Abstract
This atlas diplays informative cases on brain PET/CT and PET/MR giving an insight into the added value of this imaging tool in the clinical evaluation of various brain pathologies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
(a–d) A 30-year-old patient with non-lesional right frontotemporal lobe epilepsy. Axial 18F FDG PET (a, b) and fused 18F FDG PET/MR (c, d) show perfect agreement between the two techniques with area of hypometabolism in the right temporal lobe (a–d, arrows) representing an epileptogenic focus.
Teaching point: Alteration in FDG metabolism can help determine epileptogenic foci in patients with non-lesional epilepsy
(a–d) A 31-year-old patient with left hemisphere epilepsy. Axial fused 18F FDG PET/CT (a), axial CT (b), fused 18F FDG PET/MR (c) and T2 FLAIR (d) at the level of the thalami show area of hypometabolism in the left occipitotemporal region (a, c arrows) with corresponding high signal intensity in the periventricular region of the posterior horn of the left lateral ventricle (d, arrow) raising the suspicion of previous encephalitis.
Teaching point: Combined FDG PET/MR can assist in diagnosing location of epileptogenic focus and correlative morphological changes to determine possible underlying cause
(a, b) Patient evaluated for right hemispheric epilepsy. Axial FDG PET images (a) and Z-score maps (b) show right temporal lobe hypometabolism (a, arrows) which is confirmed on quantification assessment (b, arrows), in keeping with an epileptogenic focus.
Teaching point: The use of quantification maps can help in giving a more confident diagnosis when determining the most likely epileptogenic focus in patients with epilepsy
(a, b) Fused 68Ga DOTATATE PET/MR (a) and axial post-contrast T1WI (b) show tracer-avid extra-axial lesions in the right side of the foramen magnum, right temporal lobe laterally and left temporal lobe medially (a, arrows). The focal hyper intensity adjacent to the clivus bone is the normal tracer uptake in the pituitary gland (a, FH). These correspond to small enhancing meningeal lesions (b), in keeping with multiple meningiomas.
Teaching point: Meningiomas may be considerably small-sized, and osseous structures (e.g. skull base) may hamper the diagnosis. 68Ga DOTATATE is a tracer selective for the evaluation of somatostatin receptors which are rich in different tumours, such as neuroendocrine, meningioma and paraganglioma
(a–c) Axial fused 18FCholine PET/MR (a), ADC map (b) and DWI (c) show an 18FCholine avid lesion in the left thalamus (a, arrow), with corresponding restricted diffusion on the diffusion-weighted images (b, c arrows).
Teaching point: The use of multiparametric evaluation can help identify different components of the tumour including metabolism and cellularity
(a, b) Axial fused 18FCholine PET/MR (a) and axial post-contrast T1WI (b) show mildly avid subependymal lesions with partial intraventricular extension in the anterior horn of the lateral ventricle bilaterally (a, arrows) which correspond to non-enhancing small hypointense lesions (b).
Teaching point: Non-enhancing lesions can still present with uptake on 18FCholine imaging and might be useful for treatment evaluation
(a, b) Coronal fused 18FCholine PET/MR (a, b) show a large 18FCholine avid non-germinomatous germ cell pineal body tumour prior to treatment (a) which shows interval reduction in size and tracer uptake post-treatment (b), in keeping with partial metabolic response.
Teaching point: The importance of having appropriate metabolic imaging prior to treatment as a baseline can help with better post-treatment assessment
Axial T2W FLAIR (a), axial post-contrast T1WI (b) and axial 18FCholine PET (c) in Patients 1–3
Patient 1: A 17-year-old patient with grade I pilocytic astrocytoma demonstrates normal appearing ‘white matter’ ROI (blue), ‘non-enhancing’ tumour ROI (yellow) and ‘enhancing’ tumour ROI (pink) (a), enhancing tumour (b) with increased 18FCholine uptake in the enhancing component (c)
Patient 2: An 18-year-old patient with grade I schwannoma demonstrates a high-intensity left frontal lobe mass (a), which shows peripheral enhancement with central non-enhancing area (b) which corresponds to increased 18FCholine uptake in the enhancing component (c)
Patient 3 : A 21-year-old patient with grade IV glioblastoma (GBM) demonstrates high signal in the right temporal lobe with areas of susceptibility artefacts (a), which shows minimal enhancement at its posterior-lateral component (b, arrow) that corresponds to mildly increased 18FCholine uptake.
Teaching point: The use of multiparametric evaluation can help identify different components of the tumour and possible sites for treatment targeting
(a–c) Axial fused 18F DOPA PET/MR (a), axial T2W FLAIR (b) and axial post-contrast T1WI (c) show bilateral increased 18F DOPA tracer uptake in the thalami (left > right) (a, arrows) with corresponding high-signal changes (b, arrows) and no significant enhancement on the post-contrast image (c). The left thalamic lesion was proven upon biopsy to be a low-grade tumour with transformation into high-grade glioma.
Teaching point: 18F DOPA tracer uptake can detect early transformation of gliomas and impact treatment decision
(a–d) Coronal T2W FLAIR (a), axial post-contrast T1WI (b), axial ADC map (c), axial 18F DOPA PET (d) and axial fused 18F DOPA PET/MR (e) demonstrate a high-signal, non-enhancing area in the right frontal lobe (a, b) with diffusion restriction (c) in a patient previously operated for a high-grade glioma tumour in the right frontal lobe with similar stable postoperative MR appearances compared to prior postoperative imaging over the last 4 years. However, further imaging with 18F DOPA shows increased tracer uptake in the right frontal lobe tumour (d, e), consistent with active residual disease. The patient had further treatment 2 weeks later which demonstrated active tumour which was completely removed.
Teaching point: Functional imaging can detect residual disease in otherwise morphologically stable changes in postoperative brain tumours
(a–d) Axial fused 18F DOPA PET/MR (a, c) and axial fused 18FCholine PET/MR (b, d) in Patients 1 and 2. Patient 1: Biopsy-proven WHO grade IV left thalamic GBM demonstrates increased 18F DOPA and 18FCholine tracer uptake in the left thalamic lesion (a, b, arrows). Patient 2: Biopsy-proven WHO grade II left thalamic glioma with feature of transformation to grade III shows increased 18F DOPA tracer uptake in the left thalamus (c, arrow) but no corresponding 18FCholine tracer uptake (d).
Teaching point: The evaluation of brain lesions with different tracers can give an insight of various components within the tumour which help in assessing tumour grade and further impact management decision
(a–d) Axial fused Tau tracer PET/CT (a, c) and axial fused amyloid PET/MR (c, d) in the same patient imaged 2 weeks apart demonstrated increased Tau tracer uptake in the posterior parietal and occipital regions of the brain cortex (a, c) with amyloid PET showing completely different regions of amyloid deposition in the frontal lobes (d).
Teaching point: Tau and amyloid tracers can show different patterns of tracer distribution in the same patient. This may aid in the understanding of the different mechanisms in the degenerative changes occurring in patients presenting with dementia-like features
(a, b) Axial fused 18F-FDG PET/MR (a) and post-contrast T1WI (b) demonstrate intense increased FDG uptake in the periventricular region of the posterior horn of the left lateral ventricle (a, arrow) which corresponds to an enhancing lesion on the post-contrast MR (b), in a patient with CNS lymphoma.
Teaching point: Intense uptake on FDG can differentiate between CNS lymphoma and primary brain tumours like GBM which usually show less FDG uptake
(a–c) Axial post-contrast T1WI (a, b) and axial fused 18F-FDG PET/CT (c) demonstrated an enhancing left frontal lobe mass in a patient diagnosed with GBM (a). Follow-up postoperative MR imaging shows postoperative changes in the left frontal lobe with no convincing enhancement of residual tumour (b). Additional functional imaging with 18F-FDG PET/CT shows an avid focus in the left frontal lobe (c) which is consistent with active residual disease.
Teaching point: Functional imaging can determine the presence of residual disease in postoperative patients with unremarkable postoperative morphological imaging
(a–e) A 64-year-old patient with background AL amyloidosis treated with chemotherapy, presenting with widespread myoclonus, confusion, seizures and reduced consciousness. Axial fused 18F FDG PET/CT (a, c), axial PET (b, d) and DWI image (e) show focal increased cortical uptake in right frontal and right parietal lobes (a–d, arrows), which correspond to areas of restricted diffusion on MRI (e), raising possible vasculitis secondary to cerebral amyloid angiopathy.
Teaching point: Visualization of vascular wall uptake in small vessel vasculitis is beyond the resolution of PET, however indirect signs can be demonstrated by the presence of abnormal cortical tracer uptake in the corresponding vascular territory. Furthermore, multiparametric imaging is required in assessing these challenging cases
(a, b) Patient with previous lymphoma completed chemotherapy 2 months ago and presented with cerebellar signs, and MRI showed a right cerebellar mass. Axial fused 18F FDG PET/CT (a) and post-contrast T1WI (b) show intensely avid right cerebellar lesion (a, arrow) corresponding to the enhancing lesion (b, arrow), in keeping with relapsed CNS lymphoma .
Teaching point: Given the usual intense 18F FDG uptake in lymphoma, evaluation of areas with usually high metabolic activity like the brain is possible, and evaluation with FDG PET/CT is particularly useful in assessing disease relapse in patients with prior history of lymphoma
(a–c) Axial fused 18F FDG PET/CT (a), axial 18F FDG PET (b) and noncontrast CT (c) show a FDG-avid lesion in the left temporal lobe (a, b arrows) which corresponds to a hyperdense lesion on subsequent CT (c, arrow) in a patient who underwent PET/CT for lung cancer staging, in keeping with brain metastasis.
Teaching point: Including the brain in the whole-body PET/CT imaging can sometimes detect metastatic brain lesions and is advised to be routinely done in cases with suspected malignancies that have or are likely to have brain metastasis
(a–c) Axial fused 68Ga DOTATATE PET/CT (a), axial 68Ga DOTATATE PET (b) and contrast-enhanced T1WI MRI (c) show 68Ga DOTATATE intensely avid left temporal fossa lesion (a, b arrows) corresponding to an enhancing left temporal extra-axial lesion on MRI (c, arrow) in which the differential included dural-based metastasis and meningioma. The reminder of the68Ga DOTATATE PET/CT did not show uptake elsewhere, and findings were keeping with a meningioma.
Teaching point: Imaging with 68Ga DOTATATE PET can help narrow down the differential diagnosis due to the positive uptake in lesions with somatostatin receptors, e.g. meningiomas or other neuroendocrine tumours
(a–d) Axial fused 18F FDG PET/CT (a), axial 18F FDG PET (b), axial T2WI (c) and post-contrast T1WI (d) show area of focal reduction of tracer uptake in the right thalamus (a, b, arrows) which correspond to an area of high T2 signal and mild enhancement on MRI (c, d arrows) in a patient with multiple sclerosis.
Teaching point: Brain lesions can present as areas of reduced tracer uptake which may be missed, and comparison between both hemispheres is key
(a–c) Axial fused 18F FDG PET/CT (a), axial 18F FDG PET (b) and 3D MIP (c) in a patient with worsening left arm, leg weakness and ataxia show increased tracer uptake in the medial temporal lobes, much more marked on the left side (a–c, arrows). These appearances can be seen in limbic encephalitis.
Teaching point: Recognizing uptake patterns in certain conditions can help aid in the diagnosis
(a–d) Sagittal 18F FDG PET (a), sagittal T1WI (b), axial T2WI (c) and Z-score maps (d) show reduced FDG uptake in the left frontotemporal lobe (a, arrow) corresponding to cerebral atrophy on MRI (b, c arrows) and confirmed on quantification assessment (d, arrows), in keeping with frontotemporal dementia.
Teaching point: Multimodality imaging can help recognize different patterns of dementia
(a–d) Axial 18F FDG PET (a), axial T1WI (b), axial T2WI (c) and Z-score maps (d) show reduced FDG uptake in the frontotemporal lobes bilaterally more pronounced in the frontal lobes (a, arrows) corresponding to cerebral atrophy on MRI (b, c arrows) and confirmed on quantification assessment (d, arrows), in keeping with frontotemporal dementia .
Teaching point: Multimodality imaging can help recognize different patterns of dementia
(a–d) Sagittal 18F FDG PET (a), sagittal fused 18F FDG PET/MR (b), axial T2WI (c) and Z-score maps (d) show reduced FDG uptake in the temporoparietal lobes bilaterally (a, b arrows) corresponding to cerebral atrophy on MRI (c) and confirmed on quantification assessment (d), in keeping with Alzheimer’s dementia .
Teaching point: Multimodality imaging can help recognize different patterns of dementia
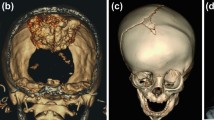
(a–c) Axial CT (a), MET/PET (b) and axial fused PET/CT (c) show increased uptake in the residual tumour in the right temporal lobe. Bottom images show the differences in uptake in the tumour region and in the contralateral normal lobe.
Teaching point: MET/PET has a significant impact in assessing tumour recurrence. Case courtesy of Dr. Castellucci, University St. Orsola Malpighi, Bologna, Italy
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Al Riyami, K., Fraioli, F. (2019). Clinical Atlas of Brain PET/CT. In: Fraioli, F. (eds) PET/CT in Brain Disorders. Clinicians’ Guides to Radionuclide Hybrid Imaging(). Springer, Cham. https://doi.org/10.1007/978-3-030-01523-7_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-01523-7_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-01522-0
Online ISBN: 978-3-030-01523-7
eBook Packages: MedicineMedicine (R0)