Abstract
In the first part of this chapter, the principal characteristics of electroencephalographic (EEG) signals (morphology, amplitude, location, rhythmicity, symmetry, etc.) and the wide spectrum of EEG frequencies, grouped in bands, are described. In the second part, the physiological rhythms and the normal graphoelements of the waking adult EEG are detailed, with particular reference to the alpha and mu rhythms. Finally, the intra- and interindividual variability, the aging effects on EEG and the concept of EEG normality are briefly discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 General Characteristics of the EEG Signals
In order to properly describe the various components of an EEG recording and to subsequently determine whether it can be classified as normal or abnormal, the first step is the detailed recognition of the isolated or repeated EEG waveforms. The main features used to describe EEG signals are principally the wave shape (morphology), the voltage (amplitude), the frequency of repetition, the spatial distribution (localization), and the modality of appearance (rhythmicity, continuity, synchrony, symmetry). These EEG features vary with age, mental state, consciousness level and individual characteristics also in physiological conditions and, therefore, these factors have to be taken into account to define an EEG as normal or abnormal.
EEG waveforms can be defined as “slow” or “sharp/spiky” on the basis of their shape or morphology (Fig. 9.1a). Slow signals are represented by rounded waveforms with a long duration in milliseconds (ms). The duration of a signal is considered as the time between the beginning of the signal and the end of a single wave or a complex of waves.
If the shape of the slow signals is particularly regular, these are defined as “monomorphic”; on the other hand, if irregularities are observed on the rounded shape, these are called “polymorphic.”
The “sharp” or “spiky” signals have a shorter duration in time. The spiky transients have various characteristics and they are pathological in relation to epileptic syndromes. However, certain sharp graphoelements can be observed also in healthy subjects, particularly in drowsiness and in sleep.
The morphology of an EEG signal is then described by the phase, which is defined from the point at which the signal leaves the isoelectric line to the point where it returns to the baseline. Depending on how many phases a signal presents, it will be classified as monophasic, biphasic, triphasic and polyphasic (Fig. 9.1b).
Transient or repeated EEG signals may occur apparently simultaneously in two or more locations of the one or both hemispheres: this EEG feature is described as synchronous. When there is a time difference between the appearance of signals in various channels, the EEG feature is - on the contrary - described as asynchronous. Sometimes, there is a short time difference between two or more deflections. However, since subtle asynchronies may also be of clinical relevance, asynchrony can be clearly demonstrated either by expanding the time scale or by using special measurement techniques.
The amplitude of an EEG signal (expressed in microvolts, μV) is also important for its characterization, from a morphological point of view. The amplitude of a wave is measured by evaluating the height of the wave, assessed in mm measured peak-to-peak, and multiplying it by the sensitivity of the amplifier, thus obtaining a value in μV/mm. The amplitude depends on various factors (i.e., location and derivation of electrodes) and the visual assessment of amplitude of EEG phenomenon in mm/μV can be very arbitrary. The exact measurement of the amplitude of an EEG signal should be performed using a special cursor at various epochs of the tracing, where the EEG phenomenon is clearly present.
When comparing the signals amplitude obtained in two or more channels of an hemisphere with those recorded from the same regions of the contralateral hemisphere, we must also describe the symmetry/asymmetry of the signals. An EEG transient - or rhythm - is symmetric when it has more or less the same amplitude in the two or more channels compared. On the contrary, an EEG phenomenon is asymmetric when its peak-to-peak amplitude is significantly lower - or higher - than that of the contralateral side.
Finally, an EEG phenomenon must be described according to the number of times that waveforms repeat themselves over a 1-s period. This characteristic is defined the frequency of the EEG signals and it is usually measured in Hertz (Hz). The frequency is the most important parameter for characterizing the ongoing EEG activities and the physiological rhythms.
Figure 9.2 schematically describes the amplitude and the frequency characteristics of different EEG signals repeating in form of rhythms.
A fundamental parameter for characterizing an EEG pattern is the recognition of its spatial representation in the scalp. For the spatial localization of EEG transients, it is fundamental to know the electrode positions and the derivations. An EEG signal is defined as focal when it is present on a single area of a cerebral hemisphere and as multifocal if it is present on different areas of a hemisphere or of both hemispheres, but asynchronously. The waveforms can be instead defined as diffuse or generalized when synchronous in all brain areas of both the hemispheres (Fig. 9.3).
Some rhythmic activities are characteristically located in specific regions of the scalp (alpha rhythm, mu rhythm, sleep spindles, etc.) and for the description it is important to define their localization, in addition to their frequency and symmetry.
A sporadic single EEG signal, clearly distinguished from the background activity, is defined as a “transient”. A stereotyped succession of two or more EEG signals represents instead a “complex”, that may be isolated or - more frequently - organized in sequences (ongoing activity). The EEG transient event and/or complexes are apparently spontaneous, or evoked by intrinsic or extrinsic stimuli. Both the transient signals and the complexes may have recurred over time at periodic or quasi-periodic intervals (continuity). These features are typical of many pathological EEG patterns and will then be described later.
2 EEG Frequencies
The wide spectrum of EEG frequencies are grouped in bands and historically named using the Greek letters. EEG activity recorded at the scalp with routine EEG instruments usually exclude the frequencies below 0.5–0.3 Hz and normally do not exceed 30 Hz. The classical frequency bands of EEG are defined as follows (Fig. 9.4):
-
Delta (δ): 0.1 to <4 Hz
-
Theta (θ): 4 to <8 Hz
-
Alpha (α): 8 to <13 Hz
-
Beta (β): > 13–30 Hz
The delta band was first described by Walter in 1936 [1] as an EEG marker for cerebral tumors and it includes the slowest EEG frequencies (<4 Hz); these can often be confused on visual inspection with artifactual oscillations and then improperly “cutted” by technicians with high-pass filters. The visual analysis of the physiological awake adult EEG is not always able to highlight the effective amount of the delta component which is masked by the other frequencies, or represents electrical artifacts. The quantitative frequency analysis of EEG tracings usually shows, also in adults, the presence of an appreciable amount of delta power. Currently, however, there is great interest in ultraslow components (0–0.3 Hz) which are termed Direct Current (DC) potentials and represent shifts of the baseline. The identification and characterization of ultraslow activity play no significant role in the clinical EEG, but they have a great interest in various experimental fields (e.g., for the study of immature cortical activity, the identification of epileptogenic zone, the relation with cortical spreading depression in migraine attacks, etc.) [2].
The theta band (4.0 to <8.0 Hz) should be divided into theta 1 (theta slower: 4.0 to <6.0 Hz) and theta 2 (theta faster: >6.0 to <8.0 Hz). Even the term “theta band” was first introduced by Walter, in 1944 [3], associated with the presence of thalamic tumors (he had chosen theta to stand for thalamus because he presumed these waves had a thalamic origin). In normal adult subjects, the theta band is poorly represented but its incidence is variable, dependent on age, individual characteristics, level of vigilance, etc. The appearance of anterior theta activity in adults can be facilitated by a particular emotional states or mental processes of problem-solving. Furthermore, when a gradual disappearance of the alpha rhythm substituted by theta activity is observed in an EEG tracing of an awake adult, this means that the subject is sleepy. Sometimes, it is difficult to attribute a physiological or pathological significance to theta activity registered in an awake adult and the decision can only be facilitated by careful assessment of the specific situation.
The alpha band (8.0 to <13 Hz) is proper for an EEG tracing registered in adults during quiet wakefulness with eyes closed. The term alpha was introduced by Berger in 1929 [4] and this frequency band is characteristic of the physiological alpha rhythm that will be described subsequently in detail.
Even within this frequency band, we can distinguish slow alpha (8.0–9.0 Hz), intermediate alpha (9.0–11 Hz) and fast alpha (11 to <13 Hz).
The beta band includes the frequencies between 13 and 30 Hz; it was first named by Berger [4]. In the experimental psychophysiologic literature, this frequency band is divided into beta 1 (13 to <20 Hz) and beta 2 (>20 to 30 Hz). A beta activity of low amplitude (<30 μV) is normally recorded over the fronto-centro-temporal regions in awake EEG of normal adults. It is sometimes more appreciable with open eyes or mental activity because, with closed eyes, it is masked by the much higher amplitude and synchronization of the alpha rhythm. The beta activity is related to mental and cognitive processes of various types, anxiety and state of alert; it is also induced or increased by drowsiness and light sleep. Furthermore, numerous drugs (barbiturates, benzodiazepines, neuroleptics, antihistamines, amphetamines, cocaine, etc.) are potent beta-activators. During the recording of a routine EEG, the anterior beta activity arising from the brain can be confused with electrical activity generate by the muscles (“muscle artifact”) and, therefore, suppressed by the technician with specific filters.
Currently, there is a great scientific interest in more rapid EEG frequency bands that are not detectable during the recording of a traditional EEG, but can be recorded with modern digital equipments. The frequencies above the beta band are traditionally defined gamma band (γ, 30–80 Hz). Successively, Curio [5] has been proposed by the following designations for the ultrafast activity: omega band (ω, 80–120 Hz), rho band (ρ, 120–500 Hz), and sigma band (σ, 500–1000 Hz). In epilepsy, experimental studies over the past decade have focused particularly on interictal High-Frequency Oscillations (HFOs) >80 Hz that seems to be promising new biomarkers in epilesy. HFOs are defined as spontaneous EEG events consisting of at least four oscillations (ripples) that clearly stand out from the background activity. HFOs are subdivided into ripples (80 to 250 Hz), fast ripples (250–500 Hz), and ultrafast ripples (>500 Hz). The ripples can be recorded by MagnetoElectroencephaloGraphy (MEG) and EEG with automatic detection methods, whereas fast and ultrafast ripples can be recorded only with intracranial EEG methods. The principal clinical application of HFOs was in the context of epilepsy surgery, followed by the assessment of epilepsy severity and monitoring of drugs response [6, 7]. Several artifacts, due to muscle contractions, movements or bad electrode contacts, should be distinguished from epileptic HFOs. The HFOs appear also to be correlated with both cognitive and perceptual-motor processes.
Including the ultraslow and ultrafast frequencies, recordable EEG frequencies with the current technology can be classified as shown in Table 9.1.
3 The Physiological Rhythms and Normal Graphoelements
3.1 Alpha Rhythm
First described by Berger in 1929 [4, 8], the alpha rhythm (or posterior dominant rhythm) is the hallmark of the awake EEG in older children and adults, with eyes closed or visually inattentive and during the psychosensorial relaxed condition [9]. The alpha rhythm has a typical location in the posterior head regions; in some subjects, the alpha rhythm is strictly confined to the occipital areas, but in others it also spreads forward to all the posterior quadrants (posterior temporal, parietal, and occipital regions). Sometimes, the posterior rhythm may even spread to the central and frontal areas (F4 and F3 electrodes), mainly in aged subjects or during drowsiness (Figs. 9.5 and 9.6).
An example of alpha rhythm in an awake adult subject with eyes closed. The tract delimited by the dotted lines shows a background alpha rhythm with a frequency of 10 Hz and with a peak of amplitude of 55 μV/cm. Alpha rhythm is typically visible on the posterior regions with a regular and sinusoidal morphology
Even the subjects blind from birth have an alpha rhythm localized in parieto-occipital areas, but the rhythm has a significant reduction of power in the blind when compared to the normally-sighted controls [10]. The morphology of alpha rhythm is mostly regular (monomorphic rhythm) with sinusoidal or fusiform shape (increase and gradual decrease in amplitude, “waxing and waning”; peaks and troughs of the waveform rounded and regular). Rarely, the alpha rhythm has a sharpened morphology (“spiky alpha,” with the negative sharp component of wave and the positive rounded component) and it is considered a normal variant, especially in older children and in young adults.
The alpha rhythm has a frequency within the range of alpha band (8 to <13 Hz), generally ranging from 9 to 11 Hz in adults. The frequency is usually the same in both hemispheres but, in the same individual, it may vary in terms of 1 or even 2 Hz. Some frequency variations of the alpha rhythm may be dependent on menstrual cycle (acceleration of alpha frequency in the premenstrual phase with reduction of its amount) [11] or be related to body temperature (higher frequencies during temperature increase) [12, 13].
Recently, it has been demonstrated that the posterior alpha rhythm is significantly slower in adult patients in the wake periods of sleep recordings (before and after sleep), compared to standard wake recordings [14].
Brief faster than baseline alpha rhythm sequences can also be recorded immediately after eyes closing (squeak phenomenon) (Fig. 9.7) [15].
Sometimes, the normal sequences of alpha rhythm are substituted by slower or faster frequencies (slow or fast alpha variants) [9, 16]. The term “slow alpha variant” is referred to the appearance of a subharmonic of the fundamental rhythm (with a ratio of 1:2 or 1:3; if, e.g., the alpha rhythm has a frequency of 12 Hz, its slow variants will have a frequency of 6 or 4 Hz, respectively) (Fig. 9.8) [17].
The alpha slow variants have the same topography and reactivity as the fundamental rhythm, but they can also be unilateral or asymmetric. More rarely, the appearance of fast variants of alpha can also be observed (16–20 Hz), for the most part endowed with alpha activity and with the same topography and reactivity. The fast variants can be activated by Intermittent Photic Stimulation (IPS) and induced by benzodiazepines.
The amplitude of posterior alpha rhythm in most adults is less than 50 μV. In order to be able to measure the amplitude in an objective manner, a digital measurement cursor must be used, checking the amplitude values randomly at various points in the tracing and then calculating a mean value. This procedure is difficult to implement during a routine EEG inspection and, therefore, visual assessment of the alpha activity amplitude can be very arbitrary; it is then preferable to make subjective quantification of the amplitude in terms of low, medium, and high. Usually, the amplitude of posterior alpha rhythm is asymmetrical on the two hemispheres, with a lower voltage in the dominant hemisphere (the left in right-handed individuals and the right in the left-handed) [18]. However, the difference in the posterior alpha rhythm amplitude between the two hemispheres usually does not exceed 20%. An asymmetry of posterior alpha rhythm is considered to be abnormal when, in the non-dominant hemisphere, its amplitude is more than threefold greater than that of the dominant hemisphere. On the other hand, when the voltage of the alpha rhythm is higher in the dominant hemisphere, the difference is considered abnormal if the amplitude is twofold higher, compared to contralateral side. Differences of amplitude less than 50% are not, however, considered to be pathological (Fig. 9.9).
The reason why the amplitude of the alpha rhythm is higher in the posterior regions of the non-dominant hemisphere is not actually well known. To explain this phenomenon, we still refer to the theory that the cortical EEG signals are always of higher amplitude in brain areas that are not too much involved in mental processes [18]. However, it is probable that the mild interhemispheric asymmetry of the alpha rhythm does not depend on hemispheric dominance, but is to be related to differences in skull thickness [19].
There are also normal EEG tracings in which the alpha activity is poorly appreciable (low amplitude or desynchronized tracings). In these cases, the desynchronization of background activity is often correlated to the state of anxiety for the examination or due to the characteristic of the subject, or it is dependent on the non-relaxing registration environment (Fig. 9.10) [16].
In addition to the frequency, the localization and the amplitude, the other fundamental characteristic of the posterior alpha rhythm is its peculiar reactivity. This physiological posterior rhythm, very well synchronized with closed eyes and in a relaxed state of wakefulness, suppresses dramatically when the eyes are opened and/or during heightened mental activity (such as arithmetic calculation), somatosensory stimuli, etc. This phenomenon is called the “blocking arrest of alpha,” discovered in his first report by Berger [4]: during EEG recording with eyes closed it is usually observed in the synchronized alpha rhythm that disappears immediately as the technician asks the subject to open his eyes or to perform specific mental tasks. However, it must be emphasized that sensory stimulation and mental activity block the alpha rhythm in less pronouncedly than the opening of the eyes [20]. Sometimes, blocking reactivity is only partial and with open eyes an alpha rhythm, poorly modulated, persists (Fig. 9.11).
On the other hand, the blocking reactivity of alpha rhythm is defined as “paradoxical” when, in subjects with eyes closed, a background activity of theta frequency, often related to drowsiness, prevails; the command to open eyes determines, as awakening reaction, the reappearance of alpha rhythm absent before.
3.1.1 Genesis of the Alpha Rhythm
The majority of authors who have studied the genesis of the alpha rhythm have established that it is a rhythm of cortical origin, but with an important thalamic influence. Bishop, in 1936, first proposed the concept of corticothalamic reverberating circuits, a concept that was later reaffirmed by many others [21]. Andersen and Andersson, in 1968, [22] proposed the theory of the thalamic pacemaker, based on similarities between human alpha activity and experimental spindle activity induced in animals by barbiturates. According to this theory, the alpha rhythm is generated on the basis of rhythmic inputs that originate from the thalamic centers. These inputs, through specific thalamocortical fibers, activate the upper cortical centers, inducing their synchronization. This type of thalamocortical excitation would also involve the activation of inhibitory interneurons, acting only at the level of the thalamic circuits. Therefore, according to this theory, an alternation of excitation/inhibition is then determined in the thalamus, which would be at the basis of the synchronization and the rhythmicity of the cortical activity.
In recent decades, the genesis of the alpha rhythm has not been further clarified and demonstrated. From both clinical and experimental data, it can be assumed that cortical alpha rhythm is the result of cortico-cortical and thalamocortical systems, interacting with each other in very complex way [23].
The neurophysiological mechanisms underlying the reactivity of the alpha rhythm (i.e., the blocking of alpha with eyes open or during mental activities) are also not well elucidated, but it is supposed that, in the desynchronization of the tracing, a fundamental role of the ponto-mesencephalic reticular formation, through its activating action toward the cerebral cortex, is involved.
3.2 Mu Rhythm (μ)
Described for the first time by Gastaut in 1952 [24], the mu rhythm (also known by discouraged terms such as rhythm en arceau, comb rhythm, rolandic rhythm, wicket rhythm and somatosensory alpha rhythm) [9, 18] is characterized by brief and/or prolonged rhythmic sequences of waves with the frequency similar to that of an alpha posterior rhythm, but with a different location and reactivity. The most typical frequency of the mu rhythm fluctuates from 7 to 11 Hz and it is often mixed with beta activity. This rhythm is typically observed in wakefulness, but it can also be observed in stages N1, N2, and R of sleep. The amplitude of the mu rhythm is generally less than 50 μV (usually lower than the amplitude of the alpha rhythm) and its maximum spatial representation is in the central regions of scalp (below the C4, C3, and Cz electrodes). The waves which constitute the mu rhythm are arciform (with sharpened negative phase and rounded positive phase) and they appear either at eyes opened or closed, in subjects with motor inactivity (Fig. 9.12) [12].
The prevalence of the mu rhythm reported in the literature during the registration of EEGs in healthy subjects or patients is very variable with values of 10–20% in young adults and with a lower incidence in children and the elderly. Probably, the prevalence of mu rhythm is higher; as a matter of fact, during closed-eye recordings, the mu rhythm can be confused with the alpha rhythm transmitted into the central regions. In addition, during routine EEG recordings, the traits of tracings performed at eyes open are very short and, therefore, the mu rhythm may not be highlighted. With more sophisticated quantitative EEG analysis, the mu rhythm in almost all healthy adult subjects may be highlighted [12, 18, 19].
The mu rhythm may be unilateral or bilateral, asynchronous and/or asymmetrical in the two hemispheres, with no particular correlation with the hemispheric dominance. Isolated reports have suggested that a unilateral mu rhythm can be associated with a structural ipsilateral cortical lesion, even in the absence of additional EEG abnormalities [25].
The most important peculiarity of the mu rhythm is its reactivity. The mu rhythm is indeed blocked by movements (active, passive, or reflex), by the tactile stimulation of body areas, or even by mental movement planning. If the mu rhythm is well evident only from one side, the best manoeuver to visualize its reactivity is to ask the subject to tighten the contralateral hand or think about performing this action (Fig. 9.13).
The proof that thinking to perform a movement is sufficient to block the mu rhythm is shown by the fact that the rhythm stops a few millisecond before the beginning of the voluntary movement itself [26]. In addition, even subjects with an amputated limb show this reactivity of the contralateral mu rhythm after thinking about the execution of the movement in the phantom limb [27].
Finally, it was noted that the mu rhythm is enhanced or sometimes facilitated by Intermittent Photic Stimulation (IPS) and pattern vision, validating the idea that, for this rhythm, the integration of sensory and visual function is relevant [12].
The mu rhythm in the scalp central areas was correlated with the beta activity (around 20 Hz) described in the motor cortex in patients during electrocorticographic recording. Also this activity could be blocked by contralateral movement or with thinking about the execution of movement [28].
Although the mu rhythm is present in a high percentage of healthy subjects and it represents a physiological normal EEG pattern, in the past it has often been attributed to a pathological significance, or interpreted as a “borderline pattern.”
One of the historical theories on the genesis of the mu rhythm was in fact that it was an expression of hyper-excitability of the rolandic cortex.
More recent studies have instead proposed to interpret the mu rhythm as an important information processing function that connects the perception with the action; specifically, it would be the expression of the processes involved in the transformation of “seeing” and “hearing” into “doing.” [29]
Table 9.2 and Fig. 9.14 summarize and compare the fundamental characteristics of the alpha rhythm and the mu rhythm.
3.3 Breach Rhythm
Breach Rhythm (BR) consists of focal sequences of rhythmic or pseudorhythmic mixed activity (theta, alpha and beta), sometimes associated with focal slowing or sharp activity, or isolated spikes. The breach rhythm develops over - or near - the area of bone skull defects, such as after craniotomy for neurosurgery or traumatic lesions, and it is not indicative of brain dysfunctions [9, 30, 31]. The breach rhythm may be considered as a consequence of the skull defect and not as an epileptiform abnormality (Figs. 9.15 and 9.16).
The genesis of BR is not fully understood, but the bone defects cause a reduced filtering effect and reduced electrical impedances. Sharpening and irregular morphology of BR may be misinterpreted, leading to a misdiagnosis of epilepsy. Therefore, a correct differential diagnosis is important for the relevant clinical consequences [32]. BR occurs in wakefulness, but it may persist also during sleep. If located in the central regions, it may be blocked by contralateral movements, because of the coexistence of an underlying mu rhythm, but this reactivity is not observed in the temporal region.
3.4 Lambda Waves
Lambda (λ) waves are physiological sharp waves occurring during visual scanning in awake subjects [9]. Their prevalence has been reported to vary between 2% and 88%, with the highest occurrence in children and in young adults [33]. They appear in occipital regions, with minimal spread to parietal and posterior temporal areas. The lambda waves morphology is biphasic or triphasic and the most prominent phase is positive. Their amplitude is usually low (20–40 μV), their duration between 200 and 300 ms, and their frequency of repetition is at intervals from 200 to 500 ms. They are mostly bilateral, synchronous and symmetrical, but they may also be unilateral or otherwise asymmetrical (Fig. 9.17).
Lambda waves are best elicited when the subject visually scans a textured or a complex picture, in a well-lit laboratory; they are closely correlated with fast saccadic eye movements (saccadic movement means the eye movement in space exploration, rapid and unconscious, followed by a fixation pause). Lambda waves appear after a saccadic movement with a latency of 70–80 ms. The disappearance of lambda waves is obtained with closing the eyes, the decrease of the ambient lighting level, or by placing a completely white sheet of paper in front of the eyes of the subject (fixation off). Therefore, from a neurophysiological point of view, lambda waves represent a sort of visual evoked responses and they are the expression of oculomotor and visual integration.
According to Billings [34] there are two different types of lambda waves. The first type would be generated by the faster conducting fibers of the optic nerve (Y-type fibers), immediately after the primary saccadic movement. The second type would be instead related to the visual impulses coming through the slower optical fibers (X-type fibers), with return to central vision during or slightly before the locking phase of the secondary corrective saccadic movement.
Recently, Alvarez et al. [35] studied the occurrence of lambda waves in adult outpatients, during prolonged EEG monitoring for unclear diagnosis of epilepsy. Lambda waves were found in 32% of prolonged recordings, mainly during watching TV, in relation to normal EEGs. Furthermore, all recordings with lambda waves also had Positive Occipital Sharp Transients of Sleep (POSTS) (Fig. 9.18).
This study showed that watching TV likely represents a powerful stimulus for lambda waves appearance and confirms the physiological benign nature of this EEG pattern. Finally, the lambda waves are of principal interest for the study of the visual system and should not be misinterpreted as epileptiform abnormalities.
4 Intraindividual and Interindividual Variability of the Normal Awake Adult EEG
The EEG of a single subject may present variations both during a specific recording session, as well as in separate recordings over time. This intraindividual variability is due to several factors, endogenous (arousal or drowsiness, anxiety, mental activity, blood sugar level, body temperature, etc.) or exogenous (laboratory lighting level and temperature, noise, etc.).
However, the changes in background activity observed in the same individual during a recording session depend mainly on the modifications in the alert level. As a matter of fact, if you can maintain in the same subject the same level of alertness and the same environmental conditions, there is a good correlation between seriated EEG tracings performed at different times (intraindividual stability of EEG).
EEG intraindividual differences have been reported also in women in relation to the various ovulatory and menstrual phases. Summarizing, in preovulatory and premenstrual phases substantially, it has been observed an increase in alpha frequency and beta power; in postovulatory and menstrual phase, instead, the alpha rhythm decreases in frequency, and the absolute power of theta and alpha activity increases, while the beta power decreases [11, 12].
The interindividual EEG variations, usually in the alpha rhythm, seem to be correlated with individual characteristics (personality, intellectual level, gender, genetic factors, etc.) [36].
As regard to the gender, some very old studies reported a more symmetric distribution of alpha frequency and also a higher beta amplitudes in females. However, other authors have successively found that the alpha rhythm is better represented in males than in females [37] or that there is no correlation between the EEG and sex of the subjects [38]. These discordant reports probably depend on dissimilar - and not comparable - experimental methods in EEG studies.
5 Age Effect on the EEG of Wakefulness
The characteristics of neonatal EEG are treated in detail in Chap. 11.
In the first few years of life (1–3), the awake EEG is dominated by diffuse slow delta-theta activity, with high amplitude. This slow activity gradually tends to become rhythmic and with a prevalence in the central and parietal regions. In particular, from 3 to 12 months of life, the posterior background activity - considered a precursor of the subsequent alpha rhythm - has a frequency of about 4 Hz, is quite rhythmic, and is partially reactive to the opening-closing of the eyes. In the 2nd year of life, this activity reaches the frequency of about 6–7 Hz and in the third year of age it is around 7–8 Hz, with a more evident reactivity. From the 3rd year of age, therefore, an immature alpha rhythm, with low frequency and partial posterior localization, is already recognizable. The mid-posterior background activity at this age is of high amplitude and mixed with slower rhythms at 2–5 Hz.
From 3 to 5 years of age, the posterior rhythm is maintained at a frequency around 8 Hz, interrupted at intervals by 1.5–4 Hz sequences, and the tracing shows abundant theta activity in anterior regions and/or diffuse, at 5–7 Hz. Hyper Ventilation (HV, activation procedure that can be tested in laboratory with a good cooperation already from 3 to 4 years) shows mostly a widespread, hypersynchronous, wide-voltage slow activity; a photic driving response, particularly at low frequencies, is observed during the Intermittent Photic Stimulation (IPS).
From 6 to 12–15 years, the alpha rhythm progressively reaches the frequency of about 10 Hz, although it is always of high amplitude and mixed with slower theta activity (“posterior slow waves of youth”); sometimes, this theta activity, confined in temporal posterior regions, is rhythmic and at subharmonic alpha frequency (slow alpha variant) (Figs. 9.19 and 9.20).
From 12 to 15 years onward, EEG acquires progressively all the characteristics of the adult, both in basal and during activation tests, with final mature pattern at around 18–20 years. In the EEG maturative process, however, the interindividual variability must always be taken into great consideration, since it has a decisive influence on when a mature waking EEG pattern can be achieved [39,40,41,42,43].
From about 20 years, the physiological awake EEG maintains stable characteristics. From the age of 50 onward, a slight increase in theta activity and/or a slight decline in alpha frequency may begin to appear, although consistent with a normal EEG for age. According to some authors, the alpha rhythm slows down by 0.08 Hz per year from the age of 60, but this fact has not been confirmed by others [44,45,46]. A more recent review by Rossini et al. [47] describe resting EEG changes across physiological aging, with gradual amplitude decrease of alpha rhythm and a global slowing of the background activity. However, an alpha rhythm at a frequency of 7.5–8 Hz in subjects over 80 years can be considered completely normal. Furthermore, in the elderly, the posterior physiological rhythm is of lower amplitude and tends to spread to the anterior regions (Figs. 9.21 and 9.22). Frequently, the slow alpha variants are also observed in the posterior regions.
In subjects over the age of 60, theta activity is frequently observed in temporal regions, mainly in the left side; this slow activity is considered physiological if it does not exceed 10–15% of the total registration period. HV increases slow activity and IPS less frequently induces posterior photic driving responses. In conclusion, however, even during aging, the interindividual variability of EEG must be taken into account; in fact, 90-year-olds or even centenarians can still present an alpha rhythm at a frequency of 9–10 Hz.
6 The Concept of Normality of EEG
First of all, it must be premised that the interpretation of an EEG is always subjective and that it can be influenced by multiple factors, mainly dependent on the experience of the technologists and of the clinical neurophysiologists. If the technician has not been able to recognize and eliminate from the recording an artefactual activity that can be easily mistaken for pathological changes, this can obviously lead to misinterpretations. It is also very important that the technician assesses the level of awareness of the patient during the recording session: focal and/or diffuse slowings may depend on variations in the subject’s state of arousal or attention, which could also lead to incorrect interpretation of the tracing. In a routine EEG laboratory, the tracings should always be accompanied by an anamnestic data sheet containing complete information on the patient, from the personal data to the more specific clinical ones. Even if it is a laboratory test, the EEG must be interpreted in light of the patient’s age, their clinical history, the reasons for the request, any pharmacological therapies, etc. Given that the tracing has been acquired correctly by technicians and that it is accompanied by all the necessary information, the interpretation of the EEG recording as normal or abnormal depends on the clinical neurophysiologist, who will prepare a report based on his theoretical preparation and on his practical experience. The theoretical knowledge of clinical EEG is obviously indispensable and it would be preferable that those who dedicate themselves to the reporting of EEG examinations are specialized in Clinical Neurophysiology or have attended at least specific residential courses. The theoretical preparation, however, has very little value if not accompanied by extensive experience in EEG, which should be certified only after a large number of tracings actually evaluated under supervision. It is well known that routine EEGs are frequently misinterpreted by neurologists without neurophysiology fellowship training (as the majority of neurologists interpreting EEG are). Misinterpretation of routine EEGs leads to the misdiagnosis of epilepsy and the inappropriate use of antiepileptic drugs, as well as to an inadequate diagnosis and treatment of non-epileptic seizures [32, 48]. Only with appropriate practical experience will neurologists be able to correctly differentiate a normal EEG recording from an abnormal one, taking into account that there are unusual and/or borderline patterns and that what can be considered “normal” for an individual is not necessarily for another. In general, however, for a correct interpretation of EEGs, it is essential that there is a continuous exchange of information between the technician and neurophysiologist and that the technician participates directly, where possible, in the reporting phase. Equally important is that the neurophysiologist does not get stuck in his position and that he is also able to acquire an EEG independently. In the initial training periods, all medical doctors interested in electroencephalography should spend a period in a laboratory, in close contact with the patient, the technician and the equipment. We must never forget that a normal EEG in basal conditions could become pathological during activation tests and that they must be performed according to correct and universally accepted criteria. However, activation tests can sometimes highlight EEG modifications with respect to the baseline tracing which, although they are completely physiological for that subject or that situation, can be instead interpreted as abnormal and, therefore, as pathological. Equally, it is sometimes necessary to repeat the EEG recording because, in some pathologies, seriated tracings have a higher probability of highlighting pathological changes: so it is not universal that a first EEG considered normal may not be followed by successive registrations with clear abnormalities. When you are not sure that a certain pattern is normal or pathological, it is always advisable to repeat the EEG recording, with the perspective that the repetition of a diagnostic exam is always better than an incorrect report. It can also happen that the neurophysiologist is so uncertain in the assessment of an EEG that they request the opinion of a second expert; in this case it is better that the second evaluation is carried out blindly, without knowing the clinical data. Subsequently, the two experts can cooperate together an electro-clinical correlation and reach a shared EEG report.
However, the variability of interindividual assessment is notable [49]. A recent study of Halford et al. [50] has shown that interrater agreement among academic neurophysiologists in epileptiform transients identification varies considerably and that the American Board of Clinical Neurophysiology certification is associated with improved performance.
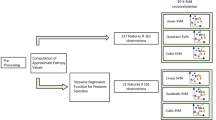
To overcome the problem of interindividual evaluation variability of EEG features, there is a need to find a computerized tools to improve the quality of EEG assessment and reporting in clinical practice and to improve education in EEG [51].
Finally, there is the possibility of referring to specific automated software for objective EEG evaluations (computerized signal analysis, brain mapping, automatic detection of epileptiform transients, etc.). How these methods are useful in clinical practice to a better discern, compared to the visual inspection, between normal and abnormal EEGs, is questionable. With these devices, it will be easier to characterize and quantify some EEG parameters, but current abnormality detection softwares have an insufficient sensitivity requiring, however, a neurophysiologist to examine each EEG.
References
Walter WG. The location of cerebral tumours by electroencephalography. Lancet. 1936;II:305–8.
Vanhatalo S, Voipio J, Kaila K. Infraslow EEG activity. In: Schomer DL, Lopes da Silva FH, editors. Electroencephalography. Basic principles, clinical applications, and related fields. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 741–8.
Walter WG, Dovey VJ. Electroencephalography in cases of subcortical tumours. J Neurol Neurosurg Psychiatry. 1944;7:57–65.
Berger H. Uber das Elektrenkephalogramm des Menschen. Arch Psychiatr Nervenkr. 1929;87:527–70.
Curio G. Ultrafast EEG activities. In: Niedermeyer E, Lopes Da Silva F, editors. Electroencephalography. Basic principles, clinical applications, and related fields. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 495–504.
Frauscher B, Bartolomei F, Kobayashi K, et al. High frequency oscillations: the state of clinical research. Epilepsia. 2017;58:1316–29.
Zijmans M, Worrell GA, Dumpelmann M, et al. How to record high-frequency oscillations in epilepsy: a practical guideline. Epilepsia. 2017;58:495–504.
Adrian ED, Mathews BHC. The Berger rhythm: potential changes from the occipital lobes in man. Brain. 1934;57:355–85.
Kane N, Acharya J, Benickzy S, et al. A revised glossary of terms most commonly used by clinical electroencephalographers and updated proposal for the report format of the EEG findings. Clin Neurophysiol Pract. 2017;2:170–85.
Kriegseis A, Henninhausen E, Rosler F, Roder B. Reduced EEG alpha activity over parieto-occipital brain areas in congenitally blind adults. Clin Neurophysiol. 2006;117:1560–73.
Harding GFA. Thompson CRS. EEG rhythms and the internal milieu. In: Remond A, editor. Handbook of electroencephalography and clinical neurophysiology, vol. 6A. Amsterdam: Elsevier; 1976. p. 176–94.
Chang BS, Schomer DL, Niedermeyer E. Normal EEG and sleep: adults and elderly. In: Schomer DL, Lopes da Silva FH, editors. Electroencephalography. Basic principles, clinical applications, and related fields. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 183–214.
Tatum WO IV. Normal adult EEG. In: Ebersole JS, editor. Current practice of clinical electroencephalography. 4th ed. Philadelphia: Wolters Kluwer Health; 2014. p. 90–124.
Meritam P, Gardella E, Alving J, et al. Diagnostic yield of standard-wake and sleep EEG recordings. Clin Neurophysiol. 2018;129:713–6.
Stom van Leeuwen W, Bekkering DH. Some results obtained with the EEG-spectrograph. Electroencephalogr Clin Neurophysiol. 1958;10:563–70.
Cooper R, Binnie C, Billings R. Techniques in clinical neurophysiology. EEG phenomenology. Amsterdam: Elsevier; 2003. p. 169–221.
Kuhlo W. Slow posterior activities. In: Chatrian GE, Lairy GC, editors. The EEG of waking adult. Handbook of electroencephalography and clinical neurophysiology, vol. 6A. Amsterdam: Elsevier; 1976. p. 89–104.
Libenson MH. Visual analysis of the EEG: wakefulness, drowsiness and sleep. In: Libenson MH, editor. Practical approach to electroencephalography. Philadelphia: Saunders Elsevier; 2010. p. 5–30.
Krishnan V, Chang BS, Schomer DL. Normal EEG in wakefulness and sleep: adults. and elderly. In: Schomer DL, Lopes da Silva FH, editors. Neidermeyer’s electroencephalography. Basic principles, clinical applications, and related fields. Oxford: Oxford University Press; 2018. p. 202–28.
Niedermeyer E, Krauss GL, Peyser CE. The electroencephalogram and mental activation. Clin Electroencephalogr. 1989;20:215–26.
Bishop GH. The interpretation of cortical potentials. Cold Spring Harb Symp Quant Biol. 1936;4:305–19.
Andersen P, Andersson SA. Physiological basis of the alpha rhythm, Neuroscience series, vol. 1. New York: Appleton Century Crofts; 1968: 235p.
Steriade M, Gloor P, Llinas RR, et al. Basic mechanisms of cerebral rhythmic activities. Electroencephalogr Clin Neurophysiol. 1990;76:481–508.
Gastaut H. Etude électrocorticographique de la réactivité des rythmes rolandiques. Rev Neurol. 1952;87:176–82.
Yamak R, Beydoun AA, Dirani MM, et al. Unilateral mu rhythm and associated cortical lesions on brain MRI. J Clin Neurophysiol. 2017;34:144–50.
Chatrian GE. The mu rhythm. In: Remond A, editor. Handbook of electroencephalography and clinical neurophysiology, vol. 6. Amsterdam: Elsevier; 1976. p. 46–69.
Gastaut H, Naquet R, Gastaut Y. A study of the mu rhythm in subjects lacking one or more limbs. Electroencephalogr Clin Neurophysiol. 1965;18:720–1.
Jasper HH, Penfield W. Electrocorticograms in man: effects of voluntary movement upon the electrical activity of the precentral gyrus. Arch Psychiatr Nervenkr. 1949;183:163–74.
Pineda JA. The functional significance of mu rhythms: translating “seing” and “hearing” into “doing”. Brain Res Rev. 2005;50:57–68.
Cobb WA, Guiloff RJ, Cast J. Breach rhythm: the EEG related to skull defects. Electroencephalogr Clin Neurophysiol. 1979;47:251–71.
Brigo F, Cicero R, Fiaschi A, Bongiovanni LG. The breach rhythm. Clin Neurophysiol. 2011;122:2116–20.
Benbadis SR, Tatum WO. Overinterpretation of EEGs and misdiagnosis of epilepsy. J Clin Neurophysiol. 2003;20:42–4.
Chatrian GE. The lambda waves. In: Remond A, editor. Handbook of electroencephalography and clinical neurophysiology, vol. 6A. Amsterdam: Elsevier; 1976. p. 123–49.
Billings RJ. The origin of the occipital lambda wave in man. Electroencephalogr Clin Neurophysiol. 1989;72:95–113.
Alvarez V, Maeder-Ingvar M, Rossetti A. Watching television: a previously unrecognized powerful trigger of lambda waves. J Clin Neurophysiol. 2011;28:400–3.
Shaw JC. The Brain’s alpha rhythms and the mind. Amsterdam: Elsevier; 2003.
Matsuura M, Yamamoto K, Fukuzawa H, et al. Age development and sex differences of various EEG elements in healthy children and adults. Electroencephalogr Clin Neurophysiol. 1985;60:394–406.
Ehlers CL, Kupfer DJ, Buysse DJ, et al. The Pittsburgh study of normal EEG sleep in young adults: focus on the relationship between waking and sleeping EEG spectral patterns. Electroencephalogr Clin Neurophysiol. 1998;106:199–205.
Petersen I, Eeg-Olofsson O. The development of the electroencephalogram in normal children from the age of 1 through 15 years. Neuropediatrie. 1971;2:247–304.
Eeg-Olofsson O, Petersen I, Selden U. The development of the electroencephalogram in normal children from the age of 1 through 15 years. Paroxysmal activity. Neuropaediatrie. 1971;2:375–404.
Eeg-Olofson. The development of the electroencephalogram in normal adolescents from the age of 16 through 21 years. Neuropaediatrie. 1971;3:11–45.
Duffy FH, Albert MS, McAnuty G, Garvey AJ. Age-related differences in brain electrical activity of healthy subjects. Ann Neurol. 1984;16:430–8.
Marcuse LV, Schneider M, Mortati KA, et al. Quantitative analysis of the posterior-dominant rhythm in healthy adolescents. Clin Neurophysiol. 2008;119:1778–81.
Wang HS, Busse EW. EEG of healthy old persons. A longitudinal study. I. Dominant background activity and occipital rhythm. J Gerontol. 1969;24:419–26.
Giaquinto S, Nolfe G. The EEG in the normal elderly: a contribution to the interpretation of aging and dementia. Electroencephalogr Clin Neurophysiol. 1986;63:540–6.
Klass DW, Brenner RP. Electroencephalography of the elderly. J Clin Neurophysiol. 1995;12:116–31.
Rossini PM, Rossi S, Babiloni C, et al. Clinical neurophysiology of aging brain: from normal aging to neurodegeneration. Prog Neurobiol. 2007;83:375–400.
Benbadis SR. Errors in EEGs and the misdiagnosis of epilepsy: importance, causes, consequences, and proposed remedies. Epilepsy Behav. 2007;11:257–62.
Williams GW, Luders HO, Brickner A, et al. Interobserver variability in EEG interpretation. Neurology. 1985;35:1714–9.
Halford JJ, Arain A, Kalamangalam GP, et al. Characteristics of EEG interpreters associated with higher interrater agreement. J Clin Neurophysiol. 2017;34:168–73.
Beniczky S, Aurlien H, Brogger JC, et al. Standardized computer-based organized reporting of EEG: SCORE—second version. Clin Neurophysiol. 2017;128:2334–46.
Acknowledgment
I am grateful to neurophysiologist Dr Patrizia Pulitano for her help in selecting and editing the EEG figures and to neurologist Dr Edoardo Vicenzini in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mecarelli, O. (2019). Normal Awake Adult EEG. In: Mecarelli, O. (eds) Clinical Electroencephalography. Springer, Cham. https://doi.org/10.1007/978-3-030-04573-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-04573-9_9
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04572-2
Online ISBN: 978-3-030-04573-9
eBook Packages: MedicineMedicine (R0)