Abstract
This chapter is a clinical overview of resilience as a measure of outcome and recovery in schizophrenia. The chapter starts with an elucidation of the concept of resilience as applied in psychiatry. The basic neurobiology of resilience and resilience as a psychobiological construct for the pathogenesis of psychiatric disorders is discussed. This is followed by a discussion of specific factors in the neurobiology and genetics of mechanisms that enhance resilience and also play a role in the recovery from schizophrenia. Studies in the realm of schizophrenia and resilience (both long term and short term) and neuroimaging data are discussed, and certain points of relevance from a clinical perspective for resilience and recovery from schizophrenia are discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
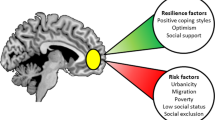
Resilience is the capacity and dynamic process of overcoming stress and adversity while maintaining normal psychological and physical functioning and bouncing back to earlier levels of function [1]. Each individual shall experience stress, and everybody is exposed to trauma at some point of time in their lives. Resilience has now been implicated as a psychobiological construct as an important factor in the maintenance of remission, in the prevention of relapse, and during recovery from psychiatric illnesses [2]. The role of resilience has been explored across research in all psychiatric disorders like post-traumatic stress disorder, affective disorders, depression, and schizophrenia. The understanding of resilience is of great relevance in building effective coping styles, dealing with maladaptive coping, and understanding the stress response in psychiatric illnesses [3]. Resilience has huge psychological, social, biological, and neuroendocrine underpinnings that affect the outcome of psychiatric disorders. Mechanisms that include genetic, epigenetic, developmental, psychological, and neurochemical factors that play a role in resilience development and promotion have been identified with respect to psychiatric disorders [4]. Resilience plays a very important role in the response and recovery of schizophrenia as well as in the prevention of relapse and also matters when we look at how the family of a patient with schizophrenia copes with the illness. This chapter aims to present an overview of the role of resilience in promoting recovery and positive outcomes in schizophrenia.
The Concept of Resilience
Within the field of psychology, early inquiry examining resilience represented a paradigm shift from looking at risk factors that led to psychosocial problems to the identification of strengths of an individual [5]. Resilience is the ability to adapt successfully in the face of stress, adversity, or any situation/event that leads to a negative emotional experience. As formally defined, resilience is the ability of individuals to bounce back after trauma and return to their previous psychological selves [6]. Resilience is a construct with inherent biological and psychological factors that affect it [7] and consequently lead to substantial ramifications. It is also implicated as a marker of psychopathology in various disorders and plays a role in the recovery from trauma and stressful events [8]. It is crucial to note that in the definition of resilience, psychological and physical functioning are maintained in the face of adversity. Although the understanding of resilience is nascent, recent investigations have identified several mechanisms encompassing genetic, epigenetic, developmental, psychological, and neurochemical factors that underlie the development of and enhancement of resilience and factors that predict vulnerability to stress and susceptibility to psychiatric disorders in the face of stress and trauma [9].
Resilience is an individualistic and contextualized construct that builds, depending on the experience that one goes through. The extent of level of resilience also varies depending on the internal and external sources of support and protection available to the individual. The individual traits that allow the more flexible outcomes undoubtedly depend upon a foundational capacity of that individual that is built upon experiences in the life course, particularly early, that promote the development of healthy brain architecture supporting cognitive flexibility that allows the brain to continue to change with ongoing experiences. There is no single agreed-upon definition of resilience, but the construct is understood under various lenses depending on the context of study [10].
Resilience as a Psychobiological Construct
With the paradigm shift in understanding the concept of resilience, the construct (of resilience) is increasingly being understood as a psychobiological one, especially in the context of psychiatric disorders. Quintessential to remember is that resilience can be a protective factor against the development of mental disorders and also be a risk factor for a number of clinical conditions [11]. It has been well established that resilience is lower in individuals suffering from a psychiatric condition or disorder and that higher levels of resilience may prevent the development of an illness or minimize the severity of illness [12]. Trauma, its intensity, and the number of traumatic incidences are inversely proportional to resilience. The lesser the frequency and intensity of trauma, the higher the resilience and vice versa. However, this is a simplistic understanding to the relationship between trauma and resilience, and there are multiple variables including the personality organization, available support, nature of protection in environment, and several other factors that influence the interplay [13]. Having suffered trauma once is enough to influence the way in which the brain functions and is structured to manage trauma. This brings us to an understanding that every individual who has suffered trauma reacts to and manages it differently—even if the nature of trauma has been similar. Therefore, their brains undergo differential functional and structural changes. This functional and structural change is markedly different between individuals who have, and those who have not, undergone traumatic experiences [14]. Resilience helps to minimize the extent of pathogenesis in developmental process or transition from health to disease or wellness or illness by facilitating or arresting conversion to illness.
There is a strong argument which claims that response to trauma develops through resilience, and although some neurobiological changes correlate with resilience and trauma, it is unclear whether the nature and degree of response to trauma are dependent on the extent of neurobiological changes alone. The level for resilience protection and modification also depends on other complex factors that shape the influence of resilience on individuals experiencing trauma [15]. The capacity to which resilience is able to act as a preventative measure seems to have a strong correlation to ingrained psychosocial factors. Human cognitive factors have been recognized as potential possible factors that may help determine the level of resilience in an individual, depending on the way an individual responds to trauma. The cognitive factors that act to maintain and uphold resilience are active coping, cognitive flexibility, and social support [16]. Research claims that resilience is mediated by adaptive changes in several neural circuits involving numerous neurotransmitter and molecular pathways [2]. Along with psychosocial factors, it is also the interplay with neurobiological factors that determines resilience as an outcome in psychiatric illnesses.
Linked with the concept of resilience is the concept of allostasis. The active process of responding to challenges and adaptive changes is called allostasis. This process involves multiple mediators such as the autonomic nervous system, cortisol, immune and inflammatory markers, metabolic factors, and neuromodulators within the brain that interact in a nonlinear fashion with each other and promote adaptation in the short run as long as they are turned on efficiently when needed and turned off promptly when no longer needed [17]. Neurobiological research has implicated several brain structures and molecular models that are involved in the stress and trauma reaction/coping. Of all, the cortical and limbic structures are most involved. The mechanism of trauma can be simply understood by the activity of the cortical and limbic structures on the hypothalamic–pituitary–adrenal (HPA) axis and their influence on glucocorticoid-mediated negative feedback that acts as major trigger for the fearful memories (stress/trauma) [18]. Neurochemical and neuroendocrine changes occurring in response to trauma may lead to neuronal loss and functional disconnectivity. Changes in neuroplasticity, HPA axis response to stress, and neurotransmissions of dopamine, serotonin, and norepinephrine play an important role in maintaining homeostasis of resilience plasticity [3].
Resilience is increasingly being studied in the phenomenon of mental illnesses and more so recently with patients suffering from schizophrenia [19]. Evidence says that 80% of patients with first episode of schizophrenia will have another episode in the span of 5 years. Social and clinical recovery in these patients is low. The state of transition from illness to wellness has grown with the revolutionary interventions for disorders like schizophrenia [20]. Cognitive dysfunction is one of the earliest signs of the illness, which begins with deteriorating memory functions, learning, and social cognition and finally impairment. Cognitive dysfunction further leads to socio-occupational and functional impairments. Due to this, an individual’s psychosocial responses to stressors inevitably come down. Thus, resilience as a phenomenon is directly impacted in outcome of the illness. Though there is no clearly explained association between cognitive impairment and poor outcomes in schizophrenia, several neurobiological and psychobiological processes explain the mechanism of a pathway for poor outcomes from cognitive impairment [21, 22].
Critical Aspects of the Neurobiology of Resilience Relevant to Outcome and Recovery in Schizophrenia
In last few years, there has been increasing interest in the active, adaptive coping mechanisms of resilience, with a lot of work focusing on the neurobiological correlates that are associated with resilience. The human brain exhibits a remarkable degree of resilience in the face of extreme stress, resisting the development of neuropsychiatric disorders. The brain perceives potential threats and determines the response, thus acting as a central organ of stress [23]. Moreover, the brain is a plastic organ that changes its architecture, gene expression, and function through internal neurobiological and hormonal mechanisms when faced with stress. The goal is to recognize those biological changes that underlie flexible adaptability, and to recognize these factors that indicate resilience, particularly when the individual is challenged by new circumstances [24]. This is governed by early life experiences that determine individual differences in such capabilities by laying down the brain architecture that determines the flexible adaptation or the lack thereof [25].
Genetics
Genetic factors contribute to the risk, as well as resilience, of the psychiatric disorders. Huge research work has been done to identify the candidate genes with relatively weak associations. The field is now pivoting increasingly to genome-wide studies on large numbers of people to parse the complex genetic contributions to psychiatric disorders [26].
Hypothalamic–Pituitary–Adrenal Axis-Related Genes
Regulation of the HPA axis is affected by genetic factors. Functional variants of the brain mineralocorticoid receptor (MR) and glucocorticoid receptor (GR), which are respectively involved in setting the threshold and regulating the termination of the HPA axis response to stress, have also been identified in humans [27]. Interestingly, four SNPs of FKBP5 (rs9296158, rs3800373, rs1360780, and rs9470080), a gene that codes for a “chaperone” protein that regulates GR sensitivity, were found in patients with PTSD [28]. Many such genes are now being investigated for schizophrenia.
The Human Serotonin Transporter Gene (5-HTTLPR; aka SLC6A4)
The short allele is associated with decreased serotonin transporter availability and a resulting lower reuptake of serotonin from synaptic clefts, leading to risk for depression when exposed to stressful life events. An association between the long allele of 5-HTTLPR and emotional resilience has been found [29].
COMT
Val158 Met gene polymorphism that codes for COMT is linked to resilience. Individuals with the low-functioning Met158 allele have higher circulating levels dopamine and noradrenaline. Thus, they tend to exhibit higher anxiety levels, increased plasma adrenaline levels in response to stress, and lower resilience to negative mood states [30]. Recent research has focused on the implications of the COMT gene in schizophrenia [31].
Neuropeptide Y
The level of neuropeptide Y mRNA expression showed an inverse correlation with trait anxiety, as well as a direct correlation with levels of stress-induced endogenous opioid release, which is implicated in the suppression of pain and stress responses [32]. Neuropeptide Y has also been implicated in the neurobiology of schizophrenia as per new research [33].
Brain-Derived Neurotrophic Factor (BDNF)
A single nucleotide polymorphism (G196A, Val66Met) in the gene that encodes BDNF in humans significantly impairs BDNF’s intracellular trafficking and activity-dependent release Met66 allele. This leads to reduced BDNF function with greater anxiety-like behavior and impaired hippocampus-dependent learning, but resilient to chronic stress [34]. BDNF genes play a role in the pathogenesis of depressive features and negative symptoms that may be seen in schizophrenia [35].
Gene–Gene and Gene–Environment Interactions
Evidence of gene–gene and gene–environment interactions underlying interindividual variability in stress responses have been postulated. An interaction of 5-HTTLPR-COMT genes and stressful life events leads to the risk for depression [36]. Researchers have reported gene–environment interactions that influence the risk for depression in maltreated children. They reported that social support seems to mitigate the effects of the short allele of 5-HTTLPR61 and the 5-HTTLPR and BDNF Val66Met genotypes that cause risk of depression when exposed to stressful life events [37].
Epigenetics
Good environment for nurturing and rearing practices shows attenuated corticosteroid responses to stress and expresses higher levels of glucocorticoid receptors (GR) in the hippocampus. This enhanced GR expression is mediated by nerve growth factor-inducible protein A (NGFI-A; also known as EGR1). However, little nurturing and poor rearing practices show increased methylation of the GR gene promoter at the NGFI-A binding site in the hippocampus, an epigenetic change that is associated with reduced GR expression [38, 39]. This difference in methylation emerges in the first week of life and persists into adulthood and is passed on to their offspring. Epigenetic changes that occur during brain development are an additional means by which behavioral variability is generated in individuals, better preparing the species for a host of possible environmental challenges [40].
Neurotransmitters
Hypothalamic–Pituitary–Adrenal (HPA) Axis
Stress leads to activation of the HPA axis, which results in widespread hormonal, neurochemical, and physiological alterations in the body. Glucocorticoids thus released interact with steroid receptors, leading transcription factors to regulate cellular function. Glucocorticoid receptors (GRs) and mineralocorticoid receptors (MRs) are expressed at high levels in the hippocampus, amygdala, prefrontal cortex (PFC), and other limbic and midbrain structures, where they modulate the neural circuitry and neuroendocrine systems that underlie behavioral responses to stress [40].
Norepinephrine and Dopamine
Hyper-responsiveness of the locus ceruleus-norepinephrine system may result in chronic anxiety and fear. The norepinephrine transporter (NET) and receptors (α- and β-adrenoreceptors) involved in norepinephrine signaling have been implicated as biological mediators of stress-related psychiatric disorders and resilience. Dopamine release upon stress is increased in the PFC and inhibited in the nucleus accumbens, an area mainly associated with the reward pathway. Some studies have found decreased levels of circulating dopamine in depression [41]. There have been many research reports on the role of norepinephrine in the genesis of negative symptoms in schizophrenia [42].
Dehydroepiandrosterone (DHEA)
DHEA is a precursor for the synthesis of anabolic steroids and is co-released with cortisol in response to stress. Reports have shown that blood DHEA levels increase under acute stress and that a higher level of DHEA, or a higher DHEA to cortisol ratio, is associated with less dissociative symptoms and superior performance in healthy subjects undergoing military survival training [43]. The role of DHEA in schizophrenia is currently being investigated [44].
Serotonin
Acute stress leads to increased serotonin turnover in multiple brain areas. Serotonin affects the regulation of stress response and emotional behavior through 5-HT1–7 receptors [45]. Literature abounds with data on the role of specific serotonin receptors in the genesis of certain symptoms and in the psychopathology of schizophrenia [46].
Testosterone
Testosterone has been strongly linked to social rank and aggression. It serves as a pro-resilience factor by promoting positive mood and social connectedness [47]. There are reviews on the role of testosterone as a treatment option in the long-term management of schizophrenia. Low testosterone levels have been linked to negative symptoms in schizophrenia [48].
BDNF
Hippocampal BDNF expression contributed critically to resilient adaptations to chronic stress. BDNF acts through its two main receptors Trk-B and p75 [49]. Central administration of BDNF has antidepressant-like effects and can enhance hippocampal neurogenesis. Evidence from animal and human studies shows that administration of antidepressants can lead to increase of BDNF and TrkB expression in the hippocampus and PFC, suggesting a role of BDNF-TrkB signaling in the behavioral effects of antidepressants. Nevertheless, there is also evidence for antidepressant effects without changes in BDNF or neurogenesis [50].
Glutamate, GABA, and endocannabinoids
Glutamate, GABA, and endocannabinoids have also been widely studied and implicated in the stress response, resilience, and pathophysiology of mood and anxiety disorders. The dysregulation of these systems can lead to profound deficits in successful adaptation to acute and chronic stress. Pharmacological studies targeting these systems in psychiatric disorders have begun to show promising results in achieving therapeutic effects [51,52,53]. The endocannabinoids have been extensively studied in the pathogenesis and treatment of schizophrenia, and their relation to the genesis of psychosis is also under investigation [54].
Glutamatergic Signaling and Synaptic Connectivity
Animal models have been used to understand circuit-level synaptic changes in glutamate systems with far greater precision. The literature supports the idea that chronic stress reduces dendritic arborization and glutamatergic dendritic spine density of pyramidal neurons in the PFC and hippocampus and reduces hippocampus neurogenesis while increasing dendritic spine number or branching in amygdala and NAc [55]. Studies have shown greater degree of c-Fos, FosB, or ΔFosB expression in glutamatergic neurons of mPFC (infralimbic, paralimbic PFC) of resilient mice following chronic predator or social defeat stress [56]. Increased expression of these immediate early genes would suggest increased neuronal activation within this brain region, which might represent a pro-resilience adaptation.
Neural Circuits of Resilience
Animal and human studies have identified functional neural circuits and interactions among multiple brain regions, such as the amygdala, PFC, and nucleus accumbens, that are involved in the regulation of adaptive psychobiological responses to stress and adversities. Reduced insular activation under stress has been linked to greater non-reactivity to inner experience, a key component of trait mindfulness which may protect against negative bias and reduce depression vulnerability [57]. By potentially targeting the top-down and bottom-up regulation of these neural circuits, psychotherapeutic interventions including cognitive behavioral therapy with cognitive reappraisal, positive emotion exercises, coping skill training, well-being therapy, and mindfulness meditation can be efficacious approaches to build and enhance resilient psychosocial responses to stress [58].
Resilience and Schizophrenia
The clinical expression of schizophrenia is diverse, and this significant heterogeneity is still unexplained. Schizophrenia is not a single disease entity, and there are several etiological factors and various pathophysiological mechanisms involved, with the most recent concept being a neurodevelopmental disorder [59]. Schizophrenia has a profound impact on the individual life and may lead to several adversities. Resilience represents positive adaptation in the face of adversity and has received increasing attention as a factor contributing to recovery in individuals with schizophrenia. Resilience is thus becoming an important topic as there is evidence that it increases the probability for long-term recovery [60]. This section shall look at important studies at the intersection of resilience and schizophrenia.
Resilience and Schizophrenia: Long-Term Follow-up Studies
Follow-up studies reveal that patients who have fully recovered from schizophrenia have the ability to endure setbacks without giving up hope. This quality of recovery is referred to as resilience, a construct which means “bouncing back” from difficult experiences [61]. A Norwegian study describes patients with fully recovered schizophrenia who were followed up for a period of 15 years. It consisted of 17 subjects interviewed with semi-structured interview and Connor-Davidson Resilience Scale (CD-RISC) to assess resilience. The results showed that nearly half the participants maintained full recovery. These subjects did not use any neuroleptic medication and had not done so for about 17 years. The findings represent potentially important clinical and research implications. The possibility of being cured of schizophrenia instilled hope in patients and helped reduce stigma about the disease, showing that persons with schizophrenia are not doomed to a life of disability. The results demonstrated the importance of separating the person from the disease when studying recovery in schizophrenia [62]. Optimism and willpower are personal attributes that characterize the recovered individuals in this study, which was reflected in their high scores on the resilience scale [63]. The data from this study indicate that there are important relationships between symptom severity and recovery process variables. The fully recovered participants had significantly higher resilience scores and significantly lower symptom scores than participants in remission, and there was a significant negative association between resilience and the PANSS negative subscale scores [62]. Other researchers decided to study the transcultural attributes in resilience across schizophrenia between Austria and Japan. Another objective was to examine transcultural differences in internalized stigma, self-esteem, and hopelessness, which can be expected to be relevant in this context, as well as the interrelations between these subjective elements of recovery and symptom severity. Notably, it was detected that a significant country effect with markedly lower resilience and self-esteem scores as well as higher hopelessness scores among Japanese subjects in general. In addition, both Austrian and Japanese patients indicated significantly lower degrees of resilience, self-esteem, and hope compared to healthy control subjects. This suggests that schizophrenia patients from Western European and Japanese cultures may have different needs to achieve recovery. In conclusion, it will be critical to develop culture-specific psychosocial programs and to examine their feasibility and effectiveness among these patients [63]. Kim and others described psychosocial functioning to be comprised among participants prone to ultrahigh risk [UHR] of psychosis; this dysfunction was associated with negative symptoms, adaptive coping, and resilience. In addition, baseline resilience was lower among those in the UHR group who converted to frank psychosis than among those who did not. Resilience has been shown to be lower among ultrahigh-risk individuals who convert to full-blown psychosis compared to those who do not [64]. In another study, patients meeting the full diagnostic criteria for schizophrenia were studied with resilience as the capacity to cope with and to gain insight into the illness, and resilience was shown to have a beneficial effect on the course of the illness [65].
Resilience and Schizophrenia: Developmental Studies
The parent–infant relationship is an important context for identifying very early risk and resilience factors as targets for the development of preventative interventions [66]. Authors systematically reviewed studies investigating the early caregiver–infant relationship and attachment in offspring of parents with schizophrenia. There was some evidence to support disturbances in maternal behavior among those with a diagnosis of schizophrenia, and there was more limited evidence of disturbances in infant behavior and mutuality of interaction, thus exhorting the need to investigate both sources of resilience and risk in the development of offspring of parents with a diagnosis of schizophrenia and psychosis [67]. Another study attempted to explore resilience and its correlates among the offsprings of parents with schizophrenia. The findings of the study showed that majority of the offspring reported medium resilience. High and medium resilient group had internal locus of control; engaged in coping mechanisms such as acceptance, religious coping, problem solving, and seeking social support; had positive self-concept such as likeability, task accomplishment, giftedness, and morality; had more satisfaction with emotional support; and had less non-utilization of support compared to low resilient group. The study highlights that majority of the offsprings were resilient and that the factors associated with resilience are presence of good support system, use of problem-focused coping strategies, and having positive self-concept [68].
Neuroimaging Studies
Researchers investigated the neurobiological underpinnings of resilience to self-stigma using neuropsychological and functional magnetic resonance imaging (fMRI) data. In a sample of 20 patients with schizophrenia, association strengths between social inferiority and schizophrenia were negatively correlated with activation strengths of the rostral-ventral medial prefrontal cortex (mPFC). Moreover, the mPFC activation strengths correlated negatively with activation in the right amygdala, suggesting that resilience to stigma is associated with emotion regulation [69]. There is a dearth of neurobiological and neuroimaging data on the interactions between resilience and schizophrenia, and further research in this area is warranted.
Psychological Studies
Henderson and Cock took a qualitative approach (i.e., grounded theory method) to study how ten patients experienced recovery after first-episode psychosis. Based on unstructured interviews, two styles of resilience were identified: “tenacity,” requiring effort over a period of time, and “rebounding,” springing back. In addition, internal and environmental resources including self-pacing and support from others were described as mechanisms of “harnessing resilience” [70]. Other research studied another relevant concept that potentially contributes to resilience in a sample of 74 non-remitted chronic schizophrenia patients, namely, “happiness.” While happiness was assessed using four items of the Center for Epidemiologic Studies-Depression (CES-D) scale , “trait resilience” and “event resilience” were measured using the Connor-Davidson Resilience Scale 10-item version and the Hardy-Gill Resilience Scale, respectively. Compared to healthy controls, lower levels of happiness were found in the schizophrenia group; higher levels of happiness were associated with higher resilience, along with lower perceived stress, higher optimism, and higher personal mastery [71].
Resilience and Suicide in Psychosis
Recent years have seen growing interest into concepts of resilience, but minimal research has explored resilience to suicide among psychosis. One study aimed to examine whether a proposed resilience factor—positive self-appraisals of the ability to cope with emotions and difficult situations and the ability to gain social support—could buffer against the negative impact of hopelessness among individuals with psychosis-spectrum disorders when measured cross-sectionally. Positive self-appraisals were found to moderate the association between hopelessness and suicidal ideation. For those reporting high levels of positive self-appraisals, increased levels of hopelessness were significantly less likely to lead to suicidality. These results provide cross-sectional evidence suggesting that positive self-appraisals may buffer individuals with psychosis against the pernicious impact of a well-known clinical risk factor, hopelessness. Accounting for positive self-appraisals may improve identification of individuals at high risk of suicidality and may be an important area to target for suicide interventions [72].
Critical Clinical Aspects of Resilience in the Outcome and Recovery from Schizophrenia
If one has to understand how resilience may impact outcome and recovery in schizophrenia, the understanding has to be multidimensional. Studies that involve resilience and schizophrenia have been multimodal and of different types.
Some studies have focused on resilience and psychopathology, while others have focused on resilience and the impact of schizophrenia years after the illness has set in. There are other studies that focus on resilience groups which are at risk for the development of schizophrenia, i.e., offspring of patients who suffer from schizophrenia and nonpsychotic siblings of these patients. Many studies have been done using psychological rating scales, but very few studies using biomarkers or neuroimaging exist.
There are some confounding factors when various studies of resilience and outcome in schizophrenia are analyzed. There are no standard scales for the measurement of resilience, and various studies have used different measures. There is a dearth of longitudinal follow-up studies of resilience during the entire course of an illness like schizophrenia from prodrome to maintenance phase.
There are also no studies that look at interventions and treatment methods to promote resilience. Many studies have focused on protective factors associated with benign outcomes, while others have looked at dynamic processes leading to positive adaptation following psychosis.
Most studies in realm of resilience, outcome, and recovery in schizophrenia have been cross-sectional. Many findings warrant confirmation via prospective studies. Longitudinal studies must look at resilience as a dynamic process . Development of treatment programs to enhance resilience and their incorporation in schizophrenia relapse prevention treatment algorithms must be given due consideration in the coming years.
One must understand that resilience does not have a specific role, but plays an important role in every stage of schizophrenia, from the at-risk state to the prodromal state. Resilience determines the conversion of prodromal and at-risk states into full-blown psychosis.
Resilience determines how the patient and his or her family members cope with a diagnosis of schizophrenia and their positive attributes that determine recovery from the illness. Resilience also helps the patient cope with distressing symptoms of schizophrenia, enhances understanding of the illness, and improves compliance to medication and psychosocial treatments.
Resilience also plays a role in enhancing the effectiveness of psychotherapeutic treatments used in the management of schizophrenia and is a paramount patient variable in determining treatment outcome and recovery.
Conclusion
The relationship between resilience and recovery as well as outcome in schizophrenia is multipronged and complex. Resilience is a protective factor for various psychiatric disorders in both the development and recovery phases. The same holds true for serious mental illnesses like schizophrenia. Resilience is vital in the prevention, pathogenesis, recovery, and symptom alleviation in schizophrenia. Research into resilience and its role in schizophrenia are still in a nascent stage. There is need for further long-term prospective studies that look at neurobiological substrates, biomarkers, and neural circuitry that play a role in recovery from schizophrenia using resilience as a mediating mechanism. This shall go a long way toward our understanding of recovery as a process in schizophrenia and the role of resilience in mediating that process
References
Southwick SM, Charney DS. The science of resilience: implications for the prevention and treatment of depression. Science. 2012;338(6103):79–82.
Feder A, Nestler EJ, Charney DS. Psychobiology and molecular genetics of resilience. Nat Rev Neurosci. 2009;10(6):446–57.
Russo SJ, Murrough JW, Han MH, Charney DS, Nestler EJ. Neurobiology of resilience. Nat Neurosci. 2012;15(11):1475–84.
Wu G, Feder A, Cohen H, Kim JJ, Calderon S, Charney DS, Mathé AA. Understanding resilience. Front Behav Neurosci. 2013;7:10.
Richardson GE. The metatheory of resilience and resiliency. J Clin Psychol. 2002;58(3):307–21.
Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev. 2010;30(5):479–95.
Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol. 2005;1:255–91.
Rutter M. Annual research review: resilience–clinical implications. J Child Psychol Psychiatry. 2013;54(4):474–87.
Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol. 2014;5(1):25338.
Masten AS, Obradović J. Competence and resilience in development. Ann N Y Acad Sci. 2006;1094(1):13–27.
Tusaie K, Dyer J. Resilience: a historical review of the construct. Holist Nurs Pract. 2004;18(1):3–10.
Shrivastava A, Desousa A. Resilience: a psychobiological construct for psychiatric disorders. Indian J Psychiatry. 2016;58(1):38–43.
Boss P. Loss, trauma, and resilience: therapeutic work with ambiguous loss. New York: WW Norton & Company; 2006.
Tummala-Narra P. Conceptualizing trauma and resilience across diverse contexts: a multicultural perspective. J Aggress Maltreat Trauma. 2007;14(1–2):33–53.
Rutter M. Resilience as a dynamic concept. Dev Psychopathol. 2012;24(2):335–44.
Genet JJ, Siemer M. Flexible control in processing affective and non-affective material predicts individual differences in trait resilience. Cogn Emotion. 2011;25(2):380–8.
Karatsoreos IN, McEwen BS. Psychobiological allostasis: resistance, resilience and vulnerability. Trends Cogn Sci. 2011;15(12):576–84.
Stiller AL, Drugan RC, Hazi A, Kent SP. Stress resilience and vulnerability: the association with rearing conditions, endocrine function, immunology, and anxious behavior. Psychoneuroendocrinology. 2011;36(9):1383–95.
Cicchetti D, Garmezy N. Prospects and promises in the study of resilience. Dev Psychopathol. 1993;5(4):497–502.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379(9831):2063–71.
Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. 2006;32(Suppl 1):S44–63.
Davidson RJ. Affective style, psychopathology, and resilience: brain mechanisms and plasticity. Am Psychol. 2000;55(11):1196–202.
McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87(3):873–904.
Agaibi CE, Wilson JP. Trauma, PTSD, and resilience: a review of the literature. Trauma Violence Abuse. 2005;6(3):195–216.
Fox SE, Levitt P, Nelson CA III. How the timing and quality of early experiences influence the development of brain architecture. Child Dev. 2010;81(1):28–40.
Faraone SV, Tsuang MT, Tsuang DW. Genetics of mental disorders: a guide for students, clinicians, and researchers. New York: Guilford Press; 1999.
Mehta D, Binder EB. Gene× environment vulnerability factors for PTSD: the HPA-axis. Neuropharmacology. 2012;62(2):654–62.
Gillespie CF, Phifer J, Bradley B, Ressler KJ. Risk and resilience: genetic and environmental influences on development of the stress response. Depress Anxiety. 2009;26(11):984–92.
Risch N, Herrell R, Lehner T, Liang KY, Eaves L, Hoh J, et al. Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression: a meta-analysis. JAMA. 2009;301(23):2462–71.
Caspi A, Moffitt TE. Gene–environment interactions in psychiatry: joining forces with neuroscience. Nat Rev Neurosci. 2006;7(7):583–90.
Kang JI, Kim SJ, Song YY, Namkoong K, An SK. Genetic influence of COMT and BDNF gene polymorphisms on resilience in healthy college students. Neuropsychobiology. 2013;68(3):174–80.
Cohen H, Liu T, Kozlovsky N, Kaplan Z, Zohar J, Mathé AA. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350–63.
Eaton K, Sallee FR, Sah R. Relevance of neuropeptide Y (NPY) in psychiatry. Curr Top Med Chem. 2007;7(17):1645–59.
Rothman SM, Mattson MP. Activity-dependent, stress-responsive BDNF signaling and the quest for optimal brain health and resilience throughout the lifespan. Neuroscience. 2013;239:228–40.
Dudley KJ, Li X, Kobor MS, Kippin TE, Bredy TW. Epigenetic mechanisms mediating vulnerability and resilience to psychiatric disorders. Neurosci Biobehav Rev. 2011;35(7):1544–51.
Rutter M. Implications of resilience concepts for scientific understanding. Ann N Y Acad Sci. 2006;1094(1):1–2.
Heim C, Binder EB. Current research trends in early life stress and depression: review of human studies on sensitive periods, gene–environment interactions, and epigenetics. Exp Neurol. 2012;233(1):102–11.
Zannas AS, West AE. Epigenetics and the regulation of stress vulnerability and resilience. Neuroscience. 2014;264:157–70.
Luthar SS, editor. Resilience and vulnerability: adaptation in the context of childhood adversities. Cambridge, UK: Cambridge University Press; 2003.
Kudielka BM, Kirschbaum C. Sex differences in HPA axis responses to stress: a review. Biol Psychol. 2005;69(1):113–32.
Krystal JH, Neumeister A. Noradrenergic and serotonergic mechanisms in the neurobiology of posttraumatic stress disorder and resilience. Brain Res. 2009;1293:13–23.
Maletic V, Eramo A, Gwin K, Offord SJ, Duffy RA. The role of norepinephrine and its α-adrenergic receptors in the pathophysiology and treatment of major depressive disorder and schizophrenia: a systematic review. Front Psych. 2017;8:42.
Yehuda R, Brand SR, Golier JA, Yang RK. Clinical correlates of DHEA associated with post-traumatic stress disorder. Acta Psychiatr Scand. 2006;114(3):187–93.
Gallagher P, Watson S, Smith MS, Young AH, Ferrier IN. Plasma cortisol-dehydroepiandrosterone (DHEA) ratios in schizophrenia and bipolar disorder. Schizophr Res. 2007;90(1):258–65.
Cicchetti D, Rogosch FA. Gene× environment interaction and resilience: effects of child maltreatment and serotonin, corticotropin releasing hormone, dopamine, and oxytocin genes. Dev Psychopathol. 2012;24(2):411–27.
Kapur S, Remington G. Serotonin-dopamine interaction and its relevance to schizophrenia. Am J Psychiatry. 1996;153(4):466–78.
Eisenegger C, Haushofer J, Fehr E. The role of testosterone in social interaction. Trends Cogn Sci. 2011;15(6):263–71.
Akhondzadeh S, Rezaei F, Larijani B, Nejatisafa AA, Kashani L, Abbasi SH. Correlation between testosterone, gonadotropins and prolactin and severity of negative symptoms in male patients with chronic schizophrenia. Schizophr Res. 2006;84(2):405–10.
Zhang JC, Yao W, Hashimoto K. Brain-derived neurotrophic factor (BDNF)-TrkB signaling in inflammation-related depression and potential therapeutic targets. Curr Neuropharmacol. 2016;14(7):721–31.
Karatsoreos IN, McEwen BS. Resilience and vulnerability: a neurobiological perspective. F1000 Prime Reports. 2013;5.
Manji HK, Moore GJ, Rajkowska G, Chen G. Neuroplasticity and cellular resilience in mood disorders. Mol Psychiatry. 2000;5(6):578–93.
O’Leary OF, Felice D, Galimberti S, Savignac HM, Bravo JA, Crowley T, et al. GABAB (1) receptor subunit isoforms differentially regulate stress resilience. Proc Natl Acad Sci. 2014;111(42):15232–7.
Ménard C, Pfau ML, Hodes GE, Russo SJ. Immune and neuroendocrine mechanisms of stress vulnerability and resilience. Neuropsychopharmacology. 2017;42(1):62–80.
Delahanty DL, editor. The psychobiology of trauma and resilience across the lifespan. Lanham: Jason Aronson; 2008.
Yuste R, Bonhoeffer T. Genesis of dendritic spines: insights from ultrastructural and imaging studies. Nat Rev Neurosci. 2004;5(1):24–34.
Boucher AA, Arnold JC, Hunt GE, Spiro A, Spencer J, Brown C, et al. Resilience and reduced c-Fos expression in P2X7 receptor knockout mice exposed to repeated forced swim test. Neuroscience. 2011;189:170–7.
Franklin TB, Saab BJ, Mansuy IM. Neural mechanisms of stress resilience and vulnerability. Neuron. 2012;75(5):747–61.
Singh-Taylor A, Korosi A, Molet J, Gunn BG, Baram TZ. Synaptic rewiring of stress-sensitive neurons by early-life experience: a mechanism for resilience? Neurobiol Stress. 2015;1:109–15.
Insel TR. Rethinking schizophrenia. Nature. 2010;468(7321):187–93.
Ridgway P. Restorying psychiatric disability: learning from first person recovery narratives. Psychiatr Rehabil J. 2001;24(4):335–45.
Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Austr N Z J Psychiatry. 2003;37(5):586–94.
Torgalsbøen AK. Sustaining full recovery in schizophrenia after 15 years: does resilience matter? Clin Schizophr Relat Psychoses. 2011;5(4):193–200.
Hofer A, Mizuno Y, Frajo-Apor B, Kemmler G, Suzuki T, Pardeller S, et al. Resilience, internalized stigma, self-esteem, and hopelessness among people with schizophrenia: cultural comparison in Austria and Japan. Schizophr Res. 2016;171(1):86–91.
Kim KR, Song YY, Park JY, Lee EH, Lee M, Lee SY, et al. The relationship between psychosocial functioning and resilience and negative symptoms in individuals at ultra-high risk for psychosis. Austr N Z J Psychiatry. 2013;47(8):762–71.
Reddy SK, Thirthalli J, Channaveerachari NK, Reddy KN, Ramareddy RN, Rawat VS, et al. Factors influencing access to psychiatric treatment in persons with schizophrenia: a qualitative study in a rural community. Indian J Psychiatry. 2014;56(1):54–60.
Beeghly M, Tronick E. Early resilience in the context of parent–infant relationships: a social developmental perspective. Curr Probl Pediatr Adolesc Health Care. 2011;41(7):197–201.
Blaustein ME, Kinniburgh KM. Treating traumatic stress in children and adolescents: how to foster resilience through attachment, self-regulation, and competency. New York: Guilford Press; 2010.
Herbert HS, Manjula M, Philip M. Growing up with a parent having schizophrenia: experiences and resilience in the offsprings. Indian J Psychol Med. 2013;35(2):148–53.
Raij TT, Korkeila J, Joutsenniemi K. Association of stigma resistance with emotion regulation—functional magnetic resonance imaging and neuropsychological findings. Compr Psychiatry. 2014;55:727–35.
Henderson AR, Cock A. The responses of young people to their experiences of first-episode psychosis: harnessing resilience. Commun Ment Health J. 2015;51(3):322–8.
Palmer BW, Heaton SC, Jeste DV. Older patients with schizophrenia: challenges in the coming decades. Psychiatr Serv. 1999;50(9):1178–83.
Warner R. Recovery from schizophrenia: psychiatry and political economy. London: Routledge; 2013.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Dikshit, R., Lodha, P., Shrivastava, A., De Sousa, A. (2020). Resilience as a Measure of Outcome and Recovery in Schizophrenia. In: Shrivastava, A., De Sousa, A. (eds) Schizophrenia Treatment Outcomes. Springer, Cham. https://doi.org/10.1007/978-3-030-19847-3_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-19847-3_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-19846-6
Online ISBN: 978-3-030-19847-3
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)