Abstract
The term “brain death” (BD) is used to indicate a clinical situation characterized by the irreversible loss of all brain functions; the identification of this condition is closely linked to the development of intensive care medicine that, with mechanical ventilation, allows the maintenance of somatic functions even when cerebral functions are ceased.
BD diagnosis is essentially based on the presence of three cardinal clinic criteria: 1) coma or unresponsiveness, 2) absence of brainstem reflexes 3) absence of spontaneous breathing, evaluated with apnea test. For BD diagnosis the following prerequisites must be scrupolously considered: knowledge of the proximate cause of coma and confirmation of its irreversibility; exclusion of confounding clinical variables (severe electrolyte, acid-base, endocrine disturbances); hypothermia and/or hypotension; drug intoxication or poisoning. Ancillary tests used in BD confirmation are represented by neurophysiological methods to highlight the loss of bioelectrical brain activity (EEG, evoked potential (EP)) and methods for demonstration of cerebral circulatory arrest (TransCranial Doppler (TCD); Single Photon Emission Computed Tomography ( SPECT); conventional Digital Subtraction Angiography (DSA); CT angiography; MRI angiography). There is insufficient evidence to determine whether ancillary tests are able to confirm the complete cessation of all brain functions and then, in adults, ancillary tests are not needed for the clinical diagnosis of brain death and they should never replace the clinical neurological examination.
However, even though ancillary tests are not mandatory but only optional in many countries, they continue to be used, especially when there are factors that may interfere with the complete clinical assessment or when apnea test cannot be performed. Although BD is a relatively simple clinical diagnosis, there are substantial differences in perceptions and practices regarding its declaration among countries, states and even between hospitals worldwide. There are also cultural and religious obstacles—especially in lower-income countries—to the determination of death with neurologic criteria, which lead to the suspension of mechanical ventilation. Therefore, health organizations should implement educational campaigns to improve knowledge and awareness of current criteria among the population, and national and international scientific societies should also make every efforts to validate and standardize clinical and laboratory criteria. Finally, it should reminded and underlined that the ultimate purpose of brain death determination should be to increase the number of organs donated, to improve the quality of life of organ recipients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Brain death
- Coma
- Brainstem reflexes
- Apnea test
- Electrocerebral inactivity
- Evoked potentials
- Conventional four-vessel angiography
- Computed tomography angiography
- Magnetic resonance angiography
- Single-photon emission computed tomography
- Transcranial doppler
- Organ donation
1 History of Brain Death Determination
This year recurs the 50th anniversary of publication of the criteria of Harvard Medical School that established brain death as an accepted medical phenomenon [1].
“Brain Death” (BD) is the term for defining death due to the irreversible cessation of all cerebral functions. This term may be actually misleading, since it wrongly implies that there is more than one kind of death, whereas death is instead an unitary phenomenon: in subjects without artificial ventilation, physicians confirm death only with the finding of permanent cessation of respiratory and cardiocirculatory functions; in patients who are receiving mechanical ventilation, it is instead mandatory to determine the irreversible loss of all brain functions, as respiratory and cardiac functions are artificially maintained.
In the 1950s critical care medicine showed rapid development, mainly for the diffusion of artificial ventilation devices and of cardiopulmonary resuscitation procedures; consequently, critical care physicians had firstly involved in the diagnosis and management of the condition of irreversible coma, later defined brain death. Mollaret and Goulon [2] described for the first time in 1959 23 patients with coma depassé (“a state beyond coma”), without any brainstem activity and maintained alive only by mechanical ventilation. Subsequently, medical communities and scientific societies worked to create specific definitions of this new entity and to define the guidelines for its determination, especially after the first human-to-human heart transplant in 1967 performed by Christiaan Barnard (1922–2001). At that time, it was indeed already felt the need to define precise criteria for brain death diagnosis, in order to be able to proceed with organ harvest.
It was in 1968 that the “Ad Hoc Committee of Harvard Medical School” defined brain death and described the criteria for its determination. The criteria included unreceptivity and unresponsivity, no movements or breathing, no reflexes, and flat electroencephalogram (confirmatory test that should be utilized when available). The persistence of these conditions had to be revaluated at least 24 h later and hypothermia treatment or administration of CNS depressant drugs was to be excluded [1].
In 1981, the President’s Commission for the study of Ethical Problems in Medicine and Behavioral Research in the United States redefined the criteria for the diagnosis of brain death in adults and proposed a legal uniform definition of death (Uniform Determination of Death Act—UDDA). This act reports the following: “An individual who has sustained either (1) irreversible cessation of circulatory and respiratory functions, or (2) irreversible cessation of all functions of the entire brain, including the brain stem, is dead. A determination of death must be made with accepted medical standards” [3]. The UDDA did not define the acceptable diagnostic tests and medical procedures and then the Quality Standards Subcommittee of the American Academy of Neurology (AAN) in 1995 published evidence-based practice parameters for determining brain death in adults [4, 5]. The Guidelines of AAN were then updated in 2010, providing an algorithmic, unified approach to brain death determination in adults [6].
Clinical guidelines for the determination of brain death in children were first published in 1987 and later revised in 2011 [7,8,9].
2 Clinical Diagnosis of Brain Death
The prerequisites for BD diagnosis include:
-
Knowledge of the proximate cause of coma and confirmation of its irreversibility (history, examination, neuroimaging and laboratory tests).
-
Exclusion of confounding variables as severe electrolyte, acid-base and endocrine disturbances.
-
Body temperature must be normal or near-normal (>36 °C).
-
Systolic blood pressure must be ≥100 mg Hg.
-
Exclusion of drug intoxication or poisoning (for the CNS depressant drugs, if available, evaluation of drug plasma levels below therapeutic range).
Neurologic assessment. The three cardinal findings in brain death are:
-
(a)
Coma or unresponsiveness.
-
(b)
Absence of brainstem reflexes.
-
(c)
Absence of spontaneous breathing.
-
(a)
Coma. The neurologist must first ascertain that the patient does not present any kind of responsiveness, as documented by the absence of eye opening or eye movements and absence of motor responses (other than spinally mediated reflexes) to noxious stimuli. Some studies reported spontaneous and reflex complex movements after brain death, of spinal or peripheral origin (facial myokymia; transient bilateral finger tremor; repetitive leg movements; cyclical constriction and dilation in light-fixed pupils; cremasteric, plantar, and abdominal reflexes; triple flexion of the lower extremities; deep tendon reflexes; “Lazarus sign”; undulating toe reflex) [10, 11]. Additionally, small changes in tubing pressure of ventilator and ventilator autocycling may falsely suggest a patient-initiated breaths that can be excluded by disconnecting the ventilator [12, 13]. The conclusion of the AAN guidelines is that “for some patients diagnosed as brain dead, complex, non-brain-mediated spontaneous movements can falsely suggest retained brain function” [6].
-
(b)
Absence of brainstem reflexes. The neurologist must verify the absence of:
-
Pupillary reflex (usually, pupils are fixed in a midsize or dilated position, 4–9 mm diameter, not responding to light; the presence of dilated pupils is compatible with brain death because sympathetic cervical pathways may, however, remain intact; miosis suggests the possibility of drug intoxication; many drugs can influence pupils diameter, but the light response remains preserved [4]).
-
Oculocephalic and oculovestibular reflexes (the oculocephalic reflex may be elicited by turning the head to 90° on both sides and by brisk neck flexion: horizontal contralateral or vertical eye movements are absent in brain death; the oculovestibular reflex is tested with the head elevated to 30° by irrigating each ear with 50 mL of cold water, and the normal tonic deviation of the eyes toward the irrigated ear must be absent; the observation of eye movements must be protracted for 1 min after irrigation, and the time between stimulations on each side should be at least 5 min).
-
Corneal reflex (the absence of corneal reflex is demonstrated by touching the cornea with a piece of tissue paper or a cotton swab: no eyelids movement should be evoked).
-
Facial movements induced by noxious stimuli (deep pressure at temporomandibular joints and at the supraorbital ridge does not determine grimacing or facial muscle movements).
-
Pharyngeal and tracheal reflexes (the pharyngeal or gag reflex is elicited by stimulation of the posterior pharynx with a tongue blade or suction device; the tracheal or cough reflex is evoked by the insertion of a catheter into the trachea up to the level of the carina, followed by one or two suctioning passes).
-
-
(c)
Absence of spontaneous breathing. The absence of a breathing drive is tested with an apnea test, that induce a CO2 challenge. For the documentation of PaCO2 increase to above normal levels (apnea test) the following prerequisites are necessary: normotension, normothermia, euvolemia, eucapnia (PaCO2 35–45 mm Hg), absence of hypoxia and no prior evidence of CO2 retention due to chronic obstructive pulmonary disease or severe obesity. Then, the procedure for the execution of apnea test is as follows:
-
Adjust vasopressors to a systolic blood pressure ≥ 100 mm Hg.
-
Pre-oxygenate for at least 10 min with 100% oxygen to a PaO2 > 200 mm Hg.
-
Reduce ventilation frequency to 10 breaths/min.
-
Reduce Positive End-Expiratory Pressure (PEEP) to 5 cm H2O.
-
If pulse oximetry oxygen saturation remains >95%, obtain a baseline blood gas analysis.
-
Successively, the patient should be disconnected from the ventilator, delivering 100% O2 at 6 L/min by an insufflation catheter through the endotracheal tube up to the carina.
-
After the disconnection from the ventilator, the patient must be closely observed for respiratory movements for 8–10 min (respiration can manifest itself with abdominal or chest excursions and may include brief gasps).
-
The patient must be reconnected to ventilator if systolic blood pressure decreases to <90 mm Hg and if oxygen saturation is <85%.
-
After approximately 8 min from the ventilator disconnection, if no respiratory drive is observed, blood gas analysis (PaO2, PaCO2, pH, bicarbonate, base excess) can be performed.
-
The apnea test is considered positive and supportive the clinical diagnosis of brain death if respiratory movements are absent and PaCO2 is ≥60 mm Hg (or PaCO2 increase is >20 mm Hg compared to basal values). If the test is inconclusive (PaCO2 is less than 60 mm Hg), but the patient is hemodynamically stable, the procedure may be repeated with a longer period of time of ventilator disconnection (10–15 min) [4,5,6].
Apnea testing is considered an indispensable element for brain death diagnosis, but there is insufficient scientific evidence to determine the comparative safety of techniques used [6, 14].
Wijdicks et al. [15] reviewed retrospectively a large series of patients who were declared brain dead and concluded that apnea testing with an oxygen-diffusion technique is safe. Nevertheless, apnea test could not be performed in 7% of the patients because of hemodynamic instability or poor oxygenation at baseline. In 3% of patients, the test was aborted because of hypotension or hypoxemia.
Therefore, once the above clinical conditions are ascertained, there should be no need for an observation period to declare BD diagnosis. Using the criteria universally recognized, recovery of neurologic functions has indeed never been reported, and there is insufficient evidence to determine which would be the minimally acceptable observation period to ensure its irreversibility. In these regards, the length of the observation period is very variable throughout the world and also among the hospitals of the United States. Waiting period between the initial neurologic deterioration until death declaration ranged from <5 to >25 h [16,17,18]. Lustbader et al. [19] reported that, in the NY State, the time to perform a second neurological evaluation was approximately 3 times longer than that recommended in the guidelines (mean 19.2 vs. 6 h) and that it was associated with markedly higher intensive care unit costs and increased loss of viable organs. Moreover, the time lapse between the two observations may increase the likelihood of premature cardiac arrest, which accounts for up to 12% in literature [19].
3 Ancillary Tests
Ancillary tests are optional/confirmatory in the United States and in other parts of the world, but mandatory in many countries [16, 18].
Indications for ancillary tests execution are represented substantially by: difficulties for clinical examination due to anatomic limitations or injuries; apnea test that cannot be completed for hemodynamic instability or hypoxia; limitations to interpreting a positive apnea test (high levels of sedative drugs, severe neuromuscular disease, preexisting CO2 retention) or apnea test inconclusive in clinically unstable patient; high levels of CNS depressants; less than 24 h since cardiac arrest or recovery from hypothermia therapy; physician or family discomfort with brain death diagnosis (especially when the residual movements and spinal reflexes are disturbing).
The ancillary tests used in the confirmation of brain death are represented by:
-
(a)
Neurophysiological methods to highlight the loss of bioelectrical brain activity (EEG, Evoked Potentials (EPs)).
-
(b)
Methods for the demonstration of cerebral circulatory arrest (Trans Cranial Doppler (TCD); Single-Photon Emission Computed Tomography (Tc99 HMPAO SPECT); conventional and digital subtraction angiography; CT angiography; MRI angiography).
3.1 EEG
The characteristic EEG finding in BD is the Electro Cerebral Inactivity (ECI), which is defined as “the absence over all regions of the head of identifiable electrical activity of cerebral origin, whether spontaneous or induced by physiological stimuli (synonyms are electrocerebral silence, flat or isoelectric EEG, but the use of these terms is discouraged)” [20]. Tracings with ECI should be clearly distinguished from the EEG patterns with low-voltage background activity. EEG is a very sensible tool to evaluate cerebral functional activity related to cerebral perfusion: reversible EEG changes appear when the CBF decreases below 35 mL/100 g/min and cortical activity is totally suppressed when CBF reduces below 12/mL/100 g/min. After a few seconds from blood flow arrest, electrical cortical activity is suppressed, and—if the circulation is not readily reestablished—this will cause cells death and irreversible loss of all brain functions (Fig. 47.1).
An example of progressive attenuation/suppression of the background activity (a–c) up to electrocerebral inactivity (d–f), in a 77-year-old patient with cardiorespiratory failure, in absence of artificial ventilation. Note in (f) the complete absence of heartbeat. LFF 0.53 Hz, HFF 70 Hz. Sensitivity: a, b, c, d = 10 μV/mm; e, f = 2 μV/mm
An EEG with ECI cannot, however, exclude that some subcortical or brainstem functions remain preserved [21, 22], and ECI have been described also in patients with vegetative state. On the other hand, older studies assessing EEG accuracy in BD diagnosis are difficult to be interpreted, since they were performed before the development of explicit guidelines for the clinical BD declaration [23].
More recent studies conducted in countries with precise guidelines have highlighted uncommon discrepancies between clinical and electroencephalographic findings. In 71 consecutive patients declared brain dead using the German guidelines, ECI is present in 94%. In the remaining four patients, EEG tracings could not be interpreted because the presence of artifacts [24]. A retrospective study performed using Spanish guidelines showed that EEG tracings confirmed ECI in 96.5% of patients. The remaining patients (3.5%) had most frequently underlying severe brainstem damage with malignant EEG patterns, but no ECI [25]. None of these patients survived. In Italy, EEG is mandatory for brain death diagnosis, and in our series of 66 consecutive patients, we have not found discrepancies between clinical criteria for brain death according to Italian guidelines and ECI [26]. No patients meeting criteria for brain death with ECI in EEG regained neurological functions [25, 26].
In summary, EEG has a long history as a confirmatory test in BD, and it can be easily performed bedside without risks; when clinical BD assessment is performed according to the accepted guidelines, EEG features are rarely discrepant or always concurrent. False positives can occur, mainly due to the depressant effects on electrocerebral activity of sedative drugs or hypothermia. False negatives can be due to electrical interferences in ICU environment and artifacts of various origins. Sometimes, administration of muscle relaxants is necessary to achieve an EEG tracing uncontaminated by EMG activity. Rarely, EEG tracing is uninterpretable or not recordable for the poor condition of the patient’s scalp (Fig. 47.2). After all, additional limitations of the EEG as confirmatory test in brain death are represented by its nonavailability 24 h per day at many centers. Despite these limitations, EEG remains the second most common ancillary test to be used [27, 28].
3.1.1 Technical Standards for EEG Recording in Brain Death
Various national and international guidelines and laws define the minimum technical standards for EEG recording in suspected cerebral death. The contents of guidelines [6] of the American Clinical Neurophysiology Society, that is an update of the precedent guidelines [3], are summarized [29, 30]:
-
(a)
Electrocerebral inactivity is defined as the absence of nonartifactual electrical activity over 2 μV (peak to peak), at a sensitivity of 2 μV/mm (Fig. 47.3). A calibration signal of 2 or 5 μV is appropriate, and the recording should last 30 min at least.
-
All major brain areas should be explored with scalp electrodes placed according to 10–20 international system. The montage should include electrode pairs at least 10 cm apart, and an acceptable montage is Fp2-C4, C4-O2, Fp1-C3, C3-O1, T4-Cz (T8-Cz in the modified 10–10 terminology), and Cz-T3 (Cz-T7 in the modified 10–10 terminology).
A montage that includes F8-T6 (F8-P8 in the modified 10–10 terminology), F4-P4, Fz-Pz, F3-P3, and F7-T5 (F7-P7 in the modified 10–10 terminology) should be recommended. The montage must include one channel for ECG (to identify the ECG artifact) and one channel for a non-cephalic recording (e.g., on the hand, to document movement-induced artifacts).
In addition, all the preselected laboratory montages should be used.
-
(b)
Electrode impedances should be less than 10.000 ohms, but more than 100 ohms. The integrity of the entire recording system should be tested by touching each electrode of the montage, for verifying the correct connection of all electrodes with the recording machine. The filters should be set between 1 and 30 Hz, and the notch filter (at 60 or 50 Hz) can be used with care and comparing the EEG segments with the notch filter to those without.
-
(c)
To clarify the recording and to accurately assess and identify the various artifacts (physiological, mechanical, electromagnetic or electrostatic, etc.) (Fig. 47.4), it is sometimes necessary to monitor the respiration and the EMG contamination (if EMG activity obscures the EEG tracing, it may be necessary to eliminate it administrating short-term neuromuscular blocking agent) (Fig. 47.5). Furthermore, continuous video-recording is strongly encouraged to help identify any kind of artifacts.
-
(d)
During the recording there should be no reactivity to intense somatosensory, auditory, or visual stimuli. The technician must apply the various standardized stimuli and note on the tracing the time at which they were applied.
-
(e)
The EEG recordings for ECI should be performed by a qualified technologist, under supervision of a qualified electroencephalographer. Sometimes, the interpretation of an EEG performed for BD diagnosis is difficult for technical or physiological variables and, in these cases, the entire procedure should be repeated after a 6-h interval in adults and after at least 24 h in newborns and children. To limit errors in interpretation, it is important that the technologist note all pathophysiologic variables (temperature, blood pressure, oxygen saturation) and all the medications administrated.
A 56-year-old patient, 2 days after a severe anoxic insult. EEG recording with cerebral activity of low voltage at a sensitivity of 10 μV/mm (a, on the left), which is more evident at 2 μV/mm (a, on the right). After about 4 h (b), the tracing appears with electrocerebral inactivity at sensitivity of 2 μV/mm. LFF 0.53 Hz, HFF 70 Hz
3.2 Evoked Potentials
Short latency Evoked Potentials (EPs) have the advantage to be a test widely available and noninvasive, able to explore the brainstem structures and less affected by sedation and hypothermia than EEG (Fig. 47.6). The major disadvantages for this technique are represented by the necessity of the expertise in their performance and interpretation, by the possibility of false-negative results, and by the absence of potentials in patients with lesions of cervicomedullary junction.
Seriated EEG recordings in a 21-year-old patient with post-traumatic coma, sedated with Sodium Thio Pental (STP). In (a) EEG with electrocerebral inactivity; Somato Sensory Evoked Potentials (SSEPs) (a) show a persistence of low-voltage, reproducible N20 component (the plasmatic level of STP is 11 μg/mL, and the brainstem reflexes are absent). After 48 h (b) EEG with burst-suppression pattern (STP has been suspended, and plasmatic level is 8 μg/mL; the brainstem reflexes had reappeared). After 72 h (c) the background EEG activity is continuous and of high amplitude (STP: 5 μg/mL), but unreactive. After 96 h (d), EEG is again reactive to acoustic stimulus—at arrow (STP, 2.8 μg/mL)
Somato Sensory Evoked Potentials (SSEPs) assess the functional integrity of posterior columns, medial lemniscus, thalamus, and the sensorimotor cortex, and they are indicative of BD if bilateral absence of N20-P22 response to median nerve stimulation is demonstrated [5]. Generally, the absence of N20 is an indicator of poor prognosis in comatose patients, and it is predictive of BD. However, in BD early phase, the cortical components of SSEPs can be sometimes present, disappearing only over time. Wagner [31] studied the component P14 of SSEPs (presumably generated in the medial lemniscus and cuneate nucleus) and demonstrated that in all 108 patients diagnosed brain dead, the P14 potential on nasopharyngeal electrodes was absent (specificity 100%). However, the P14 potential has two generators: the greater rostral part of the P14 generator dipole is inactivated in BD, whereas the very caudal segments may be still intact for some time; furthermore, the absence of P14 can be due to lesions of the upper cervical cord and medulla. To avoid false-negative or false-positive results, recording with nasopharyngeal electrodes is advisable, but this technique is still not widespread and not sufficiently validated [32].
Brainstem Auditory Evoked Potentials (BAEPs) were found to be 100% sensitive, but only 73.7% specific, and BAEPs may be transiently absent after an anoxic insult [33]. Facco et al., in a series of 130 brain dead patients, demonstrated that BAEPs were absent in 70.8%, while SSEPs confirmed the absence of brainstem activity in 93.7% of cases [34]. These authors concluded that the combined use of SSEPs and BAEPs was able to confirm BD in almost all patients, excluding this diagnosis in a few cases (about 5% in their series) that show residual brainstem activity; they also emphasize the utility of a more complete (not only EEG-based) neurophysiological investigation in BD to improve patients’ management and the certainty of diagnosis. Obviously, none of these patients survived, but they were not declared dead until the disappearance of all evoked potentials [34].
3.3 Assessment of Cerebral Blood Flow
Increase of intracranial hypertension is the condition at the basis of absence of Cerebral Blood Flow (CBF). When the intracranial pressure overrides the mean arterial blood pressure, a mechanical hindrance to blood stream entrance in intracranial arteries, in the intact skull, occurs. This condition is typically referred to as “Cerebral Circulatory Arrest” (CCA), since most techniques aimed at this evaluation actually investigate cerebral circulation and not cerebral perfusion.
Several conventional radiological techniques may be applied to identify CCA: conventional angiography represents the “gold standard,” while less invasive techniques, such as CT and MR angiographies, both with perfusion studies, are nowadays also being used. Single-photon emission computed tomography (SPECT) and xenon-CT are dedicated to the investigation of cerebral perfusion, but these investigations may be less commonly available. All these radiological techniques, though expensive, are time-consuming and require the patient to be delivered to the radiological unit to perform the exam, further dilating the time to the final death declaration, a crucial point for eventual organ harvest. Moreover, contrast agent administration may induce further organ damage, eventually reducing the possibility of organ donation. For these reasons, Trans Cranial Doppler (TCD) ultrasound is commonly used for detecting CCA easily and at the bed of the patient, with high sensibility and specificity, when performed with strict protocols. Recently, even the optic nerve sheath diameter evaluation has been correlated with marked intracranial hypertension and, thus, correlated with development of malignant intracranial hypertension and brain death in critically care patients.
3.3.1 Conventional Four-Vessel Angiography
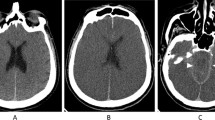
Conventional angiography is classically considered to be the gold standard method for CCA diagnosis. This technique is relatively easy to perform and to interpret and may be executed in 30–60 min. Examinations for BD are usually performed with contrast medium injections in the aortic arch with a “pig tail” catheter, but the separate contrast injections performed in either the common or the internal carotid arteries, as well as in both the vertebral arteries, have also been used. Angiographic CCA findings consist in the lack of contrast diffusion in the internal carotid arteries beyond the carotid siphon and beyond the dural penetration of vertebral arteries, with normal visualization of the external carotid arteries (positive control) (Fig. 47.7).
Some opacification in the proximal middle or anterior cerebral arteries are described in 30% of patients [35], and this may be due to the selective injection of individual vessels and to high injection flow rates that force contrast medium into the intracranial vessels [36]. The vein system should not be visualized, though occasional visualization of the superior longitudinal sinus may be possible through meningeal veins. In literature, no false-positive cases have been reported, whereas some false-negative cases are described, where patients have been clinically declared brain dead, but they continue to have some intracranial blood flow [22].
Despite considered the “gold standard,” conventional angiography has numerous disadvantages: it is an invasive and expensive procedure, it cannot be performed bedside, and it is not readily available in many hospitals; it requires the insertion of a catheter in the arterial circulation, with potential risk for vessel damage and dissections along the catheter course; the contrast medium may produce organ toxicity, especially for the kidneys, that is unfavorable in case of their harvest [22, 32].
3.3.2 Computed Tomography Angiography (CTA) and CT Perfusion
Being nowadays CTA routinely performed in vessel assessment for cerebrovascular diseases, it is the natural evolution of the technique to be used to assess CCA, and it is also well accepted in European countries as an ancillary test for BD determination. As in conventional angiography, CCA is diagnosed when the lack of visualization of intracranial arteries beyond the siphon and beyond the dural penetration of vertebral arteries is observed. CTA is a rapid and widely available method for assessing brain blood flow, far less invasive than conventional angiography; however, as iodinated contrast is to be used, the potential risk of contrast-mediated tissue injury is still present. Systematic reviews have assessed the accuracy of CTA as confirmatory test for BD declaration and reported a pooled sensitivity of 84% [37], and false-positive uncommon cases have been described [38].
In regard to CT perfusion, this technique has been adopted to quantify brain perfusion in stroke, and its subsequent post-processing calculations to generate perfusion parameters (mean transit time, cerebral blood flow, and volume) would also add functional information that could increase sensitivity for the BD diagnosis. However, it requires brain parenchyma appropriate assessment and specific trained personnel to correctly interpret its findings. Further studies will help to standardize the technique [39].
3.3.3 Magnetic Resonance Angiography (MRA) and MR Perfusion
In clinically confirmed brain dead patients, MR imaging may demonstrate in BD the lack of the normal intracranial arterial flow voids, due to the intracranial hypertension and to the slowing of blood flow within cerebral arteries. MRA imaging without contrast agents uses the “time-of-flight” sequences that are related to the “moving blood,” and, similarly to the other techniques, this will lead to the lack of visualization of the intracranial circulation in CCA. However, MR imaging takes longer time, it is more prone to develop artifacts, and it requires compatibility of the devices that usually these critical patients have attached. MR perfusion with contrast agents may also be considered a promising technique, with data similar to those of the perfusion CT, with no available data in the brain death setting [40,41,42].
3.3.4 Single-Photon Emission Computed Tomography (SPECT)
Brain perfusion scintigraphy with specific brain radionuclide 99mTc-HMPAO (Hexa Methyl Propylene Amine Oxime) represents a well-studied method for BD diagnosis [43]. The radionuclide overrides the blood-brain barrier, with uptake from cerebral neurons after the initial blood flow passage, indicating not only the presence of flow, but also the presence of cerebral activity. Nuclear medicine divisions are necessary to perform this examination, and CCA finding consists in the lack of intracranial tracing uptake, the so-called “hollow skull” [44]. Planar anterior and both lateral images are recommended to be acquired immediately, after between 30 and 60 min and at 2 h after radionuclide injection (740 MBq [20 mCi] -Tc-99 m with a HMPAO and saline 5 mL). Multiprojection static planar imaging can also be used to evaluate the cerebral hemispheres, basal ganglia, thalami, and cerebellum, with progressive 5° rotation of the scanner, 20 s/step, for 360° and for a total exam duration of 25 min. The current use of SPECT is primarily supplemental, to help differentiate overlying scalp from intracerebral activity. The reliability of SPECT to exclude flow and metabolism in the brainstem remains to be scientifically validated. SPECT imaging can be technically difficult in the context of BD confirmation. Typical issues encountered for SPECT imaging include indeed the difficulty of bringing the gamma camera detectors sufficiently close to the patient, presence of tubes and lines in the detector orbit acting as impediments to detector rotation, and the requirement of moving the patient to the imaging table. The specificity of SPECT was estimated to be of 100% and sensitivity of 88% [45,46,47].
3.3.5 Transcranial Doppler
In the presence of adequate temporal and occipital bone windows, i.e., in 95% of cases, TCD ultrasound equipments with a 2 MHz probe can easily insonate the intracranial basal cerebral arteries [26, 48, 49]. Characteristic changes of blood flow velocity waveforms are proportional to the increase of intracerebral pressure, up to CCA development. Four pathognomonic stages are identified (Fig. 47.8):
-
1.
Increased resistive indices: the increase of the intracranial pressure induces gradual reduction of diastolic blood flow velocities over systolic flow velocities. This stage, indicative of increased intracranial pressure, is not yet representative of CCA (Fig. 47.8b).
-
2.
Oscillating/reverberating flow: the flow direction in the diastolic phase becomes inverted, i.e., during systole blood flow is directed toward the brain and during diastole is directed away from the brain. When both the phases are equal, this corresponds to the CCA (Fig. 47.8c, d).
-
3.
Systolic spikes: short (<200 ms) and slow velocity (<50 cm/s) ortodromic systolic spikes are expression of further reduction of blood flow movements. High pass filters of ultrasound equipments may participate to cut off slow velocity signals and, thus, should they be set as low as possible (50 Hz) (Fig. 47.8e).
-
4.
Absence of signal: when flow stop becomes more proximal, no signal could be detected in the intracranial arteries (Fig. 47.8f) These findings alone, however, performed in a single examination could also be related to transmission problems through thick and inadequate temporal bone windows and may not be conclusive. Thus, absence of signal is probative of CCA only when the same operator had already performed the examination before, demonstrating the adequacy of the temporal bone windows. In such cases, findings in the vertebral arteries—as well as in the extracranial cervical arteries—represent an important criterion to be added for the diagnosis.
Trans Cranial Doppler (TCD) middle cerebral artery spectrum evolution during intracranial hypertension. (a) Normal spectrum; (b) increased resistive indices, flow is still present; (c, d) Oscillating/reverberating flow with various degree of reversal flow reduction, cerebral circulatory arrest (CCA); (e) systolic spikes; (f) absence of flow
For CCA diagnosis, a single operator should carry out two examinations at a 20–30 min interval, in hemodynamic stable conditions (Systolic Blood Pressure, SBP >100 mm Hg, Mean Arterial Blood Pressure MABP >70 mm Hg), identifying the typical CCA patterns in any of the intracerebral arteries, through temporal and occipital insonation. These findings should also be confirmed in the extracranial circulation. Recently, the use of color-coded transcranial Doppler has also been proposed for the CCA diagnosis, considering that the direct visualization of the brain structures could be of help in discriminating the adequacy of the bone windows and for the detection of the above-described typical Doppler patterns. Though TCD is easily and quickly performed bedside, the main criticism regards the expertise of the operator requiring dedicated, expert and well-formed physicians to obtain a reliable diagnosis. In our experience, CCA diagnosis performed with TCD, when CBF evaluation is requested, is useful to significantly reduce the time to final BD declaration in respect to angiography [26]. Transcranial Doppler—and in general techniques aimed at flow investigation—usually has a very high (up to 100%) specificity, i.e., the identification of CCA consistent with BD diagnosis, but lower sensitivity (90–95%), since the persistence of cerebral blood flow may be observed even after BD, in cases of skull fenestration (decompressive craniectomy, infants with non-ossified fontanelles, ventricular derivation) [50].
An important concept, at the bases of these “false-negative” results, has to be discussed when considering cerebral blood flow for the diagnosis of BD, regardless the technique used. BD is—by definition—the irreversible loss of any cerebral neuronal activity, and it implies that neurons are not functional and they have no metabolism at all. As regards the false-negative persistence, to various degrees, of “blood flow” when BD has already occurred, it has to be underlined that only scintigraphy and PET scans are actually able to really display brain metabolism. All the other techniques, investigating blood flow as “circulation,” are based on the assumption that if there is metabolism, there is “flow”, but this might not be true backward. As a matter of fact, the condition necessary to induce CCA inside the skull is the increase of the intracranial pressure, overriding the mean arterial blood pressure and, thus, inducing the mechanical forces to interrupt circulation. However, if cerebral damage had already occurred or neuronal degeneration had already developed over time—as it may occur in ICUs during a long follow-up of these neurocritical patients—decompressive craniectomy (or other treatments aimed at reducing ICP, such as ventricular derivation) only reduces the mechanical forces induced by the swollen dead brain, with consequent lowering of intracranial pressure and restoring a “cerebral circulation” (i.e., blood that enters the arterial bed drained out from the vein system), but in absence of cerebral function. To make a simple analogy, in the case of a compartment syndrome for muscular damage, fasciotomy restores blood flow, but if the necrosis had already occurred in the muscle, flow restoration doesn’t restore muscular cell activity. Then, to summarize, detection of CCA—regardless of the technique used—in cases of an intact skull has 100% specificity for BD diagnosis. In cases of non-intact skull, when however the brain is swollen and fenestration is not able to compensate for the malignant intracranial pressure, CCA may however occur, and its detection is supportive of BD; usually, in these cases, craniectomies are swollen and hard, and flow spectra may be asymmetric due to the higher “blood movement” in the open skull side and that could be misinterpreted as flow persistence with other techniques (Fig. 47.9). Last, in cases of skull fenestration and clinical and/or instrumental BD suspicion, “persistence” of cerebral blood flow detected with TCD—or with other CBF investigating techniques—only indicates that the assessment of cerebral blood blow cannot be used to support in these cases BD diagnosis and that this false-negative - though “expected” - result only represents that we are evaluating circulation and not metabolism (Fig. 47.10) [51, 52].
Trans Cranial Doppler (TCD) showing Cerebral Circulatory Arrest (CCA) despite left decompressive craniectomy. TCD spectra are asymmetric, with reverberating flow and high velocities in the open side (a) and with only systolic spikes in the intact skull side (b). This finding is consistent with higher intracranial pressure in the intact skull side, that induces the disappearance of retrograde flow. In the open side, minimal compensation due to the absence of the bone still preserves higher blood movements with persistance of reverberant flow, though with higher velocities than expected. Decompressive craniectomy is, however, tense and swollen
Example of “flow persistence” after decompressive craniectomy; Trans Cranial Doppler (TCD) and EEG coregistration in a patient with right hemisphere hemorrhage due to right siphon aneurism rupture. At the first stage, when the patient clinically worsened, TCD showed only increased resistive indices (a), with persistence of asymmetric cerebral activity at EEG (b). After decompressive craniectomy, TCD shows normalization of intracranial resistive indices (c), but EEG (d) shows electro cortical inactivity.
Another sonographic exam that can be performed in the follow up neurocritical patients, for the early identification of critical malignant intracranial hypertension, is the Optic Nerve Sheath Diameter (ONSD) measurement [53]. Several clinical studies have indeed correlated the increase of ONSD as a reliable, noninvasive method to detect intracranial hypertension in neurosurgery and ICUs. ONSD is indeed directly connected with the subarachnoid space, and—differently from the inextensible—the intraorbital subarachnoid meningeal prolongation around the optic nerve is free of swelling with the pressure increase in the cerebrospinal fluid. Historically, the sign of the papilledema is a typical expression of this phenomenon. Even though the detection of ONSD enlargement of up to 0.6–0.7 cm could not alone be indicative for BD diagnosis, this very simple measurement performed through the eye during follow-up in ICU could help to identify those patients who—sedated—are developing signs of malignant intracranial hypertension and that could be then at risk of BD development [54].
In conclusion, ancillary tests, even though they are not mandatory in many countries, will continue to be used when there are factors that interfere with complete clinical assessment or the apnea test cannot be performed. Furthermore, ancillary tests are sometimes used to shorten the duration of the observation period. However, it must be emphasized that the Report of the Quality Standards Subcommittee of the American Academy of Neurology stresses that there is insufficient evidence to determine whether ancillary tests, even those using newer technologies, are able to confirm the complete cessation of all brain functions [6]. Consequently, according to AAN report, ancillary tests are not needed for the clinical BD diagnosis in adults, and they must never replace the neurological clinical examination. Wijdicks, an expert of BD determination, considers ancillary tests “not accurate, not conclusive, not pertinent and not warranted” and considers them to be mandatory by law - or performed as confirmatory - mainly as “a safeguard” [55]. Table 47.1 summarizes the principal advantages and disadvantages of the ancillary tests above described.
4 Pediatric Brain Death Determination
The first guidelines for adult BD determination were applied only to children older than 5 years. In the UDDA it is written indeed that “the brains of infants and young children have increased resistance to damage and may recover substantial functions even after exhibiting unresponsiveness for longer periods compared with adults” [3].
A special Task Force of American Academy of Pediatrics developed first clinical guidelines for BD determination in children in 1987 [7] and these guidelines were revised in 2011 [8]. Successively, an international expert panel published a unifying guideline describing death as “the permanent loss of capacity for consciousness and all brainstem functions” [56].
The prerequisites and the clinical neurologic examination for BD diagnosis in children basically follow the same criteria already described for adults: the cause for irreversible acute brain insult must be identified, confounding factors must be excluded, and the brainstem reflexes must be absent. The differences are represented by [57]:
-
The first examination must be carried out at least 24 h from ICU admission.
-
Two examinations are recommended (in adults: single examination), with an inter-examination observation period of 24 h for term newborns (37-week gestational age) to 30 days of age and 12 h for infants and children (over 30 days to 18 years).
-
Body temperature should be maintained over 35 °C.
-
PaCO2 at apnea test should be both 20 mm Hg above the baseline and ≥ 60 mm hg.
-
The examinations should be performed by different attending physicians “qualified and competent to perform BD examination”: pediatric intensivists, neonatologists, pediatric neurologists and neurosurgeons (adult guidelines allow that “it seems reasonable to require that all physicians making a determination of BD are intimately familiar with BD criteria and have demonstrated competence in this complex examination,” but they not specify how the physician should be or how the competence should be determined).
-
The time of the second neurologic examination is the time of death.
Ancillary tests (EEG and cerebral blow flow study) are not required to establish BD and they are not a substitute for the neurologic examination; they can be performed to reduce the observation period between examinations, but a second clinical evaluation and apnea test should still be performed.
5 Brain Death Worldwide
Despite a general consensus on the concept of “brain death,” the criteria and the laws for its determination vary among countries (Table 47.2). Wijdicks in 2002 published the results of the first comprehensive survey on BD criteria throughout the world [16]. Legal standards on organ transplantation were present in 69% of 80 countries surveyed and practice guidelines for brain death for adults in 88%. These guidelines specified the exclusion of confounding factors and required irreversible coma and absence of brainstem reflexes for the diagnosis. Apnea test using a PaCO2 measure was recommended only in 59% of the surveyed countries. Differences were also found in the time of observation and required expertise of physicians. Confirmatory ancillary tests were mandatory only in 40% of practice guidelines. Wijdicks concluded that “this survey shows that major differences are not so much in the acceptance of the concept of BD, but in the procedures physicians use to make the final diagnosis”. Successively, the differences and the adherence to the AAN guidelines [6] in BD guidelines among the various hospitals in the United States have been evaluated [17]. The results demonstrated a wide variability in the guidelines’ requirements for evaluation of the prerequisites, neurological examination, apnea testing and ancillary test performing. Surprisingly, many institutions do not require a specific level of expertise of physicians and do not consider necessary the availability of neurologists or neurosurgeons on a 24 h basis [17]. Citerio et al. in 2014 [58] published the results of a survey conducted through a web-based questionnaire in 33 European countries. The study demonstrates that, although laws or guidelines for brain death diagnosis are available in all European countries, there are still disparities, in particular regarding the use of ancillary tests as confirmation of the clinical examination. More recently, the practices and perceptions of BD determination worldwide has been assessed by an electronic survey conducted in 91 countries [18]. Overall, legal provisions for brain death are present in 70% of surveyed countries and institutional protocols in 77% of them, but in practice only 22% of low-income vs 97% of high-income countries had an institutional protocol. Among institutions with a formalized brain death protocol, there are marked variabilities in requisite examination findings; apnea testing; necessity and type of ancillary testing (EEG is the most common required test); time to declaration; number and qualifications of physicians present; and distinct pediatric criteria [18].
The high variability in BD determination worldwide is due also to ethical and religious principles. Most Christians accept BD without serious exception. Pope John Paul II in 2000, before an International Transplant Society meeting, affirmed BD to be compatible with catholic principles [59]. The Jewish religion accept BD, with the exception of the most traditionalist part of Judaism. Several Islamic countries, including Saudi Arabia and Iran, permit BD determination and organ transplantation [60]. The BD concept is accepted also in Hindu culture in India and by Shinto-Confucian religious authorities in Japan [61].
6 Legal Aspects of Brain Death Determination in Italy
In Italy, BD determination is currently defined by a decree of the Ministry of Health of 12 June 2008, which is valid throughout the entire national territory [62]. The law of 2008 represents a revision of the previous laws, the n. 644 of 2 December 1975 and n. 578 of 29 December 1994. The current decree redefines all the conditions, in patients with severe brain lesions undergoing resuscitation therapies that must lead physicians to immediately alert healthcare management of the presence of a case of irreversible loss of all brain functions. These conditions are literally defined in the law as follows:
-
Absence of vigilance and consciousness.
-
Absence of brainstem reflexes (pupillary, corneal, oculocephalic and oculovestibular, facial movements induced by noxious stimuli, pharyngeal and tracheal reflexes).
-
Absence of spontaneous breathing (apnea test performed according to the methods described above and demonstrating a PaCO2 ≥ 60 mm Hg and a pH ≤ 7.40).
-
Absence of cerebral electrical activity (EEG mandatory).
The procedure for BD determination can only be started in patients with clear etiopathology of brain injury and exclusion of confounding factors (alterations of thermal and cardiocirculatory homeostasis, major endocrine disorders).
The characteristics of these confounding factors and the procedures to be implemented in the event of their presence have been defined in the Guidelines of the National Transplant Center [63]:
-
Body temperature must be maintained above 35 °C.
-
Severe hypoglycemia and arterial hypotension must be corrected before BD validation procedures.
-
In case of antiepileptic drug administration (including benzodiazepines), the drug level within therapeutic range excludes any possibility of significant interference with BD validation; the administration of other CNS depressant drugs needs to be evaluated singularly, considering pharmacokinetics of specific drug and posology; administration of specific antidotes may be considered when available.
In newborns, BD can be determined only if birth happened after a 38-week gestational period and anyway only after 7 days of extrauterine life.
In patients with postanoxic coma, the observation period can start only 24 h after the anoxic insult, but this latency period can however be drastically reduced if CCA is demonstrated.
The observation period must last 6 h at least, without differences between children and adult patients.
The simultaneous presence of all conditions must be detected twice (at the beginning and at the end of observation period) by three physicians jointly: a neurophysiologist or neurologist or neurosurgeon expert in EEG, a coroner and an anesthesiologist. The time of the first examination is the time of death.
6.1 Modalities for the Execution of EEG
The Italian law of 2008 [62] establishes that the mandatory EEG recording of more than 30 min (two continuous recording, at the beginning and at the end of observation period of 6 h) must be performed by a qualified EEG technician, under a supervision of a qualified physician (neurophysiologist or neurologist or neurosurgeon expert of EEG). The EEG must demonstrate the absence of cerebral electrical activity ≥2 μV, spontaneous and/or stimulus-induced (acoustic and nociceptive stimuli). The montage of scalp electrodes and other technical parameters of recording are substantially the same as previously described (see Table 47.3).
The short latency EPs (SSEPs, BAEPs) are considered by the Italian law optional and additional to EEG recording, especially when there are confounding factors.
The demonstration of CCA is mandatory in Italy in:
-
Children <1 year of age.
-
Treatment with high doses of CNS depressant drugs.
-
Situations in which the etiopathogenesis of brain injury is uncertain and/or the clinical examination, apnea test, and EEG cannot be performed.
-
After an anoxic insult, when physicians decide to start the observation before 24 h from the insult itself. The absence of CBF testing must not be repeated.
The guidelines of the National Transplant Center recommend for the assessment of CCA conventional angiography; single-photon emission computed tomography; transcranial Doppler; and computed tomography angiography [63].
6.2 Donation of Organs in Italy
The procedures for the detection of BD are regulated in Italy by the law, and each large hospital is equipped with a commission for the assessment of death, composed of three physicians and with the availability of an EEG technician 24 h/day, to be able to perform the mandatory EEG as soon as possible. BD detection is performed even when his family does not give consent for organ harvesting for transplantation purposes. Once the evaluation procedure for BD has been completed, if the consensus is expressed, the beating heart patient is taken to the operating room for organ harvesting; otherwise, artificial ventilation is suspended and the corpse returned to the family members for the funeral (Fig. 47.11). Despite the law and the correct information that the resuscitators give to the relatives of the critically ill patients, the percentage of opposition to organ donation is about 40%, higher in the regions of Southern Italy than in the North.
In our series of 66 consecutive patients [26], observed over a 1-year period (2010) at Azienda Ospedaliero-Universitaria Policlinico Umberto I (Sapienza University of Rome) and who fulfilled the clinical criteria for BD diagnosis, EEG always demonstrated the electrocortical inactivity, and during the 6 h observation period, no clinical vital signs neither EEG activity did reappear in any of patients. In the time lapse between the two observations requested by law, the premature cardiac arrest occurs only in 4.5% of cases, against 12% reported by Lustbader et al. in hospitals of New York State [19].
While only one observation may be considered medically and scientifically correct, a 6 h delay before BD declaration may be an advantage in those countries such as Italy where, for cultural reasons, additional time is needed to reassure relatives that death has occurred and to explain the reasons and possibly obtain consent to donation. As a matter of fact, in our population time to BD declaration was longer when cerebral blood flow was evaluated: the time to complete the brain death evaluation procedure was 400 ± 17 min with EEG only vs. 443 ± 32 min with TCD up to 525 ± 20 with conventional angiography [26]. In our experience, a multimodal neurophysiological continuous monitoring of comatose patients after severe brain injury may also help to promptly identify cortical electrical inactivity and rapidly diagnose BD.
In Italy, the National Transplant Center performs the following functions:
-
Keeps the lists of people awaiting transplantation, with particular reference to the type and urgency of the transplant requested, in order to allow the identification of the recipients.
-
Defines the guidelines for regional or interregional centers for transplantation in order to standardize the sampling and transplantation activities in Italy.
-
Promotes and coordinates relations with foreign sector institutions in order to facilitate the exchange of organs.
In 2017, the waiting list of patients for organ transplants was 8958 people. BD assessment carried out were 2738 and the donors 1718 (63%), therefore, with a percentage of opposition to donation of 37%. Among the 1718 donors, organs were used only in 1437 (in other cases the organs were not eligible for donation) (Fig. 47.12).
Number of cases of brain death declaration in 2017 (a) in the various Italian regions and comparison with the number of organ donors (b). Data available on http://www.trapianti.salute.gov.it/cnt
References
Beecher H. A definition of irreversible coma. Report of the ad hoc committee. A definition of irreversible coma. Report of the ad hoc Committee of the Harvard Medical School to examine the definition of brain death. JAMA. 1968;205:337–40.
Mollaret P, Goulon M. Le coma dépassé. Rev Neurol. 1959;101:3–15.
Guidelines for the determination of death: report of the medical consultants on the diagnosis of death to the President’s commission for the study of ethical problems in medicine and biochemical and behavioral research. JAMA. 1981;246:2184–6.
Wijdicks EFM. Determining brain death in adults. Neurology. 1995;45:1003–11.
Practice parameters for determining brain death in adults (summary statement). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1995;45:1012–4.
Wijdicks EFM, Varelas PN, Gronseth GS, Greer DM. Evidence-based guideline update: determining brain death in adults. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74:1911–8.
Report of Special Task Force. Guidelines for the determination of brain death in children. American Academy of Pediatrics Task Force on Brain Death in Children. Pediatrics. 1987;80:298–300.
Nakagawa TA, Ashwal S, Mathur M, Mysore M, Society of Critical Care Medicine, Section on Critical Care and Section on Neurology of American Academy of Pediatrics, Child Neurology Society. Clinical Report—Guidelines for the determination of Brain Death in Infants and Children: An update of the 1987 Task Force Recommendations. Pediatrics. 2011;128:e720–40.
Mathur M, Ashwal S. Pediatric death determination. Semin Neurol. 2015;35:116–24.
Saposnik G, Bueri J, Maurino J, et al. Spontaneous and reflex movements in brain death. Neurology. 2008;71:1240–4.
Scripko PD, Greer DM. An update on Brain Death Criteria. A simple algorithm with complex questions. Neurologist. 2011;17:237–40.
Willatts SM, Drummond G. Brain death and ventilator trigger settings. Anaesthesia. 2000;55:676–84.
Wijdicks EFM, Manno EM, Holets SR. Ventilator self-cycling may falsely suggest patient effort during brain death determination. Neurology. 2005;65:774.
Lang CJG, Heckmann JG. Apnea testing for the diagnosis of brain death. Acta Neurol Scand. 2005;112:358–69.
Wijdicks EFM, Rabinstein AA, Manno EM, Atkinson JD. Pronouncing brain death. Contemporary practice and safety of the apnea test. Neurology. 2008;71:1240–4.
Wijdicks EFM. Brain death worldwide. Accepted fact but no global consensus in diagnostic criteria. Neurology. 2002;58:20–5.
Greer DM, Varelas PN, Haque S, Wijdicks EFM. Variability of brain death determination guidelines in leading US neurologic institutions. Neurology. 2008;70:284–9.
Wahlster S, Wijdicks EFM, Patel V, et al. Brain death declaration. Practices and perceptions worldwide. Neurology. 2015;84:1870–9.
Lustbader D, O’Hara D, Wijdicks EFM, et al. Second brain death examination may negatively affect organ donation. Neurology. 2011;76:119–24.
Kane N, Acharya J, Benickzy S, et al. A revised glossary of terms most commonly used by clinical electroencephalographers and updated proposal for the report format of the EEG findings. Revision 2017. Clin Neurophysiol Pract. 2017;2:170–85.
Young GB, Lee D. A critique of ancillary tests for brain death. Neurocrit Care. 2004;1:499–508.
Kramer AH. Ancillary testing in brain death. Semin Neurol. 2015;35:125–38.
Grigg MM, Kelly MA, Celesia GG, Ghobrial MW, Ross ER. Electroencephalographic activity after brain death. Arch Neurol. 1987;44:948–54.
Welschehold S, Boor S, Reuland K, et al. Technical aids in the diagnosis of brain death: a comparison of SEP, AEP, EEG, TCD and CT angiography. Dtsch Arztebl Int. 2012;109:624–30.
Fernandez-Torre JL, Hernandez-Hernandez MA, Munoz-Esteban C. Non confirmatory electroencephalography in patients meeting clinical criteria for brain death: scenario and impact on organ donation. Clin Neurophysiol. 2013;124:2362–7.
Vicenzini E, Pro S, Pulitano P, et al. Current practice of brain death determination and use of confirmatory tests in an Italian university hospital: a report of 66 cases. Minerva Anestesiol. 2013;79:485–91.
Shappell CN, Frank JI, Husari K, et al. Practice variability in brain death determination: a call to action. Neurology. 2013;81:2009–14.
Orban J-C, Ferret E, Jambou P, Ichai C, AzuRéa Group. Confirmation of brain death diagnosis: a study of French practice. Anaesth Crit Care Pain Med. 2015;34:145–50.
American Clinical Neurophysiology Society. Guideline 3: minimum technical standards for EEG recording in suspected cerebral death. J Clin Neurophysiol. 2006;23:97–104.
Stecker MM, Sabau D, Sullivan L, et al. American Clinical Neurophysiology Society Guideline 6: minimum technical standards for EEG recording in suspected cerebral death. J Clin Neurophysiol. 2016;33:324–7.
Wagner W. Scalp, earlobe and nasopharyngeal recordings of median nerve somatosensory evoked P14 potential in coma and brain death. Brain. 1996;119:1507–21.
Busl KM, Greer DM. Pitfalls in the diagnosis of brain death. Neurocrit Care. 2009;11:276–87.
Bhattarai BK. An analysis of brain stem evoked potentials (BAEP) in brain death and its usefulness in the diagnosis of brain death. J Anaesth Clin Pharmacol. 2002;18:397–404.
Facco E, Munari M, Gallo F, et al. Role of short latency evoked potentials in the diagnosis of brain death. Clin Neurophysiol. 2002;113:1855–66.
Savard M, Turgeon AF, Gariépy JL, Trottier F, Langevin S. Selective 4 vessel angiography in brain death: a retrospective study. Can J Neurol Sci. 2010;37:492–7.
Braum M, Ducrocq X, Huot JC, et al. Intravenous angiography in brain death: report of 140 patients. Neuroradiology. 1997;39:400–5.
Kramer AH, Roberts DJ. Computed tomography angiography in the diagnosis of brain death: a systematic review and meta-analysis. Neurocrit Care. 2014;21:539–50.
Greer DM, Strozyk D, Schwamm LH. False positive CT angiography in brain death. Neurocrit Care. 2009;11:272–5.
Shankar JJ, Vandorpe R. CT perfusion for confirmation of brain death. Am J Neuroradiol. 2013;34:1175–9.
Heran MK, Heran NS, Shemie SD. A review of ancillary tests in evaluating brain death. Can J Neurol Sci. 2008;35:409–19.
Selkuk H, Albayram S, Tureci E, et al. Diffusion-weighted imaging findings in brain death. Neuroradiology. 2012;54:547–54.
Luchtmann M, Bernarding J, Beuing O, et al. Controversies of diffusion weighted imaging in the diagnosis of brain death. J Neuroimaging. 2013;23:463–8.
Wieler H, Marohl K, Kaiser KP, Klawki P, Frössler H. Tc-99m HMPAO cerebral scintigraphy. A reliable, noninvasive method for determination of brain death. Clin Nucl Med. 1993;18:104–9.
Abdel-Dayem HM, Bahar RH, Sigurdsson GH, et al. The hollow skull: a sign of brain death in Tc-99m HM-PAO brain scintigraphy. Clin Nucl Med. 1989;14:912–6.
Bertagna F, Barozzi O, Puta E, et al. Residual brain viability, evaluated by (99m)TC-ECD SPECT, in patients with suspected brain death and with confounding clinical factors. Nucl Med Commun. 2009;30:815–21.
Berenguer CM, Davis FE, Howington JU. Brain death confirmation: comparison of computed tomographic angiography with nuclear medicine perfusion scan. J Trauma. 2010;68:553–9.
Joffe AR, Lequier L, Cave D. Specificity of radionuclide brain blood flow testing in brain death: case report and review. J Intensive Care Med. 2010;25:53–64.
Ducrocq X, Hassler W, Moritake K, et al. Consensus opinion on diagnosis of cerebral circulatory arrest using Doppler-sonography: Task Force Group on cerebral death of the Neurosonology Research Group of the World Federation of Neurology. J Neurol Sci. 1998;159:145–50.
Monteiro LM, Bollen CW, van Huffelen AC, et al. Transcranial doppler ultrasonography to confirm brain death: a meta-analysis. Intensive Care Med. 2006;32:1937–44.
de Freitas GR, André C. Sensitivity of transcranial Doppler for confirming brain death: a prospective study of 270 cases. Acta Neurol Scand. 2006;113:426–32.
Vicenzini E, Pro S, Randi F, et al. Transcranial Doppler for brain death after decompressive craniectomy: persistence of cerebral blood flow with flat EEG. Intensive Care Med. 2010;36:2163–4.
Vicenzini E, Pulitano P, Cicchetti R, et al. Transcranial Doppler for brain death in infants: the role of the fontanelles. Eur Neurol. 2010;63:164–9.
Topcluogu MA, Arsava EM, Bas DF, Kozak HH. Transorbital ultrasonographic measurement of optic nerve sheath diameter in brain death. J Neuroimaging. 2017;25:906–9.
Toscano M, Spadetta G, Pulitano P, et al. Optic nerve sheath diameter ultrasound evaluation in intensive care unit: possible role and clinical aspects in neurological critical patients’ daily monitoring. Biomed Res Int. 2017;2017:1621428.
Wijdicks EFM. The case against confirmatory tests for determining brain death in adults. Neurology. 2010;75:77–83.
Shemie SD, Hornby L, Baker A, et al. The international guidelines for determination of death phase 1 participants, in collaboration with the World Health Organization. International Guideline Development for the Determination of Death. Intensive Care Med. 2014;40:788–97.
Mathur M, Ashwal S. Pediatric brain death determination. Semin Neurol. 2015;35:116–24.
Citerio G, Crippa IA, Bronco A, Vargiolu A, Smith M. Variability in brain death determination in Europe: looking for a solution. Neurocrit Care. 2014;21:376–82.
Furton EJ. Brain death, the soul, and organic life. Natl Cathl Bioeth Q. 2002;2:455–70.
Akrami SM, Osati Z, Zahedi F, Raza M. Brain death: recent ethical and religious considerations in Iran. Transplant Proc. 2004;36:2883–7.
Lock M. Contesting the natural in Japan: moral dilemmas and technologies of dying. Cult Med Psychiatry. 1995;19:1–38.
Decreto Ministero della Salute dell’ 11 aprile 2008. Aggiornamento del Decreto del 22 agosto 1994, n. 582 relativo al Regolamento recante le modalità per l’accertamento e la certificazione di morte. Gazzetta Ufficiale n. 136 del 12 giugno 2008. http://www.gazzettaufficiale.it/gazzetta/serie_generale/caricaDettaglio?dataPubblicazioneGazzetta=2008-06-12&numeroGazzetta=136
Centro Nazionale Trapianti. Linee Guida. Applicazione delle indagini strumentali di flusso ematico cerebrale. Versione aggiornata al 20 febbraio 2009. http://www.trapianti.salute.gov.it
Acknowledgments
We are very grateful to Dr. Patrizia Pulitano for her help in selecting and editing the EEG figures.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mecarelli, O., Vicenzini, E. (2019). Brain Death. In: Mecarelli, O. (eds) Clinical Electroencephalography. Springer, Cham. https://doi.org/10.1007/978-3-030-04573-9_47
Download citation
DOI: https://doi.org/10.1007/978-3-030-04573-9_47
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04572-2
Online ISBN: 978-3-030-04573-9
eBook Packages: MedicineMedicine (R0)