Abstract
Given the poor outcome of subarachnoid hemorrhage due to rupture of intracranial aneurysms (IAs) and high prevalence of IAs in general public, elucidation of mechanisms underlying the pathogenesis of the disease and development of effective treatment are mandatory for social health. Recent experimental findings have revealed the crucial contribution of macrophage-mediated chronic inflammation to and greatly promoted our understanding of the pathogenesis. Also a series of studies have proposed the potential of anti-inflammatory drugs as therapeutic ones. In this process, a rodent model of IAs plays an indispensable role. Basic concept of IA induction in such kind of models is that IA formation is triggered by hemodynamic stress loaded on damaged arterial walls. To be more precise, although detailed procedures are different among researchers, animals are subjected to a ligation of a unilateral carotid artery and systemic hypertension achieved by a salt overloading, and IAs are induced at the contralateral bifurcation site. Importantly, trigger of IA formation in the model mimics human one, and IA lesions induced share similarity in histology with human ones such as degenerative changes of media. For further elucidating the pathogenesis, we need to well understand variations, usefulness, and also limits of this model.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Intracranial aneurysm
- Subarachnoid hemorrhage
- Hemodynamic stress
- Chronic inflammation
- Macrophage
- Animal model
Introduction
Given the poor outcome of subarachnoid hemorrhage due to rupture of intracranial aneurysm (IA) once after the onset and high prevalence of IAs in general public [10, 15] , development of preemptive medical treatment for IAs, incidentally found through a brain check or so, is mandatory for social health [4] . To achieve this goal, mechanisms underlying the pathogenesis of IAs should be well understood. In this process, rodent models of IAs have greatly contributed to the conceptualization of IAs as a macrophage-mediated chronic inflammatory disease affecting cerebral arteries and also to the identification of therapeutic targets for IAs.
Animal Model of IAs
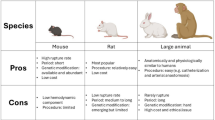
To clarify the pathogenesis of IAs, an animal model in which IA lesion is induced by biological processes well-mimicking human pathology is essential. Dr. Nobuo Hashimoto established the IA model in rats in accordance with such a requirement first at 1978 [8], and this kind of model has been used for about 40 years as a major one in the field. The basic concept to induce IAs in this model (the Hashimoto model) is “loading hemodynamic stress to damaged arterial walls” via referencing the putative trigger, hemodynamic stress, and histological characteristics, i.e., degenerative changes of media and disruption of internal elastic lamina, of human IAs. To achieve this concept, β-aminopropionitrile (BAPN) [14] , a selective inhibitor of lysyl oxidase which mediates cross-linking of collagen and elastin, is administered to rats to fragile arterial walls, and the ligation of a unilateral common carotid artery (Figs. 1 and 2) and the uninephrectomy and administration of sodium chloride and deoxycorticosterone acetate were applied to alternate and increase hemodynamic stress to bifurcation sites of cerebral arteries [8] . After reported in 1978 [8] , this model has underwent modifications [1, 3, 11, 13] (Table 1) and also applied to other experimental animal species like mouse [12] and monkey [9] .
Schematic drawing of the vasculature from carotid artery to the circle of Willis. Points of an arterial ligation to alternate circulatory dynamics in the circle of Willis are indicated as 1 (common carotid artery), 2 (external carotid artery) or 3 (pterygopalatine artery). Red arrows indicate alternation or increase of blood flow. CCA common carotid artery, ICA internal carotid artery, ECA external carotid artery, PPA pterygopalatine artery, MCA middle cerebral artery, ACA anterior cerebral artery, OA olfactory artery, PCA posterior cerebral artery, Acom anterior communicating artery, Pcom posterior communicating artery, BA basilar artery, VA vertebral artery
Magnetic resonance angiography (MRA) imaging of the circle of Willis before and after a ligation of a unilateral common carotid artery. Representative MRA images from a sham-treated (Pre-Ligation, the left panel) or surgically manipulated rat (Post-Ligation, the right panel) are shown. Noted the remarkable change of signal intensity and the tortuous change in the anterior circulation in response to a ligation of a left common carotid artery. Lt left side, ICA internal carotid artery, MCA middle cerebral artery, ACA anterior cerebral artery, OA olfactory artery, BA basilar artery
This kind of IA model shares common pathological features with human ones such as disruption of internal elastic lamina and degenerative changes of media (Fig. 3a). Importantly, IA lesions are spontaneously induced due to increase of hemodynamic stress loaded on bifurcation sites without direct handling of cerebral arteries, making lesions mimicking human pathology more precisely and analysis and interpretation much easier. Furthermore, incidence of IAs in rat model is high, almost 100% at the anterior cerebral—olfactory artery bifurcation in our current model [1] (Table 1), enough to examine mechanisms underlying formation and progression of IAs. Indeed, this model has greatly contributed to conceptualization of IAs as a macrophage-mediated chronic inflammatory disease and successfully identified some therapeutic targets [1, 2, 18] (Table 2). In addition to high incidence, IA is gradually enlarged and degeneration of media such as a loss of medial smooth muscle cells is also gradually exacerbated within a small deviation after the induction. Thereby, IAs with a specific stage can be selectively analyzed, i.e., effect of interventional drugs on initiation, degeneration of media, or size of IAs. In some derivative models from the original Hashimoto model, subarachnoid hemorrhage occurs at a relatively high rate, at around 50%, during experimental period [11] (Table 1, Fig. 3b). Thus, effect of interventional drugs or genetic modification on rupture of IAs may be assessable. Also, mechanisms triggering rupture of IAs which still remain elusive can be addressed.
Histopathological examination of intracranial aneurysm lesions induced in rats and onset of subarachnoid hemorrhage in a rat model. (a) Disruption of internal elastic lamina and thinning of medial smooth muscle cell layer in the intracranial lesion induced in a rat model. Images after Elastica van Gieson staining (left and middle panels) to visualize internal elastic lamina and of immunostaining for alpha-smooth muscle actin to visualize medial smooth muscle cells (right panels) from control arterial walls (lower panels) or aneurysm lesions at an anterior cerebral (ACA)—olfactory (OA) bifurcation site of a rat model (upper panels) are shown. Magnified images corresponding to the square in left panels are shown in middle panels. Arrow heads indicate disrupted portion of internal elastic lamina. Bar, 10 μm. (b) Macroscopic view of brain surface and the circle of Willis from autopsy after onset of subarachnoid hemorrhage in rats. ICA internal carotid artery, MCA middle cerebral artery
Special Insight in Some Modifiable Factors
BAPN
As BAPN inhibits cross-linking of collagens and elastin through irreversibly inhibiting enzymatic activity of lysyl oxidase [14] , this compound induces fragility of arterial walls and thus facilitates degenerative changes and resultant IA progression. Thereby, addition of BAPN to chow or drinking water greatly contributes to reduction of experimental period and may be helpful to make animal experiments like an evaluation of suppressive effect of drugs on progression of IAs easier and less expensive. However, as BAPN interferes a turnover of extracellular matrix which presumably occurs during IA progression to counteract to excessive degeneration of media, careful considerations to the usage of BAPN and if used cautious interpretations should be paid especially when researchers aim to examine something related with extracellular matrix.
Strains
Incidence of subarachnoid hemorrhage has the great difference in races, i.e., over three times higher in Japanese and Finnish although incidence of IAs is similar [7, 10, 15, 17] . In rats, the similar difference of incidence and progression of IAs among strains such as Sprague-Dawley (SD) rat, Lewis (Lew) rat, and Long-Evans rat is observed. SD rats, presumably the most popular rat strain used for creating the Hashimoto model (Table 1), develop larger IAs with more degenerative changes. Careful examination of differences in IA progression among each rat strain may reveal some important insights regarding mechanisms regulating progression or rupture of IAs.
Ligation of Pterygopalatine Artery
In the Hashimoto model , IAs are induced by an increase of hemodynamic stress loaded on bifurcation sites of cerebral arteries. In this process, a unilateral ligation of a common carotid artery is applied to increase blood flow in a contralateral carotid artery (Figs. 1 and 2). In addition of a ligation of common carotid artery, a ligation of a contralateral external carotid artery of course further increases a blood flow in an internal carotid artery. Intriguingly, as recently reported, in rodents unlike primates, a pterygopalatine artery is branched as a most proximal branch of an internal carotid artery, and thus a ligation of this artery moreover increases a hemodynamic stress presumably resulting in the exacerbation of IA progression [5, 11] (Fig. 1).
Limitations
As described above, the Hashimoto model has greatly contributed to our understanding of the pathogenesis underlying IA formation and progression, and thus its establishment is really a breakthrough in the field. However, there are of course some limitations in the Hashimoto model we should well recognize. First, size of IAs induced in this model is small, usually within 0.1 mm in diameter. As a natural consequence, imaging of a lesion is quite challenging given the resolution of imaging modalities used for analysis such as MRA (Fig. 2) and CTA, making the sequential following up of a same lesion quite difficult. Second, IAs induced in the Hashimoto model usually have a broad neck unlike many human ones (Fig. 3a). Thence, hemodynamic status of IA lesions seems to be considerable different from human ones. Taken together with the small size for imaging, the Hashimoto model may not be suitable for computational flow dynamic (CFD) analysis to evaluate hemodynamic status regulating IA progression.
Although there are certainly some limitations about the Hashimoto model, this model has revealed many important insights regarding the pathogenesis of IAs [2, 6, 16] .
References
Aoki T, Frosen J, Fukuda M, Bando K, Shioi G, Tsuji K, Ollikainen E, Nozaki K, Laakkonen J, Narumiya S. Prostaglandin E2-EP2-NF-kappaB signaling in macrophages as a potential therapeutic target for intracranial aneurysms. Sci Signal. 2017;10.
Aoki T, Nishimura M. Targeting chronic inflammation in cerebral aneurysms: focusing on NF-kappaB as a putative target of medical therapy. Expert Opin Ther Targets. 2010;14:265–73.
Aoki T, Nishimura M. The development and the use of experimental animal models to study the underlying mechanisms of CA formation. J Biomed Biotechnol. 2011;2011:535921.
Aoki T, Nozaki K. Preemptive medicine for cerebral aneurysms. Neurol Med Chir. 2016;56:552–68.
Cai J, He C, Yuan F, Chen L, Ling F. A novel haemodynamic cerebral aneurysm model of rats with normal blood pressure. J Clin Neurosci. 2012;19:135–8.
Fukuda M, Aoki T. Molecular basis for intracranial aneurysm formation. Acta Neurochir Suppl. 2015;120:13–5.
Greving JP, Wermer MJ, Brown RD Jr, Morita A, Juvela S, Yonekura M, Ishibashi T, Torner JC, Nakayama T, Rinkel GJ, Algra A. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol. 2014;13:59–66.
Hashimoto N, Handa H, Hazama F. Experimentally induced cerebral aneurysms in rats. Surg Neurol. 1978;10:3–8.
Hashimoto N, Kim C, Kikuchi H, Kojima M, Kang Y, Hazama F. Experimental induction of cerebral aneurysms in monkeys. J Neurosurg. 1987;67:903–5.
Iwamoto H, Kiyohara Y, Fujishima M, Kato I, Nakayama K, Sueishi K, Tsuneyoshi M. Prevalence of intracranial saccular aneurysms in a Japanese community based on a consecutive autopsy series during a 30-year observation period. The Hisayama study. Stroke. 1999;30:1390–5.
Miyamoto T, Kung DK, Kitazato KT, Yagi K, Shimada K, Tada Y, Korai M, Kurashiki Y, Kinouchi T, Kanematsu Y, Satomi J, Hashimoto T, Nagahiro S. Site-specific elevation of interleukin-1beta and matrix metalloproteinase-9 in the Willis circle by hemodynamic changes is associated with rupture in a novel rat cerebral aneurysm model. J Cereb Blood Flow Metab. 2017;37:2795–805.
Morimoto M, Miyamoto S, Mizoguchi A, Kume N, Kita T, Hashimoto N. Mouse model of cerebral aneurysm: experimental induction by renal hypertension and local hemodynamic changes. Stroke. 2002;33:1911–5.
Nagata I, Handa H, Hashimoto N, Hazama F. Experimentally induced cerebral aneurysms in rats: part VI. Hypertension. Surg Neurol. 1980;14:477–9.
Narayanan AS, Siegel RC, Martin GR. On the inhibition of lysyl oxidase by-aminopropionitrile. Biochem Biophys Res Commun. 1972;46:745–51.
Rinkel GJ, Djibuti M, Algra A, van Gijn J. Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke. 1998;29:251–6.
Turjman AS, Turjman F, Edelman ER. Role of fluid dynamics and inflammation in intracranial aneurysm formation. Circulation. 2014;129:373–82.
Wermer MJ, van der Schaaf IC, Algra A, Rinkel GJ. Risk of rupture of unruptured intracranial aneurysms in relation to patient and aneurysm characteristics: an updated meta-analysis. Stroke. 2007;38:1404–10.
Yamamoto R, Aoki T, Koseki H, Fukuda M, Hirose J, Tsuji K, Takizawa K, Nakamura S, Miyata H, Hamakawa N, Kasuya H, Nozaki K, Hirayama Y, Aramori I, Narumiya S. A sphingosine-1-phosphate receptor type 1 agonist, ASP4058, suppresses intracranial aneurysm through promoting endothelial integrity and blocking macrophage transmigration. Br J Pharmacol. 2017;174:2085–101.
Acknowledgment
The authors express their sincere gratitude to all the researchers, assistants, secretaries, and grants supporting their research works.
Conflict of Interest: The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Aoki, T., Miyata, H., Abekura, Y., Koseki, H., Shimizu, K. (2020). Rat Model of Intracranial Aneurysm: Variations, Usefulness, and Limitations of the Hashimoto Model. In: Martin, R., Boling, W., Chen, G., Zhang, J. (eds) Subarachnoid Hemorrhage. Acta Neurochirurgica Supplement, vol 127. Springer, Cham. https://doi.org/10.1007/978-3-030-04615-6_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-04615-6_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04614-9
Online ISBN: 978-3-030-04615-6
eBook Packages: MedicineMedicine (R0)