Abstract
Mankind is in continuous exposure of varying infectious agents either through air, food or water. Air is the most common vector for the allergen. Amongst all the infections caused, the fungi Aspergillus is the most frequent disease-causing mould. It leads to the pathological condition depending upon the host’s immune status or pulmonary structure. Chronic obstructive pulmonary disease (COPD) and invasive pulmonary aspergillosis (IPA) are the two most common pulmonary diseases. These pulmonary impairments dramatically increase with the growing number of patients possessing impaired immune state which directly affects the management of malignancy, organ transplantation and autoimmune and inflammatory conditions of critically ill patients. The biggest challenge is to develop a technique which could allow us to detect the disease at earlier stages and to treat them before developing the co-morbidities. With the current advancement and development of effective and better-tolerated antifungal agents, we have been able to lower the mortality rate up to a certain level, but, still, we have much to go. To cope up with the disease and adverse effects, we should first need to explore the epidemiology and pathophysiology of the disease so that we may be able to come up with the better treatment options for the condition. The present chapter deals with the epidemiology, pathophysiology and symptoms of COPD along with the IPA.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Aspergillus
- Chronic obstructive pulmonary disease (COPD)
- Invasive pulmonary aspergillosis (IPA)
- Pulmonary disease
7.1 Introduction
Aspergillus fungi of class Eurotiomycetes is the most frequently occurring fungi among this class. They are the inhabitants of humid soil. Amongst 250 species reported till date, Aspergillus fumigatus causes 90% of human infections. Although A. fumigatus is the chief infectious pathogen of human, other examples include A. lentulus, A. fumigatiaffinis, A. fumisynnematus and A. felis (Balajee and Marr 2006; Barrs et al. 2013). Its pathogenicity lies in the high sporulating capacity, and due to this very reason, the spore concentration ranging in the air increases from 1 to 100 (Streifel et al. 1983; Latgé 2001). These spores later release conidia in the air which are capable enough to reach the alveoli due to its minute diameter of 2–3 mm. The air laden with these spores when inhaled majorly affects lung. With these disease-causing properties of Aspergillus, it was found that it may result in severe pathological conditions like chronic obstructive pulmonary disease (COPD), allergic bronchopulmonary aspergillosis and aspergilloma (McNeil et al. 2001). The current chapter deals with the COPD and its association with Aspergillus infection.
According to the WHO and the National Heart, Lung, and Blood Institute, COPD is defined as a “disease state characterised by airflow limitation that is not fully reversible”. Similarly, a disease called IPA is indicated by the lung parenchyma invasion and necrosis due to Aspergillus spp. It is further divided into two classes on the basis of invasion: subacute IPA representing the direct invasion of lung parenchyma by hyphal elements but with a slowly progressively COPD cavitary lung disease and chronic pulmonary aspergillosis which shows radiological signs of tissue destruction, but without evidence of hyphal invasion, with microbiological markers of Aspergillus infection. The term tracheobronchitis is used when Aspergillus organisms invade the tracheobronchial tree. Recent data are obtained through studies performed by autopsy, and an exponential increase has been found over the last 20 years (Groll et al. 1996; Yamazaki et al. 1999; Kontoyiannis and Bodey 2002). To keep this in check, the medications include immunosuppressive and corticosteroid therapies. Due to the adverse effect of these drugs, mortality rate has been increased further (Warnock et al. 2001; Pegues et al. 2001). Later a few clinical studies have shown the association of IPA with that of COPD. Due to the IPA association, doctors prefer steroids above other treatments available. This treatment even worsens the condition of the patient (Rello et al. 1998; Bulpa et al. 2001; Dimopoulos et al. 2003; Meersseman et al. 2004; Ader et al. 2005; Garnacho-Montero et al. 2005). With the colonization of Aspergillus spp. in lung airways, possibility of IPA in COPD increases, and thus (Pepys et al. 1959; Yu et al. 1986) it becomes critical to detect it at an early stage. It is specific in severe (Global Initiative for Chronic Obstructive Lung Disease (GOLD)) steroid-dependent stage IV COPD patients. To come up with the better therapeutic targets for any of the disease, we need to focus firstly on the epidemiology of the disease along with the pathophysiology and symptoms commonly occurring in that disease. The underneath topics will deal with the epidemiology, pathophysiology and symptoms associated with the disease in detail.
The respective figure shows the pathophysiology and steps of spore invasion in human respiratory tract (Dagenais and Keller 2009)
7.2 Epidemiology
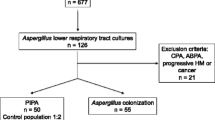
Although the occurrence of COPD in IPA patients is very less and poorly documented, it has been shown through various demographic data that patients with COPD are at greater risk of developing IPA. Assessment of the incidence of IPA in the population is difficult due to the lack of a consistent case, lack of a particular definition and lack of infection surveillance measures. Above all, the next problem lies in distinguishing the colonization of Aspergillus spp. with that of IPA, particularly at an early stage. However, there is growing evidence of data suggesting that COPD patients are at a greater risk of IPA. A review by Lin et al. (2001) of 50 patients shows that COPD was the underlying condition in 26 out of 1,941 (1.3%) patients with aspergillosis. In one large study conducted by Patterson et al. (2000a), 9% of 595 patients with invasive aspergillosis (IA) suffered from pulmonary disease, without a distinct pulmonary disorder. A study performed by Rodrigues et al. (1992) reported that COPD patients contribute to 1% of all cases of IPA in their institution. Steroidal drugs are shown to play a pivotal role in the emergence of IPA. Some authors have also investigated the correlation between the daily dose of corticosteroids and the probability of developing IA. It was suggested that the average dose of 1.25 mg/kg-1/day-1 of prednisone in renal transplant patients is the best method to develop a model for IPA (Gustafson et al. 1983). But the case was a bit different in the haematological patients treated with peripheral blood or bone marrow transplantation. In them, a dosage of 1 mg/kg-1/day-1 of prednisone for 21 days was enough to develop IPA (Grow et al. 2002). On summarising the data it was found that a dosage of 0.2 mg of prednisone per day or a cumulative dosage of 0.7 mg was associated with an increased risk of infections (Stuck et al. 1989). Various data provided by different authors support the patients undergoing corticotherapy for a longer duration of time are at a higher risk of developing COPD with IPA (Rello et al. 1998; Bulpa et al. 2001; Ader et al. 2005; Muquim et al. 2005). Despite the close association between steroids and IPA in COPD patients, it has been reported that some COPD patients may develop IPA without steroid exposure (Ali et al. 2003). Moreover, it has been reported that some infections, in particular viral infection, such as influenza (Urban et al. 1985; Bulpa et al. 1995) or cytomegalovirus (Warnock et al. 2001), may precede IPA, suggesting a role in causation (Ordronneau et al. 1987). Later, we will discuss the pathophysiology of the disease.
7.3 Pathophysiology
Aspergillus spp. is an airborne pathogen with a spore size of 2–3 mm in diameter. It is widely spread in the air, and when a person inhales spore-containing air, these penetrate through the airways to the lungs. Although the majority of conidia are excluded from the lungs by the ciliary action of the bronchial epithelium, some make their way through the respiratory tract to the lungs, hence leading to pathological conditions. In COPD patients, ciliary activity is impaired by tobacco smoke and multiple episodes of infection, as well as repeated epithelial damage. Thus, the impairment in defence mechanisms of the airways facilitates the binding of conidia to the epithelial layer (Latgé 2001). Stages of Aspergillus infection are depicted in the diagram below:
The phagocytic system is the next one in line to be affected (Shoham and Levitz 2005). It comprises the alveolar macrophages (AM) that play a prominent role in destroying the A. fumigatus conidia and the neutrophils that kill hyphae and germinating spores (Schaffner et al. 1982; Levitz 1992; Roilides et al. 1993; Balloy et al. 2005). Other immune cells such as natural killer lymphocytes (Morrison et al. 2003) and the innate pulmonary host defences also play a role in protecting individuals against IPA (Walsh et al. 2005; Feldmesser 2005) and thus the COPD.
Steps of germination and dissemination of fungal hyphae (Ben-Ami et al 2010)
7.4 Prevention of Infection
Due to difficulty in diagnosis associated with IPA, mortality rate is still high (up to 90%, depending on the underlying disease), thus making prevention of infection very important (Warnock et al. 2001). The avoidance of infections may be taken in the following ways:
-
To eliminate obvious environmental sources of Aspergillus spp.
-
Cleaning the surfaces to avoid dust accumulation. Moreover to prevent outbreaks, environmental protection by enriching solid barriers must be applied during construction (Patterson et al. 2000a, b).
-
Environmental protection by impenetrable barriers must be implemented during construction (Oren et al. 2001).
-
COPD patients should wear a high-efficiency mask or avoid exposure.
-
Prevention must be focused on the avoidance of high load sources, e.g., constructions, cellars or lofts, composts, etc.
-
IPA could also be a water-borne infection (Warris and Verweij 2005), and pillows may contain high loads of Aspergillus (Woodcock et al. 2006). Finally, if the patient is receiving corticosteroids, the dose should be decreased as much as possible or even stopped altogether.
-
The dose of corticosteroids should be kept in check or should be decreased or stopped if possible.
7.5 Prognosis
Therapy of COPD with a fungal infection includes voriconazole. It was considered to be the first-line treatment of the disease (Caillot et al. 2001). The study was conducted on the guinea pigs with a dosage of 10 mg/kg/day. To turn our target to a better treatment option, the focus was made on amphotericin B at 1 and 1.25 mg/kg/day, respectively (Maertens et al. 2002; Montoya et al. 2003). Another study concluded that the efficacy of high-dose liposomal amphotericin B (at 5 and 10 mg/kg) was superior to that of voriconazole (10 mg/kg) in a mouse model of pulmonary aspergillosis (Comstock et al. 1974). Apart from these two drugs with distinct doses, it became necessary to design a clinical trial with a better formulation.
Due to economic constraints, voriconazole is still the prescribed treatment than amphotericin. Properties of the drug are as follows:
-
Synthetic triazole.
-
Exerts an inhibitory effect on two kinds of Aspergillus by cytochrome P450-dependent enzymes and the fungal respiration chain.
-
Triazoles are generally considered as fungistatic.
-
The drugs given in association with voriconazole concentrations are erythromycin, indinavir, ranitidine, cimetidine and omeprazole. Drugs that potentially decrease voriconazole concentrations are principally rifampicin and phenytoin.
7.6 Symptoms
Symptoms of the disease are not clearly distinguishable as pulmonary disease shows some common features, but some of the key features include:
-
Fever and chills
-
A cough that brings up blood (hemoptysis)
-
Shortness of breath
-
Chest or joint pain
-
Headaches or eye symptoms
-
Skin lesions
7.7 Conclusion
The pulmonary diseases are attributed to airborne foreign particles. Spores of Aspergillus are found to be a newer target to cause a fatal disease like COPD. This chronic disease when not treated at an earlier stage may lead to the development of another asymptomatic condition called invasive pulmonary aspergillosis. The symptoms and diagnosis of these pathogenic conditions are less distinct, and hence it becomes a challenge to cure them at an earlier stage. Due to the continuous advancement of technology, we have achieved success at certain levels. Drugs like voriconazole have been developed which aid in the treatment of the disease. Thus from the above chapter we may conclude that the chronic pulmonary disease may arise due to fungal penetration in lungs.
References
Ader F, Nseir S, Le Berre R et al (2005) Invasive pulmonary aspergillosis in chronic obstructive pulmonary disease: an emerging fungal pathogen. Clin Microbiol Infect 11(6):427–429
Ali ZA, Ali AA, Tempest ME et al (2003) Invasive pulmonary aspergillosis complicating chronic obstructive pulmonary disease in an immunocompetent patient. J Postgrad Med 49(1):78–80
Balajee SA, Marr KA (2006) Phenotypic and genotypic identification of human pathogenic aspergilli. Future Microbiol 1(4):435–445
Balloy V, Huerre M, Latgé JP et al (2005) Differences in patterns of infection and inflammation for corticosteroid treatment and chemotherapy in experimental invasive pulmonary aspergillosis. Infect Immun 73(1):494–503
Barrs VR, van Doorn TM, Houbraken J et al (2013) Aspergillus felis sp. nov., an emerging agent of invasive aspergillosis in humans, cats, and dogs. PLoS One 8(6):e64871
Bulpa P, Dive A, Delos M et al (1995) Aspergillose pulmonaire invasive et infection à virus influenza chez des patients bronchitiques chroniques? [Invasive pulmonary aspergillosis and influenza virus infection in patients with chronic bronchitis?]. Rev Pneumol Clin 51(5):300–301
Bulpa PA, Dive AM, Garrino MG et al (2001) Chronic obstructive pulmonary disease patients with invasive pulmonary aspergillosis: benefits of intensive care? Intensive Care Med 27(1):59–57
Caillot D, Mannone L, Cuisenier B et al (2001) Role of early diagnosis and aggressive surgery in the management of invasive pulmonary aspergillosis in neutropenic patients. Clin Microbiol Infect 7(2):54–61
Comstock GW, Palmer CE, Stone RW et al (1974) Fungi in the sputum of normal men. Mycopathol Mycol Appl 54(1):55–62
Dagenais TR, Keller NP (2009) Pathogenesis of Aspergillus fumigatus in Invasive Aspergillosis. Clin Microbiol Rev. 22(3):447–465. https://doi.org/10.1128/CMR.00055-08
Dimopoulos G, Piagnerelli M, Berré J et al (2003) Disseminated aspergillosis in intensive care unit patients: an autopsy study. J Chemother 15(1):71–75
Feldmesser M (2005) Prospects of vaccines for invasive aspergillosis. Med Mycol 43(7):571–587
Garnacho-Montero J, Amaya-Villar R, Ortiz-Leyba C et al (2005) Isolation of Aspergillus spp. From the respiratory tract in critically ill patients: risk factors, clinical presentation and outcome. Crit Care 9(3):R191–R199
Groll AH, Shah PM, Mentzel C et al (1996) Trends in the postmortem epidemiology of invasive fungal infections at a University Hospital. J Infect 33(1):23–32
Grow WB, Moreb JS, Roque D et al (2002) Infections post-transplant. Late onset of invasive Aspergillus infection in bone marrow transplant patients at a university hospital. Bone Marrow Transplant 29(1):15–19
Gustafson TL, Schaffner W, Lavely GB et al (1983) Invasive aspergillosis in renal transplant recipients: correlation with corticosteroid therapy. J Infect Dis 148(2):230–238
Kontoyiannis DP, Bodey GP (2002) Invasive aspergillosis in 2002: an update. Eur J Clin Microbiol Infect Dis 21(3):161–172
Latgé JP (2001) The pathobiology of Aspergillus fumigatus. Trends Microbiol 9(8):382–389
Levitz SM (1992) Overview of host defences in fungal infections. Clin Infect Dis 14(1):S37–S42
Lin SJ, Schranz J, Teutsch SM (2001) Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis 32(3):358–366
Maertens J, Van Eldere J, Verhaegen J et al (2002) Use of circulating galactomannan screening for early diagnosis of invasive aspergillosis in allogeneic stem cell transplant recipients. J Infect Dis 186(9):1297–1306
McNeil MM, Nash SL, Hajjeh RA et al (2001) Trends in mortality due to invasive mycotic diseases in the United States, 1980–1997. Clin Infect Dis 33(5):641–647
Meersseman W, Vandecasteele SJ, Wilmer A et al (2004) Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med 170(6):621–625
Montoya JG, Chaparro SV, Celis D et al (2003) Invasive aspergillosis in the setting of cardiac transplantation. Clin Infect Dis 37(3):S281–S292
Morrison BE, Park SJ, Mooney JM et al (2003) Chemokine-mediated recruitment of NK cells is a critical host defense mechanism in invasive aspergillosis. J Clin Invest 112(12):1862–1870
Muquim A, Dial S, Menzies D (2005) Invasive aspergillosis in patients with chronic obstructive pulmonary diseases. Can Respir J 12(4):199–204
Ordronneau J, de Lajartre AY, Chollet S et al (1987) Aspergillose invasive disséminée associée à une infection à mycoplasma pneumoniae. [Disseminated invasive aspergillosis associated with Mycoplasma pneumoniae infection]. Rev Mal Resp 4(5):273–275
Oren I, Haddad N, Finkelstein R et al (2001) Invasive pulmonary aspergillosis in neutropenic patients during hospital construction: before and after chemoprophylaxis and institution of HEPA filters. Am J Hematol 66(4):257–262
Patterson TF, Kirkpatrick WR, White M et al (2000a) Invasive aspergillosis: disease spectrum, treatment practices and outcomes. Medicine 79(4):250–260
Patterson JE, Peters J, Calhoon JH et al (2000b) Investigation and control of aspergillosis and other filamentous fungal infections in solid organ transplant recipients. Transpl Infect Dis 2(1):22–28
Pegues CF, Daar ES, Murthy AR (2001) The epidemiology of invasive pulmonary aspergillosis at a large teaching hospital. Infect Control Hosp Epidemiol 22(6):370–374
Pepys J, Riddell RW, Citron KM et al (1959) Clinical and immunologic significance of Aspergillus fumigatus in the sputum. Am Rev Respir Dis 80:167–180
Rello J, Esandi ME, Mariscal D et al (1998) Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: report of eight cases and review. Clin Infect Dis 26(6):1473–1475
Rodrigues J, Niederman MS, Fein AM et al (1992) Nonresolving pneumonia in steroid-treated patients with obstructive lung disease. Am J Med 93(1):29–34
Roilides E, Uhlig K, Venzon D et al (1993) Prevention of corticosteroid-induced suppression of human polymorphonuclear leukocyte-induced damage of Aspergillus fumigatus hyphae by granulocyte colony stimulating factor and gamma interferon. Infect Immun 61(11):4870–4877
Ben-Ami R, Lewis RE, Dimitrios P (2010) Kontoyiannis. Enemy of the (immunosuppressed) state: an update on the pathogenesis of Aspergillus fumigatus infection. Br J Haematol. 150(4):406–417. https://doi.org/10.1111/j.1365-2141.2010.08283.x
Schaffner A, Douglas H, Braude A (1982) Selective protection against Conidia by mononuclear and against Mycelia by polymorphonuclear phagocytes in resistance to Aspergillus. J Clin Invest 69(3):617–631
Shoham S, Levitz S (2005) The immune response to fungal infections. Br J Haematol 129(5):569–582
Streifel AJ, Lauer JL, Vesley D et al (1983) Aspergillus fumigatus and other thermos tolerant fungi generated by hospital building demolition. Appl Environ Microbiol 46(2):375–378
Stuck AE, Minder CE, Frey FJ (1989) Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis 11(6):954–963
Urban P, Chevrolet JC, Schifferli J et al (1985) Aspergillose pulmonaire invasive associée à une infection aiguë à virus influenza. [Invasive pulmonary aspergillosis associated with an acute influenza virus infection]. Rev Mal Resp 2(4):255–257
Walsh TJ, Roilides E, Cortez K et al (2005) Control, immunoregulation, and expression of innate pulmonary host defenses against Aspergillus fumigatus. Med Mycol 43(1):S165–S172
Warnock DW, Hajjeh RA, Lasker BA (2001) Epidemiology and prevention of invasive aspergillosis. Curr Infect Dis Rep 3(6):507–516
Warris A, Verweij PE (2005) Clinical implications of environmental sources for Aspergillus. Med Mycol 43(1):S59–S65
Woodcock A, Steel N, Moore C et al (2006) Fungal contamination of bedding. Allergy 61(1):140–142
Yamazaki T, Kume H, Murase S et al (1999) Epidemiology of visceral mycoses: analysis of data in Annual of the Pathological Autopsy Cases in Japan. J Clin Microbiol 37(6):1732–1738
Yu VL, Muder RR, Poorsattar A (1986) Significance of isolation of Aspergillus from the respiratory tract in diagnosis of invasive pulmonary aspergillosis. Results from a three-year prospective study. Am J Med 81(2):249–254
Acknowledgement
Dr. Suchit Swaroop acknowledges the Experimental and Public Health Laboratory, Department of Zoology, University of Lucknow, for providing the facilities and space to conduct the study.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kumar, S., Swaroop, S. (2019). Collateral Development of Invasive Pulmonary Aspergillosis (IPA) in Chronic Obstructive Pulmonary Disease (COPD) Patients. In: Gupta, A., Singh, N. (eds) Recent Developments in Fungal Diseases of Laboratory Animals. Fungal Biology. Springer, Cham. https://doi.org/10.1007/978-3-030-18586-2_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-18586-2_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-18585-5
Online ISBN: 978-3-030-18586-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)