Abstract
Cardiac tumors are rare entities [1, 2]. Because of the rarity, it is difficult to investigate systematically large series of cardiac tumors using ancillary or biomolecular and experimental methods of investigation. As a consequence, scarce innovative information is available concerning the histogenesis of the majority of cardiac tumors. Myxomas are the most frequent neoplasms, accounting for 50 % of all tumors (Reynen K. N Engl J Med 333:1610–17, 1995; Burke AP, Virmani R. Atlas of tumor pathology, 3rd ed. Armed Forced Institute of Pathology: Washington, DC. p. 121–46, 1996), and the most investigated primary cardiac tumor. Nevertheless, the origin of myxoma remains uncertain. In this chapter, we summarize the most recent novelties in the biomolecular and immunohistochemical investigation of primary cardiac tumors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
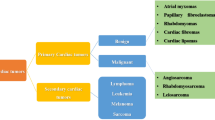
Cardiac tumors are rare entities [1, 2]. Because of the rarity, it is difficult to investigate systematically large series of cardiac tumors using ancillary or biomolecular and experimental methods of investigation. As a consequence, scarce innovative information is available concerning the histogenesis of the majority of cardiac tumors. Myxomas are the most frequent neoplasms, accounting for 50% of all tumors [1, 2], and the most investigated primary cardiac tumor. Nevertheless, the origin of myxoma remains uncertain. In this chapter, we summarize the most recent novelties in the biomolecular, immunohistochemical and genetic investigation of primary cardiac tumors.
Cardiac Myxoma
Novelties in Immunohistochemical Findings
Myxoma is the most frequent primary tumor of the heart [1]. Its name derives from myxoid appearance of a mucopolysaccharide-rich extracellular matrix [2]. Myxoma usually arises from the inter-atrial septum, more frequently on the left side [1, 2]. The histogenesis of cardiac myxoma was for a long time considered uncertain, because of the nature of the morphological and immunohistochemical findings obtained after the characterization of this tumor. In fact, a variable expression of proteins typical of different adult cell phenotypes has been reported, even in the same tumor, suggesting an epithelial, endothelial, myogenic, myofibroblastic, or neural origin, respectively [3–10]. In adult myocardium, two sarcomeric actins, α-cardiac and α-skeletal actin, are co-expressed and represent the predominant isoforms [11]; in addition, α-smooth muscle actin (α-actin) is transiently observed in cardiomyocytes during the early stage of fetal cardiac development [12]. In Table 13.1 are reported the comparisons between microscopic and immunohistochemical findings (as percentages of positive cardiac myxoma cells) in a series of thirty tumors [13]. Although cardiac myxomas variably expressed vimentin, Notch1, CALB2, and smooth muscle antigens such as α-actin and caldesmon were the most frequently observed with a diffuse cytoplasmic immunoreactivity, followed by CD34. It is worth noting that α-cardiac actin was observed in a few cases and α-skeletal actin was always absent. Single or multinucleated cells were CD34 positive mainly in the superficial areas of tumors, whereas interstitial or perivascular cells were more α-smooth muscle actin positive. The immunophenotype of vascular structures of cardiac myxoma has been also investigated [13]. As concerning the complex vascular structures, enlarged ring structures are in the majority of cases CD34 positive and only focally α-actin positive. Lacunae, other complex vascular-like structures of cardiac myxoma, are characterized by wide vascular-like spaces covered by single or multilayered CD34 positive and α-actin negative cells, whereas parietal cells are positive for the myocytic marker α-actin, suggesting an endothelial and pericyte-like differentiation, respectively (Fig. 13.1). Rarely, parietal cells of ring structures were also focally α-cardiac actin positive. Thick arterial-like structures of cardiac myxoma were of two different types: the first, larger and with a thick wall, covered by CD34 positive endothelial-like cells with α-actin positive parietal cells, were observed throughout the entire myxoma tissue; the second type, smaller and mainly at the parietal edge, resembled morphologically and immunohistochemically the normal atrial vasculature. Finally, confocal microscopy well documents the presence of CD34 and α-actin positive myxoma cells; rare myxoma cells, including multinucleated cells, focally co-expressed both proteins (Fig. 13.2), suggesting a precursor or an intermediate cell phenotype [13].
Immunohistochemical characterization of vascular complex structures of cardiac myxoma. (a, b) Complex structures from wide vascular-like spaces with a thin wall constituted by one or more layers of flattened (a) CD34 positive and (b) focally α-smooth muscle actin positive cells. (c, d) Elongated multilayered structures, with (c) abundant CD34 positive and (d) rare parietal α-smooth muscle actin positive cells. Diaminobenzidine as chromogen; original magnification, ×125
Co-expression of endothelial and myogenic markers in cardiac myxoma. Immunofluorescent staining of α-smooth muscle actin (left, red) and CD34 (middle, green) of cardiac myxoma cell, sometimes multinucleated; merged image (right) shows co-expression of both endothelial and myocytic antigens. Original magnification, ×400
Biomolecular Analysis of Cardiac Myxomas
The availability of methods of investigation of gene expression, in particular reverse transcriptase-polymerase chain reaction (RT-PCR) and Real Time-PCR, may help to better characterize phenotypic features of cardiac tumor cells. Unfortunately, the optimal results are obtained after mRNA extraction from fresh tissue and, for their intrinsic rarity, a systematized tissue banking of cardiac tumor tissues is quite difficult. When possible, gene transcripts recapitulating specific phenotypes can be also useful to trace differentiation of tumor cells. In cardiac myxoma, PCR analysis performed on RNA extracted from frozen tissue from eight consecutive cases of cardiac myxoma [13] revealed CALB2 (calretinin) and Sox9 transcripts in all cases, Notch1 and NFATcI transcripts in 87.5 and 37.5% of cases, respectively, whereas all cases were negative for ErbB3 and Wilms’ tumor transcription factor (Fig. 13.3).
Primitive mesenchymal markers gene expression in cardiac myxoma. Agarose gel after ethidium bromide staining documents RT-PCR analysis of transcripts from eight consecutive cardiac myxomas mRNA showing variable CD34, MMP-2, TIMP-1, Sox9, CALB2, and Notch1 transcripts, while ErbB3 and WT1 transcripts are absent; β2microglobulin is used as housekeeping gene. Modified from Orlandi et al. [13]
Myxoma Cell Phenotype and Clinical Behavior of Cardiac Myxomas
Cardiac myxomas are benign tumors which are unable to infiltrate the myocardium or give rise to metastases [1, 2]. Nevertheless, they are considered “clinically malignant” tumors because of their susceptibility to embolize to distant organs [1, 2, 14]. As a matter of fact, clinical signs of tumor embolism represent the primary manifestation in 30–50% of cases. Since most myxomas are left atrium-located, emboli prevalently involve peripheral districts, in particular cerebral arteries, including retinal artery [1, 2, 14]. Echocardiographic polypoid and irregular macroscopic aspects, changes in the composition of the myxomatous matrix, as well as the autocrine production of IL-6 have been considered [14–17]. Another hypothesis considers apoptosis as relevant for myxoma tissue remodeling and, consequently, for the clinical behavior of these cardiac tumors [18]. Successively, other researchers identified at both mRNA and protein levels the extrinsic Fas/FasL-dependent final common apoptotic pathway of myxoma cells [19]. More recently, a series of 27 left atrial myxomas, 10 of them with clinical signs of peripheral embolism, have been investigated by several methods, documenting in embolic myxomas higher expression and activity of matrix metalloproteinases (MMPs), in particular MT1-MMP, pro-MMP-2, and pro-MMP-9, whereas pro-MMP-1, MMP-3, and TIMP-1 levels were similar to those of non-embolic tumors [20]. MMPs are a large family of zinc-dependent proteolytic enzymes that degrade the extracellular matrix in both normal and pathological processes [21–23]. MMPs are released into the extracellular milieu in a proenzyme state or membrane-bound enzymes that undergo intracellular activation and are proteolitically active when inserted into the cell membrane. Increased expression of MMPs associated more frequently with the irregular or polypoid aspect of cardiac myxomas [20]. Consequently, it is possible to hypothesize that increased MMP expression and activity can induce a remodeling of tumor extracellular matrix, with a consequent increase of friability and, consequently, of the risk of embolism of cardiac myxoma. Nevertheless, in some cases of non-embolic irregular myxomas, MMP expression did not significantly differ from non-embolic smooth tumors, suggesting that embolism is not the natural consequence of the irregular macroscopic appearance. Moreover, these studies in vivo do not clarify if increased MMP activity is an intrinsic feature of myxoma cells or, alternatively, it is related to an increased susceptibility to locally delivered cytokines [17]. Nevertheless, embolic myxoma cells retain higher MT1-MMP and pro-MMP-2 levels in basal condition and after stimulation with IL-1β and IL-6 in vitro [20].
The Origin of Cardiac Myxoma: An Update
The heterogeneous phenotype of myxoma cells gave origin to several interpretations concerning the histogenesis of cardiac myxoma. The presence of endothelial marker and cytoplasmic neuropeptides such as protein gene product 9.5, S100 protein and neuron-specific enolase in more than half of a series of cardiac myxomas supports the hypothesis that myxoma cells originate from pluripotent mesenchymal cells capable of neural and endothelial differentiation [9]. Another explanation for heterogeneous differentiation in cardiac myxoma is its origin from a pluripotential cell or from a subendothelial vasiform reserve cell, on the basis of the expression of transcripts characteristic of cardiac cushion development and/or primitive cardiac mesenchymal differentiation [3, 4, 24]. Some morphologic homologies between cardiac myxoma cells and those of embryonic cardiac cushion cells support this hypothesis. A cardiomyogenic derivation of cardiac myxomas was based on the finding of transcripts for Nkx2.5/Csx, typical of the cardiac homeobox gene, recapitulating a primitive cardiomyocytic phenotype and supporting an embryonic cardiomyocytic progenitor cell as precursor [25]. Although Nkx2.5/Csx encodes for a gene required for specification of cardiac precursor cells, its expression is maintained throughout development [25]. Moreover, Nkx2.5/Csx is documented during development of other tissues, including skeletal myoblasts and promotes neuronal differentiation in vitro [26, 27]. This explains the previously reported expression of neural markers [9] as a demonstration of a possible neurogenic origin of cardiac myxoma cells. Investigation of actin isoform expression can be useful to trace the origin of cardiac myxoma cells. In particular, the diffuse presence of α-smooth muscle actin, the paucity of α-cardiac actin, and the absence of α-skeletal actin isoform expression have been described in cardiac myxomas [20]; α-smooth muscle actin is reported to be transiently expressed in human cardiomyocytes during early stages of fetal development [28]. This finding supports that myxoma cells are phenotypically reconducible to a more primitive cardiac progenitor or primordial cardiac stem cell. In fact, in the 20-week-old fetal heart, a time when septation is complete and the heart exhibits all the morphological characteristics of the adult heart, α-cardiac actin is the major isoform and uniformly expressed [12]. The mesenchymal origin and the subsequent endothelial differentiation are further supported from ultrastructural study of cardiac myxomas [20, 29, 30]. The presence of a limited number of myxoma cells co-expressing the primitive endothelial and myocytic markers CD34 and α-actin supports the hypothesis that myxoma cells can derive from a common cardiac early precursor cell [25]. The origin of cardiac myxoma in atrial cavity in association with fibrous septa or fossa ovalis suggests a relationship with fibrous cardiac structures and their development [1, 2]. Endocardial cushions are the precursors of mature heart valves and cardiac septa [31–34]. Embryonic endocardial cells of the outflow tract and atrioventricular canal change their phenotype from endothelial to mesenchymal cells during the so-called endothelial–mesenchymal transformation, leading to cardiac septation and mature valve formation. During this phase, embryonic endocardial cells progressively express α-smooth muscle actin and lose endothelial antigens [33]. Cardiac jelly, an acellular matrix rich in fibronectin and proteoglycans, separates the primitive endocardium from myocardium and favors the initiation of the endothelial–mesenchymal transformation [31–34]. Cardiac jelly appears very similar to extracellular matrix of cardiac myxoma. Transient ectopic activation of Notch1 in zebrafish embryos leads to hypercellular cardiac valves, whereas its inhibition prevents valve development [35]. Notch activation in endothelial cells determines downregulation of endothelial markers and upregulation of mesenchymal ones, including α-smooth muscle actin and fibronectin [35]. Moreover, RT-PCR shows in cardiac myxomas the presence of Sox9 and NFATcI transcripts [20]. Sox9 has been indicated to play an essential role in early phases of endocardial cushion differentiation, when endocardial endothelial cells migrate into the cardiac jelly [36]. NFATcI expression is critical during signal-transduction processes required for cardiac valve formation and is normally abolished after endocardial cushion cell migration [37]. The presence of phenotypic markers of endothelial–mesenchymal transformation may be related to the persistence of developmental remnants or stem cells in adult heart or, alternatively, to de novo re-expression of a developmental phenotype in adult cardiac cells.
Carney’s Complex
Carney’s complex is a neuroendocrine-cardiac syndrome characterized by (a) familial recurrent myxomas; (b) pigmented skin lesions, schwannomas, and recurrent mucocutaneous myxomas; and (c) endocrine abnormalities, including Cushing syndrome and acromegaly, and malignancies [38]. One-third of the patients with Carney’s syndrome display at presentation mucocutaneous myxomas of the eyelid, external ear canal, breast, and oropharynx. About two-thirds of these patients have cardiac tumors, and 75% various skin pigmented lesions, including blue nevi and café au lait spots [39]. Carney’s complex is characterized by an autosomal dominant transmission with incomplete penetrance. Linkage studies have revealed genetic foci at 2p16 and 17q22–24 [40, 41]. Among the families mapping to 17q, mutations in the gene encoding the protein kinase A type I-α regulatory subunit have been identified [42]. In patients with Carney’s complex, cardiac tumors recur in more than 20% of cases, and account for more than 50% of causes of death [39]. Consequently, patients with established Carney’s complex require vigorous screening for cardiac tumors, in particular to exclude multiple locations. Routinary echocardiographic screening of the first-degree relatives seems appropriate for familial myxomas [43].
Genetic Features of Cardiac Non-myxomatous Tumors
Non-myxomatous cardiac benign tumors are rare and sometimes arising in the setting of genetic syndromes (Table 13.2). Molecular genetic investigation of cardiac primary non-myxomatous tumors has provided relevant information to elucidate many mechanisms of cardiac cell developmental growth. Cytogenetic studies have targeted candidate chromosomal loci that may be perturbed during the pathogenesis of cardiac lipoma. Common cutaneous lipomas have been associated with rearrangements of chromosome band 12q15. Cytogenetic analysis of an unusual giant cardiac lipoma in a patient with a history of multiple lipomatosis demonstrated no abnormalities of chromosome 12, but a translocation (2, 19) (p13; p13.2) [48]. Rhabdomyoma, the most common pediatric cardiac neoplasm, is frequently associated with tuberous sclerosis by mutations in the tuberous sclerosis complex-1 and - 2 that codify two proteins, hamartin and tuberin. Tuberous sclerosis complex is a genetic disorder characterized by the formation of hamartomas in multiple organs, including rhabdomyomas in the heart [49]. Hamartin and tuberin antagonize the mammalian target of rapamycin signaling pathway, thus regulating cell growth and proliferation. Nonsense mutations in the hamartin and tuberin genes have been identified as causative of cardiac rhabdomyomas [49]. Many complications have been reported in association with nevoid basal cell carcinoma syndrome, also known as Gorlin–Goltz or Gorlin syndrome [50, 51]. The hallmark of this syndrome is the presence of multiple basal cell carcinomas, which may appear early in infancy. Other associated features may include craniofacial, central nervous system, musculoskeletal, and genitourinary anomalies. Approximately 3% of cases are associated with cardiac fibromas, which may present later during adulthood rather than the typical infancy or childhood period [51]. Consequently, cardiac fibromas are generally not considered part of the syndrome and judged as minor diagnostic criteria [50]. Nevertheless, the investigation of Gorlin syndrome has shed light on the etiology of cardiac fibromas. It is caused by mutations in the PTCH1 gene, which acts as a cell cycle regulator and regulates cell growth, commitment, and differentiation [51].
Cardiac Sarcomas
Introduction
Primary cardiac sarcomas are by definition malignant neoplasms deriving from mesenchymal cells and confined to the heart at the time of diagnosis. Most cardiac sarcomas have the same histological appearance as their soft tissue counterpart. Primary heart sarcomas are exceptionally rare and represent approximately 10% of total primary cardiac tumors [2, 52]; cardiac metastases at autopsy are 20–40 times more frequent than primary tumors [53]. For many years, no universally accepted classification of primary cardiac sarcomas existed. The difficulty derived from the rarity and lack of systematic studies, with only a few series of cardiac sarcomas in the literature. Virtually, all soft tissue sarcoma types have also been found to arise in the heart. The recent WHO classification system of cardiac tumors proposed in 2004 [54] is largely based on the soft tissue classification counterpart and only the most frequent malignant entities are listed, since the majority of cardiac sarcomas have limited areas with morphologically recognizable differentiation. Moreover, despite a careful immunohistochemical investigation, they frequently lack tissue-specific antigens.
Immunohistochemical Features of Cardiac Sarcomas
Despite a careful immunohistochemical investigation, cardiac sarcomas generally lack tissue-specific antigens. Main immunohistochemical findings are schematically reported in Table 13.3 and can be useful in supporting morphological criteria of diagnosis in some specific cases. Angiosarcoma is microscopically characterized by vascular differentiation with channels covered by endothelial cells exhibiting marked atypia. Factor VIII or CD34 positive immunodetection of malignant cells represents useful markers of endothelial differentiation; moreover, cytokeratins can be diffusely positive in epithelioid areas of angiosarcoma [2]. Undifferentiated sarcoma is defined as a cardiac sarcoma with no specific histological pattern or undifferentiated [53]. Nowadays, undifferentiated sarcoma is considered synonymous with pleomorphic malignant fibrous histiocytoma [54]. Undifferentiated sarcoma must be distinguished from embryonal rhabdomyosarcoma and metastatic small cell cancer. Immunostaining is crucial, epithelial, neural, or endothelial markers being usually negative and vimentin typically positive; high grade undifferentiated sarcomas can exhibit focal α-actin positive areas, but the latter are generally limited in their extension [54]. Leiomyosarcoma is a malignant tumor showing phenotypic and ultrastructural smooth muscle differentiation. Immunostaining for desmin and α-actin is usually diffusely positive, whereas epithelial, vascular, and neural markers are negative [55, 56]. Rhabdomyosarcoma is considered as a malignant tumor showing striated muscle differentiation [2, 54]. Rhabdomyosarcoma usually arises in the ventricular wall and is microscopically composed of small cells with the presence of recognizable rhabdomyoblasts with the characteristic cross striations by Masson’s trichrome and a diffuse desmin positive immunostaining [2, 57]. Rhabdomyosarcoma can express other muscle markers, including myogenin, myoD1, sarcomeric actin, muscle-specific actin, and myoglobin. Among these, myogenin and myoD1 seem to be more specific [58]. Synovial sarcoma is a biphasic malignant tumor usually located in the atria or pericardial surface. The latter localization should be considered for distinction from malignant mesothelioma. In the heart, the monophasic variant of synovial sarcoma is more common. A differential diagnosis between malignant mesothelioma and synovial sarcoma may be challenging on the basis of morphological aspect and immunophenotype, both being positive for cytokeratins, calretinin, and vimentin [54].
Genetic Features of Cardiac Sarcomas
At present, the molecular histogenesis of cardiac sarcomas is poorly known and there are no specific genetic mutations reported. This is likely due to the rarity and consequent absence of a systematically characterized large series of cardiac sarcomas. Moreover, as concerning genetic characterization of cardiac sarcomas, K-ras mutation and the absence of p53 mutations have been observed in three cases of angiosarcomas and two of rhabdomyosarcomas [59]. p53 mutations in two primary cardiac angiosarcomas have been reported [60]. Cytogenetic features can represent a useful diagnostic tool and can be detected by using reverse transcriptase-polymerase chain reaction or fluorescence in situ hybridization techniques. Accordingly, synovial sarcomas typically harbor t(X; 18)(p21.2; q11.2) resulting in SS18-SSX1 fusion transcripts, including the reported unique case with a cardiac localization in the examined series [61]. The same SYT-SSX1 fusion transcript identified by molecular genetic studies has been also reported in two cases of primary cardiac synovial sarcoma arising in left atrium and ventricle and on the anterior mitral leaflet [62, 63]. Cytogenetic analysis has been reported to help to distinguish low-grade fibromyxoid sarcoma from either more benign or more malignant tumor types [64]. Cytogenetic investigation also identified a recurrent balanced translocation t(7; 16)(q32–34; p11), later shown by molecular genetic approaches to result in a FUS/CREB3L2 fusion gene. Reverse transcriptase-polymerase chain reaction analysis disclosed a FUS/CREB3L2 fusion transcript in 96% of cases classified as low-grade fibromyxoid sarcoma after the histological reevaluation and from which RNA of sufficient quality could be extracted, whereas a FUS/CREB3L2 fusion transcript was absent in other tumor types [65]. The proteins encoded by a CREB3L1 and CREB3L2 genes belong to the basic leucine-zipper family of transcription factors. A similar t(7;16)(q32–34; p11) translocation by FISH analysis was documented in a primary intracardiac large low-grade fibromyxoid sarcoma of the right atrium [65]. Cytogenetic and molecular genetic studies performed in one case [66] of pleomorphic malignant fibrous histiocytoma removed from the left atrium of a 15-year-old girl [65] revealed several alterations previously associated with adult malignant fibrous histiocytoma, including abnormalities of 11p11 and 19p13 chromosomal bands. Moreover, pleomorphic malignant fibrous histiocytoma demonstrated homogeneously staining regions and double minute chromosomes, in particular the co-amplification of the 12q13–14 chromosome; the latter amplicon was not previously detected in pediatric malignant fibrous histiocytoma. This cytogenetic and molecular genetic evidence suggests that pediatric and adult malignant fibrous histiocytoma, although histogenetically related, are distinct malignancies [66].
References
Reynen K. Cardiac myxomas. N Engl J Med. 1995;333:1610–7.
Burke AP, Virmani R. Tumors of the heart and great vessels. In: Burke AP, Virmani R, editors. Atlas of tumor pathology. 3rd ed. Washington DC: Armed Forced Institute of Pathology; 1996. p. 121–46.
Lie JT. The identity and histogenesis of cardiac myxomas. A controversy put to rest. Arch Pathol Lab Med. 1989;113:724–6.
Tazelaar HD, Locke TJ, McGregor CG. Pathology of surgically excised primary cardiac tumors. Mayo Clin Proc. 1992;67:957–65.
Boxer ME. Cardiac myxoma: an immunoperoxidase study of histogenesis. Histopathology. 1984;8:861–72.
Goldman BI, Frydman C, Harpaz N, Ryan SF, Loiterman D. Glandular cardiac myxomas. Histologic, immunohistochemical, and ultrastructural evidence of epithelial differentiation. Cancer. 1987;59:1767–75.
Govoni E, Severi B, Cenacchi G, Laschi R, Pileri S, Rivano MT, Alampi G, Branzi A. Ultrastructural and immunohistochemical contribution to the histogenesis of human cardiac myxoma. Ultrastruct Pathol. 1988;12:221–33.
Landon G, Ordonez NG, Guarda LA. Cardiac myxomas. An immunohistochemical study using endothelial, histiocytic, and smooth-muscle cell markers. Arch Pathol Lab Med. 1986;110:116–20.
Pucci A, Gagliardotto P, Zanini C, Pansini S, di Summa M, Mollo F. Histopathologic and clinical characterization of cardiac myxoma: review of 53 cases from a single institution. Am Heart J. 2000;140:134–8.
McComb RD. Heterogeneous expression of factor VIII/von Willebrand factor by cardiac myxoma cells. Am J Surg Pathol. 1984;8:539–44.
Vandekerckhove J, Bugaisky G, Buckingham M. Simultaneous expression of skeletal muscle and heart actin proteins in various striated muscle tissues and cells. A quantitative determination of the two actin isoforms. J Biol Chem. 1986;261:1838–43.
Suurmeijer AJ, Clement S, Francesconi A, Bocchi L, Angelini A, Van Veldhuisen DJ, Spagnoli LG, Gabbiani G, Orlandi A. Alpha-actin isoform distribution in normal and failing human heart: a morphological, morphometric, and biochemical study. J Pathol. 2003;199:387–97.
Orlandi A, Ciucci A, Ferlosio A, Genta R, Spagnoli LG, Gabbiani G. Cardiac myxoma cells exhibit embryonic endocardial stem cell features. J Pathol. 2006;209:231–9.
Ha JW, Kang WC, Chung N, Chang BC, Rim SJ, Kwon JW, Jang Y, Shim WH, Cho SY, Kim SS, Cho SH. Echocardiographic and morphologic characteristics of left atrial myxoma and their relation to systemic embolism. Am J Cardiol. 1999;83:1579–82.
Kairemo KJ, Blomqvist CP, Miettinen M. Cardiac myxomas. N Engl J Med. 1996;334:1407–8.
Negishi M, Sakamoto H, Sakamaki T, Ishikawa O, Kanda T, Tamura J, Kurabayashi M, Nagai R. Disaccharide analysis of glycosaminoglycans synthesized by cardiac myxoma cells in tumor tissues and in cell culture. Life Sci. 2003;73:849–56.
Parissis JT, Mentzikof D, Georgopoulou M, Gikopoulos M, Kanapitsas A, Merkouris K, Kefalas C. Correlation of interleukin-6 gene expression to immunologic features in patients with cardiac myxomas. J Interferon Cytokine Res. 1996;16:589–93.
Suzuki M, Hamada M, Hiwada K. Apoptosis in cardiac myxoma. Ann Intern Med. 2000;132:681.
Liu CC, Jung SM, Orlandi A, Yeh TS, Lin YS, Shiu TF, Wu HH, Chu JJ, Lin PJ, Chu PH. The Fas-mediated apoptotic pathway in cardiac myxoma. Int J Surg Pathol. 2010;18:493–8.
Orlandi A, Ciucci A, Ferlosio A, Pellegrino A, Chiariello L, Spagnoli LG. Increased expression and activity of matrix metalloproteinases characterize embolic cardiac myxomas. Am J Pathol. 2005;166:1619–28.
Oh J, Takahashi R, Kondo S, Mizoguchi A, Adachi E, Sasahara RM, Nishimura S, Imamura Y, Kitayama H, Alexander DB, Ide C, Horan TP, Arakawa T, Yoshida H, Nishikawa S, Itoh Y, Seiki M, Itohara S, Takahashi C, Noda M. The membrane-anchored MMP inhibitor RECK is a key regulator of extracellular matrix integrity and angiogenesis. Cell. 2001;107:789–800.
Dollery CM, McEwan JR, Henney AM. Matrix metalloproteinases and cardiovascular disease. Circ Res. 1995;77:863–8.
Singer CF, Kronsteiner N, Marton E, Kubista M, Cullen KJ, Hirtenlehner K, Seifert M, Kubista E. MMP-2 and MMP-9 expression in breast cancer-derived human fibroblasts is differentially regulated by stromal–epithelial interactions. Breast Cancer Res Treat. 2002;72:69–77.
Markwald RR, Fitzharris TP, Manasek FJ. Structural development of endocardial cushions. Am J Anat 1977;148:85–119.
Kodama H, Hirotani T, Suzuki Y, Ogawa S, Yamazaki K. Cardiomyogenic differentiation in cardiac myxoma expressing lineage-specific transcription factors. Am J Pathol. 2002;161:381–9.
Schwartz RJ, Olson EN. Building the heart piece by piece: modularity of cis-elements regulating Nkx2.5 transcription. Development. 1999;126:4187–92.
Riazi AM, Lee H, Hsu C, Van Arsdell G. CSX/Nkx2.5 modulates differentiation of skeletal myoblasts and promotes differentiation into neuronal cells in vitro. J Biol Chem. 2005;280:10716–20.
Sugi Y, Lough J. Onset of expression and regional deposition of alpha-smooth and sarcomeric actin during avian heart development. Dev Dyn. 1992;193:116–24.
Valente M. Structural profile of cardiac myxoma. Appl Pathol. 1983;1:251–63.
Zhang PF, Jones JW, Anderson WR. Cardiac myxomas correlative study by light, transmission, and scanning electron microscopy. Am J Cardiovasc Pathol. 1989;2:295–300.
Sugi Y, Markwald RR. Formation and early morphogenesis of endocardial endothelial precursor cells and the role of endoderm. Dev Biol. 1996;175:66–83.
Gitler AD, Lu MM, Jiang YQ, Epstein JA, Gruber PJ. Molecular markers of cardiac endocardial cushion development. Dev Dyn. 2003;228:643–50.
Nakajima Y, Mironov V, Yamagishi T, Nakamura H, Markwald RR. Expression of smooth muscle alpha-actin in mesenchymal cells during formation of avian endocardial cushion tissue: a role for transforming growth factor beta3. Dev Dyn. 1997;209:296–309.
Moorman A, Webb S, Brown NA, Lamers W, Anderson RH. Development of the heart: (1) formation of the cardiac chambers and arterial trunks. Heart. 2003;89:806–14.
Noseda M, McLean G, Niessen K, Chang L, Pollet I, Montpetit R, Shahidi R, Dorovini-Zis K, Li L, Beckstead B, Durand RE, Hoodless PA, Karsan A. Notch activation results in phenotypic and functional changes consistent with endothelial-to-mesenchymal transformation. Circ Res. 2004;94:910–7.
Akiyama H, Chaboissier MC, Behringer RR, Rowitch DH, Schedl A, Epstein JA, de Crombrugghe B. Essential role of Sox9 in the pathway that controls formation of cardiac valves and septa. Proc Natl Acad Sci USA. 2004;101:6502–7.
Ranger AM, Grusby MJ, Hodge MR, Gravallese EM, de la Brousse FC, Hoey T, Mickanin C, Baldwin HS, Glimcher LH. The transcription factor NF-ATc is essential for cardiac valve formation. Nature. 1998;392:186–90.
Carney JA, Gordon H, Carpenter PC, Shenoy BV, Go VL. The complex of myxomas, spotty pigmentation, and endocrine overactivity. Medicine (Baltimore). 1985;64:270–83.
Pinede L, Duhaut P, Loire R. Clinical presentation of left atrial cardiac myxoma: a series of 112 consecutive cases. Medicine (Baltimore). 2001;80:159–72.
Stratakis CA, Carney JA, Lin JP, Papanicolaou DA, Karl M, Kastner DL, Pras E, Chrousos GP. Carney complex, a familial multiple neoplasia and lentiginosis syndrome: analysis of 11 kindreds and linkage to the short arm of chromosome 2. J Clin Invest. 1996;97:699–705.
Dijkuizen T, van den Berg E, Molenaar WM, Meuzelaar JJ, de Jong B. Rearrangements involving 12p12 in two cases of cardiac myxoma. Cancer Genet Cytogenet. 1995;82:161–2.
Kirscher LS, Carney JA, Pack SD, Taymans SE, Giatzakis C, Cho YS, Cho-Chung YS, Stratakis CA. Mutations of the gene encoding the protein kinase A type I-alpha regulatory subunit in patients with the Carney complex. Nat Genet. 2000;26:89–92.
Grebenc ML, Rosado-de-Christenson ML, Green CE, Burke AP, Galvin JR. Cardiac myxoma: imaging features in 83 patients. Radiographics. 2002;22:673–89.
Curatolo P, Bombardieri R, Jozwiak S. Tuberous sclerosis. Lancet. 2008;372:57–668.
Wilkes D, Charitakis K, Basson CT. Inherited disposition to cardiac myxoma development. Nat Rev Cancer. 2006;6:157–65.
Lo Muzio L. Nevoid basal cell carcinoma syndrome (Gorlin syndrome). Orphanet J Rare Dis. 2008;3:32.
Callender GG, Rich TA, Perrier ND. Multiple endocrine neoplasia syndromes. Surg Clin North Am. 2008;88:863–95.
Vaughan CJ, Weremowicz S, Goldstein MM, Casey M, Hart M, Hahn RT, Devereux RB, Girardi L, Schoen FJ, Fletcher JA, Morton CC, Basson CT. A t(2;19)(p13; p13.2) in a giant invasive cardiac lipoma from a patient with multiple lipomatosis. Genes Chromosomes Cancer. 2000;28:133–7.
Madueme P, Hinton R. Tuberous sclerosis and cardiac rhabdomyomas: a case report and review of the literature. Congenit Heart Dis. 2011;6:183–7.
Evans DG, Ladusans EJ, Rimmer S, Burnell LD, Thakker N, Farndon PA. Complications of the naevoid basal cell carcinoma syndrome: results of a population based study. J Med Genet. 1993;30:460–4.
Gorlin RJ. Nevoid basal cell carcinoma (Gorlin) syndrome. Genet Med. 2004;6:530–9.
Orlandi A, Ferlosio A, Roselli M, Chiariello L, Spagnoli LG. Cardiac sarcomas: an update. J Thorac Oncol. 2010;9:1483–9.
Lymbumer R. Tumours of the heart: histopathological and clinical study. Can Med Assoc J. 1934;30:368–73.
Burke A, Veinot J, Loire R. Tumours of the heart. In: Travis W, Brambilla E, Müller H, Harris C, editors. Tumours of the lung, pleura, thymus and heart. Lyon: IARC Press; 2004. p. 251–88.
Mazzola A, Spano JP, Valente M, Gregoriani R, Villani C, Di Eusanio M, Ciocca M, Minuti U, Giancola R, Basso C, Thiene G. Leiomyosarcoma of the left atrium mimicking a left atrial myxoma. J Thorac Cardiovasc Surg. 2006;131:224–6.
Basso C, Valente M, Poletti A, Casarotto D, Thiene G. Surgical pathology of primary cardiac and pericardial tumors. Eur J Cardiothorac Surg. 1997;12:730–7.
Castorino F, Masiello P, Quattrocchi E, Di Benedetto G. Primary cardiac rhabdomyosarcoma of the left atrium: an unusual presentation. Tex Heart Inst J. 2000;27:206–8.
Cessna MH, Zhou H, Perkins SL, Tripp SR, Layfield L, Daines C, Coffin CM. Are myogenin and myoD1 expression specific for rhabdomyosarcoma? A study of 150 cases, with emphasis on spindle cell mimics. Am J Surg Pathol. 2001;25:1150–7.
Garcia JM, Gonzalez R, Silva JM, Dominguez G, Vegazo IS, Gamallo C, Provencio M, España P, Bonilla F. Mutational status of K-ras and TP53 genes in primary sarcomas of the heart. Br J Cancer. 2000;82:1183–5.
Naka N, Tomita Y, Nakanishi H, Araki N, Hongyo T, Ochi T, Aozasa K. Mutations of p53 tumor-suppressor gene in angiosarcoma. Int J Cancer. 1997;71:952–5.
Amary MF, Berisha F, Bernardi Fdel C, Herbert A, James M, Reis-Filho JS, Fisher C, Nicholson AG, Tirabosco R, Diss TC, Flanagan AM. Detection of SS18-SSX fusion transcripts in formalin-fixed paraffin-embedded neoplasms: analysis of conventional RT-PCR, qRT-PCR and dual color FISH as diagnostic tools for synovial sarcoma. Mod Pathol. 2007;20:482–96.
Hazelbag HM, Szuhai K, Tanke HJ, Rosenberg C, Hogendoorn PC. Primary synovial sarcoma of the heart: a cytogenetic and molecular genetic analysis combining RT-PCR and COBRA-FISH of a case with a complex karyotype. Mod Pathol. 2004;17:1434–9.
Miller DV, Deb A, Edwards WD, Zehr KJ, Oliveira AM. Primary synovial sarcoma of the mitral valve. Cardiovasc Pathol. 2005;14:331–3.
Mertens F, Fletcher CD, Antonescu CR, Coindre JM, Colecchia M, Domanski HA, Downs-Kelly E, Fisher C, Goldblum JR, Guillou L, Reid R, Rosai J, Sciot R, Mandahl N, Panagopoulos I. Clinicopathologic and molecular genetic characterization of low-grade fibromyxoid sarcoma, and cloning of a novel FUS/CREB3L1 fusion gene. Lab Invest. 2005;85:408–15.
Jakowski JD, Wakely Jr PE. Primary intrathoracic low-grade fibromyxoid sarcoma. Hum Pathol. 2008;39:623–8.
Palmer JL, Masui S, Pritchard S, Kalousek DK, Sorensen PH. Cytogenetic and molecular genetic analysis of a pediatric pleomorphic sarcoma reveals similarities to adult malignant fibrous histiocytoma. Cancer Genet Cytogenet. 1997;95:141–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Orlandi, A., Spagnoli, L.G. (2013). Novelties in Immunohistochemical and Molecular Study of Cardiac Tumors. In: Basso, C., Valente, M., Thiene, G. (eds) Cardiac Tumor Pathology. Current Clinical Pathology. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-62703-143-1_13
Download citation
DOI: https://doi.org/10.1007/978-1-62703-143-1_13
Published:
Publisher Name: Humana Press, Totowa, NJ
Print ISBN: 978-1-62703-142-4
Online ISBN: 978-1-62703-143-1
eBook Packages: MedicineMedicine (R0)