Abstract
Trypanosoma cruzi, etiological agent of Chagas disease, has evolved a complex interaction with mammalian cells and insect vector’s intestine. During its journey between these environments, it is subject to stressful changes. To overcome them, parasites use numerous strategies. Different stages contact diverse compartments of hosts and vectors thus assuring survival and multiplication. Surface proteins, some identified in particular stages of the protozoan, are critical for interaction with the milieu although their relevance is not totally understood for many. Parasite molecules allow T. cruzi to progress in the vector intestine, to duplicate and differentiate in order to become the infective stage for mammals. Surface molecules also allow parasites to advance through intracellular matrix of the mammals to reach the cells and, after recognition, invade them and adapt to survive but also to multiply and differentiate to circulating trypomastigotes thus assuring life cycle continuity. In this chapter we summarize T. cruzi pathways of humans and other reservoirs of infection as well as the participation of different T. cruzi lineages in geographical distribution and human disease. Finally, we review some of the mechanisms used by the parasite to reach, enter, and survive inside the host cell described so far.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Trypanosoma cruzi life cycle
- T. cruzi-vector interaction
- Host cell-parasite interaction
- Parasite-derived molecules
- Host cell invasion
- Parasitophorous vacuole
Trypanosoma cruzi is the etiological agent of American trypanosomiasis also known as Chagas disease. This is a complex health issue that should neither be merely approached from the understanding of parasite interaction with the insect vector and with the host cell, which is the matter of this chapter, nor from the point of view of patients and their clinical outcomes. Indeed, social and cultural determinants of people that suffer the disease must also be taken into consideration.
1 The Etiological Agent
Trypanosoma cruzi is a protozoan belonging to the Trypanosomatidae family. Other digenetic parasites of medical importance as the genus Leishmania are included in this family which is placed in the order Kinetoplastida. Microorganisms of this order are characterized by the presence of a structure called kinetoplast, which contains about 20% of the total DNA distributed in maxi- and minicircles, and a flagellum that is released by the anterior end of the parasite. The flagellum, well developed in the extracellular stages, grows in the proximity of the kinetoplast and emerges through the flagellar pocket with a location in relation to the nucleus which differs according to the parasitic stage. In natural conditions this parasite accomplishes an indirect life cycle, requiring two hosts to complete it: mammals are definitive and triatominae insects intermediate hosts.
1.1 Parasitic Stages
-
Trypomastigote : Nondividing elongated form (20–30 μm) with a vesicular nucleus and the kinetoplast located behind it. The flagellum grows near the kinetoplast and emerges from the side of parasite’s body running under the cytoplasmic membrane to be released by the anterior end, thus giving the image of an extensive undulating membrane. This parasitic form is found in the insect vector and in the mammal.
-
(a)
Metacyclic trypomastigote: The result of epimastigote differentiation at the distal portion of the vector’s intestine or rectum. Being the infective form for the mammalian host, it is deposited with the feces of the insect and penetrates mucous membranes or skin lesions. Inside the host cell, this stage differentiates to the amastigote.
-
(b)
Blood trypomastigote: The infective form for both the insect vector and the mammalian host. It differentiates from the intracellular amastigote and can disseminate through the bloodstream to invade new cells. It enters the vector with the ingested blood from an infected mammal and differentiates to epimastigote in the digestive tract to begin the cycle in the intermediate host.
-
(a)
-
Epimastigote : Duplicative form that divides by binary fission, noninfective to the mammalian host and found in the midgut of the insect vector. It presents a fusiform aspect (20–30 μm in length), with a kinetoplast located between the nucleus and the flagellum. This last one grows next to the kinetoplast and emerges from the membrane body free in almost all its extension thus having a short undulating membrane.
-
Spheromastigote : This is an extracellular stage that differentiates in the midgut of the insect vector and divides by binary fission. It measures between 2 and 4 μm being morphologically similar to the amastigote but with a free flagellum that emerges from, and surrounds, the parasite body. This form is usually found in reduced numbers but increases under stress conditions. Epimastigotes also differentiate from these spheromastigotes while progressing toward the distal portion of the triatomine intestine (reviewed by [1]; reviewed by [2]).
-
Amastigote : The intracellular duplicative stage found in the mammalian host. It originates from the differentiation of metacyclic and blood trypomastigotes in the cytoplasm of infected host cells. It has a rounded shape, a large nucleus, a kinetoplast, and a short flagellum sequestered inside a flagellar pocket. Measuring 2–2.5 μm, it multiplies by binary fission.
-
Scheme of the most relevant T. cruzi stages can be seen in Fig. 1.
1.2 Parasite Body
The parasite body is delimited by a plasma membrane formed by a lipid bilayer. Most of the surface proteins are inserted through a glycosylphosphatidylinositol anchor which is a distinctive feature of the trypanosome parasites [3]. Under the inner leaflet, a network of subpellicular microtubules constituted by filaments of actin and tubulin organize the cytoskeleton. The membrane participates in complex functions such as cell differentiation, motility, and tissue migration. These protozoa possess well-developed endoplasmic reticulum, ribosomes, and Golgi apparatus. The kinetoplast is within the only mitochondria that runs through the cytoplasm of the protozoa. They also possess other specialized organelles: glycosomes that concentrate and compartmentalize the enzymes of the glycolytic pathway [4] and acidocalcisomes, with acidic pH and high content of calcium ions, that participate in the maintenance of intracellular pH and osmoregulation [5, 6].
The flagellar pocket from which the flagellum emerges is formed by a plasma membrane invagination. The flagellum has a typical structure of nine pairs of peripheral microtubules and a central pair and is associated with the basal corpuscle which in turn is composed of nine triplets of peripheral microtubules. The plasma membrane which constitutes the flagellar pocket does not present the subpellicular microtubule network. In this region and in the cytostome, another invagination of the plasma membrane found in some stages of the parasite, pinocytic vesicles can be observed that allow the incorporation of macromolecules and other substances into the cellular cytoplasm.
Considering that the parasite must adapt to diverse habitats such as insect vector’s intestine and mammalian host’s circulation and tissues, it is reasonable that each stage has its own antigenic, chemical, physiological, and morphological characteristics.
1.3 Taxonomic Classification
Protist kingdom
Subkingdom: Protozoa
Phylum: Sarcomastigophora
Class: Zoomastigophora
Order: Kinetoplastida
Family: Trypanosomatidae
Genus: Trypanosoma
Section: Stercoraria
Subgenera: Schizotrypanum
Species: Trypanosoma cruzi
According to Hoare [7], the genus Trypanosoma is divided into two sections: Salivaria, which comprises pathogenic species whose infective form is transmitted in saliva of the insect vectors (African trypanosomes), and Stercoraria, whose species complete their evolutionary cycle in the hindgut and are transmitted with the feces of the insect vectors. The species of the Stercoraria section are nonpathogenic except for T. cruzi.
1.4 Intraspecific Variation
Intraspecific variation in T. cruzi was first observed by Carlos Chagas [8] that mentioned, among others, differences in the virulence of this parasite recovered from a patient when injected into different experimental hosts as well as in the morphology of the circulating trypomastigotes. Differences in morphology among strains [9,10,11] as well as those related to virulence and lethal capacity [12, 13] have been confirmed in mouse experimental model of infection. Others, such as tissue tropism [14, 15], modulation of immune response [16, 17], pathological features [18], and placental pattern infection and interference in fertility in a strain-dependent manner [19, 20], had been reported, too.
First attempts to group T. cruzi strains were related to characterization of biodemes , zymodemes, and schizodemes . The biodemes were described by Andrade [21, 22], zymodemes by Miles et al. [23], and schizodemes by Morel et al. [24]. In [25], Souto et al., based on DNA markers, defined two major phylogenetic lineages: TcI and TcII. The latter, due to its heterogenicity, was subdivided into five groups (TcIIa–e). An experts meeting revised the T. cruzi nomenclature to reach a consensus, and T. cruzi lineages were classified into six “discrete typing units” (DTU ) [26]. The term DTU was proposed by Tibayrenc in [27] to underline that these discrete genetic entities “can be characterized by given genetic markers or given sets genetic markers.” Still, all DTUs are able to infect humans. The geographical distribution of each DTU has been already described [28, 29] in a nice review recently published.
TcI has a great geographic range dispersion in the three American continents and is associated with sylvatic and domestic cycles. In the sylvatic cycle, Rhodnius species with arboreal niches are its primary vectors, and mammals with sylvatic habits are the primary hosts. This DTU has been reported to have important genetic heterogenicity. Hernández et al. [30] referred two subdivisions of TcI (TcIDom and TcI sylvatic). In Colombia, they reported as the main DTU TcI and when referred to human infection the predominant genotype was TcIDom during the chronic phase. In México, Central America, and the northern of South America, TcI predominates in the human infection being associated in these regions with cardiomyopathy [31].
TcII has been isolated in the southern and central regions in South America. In humans it has been associated with cardiac and digestive manifestations. In the Southern Cone, this DTU is rarely found except in some areas of central and east of Brazil [28] and is usually related to the domestic rather than with the sylvatic cycle [32].
Regarding DTU TcIII, human infection is extremely rare with only few cases reported in Colombia [28, 31]. It has been isolated from domestic dogs in the northeastern of Argentina, and Triatoma infestans is the most feasible vector ([28];· [33]). In the Paraguayan Chaco, Acosta et al. [34] reported that armadillo species are the principal reservoir of this DTU in the sylvatic area.
TcIV is present in North and South America, showing distinct lineages in both geographic areas [35]. It is the secondary agent for Chagas disease in Venezuela and associated with human outbreaks in the Western Brazilian Amazon [31, 36].
In the southern and central areas of the southern South American countries, TcV and TcVI are the most prevalent DTU infecting humans. Both are natural hybrids of lineages II and III and are responsible for chronic Chagas disease as well as the infections by vertical transmission [28, 29]. In the northern of Argentina, Diosque et al. [37] reported five genotypes circulating in the area under study. One of these genotypes was TcV—associated with humans—and the other TcVI, associated with dogs. Authors did not find apparent association between these T. cruzi genotypes and the domiciliated vector T. infestans. Also in the north of Argentina (Santiago del Estero Province), TcVI was the most frequent DTU in the same vector in rural areas, while TcV predominated in vectors recovered from communities where house infestation was higher [38]. The same group reported, in the Argentinean Chaco, TcVI as the first DTU infecting T. infestans and TcV the second. Bugs infected with TcV were captured in domicilies, while those infected with TcVI, both in domicilies and peridomicilies [39]. The initially described geographic restriction of these DTUs to the Southern Cone of South America may not be so strict. In Colombia, even when the most prevalent DTU was TcI, all remaining DTUs have been reported in domestic and sylvatic foci, including TcV and TcVI [40].
Research has been conducted by several authors trying to correlate particular DTUs with the pathogenesis and clinical outcome of the disease. Studies on the field regarding tissue tropisms [41, 42], cardiomyopathy [15], immune response [43], immune suppression [44, 45], cytokines profile [46], and sensitivity/resistance to parasiticide drugs [47,48,49] have been reported.
However, the complexity of T. cruzi population added to the diversity of the genetic background of human hosts makes it difficult to confirm any association [50, 51]. On the other hand, both vector and mammals can be infected with more than one DTU. This might result in misinterpretations due to differences in duplication speed or in tropisms for the diverse parasite populations [28]. Up to date, major progresses have been related to the ecoepidemiology of T. cruzi DTUs. Other correlations require additional studies.
1.5 T. cruzi Surface Molecules
Several surface proteins have been identified in the different stages of this protozoan, but for a large number of them, their relevance is not yet understood. Alves et al. [52] analyzed T. cruzi glycoprotein profile and reported 334 different glycoproteins exclusive of tissue culture-derived trypomastigotes (the in vitro equivalent to the circulating trypomastigote stage) and 170 exclusive of the epimastigote stage. Other authors, studying molecules released by the trypomastigote stage to the culture medium, identified 540 different proteins [53]. Many of these proteins are constitutively or transiently present at the parasite surface, whereas others are secreted to the media. For some, relevance to survival or the biological cycle of the parasite is known, either because of their role in adhesion, host cell recognition, and invasion or in mechanisms of the parasite differentiation. Diverse stage-specific proteins have been identified whose functions are being studied and disclosed.
In Table 1 some relevant molecules of the infective parasitic stages as well as their main features and assigned functions are mentioned.
2 Intermediate Host
The first record of triatominaes in America dates from the year 1590, when the priest Ronaldo de Lizarraga described them and their hematophagous habits on its expedition to Argentina [74]. On the other hand, Charles Darwin made a clear account of these bloodsucking insects in his journey through South America. He noted in the diary he kept during his voyage at the Beagle, on the 25th of March 1835: “At night I experienced an attack (for it deserves no less a name) of the Benchuca (a species of Reduvius) the great black bug of the Pampas. It is most disgusting to feel soft wingless insects, about an inch long, crawling over one’s body. Before sucking they are quite thin, but afterwards become round and bloated with blood, and in this state they are easily crushed” [75].
2.1 Taxonomic Classification
Animalia Kingdom
Phylum: Arthropoda
Class: Insecta
Order: Hemiptera
Family: Reduviidae
Subfamily: Triatominae
Genus: Panstrongylus, Triatoma, Rhodnius, etc.
2.2 Main Species of Vectors and Geographic Distribution
There are more than 130 bloodsucking Hemiptera of the family Reduviidae that can potentially participate as intermediate hosts of T. cruzi, although only a few species are competent vectors [76]. Among the most important for human transmission are those that acquired domiciliary habits as Triatoma infestans, Rhodnius prolixus, Panstrongylus megistus, and Triatoma dimidiata.
T. infestans is the main vector in endemic sub-Amazonian areas and countries of the Southern Cone. In Brazil, at the sub-Amazonian Atlantic coast, it coexists with P. megistus. R. prolixus is distributed in Central America and Colombia, and T. dimidiata extends from northern Mexico and Central America to the Pacific coast in Colombia and Ecuador [77]. In Argentina and Chile, the main responsible species for the transmission of T. cruzi is T. infestans, an anthropophilic vector that extends to the parallel 45° South.
2.3 Biological Cycle of the Insect Vector
The life cycle of triatomines includes egg stages, five nymphal or immature stages that molt into the male and female adults (imagoes) (Figs. 2 and 3). This hematophagous insect feeds through a proboscis (sucking organ). Its digestive system comprehends an initial portion of the intestine (pharynx and esophagus), followed by the middle intestine which is divided into the anterior midgut (stomach where the concentration and lysis of red blood cells begin) and the posterior midgut (where blood is digested and nutrients absorbed) (Fig. 4). The middle intestine is of endodermal origin, ending in the rectum, which, like the pharynx and esophagus, is of ectodermal origin. Having an incomplete metamorphosis, the nymphs share the same habitat and eating habits of the adult stages thus being hematophagous and able to become infected and transmit T. cruzi. As in other bloodsucking insects, the salivary glands secrete anticoagulant substances that prevent ingested blood from clotting. Blood feeding is necessary for molting (ecdysis). A full blood meal distends the abdomen, and the mechanical effect acts on neurosecretory cells that stimulate the secretion of ecdysone to the hemolymph, thus regulating the process of ecdysis as well as the levels of the juvenile hormone involved in the growth of nymphal stages [1, 2, 78]. After each meal insects can spend prolonged periods without feeding. Usually only one feed is required between each molting.
Evolutive stages of triatomines. From: Ministerio de Salud de la Nación (www.msal.gov.ar)
Adult of Triatoma infestans. From: Ministerio de Salud de la Nación (www.msal.gov.ar)
3 Trypanosoma cruzi Life Cycle
The vector can ingest circulating trypomastigotes when it feds on an infected host. Infection depends not only on the number of parasites present in the blood meal but also on the virulence of the ingested parasite population [79, 80]. Blood trypomastigotes differentiate into epimastigotes in the anterior midgut of the insect vector (stomach). Some spheromastigotes may also be found which, like epimastigotes, are duplicative but not infective stages (reviewed by [1]). Epimastigotes progress to the posterior intestine, and, at the level of the rectum, they differentiate into metacyclic trypomastigotes. This process is known as metacyclogenesis (Fig. 5). Metacyclic trypomastigotes are eliminated with the feces of the vector when it defecates while feeding from the definitive host. Infective to mammals, metacyclic trypomastigotes enter the definitive host through the bite, skin lesions, or mucous membranes. Metacyclic trypomastigotes infect phagocytic and non-phagocytic cells near the site of entry. Inside the cells they differentiate to amastigotes which divide actively and subsequently differentiate into trypomastigotes. This stage can enter new cells in the proximity or can reach circulation to disseminate through other tissues or to be ingested by a new vector. Following penetration into the cells, trypomastigotes are surrounded by a parasitophorous vacuole in the host cell cytoplasm. Immediately, the process of transformation to the amastigote stage begins, together with the disruption of the membrane vacuole. Subsequently, the amastigote, free in the cytoplasm, begins the process of binary cell division that continues for several days, depending of the T. cruzi strain [81]. Then the process of differentiation of these forms into trypomastigotes begins. In this transition the parasite acquires a free and long flagellum being the activity of motile parasitic form apparently responsible for the cell rupture and its release to the intercellular space [82]. The cycle restarts when a triatomine is fed on the infected mammal.
Biological cycle of T. cruzi. (1) Triatomine bug takes a meal and passes metacyclics in feces; trypomastigotes enter through a wound or through mucosal membrane such as conjunctiva. (2) Metacyclic trypomastigotes penetrate various cells at bite wound site. Inside these cells they differentiate into amastigotes. (3) Amastigotes multiply by binary fission inside the cell. (4) Intracellular amastigotes differentiate into trypomastigotes, burst out the cells, and enter the bloodstream. Circulating trypomastigotes can invade other cells differentiating into amastigotes in new cell sites. (5) Triatomine bugs take a blood meal containing circulating trypomastigotes. (6) In the midgut they differentiate to epimastigotes. (7) Epimastigotes duplicate in the midgut. (8) Epimastigotes differentiate to metacycle in the hindgut. i infective stage, d diagnostic stage. Adapted from PHIL.CDC/Alexander J. da Silva/Melanie Moser
3.1 Domestic Cycle
T. cruzi household life cycle occurs between man or domestic animals (such as dogs, cats, rodents) and insects with domiciliary habits (such as T. infestans). This cycle takes place in endemic areas in the context of precarious dwellings. In these houses all vector stages raise in holes, wall irregularities, and ceilings depending on the material used (straw, palm leaves, wood) or are located behind pictures and furniture. Adults and nymphal stages leave these places at night to feed. Dogs are ideal reservoirs for the maintenance of the cycle since, in general, they present high parasitemia and cohabit with man and insects inside the house [83,84,85].
Vector control to interrupt the domiciliary cycle has been addressed in the American region in collaboration between the countries of the region and PAHO. With the implementation of several initiatives (Southern Cone, Central America and Belize, Andean, Amazon basin), interrupting T. cruzi transmission by T. infestans has been certified in countries such as Chile, Uruguay, and Brazil—excluding the area of the Amazon. In other regions this has been partially achieved as in some provinces of Argentina [86, 87]. However, we must bear in mind that dwellings free of domiciliary vectors can be reinfested if a strict and sustained epidemiological surveillance is not carried out [88].
The peridomicile is the space near the house used by the man to carry out its activities, including the nocturnal rest, and to maintain domestic animals as in corrals, chicken coops, dovecotes, etc. Being an extension of the house, domestic animals as well as wild ones can enter and leave, and light and blood supply can attract wild triatominae to this area. Therefore, this space can function as a bridge between domestic and wild cycle. In a study carried out in northwestern Argentina, in the Province of Misiones, an area reported free of vector transmission by T. infestans, the relevance of this bridge has been evidenced by the high infection rates found in marsupials of rural areas near the houses and by the documented infection of two vampire bats caught inside a house [89].
3.2 Sylvatic Life Cycle
The primary cycle of T. cruzi is precisely the wild one, being the human infection very recent in an evolutionary scale. Being essentially enzootic, the protozoon circulates in extensive areas of America among numerous mammals and vectors that vary according to environmental factors and food availability. It is considered that the infection causes very mild or does not cause damage to natural hosts. In this cycle definitive hosts comprise wild animals such as marsupials, rodents, foxes, bats, or monkeys, among others. Vectors are adapted to live in nests of birds, weasels, and rodents, caves of bats or other animals, tree holes, etc. Palms are colonized in extense areas of Central America, Ecuador, and Venezuela mainly, but not exclusively, by species of the Rhodnius genus. Palms are also a common habitat of sylvatic vectors in Brazil [90, 91].
4 Non-vectorial Pathways of T. cruzi Infection
This protozoan parasite can infect humans by routes not requiring the participation of the insect vector. Such routes, mainly blood transfusion and mother to child transmission, are responsible for Chagas disease transmission in vector-free regions and for disease emergence in Europe, the United States of America, Canada, and Asian developed countries [92, 93].
4.1 Blood Transfusions
Most chronically infected people which are asymptomatic but with fluctuating parasitemia are unaware of their infection status. This situation makes blood donation a risk for T. cruzi transmission that is proportional to Chagas disease prevalence among blood donors. To avoid this risk, screening coverage in blood banks must be adopted and blood units from reactive donors discarded. In areas where the infection rate of potential donors is very high and/or blood screening unfeasible, some strategies of parasite reduction—mainly against bloodstream trypomastigotes—have been proposed. The only strategy currently used is the treatment with gentian violet 1: 4000 for 24 h at 4 °C. This treatment, although highly effective, does not guarantee 100% elimination of the parasites, depending on the parasite population [94, 95].
In most endemic countries, the coverage has reached almost 100% in the last years. In these countries, serological control is mandatory and has been legislated, which has significantly reduced the risk of transmission [92].
4.2 Congenital or Connatal Route
Any women with Chagas disease can transmit T. cruzi to the fetus both transplacentally during pregnancy and at the time of delivery. Child infection status should be studied at birth and during the first months of life using direct diagnostic methods and serologically after 8–10 months. When positive, infants should be treated with parasiticide drugs [96]. The transmission rate is usually low (2–10%) with variations between endemic regions. An infected mother who has transmitted the infection to a child will not necessarily transmit the infection in succeeding pregnancies. In a study conducted by Juiz et al. [97], an association between polymorphisms in genes expressed in the placenta and susceptibility to congenital infection was demonstrated. The authors suggest that polymorphisms of proteins participating in extracellular matrix remodeling can mediate susceptibility to vertical transmission of the parasite.
4.3 Organ or Tissue Transplantation
The ideal conditions to carry out a solid organ transplant are having both donor and recipient free of T. cruzi infection. When this aim is not feasible mainly due to the high prevalence of Chagas disease in some endemic areas, there are rules strictly regulated by the competent institutions of affected countries. With few exceptions, when the patient is infected and the organ to be transplanted comes from a healthy individual, the transplant can be performed. The transplant receptor must be periodically studied to determine whether the immunosuppressive treatment administered to avoid graft rejection lead to reactivation of the infection to promptly initiate parasiticide treatment. When the donor is infected, the recommendation to transplant depends on the organ to be transplanted and on the infection status of the recipient. It is feasible to perform transplants of various solid organs with varying degrees of success [98,99,100,101]. In Argentina the institution which reviews and updates the procedures as established by transplants Law No. 24,193 is INCUCAI. Its Resolution 269/99 indicates for Chagas disease specifically the conditions to perform transplants (https://www.incucai.gov.ar/files/docs-incucai/Legislacion/03-ResIncucai/Procuracion-y-trasplante-de-organos/07-res_incucai_269_99.pdf).
4.4 Oral Route
This mode of infection occurs upon ingestion of food or beverages contaminated with feces from T. cruzi infected triatomine bugs. It is more common in regions with sylvatic cycles and less frequent outside. In recent years outbreaks of acute infection have been reported in Brazil, Venezuela, and Colombia. Metacyclic trypomastigotes express at their surface the glycoprotein Gp82, which has an adhesion site for gastric mucins. The parasite adheres to them and penetrates the epithelial cells of the stomach multiplying then spreading through the bloodstream [66, 67].
4.5 Laboratory Accidents
Infection can occur among health workers and scientists through the manipulation of blood, tissues, or culture media containing trypomastigotes or amastigotes of this parasite. The risk of having an accident can be minimized by following biosecurity recommendations. The routes of infection can be percutaneous, inoculation, or oral.
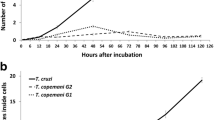
5 The Parasite in the Insect Vector
The digestive tract of triatominaes is the anatomical site where the parasite develops part of its biological cycle. Insects feed on blood, both from mammals and birds. While birds are resistant to infection by T. cruzi, mammals are not. Accordingly, circulating trypomastigotes enter vectors that feed on infected mammals including man. The digestive tract of the vector is a hostile medium for the parasites in which they are subject to changes in temperature or the presence of molecules and intestinal microbiota particular of insects, among others. During the first 24 h post-meal, the number of ingested trypomastigotes decreases significantly at the stomach level. With the purpose of adapting to the new microenvironment and to avoid the deleterious action of insects on the trypomastigotes, the protozoa differentiate into intermediate forms to finally transform into the duplicative epimastigotes. When they pass to the posterior intestine, epimastigotes adhere to the cells of the outer membrane of the microvilli and pursue multiplication. After a couple of months, numerous epimastigotes reach the rectum, adhere to the hydrophobic wax layer of its cuticle, and differentiate into metacyclic trypomastigotes ([102]; review by [2]; review by [103]).
5.1 Metacyclogenesis
Numerous stimuli have been described that play a role in inducting differentiation to metacyclic forms. The activity of vector intestine extracts in metacyclogenesis has been reported [104,105,106], and isolated factors of insect’s hindgut inducing in vitro differentiation have been characterized [107]. Among these factors are a fragment of αD-globin and a peptide that activates adenylyl cyclase in the membrane of epimastigotes [108], and others are free fatty acids, mainly oleic acid [109, 110]. The differentiation mechanism is promoted by the physicochemical characteristics of vector’s intestine [111]. Other authors have demonstrated that insect’s long fasting periods that cause metabolic stress trigger metacyclogenesis. This effect can be reproduced in vitro when culturing epimastigotes in poor culture media that induce nutritional stress such as TAU and M16 media [1, 112, 113]. Hamedi et al. [114] have reported that during in vitro starvation-induced metacyclogenesis, there is an increase in the expression of adenylyl cyclase, coincident with the observations made by Fraidenraich et al. [108] using insect extract stimulation.
5.2 Selectivity Among the Parasitic Populations and the Vectors
Each triatominae species has a different affinity for the diverse parasitic populations. So, the infection rate and the success of metacyclogenesis will correlate to the greater or lesser affinity between vector and parasite. In this sense, it has been reported that, in a single triatominae species, the rate of metacyclogenesis can vary depending on the T. cruzi strain used. On the other hand, different numbers of metacyclic trypomastigotes can be recovered among different triatominae species infected with the same parasitic population [79, 115,116,117].
6 The Mammalian Host
T. cruzi has a low specificity for definitive hosts thus having the capacity to infect virtually any mammal. Humans, and domestic animals like dogs and cats, usually become infected inside human dwellings or in the peridomicilia. Domestic animals as goats, guinea pigs, and domiciliated rodents can also become infected in the peridomicilia. All of them are reservoirs of the parasite (among which the dog stands out as already mentioned), and they are of the utmost importance as they can be responsible for the transmission of T. cruzi to man. In wild areas, several mammals, including the opossum, the only marsupial species in South American, are naturally infected, and some of them, having high parasitemia, act as very efficient reservoirs. Monkeys, armadillos, wild rodents, and bats can become infected at variable rates.
During the vectorial cycle of T. cruzi, metacyclic trypomastigotes are responsible for the initiation of infection in the definitive host. This stage is unable to penetrate intact skin but takes advantage of skin abrasions or the mucous membranes to enter the host. Once inside host tissues, trypomastigotes transit through the extracellular matrix to contact the target cell [118,119,120]. This stage invades cells near the site of entry first and differentiates into intracellular diving amastigotes. Depending on the parasite population, the number of successive divisions varies [81]. Then, amastigotes differentiate into circulating trypomastigotes, which break down the cell, disseminate through blood, and reach various tissues where they initiate new cycles of intracellular multiplication.
In the different periods of infection, parasitemia levels vary, being during the chronic phase extremely low and fluctuating but enough to infect a vector insect while ingesting blood from an infected mammal.
6.1 Any Cell Can Be Host of T. cruzi
As already mentioned, T. cruzi can invade a wide range of vertebrate hosts being capable of dwelling inside virtually any nucleated cell including diverse laboratory cell lines. The process of invasion, infection, and differentiation occurs even in cells whose nuclei have been removed, thus indicating the independence of this process on host transcriptional machinery [121, 122]. In natural mammalian infection, metacyclic trypomastigotes locally invade epithelial cells, macrophages, fibroblasts, and adipocytes, and then circulating trypomastigotes disseminate to diverse tissues infecting muscle cells, cardiomyocytes, and nerve cells [123]. This high degree of versatility can only be achieved through the development of multiple invasion strategies by this ubiquitous protozoan. Controversies also arise considering the myriad of host cell-entry mechanisms described so far being difficult to conceal a uniform model. Different host cell types, parasite isolates, or strains and even different parasite stages take part in in vitro models of host-parasite interaction giving sometimes opposite results. These features can also reflect T. cruzi ability to use tailored mechanisms of entry according to the characteristics of host cell contacted.
6.2 Navigating Across the Extracellular Matrix
Invasive stages of T. cruzi (e.g., bloodstream trypomastigotes, metacyclic trypomastigotes, and extracellular amastigotes) are known to interact with different components of the extracellular matrix (ECM) as the proteins laminin, thrombospondin, collagen, and fibronectin and proteoglycans (heparin, heparan sulfate). T. cruzi exploits them to reach host cells and initiate the process of cell invasion. Infective forms of the parasite upregulate the expression of ECM components laminin gamma 1 or thrombospondin 1, but their silencing by RNAi reveals a dramatic reduction of cell infection [120]. To infect muscle cells, T. cruzi must cross the basal lamina that surrounds them. For this, the trypomastigote stage-specific surface molecule Gp83 mediates the upregulation of laminin gamma 1, thus participating in parasite adhesion to the host cell. This observation correlates with the finding of laminin deposited in hearts of T. cruzi-infected patients [124]. Calreticulin is a well-conserved intracellular calcium-binding chaperone; it has been described in diverse parasite species including T. cruzi [125]. Parasite calreticulin (TcCRT/Tc45) is also expressed at the surface of infective trypomastigotes and may act as a receptor for the collagen tail of C1q and for mannan-binding lectin to promote phagocytosis through C1qR. Surface-expressed TcCRT is also known to interact with host thrombospondin 1 enhancing cellular infection [126]. The ECM human lectin, galectin-3, binds to a 45 kDa trypomastigote surface mucin in a lectin manner. This lectin simultaneously binds to laminin of basement membranes via carbohydrate recognition domains, thus providing a bridge between the parasite and muscle cells [127, 128]. Considering that galectin-3 concentrations in fluids can increase during microbial infection [129], T. cruzi may have adapted this trapping mechanism to recruit parasites at the ECM enabling cellular invasion. The prolyl oligopeptidase Tc80 secreted by infective trypomastigotes is involved in collagen and fibronectin hydrolysis. Selective inhibitors of its proteinase activity can block parasite entry to the host cell [130]. Some reports suggest that parasite proteases as Tc85 a glycoprotein from the Gp85/trans-sialidase (Gp85/TS) multigene family interact with diverse components of the ECM as laminin, the intermediate filament proteins cytokeratin and vimentin, fibronectin, mucin, and the prokineticin-2 receptor [118, 131]. Regarding the interaction of the metacyclic trypomastigotes, the infective stage from the insect vector, with components of the extracellular matrix, Maeda and coworkers described that this parasitic stage binds and degrades fibronectin by means of the stage-specific glycoprotein Gp82 [119]. Cruzipain, the major T. cruzi cysteine proteinase which also digests fibronectin, acts synergistically to increased metacyclic trypomastigote internalization. Considering the diverse nature and composition of the extracellular matrix between different tissues and the dynamics of this extracellular mesh, it is tempting to suggest that T. cruzi-ECM interactions are relevant for parasite virulence and tissue tropism. Furthermore, changes in the physiological condition of ECM driven by chronic infection may have implications for the pathogenesis of the disease in target tissues.
6.3 Attaching to the Host Cell Surface
Most of the knowledge on the interaction between parasites and cells has been obtained from in vitro studies. Trypomastigotes can initiate the process of cell invasion once they have recognized cell surface receptors at the host cell. These receptors have not been clearly identified, but they interact with a large number of well-characterized parasite’s surface-membrane protein ligands. Parasite ligands are grouped into different families as mucins, trans-sialidases (TS), TS-like proteins, and membrane proteins. The best characterized are members of the Gp85/trans-sialidase family [132]. However, recently some underrepresented families as the TcTASV members have attracted attention [64, 65]
6.3.1 Role of Gp82 and Gp90 in Oral Infection
Mucin-like surface glycoproteins are expressed in the outer membrane of metacyclic trypomastigotes which makes this parasite stage resistant to gastric environment. Owing to this, this stage is able to invade intestinal epithelial cells of mammals.
At least two main glycoproteins, Gp82 and Gp90, which belong to the Gp85/TS superfamily, are known to participate in host cell invasion. While Gp82 has a central role in host cell recognition and invasion, Gp90 negatively regulates parasite entry [68].
Gp82 is highly conserved among T. cruzi strains and binds gastric mucins [67] being the peptide p7 the chief mucin-binding site, followed by p10 [66]. Gp82 is attached to the outer membrane of the parasite by a glycosylphosphatidylinositol anchor and confers resistance to the low pH of the stomach. Gp82-mucin signaling though results in an increase of intracellular Ca2+, thus launching the invasion process. Those T. cruzi strains that are deficient in Gp82 are poorly invasive.
Parasite strains that express high levels of Gp90 are likewise poorly invasive. This molecule binds the target cell but fails to induce or induces low Ca2+ mobilization [133]. This glycoprotein possesses various isoforms, some of them susceptible to gastric pepsin digestion. Thus, infectivity of a T. cruzi strain may be exacerbated according to Gp90 sensitivity to these gastric juices [69].
6.3.2 Role of Gp85/TS in Adhesion and Survival into Mammalian Host Cells
First identified as a 85 kDa surface protein of T. cruzi, it is now known to belong to a multigene glycoprotein superfamily named Gp 85/TS [134]. Every member of this superfamily shares a sialidase domain with a peptide motive called FLY. Due to its complexity, the superfamily was subdivided into groups [135]. Proteins from group I are those which possess TS with enzymatic activity, while those of group II lack from this activity.
Gp85 without enzymatic activity have been associated with mammalian cell invasion. Mattos et al. [136] reported that the N-terminus of Gp85 binds to laminin and induces dephosphorylation of cytoskeletal proteins. Otherwise, at the C-terminus, the FLY sequence binds to cytokeratin, major constituents of intermediate filaments in the host cells, which results in increased cell invasion. A small peptide motif (TS9) reported by Teixeira et al. [131] shared by all Tc85 proteins is also capable to bind cytokeratin, as well as vimentin. Both FLY and TS9 are located inside of a laminin-G-like domain at the C-terminus. The authors propose that TS9 and FLY, which are far separated in a linear sequence, could be located next to each other in a tridimensional conformation, thus displaying a nonlinear keratin-binding site. This plasticity of parasite surface protein helps to overcome the barriers of ECM and those of host cell membrane [58]. FLY conserved sequence also binds to endothelium with a significant avidity for heart vasculature reinforcing its role in cell invasion and implications in homing [137].
Zingales et al. [138] described how trypomastigotes incorporate to their surface sialic acid from compounds as fetuin but not free sialic acid directly. Parasites with TS enzymatic activity can transfer sialic acid from glycoconjugates of the hosts to acceptor mucin molecules exposed in their outer membrane. Sialidation of parasite surface proteins is required for invasion of mammalian cells [60]. TS molecule comprises two domains, the C-terminus which is an immunodominant antigen made of amino acid repeats (shed acute-phase antigen—SAPA) and the N-terminus which possesses the enzymatic activity [139, 140]. Even though both are antigenic, SAPA is immunodominant producing an early strong antibody response during acute infection. These antibodies react specifically against the nonenzymatic portion of the whole molecule [141]. It has been speculated that this is a parasite strategy to delay an antibody response against the enzymatic activity leading to its neutralization.
TS is the major virulence factor of T. cruzi. It is engaged in numerous steps that allow host cell invasion and adaptation to the intracellular lifestyle (review by [59]). The first obstacles that parasites must avoid are innate mammal defense mechanisms as complement lytic activity and macrophage activation. Trypomastigotes, but not epimastigotes, are resistant to complement lysis due to the presence of a surface molecule similar to human decay-accelerating factor which interferes with the C3 convertase, thus inhibiting complement cascade [142]. After skewing this obstacle and getting across the ECM, the parasite proceeds to invade the cell using diverse mechanisms described in Sects. 7.1–7.3. Inside of the parasitophorous vacuole (PV; see Sect. 9), trypomastigotes and amastigotes secrete lytic factors which are active at low pHs and specially on desialidated membranes. So, when lysosomes fused and acidified inside the PV, TS enhances parasite resistance to this environment and contributes to the disruption of the PV membranes, setting parasites free in the cytoplasm (see Sect. 9.2). This is one of the most relevant TS activities [61, 143].
TS also plays an important role in the modulation of host immune response [144, 145]. Ruiz Díaz et al. [146] reported how TS deflects the Th1 phenotype, which is protective against T. cruzi but also promotes host tissue damage, while stimulating a Th2 phenotype response. This strategy is useful for T. cruzi establishment and to reach an equilibrium between host and parasite, with survival of the former and persistence of the latter.
7 One Parasite with Multiple Mechanisms to Enter the Host Cell
In a remarkable fashion, trypomastigotes can enter both phagocytic and nonprofessional phagocytic cells to finally access host cell lysosomes. Establishment in a lysosomal-based vacuole is required for a successful infection. For this, the parasite has evolved to exploit assorted cellular pathways to reach this host cell compartment. Excellent reviews have been published on this subject; thus we offer here a brief description of some of the proposed mechanisms [122, 147, 148].
7.1 Lysosomal-Dependent Exocytic Pathway
In 1991, Schenkman et al. [149] demonstrated that T. cruzi entered nonprofessional phagocytic cells by an actin-independent mechanism distinct from phagocytosis. Later, it was verified that lysosomes are recruited to the plasma membrane at parasite attachment sites and that a vacuole is formed around the parasite by the fusion of lysosomes with the plasma membrane [150, 151]. The vacuole formation involves lipid remodeling by the delivery of acid sphingomyelinase that enriches in ceramides the outer leaflet of the plasma membrane [152]. By this route, parasites are readily directed to an acidic lysosomal vacuole. Reduction of peripheral lysosomes or inhibition of lysosomal fusion with plasma membrane results in reduced T. cruzi infection. The exocytosis of lysosomes ensues rapidly following parasite contact in a unidirectional movement toward the plasma membrane-parasite attachment site [153]. This process appears to depend on the Ca2+-binding protein synaptotagmin VI and kinesin motors on microtubules that require Ca2+-calmodulin [154, 155]. The parasite has the ability to trigger a mobilization of Ca2+ stores near the attachment site in a phospholipase C and inositol 1,4,5-triphosphate-dependent manner [156, 157]. Different works have suggested a participation of host cell plasma membrane lipid rafts and their associated proteins in T. cruzi invasion process. These microdomains are involved in T. cruzi entry in phagocytic and non-phagocytic cells as membrane cholesterol depletion by methyl-beta cyclodextrin, which hampers lysosomal recruitment to the plasma membrane, decreased in vitro T. cruzi infectivity [158]. Interestingly, this process of lysosome fusion with plasma membrane, first described for T. cruzi invasion, has been recognized as a plasma membrane wound repair mechanism regulated by intracellular calcium levels [159, 160]. These findings offer a conceivable explanation for the tissue tropism exhibited by T. cruzi within its vertebrate host and for a part of Chagas disease pathogenesis, as muscle cells exhibit increased in vivo plasma membrane injury with respect to other cell types [152, 161].
7.2 Endocytic Pathway
Early studies showed that, in conditions where parasite internalization and lysosomal association were inhibited, a fraction of vacuoles were initially devoid of lysosomal markers but gradually acquired lysosome-associated membrane protein 1 (lamp-1) and a fluid-phase endocytic tracer from the lysosomal compartment [149, 162, 163]. These experiments revealed that the parasite can also enter a vacuole composed of invaginated plasma membrane that subsequently fuses with endosomes and lysosomes. These lysosome-independent pathways have been observed in diverse mammalian cell lines and primary cardiomyocytes [163]. The membrane trafficking that leads to the final lysosomal location of the parasite is not completely understood. The GTPase dynamin, which plays an important role in clathrin-mediated endocytosis, and the GTPases Rab5 from early endosomes as well as Rab7 from late endosomes are required for host cell infection [164]. The findings revealed for the first time that the sources of donor membranes are diverse and include early and late endosomes prior to lysosome fusion of the endocytic vacuole [164]. Quantitative analysis has shown that this process represents 50% of parasite internalization and in 20% of them, the participation of early endosomes is detected by early endosome antigen 1 labeling of the vacuoles 10 min after infection [162].
7.3 The Autophagic Mode of Entry
The work from Romano and coworkers has recently established a connection between T. cruzi and host cell autophagic pathway. LC3, the most relevant autophagosome marker, colocalized with the T. cruzi parasitophorous vacuole (PV) following in vitro infection of Chinese hamster ovary cells with trypomastigotes. Real-time video microscopy revealed that, less than 1 h after infection, green fluorescent protein-tagged LC3 molecules already decorate autophagosomes which concentrated at the cytosolic face of the plasma membrane in the vicinity of T. cruzi contact sites. This interaction with LC3-positive compartments occurred early from the moment of PV formation and persisted until parasites located freely in the cytosol. Indeed, amastigotes located free in the cytoplasm (48–72 h postinfection) no longer colocalized with LC3 molecules. The relevance of autophagy mechanisms for T. cruzi invasion was demonstrated in studies where autophagy was induced by starvation or treatment with the mTOR inhibitor rapamycin [165]. Autophagy induction increased infection, and the absence of genes necessary for the early steps of autophagic pathway beclin-1 or Atg5 decreased this rate [165, 166]. Under autophagic conditions as starvation, host cells produce new sets of autolysosomal vesicles. These vesicles can be clustered to the cell membrane by infective trypomastigotes that exploit lysosomal exocytosis machinery to generate a PV to shelter them. Under full nutrient media in vitro conditions, cells produce a limited number of acidic lysosomes, thus reducing T. cruzi colonization. In experimental murine infection, it has been demonstrated that under starvation conditions tissues like heart and skeletal muscles are prone to establish sustained autophagy [167]. Romano et al. [168] suggest that, in human Chagas disease, life conditions of T. cruzi-infected individuals as nutritional deficit could induce autophagy, thus promoting tissue infection and chronic disease
7.4 Phosphatidylinositol 3-Kinase Signaling and the Parasitophorous Vacuole
The mechanisms of T. cruzi cell invasion described so far show that in the early steps of PV assembly, donor membranes can be from plasma membrane, lysosomes, endosomes, and even autophagosomes. However, the host cell signaling pathways that must be activated during T. cruzi invasion are less understood. Wilkowsky and coworkers demonstrated for the first time that non-phagocytic pathways of cell invasion decreased by wortmannin a phosphatidylinositol 3-kinase inhibitor [169]. They showed that molecules in the plasma membrane of trypomastigotes, but not of epimastigotes, were able to activate the host PI3K/PKB/Akt signal transduction cascade, relevant for cell proliferation, cytoskeleton reorganization, and membrane trafficking. In parallel, Chuenkova et al. [170] demonstrated that T. cruzi trans-sialidase was able to activate PI3/AKT signaling. First, it was acknowledged that PI3 kinase was relevant for lysosomal-independent T. cruzi invasion, but further experiments demonstrated the participation of this cascade in lysosomal-dependent pathway, thus revealing the universality of this signaling [163]. As seen with other signal transduction molecules like Ca2+, the PI3K/PKB cascade could be a common pathway used by several pathogens to invade and survive within host cells. Further work from Andrade and Andrews [171] described an alternative pathway of invasion which is lysosome-independent and wortmannin insensitive.
8 How to Survive Inside a Professional Phagocytic Cell?
Macrophages are one of the major targets of T. cruzi particularly following vectorial infection where metacyclic trypomastigotes deposited by the insect host can be spotted and captured by tissue-resident macrophages. Later, amastigotes released by disrupted cells are also engulfed by these professional phagocytic cells. Parasites are directed to phagolysosomes where they can be efficiently destroyed by oxidative species, a major effector mechanism of the antiparasitic innate immune response [172, 173]. The capacity of invading parasites to modulate macrophage activation before they can reach their cytoplasm is central to parasite survival. To cope with oxidative burst, parasites have evolved an antioxidant network shaped by enzymes and nonenzymatic redox-active molecules with varied subcellular distribution (e.g., endoplasmic reticulum, glycosomes, mitochondrion, and cytosol) [174]. It has been proposed that the potency of the antioxidant “shield” may vary between T. cruzi isolates thus dictating their final fate within the macrophage. Accordingly, the antioxidant complex can be considered as a T. cruzi virulence factor ([174, 175].; [176]). Alternatively, some parasites may survive inside professional phagocytic cells by invading them in non-phagocytic/active pathways as revealed by experiments where inhibition of actin polymerization failed to completely abrogate macrophage infection [177].
9 The Parasitophorous Vacuole (PV)
9.1 PV Always Ends Up as a Lysosomal Compartment
Regardless of the endocytic mechanism that takes place for parasite entry to the host cell, PVs always result in an acidic lysosomal compartment. Fusion with lysosomes occurs at the site of parasite entry or after entry with an already preformed PVs. Microtubules appear to be necessary for targeting lysosomes to these places. Upon entry, PVs also recruit endocytic vesicles (initial and late endosomes) in a process that together with the fusion of lysosomes leads to PV maturation through acidification. Lysosomal fusion is essential to the retention of parasite inside the cell as its blockade by wortmannin results in their exit to the extracellular milieu [171]. In addition to this finding, Woolsey and Burleigh demonstrated that the actin cytoskeleton-dependent processes of PV fusion with endosomal and lysosomal vesicles are necessary for parasite retention. In fact, the process of reversible invasion increased notably in cytochalasin D-treated host cells [162].
9.2 Degradation of the PV and Cytosolic Settlement
The establishment of productive intracellular infection depends on parasite location inside PV transformed into lysosomal compartments prior to their multiplication free in the host cell cytosol. In this continuous process, the parasite breaks down the vacuolar membrane in a lysosome- and pH-dependent mechanism [178, 179]. Early studies demonstrated that parasite trypomastigotes and amastigotes secreted a pore-forming factor related to complement component C9, the hemolysin TcTox [180], and another C9 cross-reactive membrane-targeted protein with hemolytic activity, LYT1 [181], whose precise role in PV disruption has not been demonstrated. It is proposed that both lytic molecules which are expressed and optimally active at the acidic pH brought by lysosomal fusion of the PV would promote membrane breakdown and cytosolic localization of the parasite. Surface TS enhances parasite resistance to this acidic environment while facilitating membrane destabilization. In fact, it was demonstrated that residence inside the vacuolar space increases parasite secretion of TS. Desyalidation of vacuolar membrane molecules, like LAMP-1, is a process suggested to foster the insertion of TcTox into the lipid bilayer [144].
10 Parasite Differentiation
The differentiation of infective trypomastigotes to intracellular amastigotes in the host cell cytoplasm is poorly understood, but in vitro evidence shows that it can take from 2 to 8 h depending on the infective strain. Launching trypomastigote-amastigote differentiation appears to require, among other signaling factors, the acidic pH provided by the lysosomal compartment [182] in a process also dependent on l-proline [183] and on phosphorylation/dephosphorylation events [184]. Quiescent amastigotes reenter the cell cycle and replicate in the cytosol a limited number of times until they occupy the host cell volume to further differentiate into trypomastigotes. This motile T. cruzi stage destroys the host cell plasma membrane [185] to initiate another infection cycle. The mechanism of host cell death remains controversial as infection leads to fibroblast death in a non-apoptotic way [186], whereas other cell types as cardiomyocytes and macrophages appear to die from apoptosis [187].
11 Extracellular Amastigote Entry to the Host Cells
Amastigotes which are prematurely released by ruptured host cells have the chance to return to the replication cycle when taken up by neighboring cells. In contrast to the active mechanisms used by trypomastigotes, extracellular amastigotes enter the cell by elicitation of actin-dependent mechanisms even in non-phagocytic cells [188]. Remarkably, the capacity of amastigotes to induce phagocytosis in non-phagocytic cells is parasite strain-dependent being extracellular amastigotes from the less infective strains mainly engulfed by macrophages [189, 190]. Once inside the host cells, amastigotes have the same ability than trypomastigotes to disrupt the PV to replicate freely in the cytosol and differentiated to infective trypomastigotes.
12 Concluding Remarks
In this chapter we intended to highlight the complexity of this parasite and its biological cycle. Different parasitic stages with differences in duplicative and/or infective capacity are accompanied by a significant intraspecific genotypic diversity. This parasite has evolved the capacity to invade a vast number of insect vector species and a wide range of mammalians in domestic and sylvatic cycles. This has made virtually impracticable all attempts of parasite eradication. A large number of molecules interact with the various cell types that can become host for the intracellular form of the parasite which can escape from immune surveillance and drugs in hidden niches. Such complexity has been demonstrated by the limited success in controlling this parasite. So far, much progress has been made, but we are still far from understanding how to successfully hamper with the progress of the infection and thus prevent Chagas disease.
References
Kollien AH, Schaub GA. The development of Trypanosoma cruzi in Triatominae. Parasitol Today. 2000;16(9):381–7.
Garcia ES, Genta FA, de Azambuja P, Schaub GA. Interactions between intestinal compounds of triatomines and T. cruzi. Trends Parasitol. 2010a;26(10):499–505.
Ferguson MA. The estructure, biosintesis and functions of glycosylphospatidyilinositol anchors, and the contributions of trypanosome research. J Cell Sci. 1999;112:2799–809.
Opperdoes RF, Michels PA. The glicosome of the kinetoplastida. Biochimie. 1993;75(3-4):231–4.
Docampo R, Moreno SN. Acidocalcisome: a novel Ca2+ storage compartment in trypanosomatids and apiocomplexan parasites. Parasitol Today. 1999;15(11):443–8.
Docampo R, de Souza W, Miranda K, Rohloff P, Moreno SN. Acidocalcisomes – conserved from bacteria to man. Nat Rev Microbiol. 2005;3(3):251–61.
Hoare C. The trypanosomes of mammals. Oxford, England: Blackwell Scientific Publications; 1972. p. 60. Chapter 5.
Chagas C. Nova tripanozomiase humana: estudos sobre a morfolojia e o ciclo evolutivo do Schizotrypanum cruzi n. gen., n. sp., ajente etiolojico de nova entidade morbida do homem. Mem Inst Oswaldo Cruz. 1909;1:159–218. Cited in Cruz RE, Macedo AM, Barnabe C, Freitas JM, Chiari E, Veloso CM, et al. Further genetic characterization of the two Trypanosoma cruzi Berenice strains (Be-62 and Be-78) isolated from the first human case of Chagas disease (Chagas, 1909) Acta Trop. 2006; 97: 239–46.
Bertelli M, Brener Z. Infection of Tissue Culture Cells with Bloodstream Trypomastigotes of Trypanosoma cruzi. J Parasitol. 1981;66(6):992–7.
Brener Z. The behavior of slender and stout forms of Trypanosoma cruzi in the blood-stream of normal and immune mice. Ann Trop Med Parasitol. 1969;63(2):215–20.
Schmatz DM, Boltz RC, Murray PK. Trypanosoma cruzi: separation of broad and slender trypomastigotes using a continuous hypaque gradient. Parasitology. 1983;87(Pt 2):219–27.
Borges MM, De Andrade SG, Pilatti CG, do Prado Júnior JC, Kloetzel JK. Macrophage activation and histopathological findings in Calomys callosus and Swiss mice infected with several strains of Trypanosoma cruzi. Mem Inst Oswaldo Cruz. 1992;87(4):493–502.
Risso MG, Garbarino GB, Mocetti E, Campetella O, Gonzalez Cappa SM, Buscaglia CA, et al. Differential expression of a virulence factor, the trans-sialidase, by the main Trypanosoma cruzi phylogenetic lineages. J Infect Dis. 2004;189(12):2250–9.
Botero LA, Mejía AM, Triana O. Caracterización biológica y genética de dos clones pertenecientes a los grupos I y II de Trypanosoma cruzi de Colombia. Biomedica. 2007;27(Suppl 1):64–74.
Melo RC, Brener Z. Tissue tropism of different Trypanosoma cruzi strains. J Parasitol. 1978;64(3):475–82.
Alba Soto CD, Mirkin GA, Solana ME, González Cappa SM. Trypanosoma cruzi infection modulates in vivo expression of major histocompatibility complex class II molecules on antigen-presenting cells and T-cell stimulatory activity of dendritic cells in a strain-dependent manner. Infect Immun. 2003;71(3):1194–9.
Mirkin GA, Celentano AM, Malchiodi EL, Jones M, González Cappa SM. Different Trypanosoma cruzi strains promote neuromyopathic damage mediated by distinct T lymphocyte subsets. Clin Exp Immunol. 1997;107(2):328–34.
Mirkin GA, Jones M, Sanz OP, Rey R, Sica RE, González Cappa SM. Experimental Chagas’ disease: electrophysiology and cell composition of the neuromyopathic inflammatory lesions in mice infected with a myotropic and a pantropic strain of Trypanosoma cruzi. Clin Immunol Immunopathol. 1994;73(1):69–79.
Andrade SG. The influence of the strain of Trypanosoma cruzi in placental infections in mice. Trans R Soc Trop Med Hyg. 1982;76(1):123–8.
Solana ME, Celentano AM, Tekiel V, Jones M, González Cappa SM. Trypanosoma cruzi: effect of parasite subpopulation on murine pregnancy outcome. J Parasitol. 2002;88(1):102–6.
Andrade SG. Caracterizaçao de cepas de Trypanosoma cruzi isoladas no Recôncavo Baiano. Rev Patol Trop. 1974;3:65–121.
Andrade SG. Influence of Trypanosoma cruzi strain on the pathogenesis of chronic myocardiopathy in mice. Mem Inst Oswaldo Cruz. 1990;85(1):17–27.
Miles MA, Toye PJ, Oswald SC, Godfrey DG. The identification by isoenzyme patterns of two distinct strain-groups of Trypanosoma cruzi, circulating independently in a rural area of Brazil. Trans R Soc Trop Med Hyg. 1977;71(3):217–25.
Morel C, Chiari E, Camargo EP, Mattei DM, Romanha AJ, Simpson L. Strains and clones of Trypanosoma cruzi can be characterized by pattern of restriction endonuclease products of kinetoplast DNA minicircles. Proc Natl Acad Sci U S A. 1980;77(11):6810–4.
Souto RP, Fernandes O, Macedo AM, Campbell DA, Zingales B. DNA markers define two major phylogenetic lineages of Trypanosoma cruzi. Mol Biochem Parasitol. 1996;83(2):141–52.
Zingales B, Andrade SG, Briones MR, Campbell DA, Chiari E, Fernandes O, et al. Second Satellite Meeting. A new consensus for Trypanosoma cruzi intraspecific nomenclature: second revision meeting recommends TcI to TcVI. Mem Inst Oswaldo Cruz. 2009;104(7):1051–4.
Tibayrenc M. Genetic epidemiology of parasitic protozoa and other infectious agents: the need for an integrated approach. Int J Parasitol. 1998;28(1):85–104.
Zingales B. Trypanosoma cruzi genetic diversity: something new for something known about Chagas disease manifestations, serodiagnosis and drug sensitivity. Acta Trop. 2018;184:38. https://doi.org/10.1016/j.actatropica.2017.09.017. Review. pii: S0001-706X(17)30426-6.
Zingales B, Miles MA, Campbell DA, Tibayrenc M, Macedo AM, Teixeira MM, et al. The revised Trypanosoma cruzi subspecific nomenclature: rationale, epidemiological relevance and research applications. Infect Genet Evol. 2012;12(2):240–53.
Hernández C, Cucunubá Z, Flórez C, Olivera M, Valencia C, Zambrano P, et al. Molecular diagnosis of Chagas disease in colombia: parasitic loads and discrete typing units in patients from acute and chronic phases. PLoS Negl Trop Dis. 2016;10(9):e0004997.
Ramírez JD, Guhl F, Rendón LM, Rosas F, Marin-Neto JA, Morillo CA. Chagas cardiomyopathy manifestations and Trypanosoma cruzi genotypes circulating in chronic Chagasic patients. PLoS Negl Trop Dis. 2010;4(11):e899.
Brenière SF, Waleckx E, Barnabé C. Over six thousand Trypanosoma cruzi strains classified into discrete typing units (DTUs): attempt at an inventory. PLoS Negl Trop Dis. 2016;10(8):e0004792.
Cardinal MV, Lauricella MA, Ceballos LA, Lanati L, Marcet PL, Levin MJ, et al. Molecular epidemiology of domestic and sylvatic Trypanosoma cruzi infection in rural northwestern Argentina. Int J Parasitol. 2008;38(13):1533–43.
Acosta N, López E, Lewis MD, Llewellyn MS, Gómez A, Román F, et al. Hosts and vectors of Trypanosoma cruzi discrete typing units in the Chagas disease endemic region of the Paraguayan Chaco. Parasitology. 2017;144(7):884–98.
Marcili A, Lima L, Valente VC, Valente SA, Batista JS, Junqueira AC, et al. Comparative phylogeography of Trypanosoma cruzi TCIIc: new hosts, association with terrestrial ecotopes, and spatial clustering. Infect Genet Evol. 2009;9(6):1265–74.
Monteiro WM, Magalhães LK, de Sá AR, Gomes ML, Toledo MJ, Borges L, et al. Trypanosoma cruzi IV causing outbreaks of acute Chagas disease and infections by different haplotypes in the Western Brazilian Amazonia. PLoS One. 2012;7(7):e41284. https://doi.org/10.1371/journal.pone.0041284.
Diosque P, Barnabé C, Padilla AM, Marco JD, Cardozo RM, Cimino RO, et al. Multilocus enzyme electrophoresis analysis of Trypanosoma cruzi isolates from a geographically restricted endemic area for Chagas’ disease in Argentina. Int J Parasitol. 2003;33(10):997–1003.
Fernández MP, Cecere MC, Lanati LA, Lauricella MA, Schijman AG, Gürtler RE, et al. Geographic variation of Trypanosoma cruzi discrete typing units from Triatoma infestans at different spatial scales. Acta Trop. 2014;140:10–8.
Maffey L, Cardinal MV, Ordóñez-Krasnowski PC, Lanati LA, Lauricella MA, Schijman AG, et al. Direct molecular identification of Trypanosoma cruzi discrete typing units in domestic and peridomestic Triatoma infestans and Triatoma sordida from the Argentine Chaco. Parasitology. 2012;139(12):1570–9.
Guhl F, Ramírez JD. Retrospective molecular integrated epidemiology of Chagas disease in Colombia. Infect Genet Evol. 2013;20:148–54.
Cura CI, Lucero RH, Bisio M, Oshiro E, Formichelli LB, Burgos JM, et al. Trypanosoma cruzi discrete typing units in Chagas disease patients from endemic and non-endemic regions of Argentina. Parasitology. 2012;139(4):516–21.
Duz AL, Vieira PM, Roatt BM, Aguiar-Soares RD, Cardoso JM, Oliveira FC, et al. The TcI and TcII Trypanosoma cruzi experimental infections induce distinct immunoresponses and cardiac fibrosis in dogs. Mem Inst Oswaldo Cruz. 2014;109(8):1005–13.
Marin-Neto JA, Cunha-Neto E, Maciel BC, Simões MV. Pathogenesis of chronic Chagas heart disease. Circulation. 2007;115:1109–23.
Burgos JM, Begher S, Silva HM, Bisio M, Duffy T, Levin MJ, et al. Molecular identification of Trypanosoma cruzi I tropism for central nervous system in Chagas reactivation due to AIDS. Am J Trop Med Hyg. 2008;78(2):294–7.
Burgos JM, Diez M, Vigliano C, Bisio M, Risso M, Duffy T, et al. Molecular identification of Trypanosoma cruzi discrete typing units in end-stage chronic Chagas heart disease and reactivation after heart transplantation. Clin Infect Dis. 2010;51(5):485–95.
Poveda C, Fresno M, Gironès N, Martins-Filho OA, Ramírez JD, Santi-Rocca J. Cytokine profiling in Chagas disease: towards understanding the association with infecting Trypanosoma cruzi discrete typing units (a BENEFIT TRIAL sub-study). PLoS One. 2014;9(3):e91154.
Mejía-Jaramillo AM, Fernández GJ, Montilla M, Nicholls RS, Triana-Chávez O. Trypanosoma cruzi strains resistant to benznidazole occurring in Colombia. Biomedica. 2012;32(2):196–205.
Rumi MM, Pérez Brandán C, Gil JF, D’Amato AM, Ragone PG, Lauthier JJ, et al. Benznidazole treatment in chronic children infected with Trypanosoma cruzi: serological and molecular follow-up of patients and identification of Discrete Typing Units. Acta Trop. 2013;128(1):130–6.
Zingales B, Araujo RG, Moreno M, Franco J, Aguiar PH, Nunes SL, et al. A novel ABCG-like transporter of Trypanosoma cruzi is involved in natural resistance to benznidazole. Mem Inst Oswaldo Cruz. 2015;110(3):433–44.
Andrade LO, Machado CR, Chiari E, Pena SD, Macedo AM. Differential tissue distribution of diverse clones of Trypanosoma cruzi in infected mice. Mol Biochem Parasitol. 1999;100(2):163–72.
Freitas JM, Andrade LO, Pires SF, Lima R, Chiari E, Santos RR, et al. The MHC Gene Region of Murine Hosts Influences the Differential Tissue Tropism of Infecting Trypanosoma cruzi Strains. PLoS One. 2009;4(4):e5113.
Alves MJ, Kawahara R, Viner R, Colli W, Mattos EC, Thaysen-Andersen M, et al. Comprehensive glycoprofiling of the epimastigote and trypomastigote stages of Trypanosoma cruzi. J Proteomics. 2017;151:182–92.
Queiroz RM, Ricart CA, Machado MO, Bastos IM, de Santana JM, de Sousa MV, et al. Insight into the exoproteome of the tissue-derived trypomastigote form of Trypanosoma cruzi. Front Chem. 2016;4:42.
Kahn SJ, Wleklinski M, Ezekowitz RA, Coder D, Aruffo A, Farr A. The major surface glycoprotein of Trypanosoma cruzi amastigotes are ligands of the human serum mannose-binding protein. Infect Immun. 1996;64(7):2649–56.
Santos MA, Garg N, Tarleton RL. The identification and molecular characterization of Trypanosoma cruzi amastigote surface protein-1, a member of the trans-sialidase gene super-family. Mol Biochem Parasitol. 1997;86(1):1–11.
Turner CW, Lima MF, Villalta F. Trypanosoma cruzi uses a 45-kDa mucin for adhesion to mammalian cells. Biochem Biophys Res Commun. 2002;290(1):29–34.
Alves MJM, Colli W. Adhesion to the host cell and intracellular survival. Critical review. IUBMB Life. 2007;59(4-5):274–9.
Magdesian MH, Giordano R, Ulrich H, Juliano MA, Juliano L, Schumacher RI, et al. Infection by Trypanosoma cruzi. Identification of a parasite ligand and its host cell receptor. J Biol Chem. 2001;276(22):19382–9.
Freire-de-Lima L, Fonseca LM, Oeltmann T, Mendonça-Previato L, Previato JO. The trans-sialidase, the major Trypanosoma cruzi virulence factor: three decades of studies. Glycobiology. 2015;25(11):1142–9.
Schenkman S, Jiang MS, Hart GW, Nussenzweig V. A novel cell surface trans-sialidase of Trypanosoma cruzi generates a stage-specific epitope required for invasion of mammalian cells. Cell. 1991a;65(7):1117–25.
Rubin-de-Celis SS, Uemura H, Yoshida N, Schenkman S. Expression of trypomastigote trans-sialidase in metacyclic forms of Trypanosoma cruzi increases parasite escape from its parasitophorous vacuole. Cell Microbiol. 2006;8(12):1888–90.
Nardy AF, Freire-de-Lima CG, Pérez AR, Morrot A. Role of Trypanosoma cruzi Trans-sialidase on the Escape from Host Immune Surveillance. Front Microbiol. 2016;7:348. https://doi.org/10.3389/fmicb.2016.00348. Mini Review.
Cánepa GE, Degese MS, Budu A, Garcia CR, Buscaglia CA. Involvement of TSSA (trypomastigote small surface antigen) in Trypanosoma cruzi invasion of mammalian cells. Biochem J. 2012;444(2):211–8.
García EA, Ziliani M, Agüero F, Bernabó G, Sánchez DO, Tekiel V. TcTASV: a novel protein family in Trypanosoma cruzi identified from a subtractive trypomastigote cDNA library. PLoS Negl Trop Dis. 2010b;4(10):e841. https://doi.org/10.1371/journal.pntd.0000841.
Bernabó G, Levy G, Ziliani M, Caeiro LD, Sánchez DO, Tekiel V. TcTASV-C, a protein family in Trypanosoma cruzi that is predominantly trypomastigote-stage specific and secreted to the medium. PLoS One. 2013;8(7):e71192.
Staquicini DI, Martins RM, Macedo S, Sasso GR, Atayde VD, Juliano MA, et al. Role of GP82 in the selective binding to gastric mucin during oral infection with Trypanosoma cruzi. PLoS Negl Trop Dis. 2010;4(3):e613.
Cortez C, Sobreira TJ, Maeda FY, Yoshida N. The gp82 surface molecule of Trypanosoma cruzi metacyclic forms. Subcell Biochem. 2014;74:137–50.
Correa PR, Cordero EM, Gentil LG, Bayer-Santos E, da Silveira JF. Genetic structure and expresión of the surface glycoprotein GP82, the main adhesin of Trypanosoma cruzi metacyclic trypomastigotes. Scientific World Journal. 2013;2013:156734.
Yoshida N. Molecular mechanisms of Trypanosoma cruzi infection by oral route. Mem Inst Oswaldo Cruz. 2009;104(Suppl 1):101–7.
Rodrigues JPF, Santana GHT, Juliano MA, Yoshida N. Inhibition of host cell lysosome spreading by Trypanosoma cruzi metacyclic stage-specific surface molecule gp90 downregulates parasite invasion. Infect Immun. 2017;85(9):e00302–17. https://doi.org/10.1128/IAI.00302-17.
Cazzulo JJ. Proteinases of Trypanosoma cruzi: patential targets for the chemotherapy of Changas desease. Curr Top Med Chem. 2002;2(11):1261–71.
San Francisco J, Barría I, Gutiérrez B, Neira I, Muñoz C, Sagua H, et al. Decreased cruzipain and gp85/trans-sialidase family protein expression contributes to loss of Trypanosoma cruzi trypomastigote virulence. Microbes Infect. 2017;19(1):55–61.
Stoka V, Nycander M, Lenarcic B, Labriola C, Cazzulo JJ, Björk I, et al. Inhibition of cruzipain, the major cysteine proteinase of the protozoan parasite, Trypanosoma cruzi, by proteinase inhibitors of the cystatin superfamily. FEBS Lett. 1995;370(1-2):101–4.
Pinto Dìas JC, Schofield CJ. History of Chagas Disease as a public health problem in Latin America. In: Teixeira A, Vinaud M, Castro AM, editors. Emerging Chagas Disease. Sharjah: Bentham; 2009. p. 1–9. Chapter 1.
Darwin C. Journal of researches into the geology and natural history of the various countries visited by H.M.S. Beagle, under the command of captain Fitzroy, R.N. from 1832 to 1836. London: Henry Colburn; 1839.
Zeledón R, Rabinovich JE. Chagas Disease: an ecological appraisal with special enphasis on its insect vector. Annu Rev Entomol. 1981;26:101–33.
Shelock IA. Vectores. In: Brener Z, Andrade ZA, Barral-Netto M, editors. Trypanosoma cruzi e doença de Chagas, vol. 3. 2nd ed. Río de Janeiro: Wanabara Koogan SA; 2000. p. 21–40.
Garcia ES, de Azambuja P. Fisiología de Triatomíneos: desenvolvimento, reproduçao e interaçao com Trypanosoma cruzi. In: Brener Z, Andrade Z, Barral-Netto M, editors. Trypanosoma cruzi e doença de Chagas, vol. 4. 2nd ed. Río de Janeiro: Wanabara Koogan SA; 2000. p. 41–7.
García DS, Dvorak JA. Growth and development of two Trypanosoma cruzi clones in the arthropod Dipetalogaster maximun. Am J Trop Med Hyg. 1982;31(2):259–62.
Lammel EL, de Isola EL, Korn C, Gonzalez Cappa SM. Trypanosoma cruzi: comparative Studies of infectivity of parasite ingested by Triatoma infestans and those present in their feces. Acta Trop. 1981;38(2):107–14.
Dvorak JA. A new in vitro approach to quantitation of Trypanosoma cruzi-vertebrate cell interaction. In: Proc. Symposium on New approaches in American Trypanosomiasis research. Washington, DC: PAHO/WHO; 1976. p. 109–20. Scientific Publication No 318.
de Souza W. O parasito e sua interaçao com os hospedeiros. In: Brener Z, Andrade Z, Barral-Netto M, editors. Trypanosoma cruzi e doença de Chagas, vol. 7. 2nd ed. Río de Janeiro: Wanabara Koogan SA; 2000. p. 88–126.
Enriquez GF, Bua J, Orozco MM, Wirth S, Schijman AG, Gürtler RE, et al. High levels of Trypanosoma cruzi DNA determined by qPCR and infectiousness to Triatoma infestans support dogs and cats are major sources of parasites for domestic transmission. Infect Genet Evol. 2014;25:36–43.
Gürtler RE, Cécere MC, Rubel DN, Petersen RM, Schweigmann NJ, Lauricella MA, et al. Chagas disease in north-west Argentina: infected dogs as a risk factor for the domestic transmission of Trypanosoma cruzi. Trans R Soc Trop Med Hyg. 1991;85(6):741–5.
Ramírez JD, Turriago B, Tapia-Calle G, Guhl F. Understanding the role of dogs (Canis lupus familiaris) in the transmission dynamics of Trypanosoma cruzi genotypes in Colombia. Vet Parasitol. 2013;196(1-2):216–9.
Moncayo A. Current epidemiological trends after the interruption of vectorial and transfusional transmission in the southern Cone Countries. Mem Inst Oswaldo Cruz. 2003;98(5):577–91.
Moncayo A, Silveira AC. Current epidemiological trends for Chagas disease in Latin America and future challenges in epidemiology, surveillance and health policy. Mem I Oswaldo Cruz. 2009;104(Suppl 1):17–309.
Reyes M, Torres A, Esteban L, Flórez M, Angulo VM. Riesgo de transmisión de la enfermedad de Chagas por intrusión de triatominos y mamíferos silvestres en Bucaramanga, Santander, Colombia. Biomédica. 2017;37:68–78.
Argibay HD, Orozco MM, Cardinal MV, Rinas MA, Arnaiz M, Mena Segura C, et al. First finding of Trypanosoma cruzi II in vampire bats from a district free o domestic vector-born transmssion in Northeastern Argentina. Parasitology. 2016;143(11):1358–68.
Gurgel-Gonçalves R, Cura C, Schijman AG, Cuba CA. Infestation of Mauritia flexuosa palms by triatomines (Hemiptera: Reduviidae), vectors of Trypanosoma cruzi and Trypanosoma rangeli in the Brazilian savanna. Acta Trop. 2012;121(2):105–11.
Miles MA, Arias JR, de Souza AA. Chagas’ disease in the Amazon basin: V. Periurban palms as habitats of Rhodnius robustus and Rhodnius pictipes-triatomine vectors of Chagas’ disease. Mem Inst Oswaldo Cruz. 1983;78(4):391–8.
Schmunis GA. Prevention of transfusional Trypanosoma cruzi infection in Latin America. Mem Inst Oswaldo Cruz. 1999;94(Suppl 1):93–101.
Yadon ZE, Schmunis GA. Congenital Chagas disease: estimating the potential risk in the United States. Am J Trop Med Hyg. 2009;81(6):927–33.
Celentano AM, González Cappa SM. Chagas’ disease and blood transfusion: trypanocidal activity of maprotiline hydrochloride and gentian violet. Medicina. 1988;48(3):265–8.
Hammond DJ, Croft SL, Hogg J, Gutteridge WE. A strategy for the prevention of the transmission of Chagas’ disease during blood transfusion. Acta Trop. 1986;43:367–78.
Carlier Y, Torrico F, Sosa-Estani S, Russomando G, Luquetti A, Freilij H, et al. Congenital Chagas disease: recommendations for diagnosis, treatment and control of newborns, siblings and pregnant women. PLoS Negl Trop Dis. 2011;5(10):e1250.
Juiz NA, Cayo NM, Burgos M, Salvo ME, Nasser JR, Búa J, et al. Human polymorphisms in placentally expressed genes and their association with susceptibility to congenital Trypanosoma cruzi infection. Infect Dis. 2016;213(8):1299–306.
Barcán L, Luna C, Clara L, Sinagra A, Valledor A, De Rissio AM, et al. Transmission of T. cruzi infection via liver transplantation to a nonreactive recipient for Chagas’ disease. Liver Transpl. 2005;11(9):1112–6.
Bocchi EA, Fiorelli A. The paradox of survival results after heart transplantation for cardiomyopathy caused by Trypanosoma cruzi. First Guidelines Group for Heart Transplantation of the Brazilian Society of Cardiology. Ann Thorac Surg. 2001;71(6):1833–8.
Casadei D, Chagas’ Disease Argentine Collaborative Transplant Consortium. Chagas’ disease and solid organ transplantation. Transplant Proc. 2010;42(9):3354–9.
Kransdorf EP, Zakowski PC, Kobashigawa JA. Chagas disease in solid organ and heart transplantation. Curr Opin Infect Dis. 2014;27(5):418–24.
Kleffmann T, Schmidt J, Schaub GA. Attachment to Trypanosoma cruzi epimastigotes to hydrophobic substrates and use of this property to separate stages and promote metacyclogenesis. J Eukaryot Microbiol. 1998;45(5):548–55.
Guarneri AA, Lorenzo MG. Triatomine physiology in the context of trypanosome infection. J Insect Physiol. 2017;97:66–76.
de Isola EL, Lammel EM, Katzin VJ, GonzalezCappa SM. Influence of organ extracts of Triatoma infestans on differentiation of Trypanosoma cruzi. J Parasitol. 1981;67(1):53–8.
Isola EL, Lammel EM, Giovanniello O, Katzin AM, González Cappa SM. Trypanosoma cruzi morphogenesis: preliminary purification of an active fraction from hemolymph and intestinal homogenate of Triatoma infestans. J Parasitol. 1986b;72(3):467–9.
Lammel EM, Barbieri MA, Wilkowsky SE, Bertini F, Isola EL. Trypanosoma cruzi: involvemente of intracellular calciun in multiplication and differentiation. Exp Parasitol. 1996;83(2):240–9.
Isola EL, Lammel EM, González Cappa SM. Trypanosoma cruzi diferenciation after interaction of epimastigote and Triatoma infestans intestine homogenate. Exp Parasitol. 1986a;62(3):329–35.
Fraidenraich D, Peña C, Isola EL, Lammel EM, Coso O, Añel AD, et al. Stimulation of Trypanosoma cruzi adenyl cyclase by an alpha D-globin fragment from Triatoma hindgat: effect on differentiation of epimastigote to trypomastigote forms. Proc Natl Acad Sci U S A. 1993;90(21):10140–4.
Belauzaran ML, Lammel EM, Giménez G, Wainszelbaum MJ, de Isola EL. Envolvement of protein kinase C isoenzymes in Trypanosoma cruzi metaciclogenesis induced by oleica cid. Parasitol Res. 2009;105(1):47–55.
Wainszelbaum MJ, Belaunzarán ML, Lammel EM, Florin-Christensen M, Florin-Christensen J, Isola EL. Free fatty acids induce cell differenciatin to infective forms in Trypanosoma cruzi. Biochem J. 2003;375(3):705–12.
Isola EL, Lammel EM, González Cappa SM. Trypanosoma cruzi: differentiation to metacyclic trypomastigotes in the presence of ADP-ribosyltransferase inhibitors. Exp Parasitol. 1987;64(3):424–9.
Contreras VT, Araujo-Jorge TC, Bonaldo MC, Thomaz N, Barbosa HS, Meirelles Mde N, et al. Biological aspects of the D28c clone of Trypanosoma cruzi after metacyclogenesis in chemical defined media. Mem Inst Oswaldo Cruz. 1988;83(1):123–33.
Contreras VT, Salles JM, Thomas N, Morel CM, Goldenberg S. In vitro differentiation of Trypanosoma cruzi under chemically defined conditions. Mol Biochem Parasitol. 1985;16(3):315–27.
Hamedi A, Botelho L, Britto C, Fragoso SP, Umaki AC, Goldenberg S, et al. In vitro metacyclogenesis of Trypanosoma cruzi induced by starvation correlates with a transient adenilyl cyclase stimulation as well as with a constitutive upregulation of adenylyn cyclase expression. Mol Biochem Parasitol. 2015;200(1-2):9–18.
Dworak ES, Araújo SM, Gomes M, Massago M, Ferreira ÉC, Toledo MJO. Sympatry influence in the interaction of Trypanosoma cruzi with triatomine. Rev Soc Bras Med Trop. 2017;50(5):629–37.
Lammel EM, Müller LA, Isola EL, González Cappa SM. Effect of vector on infectivity of Trypanosoma cruzi. Acta Trop. 1985;42(2):149–55.
Szumlewicz AP, Muller CA. Studies in search of a suitable experimental insect model for xenodiagnosis of hosts with Chagas’ disease. 2 Attempts to upgrade the reliability and the efficacy of xenodiagnosis in chronic Chagas’ disease. Mem Inst Oswaldo Cruz. 1987;82(2):259–72.
Alves MJ, Colli W. Role of the gp85/trans-sialidase superfamily of glycoproteins in the interaction of Trypanosoma cruzi with host structures. Subcell Biochem. 2008;47:58–69.
Maeda FY, Cortez C, Izidoro MA, Juliano L, Yoshida N. Fibronectin-degrading activity of Trypanosoma cruzi cysteine proteinase plays a role in host cell invasion. Infect Immun. 2014;82(12):5166–74.
Nde PN, Simmons KJ, Kleshchenko YY, Pratap S, Lima MF, Villalta F. Silencing of the laminin gamma-1 gene blocks Trypanosoma cruzi infection. Infect Immun. 2006;74(3):1643–8.
Coimbra VC, Yamamoto D, Khusal KG, Atayde VD, Fernandes MC, Mortara RA, et al. Enucleated L929 cells support invasion, differentiation, and multiplication of Trypanosoma cruzi parasites. Infect Immun. 2007;75(8):3700–6.
Epting CL, Coates BM, Engman DM. Molecular mechanisms of host cell invasion by Trypanosoma cruzi. Exp Parasitol. 2010;126(3):283–91.
Burleigh BA, Andrews NW. The mechanisms of Trypanosoma cruzi invasion of mammalian cells. Annu Rev Microbiol. 1995;49:175–200.
Milei J, Sánchez J, Storino R, Yu ZX, Denduchis B, Ferrans VJ. Antibodies to laminin and immunohistochemical localization of laminin in chronic chagasic cardiomyopathy: a review. Mol Cell Biochem. 1993;129(2):161–70.
Ferreira V, Molina MC, Valck C, Rojas A, Aguilar L, Ramírez G, et al. Role of calreticulin from parasites in its interaction with vertebrate hosts. Mol Immunol. 2004;40(17):1279–91.
Johnson CA, Kleshchenko YY, Ikejiani AO, Udoko AN, Cardenas TC, Pratap S, et al. Thrombospondin-1 interacts with Trypanosoma cruzi surface calreticulin to enhance cellular infection. PLoS One. 2012;7(7):e40614. https://doi.org/10.1371/journal.pone.0040614.
Kleshchenko YY, Moody TN, Furtak VA, Ochieng J, Lima MF, Villalta F. Human galectin-3 promotes Trypanosoma cruzi adhesion to human coronary artery smooth muscle cells. Infect Immun. 2004;72(11):6717–21.
Moody TN, Ochieng J, Villalta F. Novel mechanism that Trypanosoma cruzi uses to adhere to the extracellular matrix mediated by human galectin-3. FEBS Lett. 2000;470(3):305–8.
Sato S, Hughes RC. Control of Mac-2 surface expression on murine macrophage cell lines. Eur J Immunol. 1994;24(1):216–21.
Grellier P, Vendeville S, Joyeau R, Bastos IM, Drobecq H, Frappier F, et al. Trypanosoma cruzi prolyl oligopeptidase Tc80 is involved in nonphagocytic mammalian cell invasion by trypomastigotes. J Biol Chem. 2001;276(50):47078–86.
Teixeira AA, de Vasconcelos Vde C, Colli W, Alves MJ, Giordano RJ. Trypanosoma cruzi binds to cytokeratin through conserved peptide motifs found in the laminin-G-like domain of the gp85/trans-sialidase proteins. PLoS Negl Trop Dis. 2015;9(9):e0004099.
Weston D, Patel B, Van Voorhis WC. Virulence in Trypanosoma cruzi infection correlates with the expression of a distinct family of sialidase superfamily genes. Mol Biochem Parasitol. 1999;98(1):105–16.
Ruiz RC, Favoreto S, Dorta ML, Oshiro MEM, Ferreira AT, Manque PM, et al. Infectivity of Trypanosoma cruzi strains is associated with differential expresión of surface glycoproteins with differential CA2 signaling activity. Biochem J. 1998;330:505–11.
Alves MJ, Abuin G, Kuwajima VY, Colli W. Partial inhibition of trypomastigote entry into cultured mammalian cells by monoclonal antibodies against a surface glycoprotein of Trypanosoma cruzi. Mol Biochem Parasitol. 1986;21(1):75–82.
Freitas LM, dos Santos SL, Rodrigues-Luiz GF, Mendes TAO, Rodrigues TS, Gazzinelli RT, et al. Genomic analices, gene expresison and antigenic profile of the trans-sialidase superfamily of Trypanosoma cruzi reveal an undetected level of complexity. PLoS One. 2011;6:e25914.
Mattos EC, Tonelli RR, Colli W, Alves MJ. The Gp85 surface glycoproteins from Trypanosoma cruzi. Subcell Biochem. 2014;74:151–80.
Tonelli RR, Giordano RJ, Barbu EM, Torrecilhas AC, Kobayashi GS, Langley RR, et al. Role of the gp85/trans-sialidases in Trypanosoma cruzi tissue tropism: preferential binding of a conserved peptide motif to the vasculature in vivo. PLoS Negl Trop Dis. 2010;4(11):e864.
Zingales B, Carniol C, de Lederkremer RM, Colli W. Direct sialic acid transfer from a protein donor to glycolipids of trypomastigote forms of Trypanosoma cruzi. Mol Biochem Parasitol. 1987;26(1-2):135–44.
Campetella O, Sánchez D, Cazzulo JJ, Frasch AC. A superfamily of Trypanosoma cruzi surface antigens. Parasitol Today. 1992;8(11):378–81.
Frasch AC. Trans-sialidase, SAPA amino acid repeats and the relationship between Trypanosoma cruzi and the mammalian host. Parasitology. 1994;108(Suppl):S37–44.
Affranchino JL, Ibañez CF, Luquetti AO, Rassi A, Reyes MB, Macina RA, et al. Identification of a Trypanosoma cruzi antigen that is shed during the acute phase of Chagas’ disease. Mol Biochem Parasitol. 1989;34(3):221–8.
Tambourgi DV, Kipnis TL, da Silva WD, Joiner KA, Sher A, Heath S, et al. A partial cDNA clone of trypomastigote decay-accelerating factor (T-DAF), a developmentally regulated complement inhibitor of Trypanosoma cruzi, has genetic and functional similarities to the human complement inhibitor DAF. Infect Immun. 1993;61(9):3656–63.
Hall BF, Webster P, Ma AK, Joiner KA, Andrews NW. Desialylation of lysosomal membrane glycoproteins by Trypanosoma cruzi: a role for the surface neuraminidase in facilitating parasite entry into the host cell cytoplasm. J Exp Med. 1992;176(2):313–25.
Risso MG, Pitcovsky TA, Caccuri RL, Campetella O, Leguizamón MS. Immune system pathogenesis is prevented by the neutralization of the systemic trans-sialidase from Trypanosoma cruzi during severe infections. Parasitology. 2007;134(Pt 4):503–10.
Vercelli CA, Hidalgo AM, Hyon SH, Argibay PF. Trypanosoma cruzi trans-sialidase inhibits human lymphocyte proliferation by nonapoptotic mechanisms: implications in pathogenesis and transplant immunology. Transplant Proc. 2005;37(10):4594–7.
Ruiz Díaz P, Mucci J, Meira MA, Bogliotti Y, Musikant D, Leguizamón MS, et al. Trypanosoma cruzi trans-sialidase prevents elicitation of Th1 cell response via interleukin 10 and downregulates Th1 effector cells. Infect Immun. 2015;83(5):2099–108.
Barrias ES, de Carvalho TM, De Souza W. Trypanosoma cruzi: entry into mammalian host cells and parasitophorous vacuole formation. Front Immunol. 2013;4:186.
Caradonna KL, Burleigh BA. Mechanisms of host cell invasion by Trypanosoma cruzi. Review. Adv Parasitol. 2011;76:33–61.
Schenkman S, Robbins ES, Nussenzweig V. Attachment of Trypanosoma cruzi to mammalian cells requires parasite energy, and invasion can be independent of the target cell cytoskeleton. Infect Immun. 1991b;59(2):645–54.
Andrews NW. Lysosome recruitment during host cell invasion by Trypanosoma cruzi. Trends Cell Biol. 1995;5(3):133–7.
Tardieux I, Webster P, Ravesloot J, Boron W, Lunn JA, Heuser JE, et al. Lysosome recruitment and fusion are early events required for trypanosome invasion of mammalian cells. Cell. 1992;71(7):1117–30.
Fernandes MC, Cortez M, Flannery AR, Tam C, Mortara RA, Andrews NW. Trypanosoma cruzi subverts the sphingomyelinase-mediated plasma membrane repair pathway for cell invasion. J Exp Med. 2011;208(5):909–21.
Rodríguez A, Samoff E, Rioult MG, Chung A, Andrews NW. Host cell invasion by trypanosomes requires lysosomes and microtubule/kinesin-mediated transport. J Cell Biol. 1996;134(2):349–62.
Caler EV, Chakrabarti S, Fowler KT, Rao S, Andrews NW. The exocytosis-regulatory protein synaptotagmin VII mediates cell invasion by Trypanosoma cruzi. J Exp Med. 2001;193(9):1097–104.
Chakrabarti S, Kobayashi KS, Flavell RA, Marks CB, Miyake K, Liston DR, et al. Impaired membrane resealing and autoimmune myositis in synaptotagmin VII-deficient mice. J Cell Biol. 2003;162(4):543–9.
Rodríguez A, Rioult MG, Ora A, Andrews NW. A trypanosome-soluble factor induces IP3 formation, intracellular Ca2+ mobilization and microfilament rearrangement in host cells. J Cell Biol. 1995;129(5):1263–73.
Tardieux I, Nathanson MH, Andrews NW. Role in host cell invasion of Trypanosoma cruzi-induced cytosolic-free Ca2+ transients. J Exp Med. 1994;179(3):1017–22.
Fernandes MC, Cortez M, Geraldo Yoneyama KA, Straus AH, Yoshida N, Mortara RA. Novel strategy in Trypanosoma cruzi cell invasion: implication of cholesterol and host cell microdomains. Int J Parasitol. 2007;37(13):1431–41.
Andrews NW. Lysosomes and the plasma membrane: trypanosomes reveal a secret relationship. Review. J Cell Biol. 2002;158(3):389–94.
Reddy A, Caler EV, Andrews NW. Plasma membrane repair is mediated by Ca(2+)-regulated exocytosis of lysosomes. Cell. 2001;106(2):157–69.
McNeil PL, Steinhardt RA. Plasma membrane disruption: repair, prevention, adaptation. Review. Annu Rev Cell Dev Biol. 2003;19:697–731.
Woolsey AM, Burleigh BA. Host cell actin polymerization is required for cellular retention of Trypanosoma cruzi and early association with endosomal/lysosomal compartments. Cell Microbiol. 2004;6(9):829–38.
Woolsey AM, Sunwoo L, Petersen CA, Brachmann SM, Cantley LC, Burleigh BA. Novel PI 3-kinase-dependent mechanisms of trypanosome invasion and vacuole maturation. J Cell Sci. 2003;116(17):3611–22.
Wilkowsky SE, Barbieri MA, Stahl PD, Isola EL. Regulation of Trypanosoma cruzi invasion of nonphagocytic cells by the endocytically active GTPases dynamin, Rab5, and Rab7. Biochem Biophys Res Commun. 2002;291(3):516–21.
Romano PS, Arboit MA, Vázquez CL, Colombo MI. The autophagic pathway is a key component in the lysosomal dependent entry of Trypanosoma cruzi into the host cell. Autophagy. 2009;5(1):6–18.
Martins RM, Alves RM, Macedo S, Yoshida N. Starvation and rapamycin differentially regulate host cell lysosome exocytosis and invasion by Trypanosoma cruzi metacyclic forms. Cell Microbiol. 2011;13(7):943–54.
Mizushima N, Yamamoto A, Matsui M, Yoshimori T, Ohsumi Y. In vivo analysis of autophagy in response to nutrient starvation using transgenic mice expressing a fluorescent autophagosome marker. Mol Biol Cell. 2004;15(3):1101–11.
Romano PS, Cueto JA, Casassa AF, Vanrell MC, Gottlieb RA, Colombo MI. Molecular and cellular mechanisms involved in the Trypanosoma cruzi/host cell interplay. IUBMB Life. 2012;64(5):387–96.
Wilkowsky SE, Barbieri MA, Stahl P, Isola EL. Trypanosoma cruzi: phosphatidylinositol 3-kinase and protein kinase B activation is associated with parasite invasion. Exp Cell Res. 2001;264(2):211–8.
Chuenkova MV, Furnari FB, Cavenee WK, Pereira MA. Trypanosoma cruzi trans-sialidase: a potent and specific survival factor for human Schwann cells by means of phosphatidylinositol 3-kinase/Akt signaling. Proc Natl Acad Sci U S A. 2001;98(17):9936–41.
Andrade LO, Andrews NW. Lysosomal fusion is essential for the retention of Trypanosoma cruzi inside host cells. J Exp Med. 2004;200(9):1135–43.
Kierszenbaum F, Knecht E, Budzko DB, Pizzimenti MC. Phagocytosis: a defense mechanism against infection with Trypanosoma cruzi. J Immunol. 1974;112(5):1839–44.
Muñoz-Fernández MA, Fernández MA, Fresno M. Activation of human macrophages for the killing of intracellular Trypanosoma cruzi by TNF-alpha and IFN-gamma through a nitric oxide-dependent mechanism. Immunol Lett. 1992;33(1):35–40.
Piacenza L, Alvarez MN, Peluffo G, Radi R. Fighting the oxidative assault: the Trypanosoma cruzi journey to infection. Curr Opin Microbiol. 2009;12(4):415–21. https://doi.org/10.1016/j.mib.2009.06.011.
Celentano AM, González Cappa SM. In vivo macrophage function in experimental infection with Trypanosoma cruzi subpopulations. Acta Trop. 1993;55(3):171–80.
Zago MP, Hosakote YM, Koo SJ, Dhiman M, Piñeyro MD, Parodi-Talice A, et al. TcI Isolates of Trypanosoma cruzi Exploit the Antioxidant Network for Enhanced Intracellular Survival in Macrophages and Virulence in Mice. Infect Immun. 2016;84(6):1842–56.
Kipnis TL, Calich VL, da Silva WD. Active entry of bloodstream forms of Trypanosoma cruzi into macrophages. Parasitology. 1979;78(1):89–98.
Andrews NW. From lysosomes into the cytosol: the intracellular pathway of Trypanosoma cruzi. Braz J Med Biol Res. 1994;27(2):471–5.
Ley V, Robbins ES, Nussenzweig V, Andrews NW. The exit of Trypanosoma cruzi from the phagosome is inhibited by raising the pH of acidic compartments. J Exp Med. 1990;171(2):401–13.
Andrews NW, Abrams CK, Slatin SL, Griffiths G. A T. cruzi-secreted protein immunologically related to the complement component C9: evidence for membrane pore-forming activity at low pH. Cell. 1990;61(7):1277–87.
Manning-Cela R, Cortés A, González-Rey E, Van Voorhis WC, Swindle J, González A. LYT1 protein is required for efficient in vitro infection by Trypanosoma cruzi. Infect Immun. 2001;69(6):3916–23.
Tomlinson S, Vandekerckhove F, Frevert U, Nussenzweig V. The induction of Trypanosoma cruzi trypomastigote to amastigote transformation by low pH. Parasitology. 1995;110(Pt 5):547–54.
Tonelli RR, Silber AM, Almeida-de-Faria M, Hirata IY, Colli W, Alves MJ. L-proline is essential for the intracellular differentiation of Trypanosoma cruzi. Cell Microbiol. 2004;6(8):733–41.
Grellier P, Blum J, Santana J, Bylèn E, Mouray E, Sinou V, et al. Involvement of calyculin A-sensitive phosphatase(s) in the differentiation of Trypanosoma cruzi trypomastigotes to amastigotes. Mol Biochem Parasitol. 1999;98(2):239–52.
Costales J, Rowland EC. A role for protease activity and host-cell permeability during the process of Trypanosoma cruzi egress from infected cells. J Parasitol. 2007;93(6):1350–9.
Clark RK, Kuhn RE. Trypanosoma cruzi does not induce apoptosis in murine fibroblasts. Parasitology. 1999;118(2):167–75.
de Souza EM, Araújo-Jorge TC, Bailly C, Lansiaux A, Batista MM, Oliveira GM, et al. Host and parasite apoptosis following Trypanosoma cruzi infection in in vitro and in vivo models. Cell Tissue Res. 2003;314(2):223–35.
Mortara RA. Trypanosoma cruzi: amastigotes and trypomastigotes interact with different structures on the surface of HeLa cells. Exp Parasitol. 1991;73(1):1–14.
Ley V, Andrews NW, Robbins ES, Nussenzweig V. Amastigotes of Trypanosoma cruzi sustain an infective cycle in mammalian cells. J Exp Med. 1988;168(2):649–59.
Mortara RA, Andreoli WK, Taniwaki NN, Fernandes AB, Silva CV, Fernandes MC, et al. Mammalian cell invasion and intracellular trafficking by Trypanosoma cruzi infective forms. An Acad Bras Cienc. 2005;77(1):77–94.
Perlowagora-Szumlewics A, Moreira CJ. In vivo differentiation of Trypanosoma cruzi--1. Experimental evidence of the influence of vector species on metacyclogenesis. Mem Inst Oswaldo Cruz. 1994;89(4):603–18.
Previato JO, Andrade AF, Pessolani MC, Mendonça-Previato L. Incorporation of sialic acid into Trypanosoma cruzi macromolecules. A proposal for a new metabolic route. Mol Biochem Parasitol. 1985;16(1):85–96.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Alba Soto, C.D., González Cappa, S.M. (2019). Trypanosoma cruzi Journey from the Insect Vector to the Host Cell. In: Altcheh, J., Freilij, H. (eds) Chagas Disease. Birkhäuser Advances in Infectious Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-00054-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-00054-7_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-00053-0
Online ISBN: 978-3-030-00054-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)