Abstract
In this chapter, we systematically reviewed studies that assessed polymyxin’s effectiveness and summarized results through meta-analysis. The outcomes addressed were all-cause mortality, assuming that for patients with severe multidrug-resistant infections survival is the most important outcome, and resistance development, important for future patients. Most clinical data on polymyxins in the literature are from retrospective, observational studies at high risk of bias. The majority of clinical studies were unpowered to examine mortality controlling for other risk factors. The studies had no control of dosage regimens and treatment modifications. We identified several areas of missing data, in particular randomized controlled trials (RCTs) examining treatment options for carbapenem-resistant Gram-negative bacteria, different dosage regimens, polymyxins versus alternative antibiotics (e.g. aminoglycosides, tigecycline), and monotherapy versus specific combination therapies. Ideally, mortality and development of resistance should be examined in RCTs, with further longitudinal studies required for the latter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
11.1 Why Focus on Meta-analysis
Meta-analysis is a statistical technique of combining results from different studies. In itself the term conveys little information on the methodology of a study, as the selection criteria for the studies combined are crucial to the meta-analysis results. Systematic reviews define precisely the question addressed and the studies to be included in a meta-analysis and then attempt to include each and every study that has been performed. The advantage over a narrative review is that the information contained within the summary result is transparent and highly specific. This is also the limitation of the meta-analysis result; it addresses precisely the question addressed (patient population, intervention, comparison and outcome).
Meta-analysis provides a single point estimate summarizing all known studies that is much simpler to deal with than the many separate results of the original individual studies. However, many times the pooled estimate has poor credibility because of heterogeneity in the patient populations, interventions and outcomes assessed despite the attempt to ask specific questions. For example, addressing the question of the survival benefit of colistin-meropenem combination therapy vs. colistin monotherapy among patients with bloodstream infections is seemingly highly specific. However, the studies might evaluate mortality at different time points (in-hospital, 14-day, 28-day), colistin and meropenem might be given in different doses and schedules, patients might be infected by different Gram-negative bacteria with different MICs for meropenem. Readers of meta-analyses are advised to critically examine whether the pooled effect estimate is useful. Frequently meta-analyses will examine clinical and statistical heterogeneity and might be able to point to the factors underlying differences in results.
In this chapter, we will address systematically several questions previously reviewed in the book and try to summarize results through meta-analysis.
11.2 “Effectiveness”
The only study design appropriate to examine the effectiveness of a drug is a well-powered and well-conducted randomized controlled trial (RCT) , since only RCTs can achieve unbiased comparisons. There are no RCTs comparing colistin vs. another antibiotic for the treatment of severe infections. Historically, colistin has been considered as poorly effective and has been replaced by beta-lactams once broad-spectrum beta-lactams covering Gram-negative bacteria became available. Currently several studies and authors claim that colistin is “effective”. Its use has certainly increased in recent years and it is a primary mode of treatment for carbapenem-resistant bacteria. The question of effectiveness is important as it should determine our inclination to use colistin empirically, before we know whether the patient is infected with carbapenem-resistant bacteria. It should also determine the selection of the antibiotic to be used against carbapenem-resistant bacteria if the isolates are susceptible in-vitro to antibiotics other than colistin (e.g. an aminoglycoside, fosfomycin, tigecycline). Contained within the question of the effectiveness of colistin is also the question of optimal dosing.
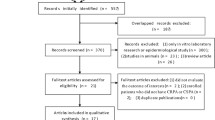
Given the lack of RCTs, we compared contemporary observational studies that assessed the effectiveness of colistin (update of a previous review [1]). The inclusion criteria were studies comparing a systemic polymyxin against a drug regimen not including a polymyxin in a comparative clinical trial, cohort (prospective or retrospective) or case-control design and reporting on mortality. We did not restrict inclusion by type of infection or bacteria.
Three studies permitted a comparison between patients given colistin vs. patients receiving inappropriate antibiotic treatment (empirical treatment) [2,3,4]. Mortality was higher with inappropriate antibiotics, with heterogeneity between the studies (Fig. 11.1). Adjusted analyses were not available.
Thirteen studies compared polymyxins to another antibiotic [5,6,7,8,9,10,11,12,13,14,15,16,17]. All studies examined patients with severe healthcare-associated infections (most commonly pneumonia and bacteremia) caused by highly-resistant bacteria. Acinetobacter baumannii and Pseudomonas aeruginosa were the common bacteria and Klebsiella pneumoniae was more rarely assessed. Polymyxins (colistin in all but two studies) were given to patients with carbapenemase-producing or phenotypically carbapenem-resistant Gram-negative bacteria (CRGNB) . Colistin was used as monotherapy in a single study [14] and in the other studies polymyxins were most commonly given in combination with other antibiotics. The comparator arm included patients with multidrug-resistant (MDR) bacteria susceptible to the non-polymyxin comparator drug and that were treated with beta-lactams (most commonly carbapenems), tobramycin (one study [8]) or tigecycline (one study [11]). Individual study results and the pooled summary for all-cause mortality are presented in Fig. 11.2. The pooled unadjusted result showed nearly twice the mortality odds with polymyxins compared to comparator drugs. The study design affected results: the meta-analysis forest plot is subcategorized by study design, from the least risk of bias (top) to the highest (bottom) and odds ratios increase from top to bottom. However, a meta-analysis of adjusted odds ratios (ORs) or odds ratios from studies using matching shows also significantly higher mortality with polymyxins with no statistical heterogeneity (adjusted OR 1.79, 95% confidence intervals (CI) 1.35–2.36, Fig. 11.3). Assessment of the effect of colistin dose on results was possible in univariate analysis only including 9 studies that reported the mean colistin dose used. The meta-regression is shown in Fig. 11.4; although, not statistically significant, a trend is shown of increasing ORs (greater advantage to comparator arm) with lower colistin dosing (presented in million IUs).
Thus, the compilation of existing studies shows that polymyxins may be more effective than no antibiotics and less effective than beta-lactams. The comparison to antibiotics potentially active against CRGNB is limited to single studies. This is based on observational studies with major limitations, of which the main is that different patients are compared. Those treated with colistin have infections caused by CRGNB while those treated with comparator antibiotics usually had carbapenem-susceptible bacteria. Therefore, these studies do not assess the effectiveness of colistin (hence “effectiveness”), but its association with mortality with many limitations. Polymyxins were administered in combination, thus results are relevant to colistin combination therapy. Colistin was given in some of the studies at a lower dose than currently recommended [18, 19] and without a loading dose and lower dosing might have been associated with a larger advantage to comparator drugs. Few retrospective studies compared colistin to polymyxin B [20,21,22,23]; the cohorts were too different to allow reasonable comparisons between groups for mortality and adjusted analyses for mortality were not conducted.
11.3 Nephrotoxicity
The same studies allowed the assessment of nephrotoxicity rates with polymyxins vs. non-polymyxins [3, 5,6,7, 9, 10, 12,13,14,15,16,17]. Nephrotoxicity was most commonly defined as at least a 1.5–2 fold increase in serum creatinine from baseline (RIFLE “risk” and above [24]). Ten studies examining colistin were identified, showing higher nephrotoxicity rates with colistin vs. comparator antibiotics, unadjusted OR 1.75 (95% CI 1.16–2.64, Fig. 11.5). Two studies examining polymyxin B did not show a significant difference vs. comparators (Fig. 11.5). None compared a polymyxin to an aminoglycoside.
Recent studies claim higher nephrotoxicity rates with colistin compared to polymyxin B [20,21,22,23]. In these studies, selection of patients depended on the type of polymyxin available (comparison between time periods or hospitals). All studies were retrospective and nephrotoxicity was similarly defined as RIFLE “risk” and above [24]. We pooled adjusted odds ratios or odds ratio reported from matched patient cohorts (non-significant univariate results taken from one study). Overall, the nephrotoxicity rate was observed to be about two-fold higher with colistin compared with polymyxin B, adjusted OR 2.12 (95% CI 1.46–3.07, Fig. 11.6).
11.4 Combination Therapy
Currently much debate surrounds the issue of polymyxin combination therapy. Empirical combination therapy is reasonable given that polymyxins are less effective than other antibiotics but more effective than no antibiotics, as shown above. The issue of debate regards combination therapy for CRGNB after receipt of the final pathogen identification and susceptibility results. Some would consider the question also pertinent for carbapenemase-producing Gram-negative bacteria that are phenotypically susceptible to carbapenems. The answer probably depends on the precise MIC of the isolate and perhaps on the type of bacterium.
The rationale for combination therapy is based on synergy , enhanced bactericidality and prevention of polymyxin-resistance development. In a systematic review and meta-analysis we analysed in-vitro interactions between polymyxins and carabapenems for different Gram-negative bacteria [25]. Synergy rates for different carbapenems and different bacteria ranged between 24% (meropenem for P. aeruginosa) to 88% (doripenem for A. baumannii). Among all carbapenem-polymyxin combinations, synergy rates were highest for A. baumannii. Among all bacteria, doripenem achieved highest synergy rates with polymyxins. Antagonism rates were low; the highest value, 24%, was observed for imipenem-polymyxin against K. pneumoniae. Bactericidal activity of the combination was greater than that of the polymyxins in most assays, increasing from 10–26% with the polymyxin to 49–74% in different isolates. Resistance developed rapidly with polymyxins alone, whereas the combination therapy generally suppressed and delayed resistance development.
While the in-vitro data appear promising, clinical results might be very different from in-vitro interactions. We compiled all clinical studies comparing colistin administered as monotherapy vs. combination therapy including colistin for the treatment of CRGNB or carbapenemase-producing Gram-negative bacteria [26]. We included RCTs and observational studies. When the same patients were included in more than one publication, we included the publication describing the largest number of patients. The outcome assessed was all-cause mortality. Results are summarized in Fig. 11.7.
Two RCTs compared colistin alone vs. colistin-rifampin for infections caused by A. baumannii [27, 28], showing no survival advantage to the combination arm. In both an advantage to colistin-rifampin was shown for secondary outcomes; clinical or microbiological cure. One RCT compared colistin alone vs. colistin-meropenem combination therapy, both administered with optimized high dosing [29]. All other studies were observational (all but two retrospective) ranging from very small case series to cohort studies, the largest analysing 250 patients. Nine studies permitted the comparison between colistin alone vs. colistin-carbapenem combination therapy [4, 29,30,31,32,33,34,35,36]. No advantage was observed to combination therapy OR 0.97, 95% CI 0.69–1.35, unadjusted except for the results of the single RCT). Similarly, the comparisons between colistin monotherapy vs. colistin combined with tigecycline, sulbactam and aminoglycoside showed no significant difference between regimens [4, 11, 30, 32, 34, 37, 38]. Four studies presented a comparison between colistin monotherapy vs. “any” combination therapy, that is difficult to translate to clinical practice. Combinations frequently included three-drug regimens. In this set of studies the combination therapy was significantly associated with higher mortality (unadjusted OR 2.09, 95% CI 1.33–3.28). The risk of bias in these studies was very high, as previously discussed [26]. The main reason underlying heterogeneity in the observational studies was carbapenem MICs, with lower MICs associated with an advantage to the combination therapy.
Thus, these meta-analyses show that despite favorable in-vitro interactions for specific antibiotic combinations , clinical studies do not demonstrate an advantage to combination therapy. The only combinations that have been tested in RCTs are those of colistin-rifampin and colistin-meropenem, and the results of the RCTs do not justify the use of this combination. Critical assessment of the observational studies shows very serious risk of bias and no significant survival advantage to specific polymyxin combinations. Lacking support for combination therapy for CRGNB, we believe that this practice should not be adopted as the routine. The discrepancy between in-vitro and clinical studies calls for well-conducted RCTs to examine specific antibiotic combinations. Such trials are under way and will determine future clinical practice.
11.5 Colistin Inhalation Therapy
Since polymyxins penetration into lung tissue is poor, nebulized colistin is sometimes being used for the treatment of respiratory tract infections. We searched for RCTs, cohort (prospective or retrospective) and case control studies comparing colistin administered as inhalation/nebulized therapy alone or with systemic treatment vs. systemic only antibiotic treatment in the treatment of ventilator-associated pneumonia or nosocomial pneumonia caused by MDR Gram-negative bacteria . We excluded studies examining patients with cystic fibrosis .
Three studies compared colistin inhalation alone vs. systemic antibiotic treatment for the treatment of pneumonia caused by A. baumannii or P. aeruginosa (one in neonates) [39,40,41]. None used matching nor reported on adjusted mortality rates. All-cause mortality was significantly lower among patients receiving colistin inhalation therapy alone compared to those treated with systemic treatment, usually polymyxins (unadjusted OR 0.37, 95% CI 0.17–0.82), with significant heterogeneity in results (Fig. 11.8).
Seven studies assessed the use of colistin inhalation as adjunctive therapy to systemic antibiotics for the treatment of A. baumannii (most commonly), P. aeruginosa or K. pneumoniae. One was a RCT [42], two used matching criteria for patients given colistin inhalations and those treated with systemic antibiotics alone [43, 44] and the remaining were unmatched and did not report an adjusted analysis for mortality [40, 45, 47]. The RCT showed no difference in mortality between study arms, while the observational studies showed a trend in favor of the adjunctive colistin inhalations , with heterogeneity in results (overall pooled OR 0.76, 95% CI 0.54–1.05, Fig. 11.9). A main concern with colistin inhalations is the induction of polymyxin-resistant bacteria, but the studies did not report on comparative resistance development rates. As expected, these studies show higher rates of eradication of the MDR bacteria from the respiratory tract with colistin inhalations.
These studies are suggestive of a possible benefit for colistin inhalation therapy, but these cannot form a basis for treatment recommendations. Selection bias is likely present in the analysis assessing colistin inhalations alone and this and other sources of bias affect the analysis of adjunctive colistin inhalations . The only RCT showed no advantage regarding survival for adjunctive colistin inhalations. Given the positive results of the observational studies, further RCTs are warranted and further observational studies should assess the long-term effects of colistin inhalations on the emergence of resistance.
11.6 Summary
Meta-analysis is an elegant tool to summarize outcome data gained from RCTs . Much of the data on polymyxins to date is based on observational studies at high risk of bias. The studies were unpowered to examine mortality, adjusting for all known risk factors for mortality. Most studies were retrospective and had no control of treatment regimens and their modification during treatment. Meta-analyses of these studies suffer from the same sources of bias and only some of the biases can be accounted for by careful analysis of the methods.
We presented here only data on mortality. The original studies examined further outcomes including clinical cure and microbiological cure. We believe that for patients with severe infections caused by MDR Gram-negative bacteria survival is ultimately the only outcome that matters to the individual patient, while resistance development is relevant epidemiologically.
Systematically reviewing the evidence highlights areas of missing data. We are mostly missing RCTs examining treatment options for CRGNBs: the two polymyxins, different doses of the polymyxins, polymyxins vs. alternative antibiotics covering CRGNBs (e.g. aminoglycosides, tigecycline) and polymyxin monotherapy vs. specific combination therapies. These RCTs should examine mortality and resistance development, although the latter should also be examined in longitudinal studies befitting the timeframe of resistance development.
References
Yahav D, Farbman L, Leibovici L et al (2012) Colistin: new lessons on an old antibiotic. Clin Microbiol Infect 18:18–29
Koomanachai P, Tiengrim S, Kiratisin P et al (2007) Efficacy and safety of colistin (colistimethate sodium) for therapy of infections caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii in Siriraj Hospital, Bangkok, Thailand. Int J Infect Dis 11:402–406
Lim SK, Lee SO, Choi SH et al (2011) The outcomes of using colistin for treating multidrug resistant Acinetobacter species bloodstream infections. J Korean Med Sci 26:325–331
Qureshi ZA, Paterson DL, Potoski BA et al (2012) Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother 56:2108–2113
Betrosian AP, Frantzeskaki F, Xanthaki A et al (2008) Efficacy and safety of high-dose ampicillin/sulbactam vs. colistin as monotherapy for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. J Infect 56:432–436
Durakovic N, Radojcic V, Boban A et al (2011) Efficacy and safety of colistin in the treatment of infections caused by multidrug-resistant Pseudomonas aeruginosa in patients with hematologic malignancy: a matched pair analysis. Intern Med 50:1009–1013
Garnacho-Montero J, Ortiz-Leyba C, Jimenez-Jimenez FJ et al (2003) Treatment of multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia (VAP) with intravenous colistin: a comparison with imipenem-susceptible VAP. Clin Infect Dis 36:1111–1118
Gounden R, Bamford C, van Zyl-Smit R et al (2009) Safety and effectiveness of colistin compared with tobramycin for multi-drug resistant Acinetobacter baumannii infections. BMC Infect Dis 9:26
Hachem RY, Chemaly RF, Ahmar CA et al (2007) Colistin is effective in treatment of infections caused by multidrug-resistant Pseudomonas aeruginosa in cancer patients. Antimicrob Agents Chemother 51:1905–1911
Kallel H, Hergafi L, Bahloul M et al (2007) Safety and efficacy of colistin compared with imipenem in the treatment of ventilator-associated pneumonia: a matched case-control study. Intensive Care Med 33:1162–1167
Ku K, Pogue JM, Moshos J et al (2012) Retrospective evaluation of colistin versus tigecycline for the treatment of Acinetobacter baumannii and/or carbapenem-resistant Enterobacteriaceae infections. Am J Infect Control 40:983–987
Kvitko CH, Rigatto MH, Moro AL et al (2011) Polymyxin B versus other antimicrobials for the treatment of pseudomonas aeruginosa bacteraemia. J Antimicrob Chemother 66:175–179
Oliveira MS, Prado GV, Costa SF et al (2008) Ampicillin/sulbactam compared with polymyxins for the treatment of infections caused by carbapenem-resistant Acinetobacter spp. J Antimicrob Chemother 61:1369–1375
Paul M, Bishara J, Levcovich A et al (2010) Effectiveness and safety of colistin: prospective comparative cohort study. J Antimicrob Chemother 65:1019–1027
Reina R, Estenssoro E, Saenz G et al (2005) Safety and efficacy of colistin in Acinetobacter and Pseudomonas infections: a prospective cohort study. Intensive Care Med 31:1058–1065
Rigatto MH, Ribeiro VB, Konzen D et al (2013) Comparison of polymyxin B with other antimicrobials in the treatment of ventilator-associated pneumonia and tracheobronchitis caused by Pseudomonas aeruginosa or Acinetobacter baumannii. Infection 41:321–328
Rios FG, Luna CM, Maskin B et al (2007) Ventilator-associated pneumonia due to colistin susceptible-only microorganisms. Eur Respir J 30:307–313
Couet W, Gregoire N, Marchand S et al (2012) Colistin pharmacokinetics: the fog is lifting. Clin Microbiol Infect 18:30–39
Plachouras D, Karvanen M, Friberg LE et al (2009) Population pharmacokinetic analysis of colistin methanesulfonate and colistin after intravenous administration in critically ill patients with infections caused by gram-negative bacteria. Antimicrob Agents Chemother 53:3430–3436
Akajagbor DS, Wilson SL, Shere-Wolfe KD et al (2013) Higher incidence of acute kidney injury with intravenous colistimethate sodium compared with polymyxin B in critically ill patients at a tertiary care medical center. Clin Infect Dis 57:1300–1303
Oliveira MS, Prado GV, Costa SF et al (2009) Polymyxin B and colistimethate are comparable as to efficacy and renal toxicity. Diagn Microbiol Infect Dis 65:431–434
Phe K, Lee Y, McDaneld PM et al (2014) In vitro assessment and multicenter cohort study of comparative nephrotoxicity rates associated with colistimethate versus polymyxin B therapy. Antimicrob Agents Chemother 58:2740–2746
Tuon FF, Rigatto MH, Lopes CK et al (2014) Risk factors for acute kidney injury in patients treated with polymyxin B or colistin methanesulfonate sodium. Int J Antimicrob Agents 43:349–352
Bellomo R, Ronco C, Kellum JA et al (2004) Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8:R204–R212
Zusman O, Avni T, Leibovici L et al (2013) Systematic review and meta-analysis of in vitro synergy of polymyxins and carbapenems. Antimicrob Agents Chemother 57:5104–5111
Paul M, Carmeli Y, Durante-Mangoni E et al (2014) Combination therapy for carbapenem-resistant gram-negative bacteria. J Antimicrob Chemother
Aydemir H, Akduman D, Piskin N et al (2013) Colistin vs. the combination of colistin and rifampicin for the treatment of carbapenem-resistant Acinetobacter baumannii ventilator-associated pneumonia. Epidemiol Infect 141:1214–1222
Durante-Mangoni E, Signoriello G, Andini R et al (2013) Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: a multicenter, randomized clinical trial. Clin Infect Dis 57:349–358
Paul M, Daikos GL, Durante-Mangoni E et al (2018) Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: an open-label, randomised controlled trial., Lancet Infect Dis 18(4):391–400. https://doi.org/10.1016/S1473-3099(18)30099-9
Batirel A, Balkan II, Karabay O et al (2014) Comparison of colistin-carbapenem, colistin-sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Infect Dis 33(8):1311–1322. https://doi.org/10.1007/s10096-014-2070-6
Bergamasco MD, Barroso Barbosa M, de Oliveira Garcia D et al (2012) Infection with Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae in solid organ transplantation. Transpl Infect Dis 14:198–205
Daikos GL, Tsaousi S, Tzouvelekis LS et al (2014) Carbapenemase-producing Klebsiella pneumoniae bloodstream infections: lowering mortality by antibiotic combination schemes and the role of Carbapenems. Antimicrob Agents Chemother 58:2322–2328
Falagas ME, Rafailidis PI, Kasiakou SK et al (2006) Effectiveness and nephrotoxicity of colistin monotherapy vs. colistin-meropenem combination therapy for multidrug-resistant gram-negative bacterial infections. Clin Microbiol Infect 12:1227–1230
Navarro-San Francisco C, Mora-Rillo M, Romero-Gomez MP et al (2013) Bacteraemia due to OXA-48-carbapenemase-producing Enterobacteriaceae: a major clinical challenge. Clin Microbiol Infect 19:E72–E79
Souli M, Kontopidou FV, Papadomichelakis E et al (2008) Clinical experience of serious infections caused by Enterobacteriaceae producing VIM-1 metallo-beta-lactamase in a Greek University Hospital. Clin Infect Dis 46:847–854
Tuon FF, Rocha JL, Arend LN et al (2013) Treatment and outcome of nine cases of KPC-producing Klebsiella pneumoniae meningitis. J Infect 67:161–164
Kalin G, Alp E, Akin A et al (2013) Comparison of colistin and colistin/sulbactam for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. Infect 42:37–42
Kontopidou F, Giamarellou H, Katerelos P et al (2014) Infections caused by carbapenem-resistant Klebsiella pneumoniae among patients in intensive care units in Greece: a multi-centre study on clinical outcome and therapeutic options. Clin Microbiol Infect 20:O117–O123
Lu Q, Luo R, Bodin L et al (2012) Efficacy of high-dose nebulized colistin in ventilator-associated pneumonia caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Anesthesiology 117:1335–1347
Naesens R, Vlieghe E, Verbrugghe W et al (2011) A retrospective observational study on the efficacy of colistin by inhalation as compared to parenteral administration for the treatment of nosocomial pneumonia associated with multidrug-resistant Pseudomonas aeruginosa. BMC Infect Dis 11:317
Nakwan N, Wannaro J, Thongmak T et al (2011) Safety in treatment of ventilator-associated pneumonia due to extensive drug-resistant Acinetobacter baumannii with aerosolized colistin in neonates: a preliminary report. Pediatr Pulmonol 46:60–66
Rattanaumpawan P, Lorsutthitham J, Ungprasert P et al (2010) Randomized controlled trial of nebulized colistimethate sodium as adjunctive therapy of ventilator-associated pneumonia caused by gram-negative bacteria. J Antimicrob Chemother 65:2645–2649
Kofteridis DP, Alexopoulou C, Valachis A et al (2010) Aerosolized plus intravenous colistin versus intravenous colistin alone for the treatment of ventilator-associated pneumonia: a matched case-control study. Clin Infect Dis 51:1238–1244
Tumbarello M, De Pascale G, Trecarichi EM et al (2013) Effect of aerosolized colistin as adjunctive treatment on the outcomes of microbiologically documented ventilator-associated pneumonia caused by colistin-only susceptible gram-negative bacteria. Chest 144:1768–1775
Kalin G, Alp E, Coskun R et al (2012) Use of high-dose IV and aerosolized colistin for the treatment of multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia: do we really need this treatment? J Infect Chemother 18:872–877
Korbila IP, Michalopoulos A, Rafailidis PI et al (2010) Inhaled colistin as adjunctive therapy to intravenous colistin for the treatment of microbiologically documented ventilator-associated pneumonia: a comparative cohort study. Clin Microbiol Infect 16:1230–1236
Livermore DM, Hill RL, Thomson H et al (2010) Antimicrobial treatment and clinical outcome for infections with carbapenem- and multiply-resistant Acinetobacter baumannii around London. Int J Antimicrob Agents 35:19–24
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Paul, M., Zusman, O., Leibovici, L. (2019). Meta-analysis of Polymyxin Use in Patients. In: Li, J., Nation, R., Kaye, K. (eds) Polymyxin Antibiotics: From Laboratory Bench to Bedside. Advances in Experimental Medicine and Biology, vol 1145. Springer, Cham. https://doi.org/10.1007/978-3-030-16373-0_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-16373-0_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16371-6
Online ISBN: 978-3-030-16373-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)