Abstract
The identification of sensitizing mutations in the epidermal growth factor receptor (EGFR) gene in patients with non-small cell lung cancer (NSCLC) and the development of EGFR-tyrosine kinase inhibitors (EGFR TKIs) to target these mutations have dramatically improved outcomes for this subset of patients. For patients with EGFR-mutated NSCLC, the use of EGFR TKIs is associated with improved efficacy and quality of life compared to chemotherapy. The latest generation EGFR TKI, osimertinib, is highly effective in treating acquired resistance due to the T790M mutation as well as treating central nervous system metastases. As first-line treatment, its use has led to the longest median progression-free survival to date for patients with EGFR-mutated NSCLC. Acquired resistance to osimertinib is caused by multiple mechanisms, and numerous trials are currently underway to address this. Future studies should also aim to address the historically refractory EGFR exon 20 insertions, and current agents under study are promising.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Epidermal growth factor receptor (EGFR) mutation
- Tyrosine kinase inhibitor (TKI)
- Exon 20 insertions
- T790M
- Osimertinib resistance
Background
Somatic activating mutations in the epidermal growth factor receptor (EGFR) gene are the most common targetable molecular alteration in non-small cell lung cancer (NSCLC) [1]. EGFR mutations are predominantly found in adenocarcinoma, never smokers, and those of East Asian descent [2, 3]. In the United States and Europe, 10–17% of patients with NSCLC harbor an EGFR mutation, and in East Asia the frequency is 35–38% [4,5,6,7,8]. Identifying these mutations is of critical clinical importance given the highly active treatment options available for this subset of patients.
Since the discovery of epidermal growth factor (EGF) in 1962 by Stephen Cohen, and the characterization of its cell surface receptor (now known as EGFR) in 1975, extensive studies of the receptor and its family have led to revolutionary insights into the fields of growth factor and cancer biology [9,10,11]. EGFR was one of the first receptor tyrosine kinases (RTK) for which ligand-dependent dimerization was proposed as the mechanism of RTK activity [12]. It was also the first cell surface receptor to be proposed as a target for cancer therapy [13] and the first receptor to have a monoclonal antibody directed against it to inhibit cancer growth [14, 15].
EGFR (HER1, ErbB1) is an RTK expressed on the surface of cells of mesodermal and ectodermal origin, and it mediates cell growth, proliferation, and differentiation in numerous organs [16, 17]. EGFR belongs to the ErbB family of RTKs, which also includes HER2 (ErbB2), HER3 (ErbB3), and HER4 (ErbB4). EGFR binds at least seven highly variable growth factor ligands [18]. Upon stimulation, EGFR undergoes combinatorial homo- or hetero-dimerization with one of the proteins of the HER family, thereby activating an expansive signaling network [16, 19, 20]. The EGFR transmembrane protein has a large extracellular component (with 4 domains, ~620 amino acids) that primarily serves as ligand-binding sites and which is anchored by a short helical transmembrane domain to the intracellular tyrosine kinase domain (TKD) (Fig. 1) [18].
Schematic representation of the epidermal growth factor receptor (EGFR) and its position on the cellular membrane. The extracellular component consists of four large domains which contain ligand-binding sites for growth factors including epidermal growth factor (EGF). The intracellular component consists of the tyrosine kinase domain followed by the regulatory domain. EGFR tyrosine kinase inhibitors (TKIs) and ATP compete for binding to the phosphate-binding (P) loop. Exon 20 contains two critical features, the alpha-C helix followed by a distal A loop. “ATP” = adenosine triphosphate. “PD” = Progression of disease
EGFR is believed to play a role in the pathogenesis of lung cancer and is overexpressed in a majority of NSCLCs [21, 22]. However, the clinical importance of EGFR expression in the general NSCLC population is unclear. There was some suggestion that EGFR expression may serve as a predictive biomarker [21], but this has been superseded by mutational analysis after the identification of actionable driver mutations in the EGFR gene.
The EGFR gene is located on chromosomal region 7p11.2 [23]. EGFR-mutated NSCLC is driven by “activating” gain-of-function mutations which cluster around the ATP-binding pocket of the TKD and lead to constituent, ligand-independent activation of the EGFR receptor. This in turn promotes prosurvival and antiapoptotic signals such as phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT) and extracellular signal-regulated kinase (ERK)/mitogen-activated protein kinase (MAPK) [24]. Approximately 85–90% of activating mutations are either exon 19 in-frame deletions affecting amino acids 747–750 (40–45%) or the point mutation L858R in exon 21 [7, 8, 24, 25]. These mutations are associated with hypersensitivity to small molecule tyrosine kinase inhibitors (TKIs) and are thus termed “sensitizing” EGFR mutations, with the exon 19 deletion consistently associated with better survival outcomes with therapy [26,27,28,29,30]. The remaining 10–15% involve exons 18, 20, and 21. Many, but not all, of these mutations have been found to be sensitive to targeted therapy.
First-Generation TKIs and Early Trials in Lung Cancer
EGFR TKIs entered clinical development in late 1990s. First-generation inhibitors , erlotinib, gefitinib, and icotinib [31] bind competitively and reversibly to the ATP-binding site (Fig. 1), preventing autophosphorylation and downstream signaling, thereby preventing EGFR-dependent cell proliferation [32,33,34]. In 2003, two single-arm phase II trials (IDEAL1 and IDEAL2) demonstrated clinical efficacy of gefitinib in patients with previously treated NSCLC, with response rates of approximately 15% [35, 36]. Of note, more responses were observed in women, patients with adenocarcinoma, never smokers, and those of Asian descent. This compared favorably to chemotherapy , which had an approximately 5% response rate in this population [36]. In 2003, gefitinib became the first US Food and Drug Administration (FDA) approved EGFR TKI for NSCLC.
Soon after, the double-blind placebo-controlled randomized phase III trial (ISEL) failed to find overall survival benefit for gefitinib with best supportive care (BSC) compared to placebo with BSC in unselected NSCLC patients [37]. Considering these results as well as those form IBREESE (gefitinib with BSC vs placebo with BSC), which terminated early and INTEREST (non-inferiority trial of gefitinib vs docetaxel), the FDA withdrew its original approval for gefitinib in 2005 [38, 39]. However, there were already clues to a yet unidentified subset of responders in the trial because the Kaplan-Meier survival curves crossed. There was an early drop off in non-responders, and a clear separation of survival curves at approximately four months. Several follow-up trials evaluated the benefit of adding an EGFR TKI to standard first-line chemotherapy. At least four large randomized controlled trials in unselected, advanced NSCLC patients showed no benefit of the addition of EGFR TKI to standard chemotherapy [40,41,42,43]. Once again, these trials were conducted in an unselected group of patients.
The publication of two landmark analyses in 2004 by Lynch et al. and Paez et al. demonstrated that the subset of patients who responded to gefitinib harbored activating EGFR mutations (namely, L858R and exon 19 deletions) [7, 8]. This led to a paradigm shift for future trial development, and the history of EGFR TKI clinical trials should be interpreted by differentiating the era of unselected patient enrollment versus the era incorporating EGFR mutation testing. The trial that ushered in this modern era and transformed targeted therapy for NSCLC is the IPASS trial.
EGFR TKIs for Patients with Mutations in EGFR
For the first time, the 2009 IPASS trial prospectively demonstrated in a randomized controlled trial that EGFR TKIs were superior to chemotherapy as first-line therapy for patients with EGFR mutations [44]. The biomarker analysis was a preplanned subset analysis of 40% of the 683 randomly assigned patients for whom EGFR mutation status could be evaluated, and found an objective response rate (ORR) of 71% and a PFS of 9.5 months for the gefitinib arm compared to 6.3 months for the chemotherapy arm (Table 1) [45]. Over the next half decade, several large trials would be undertaken to look at the efficacy of EGFR TKI vs chemotherapy (Table 1). IFUM fulfilled the European Medicines Agency (EMA) requirement for a single-arm validation trial in Caucasians, confirming the efficacy of gefitinib in Caucasian patients with sensitizing EGFR mutations [46]. On July 13, 2015, gefitinib was approved for first-line treatment of patients with metastatic NSCLC with exon 19 deletions or L858R mutations. Erlotinib and gefitinib have both been approved and marketed in numerous countries, whereas icotinib has been approved and widely prescribed only in China [47].
Individual trials and meta-analyses have consistently found that EGFR TKIs prolong PFS compared to chemotherapy in patients with EGFR-mutated NSCLC; however, until recently, trials have not shown an improvement in OS [48,49,50]. With good consistency across trials of erlotinib or gefitinib versus chemotherapy, the median PFS is estimated as 11.0 months vs 5.6 months for chemotherapy (HR 0.37, P < 0.001) [51]. Randomized phase III trials comparing erlotinib to gefitinib for EGFR-mutated NSCLC patients have demonstrated similar efficacy of both [52, 53]. As front-line therapy in patients with EGFR-mutated disease, the TKI response rate is 67%, as compared to 30% for chemotherapy (RR 5.68, P < 0.001) [50]. The lack of OS benefit has been ascribed to crossover from the chemotherapy arm to an appropriate TKI, within or outside of the clinical trial [51, 54, 55]. Even without the OS benefit, first-line TKI has been the preferred treatment option for EGFR-mutated NSCLC due to the ease of an oral therapy, the higher response rate, and an improved quality of life (QOL) [51, 56, 57].
Despite an average of nearly a year of PFS with an EGFR TKI, it was seen that nearly all patients would eventually progress. At the time of progression, continuing gefitinib into subsequent lines of therapy was shown to be detrimental. In the phase III IMPRESS trial, chemotherapy-naïve EGFR-mutated patients who progressed on first-line gefitinib were randomized to receive either cisplatin and pemetrexed versus the same chemotherapy plus gefitinib [58]. The study found that continuing gefitinib had a detrimental effect on survival with an OS of 13.4 months compared to 19.5 months for the chemotherapy arm (HR = 1.44, P = 0.016) [59]. Data from IMPRESS warns that continuing an EGFR TKI at progression may cause harm, and interestingly, this detriment was associated with a specific secondary mutation, T790M (HR 1.49, P = 0.043 for T790M+ patients vs HR 1.15, P = 0.609 in T790M- patients) [58, 59].
Second-Generation TKIs
The second-generation inhibitors, afatinib and dacomitinib, were introduced as a treatment for those who progressed on a prior generation TKI. Unlike the first-generation inhibitors, the second-generation EGFR TKIs bind covalently and irreversibly [60]. These drugs also tend to have less selective activity, inhibiting other HER family proteins including HER2. Preclinical data of second-generation TKIs was promising, demonstrating potent activity in lung cancer models resistant to first-generation inhibitors [60,61,62,63]. The phase IIb/III trial, LUX-Lung 1, randomized patients who had progressive disease after at least three months of treatment on erlotinib or gefitinib to either afatinib or placebo [64]. There was no overall survival benefit (HR 1.08, P = 0.74), the ORR on afatinib was 7%, and the PFS was 3.3 months vs 1.1 months (HR 0.38, P < 0.0001). The phase II trial of dacomitinib in patients who progressed on chemotherapy and an EGFR TKI was similarly sobering, with an ORR of only 5.2% [65].
Both afatinib and dacomitinib were associated with significant on-target toxicity, primarily rash and diarrhea [64, 65]. Pooled analysis from 21 trials of 1468 patients found statistically higher grade 3 or greater rash with afatinib than with erlotinib or gefitinib (15% vs 8.8% vs 3.5%, respectively) [66]. Grade 3 or higher diarrhea was also more frequent in patients on afatinib than in those on erlotinib or gefitinib (9.6% vs 2.7% vs 1.1%, respectively; odds ratio 3.80 for afatinib vs erlotinib, P < 0.0001). More patients discontinued treatment because of an adverse event (AE) on afatinib than erlotinib (7.2% vs 4.1%, P = 0.040), but discontinuation rates were similar for afatinib and gefitinib (7.2% vs 7.6%). The treatment interruption rate in trials due to an AE did not vary significantly between afatinib and gefitinib or erlotinib and ranged from 11% to 28% [67]. However, more patients on afatinib required dose reductions. Across trials, discontinuation rates on gefitinib or erlotinib ranged from 6% to 21% (IPASS, OPTIMAL, and EURTAC) [68] as compared to 28.0–53.5% on afatinib (LUX-Lung 3 and LUX-Lung 6) [69]. In the head-to-head phase II trial LUX-Lung 7 randomizing patients to afatinib or gefitinib, 42% of patients required a dose reduction on afatinib, as compared to only 2% with gefitinib [70].
Other trials investigated the possible benefit from a second-generation TKI for front-line therapy. The PFS benefit of afatinib over platinum doublet chemotherapy in the LUX-Lung 3 and LUX-Lung 6 randomized phase III trials (Table 1) is similar to that seen with erlotinib or gefitinib (approximately 11 vs 6 months) [71, 72]. Although there was no OS advantage in the overall population of either trial, preplanned subgroup analyses in both trials found an OS advantage of the TKI over chemotherapy in patients with an exon 19 deletion [27]. The OS benefit is noteworthy given the lack of OS benefit with TKIs in prior studies.
Two large head-to-head trials have compared second-generation to first-generation TKIs. In LUX-Lung 7, patients with EGFR-mutated NSCLC were randomized to afatinib or gefitinib. The trial failed to find an OS improvement, and reported a statistically significant PFS benefit with a difference in the medians of a meager three days (HR 0.74, P = 0.0178) [73]. On the other hand, ARCHER 1050, the phase III randomized controlled trial of dacomitinib versus gefitinib as first-line treatment for patients with activating EGFR mutations, showed a PFS improvement of 14.7 vs 9.2 months (HR 0.59, P < 0.0001) [74]. More strikingly, there was a significant OS advantage for the dacomitinib arm (34.1 vs 26.8 months, HR 0.76, P = 0.044) [75]. This is the first head-to-head randomized trial of two TKIs to show an OS advantage. Of note, patients with central nervous system (CNS) metastases and rare EGFR mutations were excluded from the trial. In addition, there was significantly higher toxicity, with 51% of subjects experiencing a grade 3 adverse event in the dacomitinib arm (most commonly rash or diarrhea) compared to 30% in the gefitinib arm [74]. Given these factors, the clinical utility of dacomitinib has been questioned, but remains an option. In 2018, dacomitinib was approved by the FDA for the first-line treatment of patients with NSCLC harboring an EGFR exon 19 deletion or L858R mutation [76]. With the recent arrival of the third-generation TKIs, some have said that the second generation has been altogether bypassed, referring to it as the “lost generation” [77, 78].
T790M Mutation
Despite the dramatic responses seen in patients with activating EGFR mutations on first- and second-generation EGFR TKIs, unfortunately nearly all patients will eventually develop resistant and progressive cancer. Initial insights into the mechanism of resistance came from analysis of tumor biopsies from a patient who relapsed after two years of complete remission on an EGFR TKI [79]. Tumor DNA sequencing before treatment and at the time of relapse revealed the acquisition of a second mutation, T790M in exon 20, which replaces threonine with methionine at position 790. Here, threonine is a “gatekeeper” amino acid because it lies at the entrance to a hydrophobic pocket in the ATP-binding cleft of the EGFR protein, critically determining the specificity of inhibitors.
Initial crystallographic evidence suggested that incorporation of the bulkier methionine side chain sterically hindered the interaction of the first- and second-generation EGFR TKIs [79]. Subsequent analysis showed that the effect was mediated by two factors; not only did methionine block drug binding, it also caused increased ATP affinity at the binding pocket, thereby outcompeting the therapeutic drug [80]. Although second-generation TKIs bind more avidly and irreversibly, and can inhibit T790M-positive clones in vitro, the necessary drug concentrations were not clinically achievable due to skin and gastrointestinal toxicity [81]. In patients treated with first- and second-generation inhibitors, the T790M resistance mutation is detected in approximately 50–60% of patients at the time of progression [82,83,84]. T790M has generally been associated with a slower rate of growth and an improved prognosis. In a retrospective analysis of 97 patients treated with EGFR TKIs, the PFS was 12.0 months on initial TKI in those who acquired the T790M mutation, as compared to 9.0 months for those who were T790M-negative (P = 0.021) [85].
Third-Generation TKIs
Understanding this mechanism of acquired resistance led to the development of third-generation EGFR TKIs. These include rociletinib [86, 87], olmutinib [88], nazartinib [89], avitinib [90], ASP8273 [91], PF-06747775 [92], and osimertinib (AZD9291), the only third-generation EGFR TKI approved for clinical use. Osimertinib is active against exon 19 deletions, exon 21 mutations, and also the exon 20 T790M mutations. It is preferentially selective for mutated EGFR, and therefore toxicity at therapeutic doses is lower than for first- and second-generation agents. Notably, osimertinib is able to cross the blood-brain barrier, making it active against disease in the CNS [93].
The safety and tolerability of osimertinib was studied in the phase I trial, AURA. Among 253 patients there were no dose-limiting toxicities observed across all dose levels (20–240 mg) [94]. The most common adverse event was diarrhea (47%), followed by rash, nausea, and decreased appetite. Only 6% of patients discontinued treatment because of a treatment-related adverse event. The phase II AURA extension and AURA2 trial both demonstrated similar tolerability [94]. In the phase III trial (AURA3), grade 3 or higher adverse events occurred in 23% of patients, half of what was experienced in the chemotherapy arm (47%) [95]. Osimertinib toxicity is dose-dependent and is associated with fewer gastrointestinal and dermatologic adverse events than with other approved EGFR TKIs.
The phase III trial of osimertinib (AURA3) randomly assigned 419 patients with advanced T790M-positive NSCLC who had progressed on prior EGFR TKIs to receive either osimertinib or chemotherapy with a platinum agent and pemetrexed [95]. Osimertinib more than doubled PFS when compared to chemotherapy (10.1 vs 4.4 months, HR of 0.30 P < 0.001) with an unprecedented response rate of 71% in this resistant population [95]. This led to the FDA granting approval of osimertinib for NSCLC after progression on a prior EGFR TKI with the demonstration of the T790M mutation [96]. Additional data from the United Kingdom confirmed the cost-effectiveness of osimertinib over chemotherapy for this patient population [97].
Even during the initial phase I AURA trial, osimertinib was studied as a potential first-line treatment [98]. In a double-blind randomized controlled trial of untreated EGFR-mutated NSCLC patients (FLAURA), the use of osimertinib led to a median PFS of 18.9 months compared to 10.3 months for those treated with first-generation EGFR TKIs, erlotinib or gefitinib. The HR for PD or death was 0.46 (P < 0.001), and the benefit of osimertinib over the first-generation EGFR TKI persisted in all subgroup analyses [99]. Patients on osimertinib reported fewer grade 3 or higher adverse events than those on erlotinib or gefitinib (34% vs 45%), and fewer patients experienced rashes (58% vs 78% on erlotinib or gefitinib). On April 18, 2018, the FDA approved osimertinib as first-line therapy for patients with metastatic NSCLC harboring a driver EGFR mutation [100]. At the time of publication of the FLAURA dataset, only 18-month OS was available, reported as 83% for the osimertinib arm compared to 71% for first-generation TKIs (HR = 0.63, P = 0.007). It remains to be seen if this will result in a significant long-term OS advantage.
Liquid Biopsy to Detect Mutations in EGFR
Detection of EGFR mutations such as T790M is critical to precision treatment for patients with NSCLC in the era of targeted therapy. “Liquid biopsy ” is the method of detecting molecular alterations in circulating tumor DNA (ctDNA) or other nucleic acids from blood or other body fluids. Lack of available tissue for molecular profiling [38, 44, 101,102,103], risk of biopsy complications [104], significant delay with tissue biopsy [105], and increased cost of biopsy [106], all lead to potential advantages of liquid biopsy. More so, single-site tissue biopsies may not represent the predominant resistance mechanisms in a patient and may miss the emergence of a clinically significant clone [107, 108]. This is due to the marked tumor heterogeneity that has been seen in NSCLC [28, 109,110,111,112].
Next-generation sequencing has led to methods which allow ultra-deep sequencing for detection of actionable mutations in EGFR [113], de novo resistance mutations [114], and the emergence of acquired resistance during treatment [108, 115, 116]. In January 2015, the EMA approved the use of the therascreen liquid biopsy assay for detection of EGFR mutations in patients for whom tissue biopsy is not possible. In June 2016, the Cobas EGFR mutation test v2 was approved by the FDA to detect exon 19 deletions and the L858R mutation in plasma, and was extended in September 2016 to cover the T790M resistance mutation as well.
Prospective studies have demonstrated that plasma T790M can predict responders to osimertinib or rociletinib as well as tissue biopsy [113, 117, 118], and even detection of very low allele fractions of T790M in ctDNA may be clinically relevant [113]. Given the advantages over tissue biopsy, liquid biopsy can be considered one of the standard options for detecting acquired resistance mutations [108].
Patients with Brain Metastases
Patients with EGFR-mutated NSCLC have a higher risk for developing brain metastasis [119,120,121]. Historically, whole brain radiation therapy (WBRT) and stereotactic radiosurgery (SRS) have been the standard of care treatment for NSCLC patients with brain metastases. In the era prior to osimertinib use, the median OS after radiotherapy for patients with brain metastases was approximately 14 months [122]. Data regarding the efficacy of EGFR TKI for NSCLC with previously untreated brain metastases is limited since most trials have required prior radiation treatment of brain lesions [123].
A retrospective multi-institutional analysis studied 351 patients with EGFR TKI-naive EGFR-mutant NSCLC who developed brain metastases. Patients either received SRS followed by EGFR TKI, WBRT followed by EGFR TKI, or upfront EGFR TKI followed by SRS or WBRT as needed. The OS for the upfront SRS, WBRT, and EGFR TKI cohorts was 46, 30, and 25 months, respectively (P < 0.001) [124]. SRS does appear to be a valid option for front-line therapy; however, this approach may vary in the era of osimertinib, which has high efficacy against CNS disease.
In light of cognitive decline and radiation necrosis associated with brain radiation, the use of upfront radiotherapy has been questioned with the availability of osimertinib. In the BLOOM trial, 32 patients who had progressed on prior EGFR TKI therapy and had positive cerebrospinal fluid demonstrating leptomeningeal metastases were treated with 160 mg osimertinib daily [125]. Of 8 patients with neurologic symptoms, 7 had improvement, and one had stable disease. Out of 15 asymptomatic patients, 87% remained asymptomatic. In patients with parenchymal brain metastases, the intracranial ORR was 63% [126].
Although the BLOOM study used a 160 mg dose of osimertinib, both preclinical and clinical data suggest that low-dose osimertinib may have meaningful CNS activity as well [81, 94]. Of 144 patients in AURA3 with CNS metastases, the median PFS was twice as long in the osimertinib cohort vs the chemotherapy cohort (8.5 vs 4.2 months, HR 0.32, CI 0.21–0.49) with an overall response rate of 70% vs 31% (P = 0.015) [93, 95]. In the 116 patients with brain metastases in FLAURA, the median PFS was 15.2 with osimertinib compared to 9.6 months with erlotinib or gefitinib (HR 0.47, P = 0.0009). Osimertinib’s efficacy for brain metastasis and leptomeningeal disease, one of the poorest prognostic groups of NSCLC, further solidifies its role in the treatment of EGFR-mutated disease. At this point, there is no clear consensus on whether osimertinib alone should be used upfront for brain metastases or whether WBRT or SRS should be incorporated into the treatment regimen, although many defer WBRT if possible. Further prospective studies are required for these clinically important questions.
Special Populations: Elderly or Poor Performance Status
Since no trials have exclusively enrolled elderly patients, most data is retrospective. One study from 20 centers (OCTOMUT) looked at patients aged 80 or older treated with front-line EGFR TKIs and found that the clinical outcomes and toxicity profile were comparable to those published in the literature [127]. A large retrospective analysis of Japanese patients in the phase IV POLARSTAR study of erlotinib in previously treated NSCLC patients included 7848 patients less than 75 years old, 1911 patients aged 75–84, and 148 patients 85 years or older. It found non-inferior tolerability and efficacy of erlotinib in elderly patients [128]. A meta-analysis actually suggests that EGFR TKIs may have more PFS benefit in elderly patients (HR 0.39, P = 0.008) than in younger patients (HR 0.48, P = 0.04) [129]. A pooled analysis of NEJ001, NEJ002, and NEJ003 studying first-line gefitinib found that in patients >70 with a good performance status (PS) the median PFS was 14.3 compared to 5.7 months with chemotherapy (P < 0.001) [130].
Studies have consistently demonstrated that EGFR TKIs are better tolerated than chemotherapy, although the vast majority of these trials only enrolled patients with an Eastern Cooperative Oncology Group (ECOG) PS of 0 to 2. A single-arm phase II trial of 72 patients with untreated advanced NSCLC and poor PS (2 or 3) found that with gefitinib, 82% reported improvement or no worsening in QOL [131]. The double-blind, placebo-controlled, phase III TOPICAL trial randomized patients with advanced NSCLC deemed unsuitable for chemotherapy because of an ECOG PS >2 or several comorbidities with an estimated life expectancy of at least 8 weeks to erlotinib or placebo. Other than the incidence of rash and diarrhea, adverse events were similar in the two groups, and they concluded that erlotinib could be an option for those for whom chemotherapy is deemed unsuitable [132]. Patients on erlotinib had significantly improved QOL for a cognitive scale (P = 0.0072) and physical functioning (P = 0.0024) as well as statistically significant improvements in pain, dyspnea, chest pain, hoarseness, and constipation. If only patients with an EGFR mutation were enrolled, it would be expected that the benefit would be even more apparent. EGFR TKIs remain a good option for patients with an EGFR mutation and poor performance status.
Exon 20 Insertions and Other Rare EGFR Mutations
In contrast to sensitizing mutations such as exon 19 deletion and the L858R substitution, in-frame insertions within exon 20 of EGFR have been associated with resistance to EGFR TKIs, with response rates <5% to available EGFR TKIs, including the third-generation EGFR TKIs [25, 133,134,135,136]. Exon 20 insertions are the third most common type of EGFR mutation and account for 4–9% of EGFR mutations in NSCLC patients [25, 135, 137]. This is a heterogeneous group of about 44 mutations which vary in position and size [137], and three-dimensional structural modeling predicts variable effects on EGFR TKI binding [135]. EGFR exon 20 contains an alpha-C helix followed by a loop (Fig. 1). The conformation of the alpha-C helix and the P-loop is altered by exon 20 insertions, leading to steric hindrance and a confined binding pocket [138]. The most deleterious “hot spot” mutations tend to occur distal to the C helix, and represent 80–90% of exon 20 insertions [25, 135].
Few therapies have shown efficacy for patients with EGFR exon 20 insertions. The second-generation heat shock protein 90 (HSP90) inhibitors (e.g., ganetespib and luminespib) have had limited success in patients with NSCLC [139,140,141,142,143]. However, luminespib may have clinical activity in patients with exon 20 insertions [144, 145], with a median PFS of 6.1 months in one single arm phase II trial [146], but is associated with ocular toxicity.
Poziotinib is a TKI that covalently and irreversibly inhibits EGFR and HER2, and is unique because of its small terminal group and flexible quinazoline core. Its small size and flexibility allow it to evade the steric hindrance which affects other EGFR TKIs [138]. In a phase II trial of poziotinib, in patients with NSCLC harboring an EGFR exon 20 insertion, the ORR at 8 weeks was 58%, and the confirmed ORR at the time of the most recent interim analysis was 38% [147]. The median PFS was 5.6 months. Notably, this was a heavily pretreated group of patients, and the ORR was 62% among those who were previously treated with an EGFR TKI. A multicenter phase II trial of poziotinib is ongoing. Another TKI, AP32788 (TAK-788), was tested in a phase I/II trial of patients with an EGFR mutation. Out of 14 evaluable patients, the 9 patients (64%) who achieved a PR or had SD also had an exon 20 insertion [148], demonstrating promising clinical activity for this subset of patients. Poziotinib and AP32788 may represent important future drug options for EGFR exon 20 mutation-positive patients.
The incorporation of next-generation sequencing technologies has aided in the characterization of rare mutations in EGFR. G719X, deletion 18, and E709X are found in 3.1%, 0.3%, and 0.3% of patients with lung cancer (X connotes one of several possible amino acids). The G719X mutations can be found in combination with S768I and L861Q mutations which account for 1.1% and 0.9% of cases, respectively [137]. In an analysis of 32 patients with metastatic NSCLC with the uncommon EGFR mutations S68I, L861Q, and/or G719X (originally enrolled in LUX-Lung 2, LUX-Lung 3, and LUX-Lung 6), the ORR by independent radiology review was 66%. Among the 21 responders, 52% responded for a year or longer [149, 150]. This led to the FDA expanding its approval of afatinib to cover these uncommon non-resistant EGFR mutations in January 2018. There is some preclinical data suggesting osimertinib activity for some of these mutations, as well [137]. There are a range of EGFR mutations with varying sensitivity to EGFR TKIs, and the precise detection of these mutations will help to further refine EGFR targeted therapy.
Anti-EGFR Monoclonal Antibodies
In comparison to EGFR TKIs, anti-EGFR monoclonal antibodies have had little role in the treatment of NSCLC. The humanized IgG1 anti-EGFR monoclonal antibody, cetuximab, has been tested in several combinations and has generally demonstrated meager clinical success for an unselected NSCLC population. In patients with stage III NSCLC, the addition of cetuximab to concurrent chemoradiation and consolidation carboplatin plus paclitaxel provided no OS benefit and was associated with more grade 3 or greater toxic effects (86% vs 70%, P < 0.0001) [151]. The addition of cetuximab to platinum-based chemotherapy for advanced NSCLC was examined in two large randomized phase III trials: FLEX in patients with “EGFR-expressing” tumors by histology or cytology and BMS099 in unselected patients. There was no change in PFS, and the OS advantage was 1.3 months (P = 0.04 for FLEX, and P = 0.169 for BMS099) [152, 153]. More recently, in the randomized phase III SWOG S0819 trial of 1313 treatment-naive patients with advanced NSCLC, the addition of cetuximab to carboplatin plus paclitaxel (and if appropriate, bevacizumab) failed to add an improvement in OS [154]. Subset analysis of patients with tumors with EGFR high copy number or amplification by fluorescence in situ hybridization (FISH) also failed to find any OS benefit. Weekly administration, additional cost, minimal or no survival advantage, and side effects (primarily grade 3 rash) led to cetuximab not being approved by either the EMA or FDA [155].
Despite their lack of success in unselected NSCLC patients, anti-EGFR monoclonal antibodies have shown some efficacy in squamous NSCLC. Although squamous NSCLC harbor a low frequency of EGFR mutations, they tend to have higher rates of EGFR overexpression compared to lung adenocarcinoma [156]. In fact, the EGFR TKIs, erlotinib and afatinib, have also demonstrated efficacy in squamous NSCLC, and afatinib has an FDA approval for pretreated squamous cell carcinoma of the lung [157, 158]. In a prespecified subset analysis of 111 patients in SWOG S0819 with squamous histology, the median overall survival was 11.8 months in the cetuximab arm vs 6.1 months for carboplatin and paclitaxel arm (HR = 0.58, P = 0.007) [154].
The second-generation fully humanized IgG1 anti-EGFR monoclonal antibody, necitumumab, was added to gemcitabine/cisplatin for patients with advanced squamous NSCLC in the randomized phase III trial, SQUIRE. There was a slight OS advantage (11.5 vs 9.9 months for the gemcitabine/cisplatin, HR 0.84, P = 0.01), at the expense of more grade 3 adverse events reported in patients receiving necitumumab (72% vs 62%) [159]. In 2015, the FDA approved necitumumab in combination with gemcitabine and cisplatin for squamous NSCLC [160]. In light of other therapies such as combination chemoimmunotherapy or docetaxel plus ramucirumab [161, 162], the role of anti-EGFR therapy for squamous NSCLC has been debated [163, 164]. Recently, the National Comprehensive Cancer Network Panel unanimously voted to delete necitumumab plus gemcitabine and cisplatin from its list of recommended therapies, citing “toxicity, cost, and limited improvement in efficacy when compared to cisplatin/gemcitabine” [165].
The most significant area of clinical success of EGFR monoclonal antibodies for NSCLC is in combination with EGFR TKIs. In a phase Ib study of 126 heavily pretreated patients who had acquired resistance to erlotinib or gefitinib, the combination of afatinib with cetuximab led to an ORR of 29% and median PFS 4.7 months (regardless of T790M mutation status) [166, 167]. This suggests that at the time of acquired resistance a certain proportion of patients retain dependence on EGFR-mediated signaling that may be overcome with dual EGFR blockade. Given the improved efficacy and toxicity profile of osimertinib compared to afatinib across trials, there are at least three ongoing phase I trials of osimertinib in combination with necitumumab [168].
Addition of Chemotherapy to First-Line EGFR TKI
It has been hypothesized that the addition of chemotherapy to EGFR TKI could postpone the emergence of acquired resistance. The first trial to assess an EGFR TKI plus chemotherapy compared to an EGFR TKI alone in an exclusively EGFR mutation-positive population was a randomized phase II trial conducted in Asia of 191 patients with advanced NSCLC with activating EGFR mutations who received pemetrexed with gefitinib or gefitinib alone [169]. The combination prolonged PFS to 15.8 months vs 10.9 months, which was intriguing but did not reach statistical significance (HR = 0.68, P = 0.18). There is an ongoing confirmatory phase III study, AGAIN (JCOG1404/WJOG8214L), in which patients are randomized to gefitinib or gefitinib with cisplatin and pemetrexed as first-line treatment. Currently, it is unclear whether the addition of chemotherapy to an EGFR TKI offers benefit, and single-agent EGFR TKI remains the standard of care first-line treatment [165].
Bevacizumab Added to EGFR TKI
Bevacizumab is a humanized monoclonal antibody against the vascular endothelial growth factor receptor (VEGFR). The addition of bevacizumab to chemotherapy has been shown to improve OS and PFS in patients with NSCLC [170, 171]. In unselected patients with advanced, pretreated NSCLC, the double-blind phase III trial (BeTa) randomized patients to bevacizumab and erlotinib or erlotinib alone. Addition of bevacizumab to erlotinib resulted in a minimal PFS advantage of 3.4 months as compared to 1.7 months with erlotinib alone (HR 0.62, 95% CI 0.52–0.75), without any OS advantage [172]. Post hoc subset analysis failed to demonstrate any PFS or OS benefit among patients harboring EGFR mutations in this population [172].
More recent trials prospectively examining the use of bevacizumab with an EGFR TKI in patients selected for EGFR mutations have shown more promising results. In the randomized phase II study (JO25567) of upfront bevacizumab with erlotinib in patients with activating EGFR mutations, the PFS was 16.0 months in the erlotinib plus bevacizumab group compared to 9.7 months in the erlotinib group (HR 0.54, P = 0.0015) [30]. The most common grade 3 adverse reactions included hypertension (60% vs 10%), rash (25% vs 19%), and proteinuria (8% vs 0). In another randomized phase III trial (NEJ026) of patients with treatment-naive EGFR-mutated NSCLC, the study met its primary endpoint for PFS at the interim analysis with a PFS of 16.9 months in the bevacizumab and erlotinib arm compared to 13.3 months in the erlotinib arm (HR = 0.605, P = 0.0157) [173]. Both randomized trials provide evidence for combining an EGFR TKI with bevacizumab as first-line therapy, and in 2016 the European Medicines Agency (EMA) approved the combination, although no OS benefit has been found at this time.
Current combination studies are evaluating similar strategies, including some with osimertinib as the TKI and others with ramucirumab as a VEGFR monoclonal antibody. Randomized phase II trials of osimertinib and bevacizumab versus osimertinib are ongoing (BOOSTER; NCT03133546) as is the phase III CAURAL trial with an arm of osimertinib with bevacizumab (NCT02454933). The RELAY study (NCT02411448) is a randomized phase Ib/III study to investigate the safety and efficacy of ramucirumab and erlotinib, and it has a substudy arm looking at combination treatment with osimertinib. These trials may help define a potential role for VEGF pathway inhibitors in the first-line treatment for EGFR-mutated patients.
Immune Checkpoint Inhibition
Immune checkpoint inhibitors (ICIs) have dramatically changed the treatment landscape and prognosis of advanced NSCLC [174, 175], yet response rates to monotherapy in unselected patients are generally less than 20%. Therefore, there is a critical need to define those patients who are most likely to benefit. Blocking the programmed-death ligand 1 (PD-L1) or its receptor (PD-1) has demonstrated less success in patients with EGFR mutations compared to those with wild-type EGFR. A recent analysis of 1588 patients with NSCLC who had progressed on at least one prior therapy and were treated with nivolumab showed a lower ORR in the those with EGFR-mutated disease of 8.8%, compared to 19.6% for those with wild-type EGFR (P = 0.007) [176]. A meta-analysis of ICIs in metastatic NSCLC disease showed no benefit of an ICI compared to docetaxel for EGFR-mutated patients [177], further dampening the excitement for using ICIs in this population.
The combination of PD-L1 blockade and EGFR TKI has also been explored. However, this appears to be associated with significant toxicity. In the phase Ib TATTON trial, the combination of osimertinib and durvalumab was associated with interstitial lung disease in 38% of patients [178]. The study arm was closed prematurely as was the phase III CAURAL trial (NCT02454933) of osimertinib plus durvalumab [179].
In general, immune checkpoint inhibition for EGFR-mutated NSCLC has been disappointing, reflecting the different pathogenesis of this oncogene-driven subset of NSCLC. In part, this may be due to low tobacco exposure and the low resultant mutation burden and neo-antigen expression seen in EGFR-positive disease. One exception is the IMpower 150 trial of carboplatin, paclitaxel, and bevacizumab (BCP) compared to the same regimen with the PDL1 inhibitor, atezolizumab (ABCP) for patients with non-squamous NSCLC [180]. In patients without an EGFR or ALK mutation, there was a 4.5 month OS benefit (median OS 19.2 months vs 14.7 months, HR = 0.78, P = 0.016) in the ABCP arm. The combination is FDA approved for patients with non-squamous NSCLC without EGFR or ALK mutations [181]. This trial included 80 patients with an EGFR mutation and 34 with EML4-ALK fusion, another actionable NSCLC mutation; among these patients taken as a group, PFS was longer with ABCP than with BCP (median, 9.7 months vs 6.1 months; unstratified hazard ratio, 0.59; 95% CI, 0.37–0.94). Although this dataset contains relatively few patients, ABCP does offer a treatment option for EGFR-mutated NSCLC, particularly at the point that EGFR-targeted therapy options have been exhausted.
Resistance to Osimertinib and Future Directions
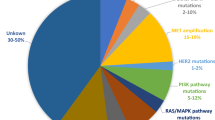
There are multiple causes of resistance to third-generation inhibitors, including EGFR or mesenchymal–epithelial transition factor (MET) amplification [182]; acquisition of resistance mutations such as C797S, L718X, and L792X [183]; and small cell transformation [168, 184, 185]. At the time of progression on osimertinib, approximately 22–40% of patients can be found to have the C797S point mutation in exon 20, a tertiary mutation that removes an important cysteine residue [114, 186]. Unlike the reversible EGFR TKIs, a defining feature of second- and third-generation inhibitors is covalent bonding to the cysteine at the 797 position, a residue at the edge of the EGFR ATP-binding cleft [80]. Due to a mutation changing the cysteine to a serine, covalent inhibitors can no longer bind to the protein. The T790M and C797S can exist in a cis position, in which a single allele has both the T790M and the C797S mutations, or in a trans position, with T790M and C797S on different alleles. Preclinical data and some clinical data suggest that the cis relationship is predominant and would be resistant to all known EGFR TKIs [187,188,189]. In contrast, if C797S and T790M are in the trans position, combined or alternating first-generation and third-generation inhibitors may be beneficial [190, 191].
The C797S mutation prevents binding of covalent inhibitors to EGFR at the ATP-binding pocket, but this may theoretically be circumvented by binding to a different site than the catalytic active site. EAI045 is one such selective allosteric inhibitor that was identified in high-throughput screens. It binds tightly to an allosteric site created by displacement of the C helix in the inactive confirmation of EGFR [192, 193]. EAI045 demonstrates selectivity and efficacy in mouse models harboring the EGFR C797S mutation (L858R/T790M/C797S) in combination with cetuximab [193]. The synergy with cetuximab seems critical to EAI045’s activity against C797S-mutated NSCLC. It remains to be seen whether other ongoing high-throughput screens will identify other potent allosteric inhibitors of EGFR and whether they will rely on the use of combination EGFR blockade as well [194].
Brigatinib is a small molecule inhibitor of both ALK and EGFR [195]. In preclinical models, “triple-mutant EGFR”-positive cells (activating EGFR mutation/T790M/C797S) responded to the combination of brigatinib with an anti-EGFR monoclonal antibody, cetuximab or panitumumab [196]. Single-agent activity of brigatinib in a phase I/II trial was only 5% [197], possibly compounded by low plasma concentrations [196], but the addition of an anti-EGFR monoclonal antibody remains to be clinically tested. The preclinical data with brigatinib and EAI045 in laboratory models with a C797S mutation demonstrate that combination therapies with an anti-EGFR monoclonal antibody may lead to overcoming resistance to osimertinib.
HER2 and MET amplification have been recognized as EGFR-independent mechanisms of acquired resistance to osimertinib, and result in continued activation of ERK and AKT [168, 198]. In patients with MET activation, the MET inhibitor, crizotinib, shows activity in preclinical models and case reports [182, 199, 200]. In the phase Ib/II TATTON trial, the combination of osimertinib with the MET inhibitor savolitinib was studied in patients with T790M EGFR-mutated NSCLC and MET amplification. In those who had not previously received a third-generation EGFR TKI, 43% of patients achieved a PR. In those previously treated with a third-generation EGFR TKI the PR rate was 20% [201]. To target both MET and EGFR, the bispecific antibody, LY3164530, was tested in a phase I trial in patients with advanced and metastatic cancer [202]. The authors concluded that the significant toxicities along with a lack of potential predictive biomarkers limited future development, but other dual-targeted agents are under development, including JNJ-61186372.
In HER2 amplified cells with acquired resistance to osimertinib, trastuzumab emtansine has shown preclinical activity [203]. In an animal tumor model that initially responds to osimertinib but eventually relapses, the addition of cetuximab and trastuzumab to osimertinib resulted in rapid and durable inhibition of tumor recurrence [204]. The authors also demonstrated benefit with the addition of an anti-HER3 antibody. There is an ongoing phase I trial of the HER3-targeting antibody drug conjugate, U3-1402, in patients with NSCLC and an activating EGFR mutation who either progressed on osimertinib or are T790M negative at the time of disease progression [205].
Conclusion
The discovery of EGFR mutations in NSCLC and the development of EGFR TKIs to target them have helped define the modern era of precision medicine. Our understanding of the molecular mechanisms of disease and resistance has allowed us to deliver innovative ways of targeting this disease, and expanded our ability to treat patients. The latest generation of EGFR TKI, osimertinib, has shown dramatic benefits, first in overcoming T790M-mediated resistance, and more recently as the first-line therapy with the longest PFS. Given its efficacy in treating CNS metastases, we are likely to redefine the optimal sequence of treatment for this special population of patients while optimizing quality of life. We have already embarked upon the next challenge of treating acquired resistance to third-generation inhibitors with several new compounds in clinical trials. Multiple mechanisms occur in acquired resistance, and future directions to overcome this might involve combination therapy targeted to the specific resistance genotype. Whereas no effective options have been available for patients with the exon 20 insertion, early clinical data show promising results for poziotinib and AP32788. We await further reports on these agents as well as others to target rare mutations in EGFR. The story of the discovery of targeted treatment for EGFR-mutated NSCLC has taught us that a deep understanding of the molecular mechanisms of disease can lead to powerful personalized treatment.
References
Rotow J, Bivona TG. Understanding and targeting resistance mechanisms in NSCLC. Nat Rev Cancer. 2017;17(11):637–58. https://doi.org/10.1038/nrc.2017.84.
Shigematsu H, Lin L, Takahashi T, Nomura M, Suzuki M, Wistuba II, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 2005;97(5):339–46. https://doi.org/10.1093/jnci/dji055.
Tsao AS, Tang XM, Sabloff B, Xiao L, Shigematsu H, Roth J, et al. Clinicopathologic characteristics of the EGFR gene mutation in non-small cell lung cancer. J Thorac Oncol. 2006;1(3):231–9.
Rosell R, Moran T, Queralt C, Porta R, Cardenal F, Camps C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361(10):958–67. https://doi.org/10.1056/NEJMoa0904554.
Zhang YL, Yuan JQ, Wang KF, Fu XH, Han XR, Threapleton D, et al. The prevalence of EGFR mutation in patients with non-small cell lung cancer: a systematic review and meta-analysis. Oncotarget. 2016;7(48):78985–93. https://doi.org/10.18632/oncotarget.12587.
Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A. 2004;101(36):13306–11. https://doi.org/10.1073/pnas.0405220101.
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350(21):2129–39. https://doi.org/10.1056/NEJMoa040938.
Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304(5676):1497–500. https://doi.org/10.1126/science.1099314.
Cohen S. Isolation of a mouse submaxillary gland protein accelerating incisor eruption and eyelid opening in the new-born animal. J Biol Chem. 1962;237:1555–62.
Burgess AW, Cho H-S, Eigenbrot C, Ferguson KM, Garrett TPJ, Leahy DJ, et al. An open-and-shut case? Recent insights into the activation of EGF/ErbB receptors. Mol Cell. 2003;12(3):541–52. https://doi.org/10.1016/S1097-2765(03)00350-2.
Carpenter G, Lembach KJ, Morrison MM, Cohen S. Characterization of the binding of 125-I-labeled epidermal growth factor to human fibroblasts. J Biol Chem. 1975;250(11):4297–304.
Yarden Y, Schlessinger J. Epidermal growth factor induces rapid, reversible aggregation of the purified epidermal growth factor receptor. Biochemistry. 1987;26(5):1443–51.
de Larco JE, Todaro GJ. Epithelioid and fibroblastic rat kidney cell clones: epidermal growth factor (EGF) receptors and the effect of mouse sarcoma virus transformation. J Cell Physiol. 1978;94(3):335–42. https://doi.org/10.1002/jcp.1040940311.
Mendelsohn J, Masui H, Goldenberg A. Anti-epidermal growth factor receptor monoclonal antibodies may inhibit A431 tumor cell proliferation by blocking an autocrine pathway. Trans Assoc Am Phys. 1987;100:173–8.
Dokala A, Thakur SS. Extracellular region of epidermal growth factor receptor: a potential target for anti-EGFR drug discovery. Oncogene. 2017;36(17):2337–44. https://doi.org/10.1038/onc.2016.393.
Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2(2):127–37. https://doi.org/10.1038/35052073.
Ullrich A, Coussens L, Hayflick JS, Dull TJ, Gray A, Tam AW, et al. Human epidermal growth factor receptor cDNA sequence and aberrant expression of the amplified gene in A431 epidermoid carcinoma cells. Nature. 1984;309:418. https://doi.org/10.1038/309418a0.
Lemmon MA, Schlessinger J, Ferguson KM. The EGFR family: not so prototypical receptor tyrosine kinases. Cold Spring Harb Perspect Biol. 2014;6(4):a020768. https://doi.org/10.1101/cshperspect.a020768.
Garrett TPJ, McKern NM, Lou M, Elleman TC, Adams TE, Lovrecz GO, et al. Crystal structure of a truncated epidermal growth factor receptor extracellular domain bound to transforming growth factor α. Cell. 2002;110(6):763–73. https://doi.org/10.1016/S0092-8674(02)00940-6.
Schlessinger J. Cell signaling by receptor tyrosine kinases. Cell. 2000;103(2):211–25.
Hirsch FR, Varella-Garcia M, Cappuzzo F. Predictive value of EGFR and HER2 overexpression in advanced non-small-cell lung cancer. Oncogene. 2009;28:S32. https://doi.org/10.1038/onc.2009.199.
Prabhakar CN. Epidermal growth factor receptor in non-small cell lung cancer. Transl Lung Cancer Res. 2015;4(2):110–8. https://doi.org/10.3978/j.issn.2218-6751.2015.01.01.
Testa JR, Siegfried JM. Chromosome abnormalities in human non-small cell lung cancer. Cancer Res. 1992;52(9 Suppl):2702s–6s.
Sharma SV, Bell DW, Settleman J, Haber DA. Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer. 2007;7(3):169–81. https://doi.org/10.1038/nrc2088.
Yasuda H, Park E, Yun CH, Sng NJ, Lucena-Araujo AR, Yeo WL, et al. Structural, biochemical, and clinical characterization of epidermal growth factor receptor (EGFR) exon 20 insertion mutations in lung cancer. Sci Transl Med. 2013;5(216):216ra177. https://doi.org/10.1126/scitranslmed.3007205.
Wang Y, Li RQ, Ai YQ, Zhang J, Zhao PZ, Li YF, et al. Exon 19 deletion was associated with better survival outcomes in advanced lung adenocarcinoma with mutant EGFR treated with EGFR-TKIs as second-line therapy after first-line chemotherapy: a retrospective analysis of 128 patients. Clin Transl Oncol. 2015;17(9):727–36. https://doi.org/10.1007/s12094-015-1300-4.
Yang JC-H, Wu Y-L, Schuler M, Sebastian M, Popat S, Yamamoto N, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16(2):141–51. https://doi.org/10.1016/S1470-2045(14)71173-8.
Zhang Y, Sheng J, Kang S, Fang W, Yan Y, Hu Z, et al. Patients with exon 19 deletion were associated with longer progression-free survival compared to those with L858R mutation after first-line EGFR-TKIs for advanced non-small cell lung cancer: a meta-analysis. PLoS One. 2014;9(9):e107161. https://doi.org/10.1371/journal.pone.0107161.
Ichihara E, Hotta K, Nogami N, Kuyama S, Kishino D, Fujii M, et al. Phase II trial of gefitinib in combination with bevacizumab as first-line therapy for advanced non-small cell lung cancer with activating EGFR gene mutations: the Okayama Lung Cancer Study Group Trial 1001. J Thorac Oncol. 2015;10(3):486–91. https://doi.org/10.1097/jto.0000000000000434.
Seto T, Kato T, Nishio M, Goto K, Atagi S, Hosomi Y, et al. Erlotinib alone or with bevacizumab as first-line therapy in patients with advanced non-squamous non-small-cell lung cancer harbouring EGFR mutations (JO25567): an open-label, randomised, multicentre, phase 2 study. Lancet Oncol. 2014;15(11):1236–44. https://doi.org/10.1016/s1470-2045(14)70381-x.
Qu J, Wang YN, Xu P, Xiang DX, Yang R, Wei W, et al. Clinical efficacy of icotinib in lung cancer patients with different EGFR mutation status: a meta-analysis. Oncotarget. 2017;8(20):33961–71. https://doi.org/10.18632/oncotarget.15475.
Moyer JD, Barbacci EG, Iwata KK, Arnold L, Boman B, Cunningham A, et al. Induction of apoptosis and cell cycle arrest by CP-358,774, an inhibitor of epidermal growth factor receptor Tyrosine Kinase. Cancer Res. 1997;57(21):4838–48.
Barker AJ, Gibson KH, Grundy W, Godfrey AA, Barlow JJ, Healy MP, et al. Studies leading to the identification of ZD1839 (IRESSA): an orally active, selective epidermal growth factor receptor tyrosine kinase inhibitor targeted to the treatment of cancer. Bioorg Med Chem Lett. 2001;11(14):1911–4.
Ward WH, Cook PN, Slater AM, Davies DH, Holdgate GA, Green LR. Epidermal growth factor receptor tyrosine kinase. Investigation of catalytic mechanism, structure-based searching and discovery of a potent inhibitor. Biochem Pharmacol. 1994;48(4):659–66.
Fukuoka M, Yano S, Giaccone G, Tamura T, Nakagawa K, Douillard JY, et al. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (the IDEAL 1 trial) [corrected]. J Clin Oncol. 2003;21(12):2237–46. https://doi.org/10.1200/jco.2003.10.038.
Kris MG, Natale RB, Herbst RS, et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non–small cell lung cancer: a randomized trial. JAMA. 2003;290(16):2149–58. https://doi.org/10.1001/jama.290.16.2149.
Thatcher N, Chang A, Parikh P, Rodrigues Pereira J, Ciuleanu T, von Pawel J, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa survival evaluation in lung cancer). Lancet. 2005;366(9496):1527–37. https://doi.org/10.1016/s0140-6736(05)67625-8.
Kim ES, Hirsh V, Mok T, Socinski MA, Gervais R, Wu YL, et al. Gefitinib versus docetaxel in previously treated non-small-cell lung cancer (INTEREST): a randomised phase III trial. Lancet. 2008;372(9652):1809–18. https://doi.org/10.1016/s0140-6736(08)61758-4.
Kazandjian D, Blumenthal GM, Yuan W, He K, Keegan P, Pazdur R. FDA approval of Gefitinib for the treatment of patients with metastatic EGFR mutation-positive non-small cell lung cancer. Clin Cancer Res. 2016;22(6):1307–12. https://doi.org/10.1158/1078-0432.Ccr-15-2266.
Herbst RS, Giaccone G, Schiller JH, Natale RB, Miller V, Manegold C, et al. Gefitinib in combination with paclitaxel and carboplatin in advanced non-small-cell lung cancer: a phase III trial–INTACT 2. J Clin Oncol. 2004;22(5):785–94. https://doi.org/10.1200/jco.2004.07.215.
Giaccone G, Herbst RS, Manegold C, Scagliotti G, Rosell R, Miller V, et al. Gefitinib in combination with gemcitabine and cisplatin in advanced non-small-cell lung cancer: a phase III trial–INTACT 1. J Clin Oncol. 2004;22(5):777–84. https://doi.org/10.1200/jco.2004.08.001.
Gatzemeier U, Pluzanska A, Szczesna A, Kaukel E, Roubec J, De Rosa F, et al. Phase III study of erlotinib in combination with cisplatin and gemcitabine in advanced non-small-cell lung cancer: the Tarceva lung cancer investigation trial. J Clin Oncol. 2007;25(12):1545–52. https://doi.org/10.1200/jco.2005.05.1474.
Herbst RS, Prager D, Hermann R, Fehrenbacher L, Johnson BE, Sandler A, et al. TRIBUTE: a phase III trial of erlotinib hydrochloride (OSI-774) combined with carboplatin and paclitaxel chemotherapy in advanced non-small-cell lung cancer. J Clin Oncol. 2005;23(25):5892–9. https://doi.org/10.1200/jco.2005.02.840.
Mok TS, Wu Y-L, Thongprasert S, Yang C-H, Chu D-T, Saijo N, et al. Gefitinib or carboplatin–paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57. https://doi.org/10.1056/NEJMoa0810699.
Fukuoka M, Wu YL, Thongprasert S, Sunpaweravong P, Leong SS, Sriuranpong V, et al. Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol. 2011;29(21):2866–74. https://doi.org/10.1200/jco.2010.33.4235.
Douillard JY, Ostoros G, Cobo M, Ciuleanu T, McCormack R, Webster A, et al. First-line gefitinib in Caucasian EGFR mutation-positive NSCLC patients: a phase-IV, open-label, single-arm study. Br J Cancer. 2014;110(1):55–62. https://doi.org/10.1038/bjc.2013.721.
Shen YW, Zhang XM, Li ST, Lv M, Yang J, Wang F, et al. Efficacy and safety of icotinib as first-line therapy in patients with advanced non-small-cell lung cancer. Onco Targets Ther. 2016;9:929–35. https://doi.org/10.2147/ott.S98363.
Bria E, Milella M, Cuppone F, Novello S, Ceribelli A, Vaccaro V, et al. Outcome of advanced NSCLC patients harboring sensitizing EGFR mutations randomized to EGFR tyrosine kinase inhibitors or chemotherapy as first-line treatment: a meta-analysis. Ann Oncol. 2011;22(10):2277–85. https://doi.org/10.1093/annonc/mdq742.
Petrelli F, Borgonovo K, Cabiddu M, Barni S. Efficacy of EGFR tyrosine kinase inhibitors in patients with EGFR-mutated non-small-cell lung cancer: a meta-analysis of 13 randomized trials. Clin Lung Cancer. 2012;13(2):107–14. https://doi.org/10.1016/j.cllc.2011.08.005.
Gao G, Ren S, Li A, Xu J, Xu Q, Su C, et al. Epidermal growth factor receptor-tyrosine kinase inhibitor therapy is effective as first-line treatment of advanced non-small-cell lung cancer with mutated EGFR: a meta-analysis from six phase III randomized controlled trials. Int J Cancer. 2012;131(5):E822–9. https://doi.org/10.1002/ijc.27396.
Lee CK, Davies L, Wu YL, Mitsudomi T, Inoue A, Rosell R, et al. Gefitinib or Erlotinib vs chemotherapy for EGFR mutation-positive lung cancer: individual patient data meta-analysis of overall survival. J Natl Cancer Inst. 2017;109(6) https://doi.org/10.1093/jnci/djw279.
Yang JJ, Zhou Q, Yan HH, Zhang XC, Chen HJ, Tu HY, et al. A phase III randomised controlled trial of erlotinib vs gefitinib in advanced non-small cell lung cancer with EGFR mutations. Br J Cancer. 2017;116(5):568–74. https://doi.org/10.1038/bjc.2016.456.
Urata Y, Katakami N, Morita S, Kaji R, Yoshioka H, Seto T, et al. Randomized phase III study comparing Gefitinib with Erlotinib in patients with previously treated advanced lung adenocarcinoma: WJOG 5108L. J Clin Oncol. 2016;34(27):3248–57. https://doi.org/10.1200/jco.2015.63.4154.
Lee CK, Brown C, Gralla RJ, Hirsh V, Thongprasert S, Tsai CM, et al. Impact of EGFR inhibitor in non-small cell lung cancer on progression-free and overall survival: a meta-analysis. J Natl Cancer Inst. 2013;105(9):595–605. https://doi.org/10.1093/jnci/djt072.
Paz-Ares L, Soulieres D, Moecks J, Bara I, Mok T, Klughammer B. Pooled analysis of clinical outcome for EGFR TKI-treated patients with EGFR mutation-positive NSCLC. J Cell Mol Med. 2014;18(8):1519–39. https://doi.org/10.1111/jcmm.12278.
Thongprasert S, Duffield E, Saijo N, Wu YL, Yang JC, Chu DT, et al. Health-related quality-of-life in a randomized phase III first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients from Asia with advanced NSCLC (IPASS). J Thorac Oncol. 2011;6(11):1872–80. https://doi.org/10.1097/JTO.0b013e31822adaf7.
Chen G, Feng J, Zhou C, Wu YL, Liu XQ, Wang C, et al. Quality of life (QoL) analyses from OPTIMAL (CTONG-0802), a phase III, randomised, open-label study of first-line erlotinib versus chemotherapy in patients with advanced EGFR mutation-positive non-small-cell lung cancer (NSCLC). Ann Oncol. 2013;24(6):1615–22. https://doi.org/10.1093/annonc/mdt012.
Soria JC, Wu YL, Nakagawa K, Kim SW, Yang JJ, Ahn MJ, et al. Gefitinib plus chemotherapy versus placebo plus chemotherapy in EGFR-mutation-positive non-small-cell lung cancer after progression on first-line gefitinib (IMPRESS): a phase 3 randomised trial. Lancet Oncol. 2015;16(8):990–8. https://doi.org/10.1016/s1470-2045(15)00121-7.
Mok TSK, Kim SW, Wu YL, Nakagawa K, Yang JJ, Ahn MJ, et al. Gefitinib plus chemotherapy versus chemotherapy in epidermal growth factor receptor mutation-positive non-small-cell lung cancer resistant to first-line Gefitinib (IMPRESS): overall survival and biomarker analyses. J Clin Oncol. 2017;35(36):4027–34. https://doi.org/10.1200/jco.2017.73.9250.
Li D, Ambrogio L, Shimamura T, Kubo S, Takahashi M, Chirieac LR, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene. 2008;27:4702. https://doi.org/10.1038/onc.2008.109. https://www.nature.com/articles/onc2008109#supplementary-information.
Engelman JA, Zejnullahu K, Gale CM, Lifshits E, Gonzales AJ, Shimamura T, et al. PF00299804, an irreversible pan-ERBB inhibitor, is effective in lung cancer models with EGFR and ERBB2 mutations that are resistant to gefitinib. Cancer Res. 2007;67(24):11924–32. https://doi.org/10.1158/0008-5472.Can-07-1885.
Gonzales AJ, Hook KE, Althaus IW, Ellis PA, Trachet E, Delaney AM, et al. Antitumor activity and pharmacokinetic properties of PF-00299804, a second-generation irreversible pan-erbB receptor tyrosine kinase inhibitor. Mol Cancer Ther. 2008;7(7):1880–9. https://doi.org/10.1158/1535-7163.Mct-07-2232.
Yonesaka K, Kudo K, Nishida S, Takahama T, Iwasa T, Yoshida T, et al. The pan-HER family tyrosine kinase inhibitor afatinib overcomes HER3 ligand heregulin-mediated resistance to EGFR inhibitors in non-small cell lung cancer. Oncotarget. 2015;6(32):33602–11. https://doi.org/10.18632/oncotarget.5286.
Miller VA, Hirsh V, Cadranel J, Chen YM, Park K, Kim SW, et al. Afatinib versus placebo for patients with advanced, metastatic non-small-cell lung cancer after failure of erlotinib, gefitinib, or both, and one or two lines of chemotherapy (LUX-Lung 1): a phase 2b/3 randomised trial. Lancet Oncol. 2012;13(5):528–38. https://doi.org/10.1016/s1470-2045(12)70087-6.
Reckamp KL, Giaccone G, Camidge DR, Gadgeel SM, Khuri FR, Engelman JA, et al. A phase 2 trial of dacomitinib (PF-00299804), an oral, irreversible pan-HER (human epidermal growth factor receptor) inhibitor, in patients with advanced non-small cell lung cancer after failure of prior chemotherapy and erlotinib. Cancer. 2014;120(8):1145–54. https://doi.org/10.1002/cncr.28561.
Takeda M, Okamoto I, Nakagawa K. Pooled safety analysis of EGFR-TKI treatment for EGFR mutation-positive non-small cell lung cancer. Lung Cancer. 2015;88(1):74–9. https://doi.org/10.1016/j.lungcan.2015.01.026.
Wang LY, Cui JJ, Guo AX, Yin JY. Clinical efficacy and safety of afatinib in the treatment of non-small-cell lung cancer in Chinese patients. Onco Targets Ther. 2018;11:529–38. https://doi.org/10.2147/ott.S136579.
Califano R, Tariq N, Compton S, Fitzgerald DA, Harwood CA, Lal R, et al. Expert consensus on the management of adverse events from EGFR Tyrosine Kinase inhibitors in the UK. Drugs. 2015;75(12):1335–48. https://doi.org/10.1007/s40265-015-0434-6.
Yang CJ, Tsai MJ, Hung JY, Lee MH, Tsai YM, Tsai YC, et al. The clinical efficacy of Afatinib 30 mg daily as starting dose may not be inferior to Afatinib 40 mg daily in patients with stage IV lung adenocarcinoma harboring exon 19 or exon 21 mutations. BMC Pharmacol Toxicol. 2017;18(1):82. https://doi.org/10.1186/s40360-017-0190-1.
Park K, Tan E-H, O’Byrne K, Zhang L, Boyer M, Mok T, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-Lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol. 2016;17(5):577–89. https://doi.org/10.1016/S1470-2045(16)30033-X.
Sequist LV, Yang JC, Yamamoto N, O’Byrne K, Hirsh V, Mok T, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol. 2013;31(27):3327–34. https://doi.org/10.1200/jco.2012.44.2806.
Wu YL, Zhou C, Hu CP, Feng J, Lu S, Huang Y, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(2):213–22. https://doi.org/10.1016/s1470-2045(13)70604-1.
Paz-Ares L, Tan EH, O’Byrne K, Zhang L, Hirsh V, Boyer M, et al. Afatinib versus gefitinib in patients with EGFR mutation-positive advanced non-small-cell lung cancer: overall survival data from the phase IIb LUX-Lung 7 trial. Ann Oncol. 2017;28(2):270–7. https://doi.org/10.1093/annonc/mdw611.
Wu YL, Cheng Y, Zhou X, Lee KH, Nakagawa K, Niho S, et al. Dacomitinib versus gefitinib as first-line treatment for patients with EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): a randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18(11):1454–66. https://doi.org/10.1016/s1470-2045(17)30608-3.
Mok TS, Cheng Y, Zhou X, Lee KH, Nakagawa K, Niho S, et al. Improvement in overall survival in a randomized study that compared Dacomitinib with Gefitinib in patients with advanced non–small-cell lung cancer and EGFR-activating mutations. J Clin Oncol. 2018;36(22):2244–50. https://doi.org/10.1200/JCO.2018.78.7994.
FDA. VIZIMPRO (dacomitinib) tablets, for oral use. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/211288s000lbl.pdf.
Addeo A. Dacomitinib in NSCLC: a positive trial with little clinical impact. Lancet Oncol. 2018;19(1):e4. https://doi.org/10.1016/S1470-2045(17)30923-3.
Ou SHI, Soo RA. Dacomitinib in lung cancer: a “lost generation” EGFR tyrosine-kinase inhibitor from a bygone era? Drug Des Devel Ther. 2015;9:5641–53. https://doi.org/10.2147/dddt.S52787.
Kobayashi S, Boggon TJ, Dayaram T, Jänne PA, Kocher O, Meyerson M, et al. EGFR mutation and resistance of non–small-cell lung cancer to Gefitinib. N Engl J Med. 2005;352(8):786–92. https://doi.org/10.1056/NEJMoa044238.
Yun C-H, Mengwasser KE, Toms AV, Woo MS, Greulich H, Wong K-K, et al. The T790M mutation in EGFR kinase causes drug resistance by increasing the affinity for ATP. Proc Natl Acad Sci. 2008;105(6):2070–5. https://doi.org/10.1073/pnas.0709662105.
Cross DAE, Ashton SE, Ghiorghiu S, Eberlein C, Nebhan CA, Spitzler PJ, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4(9):1046–61. https://doi.org/10.1158/2159-8290.Cd-14-0337.
Oxnard GR, Arcila ME, Sima CS, Riely GJ, Chmielecki J, Kris MG, et al. Acquired resistance to EGFR Tyrosine Kinase inhibitors in EGFR-mutant lung cancer: distinct natural history of patients with tumors harboring the T790M mutation. Clin Cancer Res. 2011;17(6):1616–22. https://doi.org/10.1158/1078-0432.Ccr-10-2692.
Yu HA, Arcila ME, Rekhtman N, Sima CS, Zakowski MF, Pao W, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240–7. https://doi.org/10.1158/1078-0432.Ccr-12-2246.
Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3(75):75ra26. https://doi.org/10.1126/scitranslmed.3002003.
Gaut D, Sim MS, Yue Y, Wolf BR, Abarca PA, Carroll JM, et al. Clinical implications of the T790M mutation in disease characteristics and treatment response in patients with epidermal growth factor receptor (EGFR)-mutated non-small-cell lung cancer (NSCLC). Clin Lung Cancer. 2018;19(1):e19–28. https://doi.org/10.1016/j.cllc.2017.06.004.
Sequist LV, Soria JC, Goldman JW, Wakelee HA, Gadgeel SM, Varga A, et al. Rociletinib in EGFR-mutated non-small-cell lung cancer. N Engl J Med. 2015;372(18):1700–9. https://doi.org/10.1056/NEJMoa1413654.
Sequist LV, Soria J-C, Camidge DR. Update to Rociletinib data with the RECIST confirmed response rate. N Engl J Med. 2016;374(23):2296–7. https://doi.org/10.1056/NEJMc1602688.
Park K, Jänne PA, Yu CJ, Bazhenova L, Paz-Ares L, Baek E, et al. 412OA global phase II study of olmutinib (HM61713) in patients with T790M-positive NSCLC after failure of first-line EGFR-TKI. Ann Oncol. 2017;28(suppl_10):mdx671.001. https://doi.org/10.1093/annonc/mdx671.001.
Kim D-W, Tan DS-W, Ponce Aix S, Sequist LV, Smit EF, Hida T, et al. Preliminary phase II results of a multicenter, open-label study of nazartinib (EGF816) in adult patients with treatment-naïve EGFR-mutant non-small cell lung cancer (NSCLC). J Clin Oncol. 2018;36(15_suppl):9094. https://doi.org/10.1200/JCO.2018.36.15_suppl.9094.
Wang H, Zhang L, Zheng X, Zhang X, Si X, Wang M. The ability of avitinib to penetrate the blood brain barrier and its control of intra−/extra- cranial disease in patients of non-small cell lung cancer (NSCLC) harboring EGFR T790M mutation. J Clin Oncol. 2017;35(15_suppl):e20613. https://doi.org/10.1200/JCO.2017.35.15_suppl.e20613.
Murakami H, Nokihara H, Hayashi H, Seto T, Park K, Azuma K, et al. Clinical activity of ASP8273 in Asian patients with non-small-cell lung cancer with EGFR activating and T790M mutations. Cancer Sci. 2018;109(9):2852–62. https://doi.org/10.1111/cas.13724.
Husain H, Martins RG, Goldberg SB, Senico P, Ma W, Masters J, et al. 1358PFirst-in-human phase I study of PF-06747775, a third-generation mutant selective EGFR tyrosine kinase inhibitor (TKI) in metastatic EGFR mutant NSCLC after progression on a first-line EGFR TKI. Ann Oncol. 2017;28(suppl_5):mdx380.060. https://doi.org/10.1093/annonc/mdx380.060.
Wu YL, Ahn MJ, Garassino MC, Han JY, Katakami N, Kim HR, et al. CNS efficacy of Osimertinib in patients with T790M-positive advanced non-small-cell lung cancer: data from a randomized phase III trial (AURA3). J Clin Oncol. 2018:Jco2018779363. https://doi.org/10.1200/jco.2018.77.9363.
Gao X, Le X, Costa DB. The safety and efficacy of osimertinib for the treatment of EGFR T790M mutation positive non-small-cell lung cancer. Expert Rev Anticancer Ther. 2016;16(4):383–90. https://doi.org/10.1586/14737140.2016.1162103.
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or Platinum-Pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2017;376(7):629–40. https://doi.org/10.1056/NEJMoa1612674.
Osimertinib (TAGRISSO). U.S. Food and Drug Administration (FDA). https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm549683.htm. Accessed 12 Oct 2018.
Bertranou E, Bodnar C, Dansk V, Greystoke A, Large S, Dyer M. Cost-effectiveness of osimertinib in the UK for advanced EGFR-T790M non-small cell lung cancer. J Med Econ. 2018;21(2):113–21. https://doi.org/10.1080/13696998.2017.1377718.
Ramalingam SS, Yang JC, Lee CK, Kurata T, Kim DW, John T, et al. Osimertinib as first-line treatment of EGFR mutation-positive advanced non-small-cell lung cancer. J Clin Oncol. 2018;36(9):841–9. https://doi.org/10.1200/jco.2017.74.7576.
Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25. https://doi.org/10.1056/NEJMoa1713137.
FDA approves osimertinib for first-line treatment of metastatic NSCLC with most common EGFR mutations. U.S. Food & Drug Administation (FDA). https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm605113.htm. Accessed 13 Oct 2018.
Sundaresan TK, Sequist LV, Heymach JV, Riely GJ, Janne PA, Koch WH, et al. Detection of T790M, the acquired resistance EGFR mutation, by Tumor Biopsy versus noninvasive blood-based analyses. Clin Cancer Res. 2016;22(5):1103–10. https://doi.org/10.1158/1078-0432.ccr-15-1031.
Vanderlaan PA, Yamaguchi N, Folch E, Boucher DH, Kent MS, Gangadharan SP, et al. Success and failure rates of tumor genotyping techniques in routine pathological samples with non-small-cell lung cancer. Lung Cancer. 2014;84(1):39–44. https://doi.org/10.1016/j.lungcan.2014.01.013.
Folch E, Yamaguchi N, VanderLaan PA, Kocher ON, Boucher DH, Goldstein MA, et al. Adequacy of lymph node transbronchial needle aspirates using convex probe endobronchial ultrasound for multiple tumor genotyping techniques in non-small-cell lung cancer. J Thorac Oncol. 2013;8(11):1438–44. https://doi.org/10.1097/JTO.0b013e3182a471a9.
Overman MJ, Modak J, Kopetz S, Murthy R, Yao JC, Hicks ME, et al. Use of research biopsies in clinical trials: are risks and benefits adequately discussed? J Clin Oncol. 2013;31(1):17–22. https://doi.org/10.1200/jco.2012.43.1718.
Sacher AG, Paweletz C, Dahlberg SE, Alden RS, O’Connell A, Feeney N, et al. Prospective validation of rapid plasma genotyping for the detection of EGFR and KRAS mutations in advanced lung cancer. JAMA Oncol. 2016;2(8):1014–22. https://doi.org/10.1001/jamaoncol.2016.0173.
Lokhandwala T, Bittoni MA, Dann RA, D’Souza AO, Johnson M, Nagy RJ, et al. Costs of diagnostic assessment for lung cancer: a medicare claims analysis. Clin Lung Cancer. 2017;18(1):e27–34. https://doi.org/10.1016/j.cllc.2016.07.006.
Piotrowska Z, Niederst MJ, Mino-Kenudson M, Morales-Oyarvide V, Fulton L, Lockerman E, et al. Variation in mechanisms of acquired resistance among EGFR-mutant NSCLC patients with more than 1 Postresistant Biopsy. Int J Radiat Oncol Biol Phys. 90(5):S6–7. https://doi.org/10.1016/j.ijrobp.2014.08.032.
Goldman JW, Noor ZS, Remon J, Besse B, Rosenfeld N. Are liquid biopsies a surrogate for tissue EGFR testing? Ann Oncol. 2018;29(suppl_1):i38–46. https://doi.org/10.1093/annonc/mdx706.
Zhang J, Fujimoto J, Zhang J, Wedge DC, Song X, Zhang J, et al. Intratumor heterogeneity in localized lung adenocarcinomas delineated by multiregion sequencing. Science. 2014;346(6206):256–9. https://doi.org/10.1126/science.1256930.
de Bruin EC, McGranahan N, Mitter R, Salm M, Wedge DC, Yates L, et al. Spatial and temporal diversity in genomic instability processes defines lung cancer evolution. Science (New York, NY). 2014;346(6206):251–6. https://doi.org/10.1126/science.1253462.
Lawrence MS, Stojanov P, Polak P, Kryukov GV, Cibulskis K, Sivachenko A, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499(7457):214–8. https://doi.org/10.1038/nature12213.
Jamal-Hanjani M, Wilson GA, McGranahan N, Birkbak NJ, Watkins TBK, Veeriah S, et al. Tracking the evolution of non-small-cell lung cancer. N Engl J Med. 2017;376(22):2109–21. https://doi.org/10.1056/NEJMoa1616288.
Remon J, Caramella C, Jovelet C, Lacroix L, Lawson A, Smalley S, et al. Osimertinib benefit in EGFR-mutant NSCLC patients with T790M-mutation detected by circulating tumour DNA. Ann Oncol. 2017;28(4):784–90. https://doi.org/10.1093/annonc/mdx017.
Thress KS, Paweletz CP, Felip E, Cho BC, Stetson D, Dougherty B, et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med. 2015;21(6):560–2. https://doi.org/10.1038/nm.3854.
de Bruin EC, McGranahan N, Mitter R, Salm M, Wedge DC, Yates L, et al. Spatial and temporal diversity in genomic instability processes defines lung cancer evolution. Science. 2014;346(6206):251–6. https://doi.org/10.1126/science.1253462.
Guibert NM, Paweletz C, Hu Y, Feeney NB, Plagnol V, Poole V, et al. Early detection of competing resistance mutations using plasma next-generation sequencing (NGS) in patients (pts) with EGFR-mutant NSCLC treated with osimertinib. J Clin Oncol. 2017;35(15_suppl):11529. https://doi.org/10.1200/JCO.2017.35.15_suppl.11529.
Oxnard GR, Thress KS, Alden RS, Lawrance R, Paweletz CP, Cantarini M, et al. Association between plasma genotyping and outcomes of treatment with Osimertinib (AZD9291) in advanced non-small-cell lung cancer. J Clin Oncol. 2016;34(28):3375–82. https://doi.org/10.1200/jco.2016.66.7162.
Goldman JW, Karlovich C, Sequist LV, Melnikova V, Franovic A, Gadgeel SM, et al. EGFR genotyping of matched urine, plasma, and tumor tissue in patients with non–small-cell lung cancer treated with Rociletinib, an EGFR Tyrosine Kinase inhibitor. JCO Precis Oncol. 2018;(2):1–13. https://doi.org/10.1200/po.17.00116.
Ge M, Zhuang Y, Zhou X, Huang R, Liang X, Zhan Q. High probability and frequency of EGFR mutations in non-small cell lung cancer with brain metastases. J Neuro-Oncol. 2017;135(2):413–8. https://doi.org/10.1007/s11060-017-2590-x.
Shin DY, Na II, Kim CH, Park S, Baek H, Yang SH. EGFR mutation and brain metastasis in pulmonary adenocarcinomas. J Thorac Oncol. 2014;9(2):195–9. https://doi.org/10.1097/jto.0000000000000069.
Hsiao SH, Chou YT, Lin SE, Hsu RC, Chung CL, Kao YR, et al. Brain metastases in patients with non-small cell lung cancer: the role of mutated-EGFRs with an exon 19 deletion or L858R point mutation in cancer cell dissemination. Oncotarget. 2017;8(32):53405–18. https://doi.org/10.18632/oncotarget.18509.
Mak KS, Gainor JF, Niemierko A, Oh KS, Willers H, Choi NC, et al. Significance of targeted therapy and genetic alterations in EGFR, ALK, or KRAS on survival in patients with non–small cell lung cancer treated with radiotherapy for brain metastases. Neuro-Oncology. 2015;17(2):296–302. https://doi.org/10.1093/neuonc/nou146.
Martínez P, Mak RH, Oxnard GR. Targeted therapy as an alternative to whole-brain radiotherapy in egfr-mutant or alk-positive non–small-cell lung cancer with brain metastases. JAMA Oncol. 2017;3(9):1274–5. https://doi.org/10.1001/jamaoncol.2017.1047.
Magnuson WJ, Lester-Coll NH, Wu AJ, Yang TJ, Lockney NA, Gerber NK, et al. Management of brain metastases in Tyrosine Kinase inhibitor–Naïve epidermal growth factor receptor–mutant non–small-cell lung cancer: a retrospective multi-institutional analysis. J Clin Oncol. 2017;35(10):1070–7. https://doi.org/10.1200/JCO.2016.69.7144.
Yang JC, Cho BC, Kim CH, Kim S, Lee J, Su W, et al. Osimertinib for patients (pts) with leptomeningeal metastases (LM) from EGFR-mutant non-small cell lung cancer (NSCLC): updated results from the BLOOM study. J Clin Oncol. 2017;35(15_suppl):2020. https://doi.org/10.1200/JCO.2017.35.15_suppl.2020.
Ahn M-J, Kim D-W, Cho BC, Kim S-W, Lee J-S, Ahn JS, et al. Phase I study (BLOOM) of AXD3759, a BBB penetrable EGFR inhibitor, in TKI naïve EGFRm NSCLC patients in CNS metastases. J Clin Oncol. 2017;35(suppl 18):abst 2006.
Corre R, Gervais R, Guisier F, Tassy L, Vinas F, Lamy R, et al. Octogenarians with EGFR-mutated non-small cell lung cancer treated by tyrosine-kinase inhibitor: a multicentric real-world study assessing tolerance and efficacy (OCTOMUT study). Oncotarget. 2018;9(9):8253–62. https://doi.org/10.18632/oncotarget.23836.
Yoshioka H, Komuta K, Imamura F, Kudoh S, Seki A, Fukuoka M. Efficacy and safety of erlotinib in elderly patients in the phase IV POLARSTAR surveillance study of Japanese patients with non-small-cell lung cancer. Lung Cancer. 2014;86(2):201–6. https://doi.org/10.1016/j.lungcan.2014.09.015.
Roviello G, Zanotti L, Cappelletti MR, Gobbi A, Dester M, Paganini G, et al. Are EGFR tyrosine kinase inhibitors effective in elderly patients with EGFR-mutated non-small cell lung cancer? Clin Exp Med. 2018;18(1):15–20. https://doi.org/10.1007/s10238-017-0460-7.
Morikawa N, Minegishi Y, Inoue A, Maemondo M, Kobayashi K, Sugawara S, et al. First-line gefitinib for elderly patients with advanced NSCLC harboring EGFR mutations. A combined analysis of North-East Japan Study Group studies. Expert Opin Pharmacother. 2015;16(4):465–72. https://doi.org/10.1517/14656566.2015.1002396.
Spigel DR, Hainsworth JD, Burkett ER, Burris HA, Yardley DA, Thomas M, et al. Single-agent gefitinib in patients with untreated advanced non-small-cell lung cancer and poor performance status: a Minnie pearl cancer research network phase II trial. Clin Lung Cancer. 2005;7(2):127–32. https://doi.org/10.3816/CLC.2005.n.028.
Lee SM, Khan I, Upadhyay S, Lewanski C, Falk S, Skailes G, et al. First-line erlotinib in patients with advanced non-small-cell lung cancer unsuitable for chemotherapy (TOPICAL): a double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2012;13(11):1161–70. https://doi.org/10.1016/s1470-2045(12)70412-6.
Oxnard GR, Lo PC, Nishino M, Dahlberg SE, Lindeman NI, Butaney M, et al. Natural history and molecular characteristics of lung cancers harboring EGFR exon 20 insertions. J Thorac Oncol. 2013;8(2):179–84. https://doi.org/10.1097/JTO.0b013e3182779d18.
Yasuda H, Kobayashi S, Costa DB. EGFR exon 20 insertion mutations in non-small-cell lung cancer: preclinical data and clinical implications. Lancet Oncol. 2012;13(1):e23–31. https://doi.org/10.1016/s1470-2045(11)70129-2.
Arcila ME, Nafa K, Chaft JE, Rekhtman N, Lau C, Reva BA, et al. EGFR Exon 20 insertion mutations in lung adenocarcinomas: prevalence, molecular heterogeneity, and clinicopathologic characteristics. Mol Cancer Ther. 2013;12(2):220–9. https://doi.org/10.1158/1535-7163.Mct-12-0620.
Yang M, Xu X, Cai J, Ning J, Wery JP, Li QX. NSCLC harboring EGFR exon-20 insertions after the regulatory C-helix of kinase domain responds poorly to known EGFR inhibitors. Int J Cancer. 2016;139(1):171–6. https://doi.org/10.1002/ijc.30047.
Kobayashi Y, Mitsudomi T. Not all epidermal growth factor receptor mutations in lung cancer are created equal: perspectives for individualized treatment strategy. Cancer Sci. 2016;107(9):1179–86. https://doi.org/10.1111/cas.12996.
Robichaux JP, Elamin YY, Tan Z, Carter BW, Zhang S, Liu S, et al. Mechanisms and clinical activity of an EGFR and HER2 exon 20–selective kinase inhibitor in non–small cell lung cancer. Nat Med. 2018;24(5):638–46. https://doi.org/10.1038/s41591-018-0007-9.
Socinski MA, Goldman J, El-Hariry I, Koczywas M, Vukovic V, Horn L, et al. A multicenter phase II study of ganetespib monotherapy in patients with genotypically defined advanced non-small cell lung cancer. Clin Cancer Res. 2013;19(11):3068–77. https://doi.org/10.1158/1078-0432.Ccr-12-3381.
Ramalingam S, Goss G, Rosell R, Schmid-Bindert G, Zaric B, Andric Z, et al. A randomized phase II study of ganetespib, a heat shock protein 90 inhibitor, in combination with docetaxel in second-line therapy of advanced non-small cell lung cancer (GALAXY-1). Ann Oncol. 2015;26(8):1741–8. https://doi.org/10.1093/annonc/mdv220.
Pillai R, Fennell D, Kovcin V, Ciuleanu T, Ramlau R, Kowalski D, et al. PL03.09: phase 3 study of Ganetespib, a heat shock protein 90 inhibitor, with Docetaxel versus Docetaxel in advanced non-small cell lung cancer (GALAXY-2). J Thorac Oncol. 2017;12(1):S7–8. https://doi.org/10.1016/j.jtho.2016.11.009.
Johnson ML, Yu HA, Hart EM, Weitner BB, Rademaker AW, Patel JD, et al. Phase I/II study of HSP90 inhibitor AUY922 and Erlotinib for EGFR-mutant lung cancer with acquired resistance to epidermal growth factor receptor Tyrosine Kinase inhibitors. J Clin Oncol. 2015;33(15):1666–73. https://doi.org/10.1200/jco.2014.59.7328.
Pillai RN, Ramalingam SS. Throwing more cold water on heat shock protein 90 inhibitors in NSCLC. J Thorac Oncol. 2018;13(4):473–4. https://doi.org/10.1016/j.jtho.2018.02.010.
Felip E, Barlesi F, Besse B, Chu Q, Gandhi L, Kim SW, et al. Phase 2 study of the HSP-90 inhibitor AUY922 in previously treated and molecularly defined patients with advanced non-small cell lung cancer. J Thorac Oncol. 2018;13(4):576–84. https://doi.org/10.1016/j.jtho.2017.11.131.
Noor Z, Goldman JW, Lawler W, Melancon D, Telivala B, Braiteh F, et al. P2.13-39 a phase Ib trial of the HSP90 inhibitor AUY922 in combination with Pemetrexed in metastatic non-squamous, non-small cell lung cancer patients. J Thorac Oncol. 2018;13(10, Supplement):S813–S4. https://doi.org/10.1016/j.jtho.2018.08.1434.
Piotrowska Z, Costa DB, Huberman M, Oxnard GR, Gainor JF, Heist RS, et al. Activity of AUY922 in NSCLC patients with EGFR exon 20 insertions. J Clin Oncol. 2015;33(15_suppl):8015. https://doi.org/10.1200/jco.2015.33.15_suppl.8015.
Heymach J, Negrao M, Robichaux J, et al. OA02.06 a phase II trial of Poziotinib in EGFR and HER2 Exon 20 mutant non-small cell lung cancer (NSCLC). J Thorac Oncol. 2018;13:S323–S4.
Doebele RC, Riely GJ, Spira AI, Horn L, Piotrowska Z, Costa DB, et al. First report of safety, PK, and preliminary antitumor activity of the oral EGFR/HER2 exon 20 inhibitor TAK-788 (AP32788) in non–small cell lung cancer (NSCLC). J Clin Oncol. 2018;36(15_suppl):9015. https://doi.org/10.1200/JCO.2018.36.15_suppl.9015.
FDA. GILOTRIF (afatinib). FDA. 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/201292s014lbl.pdf. Accessed 1 Nov 2018.
Yang JC, Sequist LV, Geater SL, Tsai CM, Mok TS, Schuler M, et al. Clinical activity of afatinib in patients with advanced non-small-cell lung cancer harbouring uncommon EGFR mutations: a combined post-hoc analysis of LUX-Lung 2, LUX-Lung 3, and LUX-Lung 6. Lancet Oncol. 2015;16(7):830–8. https://doi.org/10.1016/s1470-2045(15)00026-1.
Bradley JD, Paulus R, Komaki R, Masters G, Blumenschein G, Schild S, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol. 2015;16(2):187–99. https://doi.org/10.1016/s1470-2045(14)71207-0.
Pirker R, Pereira JR, Szczesna A, von Pawel J, Krzakowski M, Ramlau R, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet. 2009;373(9674):1525–31. https://doi.org/10.1016/s0140-6736(09)60569-9.
Lynch TJ, Patel T, Dreisbach L, McCleod M, Heim WJ, Hermann RC, et al. Cetuximab and first-line taxane/carboplatin chemotherapy in advanced non-small-cell lung cancer: results of the randomized multicenter phase III trial BMS099. J Clin Oncol. 2010;28(6):911–7. https://doi.org/10.1200/jco.2009.21.9618.
Herbst RS, Redman MW, Kim ES, Semrad TJ, Bazhenova L, Masters G, et al. Cetuximab plus carboplatin and paclitaxel with or without bevacizumab versus carboplatin and paclitaxel with or without bevacizumab in advanced NSCLC (SWOG S0819): a randomised, phase 3 study. Lancet Oncol. 2018;19(1):101–14. https://doi.org/10.1016/s1470-2045(17)30694-0.
Sgambato A, Casaluce F, Maione P, Rossi A, Ciardiello F, Gridelli C. Cetuximab in advanced non-small cell lung cancer (NSCLC): the showdown? J Thorac Dis. 2014;6(6):578–80. https://doi.org/10.3978/j.issn.2072-1439.2014.06.14.
Nakamura H, Kawasaki N, Taguchi M, Kabasawa K. Survival impact of epidermal growth factor receptor overexpression in patients with non-small cell lung cancer: a meta-analysis. Thorax. 2006;61(2):140.
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, et al. Erlotinib in previously treated non–small-cell lung cancer. N Engl J Med. 2005;353(2):123–32. https://doi.org/10.1056/NEJMoa050753.
Soria J-C, Felip E, Cobo M, Lu S, Syrigos K, Lee KH, et al. Afatinib versus erlotinib as second-line treatment of patients with advanced squamous cell carcinoma of the lung (LUX-Lung 8): an open-label randomised controlled phase 3 trial. Lancet Oncol. 2015;16(8):897–907. https://doi.org/10.1016/S1470-2045(15)00006-6.
Thatcher N, Hirsch FR, Luft AV, Szczesna A, Ciuleanu TE, Dediu M, et al. Necitumumab plus gemcitabine and cisplatin versus gemcitabine and cisplatin alone as first-line therapy in patients with stage IV squamous non-small-cell lung cancer (SQUIRE): an open-label, randomised, controlled phase 3 trial. Lancet Oncol. 2015;16(7):763–74. https://doi.org/10.1016/s1470-2045(15)00021-2.
FDA. PORTRAZZA (necitumumab) injection, for intravenous use – FDA. FDA. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/125547s000lbl.pdf. Accessed 30 Oct 2018.
Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gümüş M, Mazières J, et al. Pembrolizumab plus chemotherapy for squamous non–small-cell lung cancer. N Engl J Med. 2018; https://doi.org/10.1056/NEJMoa1810865.
Garon EB, Ciuleanu TE, Arrieta O, Prabhash K, Syrigos KN, Goksel T, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384(9944):665–73. https://doi.org/10.1016/s0140-6736(14)60845-x.
Hirsch FR, Herbst RS, Gandara DR. EGFR tyrosine kinase inhibitors in squamous cell lung cancer. Lancet Oncol. 2015;16(8):872–3. https://doi.org/10.1016/S1470-2045(15)00126-6.
di Noia V, D’Argento E, Pilotto S, Grizzi G, Caccese M, Iacovelli R, et al. Necitumumab in the treatment of non-small-cell lung cancer: clinical controversies. Expert Opin Biol Ther. 2018;18(9):937–45. https://doi.org/10.1080/14712598.2018.1508445.
NCCN. NCCN Clinical practice guidelines in oncology – non-small cell lung cancer. NCCN.org. 2018. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 30 Oct 2018.
Janjigian YY, Smit EF, Groen HJ, Horn L, Gettinger S, Camidge DR, et al. Dual inhibition of EGFR with afatinib and cetuximab in kinase inhibitor-resistant EGFR-mutant lung cancer with and without T790M mutations. Cancer Discov. 2014;4(9):1036–45. https://doi.org/10.1158/2159-8290.Cd-14-0326.
Smit E, Soria JC, Janjigian YY, Groen HJM, Pao W, Calvo E, et al. 86OAfatinib (A) plus cetuximab (C) in the treatment of patients (pts) with NSCLC: the story so far. Ann Oncol. 2017;28(suppl_2):mdx091.06-mdx.06. https://doi.org/10.1093/annonc/mdx091.006.
Tang Z-H, Lu J-J. Osimertinib resistance in non-small cell lung cancer: mechanisms and therapeutic strategies. Cancer Lett. 2018;420:242–6. https://doi.org/10.1016/j.canlet.2018.02.004.
Cheng Y, Murakami H, Yang PC, He J, Nakagawa K, Kang JH, et al. Randomized phase II trial of Gefitinib with and without Pemetrexed as first-line therapy in patients with advanced nonsquamous non-small-cell lung cancer with activating epidermal growth factor receptor mutations. J Clin Oncol. 2016;34(27):3258–66. https://doi.org/10.1200/jco.2016.66.9218.
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, et al. Paclitaxel–carboplatin alone or with bevacizumab for non–small-cell lung cancer. N Engl J Med. 2006;355(24):2542–50. https://doi.org/10.1056/NEJMoa061884.
Sandler A, Yi J, Dahlberg S, Kolb MM, Wang L, Hambleton J, et al. Treatment outcomes by tumor histology in Eastern Cooperative Group Study E4599 of bevacizumab with paclitaxel/carboplatin for advanced non-small cell lung cancer. J Thorac Oncol. 2010;5(9):1416–23. https://doi.org/10.1097/JTO.0b013e3181da36f4.
Herbst RS, Ansari R, Bustin F, Flynn P, Hart L, Otterson GA, et al. Efficacy of bevacizumab plus erlotinib versus erlotinib alone in advanced non-small-cell lung cancer after failure of standard first-line chemotherapy (BeTa): a double-blind, placebo-controlled, phase 3 trial. Lancet. 2011;377(9780):1846–54. https://doi.org/10.1016/s0140-6736(11)60545-x.
Furuya N, Fukuhara T, Saito H, Watanabe K, Sugawara S, Iwasawa S, et al. Phase III study comparing bevacizumab plus erlotinib to erlotinib in patients with untreated NSCLC harboring activating EGFR mutations: NEJ026. J Clin Oncol. 2018;36(15_suppl):9006. https://doi.org/10.1200/JCO.2018.36.15_suppl.9006.
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the treatment of non–small-cell lung cancer. N Engl J Med. 2015;372(21):2018–28. https://doi.org/10.1056/NEJMoa1501824.
Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al. Pembrolizumab plus chemotherapy in metastatic non–small-cell lung cancer. N Engl J Med. 2018;378(22):2078–92. https://doi.org/10.1056/NEJMoa1801005.
Garassino MC, Gelibter AJ, Grossi F, Chiari R, Soto Parra H, Cascinu S, et al. Italian Nivolumab expanded access program in nonsquamous non-small cell lung cancer patients: results in never-smokers and EGFR-mutant patients. J Thorac Oncol. 2018;13(8):1146–55. https://doi.org/10.1016/j.jtho.2018.04.025.
Lee CK, Man J, Lord S, Links M, Gebski V, Mok T, et al. Checkpoint inhibitors in metastatic EGFR-Mutated non-small cell lung cancer-a meta-analysis. J Thorac Oncol. 2017;12(2):403–7. https://doi.org/10.1016/j.jtho.2016.10.007.
Ahn MJ, Yang J, Yu H, Saka H, Ramalingam S, Goto K, et al. 136O: Osimertinib combined with durvalumab in EGFR-mutant non-small cell lung cancer: results from the TATTON phase Ib trial. J Thorac Oncol. 2016;11(4):S115. https://doi.org/10.1016/S1556-0864(16)30246-5.
Mezquita L, Planchard D. Durvalumab for the treatment of non-small cell lung cancer. Expert Rev Respir Med. 2018;12(8):627–39. https://doi.org/10.1080/17476348.2018.1494575.
Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–301. https://doi.org/10.1056/NEJMoa1716948.
FDA. TECENTRIQ (atezolizumab) injection, for intravenous use. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761034s009lbl.pdf. Accessed 14 Jan 2019.
Ortiz-Cuaran S, Scheffler M, Plenker D, Dahmen L, Scheel AH, Fernandez-Cuesta L, et al. Heterogeneous mechanisms of primary and acquired resistance to third-generation EGFR inhibitors. Clin Cancer Res. 2016;22(19):4837.
Yang Z, Yang N, Ou Q, Xiang Y, Jiang T, Wu X, et al. Investigating novel resistance mechanisms to third-generation EGFR Tyrosine Kinase inhibitor Osimertinib in non–small cell lung cancer patients. Clin Cancer Res. 2018;24(13):3097.
Yu HA, Tian SK, Drilon AE, Borsu L, Riely GJ, Arcila ME, et al. Acquired resistance of EGFR-mutant lung cancer to a T790M-specific EGFR inhibitor: emergence of a third mutation (C797S) in the EGFR Tyrosine Kinase domain. JAMA Oncol. 2015;1(7):982–4. https://doi.org/10.1001/jamaoncol.2015.1066.
Kim TM, Song A, Kim D-W, Kim S, Ahn Y-O, Keam B, et al. Mechanisms of acquired resistance to AZD9291: a mutation-selective, irreversible EGFR inhibitor. J Thorac Oncol. 2015;10(12):1736–44. https://doi.org/10.1097/JTO.0000000000000688.
Oxnard GR, Hu Y, Mileham KF, Husain H, Costa DB, Tracy P, et al. Assessment of resistance mechanisms and clinical implications in patients with EGFR T790M-positive lung cancer and acquired resistance to Osimertinib. JAMA Oncol. 2018; https://doi.org/10.1001/jamaoncol.2018.2969.
Ou SI, Cui J, Schrock AB, Goldberg ME, Zhu VW, Albacker L, et al. Emergence of novel and dominant acquired EGFR solvent-front mutations at Gly796 (G796S/R) together with C797S/R and L792F/H mutations in one EGFR (L858R/T790M) NSCLC patient who progressed on osimertinib. Lung Cancer. 2017;108:228–31. https://doi.org/10.1016/j.lungcan.2017.04.003.
Hidaka N, Iwama E, Kubo N, Harada T, Miyawaki K, Tanaka K, et al. Most T790M mutations are present on the same EGFR allele as activating mutations in patients with non-small cell lung cancer. Lung Cancer. 2017;108:75–82. https://doi.org/10.1016/j.lungcan.2017.02.019.
Niederst MJ, Hu H, Mulvey HE, Lockerman EL, Garcia AR, Piotrowska Z, et al. The Allelic context of the C797S mutation acquired upon treatment with third-generation EGFR inhibitors impacts sensitivity to subsequent treatment strategies. Clin Cancer Res. 2015;21(17):3924–33. https://doi.org/10.1158/1078-0432.Ccr-15-0560.
Wang Z, Yang JJ, Huang J, Ye JY, Zhang XC, Tu HY, et al. Lung adenocarcinoma harboring EGFR T790M and in trans C797S responds to combination therapy of first- and third-generation EGFR TKIs and shifts allelic configuration at resistance. J Thorac Oncol. 2017;12(11):1723–7. https://doi.org/10.1016/j.jtho.2017.06.017.
Arulananda S, Do H, Musafer A, Mitchell P, Dobrovic A, John T. Combination Osimertinib and Gefitinib in C797S and T790M EGFR-mutated non-small cell lung cancer. J Thorac Oncol. 2017;12(11):1728–32. https://doi.org/10.1016/j.jtho.2017.08.006.
Zhao P, Yao M-Y, Zhu S-J, Chen J-Y, Yun C-H. Crystal structure of EGFR T790M/C797S/V948R in complex with EAI045. Biochem Biophys Res Commun. 2018;502(3):332–7. https://doi.org/10.1016/j.bbrc.2018.05.154.
Jia Y, Yun C-H, Park E, Ercan D, Manuia M, Juarez J, et al. Overcoming EGFR(T790M) and EGFR(C797S) resistance with mutant-selective allosteric inhibitors. Nature. 2016;534:129. https://doi.org/10.1038/nature17960.
Westover D, Qiao H, Ichihara E, Meador CB, Lovly CM. Mechanisms of Osimertinib resistance in EGFR mutant lung cancer. J Thorac Oncol. 2017;12(8):S1546. https://doi.org/10.1016/j.jtho.2017.06.063.
Huang W-S, Liu S, Zou D, Thomas M, Wang Y, Zhou T, et al. Discovery of Brigatinib (AP26113), a phosphine oxide-containing, potent, orally active inhibitor of anaplastic lymphoma kinase. J Med Chem. 2016;59(10):4948–64. https://doi.org/10.1021/acs.jmedchem.6b00306.
Uchibori K, Inase N, Araki M, Kamada M, Sato S, Okuno Y, et al. Brigatinib combined with anti-EGFR antibody overcomes osimertinib resistance in EGFR-mutated non-small-cell lung cancer. Nat Commun. 2017;8:14768. https://www.nature.com/articles/ncomms14768#supplementary-information. https://doi.org/10.1038/ncomms14768.
Gettinger SN, Bazhenova LA, Langer CJ, Salgia R, Gold KA, Rosell R, et al. Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial. Lancet Oncol. 2016;17(12):1683–96. https://doi.org/10.1016/s1470-2045(16)30392-8.
Planchard D, Loriot Y, André F, Gobert A, Auger N, Lacroix L, et al. EGFR-independent mechanisms of acquired resistance to AZD9291 in EGFR T790M-positive NSCLC patients. Ann Oncol. 2015;26(10):2073–8. https://doi.org/10.1093/annonc/mdv319.
Ou S-HI, Agarwal N, Ali SM. High MET amplification level as a resistance mechanism to osimertinib (AZD9291) in a patient that symptomatically responded to crizotinib treatment post-osimertinib progression. Lung Cancer. 2016;98:59–61. https://doi.org/10.1016/j.lungcan.2016.05.015.
York ER, Varella-Garcia M, Bang TJ, Aisner DL, Camidge DR. Tolerable and effective combination of full-dose crizotinib and osimertinib targeting MET amplification sequentially emerging after T790M positivity in EGFR-mutant non–small cell lung cancer. J Thorac Oncol. 2017;12(7):e85–8. https://doi.org/10.1016/j.jtho.2017.02.020.
Ahn M, Han J, Sequist L, Cho BC, Lee JS, Kim S, et al. OA 09.03 TATTON Ph Ib expansion Cohort: Osimertinib plus Savolitinib for Pts with EGFR-Mutant MET-Amplified NSCLC after progression on prior EGFR-TKI. J Thorac Oncol. 2017;12(11):S1768. https://doi.org/10.1016/j.jtho.2017.09.377.
Patnaik A, Gordon M, Tsai F, Papadopoulous K, Rasco D, Beeram SM, et al. A phase I study of LY3164530, a bispecific antibody targeting MET and EGFR, in patients with advanced or metastatic cancer. Cancer Chemother Pharmacol. 2018;82(3):407–18. https://doi.org/10.1007/s00280-018-3623-7.
La Monica S, Cretella D, Bonelli M, Fumarola C, Cavazzoni A, Digiacomo G, et al. Trastuzumab emtansine delays and overcomes resistance to the third-generation EGFR-TKI osimertinib in NSCLC EGFR mutated cell lines. J Exp Clin Cancer Res. 2017;36(1):174. https://doi.org/10.1186/s13046-017-0653-7.
Romaniello D, Mazzeo L, Mancini M, Marrocco I, Noronha A, Kreitman MS, et al. A combination of approved antibodies overcomes resistance of lung cancer to Osimertinib by blocking bypass pathways. Clin Cancer Res. 2018; https://doi.org/10.1158/1078-0432.Ccr-18-0450.
Janne PA, Yu HA, Johnson ML, Vigliotti M, Shipitofsky N, Guevara FM, et al. Phase 1 study of the anti-HER3 antibody drug conjugate U3-1402 in metastatic or unresectable EGFR-mutant NSCLC. J Clin Oncol. 2018;36(15_suppl):TPS9110–TPS. https://doi.org/10.1200/JCO.2018.36.15_suppl.TPS9110.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Noor, Z.S., Goldman, J.W. (2019). EGFR Targeted Therapy. In: Salgia, R. (eds) Targeted Therapies for Lung Cancer. Current Cancer Research. Springer, Cham. https://doi.org/10.1007/978-3-030-17832-1_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-17832-1_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-17831-4
Online ISBN: 978-3-030-17832-1
eBook Packages: MedicineMedicine (R0)