Abstract
Aim of this chapter is to provide technicians and physicians basic information about EEG laboratory organization and the modalities of electrode placement and of EEG standard recording. A synthetic part is also dedicated to patients management in the event of an epileptic seizure during the EEG recording. Finally, the opportunity to create a computer-EEG network for data transmission and communication by digital EEG is described.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Patient care
- Electrode placement
- Seizure recording
- Computer-EEG network
- Maintenance of wakefulness test
- Multiple sleep latency test
1 Environment, Patient Care, and Recording Preparation
Before each recording session, the EEG technician must check that all the necessary equipment is available and fully functional. The laboratory room must be tidy and cozy, and it should also be equipped with toys to amuse children or anything that can help to recreate the conditions triggering a seizure (television, food, etc.). If it is necessary to administer medications or to analyze the online tracings, the neurologist must be alerted.
To ensure an accurate and reliable recording, the technician should read the examination request form from the referring physician before admitting the patient, and he should also view eventual previous EEG exams. This will support the examination and planning the monitoring of specific polygraphic parameters that can supply useful additional information. The technician also has the task to collect all the information regarding the patient: complete personal data (first and last name, gender, date of birth, address, handedness); the reasons for the referral and relevant medical and neurological history, particularly concerning epileptic seizure details (type of seizure, time elapsed since the last seizure, triggers, etc.); current medications (particularly CNS drugs); information on other diseases that can require the exam limitation; the presence and location of any skull defects; previous EEG results (if available); neuroimaging results (computed tomography and/or magnetic resonance imaging).
Digital EEG systems allow the recording and storing of all of these informations as a separate text file or in the same file as the EEG data, and the technician must be sure that the information about the patient are correctly related to the recording. The neurophysiologist can then review all the patient’s clinical data, which will help him to interpret the results of the EEG recording.
An accurate preliminary explanation of the procedure to the patient is essential: what for us is a simple routine procedure may instead be cause of concern for the patient. Many people still falsely believe that electricity flows between the system and the patient’s head during the exam. In the collective imaginary, EEG is still sometimes associated with a kind of electroshock or, at any rate, to an examination that is capable of revealing mental processes. Explanation of the procedure must be of course adjusted to the patient’s comprehension ability, but it is usually useful to point out that EEG is a harmless, diagnostic and not a therapeutic exam, through which the spontaneous electric activity of the brain is recorded and during which no electricity is absolutely administered. This approach is helpful because it facilitates the patient’s relaxation, and it ensures better cooperation. Moreover, excessive anxiety can cause muscle and movement artifacts that disturb the recording, and an anxious subject will unlikely reach the necessary state of relaxation or even drowsiness, during which significant diagnostic abnormalities are more likely to arise.
After the complete and accurate explanation from the technician, the patient (or the person accompanying them) should sign an informed consent form, in particular when specific procedures carry the risk of triggering a seizure.
The same technician should carry out the entire recording; a production-line approach that involves application of electrodes and recording by different technicians is not good practice. During the EEG recording, the technical staff must not express opinions on the exam nor on other matters, and it is important to avoid unnecessary entry or exit in and out the recording room.
Recordings on young children or non-cooperating adults may present additional difficulties. The presence of a parent, a nurse, or a therapist who knows the patient well is often useful or even indispensable. On the other hand, experienced technicians can usually recognize those parents who are excessively anxious and who, instead of helping, can be counterproductive. In this case, it’s better to respectfully and gently ask them to leave the room. Examinations on very young children are preferably carried out while a parent is holding them. In these circumstances, especially after a meal, it is easier for them to fall asleep. When carrying out a recording on a non-cooperating subject, the technician must be able to cope with the situation. In these cases, it’s pointless to immediately position the head cap and electrodes, since it is necessary to first establish a physical connection with these patients, trying to get them to feel comfortable with us and with the surrounding environment. For that purpose, books, toys or other objects of interest can be used, in order to distract them from the technical procedure.
The electrodes placement on the scalp should be managed with the patient in a sitting position, accessible from all the sides. Children may be reassured by showing them a simulation of electrode positioning it on the head of a doll or on the back of the technician’s hand. Sometimes, children can be scared by the noise of the air compressors used, in certain laboratories, to attach the electrodes with collodion. In these cases, the use of a hair dryer, an object well-known to children, or of adhesive paste, is recommended.
The time necessary for the electrodes placement is very important, because it gives the technician a chance to obtain the trust of the patient, to verify the contents of the request and to obtain more details on the medical history. During a relaxed conversation with the technician, who is usually less intimidating than a physician, the patient will often spontaneously give important information, not mentioned during the formal interview with the neurologist. Thus, new information obtained should be added to the request form. Moreover, the technician must indicate:
-
conformational cranial abnormalities (which can determine inevitable asymmetries in the electrodes positioning, causing an incorrect interpretation of the EEG);
-
scalp and/or skull defects (burr holes, post-craniotomy scars, etc.) that can preclude the standard positioning of the electrodes or be a cause of peculiar EEG patterns like breach rhythm;
-
patient’s mental state and level of awareness at the beginning of and during the recording;
-
hand preference (which could also explain possible asymmetries).
During a standard EEG execution, the patient should be as relaxed as possible and this can be achieved by letting them lay on a bed in the supine position or sitting on a slightly reclined couch. The room must be dimly lit and as soundproof as possible. During the recording, the technician must be able to always monitor the patient’s behavior. If they’re particularly restless or experiencing a seizure, the use of a mattress on the floor or a hospital bed with cot sides can be required. In this case, continuous surveillance by a nurse or another technician is needed, to avoid dangerous falls. If a patient has physical deficits and arrives on a wheelchair, it would be more appropriate to leave him sitting in the chair during the execution of the exam.
Before the recording starts, the patient must be given the opportunity to use the toilet, so that it is not further needed during the exam. The patient can be asked to take off too tight or heavy items of clothing, to feel more comfortable and to avoid them sweating. In case of a hearing impairment or in foreign patients with language barriers, it may be useful to agree upon a system of signals to request the subject to open and close the eyes and to perform other procedures.
2 Electrode Placement and Control
The impedance of the electrodes must be checked after their placement on the scalp and it should be checked again after the patient is settled on the bed or couch. Modern electroencephalographs always measure impedance values, but this operation can also be carried out with portable instruments (impedance meter). The impedance check system is based on the use of a sinusoidal signal at about 10 Hz, generated by the instrument and transmitted to the electrodes connected to it, with reference to a common electrode. To determine which electrodes have suitable impedance, headboxes are equipped with a LED display, and the same display can be shown on the computer monitor.
Surface electrodes should have an impedance lower than 5 kΩ; with modern digital EEG recording equipments, impedances up to 10 kΩ are acceptable, but it is important that the impedances are balanced. Impedances should also not be below 100 Ω: this value indicates a shunt or short circuit, due to a salt bridge on the scalp [1]. Impedance of small, non-polarizable electrodes (i.e., needle electrodes) is higher than that of cup electrodes, but they are stable and may be used in special situations and for prolonged EEG recordings in comatose patients. In any case, perseverance in the attempt of lowering the impedance to try improve the recording is always beneficial, although this is not always possible, especially with young children and non-cooperating patients.
Electrodes are an essential element of electroencephalography and the technician must check that they are placed correctly and have low impedance. However, in order to lower the impedance, it is not necessary to produce abrasion on the skin. With modern high input impedance amplifiers and accurate digital filters for power line noise (60 or 50 Hz), high-quality EEG can indeed be recorded without skin abrasion [2]. Skin breakdown during placement of electrodes is quite frequent especially in children, and it must be avoided also because it can cause infections [2,3,4]. Electrodes used for EEG recordings must be disinfected with the appropriate procedures, especially when used in patients with contagious diseases. In these cases, however, disposable electrodes are recommended [1, 5].
The electrodes are of various types and they can be applied on the scalp by different methods (see Chap. 3 and 4). The use of collodion is one of the best techniques for securing EEG electrodes to the scalp, especially for long-term monitoring. However, the use of collodion, because of its inflammability and toxicity, requires accurate safety procedures for storage and utilization. Furthermore, the collodion can be removed only with acetone and its inhalation can produce nasal and conjunctival irritation, respiratory effects, nausea and vomiting, etc. When using collodion in the EEG laboratory, a simple vapor extraction system must be operative; nevertheless, collodion is not recommended for short routine recordings. The electrolyte adhesive paste, such as EC2, may substitute collodion in the electrodes placement, also for long-term monitoring, with an optimal cost-benefit ratio (Fig. 7.1) [6].
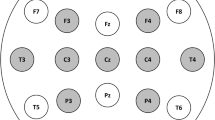
The 10-20 system is the only one officially recommended by the International Federation of Clinical Neurophysiology (IFCN) for the placement of all 21 electrodes [7]. The development of high-density EEG system and source localization methods (which refers to the use of 64–256 electrodes) has subsequently made necessary modifications of this system, and the 10-10 system has been accepted by the American Clinical Neurophysiology Society (ACNS) and IFCN for almost two decades (see Chap. 4) (Fig. 7.2) [8,9,10,11].
In the 10-10 system some electrodes from the 10-20 system were renamed: T3 and T4 were renamed to T7 and T8, and T5 and T6 were renamed to P7 and P8. In 2001, the 10-5 system was introduced [12], but the nomenclature was not yet formally accepted by the ACNS and IFCN. Very recently, the IFCN strongly recommends an array of 25 electrodes for standard EEGs including 6 electrodes of the inferior temporal chain (Fig. 7.3). The standard 10-20 system did not indeed include electrodes to record the activity of the inferior-basal and anterior part of temporal lobe. These electrodes are named, according to 10-10 system, F9-T9-P9 and F10-T10-P10 [11].
New standard montage, with the coverage of the inferior-basal and anterior part of the temporal lobe. From ref. [11], with permission
In conclusion, the 10-20 system is clinically adequate and efficient for routine standard EEG; the 10-10 system should be used in patients undergoing presurgical evaluation in Long-Term Epilepsy Monitoring Unit (LTEMU) or for additional digital analysis (i.e., electrical source imaging). Additional electrodes from the 10-10 system may also be used, sometimes, during standard EEG, especially to make a better localization of an epileptic focus.
For both clinical and educational purposes, it would be desirable to switch to T7/T8 and P7/P8 instead of T3/T4 and T5/T6, but the new terminology must be gradually accepted by the electroencephalographers and the EEG machine headboxes modified. At present, it would be an acceptable alternative to continue using the old terms or both [10]. In children, all 21/25 electrodes recommended for adults should be used [11, 13] even if, in the case of poor compliance or in critically ill children or for prolonged monitoring, the application of a smaller number of electrodes is also acceptable (Fig. 7.4).
Furthermore, in addition to scalp electrodes, it is necessary to apply other electrodes and devices to the record of polygraphic parameters, particularly ElectroCardioGram (ECG, always considered indispensable, in all recordings), ElectroOculoGram (EOG) and ElectroMyoGram (EMG) (see Chap. 15–16).
3 EEG Recording
With older analog systems, the technician had only one opportunity to acquire a satisfactory tracing to be presented to the electroencephalographer compiling the EEG report; all efforts then had to be concentrated toward achieving a sufficiently long and reliable tracing, with a modest quantity of artifacts and with a correct acquisition parameters set up. With digital technology, a wrong choice of online visualization parameters is not a real problem, since EEG can be reformatted and read offline with modified filters, sensitivity and baseline periods. However, if the tracing is not visualized correctly during the acquisition, the risk for the technician is to underestimate important elements and not act accordingly, thus impairing the correct interpretation of the exam.
In many laboratories, technical-methodological aspects are strictly standardized: a sequence of montages, not excluding any applied electrodes, is visualized; opening and closing of the eyes must follow a specific sequence; acoustic and tactile stimuli are regularly administered; photostimulation is carried out following a planned sequence, often automatically programmed, with fixed periods of stimulation and pause.
Sometimes, however, a more flexible approach is necessary. If the EEG duration itself gives an indication of the quality of the work carried out, a better quality indicator is actually represented by the variability of the average duration of the tracing, because it reflects the flexibility of the recording procedure. Although following standard procedures is fundamental, the technician must always consider that each patient is different and that even EEG recordings must have a physiological degree of variability. If the goal is, for example, to verify how the background EEG activity is altered in a disoriented subject, a few minutes of recording can be enough. On the contrary, if a patient with suspected epileptic seizures shows a normal EEG during wakefulness, extending the recording period can be helpful, both to increase the possibility to detect interictal abnormalities and to record under lower alertness conditions. With very young children, the tracings could initially be unreadable, but if the technician is patient, the child will probably fall asleep, allowing a sleep recording without artifacts.
A standard EEG is initially acquired and displayed according to predefined parameters. The sensitivity of EEG equipment is usually set in the range of 50–100 μV/cm of trace deflection [1].
A sensitivity >100 μV/cm does not allow the detection of a significant low amplitude activity, while a sensitivity <50 μV/cm increases excessively the EEG activity and limits the identification of peculiar waveforms or frequencies (Fig. 7.5).
Using digital equipments, the signals are filtered at two levels: the first analog filter is applied at the actual amplifier before digitation and cannot be changed by user; the second digital filter processes only the data for display, and its improper use does not allow the technician to evaluate correctly the recording, without however permanently altering the recorded data. The low-pass filter (High-Frequency Filter, HFF) during standard EEG recording should normally be set at 70 Hz, while the high-pass filter (Low-Frequency Filter, LFF) should be no higher than 1 Hz (corresponding to a time constant with at least 0.1 s for analog systems) (Fig. 7.6).
The increase of LFF should not be used routinely to attenuate slow artifacts, because this can also result in the disappearance of delta pathological activity. On the other hand, the reduction of HFF, to reduce excessive muscular artifacts, can distort and attenuate the sharp abnormalities. Rather than working with filters, the technician should try to prevent eye movements as much as possible and to reduce muscle activity by relaxing the patient and asking him not to contract his facial muscles. LFF can be increased to attenuate the excessive slow activities, clearly artifactual in nature (perspiration, arterial pulse, etc.).
To eliminate fast activities due to electrical interference, a 60 Hz (in North America) or 50 Hz (in Europe) notch filter should be used (Fig. 7.7); a noise source can remain however active, and it must be removed before resorting to the filter, because the presence of a disturbance can denote other technical problems like, for example, disconnection of one electrode. The notch filter should not be routinely used, but its use should be restricted to special environments (i.e., ICU recordings).
The abovementioned settings may need to be modified according to what is being displayed.
Sensitivity must be reduced if the underlying activity is so large that it saturates the channel; on the other hand, it must be increased if the tracing is less evident. However, a judicious use of low- and high-frequency filters, in the end, is advisable to emphasize or clarify specific types of EEG patterns.
Acquisition of EEG data onto a digital storage should occur at the minimum sampling rate of 256 Hz and at the resolution of at least 16 bits [14].
For the storage of various EEG recordings (standard EEG, video-EEG, A-EEG, etc.), it is preferable to use newer storage technologies, in particular digital server systems, which can facilitate review in remote locations and whose data protection with backups is on charge of hospital engineer staff. The EEG data can be reviewed on the computer screen with sufficient temporal and spatial resolution. A standard horizontal scaling should be available, with a minimum resolution of 128 data points/s on the screen for a 10-s page, but more expanded horizontal scales should also be available. A standard vertical scaling with a minimum spacing of 10 mm per channel should be used for a display of up to 21 channels [14].
With analog instruments, the most widely used paper speed was 30 mm/s, but some laboratories also used a paper speed of 15 mm/s or intermediate (20 or 25 mm/s) (Fig. 7.8).
Nowadays, with the use of digital systems and visualization of the EEG tracings on the monitor, it’s easy to change the baseline periods according to the specific needs. Users accustomed to reading the tracing on paper at 30 mm/s will continue to use this setting on the monitor and vice versa. A display of 10–20 s/page (depending on its size) corresponds roughly to a paper speed of 30 mm/s, and it should be used for routine exams. In reality, a flexible method is advised. Sometimes, it will be necessary to compress the recorded EEG tracing, in order to follow an event in its evolution or to evaluate its fluctuations (display of >20 s/page). In other cases, it may be necessary to display a short period of the recording on the monitor; this is useful, for example, to study the morphology of a graphoelement or for its correlation to polygraphic parameters. In any case, the use of nonstandard parameters can be confusing when the tracings, digitally recorded and then printed on paper, are read by physicians with different habits and preparation; for this reason, it is important that each EEG tracing clearly shows the time marker and the acquisition parameters.
Up to 16–18 and more channels can be displayed on the monitor at the same time, both in bipolar (longitudinal and transverse) and in referential derivations. With 21 electrode positions (10-20 system) and 16 channels, the number of possible montages is 21. The 10-10 system, with more than 70 electrode positions, allows the creation of a much larger number of montages [10, 15].
Additional channels must be dedicated to visualizing the polygraphic parameters, basically represented by ECG, EOG, EMG as already stated above.
The duration of standard EEG recordings varies widely among laboratories. European guidelines recommend EEG recordings of at lest 30 min [16]. Results from studies conducted on epileptic patients suggest that in epilepsy-related indications, the shortest duration of standard EEG should be 20 min [17]. Also ACNS has recently established that standard EEG recordings under baseline conditions should consist at least of 20 min of reliable and without artifacts recording, to which activation procedures (intermittent photic stimulation and hyperventilation) must follow [1].
The possibility offered by digital EEG to display many more channels simultaneously and to modify acquisition parameters and montages during review must absolutely not entail a reduction in the recording time. The EEG technician should view the EEG in bipolar (longitudinal and transverse) and referential montages during the recording, both to identify the good connection in all electrodes and to appreciate subtle abnormalities requiring, for example, additional electrode placements.
During EEG recording in basal condition, it is necessary to assess EEG changes corresponding to eye-closed and eye-open conditions, both voluntary and on request. The closing and opening of the eyes induce, respectively, the appearance and block the background alpha rhythm. In the periods immediately after eye closure, short sequences of faster alpha rhythms can appear (squeak phenomenon). Some physiological rhythms or graphoelements (i.e., mu rhythms, lambda waves) are visible only when the opening of eyes has blocked the alpha activity. The spontaneous movements of the eyes may induce artifacts that simulate frontotemporal slow activity and the eyes opening and closing helps to differentiate between pathological and artifactual activity. In addition, epileptic discharges in photosensitive subjects often manifest only in coincidence with eye closure. For all these reasons, during a standard EEG recording, unless we want the patient to fall asleep, eye opening and closing must be tested several times (every 2–3 min); if the subject is not cooperating, the technician must manually perform the opening-closing of the eyes. Finally, the patient’s response to the closing-opening eye command also allows the technician to evaluate the drowsiness and mental status of the subject.
During the EEG recording, the technician must report on the tracing all the significant events that occur, particularly the events disturbing the recording or the maneuvers and stimuli applied to the patient.
After recording under baseline conditions, activation procedures must be carried out, especially hyperventilation and photic stimulation (see Chap. 14) [1]. Execution methods for these tests must always be carefully explained to the patient and caregivers, in order to get them to cooperate and to avoid artifacts. During Hyper Ventilation (HV), the patient must carry out deep breathing, consisting of short but intense inhalations followed by prolonged exhalations, at a higher frequency than normal (normal, 10–12 breaths/min; HV, 18–20 breaths/min), for a period of 3–5 min. During hyperventilation, the patient must try to keep his head as still as possible and the eyes closed; the technician should encourage the patient to perform the test correctly, noting the quality of its effort during HV on EEG recording.
Intermittent Photic Stimulation (IPS) must be carried out before hyperventilation or at least 3 min after its conclusion. Biochemical variations and eventual EEG modifications induced by hyperventilation can indeed be prolonged for a few minutes after its interruption; consequently, performing this test before IPS can be confusing. However, as some patients can only relax after hyperventilation, in these patients it can be done before IPS, waiting a few minutes before testing the photic stimulation. Some children, however, can find photic stimulation amusing and, in these cases, it can be useful to carry it out at the beginning of the recording, to obtain a better cooperation. The correct standard procedure for performing IPS and HV is extensively described in Chap. 14. During the recording, the decision to follow a different procedure can be developed; each patient is an individual and the modality of EEG recording must sometimes be “tailored,” based on questions that the technician can deduce from the request form, previous exams or decision taken together with the doctor. IPS and HV are activation procedures that may show epileptiform interictal abnormalities that potentially may induce epileptic seizure in susceptible patients and both the patient and the caregivers must be informed of this possibility.
In our laboratory, when a clear PhotoParoxysmal Response (PPR) was recorded, the IPS is retested with the use of Z1 blue lenses of an ultraviolet material with an 80% luminance cut. The Z1 lens are indeed highly effective in controlling PPR in a large number of photosensitive patients (Fig. 7.9) [18].
Sleep recording is useful to highlight otherwise non-detectable epileptiform EEG abnormalities, in patients with a clinical history that suggests epileptic seizures. Furthermore, in very young children, sleep recordings can be essential to obtain a tracing without artifacts, as much as possible. In these cases, the recording can be carried out in the laboratory in the early afternoon, possibly shortly after lunch (nap EEG), with one of the parents holding the child who is put to sleep after electrodes application. When the child is asleep and after having verified that the EEG changes distinctive of the first NREM stages are being recorded, acoustic stimuli will have to be administered to elicit physiological graphoelements like K-complexes. Sleep EEG recordings in laboratory on adults can be achieved by putting special care into making the patient as comfortable as possible (have them take off their shoes or any tight items of clothing; supply them with a blanket; allow them to use the toilet before beginning of the acquisition; use cup electrodes or pre-cabled caps; carry out the recording in a dimly lit and soundproof room).
In some patients, EEG is required precisely to assess their state of alertness or the atypical tendency for excessive daytime sleepiness, in a state of psychosensory relaxation.
When a patient who tends to fall asleep needs to be kept awake, acoustic stimuli must be periodically administered, as well as the request to open their eyes. If the awake EEG is needed for quantitative analysis (e.g., to assess the effects of drugs), the patient can be asked to open and close their eyes alternatively every 20–30 s. Tracing epochs of 8–10 s are thus obtained, selected 5 s after each eye opening or closure, discretely stable and reliable for the computer analysis. The patient can also be engaged in mental tasks that favor concentration and retention of alertness, or they can be asked to maintain continuous pressure on a button.
Specific tests to assess alertness and/or the tendency for excessive daytime sleepiness are the Maintenance of Wakefulness Test (MWT) and the Multiple Sleep Latency Test (MSLT).
The MWT measures a patient’s ability to stay awake: the patient should not smoke for at least 30 min before the test and should not have caffeinated beverages after the awakening. Then, after applying the electrodes, he will be placed in a comfortable sitting position in a quiet dimly lit room and he will be instructed to remain awake as long as possible. Four or five polygraphic recordings, each lasting for 40 min (with a 2-h interval between each recording), must be executed, starting 1.5–3 h after waking up. A PolySomnoGraphy (PSG) before MWT is not required. Each recording ends after 40 min if no sleep occurs or after the onset of sleep onset; the sleep onset during MWT is defined as three consecutive epochs of N1 or one epoch of any other sleep stages. Even if there are no universally accepted normative data for the MWT, a mean sleep latency of <8 min is considered abnormal, whereas values of >8 min and <40 min of sleep latency are of uncertain significance.
The MSLT is a better-standardized method for the study of excessive daytime sleepiness. This test must be preceded by a nocturnal PSG and starts 2–3 h after its conclusion. The patient is asked to relax and fall asleep while sitting comfortably on a recliner or lying down on a bed, in a dimly lit quiet room. No sedative or exciting drugs should be taken before the recording. The MSLT consists of four to five nap recordings at 2-h intervals, each recording must last a maximum of 20 min. The patient preparation must include the necessary polygraphic parameters to assess the various sleep stages (EMG, EOG). The evaluated parameters are the mean sleep-onset latency and the occurrence of sleep-onset REMs within the first 15 min of sleep onset. If no sleep occurs, the recording stops after 20 min whereas, if the patient falls asleep, the test is ended 15 min after the first period of 30 s epoch in any stage of sleep. A mean sleep latency <8 min is considered pathological; values between 8 and 10 min are consistent with mild sleepiness and a mean sleep latency of 10–15 min is normal [19].
4 Ictal Event Recordings and EEG report
Clinical ictal events are more often observed by EEG technicians than physicians or any other medical staff. Although the first concern must be the patient’s safety if a sezure would arise during the examination (therefore the first thing to do is ensure that they don’t hurt themselves falling or aptly intervene in the case of suffocation or dangerous behavior), the technician should not interrupt the EEG recording. In fact, the possibility to observe seizures (like those reported on the medical history) and simultaneously record the EEG correlates constitutes a unique opportunity for the diagnostic purposes. Technicians should therefore be prepared for the phenomenology and semeiology of the various epileptic seizures, to better detect and test manifestations that need to be documented. The technician should indeed be able to carry out other actions, such as to test whether the patient is able to respond when questioned (asking him to name objects or to answer simple quesions), to test mucle tone, pupils responsiveness and to examine some reflexes. A European task force from the ILAE has recently developed a standardized ictal testing battery for patient’s testing during seizures [20]. Most of EEG laboratories are now equipped with a video-EEG system and the technician should always be ready to film the patient’s behavior in sync with the EEG recording. Obviously, the video recording does not relieve the technician from carefully observing and testing the patient during a seizure. The Video-EEG recordings can be performed if the patient or the caregivers signed the informed consent according to the institutional policies.
To obtain a reliable and useful ictal EEG recording, the electrodes must be securely placed and resistant to any sudden movements or automatisms. Should the patient have a seizure when the montage is still incomplete, the technician must start the recording as soon as possible, to try collecting as much data as possible, even with an incomplete montage. During a seizure, the technician’s task are: to give assistance to the patient to ensure they do not hurt themselves; to keep the EEG recording going and to prevent detachment of the electrodes (e.g., placing the headbox closer to the patient’s head, thus avoiding that the cables are distracted to any pulling loads); to observe the seizure and to test the patient’s interaction with the environment; to take note, as soon as the circumstances will allow it, of the observed details so that they will not be forgotten or inaccurately reported. EEG technicians should also be able to use (under the doctor’s supervision) suggestion provoking techniques, to induce non-epileptic seizures, to be differentiated from epileptic ones. Video-EEG is, in these cases, also fundamental. The suggestion provoking techniques, in addition to intermittent photic stimulation and hyperventilation, include the compression of body parts, the placing of moistened patches on the skin, verbal stimulation, etc. (Fig. 7.10).
At the end of the recording, the technician should immediately send the EEG recordings to the neurophysiologist with the electrographic or clinical seizures, as well as with other significant clinical events that occurred in the laboratory. In some patients, there may be indeed the need for other diagnostic examinations or acute medications. Some special procedures that may be riskful for the patient should be carried out only in the presence of a qualified physician, with the informed consent, in an environment with adequate resuscitation equipment.
The technician’s abilities to interpret the recorded tracing vary from case to case and from country to country, but they have certainly improved in the last few years. In the USA, several levels of specialization of the neurodiagnostic technologists are identified (please note web site https://www.aset.org). The Canadian Society of Clinical Neurophysiologists recently published a review of the laboratory standards and recommendations for EEG technologists. [21] In Italy, various universities currently operate a 3-year Bachelor Degree Course in Neurophysiopathology Techniques, which can be followed by a Master Degree Course in Diagnostic Techniques, lasting 2 more years. The Italian degree is valid and approved in the European Union; nevertheless, to provide general or specific information regarding the exam report is to-date not considered a technician’s task. The technician must explain the patient that the medical report needs a qualified physician’s expertise and that the results must be assessed and completed with the other clinical data. In many cases, active cooperation between the technician who carried out the EEG and the physician compiling the offline medical report is needed; the correct interpretation of the EEG patterns is often possible with the information provided by the technician.
To conclude, the technician’s responsibility toward the patient does not end until the patient has left the laboratory. In the case of hospitalized patients, it may be necessary to take them back to their ward or ensure that the auxiliary staff or the ambulance takes care for their transportation. In the case of outpatients, it is possible to verify whether an appointment has been fixed with the referring physician. It would be also desirable to organize a neurophysiopathology unit so that the patient can be visited, if necessary, immediately after the EEG execution.
5 Networked EEG Laboratory.
A computer network is a system that allows information to be shared between computers located in different places, even at distance from each other. Networking has revolutionized the computer system, making it possible to move from large powerful but very expensive data processors to a series of independent but interacting computers.
A network topology describes the arrangement of systems on a computer network. It defines how the computers, or nodes, within the network are arranged and connected to each other: the bus or line topology is a network setup in which each computer is connected to the others in a linear way; in the star topology all nodes are individually connected to a central connection point, which functions as a control of the network itself; a ring topology is a network configuration in which device connections create a circular data path, therefore the nodes of the network are joined by point-to-point links in a closed way; in the mesh topology each computer is interconnected with one another, allowing for most transmissions to be distributed, even if one of the connections goes down.
A computer network basically allows:
-
1.
The sharing of resources: if multiple computers are connected to each other, each of them can reach the others’ private resources. The most functional model for communication and use of information is represented by the client/server structure. Various users (clients) can connect to a superior machine (server), which shares programs into the network and can manage the database.
-
2.
Communication between different users: examples of real-time communication possibilities between remote users are represented by chat lines, audio conference and/or teleconference, etc. Thanks to the existence of networks, files can be transferred or copied from one computer to another, databases created and used by many operators; working on a remote computer (virtual terminal) is also possible. The worldwide network connection (Internet) allowed a real revolution in the communications field: e-mails made it possible to exchange correspondence between different users, even when very far away from each other, connected to the same network.
Information on the network can be transmitted mainly through the use of electric cables, optical fibers and radio waves.
Coaxial cables allow little interference and great transmission speed, but they are now disused. Information travels above all through already installed telephone lines. When the transmission passes through the telephone network, the digital signal must be transformed into analog and then digital. This happens inside the modem, a device that allows the circulation of information via the Internet. In reality, the modem modulates and demodulates: inside it there are A/D converters, which convert the data from analog to digital and vice versa. The Integrated Services Digital Network (ISDN) and Asymmetrical Digital Subscriber Line (ADSL) networks, on the other hand, allow the direct transmission of digital data (without the need for conversion) and, therefore, they enable very high transmission speeds. Transmission through optic fiber cables allows currently a much faster transmission speed and is immune to electromagnetic disturbances, and for these reasons its use will be increasingly implemented.
At local level, wireless transmission is spreading increasingly through radio waves or infrared rays (wireless local area network, Bluetooth, or Wi-Fi technology) which offer though a limited coverage. For long-distance transmission, the most widely used system nowadays is the satellite Internet with a transmitter that sends signals to a satellite sending them back with minimal delay to a receiver.
Precisely based on their geographic coverage, networks must therefore be distinguished into local (Intranet) or global (Internet) networks. Local networks can extend for a few meters (e.g., connecting several rooms in the same building: PAN, personal area network) or even for a few kilometers (connecting several floors of the same building or neighboring areas: LAN, local area network). Local networks also include the internal network of a university campus (CAN: campus area network) or the metropolitan network, which extends within a city (MAN: metropolitan area network). To protect local networks from external connections, router firewalls are used.
Networks that extend beyond the aforementioned limits and which use the Internet to communicate (the Internet is the real network of networks, capable of interconnecting billions of computers anywhere in the world) are defined as geographical or global networks (WAN: wide area network). Both in the MAN and WAN networks, public transmission channels are used and, therefore, to access the network, it will be necessary to contact a network provider. The provider will manage data received from the user and transfer it to the recipient according to the best possible route, through a device called a router.
There are official rules for the interaction between the various network components, validated and issued by the ISO (International Standards Organization). These rules are quite complex, so much so that hardware device manufacturers have to comply with the more practical standards of the Internet protocol suite (TCP/IP).
The digital technological evolution that has been briefly described above has substantially changed communication possibilities in every type of sector and also in the hospital environment. As a matter of fact, in most public hospitals there is a complex hospital information system (HIS). This system handles the administrative part, the collection of all clinical laboratory and instrumental data relating to both inpatients and outpatients; with the appropriate security measures, this database will allow to access clinical laboratory documentation by healthcare professionals. Figure 7.11 shows schematically the various network connection possibilities.
With modern digital systems, an EEG tracing can be adequately recorded anywhere and, therefore, the concept of an EEG laboratory must also be reviewed, in a broader and more dynamic perspective. Portable EEG systems can indeed reach the patients in any hospital ward and also record EEGs in emergency conditions. Permanent EEG acquisition devices can be installed in neurophysiological laboratories as well as many other departments. Therefore, nowadays, the role of EEG technicians must be reviewed: they no longer have to wait for the patient at the laboratory, but they also move to where the intervention is needed.
The recorded data can be stored inside the same recording system and then transmitted to other units (both for final storage and reporting) in various ways. Once technicians have returned to the lab, they can simply connect their laptop with a cable to the central unit (which also serves as a data storage) and then transfer all the tracings performed bedside. As an alternative, tracings can be transferred on a mobile device (like a pen drive) and then sent to the central unit. Finally, there is the more interesting possibility of remotely transferring the recorded material, using the hospital’s internal network (Intranet) or the external public network (Internet). In this modern perspective, the networked EEG laboratory can be organized in different ways, which are of increasingly complexity, but also easy to implement. Following, some examples:
-
1.
The networking of the various existing systems within a Neurophysiology Operative Unit.
The various digital systems available, placed either on the same floor or on different floors of a hospital building, can be attached to a “direct” network (via cable connection), with the possibility of communicating between them and above all with the possibility of channeling all the acquired data to a central unit, which will also act as the main storage unit.
A simple network model of this type can include:
-
(a)
Two or more EEG recording machines (e.g., named EEG1, EEG2, etc.)
-
(b)
One or more review station
-
(c)
One central unit for review and storage (file server)
With this type of organization, all EEGs recorded in the various rooms can be viewed remotely or even online, by referring physicians and then stored, both for medical and legal purposes and for their subsequent use (teaching, research, follow-up, etc.). The report can either be printed directly by the physician or sent to the computerized reception desk (Fig. 7.12).
-
(a)
-
2.
Local network connection of recording units located on different floors or buildings, within the same hospital or associated hospitals.
As already mentioned, one of the most important advantages of digital technology has been that it made available small, portable, or easily movable EEG devices, suitable for recordings in particular environments (even when disconnected from the power grid). At present, it is therefore possible, within the same hospital, to record tracings anywhere (emergency department, intensive care unit, surgery room, etc.) and then to transmit what is recorded via the Internal hospital network (Intranet) to the central unit for reporting and storage. From the same central unit, the reports can then be sent to the requesting department (Fig. 7.13).
-
3.
Remote sharing of EEG tracings
The most innovative possibility, however, is to be able to transmit the recorded EEG traces using the Internet, and this is achievable through the creation of a web server or a restricted virtual private network (VPN).
The connection via a web server is accessible from any Internet workstation and may not necessarily require the installation of specific software for review. The procedures in this case are the following: the tracings can be recorded from any workstation inside the hospital and then transferred to the web server in an accredited area; the physician gains access to the protected area with a username and password from any other workstations, both inside and outside of the hospital; once the tracing has been evaluated, the physician can generate the report in various ways, for example, by e-mail.
With the VPN, the EEG tracing is always transferred to the hospital’s internal server, which the doctor can only access with his own computer, but not necessarily while being inside the hospital. Therefore, he will be able to view the trace even at home and generate a report according to standard methods.
Thinking of a more complete organization, connected to the HIS (hospital information system), the following networked structure can be easily and inexpensively devised:
-
(a)
The HIS sends the list of the ongoing exams to the Acquisition Units (according to internal and external requests)
-
(b)
The EEG tracing is recorded anywhere inside the hospital
-
(c)
The EEG is transferred to the internal review station (which is nothing more than a slot on the specific hospital or associated hospital server)
-
(d)
The electroencephalographer connects to the VPN with their computer, regardless of where they are (at the hospital, at home, traveling, etc.), views the EEG and sends the report immediately to the HIS, which then makes it available online to the applicant.
-
(a)
All the procedures for the acquisition, transmission, review and storage of digital EEG data must be performed respecting the patient’s privacy to protect the abuse of patient’s information. Adequate security measures must protect against unauthorized users, computer viruses and accidental destruction of files.
References
Sinha SR, Sullivan S, Sabau D, et al. American clinical neurophysiology society guideline 1: minimum technical requirements for performing clinical electroencephalography. J Clin Neurophysiol. 2016;33:303–7.
Ferree TC, Luu P, Russel GS, Tucker DM. Scalp electrodes impedance, infection risk, and EEG quality. Clin Neurophysiol. 2001;112:536–44.
Jarrar R, Buchhalter J, Williams K, McKay M, Luketich C. Technical tips: electrode safety in pediatric prolonged EEG recordings. Am J Electroneurodiagnostic Technol. 2011;51:114–7.
Berlin F, Carlile JA, de Burgo MI, et al. Technical tips: electrode application and preventing skin breakdown techniques. Am J Electroneurodiagnostic Technol. 2011;51:206–19.
Scott NK. Infection prevention: 2013 review and update for neurodiagnostic technologists. Neurodiagn J. 2013;53:271–88.
Falco C, Sebastiano F, Cacciola L, et al. Scalp electrode placement by EC2 adhesive paste in long-term video-EEG monitoring. Clin Neurophysiol. 2005;116:1771–3.
Jasper HH. The 10–20 electrodes system of the International Federation. Electroencephalogr Clin Neurophysiol. 1958;10:367–80.
American Electroencephalographic Society. Guideline thirteen: guidelines for standard electrode position nomenclature. J Clin Neurophysiol. 1994;11:111–3.
Nuwer MR, Comi G, Emerson R, et al. IFCN standards for digital recording of clinical EEG. Electroencephalogr Clin Neurophysiol. 1998;106:259–61.
Achaya JN, Hani A, Cheek J, Thirumala P, Tsuchida TN. American clinical neurophysiology society guideline 2: guidelines for standard electrode position nomenclature. J Clin Neurophysiol. 2016;33:308–11.
Seeck M, Koessler L, Bast T, et al. The standardized EEG electrode array of the IFCN. Clin Neurophysiol. 2017;128:2070–7.
Oostenveld R, Praamstra P. The five percent electrode system from high-resolution EEG and ERP measurements. Clin Neurophysiol. 2001;112:713–9.
Kuratani J, Pearl PL, Sullivan L, et al. American clinical neurophysiology society guideline 5: minimum technical standards for pediatric electroencephalography. J Clin Neurophysiol. 2016;33:320–3.
Halford JJ, Sabau D, Drislane FW, Tsuchida TN, Sinha SR. American clinical neurophysiology society guideline 4: recording clinical EEG on digital media. J Clin Neurophysiol. 2016;33:317–9.
Acharya JN, Hani AJ, Thirumala PD, Tsuchida TN. American clinical neurophysiology society guideline 3: a proposal for standard montages to be used in clinical EEG. J Clin Neurophysiol. 2016;33:312–6.
Flink R, Pedersen B, Guekht AB, et al. Guidelines for the use of EEG methodology in the diagnosis of epilepsy. International league against epilepsy: commission report commission on European affairs: subcommission on European guidelines. Acta Neurol Scand. 2002;106:1–7.
Craciun L, Gardella E, Alving J, et al. How long shall we record electroencephalography? Acta Neurol Scand. 2014;129:9–11.
Capovilla G, Gambardella A, Rubboli G, et al. Suppressive efficacy by a commercial available blue lens on PPR in 610 photosensitive epilepsy patients. Epilepsia. 2006;47:529–33.
Chokroverty S, Vetrugno R. Polysomnography: technical and clinical aspects. In: Schomer DL, Lopes da Silva FH, editors. Niedermeyer’s electroencephalography. Basic principles, clinical applications, and related fields. 7th ed. Oxford: Oxford University Press; 2018. p. 897–967.
Beniczky S, Neufeld M, Diehl B, et al. Testing patients during seizures: a European consensus procedure developed by a joint taskforce of the ILAE—commission on European Affairs and the European Epilepsy Monitoring Unit Association. Epilepsia. 2016;57:1363–8.
Dash D, Dash C, Primrose S, et al. Update on minimal standards for electroencephalography in Canada: a review by the Canadian Society of Clinical Neurophysiologists. Can J Neurol Sci. 2017;44:631–42.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mecarelli, O. (2019). EEG Laboratory: Patient Care and the Role of the EEG Technician. In: Mecarelli, O. (eds) Clinical Electroencephalography. Springer, Cham. https://doi.org/10.1007/978-3-030-04573-9_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-04573-9_7
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04572-2
Online ISBN: 978-3-030-04573-9
eBook Packages: MedicineMedicine (R0)