Abstract
Combined cardiac and thoracic procedures are rare; however thanks to progress of surgical techniques and recent advances in the use of extracorporeal life support (ECLS) techniques the number of these procedures is increasing.
Anaesthesia and optimal perioperative management for these complex, high-risk surgical interventions requires an expertise in both cardiac and pulmonary physiologies, lung isolation techniques, the multiorgan impact of cardiopulmonary bypass (CPB) and additional monitoring techniques (e.g. transesophageal echocardiography-TEE). Combined procedures may include excision of invasive tumours, pulmonary endarterectomy, cardiac revascularization combined with lung resection and cardiac procedures combined with lung transplantation (e.g. PFO closure). Optimal management of these procedures remains controversial and is not well described; in fact it is mainly limited to case reports (Marseu K et al. A A Case Rep 8:61–63, 2017; Slinger et al. Perioperative care in cardiac anaesthesia and surgery. Lippincott, Williams & Wilkins, Philadelphia/Baltimore/New York/London/Buenos Aires/Hong Kong/Sydney/Tokyo, 43–48, 2006). Proponents of single-stage operations will argue in favour of the avoidance of a second surgery and anaesthetic and reduced hospital stay (Slinger et al. Perioperative care in cardiac anesthesia and surgery. Lippincott, Williams & Wilkins, Philadelphia/Baltimore/New York/London/Buenos Aires/Hong Kong/Sydney/Tokyo, 43–48, 2006; Rao et al. Ann Thorac Surg 62:342-347, 1996). The opponents will argue for divided, two-stage procedures on the basis of limiting surgical trauma, blood loss, multiorgan impact of cardiopulmonary bypass and high intensive care morbidity and thus may potentially confer a better long-term survival (Rao et al. Ann Thorac Surg 62:342-347, 1996; Ciracio et al. Eur J Cardiothorac Surg 22:35–40, 2002).
The following chapter will briefly describe the anaesthetic management for various combined thoracic and cardiac procedures. For a better understanding of why CPB is detrimental for lung function, the author will briefly describe the structure and function of the air-blood barrier and pathophysiology of its injury during procedures with use of CPB.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
From a physiologic point of view, alveolar-capillary membrane is the most important part of the respiratory system. It always undergoes micro-injury during cardiac surgery with the use of cardiopulmonary bypass. Therefore, a second insult, such as loss of part of the pulmonary parenchyma, can lead to acute lung injury and unfavourable outcomes from combined thoracic and cardiac procedures.
-
Additional insult to the respiratory system can be caused by phrenic nerve injury subsequent diaphragmatic dysfunction and disturbances in chest wall mechanics caused by sternotomy or thoracotomy.
-
Clinicians should be very selective in choosing to combine pulmonary resection and heart surgery. Concomitant pulmonary resection and cardiac surgery entail substantial additional risk, especially pulmonary complications and bleeding problems. These procedures should be performed in tertiary care centres with expertise in cardiac and thoracic surgery including use of extracorporeal life support systems.
-
Anaesthetic management must be individualized and based on preoperative assessment, extent of surgery and need to use cardiopulmonary bypass. Anaesthesiologists managing these cases should have extensive training in both cardiac and thoracic anaesthesia. An expertise in transesophageal echocardiography is strongly recommended.
Introduction
Combined cardiac and thoracic procedures are rare; however thanks to progress of surgical techniques and recent advances in use of extracorporeal life support (ECLS) techniques the number of these procedures is increasing.
Anaesthesia and optimal perioperative management for these complex, high-risk surgical interventions requires an expertise in both cardiac and pulmonary physiologies, lung isolation techniques, the multiorgan impact of cardiopulmonary bypass (CPB) and additional monitoring techniques (e.g. transesophageal echocardiography-TEE). Combined procedures may include excision of invasive tumours, pulmonary endarterectomy, cardiac revascularization combined with lung resection and cardiac procedures combined with lung transplantation (e.g. PFO closure). Optimal management of these procedures remains controversial and is not well described; in fact it is mainly limited to case reports [1, 2]. Proponents of single-stage operations will argue in favour of the avoidance of a second surgery and anaesthetic and reduced hospital stay [2, 3]. The opponents will argue for divided, two-stage procedures on the basis of limiting surgical trauma, blood loss, multiorgan impact of cardiopulmonary bypass and high intensive care morbidity and thus may potentially confer a better long-term survival [3, 4].
The following chapter will briefly describe the anaesthetic management for various combined thoracic and cardiac procedures. For a better understanding of why CPB is detrimental for lung function, the author will briefly describe the structure and function of the air-blood barrier and pathophysiology of its injury during procedures with the use of CPB.
Structure of the Alveolar-Capillary Barrier
The human lung consists of 300,000,000 alveoli. Each of them has a dense network of capillaries, which form air-blood barriers (alveolar-capillary membranes). From a physiological point of view, the air-blood barrier is the most important part of the respiratory system. It is the site of gas exchange. Additionally, the alveolar-capillary barrier separates the external environment from the pulmonary circulation, regulates transport of fluid and molecules from alveoli to capillaries and is a vital part of the natural defence mechanism of the human body (see also Chap. 7) [5].
Structure
The alveolar-capillary barrier has three components: thin processes of type I pneumocytes (epithelial cells), endothelial cells and their common basement membranes (Fig. 40.1). Typically, endothelial and epithelial cells have separate basement membranes; but the pulmonary alveolus is a unique site where the basement membranes are fused together. This creates an extremely thin barrier (0.2–0.4 μm) enabling efficient exchange of oxygen and carbon dioxide [6, 7]. The processes of type I pneumocytes are very thin and cover 95% of the alveolar surface. The remaining 5% is covered by type II pneumocytes, which produce surfactant. Type II pneumocytes (also called granular cells) reside within the “corners” of the alveoli because their large cellular structure makes them inefficient for gas exchange (Fig. 40.1). Type II pneumocytes eventually divide into type I pneumocytes (progenitor cells). During injury of the alveolar surface, the damaged type I pneumocytes are replaced by large, cubical, quickly dividing, type II pneumocytes. These large cuboidal cells create a thicker alveolar-capillary barrier leading to inefficient gas exchange.
(a) Picture presents a scheme of an air-blood barrier, which consists of endothelial cell, epithelial cell (type I pneumocyte) and their common basement membrane. Large cuboidal cell is type II pneumocyte producing surfactant contained within its cytoplasm as lamellar bodies (onion-like structures), which are exocytosed into the alveolar lumen and then transform into tubular myelin and finally monolayed of the surfactant covering the surface of type I pneumocytes. Left-hand side inset shows details of thin alveolar-capillary membrane; right-hand side inset shows a scheme on surfactant monolayer. (b) Electron microscope photograph which is showing an air-blood barrier
Tight intercellular junctions between epithelial cells (pneumocytes) are impermeable to fluid, which contrasts with endothelial cell junctions which are highly permeable to fluids and allow the continuous exchange of plasma components between capillaries and the pulmonary interstitium. The common basement membrane consists of laminin, glycosaminoglycans, collagen type IV and fibronectin [6,7,8]. Glycosaminoglycans are concentrated on one side of basement membrane regulating its permeability. Among all the components of the alveolar-capillary barrier, this is the most critical part, and its injury leads to permanent damage of the blood-gas interface [9, 10]. There are three stabilizing elements of the alveolar-capillary barrier: surfactant, the pulmonary circulation and the connective tissue of the intra-alveolar septa [7, 11].
Surfactant
Surfactant is composed from lipids (90%) and proteins (10%). The lipid component mainly consists of phosphatidylcholine (bipolar lipid) and phosphatidylglycerol [12]. Both lipids have a hydrophilic “head” and “lipophilic” tail (see Fig. 40.1a, right-hand inset]. Surfactant forms a monolayer lining the alveolar surface with the hydrophilic part directed towards the epithelial cells. The biochemical structure of the pulmonary surfactant resembles a detergent, surface-active layer, which aims to lower the surface tension and stabilizes the alveolar shape and structure. Surfactant protects the alveolus from collapse and prevents overdistension [13]. Moreover, surfactant acts as an anti-pulmonary oedema substance.
The protein component consists of four, distinct surfactant proteins – A, B, C and D (SP-A surfactant protein A, SP-B, SP-C and SP-D). These molecules play an important role in local defence mechanisms, surfactant metabolism, recirculation and spreading on the alveolar surface. Additionally they participate in local defence mechanisms. SP-A is a 28,000–36,000 kD protein and participates in monolayer formation and in recirculation of pulmonary surfactant. It has hydrophilic character. SP-D is the biggest surfactant protein (42,000 kD) and has also hydrophilic character, and its main role is to regulate local defence mechanisms. SP-B and SP-C are relatively small proteins (9.000 and 4.000 kD, respectively) with lipophilic character, and they are essential for monolayer formation [14]. Surfactant is produced in type II pneumocytes and is seen as so-called lamellar bodies (onion-like structures) (Fig. 40.2). Lamellar bodies are excreted into the alveolar lumen, transform into tubular myelin (Fig. 40.3) and then spread as a monolayer on the surface of type I pneumocytes (Fig. 40.1). The metabolism of surfactant is unique; it is recycled. Molecules of surface-active material are endocytosed back into type II pneumocytes and without any breakdown incorporated back into the lamellar bodies. Small amounts of surfactant (7–8%) are digested by alveolar macrophages. In the normal physiological situation, surfactant is not present within the pulmonary circulation (except for newborns when the lung is drying out after delivery). If surfactant is present within the pulmonary circulation, its amount reflects the extent of damage to the alveolar-capillary barrier [15, 16].
Pulmonary Circulation
Flow through the pulmonary circulation equals the systemic flow enabling effective gas exchange. The pulmonary circulation also plays an important role in metabolic and filtrating functions of the lung. The pulmonary circulation is a low-pressure system, which is influenced by gravitation forces creating West’s zones. The alveolar capillaries make contact with multiple alveoli, which increases the efficiency of gas exchange. The alveolar vessels are stabilized by a delicate network of collagen and elastic fibres, which form a continuum connected to basement membranes of the air-blood barriers. The location and structure of the alveolar capillaries make them susceptible to pressure changes occurring within the alveolar space. Rising intra-alveolar pressure will decrease the volume of the alveolar capillaries and increase their resistance.
Connective Tissue
The connective tissue (mesenchyma) of the inter-alveolar septae is responsible for both their elasticity and mechanical resistance [11, 17]. The mesenchyma consists of the cellular and extracellular components. The cellular part is largely composed from fibroblasts, which are responsible for producing extracellular elements of the connective tissue, for example, collagen fibres, elastic fibres, fibronectin, entactin, glycosaminoglycans and components of the basement membranes [7]. The extracellular connective tissue forms a continuum extending from the hilum to each alveolus [18]. Thus any structural change within the lung tissue will have a transmitted effect upon every alveolus. This means that any change of shape within the lung affects every alveolus. Collagen fibres form the main mechanical support and restrictive force. This is counterbalanced by the presence of elastic fibres, which are responsible for the elastic recoil of lung parenchyma and its compliance. Collagen fibres are interwoven with elastic fibres, and both elements aid in stabilization of the alveolar-capillary membranes. During injury, the elastic fibres are more susceptible to damage, which creates an imbalance in the resistive-elastic forces of the lung in favour of a stiffer lung with low compliance.
Lung Injury During Surgery with Use of Cardiopulmonary Bypass
Combined cardiac and thoracic surgical procedures with the use of CPB are controversial. If a cardiac procedure is performed with the use of CPB and is combined with thoracic surgery, which involves resection of lung parenchyma (lobectomy or pneumonectomy), respiratory complications may reach an incidence as high as 49% [19, 20]. It is postulated that CPB is the main causative factor of the aforementioned complications; therefore the most common injuries of the respiratory system caused by CPB will be briefly described in the following paragraphs [21,22,23].
Respiratory complications occurring after cardiac surgery with use of CPB are relatively common, but the vast majority are mild and self-limiting [24,25,26]. It is important to emphasize that the cause of lung failure after operations involving CPB is multifactorial [27, 28]; patient factors combine with the direct detrimental effects of CPB to compromise pulmonary function in the early postoperative period. A second insult to the respiratory system, such as loss of part of the pulmonary parenchyma, can be detrimental and lead to acute lung injury and unfavourable outcomes.
Prolonged mechanical ventilation after cardiac surgery occurs in about 6–7% of patients, and strongest predictors of this complication are previous cardiac surgery, lower left ventricular ejection fraction, shock, surgery involving repair of congenital heart disease and cardiopulmonary bypass time [26]. The most severe form of injury to the respiratory system – acute respiratory distress syndrome (ARDS) – occurs in 1–2% of cardiac cases with a very high mortality (40%) [10, 24].
Histological Injury
Most patients who undergo cardiac surgery with the use of CPB present some degree of histological lung injury [30]. Microscopic observations reveal a range of injuries detected within the structures of the air-blood barriers [7, 8, 30, 31]. Mild injury presents as oedema of endothelial (type I pneumocytes) and epithelial cells. More severe forms cause denuding of the basement membranes with loss of epithelial lining (Fig. 40.4). In the most severe cases, basement membranes of alveolar-capillary membranes lose their continuity, which means they are permanently damaged. The alveoli with damaged basement membrane fill with fluid and lamellar bodies (surfactant) are not able to spread on the surface of epithelial cells. Beyond the damage visualized within the alveolar-capillary membranes, authors have observed congestion within alveolar capillaries and the accumulation of polynuclear leukocytes (neutrophils), many of which are extravasated (Fig. 40.5). Upon migrating from the intravascular space to the interstitium or alveolar space, neutrophils are able to survive for 6 h. Subsequent breakdown of neutrophils will exacerbate alveolar damage by releasing an abundance of proteolytic enzymes, reactive oxygen species and free radicals [29, 32]. In summary, in all patients undergoing surgery utilizing CPB, some injury will occur within the pulmonary parenchyma [8, 30, 31].
Electron microscope photograph presenting a portion of alveolar-capillary barrier with partially “denuded” basement membrane (arrows). A, alveolar lumen; C, capillary lumen. (Permission for publication obtained from Taylor & Francis, from Ref. [29])
Electron microscope photograph showing severe microscopic injury of air-blood barrier occurring post-CPB. Alveolar lumen is filled with oedema fluid, and surfactant structures (lamellar bodies-arrows’ heads) are not able to spread. Arrows are indicating type II pneumocyte. (Permission for publication obtained from Taylor & Francis, From Ref. [29])
Systemic Inflammatory Response Syndrome
CPB causes a systemic inflammatory response syndrome (SIRS) [29, 32,33,34,35]. This leads to the activation of neutrophils, macrophages and multiple cytokines including complement and is commonly associated with free radical formation [32,33,34,35,36,37]. Complement proteins, mainly C3a and C5a, promote neutrophil activation, which can subsequently adhere to the endothelial cells and migrate into the interstitium promoting local damage and inflammation [36, 35]. The lung acts as a “filter” to activated neutrophils and therefore is often more vulnerable to CPB-related injury compared to other organs [24, 25]. In addition to the release of pro-inflammatory mediators and enzymes, activated neutrophils express surface receptors, CD11a and CD 18b, which facilitate further leukocyte-endothelial adhesion and chemotaxis. Those activated neutrophils, which remain within the lumen of the alveolar capillaries, tend to accumulate in congested blood vessels and release their contents causing “leakage” from alveolar capillaries to the extracellular spaces and alveolar lumen [29,30,31]. Neutrophils are not the only cells which are activated by an extracorporeal circuit. Macrophages also belong to the first line of cells which are stimulated by CPB [37]. They release multiple cytokines. The main cytokines involved in the inflammatory process and lung injury are interleukin 6 and 8. At the end of CPB, their concentration within the alveolar lining is much higher than within plasma [32, 33, 35].
Lipid Peroxidation
Another line of activation caused by CPB is lipid peroxidation and release of free radicals [38]. They are mainly freed as a consequence of ischemia-reperfusion injury. It should be stressed that during aortic cross-clamp, the lung has no blood supply, except for a small amount of flow coming from the bronchial arteries. During reperfusion, large amounts of free radicals are flushed from ischemic lung tissue (as a result of xanthine oxidase activation) [16]. Free radicals have a high affinity for cellular membranes causing oxidation of lipid components (so-called peroxidation) [39, 40]. Free radicals also activate leukocytes [24].
Surgical Factors
CPB is not the only cause of respiratory system dysfunction after cardiac surgery. Other common factors include:
-
Changes in lung mechanics related to sternotomy, internal mammary artery harvesting and other surgical manipulations. These present as an increased elastance of the pulmonary tissue (decreased compliance). Decreased compliance is also caused by the injury caused by CPB, i.e. increased pulmonary vasculature permeability, positive fluid balance and accumulation of neutrophils [41].
-
Atelectasis is a common postoperative complication after any major, prolonged surgery performed under general anaesthesia. Atelectasis occurs in up to 70% of patients undergoing cardiac surgery with or without the use of CPB [27, 41]. After cardiac surgery, atelectasis is observed most frequently in the left lower lobe and is considered the most common cause of an increased alveolar-arterial PO2 gradient [42, 43]. Atelectasis is also thought to be one of the main factors leading to further inflammatory injury leading to further deterioration in pulmonary function during the recovery phase after cardiac surgery. During the postoperative period, atelectasis is aggravated by pleural effusion(s) or pneumothorax, which may develop as a result of mechanical ventilation, central line cannulation or air leaks from surgical manipulations [9, 24, 27].
-
Phrenic nerve injury leading to poor diaphragmatic function. The most common cause of phrenic nerve injury is the use of cold saline flush or ice slush as a method of additional cardiac preservation. Fortunately, most of the centres have abandoned this method of cardioprotection.
-
Postoperative infections – pneumonia. All the aforementioned factors impairing pulmonary mechanics and ciliary clearance increase the risk of postoperative infections. Moreover, if a patient remains intubated for a prolonged period of time after any cardiac procedure, the risk of ventilator-associated pneumonia (VAP) increases to 44% (after 7 days of intubation) [41, 43]. Other significant risk factors for postoperative pulmonary infectious complications include cigarette smoking (a very common habit in patients undergoing combined cardiac and thoracic surgery) and the use of H2 blockers [44].
-
Massive transfusions of red blood cells and other blood products also contribute to respiratory dysfunction postoperatively [45, 46].
Prevention of Lung Injury After Cardiac Procedures
Although severe lung injury after CPB (ARDS) is uncommon (1–2%), other pulmonary complications remain a significant cause of mortality and morbidity after cardiac surgery [9, 25]. There are many patient-related risk factors, which contribute to postoperative pulmonary dysfunction, and some of them are modifiable. Among most important ones are smoking, obesity, COPD (see Chap. 2) and the use of proton-pump inhibitors [41, 43, 44]. Recently, we were also able to identify the intraoperative risk factors for prolonged mechanical surgery after surgery with the use of CPB [26]. At the same time prolonged mechanical ventilation might be detrimental to lung function aggravating injury to the remaining lung parenchyma.
There is little doubt that CPB is considered a “main culprit” of the pulmonary dysfunction occurring after cardiac surgery; however other factors also play an important role in their pathogenesis. Since the pathophysiology of respiratory complications following cardiac surgery has been extensively studied for the last 40 years, clinicians have developed multiple strategies to prevent them [24]. One of the most common approaches is the avoidance of CPB, which can be applied to coronary artery bypass surgeries [46]. On the other hand, currently available results are still inconclusive as to the true benefits of the off-pump CABG. Certainly, the new types of oxygenators (hollow fibre) and use of centrifugal pumps instead of roller pumps decrease activation of neutrophils and subsequent pulmonary dysfunction. The addition of leukoreduction filters which filter out activated polynuclear leucocytes has also been proven to have a beneficial effect [25, 27]. Similarly, a beneficial effect is observed with the use of heparin-coated circuits. Alternatively, some authors propose the use of the patient’s lungs as a natural oxygenator (so-called Drew-Anderson technique) [47]. Even though it improves the function of the respiratory system after surgery, it increases the complexity of the surgical technique (additional cannulation sites) and makes it impractical for combined cardiothoracic procedures. It seems that a much easier approach would be to continue ventilation with small tidal volumes, PEEP and the use of air during the surgical procedure and use of the vital capacity manoeuvre just prior to discontinuation of CPB [48]. One of the oldest methods used in the cardiac surgery aiming to attenuate of detrimental effects of CPB (including pulmonary dysfunction) is use of corticosteroids [49]. Even though use of methylprednisolone decreased the release of inflammatory interleukins (IL-6 and IL-8) and complement activation, it has been frequently proven to work as a double-edged sword. While preventing pulmonary complications, it can be attributed to other significant postoperative problems (sternal wound infection, insulin resistance and abdominal complications).
Among the many methods aimed at prevention of respiratory complications, we should also mention strategies used during the postoperative period. They include use of low-tidal volume ventilation, active preventions of VAP (detailed discussion is beyond the scope of this chapter), early extubation whenever possible and aggressive physiotherapy and incentive spirometry. One of the keys to achieve the above-mentioned aims is to maintain effective pain control during the postoperative period.
In summary, the incidence of postoperative pulmonary complications occurring after cardiac surgery is high, and the incidence of prolonged mechanical ventilation is 6–7% [26, 43]. Most likely the incidence of prolonged mechanical ventilation is even higher after combined cardiothoracic procedures; however there is no data in the literature. Progress in their prevention and advance in surgical and anaesthetic techniques make most of them temporary. On the other hand, given that many patients currently undergoing cardiac surgery are older and suffering from many co-morbidities, this is probably the main reason for reluctance to perform combined cardiac and thoracic procedures. The main argument against combined procedures is that most of the patients suffer some degree of lung injury related to the use of CPB, and an additional insult to lung tissue caused by surgical resection might significantly increase mortality and morbidity [50, 51].
Surgical Considerations
Many thoracic surgeons are familiar with techniques of extracorporeal circulation. There are some thoracic procedures, which are routinely performed with use of CPB. Among the most common are lung transplantation and pulmonary endarterectomy; however recently most of the centres prefer the use of VA-ECMO over CPB. Since anaesthetic management during these procedures is discussed in different chapters of this textbook, they will not be further reviewed here (see Chaps. 47 and 49). The scope of the discussion in this section will concentrate on the perioperative management of patients with intrathoracic malignancies invading cardiac or major vascular structures and patients undergoing thoracic surgery who are suffering from coexisting coronary artery disease. Many surgeons are reluctant to perform one-stage cardiac-thoracic operation because of the concerns mentioned above [50,51,52]. Moreover, surgical access to the lung structures might be difficult if surgical incision and subsequent CPB cannulation are performed via median sternotomy. Additionally, there is anxiety regarding heparin use and the possibility of excessive bleeding. Apart from the injury to the respiratory system, a frightening consideration is the possibility of dissemination of pulmonary malignancy through the use of CPB [19, 52,53,54]. On the other hand, a one-stage combined procedure avoids the need for a second major thoracic surgery [3, 53, 54]. In the case of coexisting pulmonary malignancy and coronary artery disease, the answer seems to be straightforward [21, 50, 54, 55]. Preoperative revascularizations performed by interventional cardiologists (PCI – primary coronary intervention) may cause significant time delays for subsequent cancer surgery [56]. Thus, combined surgical coronary revascularization and resection of the lung cancer may be the optimal management. In most cases, revascularization can be performed without the use of CPB (off-pump coronary artery bypass grafting – OPCABG); therefore the detrimental effects of CPB can be avoided [21, 50, 54]. The results of these combined thoracic and cardiac surgeries are encouraging; however published results usually involve small number of patients [20, 21, 57,58,59].
When considering proper management of thoracic malignancies invading heart structures, it should be mentioned that surgical resection remains the only curative option for most intrathoracic malignancies [52, 53, 59, 60, 61]. Sometimes conventional thoracic surgical techniques do not allow complete resection of a pulmonary tumour which is invading the heart or large vessels; therefore radical surgical removal may necessitate the use of CPB [52]. The most common examples are tumours involving the left atrium and pulmonary artery or infiltrating the descending portion of the aorta [53, 58, 59].
Most of the procedures involving resection or opening of the heart structures are performed via median sternotomy. Surgical exposure to some of the hilar structures is more difficult when compared to a lateral thoracotomy approach. Left lower lobectomy and mediastinal lymph nodes dissection are especially technically challenging when performed via median sternotomy. Probably in most of the cases, mediastinoscopy or EBUS are is indicated initially to rule out mediastinal spread of the disease. All these concerns raise a question as to whether aggressive treatment including surgical resection of lung parenchyma and cardiac or major vascular structures should be a routine management. The answer is clearly no. This mode of treatment should be only performed in departments that are prepared for the complexity of those cases and can offer expertise in both cardiac and thoracic surgery, and anaesthesia, and postoperative ICU care for these patients. Moreover, the functional status of the patient prepared for this type of surgery should be excellent to allow them to survive a potential prolonged stay within an intensive care setting.
Anaesthetic Management for Combined Cardiac and Thoracic Procedures
The literature describing the anaesthetic management of the patient undergoing combined thoracic and cardiac procedures is very scarce and includes mainly case reports [1, 2, 62]. Subsequent paragraphs will try to summarize current information described as individual cases and the experience of the institution where the author practices cardiac and thoracic anaesthesia. The anaesthesiologist who is looking after the patient who is scheduled to undergo combined thoracic and cardiac surgery should possess an expertise in both cardiac and thoracic anaesthesia. Quite often these procedures are complex and require management by two consultants. For most of the cases, we also require the presence of perfusionist, who will be either actively involved with management of the case requiring the use of CPB and ECLS or prepare the machine for extracorporeal circulation in a “standby” mode.
Preoperative Assessment
Apart from standard preoperative evaluations before surgery, the anaesthesiologist preparing the patient for combined cardiac and thoracic procedure must perform a detailed assessment of the respiratory and cardiovascular systems. An extensive description of respiratory system evaluation is described elsewhere in this monograph (see Chap. 2). Briefly, the anaesthesiologist who is assessing the pulmonary function should concentrate on lung mechanics, pulmonary parenchymal function and cardiorespiratory reserve. The most popular test performed to assess lung mechanics is spirometry. The value most commonly used by anaesthesiologists is the forced expiratory volume in 1 s (FEV1). FEV1 is also used to calculate the predicted postoperative FEV1 (ppo-FEV1) once part of the pulmonary parenchyma is resected. Values below 30–35% for ppo-FEV1 are considered as predictors of increased risk of respiratory complications and prolonged weaning from mechanical ventilation. Maximal oxygen consumption is used to assess cardiopulmonary reserve, and diffusing capacity of carbon monoxide is measured to estimate the gas exchange function of lung parenchyma. Any patient being prepared for a combined procedure requires a very careful airway evaluation. Intrathoracic malignancies necessitating these types of procedures often result in airway involvement, causing deviation or invasion of large airways. Moreover, they can infiltrate or compress large vascular structures. Apart from clinical symptoms, the anaesthesiologist must examine the results of computed tomography (CT) scans, which show precisely the extent of the disease and possible vascular involvement. A preoperative echocardiogram will be complimentary to the radiological examination and should routinely be performed before any cardiac surgical procedure. In the context of pulmonary resection, we should pay particular attention to the function of the right ventricle and value of right ventricular systolic pressure reflecting on pressure in pulmonary circulation.
The “second leg” of preoperative evaluation focuses on the status of the cardiovascular system. The mortality and morbidity of cardiac surgical patients are strongly influenced by their preoperative severity of the illness. The important factors included in most preoperative risk assessment scores include age, sex, left ventricular function, type of surgery, urgency of the surgery, redo cardiac surgery, unstable angina, congestive heart failure, history of peripheral vascular disease and cerebral vascular disease, renal insufficiency and history of diabetes. In most cases, this information can be obtained from the medical history, physical examination and simple laboratory findings including electro- and echocardiogram. Additionally, results of echocardiography provide a detailed description of valve structure and pathology, contractility of the left and right ventricle and morphology of most of the large vessels. In the case of poor ventricular function (ejection fraction <30%), it is recommended to consider an alternative therapeutic approach rather than combined cardiac-thoracic surgery. If the patient suffers from coronary artery disease, the degree of coronary stenosis (es) is assessed preoperatively by cardiac catheterization (coronary angiogram). This information is important for the anaesthesiologist who will be intraoperatively assessing the contractility of the particular segments of the myocardium with the use of transesophageal echocardiography (TEE).
Patients who are scheduled to undergo combined cardiac-thoracic surgery frequently suffer from multiple co-morbidities. Among the most significant, we should mention peripheral vascular disease, diabetes mellitus and kidney dysfunction. Most of these co-morbidities are aggravated during the perioperative period, and this in turn is what significantly increases mortality and morbidity. The anaesthesiologist must collect a detailed list of which medications the patient is currently taking.
Anaesthetic Management
The anaesthesiologist providing care during combined cardiac-thoracic procedures faces multiple challenges. Quite often she/he must simultaneously manage haemodynamic instability, hypoxemia, problems with ventilation and excessive bleeding. It is beyond the scope of this chapter to fully discuss all of the challenges of cardiac anaesthesia, and most of the topics related to thoracic anaesthesia are presented elsewhere in this textbook. Therefore, the author will discuss only the most important problems occurring during combined thoracic and cardiac procedures.
-
1.
Airway management. If pulmonary resection is performed before or after CPB, the patient will require lung isolation. Detailed techniques and methods of choice are discussed in Chap. 16. The position of a double lumen tube or bronchial blocker should be always verified with a fibre-optic bronchoscope. If resection of pulmonary parenchyma is to be performed during CPB, the patient can be intubated with standard, single-lumen tube.
-
2.
Management of hypoxemia during one lung ventilation is discussed in Chap. 6.
-
3.
Transesophageal echocardiography (see Chap. 20). The use of TEE is one of the key components of intraoperative anaesthetic management of patients undergoing combined cardiac and thoracic procedures. The important information obtained from intraoperative TEE during combined cardiac and thoracic procedures includes assessment of left and right ventricular function (especially important after pneumonectomy), diagnosis of new wall-motion abnormalities (coronary artery bypass surgery), evaluation of effects of valve repair/replacement and extension of the disease (e.g. lung tumour invading left atrium or pulmonary vein).
-
4.
Pulmonary artery catheter (PAC). TEE is an excellent diagnostic tool, but at current stage, its use is limited to this role. It does not allow for continuous monitoring of haemodynamic status particularly RV function and afterload for RV. Therefore, PAC is very useful in management of combined cardiac and thoracic procedures particularly during postoperative period. It allows to monitor cardiac output (read function of RV), pulmonary pressures and their changes as response to therapy and certain physiological phenomena and provides warning of RV dysfunction (high CVP, low PAD pressures or presence of square root sign in case we have RV channel in our PA line). During surgery anesthesiologist must remember to ask surgeon to palpate catheter before PA or its branch is being clamped in case pulmonary resection is being performed. If necessary PA must be pulled back prior to resection.
-
5.
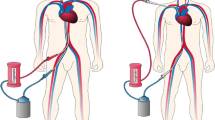
The anaesthesiologist and extracorporeal techniques (cardiopulmonary bypass, CPB, and extracorporeal lung support, ECLS). CPB has three main functions during cardiac procedures: (1) replacing function of the heart (circulation of the blood), (2) replacing function of the lungs (oxygenation and CO2 removal) and (3) diversion of the blood from the operating field to create optimal surgical conditions. To achieve these purposes, superior and inferior vena cavae are cannulated, and the blood is passively drained into the CPB venous reservoir. The blood is then oxygenated and returned back to the patient via an aortic cannula usually placed in the distal part of the ascending aorta. In the case of combined thoracic-vascular surgery including the resection of the tumour invading the descending aorta, one can use partial bypass, which diverts some of the blood from the left atrium and returns it back to one of the femoral arteries. Since the primary function of CPB is to oxygenate blood and perfuse the vital organs, an important question for the anaesthesiologist is what perfusion/oxygenation is optimal? Even though it has been over 50 years since the first human use of extracorporeal circulation, there is no definite answer. Blood is exposed multiple times to the foreign surface of the extracorporeal circuit causing SIRS and microembolization, which can affect every organ of the human body. Apart from lung injury, CPB can contribute to cognitive dysfunction, renal injury or failure, pancreatitis or, in the worst-case scenario, multiorgan dysfunction. It is the anaesthesiologist’s role to prevent or minimize these complications. Due to advancement in development of extracorporeal techniques and better availability of ECLS perfusion in some cases, venoarterial ECMO might be used instead of full CPB. It allows for using relatively small doses of heparin (typically ACT is between 140–200 s), and subsequently it leads to less significant disturbances in coagulation. On the other hand, ECLS can still cause systemic inflammatory reaction and subsequent vasoplegia. When ECLS is used, we must remember that it is entirely a closed system, which does not allow perfusionist to add any volume. When used in venoarterial configuration, it allows to offload the heart; however it does not allow full circulatory arrest.
-
6.
The anaesthetic approach to combined procedures performed without the use of CPB. Off-pump coronary artery grafting (OPCABG) is the preferred surgical management of coronary artery disease in patients who require pulmonary resection at the same time as coronary revascularization [21, 54, 56]. Revascularization is usually performed as the first part of the procedure followed by the resection of the pulmonary pathology. The most important principles of anaesthetic management for OPCABG include aggressive maintenance of normothermia to prevent bleeding and/or acidosis and preservation of haemodynamic stability during surgical manipulation of the heart. The first aim is achieved by use of warm blankets, body warmers, fluid warmers and adjustment of the room temperature in the operating theatre. Maintaining haemodynamic stability is crucial for ultimate success of the procedure; thus it requires ideal communication and cooperation between the surgeon and the anaesthesiologist. It is accomplished by a combination of inotropic support, proper volume therapy (quite often achieved by “deep” Trendelenburg position) and anti-arrhythmic prophylaxis. The surgeon should use gentle manipulations (e.g. incision of right pleura to avoid compression of the heart) and devices (e.g. Starfish™, Medtronic International Ltd., Minneapolis, MN or intracoronary shunts) in order to preserve the geometry of the heart ventricles and their contractility, and prevent mitral regurgitation.
-
7.
Haemodynamic support, right ventricular failure. Cardiothoracic anaesthesiologist must be familiar with all forms of circulatory support to provide haemodynamic stability during and after surgery. It can be achieved by optimization of pre- and after load, maintaining or improving contractility and preservation of a stable sinus rhythm. The most worrisome haemodynamic problem complicating combined cardiac-thoracic procedures is right ventricular dysfunction or failure. It is commonly caused by a rapid increase in the afterload (pressure) for the right side of the heart, especially after major resection of the pulmonary parenchyma (e.g. pneumonectomy). The warning symptoms include right ventricular distension visualized directly by the surgeon and the anaesthesiologist, a low cardiac output state and a central venous pressure (CVP) higher than the pulmonary diastolic pressure (PAD). If we are monitoring RV pressure, the analysis of pressure tracing might show characteristic square root sign warning anaesthesiologist about RV dysfunction.
The treatment includes:
-
Reduction of RV preload (e.g. promotion of diuresis with diuretics) or early introduction of renal replacement therapy if there is no response to diuretics.
-
Manoeuvres to decrease the pressure in the pulmonary circulation – hyperventilation, hyperoxia and pharmacological support. Among the intravenous agents, which decrease afterload for the RV and improve its contractility, the first choices are dobutamine and milrinone. Inhalational pulmonary vasodilators (nitric oxide or prostacyclin) are used when a lack of response to intravenous agents occurs.
-
Preservation of good perfusion pressure to the right ventricle and ventricular interdependence (norepinephrine or vasopressin) and/or the use of an intra-aortic balloon pump.
-
Since stroke volume is usually fixed in RV dysfunction or failure and in order to increase the cardiac output, it is recommended to increase heart rate (e.g. A-V pacing).
-
-
8.
Treatment of coagulopathy. Combined cardiothoracic procedures performed with the use of CPB are frequently complicated by excessive bleeding, which can have two possible causes: surgical (extensive surgery) and coagulopathy related to prolonged CPB. In cases of surgical resection of pulmonary parenchyma combined with a cardiac procedure, CPB duration often exceeds 2 h. Duration of CPB directly correlates with the magnitude of coagulopathy. There are multiple mechanisms of excessive, non-surgical bleeding caused by extracorporeal circulation; among the most important are the dilutional effect, SIRS, platelet consumption, depleted amount of clotting factors, secondary fibrinolysis, low haemoglobin and hypothermia. Treatment is based on the results of laboratory tests (INR, aPTT, fibrinogen level and platelet count) or use of point-of-care devices. Currently many tertiary care centres use them routinely; its application delivers quick assessment of coagulation status based on results obtained from a whole-blood sample. Among the most popular ones are thromboelastography (TEG) and thromboelastometry (ROTEM). In the context of high likelihood of massive bleeding and coagulopathy in our institution, for most of the combined cardiac-thoracic cases, we secure at least two, large-bore venous catheters to be able to transfuse large volumes of blood products in a relatively short period of time. In most of these cases, we use routinely infusion of tranexamic acid as an antifibrinolytic agent. We follow protocol proposed by Dowd and Karski; however infusion rate should be modified (decreased) in patients with kidney dysfunction or failure [63,64,65].
Summary
There is no complete agreement about the optimal surgical management of patients who are suffering from both cardiac and thoracic diseases requiring surgery [1, 2, 52, 62]. The arguments for one-stage procedures are avoidance of a second surgery/anaesthetic and reduced hospital stay and cost. However, two-stage procedures may be associated with less surgical trauma and blood loss and may offer better long-term survival because the consequences of cardiopulmonary bypass (CPB) are minimized.
Combined cardiac-thoracic procedures should be performed only for selected cases in specialized centres, which pose an expertise in both cardiac and thoracic anaesthesia and surgeries. This chapter briefly describes the important perioperative considerations and management. Since there is minimal literature describing the anaesthetic management for combined cardiac-thoracic procedures, the a forementioned recommendations are based on the experience and clinical practice developed in the institution where author works.
References
Marseu K, Minkovich L, Zubrinic M, Keshavjee S. Anesthetic considerations for pneumonectomy with left atrial resection on cardiopulmonary bypass in a patient with lung Cancer: a case report. A A Case Rep. 2017;8:61–3.
Slinger PD, Chang DCH, David TE, editors. Perioperative Care in Cardiac Anesthesia and Surgery. Philadelphia/Baltimore/New York/London/Buenos Aires/Homg Kong/Sydney/Tokyo: Lippincott, Williams&Wilkins; 2006. p. 43–8.
Rao V, Todd TRJ, Weisel RD, et al. Results of combined pulmonary resection and cardiac operation. Ann Thorac Surg. 1996;62:342–7.
Ciracio P, Carretta A, Calori G, Mazzone P, Zannini P. Lung resection for cancer in patients with coronary artery disease: analysis of short term results. Eur J Cardiothorac Surg. 2002;22:35–40.
Wąsowicz M, Biczysko W, Marszałek A, Yokoyama S, Nakayama I. Ultrastructural studies on selected elements of the extra cellular matrix in the developing rat lung alveolus. Folia Histochem Cytobiol. 1998;36:3–13.
Wąsowicz M, Kashima K, Yokoyama S, Nakayama I. Pulmonary surfactant migrates into the alveolar capillaries of newborn rats an immunoelectron microscopic study. Acta Anat. 1996;156:11–21.
Wąsowicz M. Biczysko W. In: Andres J, Wąsowicz M, editors. Selected problems of anesthesia and critical care in cardiovascular surgery. Kraków: Danbert; 2002. p. 174–89.
Wąsowicz M, Drwiła R, Biczysko W, Marszałek A, Florek E, Andres J. Effects of exogenous surfactant on alveolar barrier. An experimental study. Anaesth Inten Ther. 2002;34:76–80.
Wąsowicz M, Sobczyński P, Szulc R, Biczysko W. Ultrastructural changes in the lung alveoli after cardiac surgical operations with the use of cardiopulmonary bypass (CPB). Pol J Pathol. 1999;50:189–96.
Ng CSH, Wan S, Yim APC, Arifi AA. Pulmonary dysfunction after cardiac surgery. Chest. 2002;121:1269–77.
Biczysko W, Wąsowicz M, Marszałek A. Stromal compartment in the developing lung’s alveoli- an electron microscopic study. Clin Perinat Gynaecol. 1994;6:107–19.
Wąsowicz M, Biczysko W, Sobczyński P. Structure and activity of pulmonary surfactant and their implications for intensive therapy. Inten Care Emerg Med. 1998;1:35–44.
Biczysko W, Wąsowicz M, Metzner J, Marszałek A. In: Drobnik L, Jurczyk W, editors. Problems of anesthesiology and intensive therapy. Warszawa: Wydawnictwo Lekarskie PZWL; 1998. p. 96–109.
Biczysko W, Marszałek A, Wąsowicz M. Maturation of lung epithelia in transmission electron microscopic study. Clin Perinat Gynaecol. 1993;3:3–23.
Doyle I, Nicholas TE, Bernste AD. Serum surfactant protein a levels in patients with acute cardiogenic pulmonary edema and adult respiratory distress syndrome. Am J Respir Crit Care Med. 1995;152:307–17.
Sobczyński P, Wąsowicz M. In: Zapalski S, Checinski P, editors. Clinical aspects of lung reperfusion. Clinical aspects of ischemia and reperfusion. Bielsko Biała: Alfa Medica Press; 1997. p. 79–89.
Wąsowicz M, Yokoyama S, Kashima K, Nakayama I. The connective tissue compartment in the terminal region of the developing rat lung. Acta Anat. 1996;156:268–82.
Biczysko W, Wąsowicz M, Marszałek A, Florek E. Why do the lungs of premature newborns function improperly? A morphological study of the connective tissue and vascular compartments in the developing lung. Arch Perinat Med. 1999;5:19–26.
Danton MHD, Anikin VA, McManus KG, McGuigan JA, Campalani G. Simultaneous cardiac surgery with pulmonary resection: presentation of series and review of literature. Eur J Cardiothorac Surg. 1998;13:667–72.
Wiebe K, Baraki H, Macchiarini M, Haverich A. Extended pulmonary resections of advanced thoracic malignancies with support of cardiopulmonary bypass. Eur J Cardiothorac Surg. 2006;29:571–8.
Dyszkiewicz W, Jemielity M, Piwkowski C, et al. The early and late results of combined off-pump coronary artery bypass grafting and pulmonary resection in patients with concomitant lung cancer and unstable coronary heart disease. Eur J Cardiothorac Surg. 2008;34:531–5.
Spaggiari L, D’Aiuto M, Veronesi G, et al. Extended pneumonectomy with partial resection of the left atrium, without cardiopulmonary bypass for lung cancer. Ann Thorac Surg. 2005;79:234–40.
Voets AJ, Sheik Joesoef K, van Teeffelen MEJM. Synchronously occurring lung cancer (stages I-II) and coronary artery disease: concomitant versus staged surgical approach. Eur J Cardiothorac Surg. 1997;12:713–7.
Wąsowicz M. In: Andres J, Wąsowicz M, editors. Selected problems of anesthesia and critical care in cardiovascular surgery. Kraków: Danbert; 2002. p. 191–207.
Clark SC. Lung injury after cardiopulmonary bypass. Perfusion. 2006;21:225–8.
Sharma V, Rao V, Manlhiot C, Boruvka A, Fremes S, Wąsowicz M. A derived and validated score to predict prolonged mechanical ventilation in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2017;153:108–15.
Weissman C. Pulmonary complications after cardiac surgery. Semin Cardiothorac Vasc Anesth. 2004;8:185–211.
Picone AL, Lutz CJ, Finck C, et al. Multiple sequential insults cause post-pump syndrome. Ann Thorac Surg. 1999;67:978–85.
Tonz M, Milhajevic T, Von Segesser LK. Acute lung injury during cardiopulmonary bypass. Are the neutrophils responsible? Chest. 1995;198:1551–6.
Wąsowicz M, Drwiła R, Sobczyński P, Przybyłowski P, Dziatkowiak A. Lung alveolar damage during coronary artery bypass grafting with use of cardiopulmonary-bypass: and old nemesis? Br J Anaesth. 2000;84(supp 1):18.
Wąsowicz M, Sobczyński P, Drwiła R, Biczysko W, Marszałek A, Andres J. Air-blood barrier injury during cardiac operations with the use of cardiopulmonary bypass (CPB). An old story? Scand Cardiovasc J. 2003;37:216–21.
Kotani N, Hashimoto H, Sessler DI, et al. Neutrophil number and interleukin-8 and elastase concentration in bronchoalveolar lavage fluid correlate with decreased arterial oxygenation after cardiopulmonary bypass. Anesth Analg. 2000;90:1046–51.
Kotani N, Hashimoto H, Sessler DI, et al. Cardiopulmonary bypass produces greater pulmonary than systemic proinflammatory cytokines. Anesth Analg. 2000;90:1039–45.
Sinclair DG, Haslam PL, Quinlan GL, Pepper JR, Evans TW. The effects of cardiopulmonary bypass on interstitial and pulmonary endothelial permeability. Chest. 1995;108:718–24.
Kawamura T, Wakusawa R, Okada K, Inada S. Elevation of cytokines during open heart surgery with cardiopulmonary bypass: participation of interleukin 8 and 6 in reperfusion injury. Can J Anesth. 1993;40:1016–21.
Chenoweth DE, Cooper SW, Hugli TE, et al. Complement activation during cardiopulmonary bypass. Evidence for generation C3a and C5a anaphylatoxins. N Engl J Med. 1981;304:497–503.
Warner AE. Pulmonary intravascular macrophages. Role in acute lung injury. Clin Cest Med. 1996;17:125–35.
Royston D, Fleming JS, Desai JB, et al. Increased production of peroxidation products associated with cardiac operations. Evidence for free radical generation. J Thorac Cardiovasc Surg. 1986;91:75–766.
Wąsowicz M, Drwiła R, Jeleń H, Przybyłowski P, Andres J, Dziatkowiak A. Lipid peroxidation (LO) during cardiac operations with use of cardiopulmonary bypass measured by headspace chromatography. Eur J Anaesthesiol. 2001;18(supp. 22):19.
Wąsowicz M, Drwiła R, Jeleń H, Przybyłowski P, Andres J, Dziatkowiak A. Lipid peroxidation (LO) during cardiac operations with use of cardiopulmonary bypass measured by headspace chromatography. Eur J Anaesthesiol. 2001;18(supp. 22):19.
Rady MY, Ryan T, Star NY. Early onset of acute pulmonary dysfunction after cardiovascular surgery; risk factors and clinical outcomes. Crit Care Med. 1997;25:1831–9.
Magnusson L, Zemgulis V, Wicky ZS, Tyden H, Thelin S, et al. Atelectasis is a major cause of hypoxemia and shunt after cardiopulmonary bypass. Anethesiology. 1997;87:1153–63.
Bouza E, Perez A, Munoz P, et al. Ventilator-associated pneumonia after heart surgery: a prospective analysis and the value of surveillance. Crit Care Med. 2003;31:1964–70.
Gaynes R, Bizek B, Movry-Hanley J, et al. Risk factors for nosocomial pneumonia after coronary artery bypass operations. Ann Thorac Surg. 1991;51:215–8.
Karkouti K, Wijeysundera DN, Yau TM, et al. The independent association of massive blood loss with mortality in cardiac surgery. Transfusion. 2004;44:1453–62.
Taggard DP. Respiratory dysfunction after cardiac surgery: effect of avoiding cardiopulmonary bypass and the use of bilateral internal mammary artery. Eur J Cardiovasc Surg. 2000;18:31–7.
Richter JA, Meisner H, Tassani P, et al. Drew-Anderson technique attenuates systemic inflammatory response syndrome and improves respiratory function after coronary artery bypass grafting. Ann Thorac Surg. 2000;69:7783.
Minkovich L, Djaiani G, Katznelson R, et al. Effects of alveolar recruitment on arterial oxygenation in patients after cardiac surgery: a prospective, randomized, controlled clinical trial. J Cardiothorac Vasc Anesth. 2007;21:375–8.
Tassani P, Richter P, Barankay A, et al. Does high-dose methylprednisolone in aprotinin-treated patients attenuates the systemic inflammatory response during coronary artery bypass grafting procedures? J Cardiothorac Vasc Anesth. 1999;13:165–72.
Saxena P, Tam RKW. Combined off-pump coronary artery bypass surgery and pulmonary resection. Ann Thorac Surg. 2004;78:498–501.
Ng CSH, Arifi AA, Wan S, Wai S, Lee TW, Yim APC. Cardiac operation with associated pulmonary resection: a word of caution. Asian Cardiovasc Thorac J. 2002;10:362–4.
Klepetko W. Surgical intervention for T4 lung cancer with infiltration of the thoracic aorta: are we back to the archetype of surgical thinking? J Thorac Cardiovasc Surg. 2005;129:727–9.
De Perrot M, Fadel ZE, Mussot S, de Palma A, Chapelier A, Dartevelle P. Resection of locally advanced (T4) non-small cell lung cancer with cardiopulmonary bypass. Ann Thorac Surg. 2005;79:1691–7.
Dyszkiewicz W, Jemielity MM, Piwkowski CT, Perek B, Kasprzyk M. Simultaneous lung resection for cancer and myocardial revascularization without cardiopulmonary bypass (off-pump coronary artery bypass grafting). Ann Thorac Surg. 2004;77:1023–7.
Mariani M, vn Boven W, Duurkens VAM, et al. Combined off-pump coronary surgery and right lung resections through midline sternotomy. Ann Thorac Surg. 2001;71:1342–4.
Marcucci C, Chassot P-G, Gardaz J-P, Magnusson L, et al. Fatal myocardial infarction after lung resection in a patient with prophylactic preoperative coronary stenting. Br J Anaesth. 2004;92:743–7.
Shudo Y, Takahashi T, Ohta M, et al. Radical operation for invasive thymoma with intracaval, intracardiac and lung invasion. J Card Surg. 2007;22:330–2.
Nakajima J, Morota T, Matsumoto J, et al. Pulmonary intimal sarcoma treated by a left pneumonectomy with pulmonary arterioplasty under cardiopulmonary bypass: report of case. Surg Today. 2007;37:496–9.
Venuta F, Ciccone AM, Anile M, et al. Reconstruction of the pulmonary artery for lung cancer: long-term results. J Thorac Cardiovasc Surg. 2009;138:1185–91.
Ratto GB, Costa R, Vassallo G, et al. Twelve-year experience with left atrial resection in the treatment of non-small cell lung cancer. Ann Thorac Surg. 2004;78:234–7.
Francesca L, Frazier OH, Radovancevic B, De Caro LF, Reul GJ, Cooley DA. Concomitant cardiac and pulmonary operations for lung cancer. Tex Heart Inst J. 1995;22:296–300.
Lennon PF, Hartigan PM, Friedberg JS. Clinical management of patients undergoing concurrent cardiac surgery and pulmonary resection. J Cardiothorac Vac Anesth. 1998;12:587–90.
Dowd NP, Karski JM, Cheng DC, Carroll JA, Lin Y, James RL, Butterworth J. Pharmacokinetics of tranexamic acid during cardiopulmonary bypass. Anesthesiology. 2002;97(2):390–9.
Sharma V, Fan J, Jerath A, Pang KS, Bojko B, Pawliszyn J, Karski JM, Yau T, McCluskey S, Wąsowicz M. Pharmacokinetics of tranexamic acid in patients undergoing cardiac surgery with use of cardiopulmonary bypass. Anaesthesia. 2012 Nov 1;67(11):1242–50.
Jearth A, Yang JQ, Pang KS, Lobby N, Vasicic T, Reyes N, Bojko B, PAwliszyn J, Wijeysundera D, Beattie WS, Wąsowicz M. Tranexamic acid dosing for cardiac surgical patients with chronic renal dysfunction: a new dosing regimen. Anesth Analg. 2018.; published ahead of print
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Case Presentation
Case Presentation
Case
A 21-year-old patient admitted for redo cardiac surgery for resection of recurrent left atrial angiosarcoma invading pulmonary tissue which was demonstrated on a recent follow-up chest X-ray and CT scan (see Figs. 40.6 and 40.7). The proposed procedure will also involve resection of pulmonary parenchyma. His previous surgery was performed 3 years ago without complications and followed by multiple courses of chemotherapy. He has no other significant co-morbidities. Anaesthesiologist is asked to decide whether patient is going to tolerate combined cardiac-thoracic procedure and what additional test he would like to perform.
Questions
-
What additional tests would you order?
-
Will the patient tolerate procedure? What kind of thoracic procedure will the patient require to achieve complete eradication of his tumour?
-
What is your anaesthetic plan?
-
Do you have any specific concerns related to intraoperative management?
-
What kind of postoperative complications can you expect?
Picture presents intraoperative transesophageal echo findings (Figs. 40.8 and 40.9).
Questions
-
What cardiac procedure should be performed?
-
Which pulmonary veins are invaded?
-
What postoperative complications would you expect?
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wąsowicz, M. (2019). Anaesthesia for Combined Cardiac and Thoracic Procedures. In: Slinger, P. (eds) Principles and Practice of Anesthesia for Thoracic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-00859-8_40
Download citation
DOI: https://doi.org/10.1007/978-3-030-00859-8_40
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-00858-1
Online ISBN: 978-3-030-00859-8
eBook Packages: MedicineMedicine (R0)