring group had transitioned to psychosis. The estimated 12-month transition rates were 10.7 ± 5.0% for the CBT and risperidone group, 9.6 ± 4.6% for the CBT and placebo group, 21.8 ± 8.8% for the supportive therapy and placebo group, and 8.7 ± 3.8% for the monitoring group. There were no significant differences in the rate of transition between the randomized groups (log-rank test P = 0.60) or the four groups (log-rank test P = 0.59). Poor adherence to medication was also high at the 12-month follow-up. In the CBT and risperidone group, 27 subjects (62.8%) showed poor adherence, 16 (37.2%) showed partial adherence, and none showed full adherence to risperidone. All groups showed improvement on the secondary outcome measures, and there was no significant difference between the groups.
In an RCT study, adolescents and young adults (initially ages 14–30) who had previously participated in a combined treatment study were reevaluated [99]. CHR/UHR participants either received up to 2 mg risperidone as well as cognitively oriented psychotherapy (specific intervention: SPI, n = 31) or supportive psychotherapy only (needs-based intervention: NBI, n = 28). During the study, neither participants nor clinicians were blind to treatment, but research interviewers were. Thirteen SPI participants were partially or nonadherent to their medication, and 11 were fully adherent. At a medium-term follow-up, 17 from the original NBI group and 24 from the SPI group consented to be interviewed again and were assessed using symptomatology and functioning measures such as the Brief Psychiatric Rating Scale (BPRS), SANS, Quality of Life Scale (QLS), the Hamilton Rating Scales for Anxiety (HRSA) and Depression (HRSD), and the Mania Rating Scale (MRS). There was no significant difference in follow-up ratings between the two groups (×2(1) = 1.94, p = 0.164). There was also no significant difference in probability of developing psychosis between the SPI and NBI groups. However, both the SPI and NBI groups had significantly higher Mania Scale (t(22) = 3.06, p = 0.006 and t(16) = 2.41, p = 0.029, respectively) and QLS (t(23) = 2.716, p = 0.012 and t(17) = 3.86, p = 0.001, respectively) scores at the 3–4-term follow-up compared to baseline.
Future Directions
Overall, there is no clear evidence base for treatment of CHR/UHR individuals. With respect to pharmacological strategies, the use of second-generation antipsychotics is greatly limited by adverse effects that interfere with adherence. Glutamatergic strategies appear to have efficacy specifically for negative symptoms and cognitive deficits. Among psychological treatments, cognitive behavioral therapy holds promise, but such studies have been limited by low conversion rates to psychosis, such that there may be a nonspecific effect of clinical contact that is the operative ingredient. Cognitive remediation is particularly promising, as it has shown efficacy in improving cognition, with concomitant improvement in functioning. There are now clinical trials underway for exercise, which may be effective. Further, neurostimulation has not yet been tried, but a circuit-based approach to treatment, alone or in conjunction with cognitive remediation, may hold particular promise.
References
Insel TR. Rethinking schizophrenia. Nature. 2010;468:187–93.
Tandon R, Nasrallah HA, Keshavan MS. Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr Res. 2009;110(1–3):1–23.
Moscarelli M. Health and economic evaluation in schizophrenia: implications for health policies. Acta Psychiatr Scand. 1994;89:84–8.
Shrivastava A, Johnston ME, Thakar M, Shrivastava S, Sarkhel G, Sunita I, et al. Origin and impact of stigma and discrimination in schizophrenia-patients’ perception: Mumbai study. Stigma Res Action. 2011;1:67–72.
Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22(2):353–70.
Corcoran C, Gerson R, Sills-Shahar R, Nickou C, McGlashan T, Malaspina D, et al. Trajectory to a first episode of psychosis: a qualitative research study with families. Early Interv Psychiatry. 2007;1(4):308–15.
Yung AR, Nelson B, Stanford C, Simmons MB, Cosgrave EM, Killackey E, et al. Validation of “prodromal” criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophr Res. 2008;105(1–3):10–7.
Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69(3):220–9.
Beiser M, Erickson D, Fleming JA, Iacono WG. Establishing the onset of psychotic illness. Am J Psychiatry. 1993;150(9):1349–54.
Hafner H, Maurer K, Löffler W, Riecher-Rössler A. The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry. 1993;162:80–6.
Loebel AD, Lieberman JA, Alvir JM, Mayerhoff DI, Geisler SH, Szymanski SR. Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry. 1992;149(9):1183–8.
Woods SW, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Validity of the prodromal risk syndrome for first psychosis: findings from the North American Prodrome Longitudinal Study. Schizophr Bull. 2009;35(5):894–908.
Mason O, Startup M, Halpin S, Schall U, Conrad A, Carr V. Risk factors for transition to first episode psychosis among individuals with “at-risk mental states”. Schizophr Res. 2004;71(2–3):227–37.
Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22(2):353–70.
Yung AR, McGorry PD, McFarlane CA, Patton GC. The Pace Clinic: development of clinical service for young people at high risk of psychosis. Australas Psychiatry. 1995;3(5):345–9.
Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell’Olio M, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39(11–12):964–71.
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29(4):703–15.
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76.
Fusar-Poli P, Cappucciati M, Rutigliano G, Lee TY, Beverly Q, Bonoldi I, et al. Towards a standard psychometric diagnostic interview for subjects at ultra high risk of psychosis: CAARMS versus SIPS. Psychiatry J. 2016;2016:7146341.
Cannon TD, Huttunen MO, Dahlström M, Larmo I, Räsänen P, Juriloo A. Antipsychotic drug treatment in the prodromal phase of schizophrenia. Am J Psychiatry. 2002;159(7):1230–2.
Morrison AP, Bentall RP, French P, Walford L, Kilcommons A, Knight A, et al. Randomised controlled trial of early detection and cognitive therapy for preventing transition to psychosis in high-risk individuals: study design and interim analysis of transition rate and psychological risk factors. Br J Psychiatry. 2002;43:s78–84.
Morrison AP, French P, Walford L, Lewis SW, Kilcommons A, Green J, et al. Cognitive therapy for the prevention of psychosis in people at ultra-high risk: randomised controlled trial. Br J Psychiatry. 2004;185:291–7.
Morrison AP, French P, Parker S, Roberts M, Stevens H, Bentall RP, et al. Three-year follow-up of a randomized controlled trial of cognitive therapy for the prevention of psychosis in people at ultrahigh risk. Schizophr Bull. 2007;33(3):682–7.
McGorry PD, Yung AR, Phillips LJ, Yuen HP, Francey S, Cosgrave EM, et al. Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Arch Gen Psychiatry. 2002;59(10):921–8.
McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller TJ, Woods SW, et al. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis: I. Study rationale and design. Schizophr Res. 2003;61(1):7–18.
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–62.
Kaalund SS, Newburn EN, Ye T, Tao R, Li C, Deep-Soboslay A, et al. Contrasting changes in DRD1 and DRD2 splice variant expression in schizophrenia and affective disorders, and associations with SNPs in postmortem brain. Mol Psychiatry. 2014;19(12):1258–66.
Howes OD, Williams M, Ibrahim K, Leung G, Egerton A, McGuire PK, et al. Midbrain dopamine function in schizophrenia and depression: a post-mortem and positron emission tomographic imaging study. Brain. 2013;136(11):3242–51.
Kapur S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003;160(1):13–23.
Tollefson GD, Beasley CM, Tran PV, Street JS, Krueger JA, Tamura RN, et al. Olanzapine versus haloperidol in the treatment of schizophrenia and schizoaffective and schizophreniform disorders: results of an international collaborative trial. Am J Psychiatry. 1997;154(4):457–65.
Glazer WM. Review of incidence studies of tardive dyskinesia associated with typical antipsychotics. J Clin Psychiatry. 2000;61(Suppl 4):15–20.
Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles: an integrated system of multi-informant assessment. Burlington: University of Vermont, Research Center for Children, Youth & Families; 2001.
Phillips LJ, Nelson B, Yuen HP, Francey SM, Simmons M, Stanford C, et al. Randomized controlled trial of interventions for young people at ultra-high risk of psychosis: study design and baseline characteristics. Aust N Z J Psychiatry. 2009;43(9):818–29.
Yung AR, Phillips LJ, Nelson B, Francey SM, PanYuen H, Simmons MB, et al. Randomized controlled trial of interventions for young people at ultra high risk for psychosis: 6-month analysis. J Clin Psychiatry. 2011;72(4):430–40.
Woods SW, Tully EM, Walsh BC, Hawkins KA, Callahan JL, Cohen SJ, et al. Aripiprazole in the treatment of the psychosis prodrome: an open-label pilot study. Br J Psychiatry. 2007;191(51):s96–101. Available at: http://bjp.rcpsych.org/content/191/51/s96. Accessed 28 Sep 2017
Tsujino N, Nemoto T, Morita K, Katagiri N, Ito S, Mizuno M. Long-term efficacy and tolerability of perospirone for young help-seeking people at clinical high risk: a preliminary open trial. Clin Psychopharmacol Neurosci. 2013;11(3):132–6.
McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller TJ, Woods SW, et al. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis: I. Study rationale and design. Schizophr Res. 2003;61(1):7–18.
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29(4):703–15.
Woods SW, Breier A, Zipursky RB, Perkins DO, Addington J, Miller TJ, et al. Randomized trial of olanzapine versus placebo in the symptomatic acute treatment of the schizophrenic prodrome. Biol Psychiatry. 2003;54(4):453–64.
McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller T, Woods SW, et al. Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry. 2006;163(5):790–9.
Guy W, editor. ECDEU assessment manual for psychopharmacology. Rockville: US Department of Health, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration; 1976.
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(4):382–9.
Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133(5):429–35.
Hall RC. Global assessment of functioning. A modified scale. Psychosomatics. 1995;36(3):267–75.
Smesny S, Gussew A, Biesel NJ, Schack S, Walther M, Rzanny R, et al. Glutamatergic dysfunction linked to energy and membrane lipid metabolism in frontal and anterior cingulate cortices of never treated first-episode schizophrenia patients. Schizophr Res. 2015;168(1–2):322–9.
Amminger GP, Schäfer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, et al. Long-chain ω-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146–54.
Amminger PG, Schäfer MR, Schlögelhofer M, Klier C, Mcgorry P. Longer-term outcome in the prevention of psychotic disorders by the Vienna omega-3 study. Nat Commun. 2015;6:7934.
McGorry PD, Nelson B, Markulev C, Yuen HP, Schäfer MR, Mossaheb N, et al. Effect of ω-3 polyunsaturated fatty acids in young people at ultrahigh risk for psychotic disorders: the NEURAPRO Randomized Clinical Trial. JAMA Psychiat. 2017;74(1):19–27.
Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10(3):799–812.
Rybarczyk B. Social and Occupational Functioning Assessment Scale (SOFAS). In: Kreutzer JS, DeLuca J, Caplan B, editors. Encyclopedia of clinical neuropsychology. New York: Springer; 2011. p. 2313.
Auther AM, Smith CW, Cornblatt BA. Global functioning: social scale (GF: Social). Glen Oaks: Zucker Hillside Hospital; 2006.
Sayed Y, Garrison JM. The dopamine hypothesis of schizophrenia and the antagonistic action of neuroleptic drugs – a review. Psychopharmacol Bull. 1983;19(2):283–8.
Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III – the final common pathway. Schizophr Bull. 2009;35(3):549–62.
Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301–8.
Javitt DC, Zukin SR, Heresco-Levy U, Umbricht D. Has an angel shown the way? Etiological and therapeutic implications of the PCP/NMDA model of schizophrenia. Schizophr Bull. 2012;38(5):958–66.
Kantrowitz JT, Javitt DC. N-methyl-d-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull. 2010;83(3–4):108–21.
Balla A, Schneider S, Sershen H, Javitt DC. Effects of novel, high affinity glycine transport inhibitors on frontostriatal dopamine release in a rodent model of schizophrenia. Eur Neuropsychopharmacol. 2012;22(12):902–10.
Hashimoto K. Glycine transport inhibitors for the treatment of schizophrenia. Open Med Chem J. 2010;4:10–9.
Tuominen HJ, Tiihonen J, Wahlbeck K. Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2005;72(2–3):225–34.
Tsai GE, Lin P-Y. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia, a critical review and meta-analysis. Curr Pharm Des. 2010;16(5):522–37.
Singh SP, Singh V. Meta-analysis of the efficacy of adjunctive NMDA receptor modulators in chronic schizophrenia. CNS Drugs. 2011;25(10):859–85.
Woods SW, Walsh BC, Hawkins KA, Miller TJ, Saksa JR, D’Souza DC, et al. Glycine treatment of the risk syndrome for psychosis: report of two pilot studies. Eur Neuropsychopharmacol. 2013;23(8):931–40.
Kantrowitz JT, Woods SW, Petkova E, Cornblatt B, Corcoran CM, Chen H, et al. D-serine for the treatment of negative symptoms in individuals at clinical high risk of schizophrenia: a pilot, double-blind, placebo-controlled, randomised parallel group mechanistic proof-of-concept trial. Lancet Psychiatry. 2015;2(5):403–12.
Cornblatt BA, Auther AM, Niendam T, Smith CW, Zinberg J, Bearden CE, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007;33(3):688–702.
Manji HK, Moore GJ, Chen G. Lithium at 50: have the neuroprotective effects of this unique cation been overlooked? Biol Psychiatry. 1999;46(7):929–40.
Chen G, Zeng W-Z, Yuan P-X, Huang L-D, Jiang Y-M, Zhao Z-H, et al. The Mood-stabilizing agents lithium and valproate robustly increase the levels of the neuroprotective protein bcl-2 in the CNS. J Neurochem. 1999;72(2):879–82.
Berger G, Wood S, Ross M, Hamer CA, Wellard M, Pell G, et al. Neuroprotective effects of low-dose lithium in individuals at ultra-high risk for psychosis. A longitudinal MRI/MRS study. Curr Pharm Des. 2012;18:570–5.
Flatow J, Buckley P, Miller BJ. Meta-analysis of oxidative stress in schizophrenia. Biol Psychiatry. 2013;74(6):400–9.
Kirkpatrick B, Miller BJ. Inflammation and schizophrenia. Schizophr Bull. 2013;39(6):1174–9.
Garety PA. The future of psychological therapies for psychosis. World Psychiatry. 2003;2(3):147–52.
Garety PA, Fowler D, Kuipers E. Cognitive-behavioral therapy for medication-resistant symptoms. Schizophr Bull. 2000;26(1):73–86.
Kuipers E, Garety P, Fowler D, Freeman D, Dunn G, Bebbington P. Cognitive, emotional, and social processes in psychosis: refining cognitive behavioral therapy for persistent positive symptoms. Schizophr Bull. 2006;32(Suppl 1):S24–31.
Freeman D, Garety PA. Connecting neurosis and psychosis: the direct influence of emotion on delusions and hallucinations. Behav Res Ther. 2003;41(8):923–47.
Addington J, Epstein I, Liu L, French P, Boydell KM, Zipursky RB. A randomized controlled trial of cognitive behavioural therapy for individuals at clinical high risk of psychosis. Schizophr Res. 2011;125(1):54–61.
Morrison AP, French P, Stewart SLK, Birchwood M, Fowler D, Gumley AI, et al. Early detection and intervention evaluation for people at risk of psychosis: multisite randomised controlled trial. BMJ. 2012;344:e2233.
van der Gaag M, Nieman DH, Rietdijk J, Dragt S, Ising HK, Klaassen RMC, et al. Cognitive behavioral therapy for subjects at ultrahigh risk for developing psychosis: a randomized controlled clinical trial. Schizophr Bull. 2012;38(6):1180–8.
Corcoran C, Davidson L, Sills-Shahar R, Nickou C, Malaspina D, Miller T, et al. A qualitative research study of the evolution of symptoms in individuals identified as prodromal to psychosis. Psychiatry Q. 2003;74(4):313–32.
Yung AR, McGorry PD. The initial prodrome in psychosis: descriptive and qualitative aspects. Aust N Z J Psychiatry. 1996;30(5):587–99.
Miklowitz DJ, O’Brien MP, Schlosser DA, Addington J, Candan KA, Marshall C, et al. Family-focused treatment for adolescents and young adults at high risk for psychosis: results of a randomized trial. J Am Acad Child Adolesc Psychiatry. 2014;53(8):848–58.
O’Brien MP, Miklowitz DJ, Candan KA, Marshall C, Domingues I, Walsh BC, et al. A randomized trial of family focused therapy with populations at clinical high risk for psychosis: effects on interactional behavior. J Consult Clin Psychol. 2014;82(1):90–101.
Woodberry KA, Seidman LJ, Giuliano AJ, Verdi MB, Cook WL, McFarlane WR. Neuropsychological profiles in individuals at clinical high risk for psychosis: relationship to psychosis and intelligence. Schizophr Res. 2010;123(2):188–98.
Carrión RE, Cornblatt BA, McLaughlin D, Chang J, Auther AM, Olsen RH, et al. Contributions of early cortical processing and reading ability to functional status in individuals at clinical high risk for psychosis. Schizophr Res. 2015;164(1):1–7.
Rauchensteiner S, Kawohl W, Ozgurdal S, Littmann E, Gudlowski Y, Witthaus H, et al. Test-performance after cognitive training in persons at risk mental state of schizophrenia and patients with schizophrenia. Psychiatry Res. 2011;185(3):334–9.
Hooker CI, Carol EE, Eisenstein TJ, Yin H, Lincoln SH, Tully LM, et al. A pilot study of cognitive training in clinical high risk for psychosis: initial evidence of cognitive benefit. Schizophr Res. 2014;157(1–3):314–6.
Piskulic D, Barbato M, Liu L, Addington J. Pilot study of cognitive remediation therapy on cognition in young people at clinical high risk of psychosis. Psychiatry Res. 2015;225(1–2):93–8.
Bechdolf A, Wagner M, Ruhrmann S, Harrigan S, Putzfeld V, Pukrop R, et al. Preventing progression to first-episode psychosis in early initial prodromal states. Br J Psychiatry. 2012;2000(1):22–9.
Holzer L, Urben S, Passini CM, Jaugey L, Herzog MH, Halfon O, et al. A randomized controlled trial of the effectiveness of computer-assisted cognitive remediation (CACR) in adolescents with psychosis or at high risk of psychosis. Behav Cogn Psychother. 2014;42(4):421–34.
Loewy R, Fisher M, Schlosser DA, Biagianti B, Stuart B, Mathalon DH, et al. Intensive auditory cognitive training improves verbal memory in adolescents and young adults at clinical high risk for psychosis. Schizophr Bull. 2016;42(Suppl 1):S118–26.
Choi J, Corcoran CM, Fiszdon JM, Stevens M, Javitt DC, Deasy M, et al. Pupillometer-based neurofeedback cognitive training to improve processing speed and social functioning in individuals at clinical high risk for psychosis. Psychiatr Rehabil J. 2017;40(1):33–42.
Fisher M, Holland C, Merzenich MM, Vinogradov S. Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. Am J Psychiatry. 2009;166(7):805–11.
Carrión RE, Goldberg TE, McLaughlin D, Auther AM, Correll CU, Cornblatt BA. Impact of neurocognition on social and role functioning in individuals at clinical high risk for psychosis. Am J Psychiatry. 2011;168(8):806–13.
Granholm E, Verney SP, Perivoliotis D, Miura T. Effortful cognitive resource allocation and negative symptom severity in chronic schizophrenia. Schizophr Bull. 2007;33(3):831–42.
Kern RS, Liberman RP, Kopelowicz A, Mintz J, Green MF. Applications of errorless learning for improving work performance in persons with schizophrenia. Am J Psychiatry. 2002;159(11):1921–6.
Choi J, Medalia A. Intrinsic motivation and learning in a schizophrenia spectrum sample. Schizophr Res. 2010;118(1):12–9.
Nordentoft M, Thorup A, Petersen L, Øhlenschlæger J, Melau M, Christensen TØ, et al. Transition rates from schizotypal disorder to psychotic disorder for first-contact patients included in the OPUS trial. A randomized clinical trial of integrated treatment and standard treatment. Schizophr Res. 2006;83(1):29–40.
Henquet C, Murray R, Linszen D, van Os J. The environment and schizophrenia: the role of cannabis use. Schizophr Bull. 2005;31(3):608–12.
Ruhrmann S, Bechdolf A, Kühn K-U, Wagner M, Schultze-Lutter F, Janssen B, et al. Acute effects of treatment for prodromal symptoms for people putatively in a late initial prodromal state of psychosis. Br J Psychiatry. 2007;191(51):s88–95.
McGorry PD, Nelson B, Phillips LJ, Yuen HP, Francey SM, Thampi A, et al. Randomized controlled trial of interventions for young people at ultra-high risk of psychosis: twelve-month outcome. J Clin Psychiatry. 2013;74(4):349–56.
Phillips LJ, McGorry PD, Yuen HP, Ward J, Donovan K, Kelly D, et al. Medium term follow-up of a randomized controlled trial of interventions for young people at ultra high risk of psychosis. Schizophr Res. 2007;96(1):25–33.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bilgrami, Z.R., Kostek, N., Kim, I.T., Kraut, R.A., Kim, J.K., Corcoran, C.M. (2020). Attenuated Psychosis Syndrome. In: Shrivastava, A., De Sousa, A. (eds) Schizophrenia Treatment Outcomes. Springer, Cham. https://doi.org/10.1007/978-3-030-19847-3_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-19847-3_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-19846-6
Online ISBN: 978-3-030-19847-3
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)