Abstract
Objective: To identify the economic burden of diabetes management in a middle-income country and its causes. Methods: Evaluative research based on a longitudinal-type design. We used the Kessner criteria and cost technology by instrumentation. For the estimation of epidemiological changes, we developed some models under the Box–Jenkins technique for the period of time 2014–2016. The financial requirements were obtained from case management costs expected by disease and the application of an econometric adjustment factor to control effects of inflation. Results: Comparing the economic impact in 2013 versus 2015 (p < 0.05), there is a 26% increase in financial requirements. The total amount for diabetes in 2015 (US dollars) was $ 8,974,662,570. It includes $ 3,981,426,810 in direct costs and $ 4993,235,752 in indirect costs. The total direct costs expected are $ 473,135,561 for the Ministry of Health (SSA), serving to uninsured population, $ 1318,506,546 for insured population (Mexican Institute for Social Security (IMSS) and Institute for Social Security and Services for State Workers (ISSSTE)), $ 2070,341,961 to users, and $ 119,442,750 to private health insurance (PHI). Conclusions: If the risk factors and the different health-care models remain as they are currently in the institutions analyzed, the financial consequences would be of major impact for the pockets of the users, following in order of importance, IMSS, SSA, and finally ISSSTE. We suggest rethinking the process of planning, organization and allocation of resources, in terms of demand for hospital and outpatients services for patients with diabetes. On the other hand, it suggests fundamental changes in the care model, increasing significantly resources and strategies toward greater prevention and primary care actions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
In the current context of health system reforms, there is a need to generate and promote models for comprehensive analysis that will advance the generation of a critical mass that will direct and sustain the changes that, in terms of production and financing, are taking place in the different subsystems of health in Latin America. Indeed, it is not surprising that health system reform programs are central to health analysis and action, particularly when it is explicitly stated that the challenge of such reforms is to achieve a balance between supply and demand of health of the different population groups [1].
Health market imbalances are one of the major challenges to overcome in the rethinking of health systems, mainly due to the disparities that exist in contrasting the available health services versus the demands, required from the epidemiological changes. As health reform projects move forward, the cost of providing services only to the demand for hospital cases of chronic-degenerative diseases will be higher, relative to the cost of providing service to the demand for outpatient and hospital cases of infectious diseases, so to further progress of the epidemiological transition, it will have greater financial implications in the production of health-care services for the short-, medium-, and long-term demands [1, 2].
In this context, health economics is defined as the application of economics to the study, production, distribution, and consumption of health-care services. Its main task is to contribute to the improvement of health without subordinating the ethical values inherent to the health of populations [1].
In economic terms, the meaning of changes in the epidemiological and demographic profile represents an increase in the demand for care for costly diseases (treatment of chronic-degenerative diseases and accidents) that will compete with the budget allocated for the treatment of infectious diseases still unresolved.
Health economics contributes to the field of health its theoretical and methodological body to support decision-making in the allocation and use of resources. It is important to recognize the need to choose better alternatives for the allocation of resources for health care, since they are scarce to meet the new or changing needs of society. It is for this reason that cost analysis tends to be an increasingly important tool for decision of planners, managers, politicians, and providers, especially in setting priorities, funding, and regulation of services of health [1, 2].
The cost of care raises the need to develop broader perspectives for the study and resolution of priority health problems, particularly chronic-degenerative problems that require ongoing attention in the short, medium, and long term depending on the phase of the natural history of disease in patients who are at the time of diagnosis. Indeed, the economic burden in managing a health problem varies depending on the quality standards that make the economic valuation of attention to a specific health claim.
The usefulness of economic evaluation evidence in health care can sometimes increase uncertainty for decision-making. For example, it is not the same as saying that the management of chronic damage to health costs 100 US$ and that was controlled with minimum quality standards, than the same damage cost 120 US$ plus not controlled with minimum quality standards [3].
In the first case we have a comprehensive evidence, solid and very relevant to make decisions for the management of health damage to the high degree of certainty and confidence to make strategic decisions that enable more efficient and effective use of resources. In the second case, where the economic valuation does not control the quality of care, we have a situation with no conclusive evidence or relevant to make correct decisions, so that decisions in this context does not guarantee high levels of efficiency and effectiveness interventions to meet the demand for health with a specific damage such as diabetes or hypertension, as a priority public health problems not only in Mexico but throughout the world.
Regarding the epidemiological history and cost of diabetes, we note that the diabetes is a health problem that requires an integral approach, since its tendency to increase has not been addressed with the developed efforts and assigned economic resources for its resolution. The high costs in health and the demographic behavior of Mexico, in which a change in the population pyramid is noticed, will add risks for the adult population that adding to the existing cases will increase the demand of health services in the near future [4, 5].
Mexico at the moment occupies the ninth worldwide place in the diabetes prevalence. This is a truly alarming site, but the projections of the international specialists refer that for year 2025, the country will occupy the seventh place. This disease has become a worldwide epidemic due to the high rates of deaths that have been registered in the last 10 years. For example, in Mexico one third of heart attacks and half of the chronic renal failures are direct consequences of diabetes [6, 7]. For this reason, the diverse institutions of health in the country have begun to reinforce their preventive campaigns to avoid even higher costs. Indeed, by the time the diagnosis of diabetes and its complications is made, the costs for the treatment are very high, and practically the patient is gradually losing his productive life years, with important repercussions in terms of indirect costs attributable to the diabetes [8, 9]. In addition, the costs in the quality of life of these patients are very high, and at the same time, the financial burden for the health sector to control the problems associated with diabetes is not known in the majority of the countries, making difficult an efficient allocation of resources and strategic planning to face the high demand of health services [10,11,12].
In addition to the epidemiological background of diabetes, it is also noteworthy the increase in health services demand and health-care costs of this type of patients. Indeed, it is quite evident that the increased costs of health services and, by consequence, the need to increase the health expenditures and changes in the methods of resource allocation for the diabetes have provoked multiple restlessness in decisions-makers. Accordingly, it becomes imperative to incorporate the economic perspective for the analysis of the health sector [13, 14]. In economic terms the meaning of the changes in the epidemiologic and demographic profile means an increase in the demand of health care of expensive diseases (treatment of chronic-degenerative diseases and accidents) that will still compete with the budget assigned for the treatment of infectious diseases. Thus, it is important to remember that there will be a need to reassess health priorities and to establish the strategic actions that will allow optimal use and organization of health resources for each health problem, in this case for diabetes mellitus [15, 16].
In summary, the observed and estimated changes in the morbidity and mortality for diabetes mellitus will generate constant increasing changes in the expected tendencies for the health services demand for diabetes. On the other hand, the constant increasing costs of the medical care and the unknown costs of handling ambulatory case management and handling of diabetes hospital cases, as well as the unknown economic resources needed to satisfy the future health services demand, justify in a pertinent and urgent way the development of research studies of applied investigation. It will allow the measurement, development, and determination of indicators of the increasing changes in the demand, of costs of case management controlling by quality of care, and of the financial amounts that will be required to be able to face the problem of diabetes mellitus in Mexico in the next years.
Methodology
The results that are presented here were generated from a study of annual monitoring on the costs and the financial consequences of the epidemiological changes in chronic-degenerative diseases in Mexico. For the case of the diabetes, we make the following methodological precisions:
-
The changes in the health services demand for diabetes were determined by means of analysis of series of time from cases observed for period 1990–2013. The estimated models of prognosis of the demand are referred to the period of time 2014–2016. The estimation method was based on the methodology of Box–Jenkins for health prognosis [17]. The expected cases for diabetes were estimated for the health system as a whole and for each sector. For the estimation of expected direct and indirect costs for diabetes, we took the year 2015 as a cutoff year since it corresponds to half of the projection period of time.
-
The quality of care was controlled from the definition of minimum quality standards of care for case management at each institution in accordance with the standards and protocols for health care for patients with chronic-degenerative diseases. The case management was determined by means of the technique of times and movements, and its validation was made by consensus with clinical experts in the management of diabetes mellitus in different institutions of the health sector. For this task we designed seven instruments to gather information according to the functions of production and inputs required to satisfy the health sector demand (see Appendix 1 with a model format to determine costs of case management).
-
The direct costs of the case management were determined from the functions of production, the combination of inputs, the standards of quality, and the costs of the inputs for each sector.
-
The indirect costs were determined using the capital human model developed for Latin America, making the necessary adjustments for the case of Mexico. The model is based on indicators of premature mortality and temporary handicap and permanent handicap attributable to diabetes [18].
-
The financial requirements for future years, like in similar studies, were considered from the expected cases, the costs of case management taking as period of reference the last year of observed cases and applying an adjustment econometric factor to control the expected inflationary process for health services in the short, medium, and long term [19].
Results
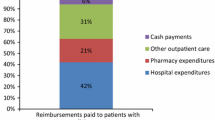
After making the estimation cases for period 2014–2016, it was decided to take as point of cutoff the year 2015 to determine the costs of diabetes mellitus care for each sector of the health system. The national annual average cost of case management was of 711 US$, and the base population estimate was 4,854,689 patients diagnosed with diabetes and treated in different institutions of the health system. The direct costs represent 46% vs 54% of indirect costs from the total costs of diabetes mellitus in Mexico. Figure 3.1 shows the distribution of the direct costs among the main items of economic impact in the management of the diabetes for different institutions of the health system.
Direct costs attributable to diabetes mellitus in Mexico, 2015: SSA. IMSS, ISSSTE, users, private health insurance (DLS). (Source: Arredondo A. (2016) Costos y consecuencias financieras del cambio en el perfil epidemiológico en México. INSP–Update of probabilistic models, January 2016). Exchange rate: January 2016, 1 US$ = 13.35 Mexican $. 95% CIs. Box–Pierce statistical test (p < 0.05). IMSS Mexican Institute for Social Security, ISSSTE Institute for Social Security and Services for State Workers, na not available, PHI private health insurance, SSA Ministry of Health
In relation to the cost of the different functions of production, it is worth noting that the inputs with the greater impact refer to medications, followed by costs of outpatient services and in smaller degree the costs of hospitalization in the cases of acute complications due to diabetes mellitus, without considering the management of chronic complications (see Fig. 3.1).
For the relative weight of the cost in the overall management of the main complications of diabetes, in all the institutions, the greater impact is in the costs for managing diabetic nephropathy, followed from largest to smallest impact by retinopathy, cardiovascular disease, diabetic neuropathy, and finally peripheral vascular disease.
With respect to the relative weight of the economic impact per origin of the costs, of the total of direct costs, the greater economic impact corresponds to the pocket of the heath service users, that is to say for each 100 US$ that are spent in diabetes in Mexico, 55 come from the pocket of the users. It follows in order of importance by its relative weight: the IMSS (27 US$ for each 100), the SSA (12 US$), and finally the ISSSTE (6 US$). What is necessary to stand out on the economic impact of diabetes among the different health institutions of the public sector is that the economic impact for the IMSS is more than double than that of the SSA and four times more than that for the ISSSTE (see Figs. 3.1 and 3.2). The same tendencies were observed when determining the costs of diabetic complications for all institutions.
Direct costs disagregated by type of complication attributable to diabetes mellitus in Mexico, 2015: SSA. IMSS, ISSSTE, users, private health insurance (DLS). (Source: Arredondo A. (2016) Costos y consecuencias financieras del cambio en el perfil epidemiológico en México. INSP–Update of probabilistic models, January 2016). Exchange rate: January 2016, 1 US$ = 13.35 Mexican $. 95% CIs. Box–Pierce statistical test (p < 0.05). IMSS Mexican Institute for Social Security, ISSSTE Institute for Social Security and Services for State Workers, na not available, PHI private health insurance, SSA Ministry of Health
With regard to the indirect costs of diabetes mellitus health care, in this dimension of costs, we were only able to estimate the indirect costs for users that sought care in the three main institutions of the public sector. These costs represent 56% of the total cost of diabetes mellitus in Mexico. They are distributed in three categories of estimation: costs by premature mortality (5%), costs by permanent handicap (95%), and costs by temporary handicap (1%) (see Figs. 3.3 and 3.4).
Indirect costs attributable to diabetes mellitus in Mexico, 2015: SSA. IMSS, ISSSTE, and private sector (DLS). (Source: Arredondo A. (2016) Costos y consecuencias financieras del cambio en el perfil epidemiológico en México. INSP–Update of probabilistic models, January 2016). Exchange rate: January 2016, 1 US$ = 13.35 Mexican $. 95% CIs. Box–Pierce statistical test (p < 0.05). IMSS Mexican Institute for Social Security, ISSSTE Institute for Social Security and Services for State Workers, na not available, PHI private health insurance, SSA Ministry of Health
Total costs attributable to diabetes mellitus in Mexico, 2014: SSA. IMSS, ISSSTE, private sector (DLS). (Source: Arredondo A. (2016) Costos y consecuencias financieras del cambio en el perfil epidemiológico en México. INSP–Update of probabilistic models, January 2016). Exchange rate: January 2016, 1 US$ = 13.35 Mexican $. 95% CIs. Box–Pierce statistical test (p < 0.05). IMSS Mexican Institute for Social Security, ISSSTE Institute for Social Security and Services for State Workers, na not available, PHI private health insurance, SSA Ministry of Health
Discussion
With respect to the costs of case management in the three public health-care institutions of interest, the results show important differences among the institutions and the hospitalized case management and outpatient cases. Before discussing the details of the results about the economic evaluation, it is important to mention that all costs were expressed in American dollars for any international comparison. From these findings it is possible to establish minimum and maximum ranges by type of disease from the three main institutions of the health system in Mexico. Indeed, on the cost of case management of hospitalized patients, the results are in a range from $675.00 to $751.00 US$. The smallest cost corresponded for the SSA and the greatest cost for the IMSS. The same tendencies are observed for the cost of the case management as outpatient cases.
The differences between costs of case management and total costs attributable to the diabetes in Mexico, observed among the different institutions of interest, are explained due to the significant differences in the specific populations that demand their services, in the cost of inputs, and in the way to combine these inputs at the time of producing the demanded service; but also the quality of the heath care whereupon each institution offers the services is an intervening and determining variable which relates to the actual cost of diabetes care for each of the main institutions of health care in Mexico. In relation to the effects of the observed epidemiological changes for the health demand of hospitalized and ambulatory services for period 2014–2016, it is expected a tendency toward an increase in the costs, although the increase is more relevant for the insured population in comparison with the uninsured population.
In the case of the insured population (IMSS and ISSSTE), they take the major amounts of financial resources. This increase responds not only due to the increase in the health demand from the changes in the epidemiological profile, but in addition to this factor, it is important to also consider the increase in the percentage rate of the projected inflationary index for period 2014–2016. It is also important to stand out that in the case of the uninsured population (SSA), it not only represents the smallest financial requirement, but also tendencies of the required financial resources are much more moderate than in the case of the insured population. From a quality of medical care perspective, social security institutions like IMSS used to provide access to their users to costly interventions, especially complications of acute diseases like those analyzed in this chapter.
When comparing the results of the direct costs for the different health-care models according to the type of institution, it is the IMSS health-care model the one that will pay the greatest cost, followed by SSA and finally ISSSTE with the smallest direct cost. The same type of tendency was observed for the case of the direct costs of the ambulatory health-care model. This pattern can be influenced by the amount of demand of medical care in each institution and by the type of utilized resources. For the uninsured, the current public insurance policy has not included yet in the medical interventions catalogue medical attention to acute kidney failure, for instance. If interventions like this were included, the costs tendency for the SSA could be modified.
With respect to the indirect costs by type of disease, it is important to stand out that the obtained cost is the minimum amount that would appear in each type of institution in agreement with the projected demand for the year 2015 as point of cutoff. On the average of the costs to the pocket of the users, it is noteworthy the high relative weight of the origin of the expenses for diabetes from the family income and its implications in the matter of equity and access to health care in Mexico. Indeed, from each 100 US$ that are spent in diabetes in Mexico, approximately 55 US$ come from the patients’ household income. This situation represents a social burden of very high impact that evidently will have a considerable effect in the measurement of the catastrophic health expenditures in the country, more importantly because it is a very expensive and of a high-priority disease that has become a public health problem in Mexico.
In relation to health-care coverage in Mexico, this is distributed more or less in the following form: 48% of the population is taken care by social security institutions; 42% of the population is taken care by institutions that serve the uninsured; and 10% of the population utilizes private care institutions. According to our results, this means that, with respect to the direct costs, out of each 100 pesos that are spent in diabetes in Mexico, 52 are spent in 10% of the population, 33 in 48% (insured) of the population, and 15 pesos in the 42% rest of the population (uninsured). With these data it is evident that there’s an equity problem and poor health-care access for the poorest population in Mexico.
Undoubtedly, it is quite evident that the problem of diabetes in Mexico not only represents a high economic and epidemiological impact. Public health-care organizations should improve their medical processes and resource allocation schemes in order to become more efficient according to their care demand and population characteristics. Under this perspective, medical services for diabetes in the social security should analyze costs reductions for high-cost interventions, while medical services for the uninsured should implement ambulatory and preventive care. For these organizations, quality improvement of medical care will be an important support to achieve efficiency and effectiveness. The economic evaluation of diabetes impacts rises in a pertinent way in terms of economic resource flow and allocation analysis. This approach could be helpful to reduce inequity and health-care accessibility for the patients with diabetes and to protect their family assets in case of economic need derived of out-of-pocket health expenditure.
With respect to the indirect costs, although they do not constitute a direct impact on the heath budget, in terms of cost and social impact, they do represent a high burden that society in general will have to assume, mainly in terms of lost productivity by premature death and handicap whether it is temporary or permanent.
The relevance to incorporate economic, epidemiological and quality of medical care aspects to the clinical perspective constitutes an integral proposal for the analysis and evaluation of the performance of the health system in the context of health system reforms. Indeed, the results of health systems research with an approach that combines economic, clinical, and epidemiological perspectives become relevant for identifying greater financial consequences in the production of health-care services for future health-care demands of chronic-degenerative diseases, particularly for the case of the diabetes mellitus.
The observed and expected changes in the epidemiological profile of diabetes, both in the public sector and in the pocket of health-care users, will lead to a financial competition in the use of resources. In such a way, the financial resource allocation for the demand or production of health services directed to diabetes will be affected by the production or demand of services for infectious diseases and other chronic diseases like hypertension. In this sense, the internal competition in the use and allocation of the economic resources requires data to estimate the approximated financial requirements to produce the services that will be demanded in short and medium terms. Therefore, the production and financing of health services for diabetes will require the incorporation of clinical, economic, and epidemiological indicators, integrated under diverse efficiency criteria.
If the risk factors and the different health-care models for ambulatory and hospitalized care remain as they are at the moment in the three institutions of analysis, the financial consequences of diabetes would be of greater impact for the IMSS, following in order of relevance the SSA and finally the ISSSTE. On the other hand, the financial requirements for the treatment of diabetes, both in the health-care demand of ambulatory and hospitalized services, would represent approximately 9% of the total budget assigned for the uninsured population and approximately the 16.5% of the assigned total budget for the insured population.
The generated analysis constitutes a tool for defining in which type of health interventions and levels of medical care to invest within the context of transformations, adjustments, or reforms of the health sector, as it is suggested in several studies. On the other hand, the estimated financial requirements constitute a base of fundamental information for strategic planning. Indeed, given the financial consequences of the expected epidemiological change, not only the need to invest greater financial resources is fundamental and justified for activities of health promotion and prevention, so that the damage to health can be diminished and controlled, avoiding the economic burden for the health systems. In summary, the economic gain in productivity and efficiency will be able to happen at the same time that the unitary costs by production functions are known for the different stages of health care. In this way it is possible to establish both the patterns of equipment needs and the patterns of productivity and efficiency of the used resources, justifying them in relation to the quality of medical care that they will generate.
With regard to equity, it is possible to affirm that every time resources are wasted, patients’ health care is compromised, and a lack of quality has been observed. In this sense, the integral planning of the costs, as an indicator of efficiency, is intimately related with the principle of equity in access to health care. The relative weight of the different inputs required in the process of care by disease allows the selection of critical inputs in health-care services, in such a way that this set of inputs must be covered in the financial resource allocation for the problem of diabetes. In addition to this type of inputs, there should be implemented preventive and quality of medical care measurements so that the conditions for a better use of the budget occur. For example, knowing that some of the critical inputs are in the expenses of hotel or hospital daybed, human resources, drugs, and solutions, the preventive and control measurements must be directed to avoid that the patients with diabetes become ill so that they require hospitalized care.
It is necessary to indicate that for greater trustworthiness, validity, and relevance of these results, it is recommended to implement systems of monitoring costs that allow to update annually or biennially the average cost of case management of diabetes to adjust in agreement with inflationary changes and changes in the costs of the inputs and more importantly changes in the tendencies of the health services demand for diabetes. Certainly to evaluate the changes in the health services demand from the expected epidemiological transition, it is also recommended that the probabilistic models are updated annually with the observed data. In this way, we will see a greater impact in the decision-making in the matter of efficient allocation and use of resources destined to the health sector. On the other hand, as regards the relative weight of diabetes costs, our direct versus indirect costs results are within similar cost ranges for other countries that have developed the economic burden of diabetes analysis [11, 20,21,22,23].
The evidence presented in this chapter constitutes a relevant input to decision-makers in order to define in which type of health interventions and levels of medical care to invest within the context of adjustments or reforms of the health sector. The estimated financial requirements constitute a base of fundamental information for strategic planning. Indeed, given the financial consequences of the epidemiological changes, not only the need to invest greater financial resources is fundamental; it also justify more activities and programs for health promotion and prevention.
In summary, the economic gain in productivity and efficiency will be able to happen at the same time that the unitary costs by production functions are known for the different stages of health care. In this way it is possible to establish both the patterns of equipment needs as well as the patterns of productivity and efficiency of the used resources, justifying them in relation to the quality of medical care that they will generate.
With regards to equity, it is possible to say that every time resources are wasted, patients’ health care is compromised, and a lack of quality has been observed. In this sense, the integral planning of the costs and quality, as an indicator of efficiency, is intimately related with the equity in access to health care.
The relative weight of the different inputs required in the process of health care by disease allows the selection of critical inputs in health-care services, in such a way that this set of inputs must be covered in the financial resource allocation for disease. In addition to these critical inputs, there should be implemented preventive and quality of medical care measurements to generate the conditions for a better use of resources. For example, knowing that some of the critical inputs are in the expenses of hospital daybed, human resources, drugs, and solutions, the preventive and control measurements must be addressed to avoid that the patients with diabetes become with complications that require hospitalized care and more expensive services.
Finally, it is necessary to indicate that for greater trustworthiness, validity, and relevance of these results, it is recommended to implement systems of monitoring costs that allow to update annually or biennially the average cost of case management of diabetes to adjust in agreement with inflationary changes and changes in the costs of the inputs and, more importantly, in concordance with changes in the trends of the health services demand for diabetes. Certainly, to evaluate the changes in the health services demand from the epidemiological transition, it is also recommended that the probabilistic models are updated annually with the observed cases by institution. In this way, we will see a greater impact in the decision-making in the matter of efficient allocation and use of resources addressed to chronic diseases.
Conclusions
With regard to the implications and to the impact for the health system and to patients, we conclude and suggest the following:
-
1.
The economic burden and financial consequences for diabetes health care constitute the fundamental basis of the information for strategic planning. Indeed, given the financial consequences of the expected epidemiological changes, not only is it essential to invest greater financial resources, but it also justifies the implementation of health prevention strategies.
-
2.
The evidence on changes in costs and in the demand for health care in diabetes patients can be used as a reference for the allocation of resources directed toward diabetes by different types of public institution. With a knowledge of likely financial requirements, each institution could then target the necessary resources for promotion, prevention, healing, and rehabilitation effectively and efficiently.
-
3.
A consequence of the implementation of cost-monitoring systems is the design and application of strategies for cost containment for weight-by-cost items. For example, knowing that the cost of medicines is high, it will be necessary for each institution to review its agreements with the pharmaceutical industry on the consolidated buying of medicines for diabetes.
-
4.
As regards the equity and diabetes care, development of economic indicators would enable the design of patterns of resource allocation based on efficiency criteria with regard to clinical, epidemiological, economic, and administrative aspects. Each institution could develop models for the distribution of resources in accordance with the changes in costs and epidemiological factors expected in future years.
-
5.
As a “Citizen Observatory of Diabetes,” social organizations could suggest and develop follow-up programs for the costs of diabetes in different public and private health institutions. The Observatory should function as a checking system that would monitor how much is being spent on managing diabetes and what the money is being spent on.
-
6.
Knowledge of the relative weight of the management of diabetes based on the annual family income, as well as precise knowledge of the cost of complications to the users, should be made available through a bulletin sent to diabetic patients and their relatives and to the community as a whole. Knowledge of the high costs of diabetes per family could lead to a greater self-awareness, as well as to effort in avoiding complications caused by diabetes.
-
7.
To avoid further impoverishment by health expenditures attributable to diabetes, a list of recommendations is needed to promote greater self-care, control of risk factors, and the benefits of carrying out these measures, and more importantly to avoid falling into a catastrophic cost situation because of diabetes (to avoid an impact >30% of the family income).
In the context of health system reforms and particularly as regards the universal coverage strategy, our results allow us to put a greater emphasis on the need to allocate more resources to health promotion and prevention, with important changes in the social aspects of diabetes as a high-priority public health problem. The treatment of diabetes should be approached from a transdisciplinary perspective: sociological (social determinants and governance indicators), clinical, economic, epidemiological, and organizational. In other words, an integrated approach to the problem of diabetes requires the development of indicators of clinical and economic efficiency, expected epidemiological changes, and social determinants associated with diabetes, as well as identifies the actors, roles, and rules for greater equity and equality of opportunity in solving the problem of diabetes. From this perspective is that it could advance to ensure effective universal coverage where patients and families would not have to pay so much for dealing with the problem of diabetes.
Concluding Remarks
-
Comparing the economic impact in 2013 versus 2015 (p < 0.05), there is a 26% increase in financial requirements. The total amount for diabetes in 2015 (US dollars) was $ 8,974,662,570. It includes $ 3,981,426,810 in direct costs and $ 4993,235,752 in indirect costs.
-
The total direct costs expected are $ 473,135,561 for the Ministry of Health (SSA), serving to uninsured population, $ 1318,506,546 for insured population (Mexican Institute for Social Security (IMSS) and Institute for Social Security and Services for State Workers (ISSSTE)), $ 2070,341,961 to users, and $ 119,442,750 to private health insurance (PHI).
-
If the risk factors and the different health-care models remain as they are currently in the institutions analyzed, the financial consequences would be of major impact for the pockets of the users, following in order of importance, IMSS, SSA, and finally ISSSTE. We suggest rethinking the process of planning, organization and allocation of resources, in terms of demand for hospital and outpatients services for patients with diabetes.
-
The diabetes in Mexico in 2015 was on average 16% of total health expenditure.
-
The analysis of different findings shows that catastrophic expenditures attributable to diabetes have a greater impact in the pockets of patients and their families in relation to the expenditure for health systems. Of every 100 US$ spent on diabetes in Mexico, 55 are from users pocket and 47 from health institutions.
-
Comparing trends in 2014 vs 2016, we show evidence that there is an increase of 9–13% on number of new cases and an increase of 26% on the economic burden.
-
The societal diabetes-attributable costs of diabetes in Mexico 2015 were estimated to be 8.9 billion US$, corresponding to 721 US$ per patient year.
-
Nearly 35% of diabetes-attributable costs were to the patients with major complications.
-
By 2015, the amount of indirect costs of disability and premature death (4.9 billion) than the direct costs of care (3.9 billion).
-
Urgent call for a strategic alliance between government, health care, businessmen, civil society, and patients with diabetes.
-
Multiple-Choice Questions (Note That Some Questions May Have More Than One Answer)
-
1.
What consequences can the late diagnosis of diabetes have?
-
(a)
Increases treatment costs
-
(b)
It improves the prognosis of the disease
-
(c)
It reduces the productive years of the person with diabetes
-
(d)
All of the above
-
(e)
Options 1 and 3
-
(a)
-
2.
In what area is the largest out-of-pocket expense of patients with diabetes and their families in Mexico?
-
(a)
In drugs
-
(b)
In treatment of complications
-
(c)
In consultations and diagnosis
-
(d)
In hospitalization
-
(e)
By transport
-
(a)
-
3.
Why is it important to invest in health promotion prevention of diabetes and its complications?
-
(a)
Because the damage to health is reduced and controlled
-
(b)
Because it avoids excessive economic burdens for health systems
-
(c)
To avoid the suffering of diabetes and its complications, for patients and families
-
(d)
All of the above
-
(e)
None of the above
-
(a)
-
4.
For the integral approach to diabetes, which of the following perspectives should work together (can mark more than one)?
-
(a)
Sociological
-
(b)
Economic
-
(c)
Epidemiological
-
(d)
Organizational
-
(e)
Clinical
-
(a)
-
5.
Which of the following actors are considered key to lower costs and the prevalence of diabetes and its complications?
-
(a)
The health system in its role of rectory
-
(b)
Organized civil society
-
(c)
Health-related industry (pharmaceuticals, equipment and technology)
-
(d)
All of the above
-
(e)
None of the above
-
(a)
-
6.
Which are the major tendencies in resources expenditure for diabetes in the Mexican case?
-
(a)
Resources expenditure tends to be the same for public and private medical care providers.
-
(b)
Costs of medical care tend to be higher for insured populations, with a considerable burden of out-of-pocket expenditure for patients.
-
(c)
Costs of medical care tend to be higher for insured populations, without out-of-pocket expenditure for patients.
-
(d)
Costs for medical care remain constant in time for all providers.
-
(e)
Nevertheless costs for medical care of diabetes tend to be higher; there’s no need to be concerned about.
-
(a)
-
7.
Why is it urgently necessary to incorporate economic evidence to improve health systems’ capacities in response to the described diabetes challenges?
-
(a)
Economics and management should not be related, because of theoretical and practical reasons.
-
(b)
Economic evidence is hard to translate for managerial purposes.
-
(c)
The medical care for diabetes is complex and hazardous; it is difficult to establish adequate resources planning.
-
(d)
Economic evidence is helpful for reducing uncertainty in the planning and decision-making processes.
-
(e)
Variations in direct and indirect costs are not relevant for an adequate planning
-
(a)
-
8.
What reasons could explain that spending resources for diabetes care used to be higher in insured populations for the Mexican case?
-
(a)
Social security health providers have developed an economic platform that creates strong commitment of health-care provision.
-
(b)
The health financing has three different sources; availability of resources tends to be higher for these providers.
-
(c)
Infrastructure and human resources for social security tend to be wider and more aligned to health needs.
-
(d)
All previous.
-
(e)
None.
-
(a)
-
9.
What is the rate of increase in the financial trends of the epidemiological changes for the period under study?
-
(a)
9–13%
-
(b)
10–12%
-
(c)
13–16%
-
(d)
14–17%
-
(e)
8–13%
-
(a)
-
10.
What is the rate of increase in epidemiological trends for the period under study?
-
(a)
23%
-
(b)
20%
-
(c)
24%
-
(d)
26%
-
(e)
28%
-
(a)
Correct Answers
-
1.
(e) Options 1 and 3
-
2.
(a) In drugs
-
3.
(d) All of the above
-
4.
(a–e)
-
5.
(d) All of the above
-
6.
(c) Costs of medical care tend to be higher for insured populations, without out-of-pocket expenditure for patients.
-
7.
(d) Economic evidence is helpful for reducing uncertainty in the planning and decision-making processes.
-
8.
(e) None.
-
9.
(a) 9–13%
-
10.
(d) 26%
References
Arredondo A, Orozco E. Libro Gerencia y Economía en Salud. Indicadores epidemiológicos y económicos: Aportes de la economía de la salud. Centro Interamericano de Estudios en Seguridad Social. Mexico, DF. ISBN: 968-6748-39-3; 2014. p. 91–112.
Pinzón Flórez CE, Chapman E, Panisset U, Arredondo A, Fitzgerald J, Reveiz L. Disponibilidad de indicadores para el seguimiento del alcance de la “Salud Universal” en América Latina y el Caribe. Rev Panam Salud Pública. 2016;39(6):330–40.
Arredondo A, Barceló A. The economic burden of out-of-pocket medical expenditures for patients seeking diabetes care in Mexico. Diabetologia. 2007;50:435–6.
Instituto Nacional de Salud Pública. Métodos de estimación de demanda esperada de enfermedades crónico-degenerativas. Informe Técnico de Memoria Metodológica. Cuernavaca, México. Febrero del 2017. p. 63–78.
Arredondo A, Zuñiga A. Economic burden of diabetes in middle-income countries: the Mexican case. Diabetes Care. 2004;29:104–9.
Secretaría de Salud, Información básica sobre recursos y servicios del Sistema Nacional de Salud. Informe Técnico. 2016. p. 68–76.
Panamerican Health Organization, Health Analysis and Information Systems, Regional Mortality Database. 2016. p. 23–37.
Caro J, Ward A, O’Brien J. Lifetime Costs of Complications Resulting From Type 2 Diabetes in the U.S. Diabetes Care. 2002;25:476–81.
Brown JB, Pedula KL, Bakst AW. The progressive cost of complications in type 2 diabetes mellitus. Arch Intern Med. 1999;159:1873–80.
International Diabetes Federation. Direct cost to the health care sector. Brussels: Diabetes Health Economics, International Diabetes Federation; 2015. p. 13–5.
Dawson KG, Gomes D, Gerstein H, Blanchard JF, Kahler KH. The economic cost of diabetes in Canada. Diabetes Care. 2002;25:1303–7.
Barcelo A, Daroca MC, Ribera R, Duarte E, Zapata A, Vohra M. Diabetes in Bolivia. Rev Panam Salud Publica. 2001;10:318–23.
International Diabetes Federation. Direct cost to the health care sector. Brussels: Diabetes Health Economics, International Diabetes Federation; 2015. p. 29–35.
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes. Estimates for the year 2000 and projections for 2030. Diabetes Care. 2014;27:1047–53.
Herman WH, Eastman RC. The effects of treatment on the direct cost of diabetes. Diabetes Care. 1998;21(Suppl 3):19–24.
Arredondo A. Out-of-pocket costs to users: medicine options for hypertension. Am J Hypertension. 2008;21:443.
Murray A. Chap. 2: Statistical modelling and statistical inference: measurement error in the explanatory variables. Box-Jenkins technique. In: Statistical modelling in GLIM. 3rd ed. New York: Oxford Science Publications, Ox. Uni. Press; 2005. p. 112–32.
Barceló A, Aedo C, Rajpathak S, Robles S. The cost of diabetes in Latin America and the Caribbean. Bull World Health Organ. 2003;81:19–27.
Banco de México, editor. Indice Nacional de Precios por Servicios Médicos en México. Cuadernos Mensuales, Base 1998=100. La Actividad Económica en México. 1983–2012. Gerencia de Investigación Económica. México, DF: Banco de México Ed; 2016. p. 46–68.
Arredondo A. Changing paradigms and challenges: evidence from epidemiological and economic burden of diabetes in Latin America. Diabet Med. 2017;34(7):1009–10.
American Diabetes Association. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26:917–32.
Zhang P, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res. 2010;87:293–301.
Bommer C, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5(6):423–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendix 1. Model Format to Determine Production Costs by Diabetes Case Management
Appendix 1. Model Format to Determine Production Costs by Diabetes Case Management
Institution -------------------------------------------------------- Production function ------------------------------------------------------------
Type of input | Measure unit | Unit cost | Quantity by case management | Average cost | Equation of depreciation | Total cost |
|---|---|---|---|---|---|---|
Human resources | ||||||
Equipment and furniture | ||||||
Drugs | ||||||
Diagnostic studies, etc. Infrastructure Maintenance services General services Total cost |
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Arredondo, A., Orozco, E., Duarte, M.B., Cuadra, S.M., Recamán, A.L., Azar, A. (2019). Economic Costs, from Individuals to Health Systems: Evidence from a Middle-Income Country. In: Rodriguez-Saldana, J. (eds) The Diabetes Textbook. Springer, Cham. https://doi.org/10.1007/978-3-030-11815-0_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-11815-0_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-11814-3
Online ISBN: 978-3-030-11815-0
eBook Packages: MedicineMedicine (R0)