Abstract
Surgery remains the cornerstone therapy for early-stage lung and esophageal cancers. It is expected that the number of thoracic procedures for lung and esophageal disease will increase in the future (Siegel et al. CA Cancer J Clin 62(4):220–241, 2012). Optimal pain management can be very challenging after thoracic surgery for multiple reasons. Not only is inadequate pain control significant for humanitarian reasons, it is also linked to increased pulmonary and extrapulmonary complications (Richardson et al. J Cardiovasc Surg 40:445–456, 1999). The risks of pulmonary complications can be mitigated by appropriate pain management (Ballantyne, Anesth Analg 86:598–612, 1998). For much of the modern era of medicine, postoperative pain management has been primarily accomplished by systemic opioids. Following thoracic surgery, intravenous opioids alone are often insufficient to adequately control pain and have been supplemented with the application of local anesthetics using various regional techniques. The most recent development in the evolution of local anesthetics is liposomal bupivacaine, a novel slow-release local anesthetic formulation. The local anesthetic is encapsulated utilizing an innovative delivery system known as DepoFoam®, without alteration to its molecular structure, and is steadily released over 72–96 h.
At the University of Texas MD Anderson Cancer Center, our pain management strategy for thoracic procedures has undergone a major change over the last few years. For the better part of the last two decades, we have utilized epidurals for postoperative pain management in patients having thoracic surgery. With the combination of long-acting local anesthetics and regional techniques such as paravertebral and posterior intercostal nerve blocks, we have moved away from the use of catheters for postoperative pain management. At our institution, we have successfully incorporated long-acting local anesthetics into surgery-specific, evidence-based treatment protocols which utilize multimodal analgesia such as nonsteroidal anti-inflammatory drugs, N-methyl-D-aspartate (NMDA) antagonists, and peripheral nerve blocks. Though initial results are promising, further studies are warranted to better understand the efficacy and long-term safety profile of long-acting local anesthetics such as liposomal bupivacaine in the thoracic surgery population.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Local anesthetics
- Liposomal bupivacaine
- Regional anesthesia
- Thoracic epidural anesthesia
- Thoracic paravertebral block
- Intercostal block
- Direct interpleural anesthesia
- Serratus plane block
- Phrenic nerve block
- Post-thoracotomy pain
- Ipsilateral shoulder pain
-
Though optimal pain management for thoracic surgery can be quite challenging considering the numerous contributing mechanisms, a comprehensive pain management strategy can improve overall patient safety and satisfaction.
-
Local anesthetics work by inhibiting membrane depolarization along neurons by binding to the alpha subunit of intracellular voltage-gated sodium channels; they may also possess some degree of antagonism toward the potassium (K+) and calcium (Ca2+) channels and NMDA receptors.
-
Liposomal bupivacaine, a novel slow-release local anesthetic formulation, encapsulates the local anesthetic by utilizing an innovative delivery system known as DepoFoam®. The bilayered lipid septa provide a stable and reliable platform for the prolonged release of medications (72–96 h) without alteration to its molecular structure.
-
Liposomal bupivacaine does not diffuse through tissues in the same manner as conventional bupivacaine. Consequently, meticulous infiltration technique is imperative to ensure best results regardless of regional technique. Decreased spread means more injections are needed in closer proximity than with traditional bupivacaine.
-
The bupivacaine contained in liposomal bupivacaine is free-base bupivacaine form, distinct from bupivacaine HCl, salt form of bupivacaine. Providers should be cognizant of the fact that different formulations of bupivacaine are not bioequivalent even if the milligram dosage is the same.
-
Alternatives to systemic opioids and thoracic epidurals include regional techniques such as the paravertebral, intercostal, phrenic, intrapleural, serratus anterior plane, as well as local wound infiltration.
-
Combining minimally invasive surgery with multimodal, regional, and pharmacological approaches to analgesia can provide a higher level of postoperative analgesia while reducing undesired side effects of narcotic usage, such as nausea, vomiting, constipation, and respiratory depression.
-
Novel long-acting local anesthetic such as liposomal bupivacaine offer a promising analgesic solution, but further studies are warranted to better understand the efficacy and long-term safety profile of these newer local anesthetics.
-
This chapter reviews the localized regional techniques currently used at the University of Texas MD Anderson Cancer Center.
Introduction
Surgery remains the cornerstone therapy for early-stage lung and esophageal cancers. It is expected that the number of thoracic procedures for lung and esophageal disease will increase in the future [1]. Optimal pain management can be very challenging after thoracic surgery for multiple reasons. There are numerous mechanisms that contribute to the pain a patient experiences: disruption of the skin and muscles, ligamentous damage, and rib fractures and dislocations, as well as chest tube and shoulder pain from diaphragmatic irritation and positioning. Not only is inadequate pain control significant for humanitarian reasons, it is also linked to increased pulmonary and extrapulmonary complications [2]. The risks of pulmonary complications can be mitigated by appropriate pain management [3]. The literature has shown that early postoperative pain is predictive of long-term pain after thoracotomy. Providers have responded by incorporating aggressive pain management strategies to decrease the high incidence of chronic pain within this vulnerable patient population [4]. The healthcare costs of chronic pain developing from acute pain can represent a significant financial burden for the patient, as well as the community. In fact, some researchers have estimated that the lifetime economic costs of a single 30-year-old patient suffering from chronic pain will reach one million US dollars [5]. For much of the modern era of medicine, postoperative pain management has been primarily accomplished by systemic opioids. Following thoracic surgery, intravenous opioids alone are often insufficient to adequately control pain and have been supplemented with the application of local anesthetics using various regional techniques.
Local anesthetics work by inhibiting the signal propagation along neurons by binding to the alpha subunit of intracellular voltage-gated sodium channels. Neurons utilize the sodium-potassium pump (Na + K+ ATPase) to maintain a negative resting potential difference of −60 to −70 mV through active transport and passive diffusion of ions [6]. The sodium-specific channels are membrane-bound proteins, made up of alpha and beta subunits that exist in three states: resting (nonconducting), open (conducting), and inactivated (nonconducting). Local anesthetics inhibit the action potential necessary to propagate signals along neurons by blocking the influx of sodium needed for membrane depolarization. Secondarily, local anesthetics may possess some degree of antagonism toward the potassium (K+) and calcium (Ca2+) channels, as well as NMDA receptors. By inhibiting the propagation of peripheral nociceptive signals, regional and local anesthesia have the potential to reduce or eliminate postoperative pain as well as mitigate the endocrine and metabolic response to surgery.
Techniques for the administration of local anesthetics to block nociception include (1) surgical site infiltration (single injection or catheter), (2) peripheral nerve blocks (single injection or catheter), and (3) neuraxial anesthesia. With the advent of liposomal local anesthetic agents, it is now possible for thoracic anesthesiologists to tailor or combine regional techniques to suit specific surgical scenarios. Significant pain reduction can be achieved for several days with single-shot injections of multiple, distinct, even unplanned surgical sites without the dependence on perineural catheters. This chapter reviews the history of local anesthetics from the coca leaf to liposomal bupivacaine, the methodology behind specific regional blocks for thoracic surgery, and how the development of long-acting, liposomal anesthetics may improve our ability to manage postoperative thoracic pain.
History of Local Anesthetics
Origins in the Americas
Derived from shrubs of the genus Erythroxylum native to Central and South America, the coca leaf held an important social, religious, and medicinal role of the Incan people from as far back as 1900 B.C. [7]. Initially reserved for the aristocracy, coca’s use became widespread following the fall of the Incan empire in 1532. From that time until the dawn of the twentieth century, most scientists championed its energizing and euphoric properties while neglecting its other effects. The full potential for medical cocaine wasn’t realized until 1880, when Russian physician Basil von Anrep of the University of Würzburg recommended its use as a surgical anesthetic based on numerous experiments upon animals and himself. It was Viennese ophthalmologist Carl Koller (1857–1944) who performed the first operation using local anesthetic on a patient with glaucoma on September 11, 1884. The impact of his work was instantaneous and global, with over 60 publications concerning local anesthesia using cocaine in the United States and Canada by the end of 1885 [8] (Table 60.1).
Synthetic Anesthetics
By the turn of the twentieth century, the potential toxicity and addictive properties of cocaine were well established, and a search for the ideal local anesthetic had begun. In 1904, German chemist Alfred Einhorn (1856–1917) patented novocaine and 17 other para-aminobenzoic derivatives which are now collectively known as ester group local anesthetics [9]. Novocaine, or alternatively named procaine, had its own limitations. Like all ester-based anesthetics, novocaine was limited by a relatively low potency and strong association with hypersensitivity and anaphylaxis among patients and healthcare workers [10]. The serious deficiencies of the ester group anesthetics encouraged the development of another group of anesthetics.
In 1946, Nils Löfgren and Bengt Lundquist developed a xylidine derivative they called “lidocaine,” whose chemical composition was distinct from novocaine and was found to be more potent and safer, with little allergenic potential [11]. Bupivacaine, mepivacaine, and most of the other amide group anesthetics would be introduced over the next half century. Amide anesthetics possess an aromatic head which is linked to a hydrocarbon chain by an amide bond rather than an ester. This results in amide anesthetics being more stable and hence less prone to causing allergic reactions as compared to ester anesthetics. As a butyl group homologue of mepivacaine, bupivacaine was initially discarded as it was found to be four times more toxic. Since its introduction in 1965, the nature of the central nervous system (CNS) and cardiac toxicity linked to bupivacaine has been well chronicled. The discovery of mepivacaine’s optically active isomers, and the extensive study of their decreased toxicology, led to the selection and development of a pure S-(-) enantiomer ropivacaine in 1996. Levobupivacaine, the S-(-) enantiomer of bupivacaine, was approved by the FDA in 1999 [12] (Table 60.2).
Current Long-Acting Local Anesthetics
Although there are a number of amino-amide anesthetics currently available, two of the most commonly used in the United States include bupivacaine and ropivacaine. Due to their longer duration of action, they have been the most common choice for the prevention and treatment of postsurgical pain by local infiltration, peripheral nerve blocks, as well as epidural and spinal anesthesia. For bupivacaine, the typical concentration ranges from 0.0625% to 0.5%. The alteration in concentration allows for a differential blockade in terms of various degrees of sensory and/or motor blockade. Lower concentrations of local anesthetic allow sensory blockade, while increasing higher concentrations provide motor blockade. The potential for cardiotoxicity with bupivacaine use is usually sufficiently mitigated by appropriate measures taken to minimize systemic absorption. Most adverse reactions are linked to direct vascular injection and infiltration of areas at higher risk of absorption or to slow metabolic degradation by the liver. Treatment of overdose or inadvertent intravascular injection has been reported in both animal and human case reports with intralipid, an intravenous lipid emulsion whose prompt administration can reverse even life-threatening cardiotoxicity. Though the precise mechanism for reversal is unclear, it is possible that the addition of the intralipid acts as a reservoir “sink” which creates a gradient that draws the lipophilic toxins away from the affected tissues. Lipid emulsions may also work by overriding the inhibition of mitochondrial carnitine-acylcarnitine translocase which provide fuel for the myocardium [13,14,15,16].
As an alternative to bupivacaine with a greater safety margin, ropivacaine was found to have less cardiotoxicity and possess better sensorimotor dissociation at lower doses. In practice, this results in greater motor sparing than bupivacaine at lower doses. Typical concentrations for ropivacaine are 0.1–1%. The onset and duration of action for ropivacaine are similar to bupivacaine though the former has less variability secondary to its more homogenous composition [17]. As with all non-liposomal local anesthetics, the duration of action has been limited by the redistribution of the anesthetic away from the targeted site.
Liposomal Bupivacaine and the Introduction of a New Class of Anesthetics
The most recent development in the evolution of local anesthetics may represent an attractive alternative in the management of postoperative pain. Liposomal bupivacaine (LB), a novel slow-release local anesthetic formulation, encapsulates the local anesthetic by utilizing an innovative delivery system known as DepoFoam®. These multivesicular liposomes consist of hundreds of water-filled polyhedral compartments which are separated by biocompatible, biodegradable, lipid-based vesicles ranging in size between 10 and 30 μm. The bilayered lipid septa provide a stable and reliable platform for the prolonged release of medications. The local anesthetic is encapsulated by DepoFoam® without alteration to its molecular structure and is steadily released over 72–96 h [18,19,20,21] (Fig. 60.1).
Safety
The safety of LB appears to be comparable to other local anesthetic agents. Initial studies by Bramlett et al. found when comparing LB to bupivacaine, both formulations were safe and well tolerated with a low incidence of adverse events [22]. Golf et al., based on application during bunionectomy, found that LB provided superior analgesia and was well tolerated and safe with a slightly higher incidence of medication-related adverse events, most notably postoperative nausea and vomiting [23]. Gorfine et al. concluded in their study of patients undergoing hemorrhoidectomy that a 300 mg formulation of LB was safe [24]. The effect of LB on QTc interval was studied by Naseem et al. who demonstrated that doses up to 750 mg did not cause significant prolongation [25]. Although initial studies evaluating the safety and efficacy were done with patients in soft tissue and orthopedic models, a recent review evaluated six randomized controlled double-blind trials in adult patients that used a single dose of LB for postoperative pain control in a more diverse group of surgical patients. Essentially, this review concluded that LB when used in therapeutic doses was well tolerated, had a higher safety margin, and showed a favorable safety profile compared to bupivacaine and control groups [26]. A Cochrane meta-analysis of liposomal bupivacaine for use in local wound infiltration (10 reports, 1377 participants) also found it to have a comparable safety profile to bupivacaine HCL [27].
Preparation and Application
LB is manufactured as a single-use 20 ml vial, which is 1.3% formulation containing a total of 266 mg of bupivacaine. The bupivacaine contained in LB is a free-base bupivacaine form which differs from other frequently used amide-type, bupivacaine-based local anesthetics which contain the salt form of bupivacaine, bupivacaine HCl. Therefore, 266 mg of bupivacaine free base is chemically the molar equivalent to 300 mg of bupivacaine HCl. Providers should be cognizant of the fact that different formulations of bupivacaine are not bioequivalent even if the milligram dosage is the same. Therefore, it is not possible to convert dosing between LB and other formulations.
Liposomal agents should be injected slowly with frequent aspiration to check for the blood and minimize the risk of intravascular injection. It is important to recognize that LB does not diffuse through tissues in the same manner as conventional bupivacaine. Consequently, meticulous infiltration technique is imperative to ensure best results regardless of regional technique. For surgical site injections, that means using a deep tissue infiltration technique with continuous injection of the anesthetic from the fascia to dermis. Decreased spread means more injections are needed in closer proximity than with traditional bupivacaine. Many surgeons in clinical practice often expand the volume of the injectate up to a total volume of 300 mL with either normal saline (0.9%) for injection or lactated Ringer’s solution. Volumes used in clinical practice range from 20 to 300 mL (diluted) depending on the size of the surgical site. The onset of action is longer than with conventional bupivacaine as a natural consequence of the slow release of the anesthetic from the liposomes. The addition of normal bupivacaine HCL to the LB at a ratio that does not exceed 1:2 can hasten the onset of sensory blockade. The addition of greater amounts of bupivacaine or the combination of LB with other unapproved anesthetics or agents can cause the premature breakdown of the liposomal matrix and potentially a dangerous uncontrolled release of the anesthetic.
Contraindications and Precautions
LB is contraindicated in obstetrical paracervical block anesthesia. Although LB has not been used in paracervical blocks, the use of bupivacaine HCl with this technique has resulted in fetal bradycardia and death; hence, it should not be used in this type of block. Furthermore, the manufacturer cautions that there is a potential risk of severe life-threatening adverse effects associated with the administration of bupivacaine; therefore, LB should be administered in a setting where trained personnel and equipment are available to promptly treat patients who show evidence of neurological or cardiac toxicity. Care should be exercised to avoid accidental intravascular injection of LB. Multiple reports have reported convulsions and cardiac arrest following accidental intravascular injection of bupivacaine and other amide-containing products.
The aforementioned studies have shown that LB is a promising drug formulation which can potentially improve the postoperative pain control in surgical patients. However, further studies are needed in both larger patient populations and wider array of patient populations to enhance the current level of knowledge of the drug’s advantages and disadvantages and define the areas of best application. Until recently there had been only two studies, both limited by their retrospective nature, on the efficacy and safety of this liposomal formulation in thoracic patients.
Regional Anesthetic Techniques for Thoracic Surgery
Thoracic Epidural Anesthesia
The infusion of local anesthetics, typically bupivacaine or ropivacaine, into the epidural space has been considered the “gold standard” for optimal pain management in postoperative pain after thoracotomy; however, this technique may not be feasible for a number of reasons: contraindications such as those patients with certain antithrombotic agents, systemic heparinization, or local and systemic infection who possess an elevated risk for epidural hematoma or abscess, respectively. Thoracic epidural anesthesia (TEA) has also been shown to have a high incidence of failure, with rates as high as 32% having been reported in the literature [28, 29]. The efficacy of the thoracic epidural is highly operator dependent, and successful catheter placement can be influenced by many factors, such as the patient’s body habitus, patient positioning, and anatomical variations. The undesirable side effects of epidural anesthesia, the resultant bilateral sympathectomy, and epidural opioid exposure are numerous and can include postoperative hypotension, decreased pulmonary function, urinary retention, and pruritus [30,31,32]. Pain management strategies have continued to evolve, and some research has begun to suggest a shift away from systemic opioids and thoracic epidurals toward regional nerve blockade with lower rates of adverse events [33].
Shift Toward More Peripheral Regional Techniques
Alternatives to thoracic epidural have been described with variable success, including techniques which target the paravertebral, intercostal, phrenic, intrapleural, serratus anterior plane, in addition to local wound infiltration. The most enduring argument which supports the continued use of thoracic epidurals is its ability to provide analgesia for several days. In contrast, the efficacy of single-shot administration of local anesthetic has naturally been limited to the duration of action for the applied local anesthetic. Anesthesia providers have attempted to prolong the analgesic benefit by utilizing other additives such as corticosteroids, epinephrine, and clonidine or by combining different local anesthetics to the anesthetic with variable success [34]. Perineural catheters can also continuously infuse local anesthetic and thus prolong the duration of regional techniques; however, there are conflicting reports about their ability to appropriately control postoperative thoracotomy pain. Plausible reasons for these conflicting reports are these catheters require greater technical expertise and are prone to migration, kinking, occlusion, and infection [35,36,37,38].
At the University of Texas MD Anderson Cancer Center, our pain management strategy for thoracic procedures has undergone a major change over the last few years. For the better part of the last two decades, we have utilized epidurals for postoperative pain management in patients having thoracic surgery. With the introduction and refinement of regional techniques such as paravertebral and intercostal blocks, surgical preference has more often favored the use of these more peripheral blocks in lieu of epidurals specifically for thoracic procedures.
Thoracic Paravertebral Blockade (Please See Figs. 59.5 and 59.6 from Chap. 59)
First introduced by Hugo Sellheim in 1905, thoracic paravertebral blockade (TPVB) fell out of favor during most of the twentieth century until its reintroduction by Eason and Wyatt in 1979. TPVB has continued to evolve with the use of various landmark techniques and adjuncts such as pressure sensors, fluoroscopy, nerve stimulators and, most recently, ultrasound-guidance. The resultant ipsilateral, segmental, somatic, and sympathetic blockade has become increasingly popular in the treatment of acute and chronic pain [39]. For patients undergoing thoracotomy, several large meta-analyses have concluded that when compared with TEA, TPVB has comparable analgesic benefit, levels of cortisol stress markers, and frequency of major complications but with improved preservation of lung function and significantly less hypotension, nausea and vomiting, pruritus, urinary retention and block failure [40,41,42,43].
In the treatment of post-thoracotomy pain, TPVB has traditionally been limited in reliability and duration. Using landmark-based techniques, TPVB has commonly been described as easy to learn and safe though failure and complication rates can be as high as 10% and 5%, respectively [44,45,46,47]. The advancement of ultrasound-guided techniques allows for the placement of local anesthetic with greater precision and reliability [48, 49]. Prior to LB, the duration of single-injection TPVB was generally limited to less than 24 h. Despite the correct needle tip position by ultrasound-guided techniques, catheter migration into the adjacent prevertebral, epidural, intercostal, and pleural space remains problematic (see Fig. 60.2) [50]. When compared to percutaneous TPVB, catheters inserted surgically have generally been even less reliable though techniques are quite variable with some institutional success being greater than others [36].
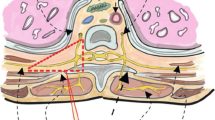
Intercostal anatomy. (Reprinted from Anaesthesia, Dravid and Paul, Copyright (2007), with permission from John Wiley and Sons. (Dravid and Paul [108]))
The combination of ultrasound-guided techniques and LB has the potential to substantially improve the reliability, duration, and therefore the practicality of the TPVB in treating post-thoracotomy pain. While the potential for TPVB and LB seems promising, there is currently insufficient data to evaluate the efficacy, safety, and practicality of utilizing LB for TPVB in thoracic surgery. At least one study found that local wound infiltration with LB was similar if not superior to TPVB with conventional bupivacaine following reconstructive breast surgery [51]. With the advent of very long-acting anesthetics, the utility of the TPVB is uncertain. Further studies on post-thoracotomy patients are needed which directly compare the use of LB and TPVB versus other more peripheral regional techniques, such as intercostal nerve blocks, before conclusions can be drawn on the future role of TPVB in thoracic surgery.
Intercostal Nerve Block
Although epidural LB use has been described as apparently being safe in healthy volunteers, more specifically, other than two retrospective studies, LB’s safety and efficacy have not been studied in thoracic surgical population. At our institution, posterior intercostal blocks with LB have replaced TEA as the preferred technique for postoperative analgesia in thoracic surgery, with patients reporting lower pain scores and using less opioids (Fig. 60.3).
Rice block methylene blue. Posterior intercostal block with LB and methylene blue. Thoracoscopic visualization allows accurate injection of LB into the intercostal space without violation of the parietal pleura. Note that the site of injection is at the level of the innermost intercostal muscles and that the drug tracks medially to the paravertebral space. Methylene blue was added to the LB for purposes of illustrating the extent of subpleural spread only. (Reprinted from The Annals of Thoracic Surgery, D Rice, Copyright (2015), with permission from Elsevier. (Rice et al. [109]))
Depending upon the surgical approach, a five-level posterior intercostal block is either done under direct visualization for open procedures or with thoracoscopic guidance for video-assisted thoracoscopic or robotic-assisted thoracoscopic procedures. Specifically, after the skin has been infiltrated with 1–2 ml of LB, a 12 mm camera thoracoscopy port is introduced at the appropriate site. Using a 22G spinal needle, the surgeon advances the needle over the superior edge of the rib approximately 5–7 cm lateral to the anatomic midline. Meticulous technique is used to advance the spinal needle to the innermost intercostal muscle without disrupting the parietal pleura. This is extremely important so that the local anesthetic remains confined to the intercostal space and is not lost to the pleural space. Typically this injection entails a 2 ml injection of LBs over the superior edges of ribs 6 through 10, but obviously the location of injection can be tailored toward other surgical sites [52]. The remaining volume of LB is injected at the remaining port sites or surgical wounds. Thoracoscopic visualization can significantly enhance the accurate injection into the intercostal space without interrupting the parietal space as local anesthetic can then egress out. Trainees can more easily appreciate the appropriate injection and demarcation of the intercostal space if 2 ml of methylene blue are added to the local injection solution (see Fig. 60.4).
Rice results. The results from one comparison of posterior intercostal block with LB vs. TEA with bupivacaine HCl. Pain scores and narcotic requirements for patients who received (A–C) LB or (D–F) thoracic epidural analgesia. The dashed lines indicate thoracotomy; the solid lines indicate minimally invasive surgery. Wilcoxon signed-rank test. (Max maximum, MSO4 morphine sulfate, POD postoperative day). (Reprinted from The Annals of Thoracic Surgery, D Rice, Copyright (2015), with permission from Elsevier. (Rice et al. [109]))
With respect to the local anesthetic solution used for intercostal blocks, many institutions use 0.5% bupivacaine as local anesthetic, although some use 0.25% bupivacaine or 1% lidocaine [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67]. The rate of infusion is generally 5–7 mL/h for an average-sized adult which typically helps establish five-level dermatomal analgesia to pinprick unilaterally.
Wanting to cover a larger surgical area, surgeons at our institution initially mixed LB with normal saline to create a larger volume to be injected into the surgical site; however, according to the updated prescribing information for LB, some of the surgeons now also utilize 0.25% bupivacaine combined with LB when performing intercostal blocks. According to the updated prescribing information, it is feasible to administer bupivacaine HCl with LB; however, this may impact the pharmacokinetic and/or physicochemical properties of LB, and this effect is concentration dependent [68]. Therefore, bupivacaine HCl and LB may be administered simultaneously in the same syringe, and bupivacaine HCl may be injected immediately prior to LB as long as the bioequivalent ratio of the dose of bupivacaine HCl solution to LB does not exceed 1:2. The typical 266 mg vial of LB may be coadministered with 150 mg of bupivacaine HCl. The toxic effects of these drugs are additive, and their administration should be used with caution including monitoring for neurologic and cardiovascular effects related to toxicity [68]. Although our institution like many other institutions mixes local anesthetics in clinical practice with the intent of getting faster onset and longer duration of local anesthetics, it should be kept in mind that mixing various local anesthetics at times can lead to variable onset, duration, and unpredictable potency. Likewise, mixing of different formulations of local anesthetics with their respective concentrations and volumes can increase the chances of drug error. Furthermore, despite having negative aspiration, usage of recommended dosage and avoidance of intravascular injections, no currently available method of monitoring can prevent local anesthetic toxicity; therefore, it is incumbent upon the anesthesia provider to be steadfastly vigilant and maintain preparation to treat systemic toxicities that may manifest unexpectedly.
Direct Interpleural Anesthesia
Although first described in 1984, interpleural blockade via the introduction of local anesthetic in between the parietal and visceral pleura has not gained widespread usage [69]. An epidural catheter is placed in the pleural space through a 16 Tuohy needle after the patient is placed in the lateral position with the operative side up. The site of insertion is in the eighth intercostal space approximately 8–10 cm from the posterior anatomic midline with the needle being introduced at 30–40° angle to the skin. The bevel of the Tuohy needle is faced upward as the needle is advanced over the rib and as the parietal pleura is entered. The plunger of the syringe may move passively inward due to the negative pressure in the pleural space during inspiration. A multi-orificed epidural catheter is then advanced 5–6 cm into the pleural space, and after negative aspiration, local anesthetic can then be injected.
Typically, bupivacaine is rebolused in intermittent boluses at either 4, 6, or 8 h; however, there are institutions which use a constant infusion of bupivacaine [56, 70,71,72,73,74,75,76,77,78,79].
The block’s potential for several different types of complications has limited its use. For instance, the most common complication is that of a pneumothorax described in 2% of the patients [80]. Other complications described include pleural effusions, Horner’s syndrome, infection, catheter displacement or rupture, and even toxic symptoms when the local anesthetic is absorbed systemically. More recently, phrenic nerve paralysis has been described as an additional complication [81]. Patient position, particularly when a patient is sitting upright, as well as site of lowest chest tube placement most likely influences the pooling of local anesthetic near the diaphragm. The decrease in forced vital capacity, especially if done bilaterally or in patients with compromised respiratory function, can further worsen respiratory status. This impairment in pulmonary function from diaphragmatic weakness is a plausible explanation for the significantly worse pulmonary function with interpleural analgesia when compared with paravertebral analgesia [56].
Serratus Plane (SAP) Block
Distal to the lateral cutaneous branches of the intercostal nerve, sensory divisions pass through the muscles of the chest. With ultrasound guidance, the practitioner can achieve analgesia of different regions of the chest by injecting local anesthetic between those muscle layers. Injection between pectoralis major and minor, the so-called Pecs I and II blocks, achieves somatic blockade of the anterior chest. Injection of anesthetic superficial to the serratus anterior muscle adjacent to the fourth and fifth intercostal spaces along the midaxillary line results in anesthesia of the lateral chest. The size of distribution is related to the volume of the injectate. With the injection of 20 ml, the area of sensory deficit covers from the scapula to the nipple, T4–T9. The initial study was small and simply demonstrated the application of the block and the subsequent sensory block and spread of local anesthetic by MRI [82]. The utility of the SAP block for thoracic surgery has yet to be determined. It has been noted that the SAP block likely doesn’t cover the posterior primary rami, the anterior cutaneous branches of the intercostal nerve and afferents of the autonomic nervous systems [83, 84].
The SAP block may be best suited for procedures with anterolateral incisions such as anterior muscle-sparing thoracotomy or anterolateral thoracotomy, though these may need to be supplemented with local wound infiltration as the incision approaches the limits of sensory blockade. The block did not extend past the inferior angle of the scapula, so this block may not be appropriate for posterior muscle-sparing thoracotomy, as is common at our institution, or thoracoscopic surgery with more posterior incision sites. It may be useful as a rescue technique for patients with a failed thoracic epidural or those experiencing pain at the chest tube site. One such case has already been reported in a patient status post esophagectomy whose epidural had failed the pain was successfully treated by the SAP block with catheter-based infusion [85]. Little research to date has validated this technique for surgery in comparison with other approaches.
Local Surgical Site Infiltration
The rationale for wound infiltration with local anesthetics is to target the most proximal and selective site responsible for the perception of pain, the peripheral nociceptors. With direct infiltration into the surgical site, the local anesthetic can simply and effectively provide analgesia for a variety of surgical procedures. Furthermore, infiltration in this manner is usually not associated with severe side effects such as local toxicity, wound infection, and impaired wound healing [86, 87]. Long-acting amide local anesthetics such as bupivacaine and ropivacaine have been shown to provide superior pain control over opioids and are commonly used in the postoperative period for infiltrative, regional, and neuraxial blocks [88,89,90]. Until recently, the duration of analgesia with infiltration into the surgical site in single doses was limited by the specific local anesthetic used. As mentioned earlier, LB diffuses within tissue less than conventional local anesthetics. A dose can be diluted to make large volumes that can then be injected using a deep infiltration technique. At our institution, some surgeons have found increased success by injecting LB invanvoverlapping, crosshatch fashion as a means to avoid patchy block (Table 60.3).
Phrenic Nerve Block and Other Blocks Targeting Ipsilateral Shoulder Pain (ISP)
The significance of post-thoracotomy ipsilateral shoulder pain (ISP) differs from incisional thoracotomy pain in quality, location, etiology, and treatment. It is a common occurrence, affecting up to 85% of patients following thoracic surgery [91, 92]. The pain can be severe despite the well-functioning TEA. The exact distribution of pain is variable but lies within the C4–C5 dermatomes, sharing a common innervation with the phrenic nerve. The duration of pain typically lasts for hours but can persist for days or longer, with some patients experiencing chronic pain more than 6 months after surgery [93, 94].
Etiology
ISP is correlated with the extent of pleural disruption, size of thoracotomy incision, transection of major bronchial airways, patient BMI, and length of surgery [95, 96]. Currently, no pharmacological or regional treatment exists which can completely eradicate or prevent the pain. ISP is considered a type of pain that is usually referred from the afferents of the phrenic nerve. Originating from the third, fourth, and fifth cervical nerve roots, the phrenic nerve contains sensory, motor, and sympathetic fibers. It provides the only afferents to the diaphragm and afferents for the pleura and pericardium of the thorax as well as the diaphragmatic peritoneum. ISP is most commonly thought to be the result of phrenic nerve impulses brought on by intraoperative pleural irritation by intrathoracic dissection, bronchial transection, and chest tube placement.
The precise etiology of post-thoracotomy ISP remains debatable. While targeted phrenic blockades are usually effective, they are not universally effective at eliminating ISP for all patients. A series of case reports concluded that there may be a dual etiology of ISP wherein some patients’ pain is caused by phrenic nerve afferents, while other patients’ ISP is from direct shoulder ligament strain [95]. In one study, suprascapular block performed postoperatively had no effect on patient’s pain [97]. When compared directly to periphrenic diaphragmatic fat pad infiltration, suprascapular nerve block was significantly less effective at preventing ISP [93]. This suggests that ISP is not related to the strain of the acromioclavicular or glenohumeral joints for most patients unless localizing signs of musculoskeletal shoulder pain are present [95, 98].
Though representing a minority of patients with ISP, patients presenting with pain localized to the shoulder, elicited with palpation or movement, benefited from suprascapular nerve block 85% of the time [98]. Unlike the interscalene nerve, the suprascapular is not adjacent to the phrenic and therefore is not associated with concomitant phrenic blockade and diaphragmatic palsy.
Treatment
NSAIDs such as intravenous diclofenac or ketorolac can be effective in reducing ISP, but they are not universally effective and should be used with caution in certain patient populations such as those with chronic renal insufficiency [99]. Neither standard TEA nor intrapleural infusion is typically effective at preventing ISP; however, lower rates have been associated with epidural catheter placement above T5 [100, 101]. Higher thoracic catheters may provide enough local anesthetic spread for a sensory blockade of phrenic nerve afferents. The resultant hypotension and decreased pulmonary function from higher epidural blocks may limit this approach in patients with low cardiopulmonary reserve.
Scawn, Pennefather, and colleagues demonstrated that injection of lidocaine into the diaphragmatic periphrenic fat pad at the end of surgery reduced the incidence of ISP for up to 2 h [91]. The injection of ropivacaine 0.2% provided a relatively selective sensory blockade which significantly reduced the incidence (32% vs. 64%) and delayed the median onset (36 vs. 16 h) of ISP with no difference in postoperative arterial blood gases [102]. It has been suggested that targeting of the phrenic nerve at alternative locations, such as the periphrenic fat pad around the hilum, may affect the efficacy of the block, but such variations have not been validated and require further study [103].
Others have shown that post-thoracotomy ISP can be significantly reduced by interscalene nerve blockade. Barak et al. employed an interscalene block with bupivacaine to reduce ISP though the effect was limited to less than 24 h [104]. The exact mechanism of pain relief from interscalene block is unclear because of the high incidence of simultaneous phrenic nerve blockade despite the use of relatively low volumes of local anesthetic and ultrasound guidance [105]. The same is true for supraclavicular nerve block which also has a high rate of simultaneous phrenic nerve involvement. The use of an ultrasound-guided supraclavicular approach to perform a targeted phrenic nerve block with ropivacaine had a 65% relative rate reduction of ISP in patients undergoing lobectomy or pneumonectomy [106]. A phrenic nerve catheter was placed, but the ISP was most severe on the day of surgery. There was no difference in rescue analgesics used on postoperative day 1. By specifically targeting the phrenic nerve for blockade, the block may more effectively reduce ISP without as much of the associated upper extremity motor weakness.
Phrenic nerve blockade is not without risks. Hemidiaphragm phrenic nerve palsy results in a decrease in vital capacity, forced expiratory volume per second, and maximum inspiratory flow [105]. These effects are well tolerated even for those with preexisting pulmonary disease but may cause respiratory distress in patients with contralateral diaphragm dysfunction. Long-acting local anesthetics such as LB should therefore be used with caution in this patient population. The use of catheter-based ropivacaine, or the development of liposomal ropivacaine, may have the advantage of more selective sensory blockade and therefore less phrenic nerve palsy.
Many of these studies utilized the relatively short-acting lidocaine, and no studies to date have evaluated agents with a duration of action exceeding 24 h. The use of short-acting agents has potentially limited the benefits of decreased ISP. The duration of ISP is variable however, and the use of long-acting agents may not be beneficial for many patients. Further prospective studies are needed to directly compare the safety and efficacy of the aforementioned techniques and to determine whether long-acting modalities such as catheter-based infusions or liposomal amide anesthetics are beneficial. Until then, practitioners should use their clinical judgment to devise a treatment strategy for ISP that is most appropriate for their patient population.
Conclusion
In summation, it is well recognized that optimal pain management for thoracic surgery remains challenging given the multiple mechanisms that contribute to postoperative pain. Combining minimally invasive surgery with multimodal, multidisciplinary regional and pharmacological approaches to analgesia can mitigate pain and suffering by acting at various levels of the nervous system. This holistic and comprehensive pain management strategy can improve overall patient safety and satisfaction by providing a higher level of postoperative analgesia while reducing the undesired side effects of narcotic usage, such as nausea, vomiting, constipation, and respiratory depression. Furthermore, improving postoperative pain control can impact hospital stay, reduce the rates of postsurgical complications and readmissions, prevent opioid dependence, and, potentially, reduce mortality [107]. At our institution, we have successfully incorporated long-acting local anesthetics into surgery-specific, evidence-based treatment protocols which utilize multimodal analgesia such as nonsteroidal anti-inflammatory drugs, N-methyl-D-aspartate (NMDA) antagonists, and peripheral nerve blocks. Although novel long-acting local anesthetic such as LB has created excitement among providers and may represent a significant advancement in the evolution of local anesthesia, it should be remembered that they are not a panacea but rather a component of a comprehensive pain strategy. Moreover, given the limited number of case reports and studies available specifically in the thoracic surgery population, further studies are warranted to better understand not only the efficacy but also the long-term safety profile of long-acting local anesthetics such as LB.
References
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62(4):220–41.
Richardson J, Sabanathan S, Shah R. Post-thoracotomy spirometric lung function: the effect of analgesia. A review. J Cardiovasc Surg. 1999;40:445–56.
Ballantyne JC, Carr DB, de Ferranti S, Suarez T, Lau J, Chalmers TC, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 1998;86:598–612.
Bayman EO, Parekh KR, Keech J, Selte A, Brennan TJ. A prospective study of chronic pain after thoracic surgery. Anesthesiol. 2017;126:938–51.
Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97(2):534–40.
Butterworth J, Mackey D, Wasnick J. Morgan & Mikhailʼs Clinical anesthesiology. 5th ed. New York [etc.]: McGraw-Hill Education/Medical; 2013.
Biondich AS, Joslin JD. Coca: high altitude remedy of the ancient Incas. Wilderness Environ Med. 2015;26(4):567–71.
Calatayud J, González A. History of the development and evolution of local anesthesia since the coca leaf. Anesthesiol. 2003;98(6):1503–8.
Link WJ. Alfred Einhorn, Sc. D: inventor of novocaine. Dent Radiog Photog. 1959;32(1):20.
Guptill AE. Novocain as a skin irritant. Dent Cosmos. 1920;62:1460–1.
Löfgren N, Lundquist B. Studies on local anaesthetics: II. Svenks Kem Tidskr. 1946;58:206–17.
Ruetsch Y, Bönibc T, Borgeatac A. From cocaine to ropivacaine: the history of local anesthetic drugs. Curr Top Med Chem. 2001;1(3):175–82.
Weinberg GL, VadeBoncouer T, Ramaraju GA, Garcia-Amaro MF, Cwik MJ. Pretreatment or resuscitation with a lipid infusion shifts the dose-response to bupivacaine-induced asystole in rats. Anesthesiol. 1998;88(4):1071–5.
Weinberg G, Ripper R, Feinstein DL, Hoffman W. Lipid emulsion infusion rescues dogs from bupivacaine-induced cardiac toxicity. Reg Anesth Pain Med. 2003;28(3):198–202.
Rosenblatt M, Abel M, Fischer G, Itzkovich C, Eisenkraft J. Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest. Anesthesiology. 2006;105(1):217–8.
Litz R, Popp M, Stehr S, Koch T. Successful resuscitation of a patient with ropivacaine-induced asystole after axillary plexus block using lipid infusion. Anaesthesia. 2006;61(8):800–1.
Klein SM, Greengrass RA, Steele SM, D'Ercole FJ, Speer KP, Gleason DH, et al. A comparison of 0.5% bupivacaine, 0.5% Ropivacaine, and 0.75% Ropivacaine for interscalene brachial plexus block. Anesth Analg. 1998;87(6):1316–9.
Angst MS, Drover DR. Pharmacology of drugs formulated with DepoFoam®: a sustained release drug delivery system for parenteral administration using multivesicular liposome technology. Clin Pharmacokinet. 2006;45(12):1153–76.
Lambert WJ, Los K. In: Rathbone MJ, et al., editors. Modified-release drug delivery technology. Volume 2. 2nd ed. New York: Informa Healthcare; 2008. p. 207–14.
Bergese S, Onel E, Portillo J. Evaluation of DepoFoam® bupivacaine for the treatment of postsurgical pain. Pain Manag. 2011;1(6):539–47.
Chahar P, Cummings KC III. Liposomal bupivacaine: a review of a new bupivacaine formulation. J Pain Res. 2012;5:257–64.
Bramlett K, Onel E, Viscusi E, Jones K. A randomized, double-blind, dose-ranging study comparing wound infiltration of DepoFoam® bupivacaine, an extended-release liposomal bupivacaine, to bupivacaine HCl for postsurgical analgesia in total knee arthroplasty. Knee. 2012;19(5):530–6.
Golf M, Daniels S, Onel E. A phase 3, randomized, placebo-controlled trial of DepoFoam®® bupivacaine (extended-release bupivacaine local analgesic) in bunionectomy. Adv Ther. 2011;28(9):776.
Gorfine S, Onel E, Patou G, Krivokapic Z. Bupivacaine extended-release liposome injection for prolonged postsurgical analgesia in patients undergoing hemorrhoidectomy: a multicenter, randomized, double-blind, placebo-controlled trial. Dis Colon Rectum. 2011;54(12):1552–9.
Naseem A, Harada T, Wang D, Arezina R, Lorch U, Onel E, et al. Bupivacaine extended release liposome injection does not prolong QTc interval in a thorough QT/QTc study in healthy volunteers. J Clin Pharmacol. 2012;52(9):1441–7.
Portillo J, Kamar N, Melibary S, Quevedo E, Bergese S. Safety of liposome extended-release bupivacaine for postoperative pain control. Front Pharmacol. 2014;5:90.
Hamilton TW, Athanassoglou V, Mellon S, Strickland LH, Trivella M, Murray D, Pandit HG. Liposomal bupivacaine infiltration at the surgical site for the management of postoperative pain. Cochrane Database Syst Rev. 2017;2:CD011419.
Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000;321(7275):1493.
Rigg J, Jamrozik K, Myles P, Silbert B, Peyton P, Parsons R, et al. Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet. 2002;359(9314):1276–82.
Leslie K, Myles P, Devereaux P, Williamson E, Rao-Melancini P, Forbes A, et al. Neuraxial block, death and serious cardiovascular morbidity in the POISE trial. Br J Anaesth. 2013;111(3):382–90.
de Leon-Casasola OA, Parker B, Lema MJ, Harrison P, Massey J. Postoperative epidural bupivacaine-morphine therapy experience with 4,227 surgical cancer patients. Anesthesiology. 1994;81(2):368–75.
Ready LB. Acute pain: lessons learned from 25,000 patients. Reg Anesth Pain Med. 1999;24(6):499–505.
Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiol. 2012;116:248–73.
Goravanchi F, Kee SS, Kowalski AM, Berger JS, French KE. A case series of thoracic paravertebral blocks using a combination of ropivacaine, clonidine, epinephrine, and dexamethasone. J Clin Anesth. 2012;24(8):664–7.
Allen M, Halgren L, Nichols F, Cassivi S, Harmsen W, Wigle D, et al. A randomized controlled trial of bupivacaine through Intracostal catheters for pain management after thoracotomy. Ann Thorac Surg. 2009;88(3):903–10.
Helms O, Mariano J, Hentz J, Santelmo N, Falcoz P, Massard G, et al. Intra-operative paravertebral block for postoperative analgesia in thoracotomy patients: a randomized, double-blind, placebo-controlled study. Eur J Cardiothorac Surg. 2011;40:902–6.
Gebhardt R, Mehran RJ, Soliz J, Cata JP, Smallwood AK, Feeley TW. Epidural versus ON-Q local anesthetic infiltrating catheter for post-thoracotomy pain control. J Cardiothorac Vasc Anesth. 2013;27:423–6.
Detterbeck FC. Efficacy of methods of intercostal nerve blockade for pain relief after thoracotomy. Ann Thorac Surg. 2005;80:1550–9.
Eason MJ, Wyatt R. Paravertebral thoracic block-a reappraisal. Anaesthesia. 1979;34:638–42.
Yeung JH, Gates S, Naidu BV, Wilson MJ, Gao SF. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2:CD009121.
Baidya DK, Khanna P, Maitra S. Analgesic efficacy and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2014;18(5):626–35.
Scarci M, Joshi A, Attia R. In patients undergoing thoracic surgery is paravertebral block as effective as epidural analgesia for pain management? Interact Cardiovasc Thorac Surg. 2010;10(1):92–6.
Matyal R, Montealegre-Gallegos M, Shnider M, Owais K, Sakamuri S, Shakil O, et al. Preemptive ultrasound-guided paravertebral block and immediate postoperative lung function. Gen Thorac Cardiovasc Surg. 2015;63(1):43–8.
Karmaker MK. Thoracic paravertebral block. Anesthesiol. 2001;95:771–80.
Richardson J, Vowden P, Sabanathan S. Bilateral paravertebral analgesia for major abdominal vascular surgery: a preliminary report. Anaesthesia. 1995;50:995–8.
Coveney E, Weltz CR, Greengrass R, Iglehart JD, Leight GS, Steele SM, et al. Use of paravertebral block anesthesia in the surgical management of breast cancer: experience in 156 cases. Ann Surg. 1998;227:496–501.
Lönnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade. Failure rate and complications. Anaesthesia. 1995;50(9):813–5.
Krediet AC, Moayeri N, van Geffen GJ, Bruhn J, Renes S, Bigeleisen PE, et al. Different approaches to ultrasound-guided thoracic paravertebral block: an illustrated review. Anesthesiol. 2015;123(2):459–74.
Denny NM. Editorial I: location, location, location! Ultrasound imaging in regional anaesthesia. Br J Anaesth. 2005;94(1):1–3.
Luyet C, Meyer C, Herrmann G, Hatch GM, Ross S, Eichenberger U. Placement of coiled catheters into the paravertebral space. Anaesthesia. 2012;67(3):250–5.
Abdelsattar JM, Boughey JC, Fahy AS, Jakub JW, Farley DR, Hieken TJ, et al. Comparative study of liposomal bupivacaine versus paravertebral block for pain control following mastectomy with immediate tissue expander reconstruction. Ann Surg Oncol. 2016;23(2):465–70.
Nunn JF, Slavin G. Posterior intercostal nerve block for pain relief after cholecystectomy. Anatomical basis and efficacy. Br J Anaesth. 1980;52:253–60.
Bilgin M, Akcali Y, Oguzkaya F. Extrapleural regional versus systemic analgesia for relieving post thoracotomy pain: a clinical study of bupivacaine compared with metamizol. J Thorac Cardiovasc Surg. 2003;126:1580–3.
Watson DS, Panian S, Kendall V, Maher DP, Peters G. Pain control after thoracotomy: bupivacaine versus lidocaine in continuous extrapleural intercostal nerve blockade. Ann Thorac Surg. 1999;67:825–9.
Sabanathan S, Smith PJ, Pradhan GN, Hashimi H, Eng JB, Mearns AJ. Continuous intercostal nerveblock for pain relief after thoracotomy. Ann Thorac Surg. 1988;46:425–6.
Richardson J, Sabanathan S, Mearns AJ, Shah RD, Goulden C. A prospective, randomized comparison of interpleural and paravertebral analgesia in thoracic surgery. Br J Anaesth. 1995;75:405–8.
Mozell EJ, Sabanathan S, Mearns AJ, Bickford-Smith PJ, Majid MR, Zografos G. Continuous extrapleural intercostal nerve block after pleurectomy. Thorax. 1991;46:21–4.
Kaiser AM, Zollinger A, De Lorenzi D, Largiader F, Weder W. Prospective, randomized comparison of extrapleural versus epidural analgesia for post thoracotomy pain. Ann Thorac Surg. 1998;66:367–72.
Deneuville M, Bisserier A, Regnard JF, Chevalier M, Levasseur P, Herve P. Continuous intercostal analgesia with 0.5% bupivacaine after thoracotomy: a randomized study. Ann Thorac Surg. 1993;55:381–5.
Richardson J, Sabanathan S, Jones J, Shah RD, Cheema S, Mearns AJ. A prospective, randomized comparison of preoperative and continuous balanced epidural or paravertebral bupivacaine on post-thoracotomy pain, pulmonary function and stress responses. Br J Anaesth. 1999;83:387–92.
Barron DJ, Tolan MJ, Lea RE. A randomized controlled trial of continuous extra-pleural analgesia post-thoracotomy: efficacy and choice of local anaesthetic. Eur J Anaesthesiol. 1999;16:236–45.
Majid AA, Hamzah H. Pain control after thoracotomy: an extrapleural tunnel to provide a continuous bupivacaine infusion for intercostal nerve blockade. Chest. 1992;101:981–4.
Perttunen K, Nilsson E, Heinonen J, Hirvisalo EL, Salo JA, Kalso E. Extradural, paravertebral and intercostal nerve blocks for post-thoracotomy pain. Br J Anaesth. 1995;75:541–7.
Richardson J, Sabanathan S, Eng J, et al. Continuous intercostal nerve block versus epidural morphine for post thoracotomy analgesia. Ann Thorac Surg. 1993;55:377–80.
Debreceni G, Molnar Z, Szelig L, Molnar TF. Continuous epidural or intercostal analgesia following thoracotomy: a prospective randomized double-blind clinical trial. Acta Anaesthesiol Scand. 2003;47:1091–5.
Matthews PJ, Govenden V. Comparison of continuous paravertebral and extradural infusions of bupivacaine for pain relief after thoracotomy. Br J Anaesth. 1989;62:204–5.
Sullivan E, Grannis FW Jr, Ferrell B, Dunst M. Continuous extrapleural intercostal nerve block with continuous infusion of lidocaine after thoracotomy: a descriptive pilot study. Chest. 1995;108:1718–23.
[Internet]. 2017 [cited 31 May 2017]. Available from: https://www.exparel.com/hcp/pdf/EXPAREL_Prescribing_Information.pdf.
Kvalheim L, Reiestad F. Interpleural catheter in the management of postoperative pain. Anesthesiol. 1984;61:A231.
Mann LJ, Young GR, Williams JK, Dent OF, McCaughan BC. Intrapleural bupivacaine in the control of post thoracotomy pain. Ann Thorac Surg. 1992;53:449–54.
Scheinin B, Lindgren L, Rosenberg PH. Treatment of post thoracotomy pain with intermittent instillations of intrapleural bupivacaine. Acta Anaesthesiol Scand. 1989;33:156–9.
Schneider RF, Villamena PC, Harvey J, Surick BG, Surick IW, Beattie EJ. Lack of efficacy of intrapleural bupivacaine for postoperative analgesia following thoracotomy. Chest. 1993;103:414–6.
Francois T, Blanloeil Y, Pillet F, Moren J, Mazoit X, Geay G, et al. Effect of interpleural administration of bupivacaine or lidocaine on pain and morphine requirement after esophagectomy with thoracotomy: a randomized, double-blind and controlled study. Anesth Analg. 1995;80:718–23.
Ferrante FM, Chan VW, Arthur GR, Rocco AG. Interpleural analgesia after thoracotomy. Anesth Analg. 1991;72:105–9.
Silomon M, Claus T, Huwer H, Biedler A, Larsen R, Molter G. Interpleural analgesia does not influence post thoracotomy pain. Anesth Analg. 2000;91:44–50.
Miguel R, Hubbell D. Pain management and spirometry following thoracotomy: a prospective, randomized study of four techniques. J Cardiothorac Vasc Anesth. 1993;7:529–34.
Symreng T, Gomez MN, Rossi N. Intrapleural bupivacaine v saline after thoracotomy: effects on pain and lung function—a double-blind study. J Cardiothorac Anesth. 1989;3:144–9.
Tartiere J, Samba D, Lefrancois C, et al. Intrapleural bupivacaine analgesia after thoraco-abdominal incision for oesophagectomy. Eur J Anaesthesiol. 1991;8:145–9.
Brockmeier V, Moen H, Karlsson BR, Fjeld NB, Reiestad F, Steen PA. Interpleural or thoracic epidural analgesia for pain after thoracotomy. A double blind study. Acta Anaesthesiol Scand. 1993;38:317–21.
Strømskag KE, Minor B, Steen PA. Side effects and complications related to interpleural analgesia: an update. Acta Anaesthesiol Scand. 1990;34:473–7.
Lander GR. Interpleural analgesia and phrenic nerve paralysis. Anaesthesia. 1993;48:315–6.
Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107–13.
Tighe SQ, Karmakar MK. Serratus plane block: do we need to learn another technique for thoracic wall blockade? Anaesthesia. 2013;68(11):1103–6.
Conacher ID. Pain relief after thoracotomy. Br J Anaesth. 1990;65:806–12.
Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician. 2015;18(3):E421–4.
Scott NB. Wound infiltration for surgery. Anaesthesia. 2010;65:67–75.
Gupta A. Wound infiltration with local anaesthetics in ambulatory surgery. Curr Opin Anesthesiol. 2010;23(6):708–13.
Ersayli DT, Gurbet A, Bekar A, Uckunkaya N, Bilgin H. Effects of perioperatively administered bupivacaine and bupivacaine-methylprednisolone on pain after lumbar discectomy. Spine. 2006;31(19):2221–6.
Kuthiala G, Chaudhary G. Ropivacaine: a review of its pharmacology and clinical use. Indian J Anaesth. 2011;55(2):104–10.
Sakai N, Inoue T, Kunugiza Y, Tomita T, Mashimo T. Continuous femoral versus epidural block for attainment of 120° knee flexion after total knee arthroplasty: a randomized controlled trial. J Arthroplasty. 2013;28(5):807–14.
Scawn NDA, Pennefather SH, Soorae A, Wang JYY, Russell GN. Ipsilateral shoulder pain after thoracotomy with epidural analgesia: the influence of phrenic nerve infiltration with lidocaine. Anesth Analg. 2001;93(2):260–4.
Yousefshahi F, Predescu O, Colizza M, Asenjo JF. Postthoracotomy ipsilateral shoulder pain: a literature review on characteristics and treatment. Pain Res Manag. 2016;2016:3652726.
Martinez-Barenys C, Busquets J, de Castro PE, Garcia-Guasch R, Perez J, Fernandez E, et al. Randomized double-blind comparison of phrenic nerve infiltration and suprascapular nerve block for ipsilateral shoulder pain after thoracic surgery. Eur J Cardiothorac Surg. 2011;40(1):106–12.
Stammberger U, Steinacher C, Hillinger S, Schmid RA, Kinsbergen T, Weder W. Early and long-term complaints following video-assisted thoracoscopic surgery: evaluation in 173 patients. Eur J Cardiothorac Surg. 2000;18:7–11.
Bamgbade OA, Dorje P, Adhikary GS. The dual etiology of ipsilateral shoulder pain after thoracic surgery. J Clin Anesth. 2007;19(4):296–8.
Bunchungmongkol N, Pipanmekaporn T, Paiboonworachat S, Saeteng S, Tantraworasin A. Incidence and risk factors associated with ipsilateral shoulder pain after thoracic surgery. J Cardiothorac Vasc Anesth. 2014;28(4):991–4.
Tan N, Agnew NM, Scawn ND, Pennefather SH, Chester M, Russell GN. Suprascapular nerve block for ipsilateral shoulder pain after thoracotomy with thoracic epidural analgesia: a double-blind comparison of 0.5% bupivacaine and 0.9% saline. Anesth Analg. 2002;94(1):199–202.
Saha S, Brish EL, Lowry AM, Boddu K. In select patients, ipsilateral post-thoracotomy shoulder pain relieved by suprascapular nerve block. Am J Ther. 2011;18(4):309–12.
Burgess FW, Anderson DM, Colonna D, Sborov MJ, Cavanaugh DG. Ipsilateral shoulder pain following thoracic surgery. Anesthesiol. 1993;78:365–8.
Pennefather SH, Akrofi ME, Kendall JB, Russell GN, Scawn NDA. Double-blind comparison of intrapleural saline and 0.25% bupivacaine for ipsilateral shoulder pain after thoracotomy in patients receiving thoracic epidural analgesia. Br J Anaesth. 2005;94(2):234–8.
Misiołek H, Karpe J, Copik M, Marcinkowski A, Jastrzębska A, Szelka A, et al. Ipsilateral shoulder pain after thoracic surgery procedures under general and regional anesthesia - a retrospective observational study. Kardiochir Torakochirurgia Pol. 2014;11(1):44–7.
Danelli G, Berti M, Casati A, Bobbio A, Ghisi D, Mele R, et al. Ipsilateral shoulder pain after thoracotomy surgery: a prospective, randomized, double-blind, placebo-controlled evaluation of the efficacy of infiltrating the phrenic nerve with 0.2% wt/vol ropivacaine. Eur J Anaesthesiol. 2007;24(7):596–601.
Rychlik IJ, Burnside N, McManus K. The phrenic nerve infiltration for ipsilateral shoulder pain. Eur J Cardiothorac Surg. 2012;41(3):716.
Barak M, Iaroshevski D, Poppa E, Ben-Nun A, Katz Y. Low-volume interscalene brachial plexus block for post-thoracotomy shoulder pain. J Cardiothorac Vasc Anesth. 2007;21(4):554–7.
Bergmann L, Martini S, Kesselmeier M, Armbruster W, Notheisen T, Adamzik M, et al. Phrenic nerve block caused by interscalene brachial plexus block: breathing effects of different sites of injection. BMC Anesthesiol. 2015;16:45.
Blichfeldt-Eckhardt MR, Laursen CB, Berg H, Holm JH, Hansen LN, Ørding H, et al. A randomised, controlled, double-blind trial of ultrasound-guided phrenic nerve block to prevent shoulder pain after thoracic surgery. Anaesthesia. 2016;71(12):1441–8.
White PF, Kehlet H. Improving postoperative pain management: what are the unresolved issues? Anesthesiol. 2010;112:220–5.
Dravid RM, Paul RE. Interpleural block – Part 1. Anaesthesia. 2007;62(10):1039–49.
Rice DC, Cata JP, Mena GE, Rodriguez-Restrepo A, Correa AM, Mehran RJ. Posterior intercostal nerve block with LB: an alternative to thoracic epidural analgesia. Ann Thorac Surg. 2015;99(6):1953–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Case Discussion
Case Discussion
A 75-year-old female is scheduled for a right VATS requiring multiple wedges due to metastatic colon cancer. Past medical history is significant for obesity (BMI 47 kg/m2), hypertension, stable coronary artery disease which is medically managed, and obstructive sleep apnea for which patient uses CPAP nightly. Patient stopped smoking 2 weeks ago but has a 100 pack-year smoking history. The patient received tramadol XR 300 mg PO and celecoxib 200 mg PO as part of her ERAS preemptive regimen. Pregabalin was held to avoid postoperative sedation given her history of sleep apnea. Additionally, the surgeon performed a deep tissue injection at the incision sites using a total of 40 cc of a solution made of 20 ml of 1.3% LB mixed with 20 ml of 0.9% sterile normal saline. During the course of the surgery, vigorous surgical bleeding required conversion to open thoracotomy incision. As the surgery is concluding, patient is administered 1 mg of hydromorphone for tachypnea. The patient wakes up in extreme pain from the thoracotomy incision site.
-
1.
How could the risk of insufficient local anesthetic coverage been decreased in this case?
-
(a)
The LB should be diluted in order to achieve an adequate volume to cover the planned surgical sites along with the most common contingencies. A maximum ratio of 14:1 normal saline to LB can be used to achieve a volume of 300 ml though typical amounts are in the range of 40–80 ml. As mentioned previously, bupivacaine HCl is the only local anesthetic not contraindicated in patients receiving LB. The bupivacaine HCl to LB ratio should not exceed 1:2 which corresponds with a maximum dose of 150 mg bupivacaine HCl for 266 mg LB. Best practice would be to administer a portion of the diluted LB around the time of incision to manage intraoperative pain (within 4 hrs after preparation in a syringe) and to inject the remainder of the solution upon surgical closure.
-
(a)
-
2.
What additional medications can be utilized in combination with LB?
-
(a)
Other analgesics such as intravenous acetaminophen, dexmedetomidine, ketamine, ketorolac, and narcotics are safe to administer following LB administration. At our institution, ketorolac is routinely given to our thoracic surgery patients during skin closure provided patient does not have contraindications such as compromised renal function and high risk for postoperative bleeding. Other local anesthetics such as lidocaine are absolutely contraindicated in a patient who has received liposomal bupivacaine.
-
(a)
-
3.
Are there any additional regional blocks which can be used in the setting of LB usage?
-
(a)
At our institution, we do not administer any local anesthetics, including bupivacaine HCl, for several days following the use of LB. That said, it may be safe to administer an appropriately low dose of bupivacaine HCl by TEA, TPVB, or intercostal block in the case of a failed LB surgical site injection. There is insufficient evidence to date on the use of regular bupivacaine HCl to supplement missed pain areas in the setting of the recent administration of LB. Though risk of bupivacaine toxicity from a slow-release LB is probably low, it is difficult to know how high free bupivacaine concentrations may rise in the setting of intravascular injection or in combination with bupivacaine HCl administered by other regional techniques. The risk benefit analysis has to be considered by the providing anesthesiologist for the given patient and situation.
-
(a)
-
4.
What if the surgeon initially administered LB by five-level posterior intercostal nerve block? The thoracotomy incision and chest tube site are well covered by the block, and the patient has minimal pain upon emergence. The patient is taken to the PACU, and the blood pressure is noted to be 85/55 mmHg with a heart rate of 55 bpm.
-
(a)
Depending on the site of injection and volume of injectate, significant spread of local anesthetic can occur from the intercostal space to the TPVS and epidural space. Consequently, relative hypotension and bradycardia can occur in the setting of posterior intercostal blockade with LB. At our institution, this presentation is most common following esophagectomy when the posterior intercostal blocks are performed within a few centimeters of the TPVS. Correctable causes of hypotension such as relative hypovolemia and cardiac dysfunction should be ruled out. If the patient is comfortable without signs or symptoms of cardiac or respiratory distress, a colloid is usually given as the blood pressure often will have some response to volume expansion even in the setting of minimal blood loss. With continued monitoring and expectant management, the relative hypotension usually resolves within the first 6-24 h following surgery.
-
(a)
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Williams, W.H., Heir, J.S., Sekhon, A.K. (2019). Long-Acting Local Anesthetics for Analgesia Following Thoracic Surgery. In: Slinger, P. (eds) Principles and Practice of Anesthesia for Thoracic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-00859-8_60
Download citation
DOI: https://doi.org/10.1007/978-3-030-00859-8_60
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-00858-1
Online ISBN: 978-3-030-00859-8
eBook Packages: MedicineMedicine (R0)