Abstract
Diphtheria, tetanus and pertussis represent an ongoing health threat across the world, and long-term immune protection does not exist for these diseases. Tetanus is the only non-communicable vaccine-preventable disease (VPD). It occurs mainly in older patients, during the warmer months when outdoor activity is higher, and its current epidemiology in Europe may be explained by lack of vaccination or waning immunity. Despite the low number of cases, tetanus is severe with high mortality, and thus, maintaining high vaccination coverage is important. Diphtheria is a potentially acute disease caused by exotoxin-producing Corynebacterium diphtheriae. It is affected by waning immunity, although the majority of reported cases are in unvaccinated adults or those with unknown vaccination status. It is therefore important to maintain high coverage rates as immunisation is the only effective method of preventing this toxin-mediated disease. Particular attention should also be given to revaccination of healthcare and social workers due to waning immunity. Finally, pertussis continues to represent a major cause of death in infants worldwide despite high vaccination coverage, whereas the clinical presentation of pertussis in adolescents and adults can be mild and often goes unrecognised. Indeed, reported pertussis incidence has increased markedly in recent years in almost all European countries, despite sustained high vaccine coverage, again highlighting the effect of waning vaccine immunity. Outbreaks in areas of high vaccination coverage highlight that vaccination strategies may need to be revisited and that consideration should be given to adolescent and adult boosters.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Lifelong immunisation is key, since it promotes the prevention of infectious diseases across the whole lifetime, with the benefits of vaccination accessible at all ages. Vaccinating children and adolescents is an investment in the future, while productivity can be enhanced by vaccinating working-age adults. Vaccination over the life course, and particularly for older adults, makes it possible to maximise the contribution of older adults to society and to the economy and also helps to ensure the sustainability of healthcare systems by reducing the burden of vaccine-preventable diseases (VPDs).
There is strong political leadership on vaccination in Europe, and the life-course approach to vaccination is moving towards concrete actions at the level of the European Union (EU). At the level of the individual EU member countries, there is also good political intent, although concrete implementation varies on the ground. Italy is a good example of vaccination policy, with a lifetime immunisation schedule approved by several scientific societies. It includes all vaccines in every age class. This is a good example of how the issue of life-course vaccination could be approached.
The analysis of available epidemiological data, not only in Italy but also at the international level, has demonstrated the impact of the immunisation interventions adopted over the years. Irrespective of whether the desired levels of coverage are achieved, each vaccine intervention modifies the epidemiology of the various diseases with a reduction in morbidity and generally a lower spreading of the corresponding infectious agents. Booster vaccines are important in this regard, in particular when the duration of protection provided by the disease or immunisation is not long lasting, and the use of vaccination has made it possible to eliminate or reduce natural boosters. Thus, waning immunity can make successfully immunised subjects become exposed to a new risk of acquiring the infection and/or the disease and transmitting it to others.
Our goals today in terms of vaccination are not only to consolidate the successes already achieved in the past but also to evaluate the consequences of the immunological pressure exerted by vaccination on the pathogens and to guarantee long-term protection.
Diphtheria, tetanus and pertussis are each examples of an ongoing health threat across the world. The question is does long-term immune protection exist for these diseases? Unfortunately, the answer is a resounding no, for all three diseases, where waning immunity is an important issue. Have we achieved a decrease of natural boosters? This question is not applicable for tetanus, because this agent is widespread everywhere, but for diphtheria and pertussis, the answer is definitely yes.
Besides, even if diphtheria has been eliminated, the reintroduction of the pathogen is still possible.
14.1 Tetanus
Tetanus is the only non-communicable VPD, so the concept of herd immunity is not applicable in this context. Data from the World Health Organization (WHO) estimate that the coverage rate with three doses of the combined diphtheria, tetanus and pertussis vaccine (DTP3) is around 86%. In 2011, it was estimated that there were over 70,000 deaths in children under 5 years of age, and in 2015 around 10,000 cases were reported. Tetanus occurs mainly in older patients, during the warmer months when outdoor activity is higher, and its current epidemiology in the EU may be explained by lack of vaccination or waning immunity. Tetanus notification in the EU is low, thanks to high coverage rates, and the number of cases is on the decline, with most occurring in the elderly. Despite the low number of cases, tetanus is severe with high mortality, and thus, maintaining high vaccination coverage is important. It also continues to pose a risk to unvaccinated people, so there is a need to implement catch-up and booster strategies, especially in areas where disease rates are highest.
14.2 Diphtheria
Diphtheria is a potentially acute disease caused by exotoxin-producing Corynebacterium diphtheriae. Morbidity and mortality result from the bacterial toxin that may cause obstructive pseudomembranes in the upper respiratory tract (croup) or damage to the myocardium and other tissues. Devastating diphtheria epidemics affecting mainly children have been described from many countries throughout history. 2015 global figures from the WHO reported 4530 cases, with an estimated DTP3 coverage of 86% and 28% of countries reaching >80% coverage in all districts.
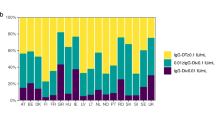
Diphtheria is affected by waning immunity, although the majority of reported cases are in unvaccinated adults or those with unknown vaccination status. It is therefore important to maintain high coverage rates. Diphtheria is a good example of how the epidemiology of a disease can be modified using vaccination. Seroprevalence in the pre-immunisation era was increasing with ageing as a consequence of natural infection and reached a plateau in adolescents and young adults due to natural boosters; in the post-immunisation era, seroprevalence is high after the completion of the vaccinal schedule in newborns but tends to decline, because of waning immunity and reduced natural boosters. The diphtheria vaccine effectively protects against the effects of the exotoxin produced by the pathogen, and immunisation is the only effective method of preventing the toxin-mediated disease. Since reported vaccine coverage is high in Europe, the probability of a widespread outbreak is low, but sporadic cases may continue to occur in unvaccinated or partially vaccinated individuals.
In terms of public health implications, enhanced diphtheria surveillance with high data completeness is warranted. Maintaining high vaccination coverage in the population is critical, and measures should be taken to improve vaccination coverage rates in under-vaccinated populations and certain risk groups (e.g. travellers planning to go to endemic areas and contacts of unvaccinated travellers returning from endemic areas, overcrowded closed groups of people under poor hygienic conditions, unvaccinated clusters and the elderly). Particular attention should also be given to revaccination of healthcare and social workers due to waning immunity, and revaccination of adult population against diphtheria every 10 years might be considered, as is currently the policy in some European countries.
14.3 Pertussis
Pertussis continues to represent a major cause of death in infants worldwide despite high vaccination coverage. Indeed, WHO figures reported 63,000 pertussis-related deaths in children aged <5 years in 2013 and over 140,000 cases across all age groups in 2015. Stratification of cases by age shows that it is not just a paediatric disease but primarily affects <1 year of age infants as well as children and adolescents up to 20 years of age. The clinical presentation of pertussis in adolescents and adults can be mild and often goes unrecognised. This poses an obvious risk of transmission to infants who are too young to have completed the primary pertussis vaccination series.
After a dramatic decline in the reported incidence of pertussis following the introduction of pertussis vaccines into national immunisation programmes some 50 years ago, reported pertussis incidence has increased markedly in recent years in almost all EU/EEA member states, as well as in other parts of the world. This increase has occurred despite sustained high vaccination coverage, highlighting the impact of waning vaccine immunity, while changes in circulating strains may also play a role. In addition, problems such as atypical forms, under-reporting, and under-diagnosis or missed diagnosis mean that figures are likely underestimated. Pertussis is the least well-controlled of all VPDs in Europe, and challenges remain to maintain high coverage and curb the resurgence of the disease. High vaccination coverage must be maintained to ensure direct protection of infants and young children, the two groups which tend to show the most severe symptoms.
Outbreaks in areas of high vaccination coverage highlight that vaccination strategies may need to be revisited and that consideration should be given to adolescent and adult boosters. Some member states have already included some of these policies in their national immunisation schedule, with strategies that include vaccination of newborns, pre-school children, adolescents, adults, healthcare workers, child-care workers, pregnant woman or application of a cocoon strategy. An overall, integrated approach is required to ensure maximum efficacy.
In summary, the distinction between vaccination schedules for children, adolescents, adults and elderly is outdated, and we now need to think in terms of lifelong immunisation. Taking into account tetanus, diphtheria and pertussis, we must consolidate successes achieved heretofore and take into consideration the outcomes of the immunological pressure exerted on pathogens and the issue of waning immunity. Boosters make it possible to guarantee protection over time of already successfully immunised subjects who are exposed anew to the risk of acquiring and/or transmitting infections.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gabutti, G. (2019). Ongoing Threats for Older Europeans: Diphtheria, Pertussis and Tetanus. In: Michel, JP., Maggi, S. (eds) Adult Vaccinations. Practical Issues in Geriatrics. Springer, Cham. https://doi.org/10.1007/978-3-030-05159-4_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-05159-4_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-05158-7
Online ISBN: 978-3-030-05159-4
eBook Packages: MedicineMedicine (R0)