Abstract
Impairment of vision is a significant, independent risk factor for falls, which are themselves a leading cause of injuries and increased healthcare costs in elderly populations. Screening and monitoring of visual function should include not only central acuity but also visual field, binocular vision , and contrast sensitivity . Correction of vision, such as by cataract surgery, has been shown to improve postural stability and reduce incidence of falls; however, caution has been advised in using multifocal glasses, as they have been shown to impair edge-contrast sensitivity and depth perception . In particular, stair negotiation is an important hazard, and exercise programs and cognitive training can reduce fall risk. Advances have been undertaken in the use of sensors to monitor falls and improve screening detection algorithms, although standardizing parameters among separate algorithms remains a challenge. In addition to complete visual and medical screening for fall risk, clinicians also should counsel patients and families on the impact of visual loss on fall risks and quality of life. Home safety inspections and reassessments of environmental hazards should be conducted regularly.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Fall risk
- Fall prevention
- Fall risk screening
- Frailty syndrome
- Postural instability
- Home safety
- Fractures
- Practice-based learning and improvement
- Systems-based learning
- Interpersonal and communication skills
A 75-year-old woman with age-related macular degeneration (ARMD) presents with new loss of vision in her right eye. Her past medical history is significant for hypertension, diabetes, and high cholesterol. Her medications are atenolol, insulin, simvastatin, and one aspirin per day. The patient is markedly hard of hearing and often forgets to turn on her hearing aids. She smokes one pack of cigarettes per day and has one glass of wine each evening. Her family history is significant for ARMD in her mother. The vision in the left eye was lost 2 years prior to presentation due to a subfoveal neovascular membrane from ARMD . She is the sole care provider for her elderly husband with Alzheimer’s dementia, and they live together in their single-family two-story home 30 miles from your office. The patient had driven herself and her husband to the appointment. Her daughter has been concerned about the increasing frailty of both parents, but the patient has refused to move previously. The patient has had four recent falls and was hospitalized 1 year ago for a hip fracture. The visual acuity was 20/200 in the right eye and counting fingers in the left eye. The pupillary, motility, slit-lamp, external, and intraocular pressure measurements were all normal. Visual field testing showed a central scotoma bilaterally. Ophthalmoscopy showed an old disciform macular scar from the prior subfoveal neovascular membrane in the left eye. The right eye showed a new subfoveal hemorrhage and underlying choroidal neovascular membrane.
Introduction
Visual loss is an important risk factor for falls in the elderly. The roles of the ophthalmologist include (1) identification of at-risk elderly patients in the eye clinic; (2) risk reduction for falls; (3) low-vision assistance for patients with impaired vision that might reduce the risk for falls; and (4) communication of the risks and the risk reduction techniques to the patient and the patient’s caregivers. Vision plays an important part in stabilization of posture, and visual impairment may increase the risk for falls independently of environmental hazards.
In the elderly population, falls are the leading cause of injury-related death and the most common cause of hospital admissions resulting from injury [1]. One estimate says that up to one-third of older adults (age 65+) fall each year and the risk of falls increases with advancing age [2]. Another study estimates about 22% or seven million Medicare beneficiaries fell in 2011 [3]. In 2000, injuries and deaths from falls cost over $19 billion, and this cost was projected to rise to more than $54.7 billion by 2020 [4].
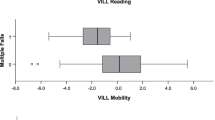
Fall risk highly correlates with frailty syndrome , a nebulously defined physiologic state in which there is reduced ability to recover from stressors [5]. Vision impairment directly impacts frailty via substantial reduction in functional capacity [5]. Another study verified a significant association between ophthalmologic surgery experience and falls in community-dwelling elderly populations [6] (Fig. 1).
Practice-Based Learning and Improvement
As visual loss is a well-documented risk factor for falls in the elderly, the ophthalmologist should be cognizant of the risks in an individual elderly patient. De Boer et al. examined a cohort of 1509 men and women and identified visual impairment as an independent risk factor for falls and fractures [7]. In the Blue Mountains Eye Study, the 2-year risk of fractures in patients with visual acuity loss, visual field deficits, and the presence of posterior subcapsular cataracts was found to be significantly higher than in persons without these findings at baseline [8]. Lord et al. studied 156 community-dwelling elderly persons and reported that impaired vision is an independent risk factor for falls, with depth perception and distant-edge-contrast sensitivity being particularly important for maintaining balance as well as detecting and avoiding environmental hazards [9]. In another prospective cohort study assessing the impact of vision on likelihood of falling, women with declines in visual acuity over 4–6 years were found to have significantly greater odds of experiencing frequent falling during the subsequent year [10]. Yet another study of fall risk assessed 1285 persons over 65 years of age and found previous falls, visual impairment, urinary incontinence, and the use of benzodiazepines to be the strongest predictors of fall risk [11]. More recently, additional studies have specifically verified visual acuity as a significant risk factor for falls and mortality in multiple settings (the USA, Sweden, Japan, Taiwan, Nigeria) and populations (independently living elderly, elderly women, patients with hip fractures , Medicare beneficiaries) [12,13,14,15,16,17].
Notably, central acuity alone may not be the only factor that is important. Lord and Menz assessed that contrast sensitivity and stereopsis are important for posture control under challenging conditions (although no effect was seen on a stable surface) [18]. Källstrand-Eriksson et al. found that stereopsis was a significant determinant of falls, along with visual acuity [13]. Pineles et al. noted that Medicare beneficiaries with disorders of binocular vision (strabismus, diplopia, amblyopia, nystagmus) had higher odds of sustaining musculoskeletal injuries, fractures , and falls [19].
Lord and Dayhew found that wearers of multifocal glasses have impaired edge-contrast sensitivity and depth perception and that the use of multifocal eyeglasses substantially increases the risk of a fall [20]. Furthermore, the population-attributable risk of falls in this cohort was found to be 35% for those wearing multifocal eyeglasses [20].
History of correction by ocular surgery also has a demonstrable association with fall risk. Schwartz et al. found that patients improved significantly in multiple postural stability indices after cataract surgery [21]. Following this, Sach et al. confirmed a decreased incidence of falls after cataract surgery using an economic analysis [22].
Practice-Based Improvement
Buckley et al. studied the impact of visual impairment on the mechanics of landing during stepping down by elderly patients (N = 12) and concluded that correcting common visual problems might be an important intervention strategy for elderly persons negotiating stairs [23]. A separate review reported that stair negotiation remains an important hazard for older persons [24]. In a randomized controlled trial, Campbell et al. assessed the efficacy and cost-effectiveness of a home safety program and a home exercise program to reduce falls and injuries in community-dwelling older people with low vision (391 women and men aged 75 years or older with visual acuity of 6/24 or worse) [25]. Participants received a home safety assessment and modification program delivered by an occupational therapist (n = 100), an exercise program prescribed at home by a physiotherapist plus vitamin D supplementation (n = 97), both interventions (n = 98), or social visits (n = 96) [25]. The main outcome measure was the number of falls and injuries resulting from falls. These authors found fewer falls occurring in the group randomized to the home safety program but not in the exercise program [25]. In light of findings from multiple studies, one systematic review reported that visual intervention strategies to improve visual function and prevent falls in older people are warranted [26].
Some studies have worked toward developing frameworks for screening, monitoring, and prevention programs that target visually impaired elderly populations [27, 28]. The proposed screening methodology includes visual acuity and visual field tests, red reflex to screen for cataracts, and dilated slit-lamp examination [27] (Fig. 2). In a randomized controlled trial, Barban et al. found that combined motor and cognitive training delivered via a touchscreen computer was effective in reducing fall risk in elderly patients [28].
There has also been a surge of promising research into the use of newer technology to monitor and predict falls [29,30,31]. Bourke et al. conducted a study incorporating machine learning to develop a lumbar sensor algorithm to detect falls [29]. A similar study conducted by Hsieh et al. uses a multiphase model to develop an algorithm for fall detection using sensors [31]. A meta-analysis aimed to develop a unified strategy for evaluating multiple fall detection algorithms and noted that dissimilarities between studies have been a barrier toward delineating common parameters associated with falls [32]. However, given the rapid expansion of studies into using sensors in elderly populations to assess falls, it is encouraging that these technologies will help significantly in preventing falls.
Fall reduction techniques and screening and monitoring programs have been shown to be useful for elderly patients with impaired or low vision. There is clear evidence that fall prevention is superior to fall treatment for elderly patients, hence the importance of steady ophthalmological care in geriatric populations.
Systems-Based Learning
The ophthalmologist should consider contacting the patient’s primary care provider as well as caregivers to inform them of the risks for falling posed by the visual loss in this elderly patient. Clinicians should be sensitive to the fact that an elderly patient may also be caring for an even more disabled or frail spouse. The loss of vision in this elderly caregiver thus might impact the care and quality of life of the spouse as well as the patient. The ophthalmologist may need to call upon the resources of a social worker, community assistance, or the family. Home safety inspections and home health visit to the patient’s living quarters might provide an opportunity for fall risk reduction. Ophthalmologists should be aware of the factors that might increase the risk for falling in their elderly patient with visual loss (e.g., poor physical conditioning and lack of activity, muscle weakness, poor balance, pre-existing difficulty with activities of daily living like dressing or bathing, cognitive impairment, dementia, and medications such as beta blockers, tranquilizers, sedatives, antidepressants). Ophthalmologists can help with fall prevention by recognizing patients at risk, including elderly patients with visual loss, and having a preprinted handout available for patients and their families that can address potential environmental home hazards (e.g., reducing clutter; improving stair railings; eliminating loose throw rugs or electrical extension cords, installing hand railing in the bathroom; and improving lighting and contrast especially on stairs). Falls in the elderly obviously impact the entire system of care including the patient and their caregivers and create potentially preventable costs to the healthcare system [3, 4, 22, 33,34,35,36,37,38].
Interpersonal and Communication Skills
The ophthalmologist may be in a position to assist the caregivers in counseling a frail, elderly patient that transfer to an assisted living situation may be helpful in reducing the risk for falls and improving the quality of life. There is also an increasingly positive outlook that newer technologies may help to monitor falls even in independently living elderly patients. Empathetic and compassionate discussions with the patient and their family might be warranted for all involved parties to make an appropriate and informed decision on placement. Patients with visual loss often have hearing loss, and the risk for morbidity increases for patients with both hearing and visual loss. A delicate and sensitive conversation with the patient may be necessary regarding the issue of the legality and safety of driving in the setting of severe visual loss.
Case Resolution
The ophthalmologist should recognize that visual loss is a risk factor for falls. Patients with visual loss would benefit from specific counseling regarding risk factor reductions and home hazard reductions to reduce fall risk. The ophthalmologist in this case helped with fall prevention in the patient by recognizing that the patient was at risk for falls including the presence of the visual loss. The ophthalmologist provided the patient and her family a handout to address potential environmental clutter. The patient and her family were very interested in the information and made numerous changes to help reduce the chance of falls.
References
Sleet DA, Moffett DB, Stevens J. CDC’s research portfolio in older adult fall prevention: a review of progress, 1985–2005, and future research directions. J Saf Res. 2008;39(3):259–67.
Centers for Disease Control and Prevention (CDC). Self-reported falls and fall-related injuries among persons aged > or =65 years–United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57(9):225–9.
Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, Adler G. Gender differences in seeking care for falls in the aged Medicare population. Am J Prev Med. 2012;43(1):59–62.
Stevens JA, Corso PS, Finkelstein EA, et al. The costs of fatal and nonfatal falls among older adults. Inj Prev. 2006;12(5):290–5.
Fhon JR, Rodrigues RA, Neira WF, Huayta VM, Robazzi ML. Fall and its association with the frailty syndrome in the elderly: systematic review with meta-analysis. Rev Esc Enferm USP. 2016;50(6):1005–13.
Eto M, Miyauchi S. Falls after ophthalmological surgery experience among the community-dwelling elderly in Japan. J Community Health Nurs. 2017;34(1):1–9.
De Boer MR, Luijm SMF, Lips P, et al. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. J Bone Min Res. 2004;19:1539–47.
Ivers RQ, Cumming RG, Mitchell P, Attebo K. Visual impairment and falls in older adults: the Blue Mountains Eye Study. J Am Geriatr Soc. 1998;46(1):58–64.
Lord SR, Dayhew J. Visual risk factors for falls in older people. J Am Geriatr Soc. 2001;49:58–64.
Coleman AL, Stone K, Ewing SK, et al. Higher risk of multiple falls among elderly women who lose visual acuity. Ophthalmology. 2004;111:857–62.
Tromp AM, Pluym SFM, Smit JH, et al. Fall-risk screening test: a prospective study on predictors for falls in community dwelling elderly. J Clin Epidemiol. 2001;54:837–44.
Rokicki W, Drozdzowska B, Czekajło A, Grzeszczak W, Wiktor K, Majewski W, Pluskiewicz W. Relationship between visual status and functional status and the risk of falls in women. The RAC-OST-POL study. Arch Med Sci. 2016;12(6):1232–8.
Källstrand-Eriksson J, Hildingh C, Bengtsson B. History of falling and visual ability among independently living elderly in Sweden. Clin Ophthalmol. 2016;10:1265–73.
Fukuoka H, Nagaya M, Toba K. The occurrence of visual and cognitive impairment, and eye diseases in the super-elderly in Japan: a cross-sectional single-center study. BMC Res Notes. 2015;8:619.
Kuang TM, Tsai SY, Liu CJ, Lee SM, Hsu WM, Chou P. The association of visual impairment and 3-year mortality among the elderly in Taiwan: the Shihpai Eye Study. J Chin Med Assoc. 2015;78(3):177–81.
Bekibele CO, Gureje O. Fall incidence in a population of elderly persons in Nigeria. Gerontology. 2010;56(3):278–83.
Loriaut P, Loriaut P, Boyer P, Massin P, Cochereau I. Visual impairment and hip fractures: a case-control study in elderly patients. Ophthalmic Res. 2014;52(4):212–6.
Lord SR, Menz HB. Visual contributions to postural stability in older adults. Gerontology. 2000;46:306–10.
Pineles SL, Repka MX, Yu F, Lum F, Coleman AL. Risk of musculoskeletal injuries, fractures, and falls in medicare beneficiaries with disorders of binocular vision. JAMA Ophthalmol. 2015;133(1):60–5.
Lord SR, Dayhew J, Howland A. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc. 2002;50:1760–6.
Schwartz S, Segal O, Barkana Y, Schwesig R, Avni I, Morad Y. The effect of cataract surgery on postural control. Invest Ophthalmol Vis Sci. 2005;46(3):920–4.
Sach TH, Foss AJ, Gregson RM, Zaman A, Osborn F, Masud T, Harwood RH. Falls and health status in elderly women following first eye cataract surgery: an economic evaluation conducted alongside a randomised controlled trial. Br J Ophthalmol. 2007;91(12):1675–9.
Buckley JG, Heasley KJ, Twigg P, Elliott DB. The effects of blurred vision on the mechanics of landing during stepping down by the elderly. Gait Posture. 2005;21:65–71.
Startzwell JK, Owens DA, Mulinger LM, Cavanagh PR. Stair negotiation in older people: a review. J Am Geriatr Soc. 2000;48:567–80.
Campbell AJ, Robertson MC, La Grow SJ, et al. Randomised controlled trial of prevention of falls in people aged > or = 75 with severe visual impairment: the VIP trial. BMJ. 2005;331(7520):817.
Abdelhafiz AH, Austin CA. Visual factors should be assessed in older people presenting with falls or hip fracture. Age Ageing. 2003;32:26–30.
Squirrell DM, Kenny J, Mawer N, Gupta M, West J, Currie ZI, et al. Screening for visual impairment in elderly patients with hip fracture: validating a simple bedside test. Eye (Lond). 2005 Jan;19(1):55–9.
Barban F, Annicchiarico R, Melideo M, Federici A, Lombardi MG, Giuli S, et al. Reducing fall risk with combined motor and cognitive training in elderly fallers. Brain Sci. 2017;7(2):pii: E19.
Bourke AK, Klenk J, Schwickert L, Aminian K, Ihlen EA, Mellone S, et al. Fall detection algorithms for real-world falls harvested from lumbar sensors in the elderly population: a machine learning approach. Conf Proc IEEE Eng Med Biol Soc. 2016;2016:3712–5.
Larizza MF, Zukerman I, Bohnert F, Busija L, Bentley SA, Russell RA, Rees G. In-home monitoring of older adults with vision impairment: exploring patients’, caregivers’ and professionals’ views. J Am Med Inform Assoc. 2014;21(1):56–63.
Hsieh CY, Liu KC, Huang CN, Chu WC, Chan CT. Novel hierarchical fall detection algorithm using a multiphase fall model. Sensors (Basel). 2017;17(2):307.
Koshmak GA, Linden M, Loutfi A, Koshmak GA, Linden M, Loutfi A, et al. Fall risk probability estimation based on supervised feature learning using public fall datasets. Conf Proc IEEE Eng Med Biol Soc. 2016;2016:752–5.
Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82:1020–3.
Kanis JA, Pitt FA. Epidemiology of osteoporosis. Bone. 1992;13(suppl 1):S7–S15.
Cummings SR, Kelsey JL, Nevitt MC, O’Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7:178–208.
Northridge ME, Nevitt MC, Kelsey JL, Link B. Home hazards and falls in the elderly: the role of health and functional status. Am J Public Health. 1995;85:509–15.
Brainsky A, Glick H, Lydick E, et al. The economic cost of hip fractures in community-dwelling older adults: a prospective study. J Am Geriatr Soc. 1997;45:281–7.
Schneider EL, Guralnick JM. The aging of America: impact on health care costs. JAMA. 1990;263:2335–40.
Acknowledgement
The authors of the chapter would like to thank Dr. David Steven Friedman for his contribution toward this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lin, W.V., Lee, A.G. (2019). Visual Loss and Falls. In: Beaver, H., Lee, A. (eds) Geriatric Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-030-04019-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-04019-2_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04017-8
Online ISBN: 978-3-030-04019-2
eBook Packages: MedicineMedicine (R0)