Abstract
Since the 1980s, cholesterol guidelines for Americans have been sponsored by The National Heart, Lung, and Blood Institute of the National Institutes of Health. These guidelines were produced by the National Cholesterol Education Program. From this program, an Adult Treatment Panel (ATP) has organized the major sets of guidelines. Three reports were issued by ATP. The third and last was updated by a smaller panel in 2004. More recently, the National Heart, Lung, and Blood Institute has turned the cholesterol guideline process over to the American College of Cardiology and the American Heart Association (ACC/AHA). Guidelines from other countries have generally followed the third ATP report. ACC/AHA guidelines have attempted to restrict their recommendations to information derived from randomized clinical trials. Thus, they are much narrower than ATP reports. The latter made recommendations on several lines of evidence, including clinical trials, epidemiology, genetics, and dietary and metabolic studies. Since the publication of ACC/AHA recommendations, considerable controversy has emerged on how best to develop cholesterol guidelines. This chapter examines this question and suggests potential approaches.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
For over 50 years, scientific evidence has grown that low-density lipoproteins (LDL) are a strong risk factor for atherosclerotic coronary heart disease (CHD). The relation between LDL levels and CHD risk is bidirectional and log-linear [1]. Bidirectional means that increasing LDL raises risk for CHD, whereas decreasing levels reduces risk. Log-linear means that progressively lower levels are accompanied by diminishing absolute risk reduction. That higher LDL levels increase atherosclerosis or CHD has been shown in laboratory animals, in patients with familial hypercholesterolemia , and in populations with higher LDL levels [1]. Over the past 30 years, randomized controlled trials (RCTs) with pre-statin and statin drugs have demonstrated that lowering of LDL levels reduces CHD [1, 2]. More recently, genetic epidemiology has shown and confirmed that a lifetime of low LDL levels, secondary to pro-protein convertase subtilisin kexin 9 (PCSK-9) null or loss-of-function mutations, essentially eliminates CHD [3].
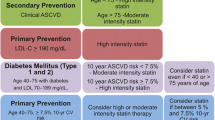
Without doubt, the strongest evidence for the relation between LDL and CHD comes from statin RCTs. A substantial number of major statin trials have shown a progressively lower risk for CHD events as LDL levels fall [1]. These trials reveal two things. First, the lower the LDL level, the lower is the risk for CHD; and second, statins are highly efficacious for reducing LDL levels and CHD risk. These RCTs have generated some debate. For example, one view holds that prevention guidelines should be constructed around LDL goals [1]; another view contends that guidelines should be defined exclusively in terms of statin therapy [4]. These two views can be considered and contrasted in this chapter. Guidelines previously divided preventive strategies into secondary prevention and primary prevention. This still appears to be a good strategy. This will be the approach taken in this chapter.
Secondary Prevention
Secondary prevention targets patients with existing or manifest atherosclerotic cardiovascular disease (ASCVD) . Included in this category are individuals with CHD, previous thrombotic stroke, peripheral arterial disease (PAD), aortic aneurysm, and other atherosclerotic diseases. Such persons are at high risk for recurrent vascular events. Once a person manifests vascular disease in one arterial bed, there is a high likelihood for events in other beds. For example, patients with PAD are at high risk for developing CHD .
Clinical Trial Evidence in Secondary Prevention
A large number of clinical trials have documented that cholesterol-lowering therapy will reduce risk for ASCVD in patients with established atherosclerotic disease [1, 2]. In the pre-statin era, meta-analysis of trials with cholesterol-lowering drugs showed a significant reduction in CHD events [5]. After the introduction of statins, a host of studies documented significant risk reduction [6–21]. These trials have convinced the medical community that cholesterol lowering is beneficial for patients with established ASCVD. They further show that statin therapy can reduce risk for future atherosclerotic events by 30–50 %. Today, use of statins in secondary prevention has become routine.
LDL-C Goals
The US National Cholesterol Education Program (NCEP) has championed the LDL-centered approach to ASCVD reduction. The NCEP Adult Treatment Panel III [1] set an LDL-C goal of < 100 mg/dL for patients with ASCVD; later, ATP III recommended an LDL-C of < 70 mg/dL for ASCVD patients at very high risk for future cardiovascular events [2]. The latter included those ASCVD patients with diabetes, metabolic syndrome, or multiple risk factors. Recently, the American Heart Association (AHA) and the American College of Cardiology (ACC) made a similar recommendation for secondary prevention [22]. Other organizations, i.e., European [23] and Canadian [24] guidelines, recommend LDL-C goals of < 1.8 mmol/L (< 70 mg/dL) or < 2.0 mmol/L (< 77 mg/dL), respectively, for those with established CHD.
Justification for these lower goals comes from several statin trials (or subgroup analyses of these trials). In these trials, very low levels of LDL-C were achieved and showed incremental benefit at these levels compared to higher on-treatment levels [15, 19–25]. Perhaps the best example to support the notion that “the lower, the better” for LDL-C comes from a recent meta-analysis that includes 38,153 patients allocated to statin therapy; in this analysis, a total of 6286 major cardiovascular events occurred in 5387 study participants during follow-up [26]. Key results of this study are shown in Table 18.1. In this analysis, compared to subjects who achieved an LDL-C > 175 mg/dL, those who reached an LDL-C 75–100 mg/dL, 50–75 mg/dL, and < 50 mg/dL had adjusted hazard ratios for major cardiovascular events of 0.56, 0.51, and 0.44, respectively.
Thus, regarding goals for LDL therapy, it is reasonable to achieve as low an LDL as possible within the bounds of realistic clinical practice. In the meta-analysis described above, 40 % of subjects given high-dose statins did not reach an LDL-C target < 70 mg/dL. For those who do not achieve very low LDL-C levels, clinical judgment is required whether to add a second LDL-lowering drug.
Other Lipid Targets
Although LDL-C is generally recognized as the primary target of lipid-lowering therapy, other lipid measures have been identified as contributing to ASCVD risk. For example, there is a growing recognition that very low-density lipoproteins (VLDL) are atherogenic like LDL. This has led to the suggestion that the cholesterol contained in LDL + VLDL, i.e., non-high-density lipoprotein cholesterol (non-HDL-C), may be a better target of lipid-lowering therapy than LDL-C alone [1, 25, 27]. At the least, non-HDL-C is equivalent to low-density lipoprotein cholesterol (LDL-C) as a target of treatment; and in the view of many, it is the preferred target. If non-HDL-C is made the primary target, the goal for patients with ASCVD would be a level of < 100 mg/dL [1].
Another view favors apolipoprotein B (apo B) as the primary target of treatment in secondary prevention [28, 29]. All atherogenic lipoproteins contain one apo B molecule per lipoprotein particle. Some authors contend that serum apo B levels are a better indicator of atherogenicity than non-HDL-C [29–32]. The usual method for measuring apo B is immunological; this method has limitations and universal standardization has not been achieved [33, 34]. Measurement of apo B moreover costs more than does estimation of non-HDL-C. Finally, there is the question of what is the appropriate goal of therapy for apo B in secondary prevention . This question has been discussed thoroughly by Harper and Jacobson [35] and by Brunzell et al. [31]. A consensus goal for total apo B has not been reached. Until agreement can be reached on what is the appropriate apo B goal for secondary prevention, it is difficult to produce a solid clinical recommendation. Standardization and costs are added limitations. Of course, all of these limitations potentially could be overcome. But even so, whether apo B is more desirable than non-HDL-C as a target in secondary prevention is doubtful [36].
Secondary Prevention Without Specific Lipid-Lowering Goals
Most RCTs in secondary prevention have been carried out with statin therapy. Recently, the ACC/AHA [4] released a new set of treatment guidelines in which no LDL-C goals were identified. Instead, these guidelines recommended that high-intensity statins be used in all patients with established ASCVD. High-intensity statins include atorvastatin 80 mg and rosuvastatin 20–40 mg. They claim that RCT evidence for other cholesterol-lowering drugs is too weak to justify any recommendations. They declined to support any particular goal for LDL-C.
ACC/AHA guidelines [4] discount the value of other lipid-lowering drugs because their efficacy in large-scale RCT have not been adequately demonstrated. Thus, the new guidelines are essentially statin-treatment guidelines. They consider LDL to be only a risk marker but without RCT-proven atherogenic potential. Therefore, these guidelines negate any value to other cholesterol-lowering agents based on their ability to lower LDL alone. This view of course runs counter to the basic premise of 25 years of the NCEP, which holds that any form of LDL reduction will reduce risk.
Combination Drug Therapy in Secondary Prevention
According to ATP III [1], but contrary to ACC/AHA guidelines [4], two drugs are available to add to high-intensity statin to increase the proportion of patients who can achieve an LDL-C < 70 mg/dL. These are bile-acid-binding resins and ezetimibe. Bile-acid-binding resins have been shown to reduce ASCVD in patients with hypercholesterolemia [37]. They reduce the absorption of bile acids by the intestine. This decreases return of bile acids to the liver, which releases feedback inhibition of bile acids on conversion of cholesterol into bile acids. The result is a reduction of hepatic cholesterol, which increases the activity of LDL receptors. By this mechanism, bile acid resins lower LDL-C levels by 15–25 %. Ezetimibe partially blocks the absorption of cholesterol, reduces the return of cholesterol to the liver, lowers hepatic cholesterol, and increases LDL receptors. This action also lowers LDL-C levels by 15–25 % [38]. The addition of bile-acid-binding resins or ezetimibe to statins enhances LDL-C reduction. For example, adding colesevelam, a bile acid resin, to atorvastatin 10 mg lowers LDL-C similarly to atorvastatin 80 mg [39]. Likewise, combining ezetimibe plus atorvastatin 40 mg lowered LDL-C more than atorvastatin 80 mg [40]. In the latter study, only 32 % of patients treated with atorvastatin 80 mg attained an LDL-C level of < 70 mg/dL, whereas 74 % of those treated with atorvastatin 40 mg + ezetimibe 10 mg achieved an LDL-C < 70 mg/dL.
Although adding colesevelam or ezetimibe to atorvastatin 80 mg undoubtedly would increase the proportion of subjects who would attain an LDL-C < 70 mg/dL, whether such a combination will reduce risk for ASCVD events has not been tested in RCTs. A very large clinical trial would be necessary to test the efficacy of these add-on drugs because: (a) the addition in LDL lowering is relatively small, and (b) the risk would already be reduced substantially by high-dose statin. To address these issues, one RCT is currently underway to test the efficacy of ezetimibe as add-on to statin therapy. The IMProved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) is a multicenter RCT designed to test whether the addition of ezetimibe to statin therapy, using ezetimibe/simvastatin, will produce increased clinical benefit on cardiovascular outcomes relative to simvastatin monotherapy in patients with acute coronary syndrome [41]. The trial was designed to recruit up to 18,000 patients, stabilized after an acute coronary syndrome. They were randomized in a 1:1 ratio to once-daily doses of either ezetimibe/simvastatin 10/40 mg or simvastatin monotherapy 40 mg or 80 mg. The primary end point is the first occurrence of an ASCVD event. The IMPROVE-IT investigators estimate a requirement for 5250 events to maintain a desired 90 % power to detect the expected reduction in cardiovascular events, the expected decrease in LDL-C levels, and the anticipated rate of loss of subjects to follow-up.
The IMPROVE-IT trial has now been completed. The results have not been published but were presented at the 2014 American Heart Association Scientific Sessions. Detailed findings of IMPROVE-IT are available on-line (clinicaltrialresults.org/Slides/AHA2014/Cannon).The results of this study can be briefly summarized. It is the first large RCT to show incremental clinical benefit when adding a non-statin agent (ezetimibe) to statin therapy. It demonstrated that “even lower is better”, that is, incremental reduction in ASCVD when mean LDL-C on statins (70 mg/dL) was reduced to 53 mg/dL. There were no adverse effects when ezetimibe was added to a statin. The authors claim that this study reaffirms the LDL hypothesis justifying combined lipid lowering drugs in secondary prevention.
Another lipid-lowering drug, nicotinic acid, has been shown to reduce ASCVD events in monotherapy [42, 43]. Nicotinic acid, when combined with statins, apparently retards progression of subclinical atherosclerosis [44, 45]. Whether nicotinic acid as an add-on to maximal statin therapy reduces risk for ASCVD events beyond statin therapy alone had not been adequately tested until recently. In 2011, nicotinic acid combined with maximal statin therapy in a smaller RCT failed to give added risk reduction in secondary prevention [46]. A larger trial of combination therapy therefore was needed to test whether nicotinic acid provides incremental benefit. Such a trial (http://clinicaltrials.gov/ct2/show/NCT00461630) has recently been completed; this trial assessed the effects extended-release niacin/laropiprant versus matching placebo on ASCVD events in 25,000 men and women with existing ASCVD and who were taking high-dose statin. A recent statement from the investigators indicates that this study failed to document benefit from niacin add-on to statin therapy. However, results of the trial have not been published.
The demand that only RCTs can be used to make lipid-lowering guidelines limits the potential for add-on drugs to give additional risk reduction beyond the use of high-dose statin in secondary prevention. However, if the IMPROVE-IT trial is positive, this would open the door to use of non-statin drugs. If not, it is doubtful whether new RCTs will be done with either bile acid resins or ezetimibe. The costs are too high. Trials with more potent lipid-lowering drugs nonetheless may be tested as add-on therapy. Several of these latter drugs can be considered.
LDL-Lowering Therapies Under Development
Microsomal triglyceride transfer protein (MTP) inhibitors block the incorporation of triglyceride into VLDL and reduce the secretion of these lipoproteins. VLDL are precursors of LDL. Reducing hepatic input of VLDL thereby reduces LDL levels. Available MTP inhibitor, Lomitapide, reduces LDL-C levels by approximately 50 % [47]. The combination of an MTP inhibitor with a statin markedly reduces LDL levels. Unfortunately, blockage of transfer of triglyceride into VLDL causes triglyceride retention in liver. The resulting fatty liver stands in the way of routine use of MTP inhibitors. But in patients with severe hypercholesterolemia, who are resistant to other lipid-lowering drugs, MTP inhibitors may be acceptable. Even so, they must be monitored carefully for liver dysfunction.
Another class of drugs that will substantially lower LDL-C levels are antisense oligonucleotides. These agents target apo B synthesis. The currently available agent is named Mipomersen. One recent study tested Mipomersen as an add-on drug to maximally tolerated statins in patients with heterozygous familial hypercholesterolemia. This product reduced LDL-C levels by an additional 26 % [48]. Like MTP inhibitors, blockage of apo B synthesis potentially causes fatty liver. In this recent study [48], Mipomersen increased liver fat content by 5 %. An increase in alanine aminotransferase values ≥ 3 times the upper limit of normal also was observed in 6 % of subjects. To date, there are only a few reported studies with the oligonucleotide; more studies will be required to determine whether this approach is safe and practical.
Another potential class of add-on drugs includes cholesterol-ester transfer protein (CETP) inhibitors. Inhibition of CETP retards transfer of cholesterol ester from HDL to VLDL and LDL. This increases HDL-C and lowers LDL-C. The first drug in this class was torcetrapib [49]. In a large RCT of 15,067 patients at high cardiovascular risk, participants received either torcetrapib plus atorvastatin or atorvastatin alone. The primary outcome was a composite of ASCVD events. Compared to atorvastatin alone, there was an increase of 72.1 % in HDL-C and a 24.9 % decrease in LDL-C. Unfortunately, torcetrapib treatment caused more ASCVD events and total deaths. Because of these side effects, the trial was terminated early. Despite this termination, testing of other CETP inhibitors has continued.
The second CETP inhibitor to be tested was dalcetrapib. This RCT recruited 15,871 with acute coronary syndromes and randomized them to dalcetrapib 600 mg or the best available evidence-based care. The primary end point was composite ASCVD [50]. During the trial, HDL-C levels in the dalcetrapib group increased by 31–40 %, whereas LDL-C were essentially unchanged. After a median of 31 months, 1135 primary end points were achieved (71 % of the projected total number). At this analysis, an independent data and safety monitoring board recommended ending the study for futility. There may be several explanations for the failure to attain a reduction in events. First, dalcetrapib was a relatively weak CETP inhibitor and failed to reduce LDL-C levels. Alternatively, a rise in HDL-C by CETP inhibition may not be antiatherogenic.
To test whether a more efficacious CETP inhibitor will be effective, a 1623-patient, a phase II trial with anaceptrapib was carried out in patients treated with statins [51]. This study showed that anaceptrapib reduced LDL-C by an additional 40 % and raised HDL-C by 138 %. To date, anaceptrapib has shown no significant side effects, and a large RCT has been initiated to determine its safety and efficacy as an add-on drug to maximal statin therapy.
Another class of LDL-lowering agents consists of the PCSK9 inhibitors. PCSK9 is a serum protein that blocks the ability of LDL receptors to remove LDL from the circulation. Apparently, PCSK9 reduces LDL receptor levels by binding and targeting the receptor for lysosomal degradation [52, 53]. Persons who have a mutation in PCSK9 that prevents the interaction of the protein with LDL receptors have a high expression of receptors and low serum levels of LDL throughout life. These persons appear to be protected against CHD [5, 54, 55]. Recently, the pharmaceutical industry has developed antibodies against PCSK9 that block its action on LDL receptors and lower LDL levels [56, 57]. The addition of PCSK9 inhibitors to statin therapy enhances LDL lowering. Although these agents are promising for achieving and exceeding an LDL-C goal of < 70 mg/dl, their efficacy and safety must be demonstrated in clinical trials.
Lifestyle Therapy in Secondary Prevention
Although in the secondary prevention arena emphasis has been on lipid-lowering drugs, nonetheless, the potential benefit of therapeutic lifestyle changes should not be overlooked. Lifestyle therapies have two major goals: (a) to reduce LDL-C levels and (b) to reduce the metabolic syndrome [1]. The first can be achieved largely by reducing intakes of saturated fats, trans fats, and dietary cholesterol. The second is best approached through both weight reduction and increased physical activity. All patients with established ASCVD should be educated and encouraged to adopt effective lifestyle therapies.
Treatment of Hypertriglyceridemia in Secondary Prevention
For patients who remain hypertriglyceridemic on statin therapy, fibrates can be considered as a second drug [58]. RCTs have reported reductions in ASCVD in primary and secondary prevention with fibrates ; a meta-analysis of these trials found that fibrates lower risk by approximately 10 % [59]. Moreover, meta-analysis in patients with hypertriglyceridemia has shown even greater reductions in risk [60]. The safest fibrate to be used with statins appears to be fenofibrate, which is largely devoid of myopathy risk [61].
In summary, the strongest evidence of benefit for risk reduction in secondary prevention trials has been obtained with RCTs using high-intensity statins (e.g., atorvastatin 80 mg). RCTs and subgroup analysis support reducing LDL-C to very low levels (60–75 mg/dL). However, the majority of subjects treated with high-intensity statins fail to achieve these levels. For this reason, consideration can be given to use of an add-on drug to maximal statin therapy to achieve this lower goal. Drugs currently available to obtain very low levels of LDL-C are bile-acid-binding resins and ezetimibe. Whether the addition of these drugs to maximal statin therapy will further reduce risk for ASCVD has not been tested, although one RCT in which ezetimibe is added to maximal statin dose is underway. Two recent clinical trials using niacin as add-on therapy to maximal statin therapy failed to document added benefit. Fenofibrate can be considered as a second drug in patients with hypertriglyceridemia. Newer drugs are currently undergoing testing to determine whether they may have some potential as add-on drugs to achieve very low LDL levels. These include CETP inhibitors, PCSK9 inhibitors, apo B synthesis inhibitors, and MTP inhibitors. Only when these trials are complete will it be known whether they are incrementally beneficial.
Primary Prevention
Because of the efficacy of statin therapy in secondary prevention trials, many investigators believe that this same drug-treatment strategy can be extended to primary prevention . Since statins are powerful LDL-lowering drugs and are relatively safe, why not just treat large segments of the population with statins before they develop ASCVD? In fact, recent ACC/AHA guidelines [4] have moved in this direction. They have done this in two ways: (a) by lowering the risk threshold for starting statins, and (b) by ignoring baseline LDL-C levels for statin initiation. Through these changes, all people will eventually become candidates for statin therapy. In other words, these guidelines are a step towards making statins a public health measure rather than a clinical therapy.
Risk Assessment: Selection of Patients for Drug Treatment
Ten-year Risk Assessment for CHD
In ATP III [1], 10-year risk for CHD is estimated by an algorithm developed by the Framingham Heart Study. These guidelines recommended that intensity of LDL-lowering therapy be adjusted according to 10-year risk for CHD. According to ATP III, risk can be categorized as high, moderately high, moderate, and low [1]. High risk was classified as a 10-year risk for hard CHD of ≥ 20 %; moderately high risk was 10–19 %; moderate risk was approximately 5–9 %; and low risk was < 5 %. This classification of risk has been widely accepted in the USA. In Europe, 10-year risk for cardiovascular mortality is preferred over morbidity for risk assessment [23].
Ten-year Risk for Total ASCVD
The ACC/AHA guidelines [4] expanded the Framingham end point to include both CHD and stroke. Here the algorithm to assess ASCVD risk becomes all-important for selection of patients for statin therapy. If it overpredicts risk, more low-risk persons will be selected for drug therapy. Prior to ACC/AHA guidelines, Framingham investigators published a risk-prediction algorithm that includes CHD, stroke, peripheral vascular disease, and heart failure [62]. To date, it has not been tested for its practicality. One study showed that its use will markedly change therapeutic strategies [63]. ACC/AHA instead utilized a different algorithm to predict ASCVD. This algorithm was obtained by combining data from five large epidemiologic studies sponsored by NHLBI [64]. Since the publication of the ACC/AHA algorithm, a question has been raised as to whether it overestimates risk in the current US population. If so, an excess of low-risk patients would be treated with statins. There is some evidence that population risk has declined since the earlier studies contained in this algorithm. For example, Ridker and Cook [65] recently reported that three US populations have approximately half the risk calculated by the ACC/AHA algorithm. Moreover, several studies have indicated that the Framingham algorithm, which is contained in the new ACC/AHA tool, overestimates risk in several European populations [66–72].
This uncertainty must be taken into account when estimating risk in the US population; it requires considerable clinical judgment as to whether patients at low risk are being overtreated with cholesterol-lowering drugs.
The uncertainty over the reliability of the ACC/AHA algorithm requires us to consider another metric for statin therapy namely the number needed to treat (NNT) to prevent one ASCVD event over 10 years. This is illustrated in Table 18.2. If we assume that statin therapy reduces risk for ASCVD by 40 % and if the ACC/AHA algorithm is correct, the NNT for each risk category is shown in the first column. But if the algorithm overestimates risk by twofold, NNT is shown in the second column. As low risk, the NNT is relatively high, but particularly so if risk is overestimated. A more acceptable NNT is obtained as the risk becomes higher. There is no consensus number on NNT for statin drugs, so a decision about initiation of drug therapy depends on agreement between physician and patient.
Assessment of Lifetime Risk
The 10-year risk assessment for ASCVD is problematic because the purpose of primary prevention is to reduce lifetime risk. This fact has led to increased interest in estimating lifetime risk [73–77]. Donald Lloyd-Jones and associates [73, 78–85] have published a series of papers on estimation of lifetime risk. Other investigators have projected lifetime risk based on Framingham data [75]. Another lifetime risk predictor is the QRISK model [77, 86, 87]. This model was derived from a prospective cohort study with data from general practices in the UK between 1994 and 2010. Recent guidelines from the International Atherosclerosis Society [88] have adopted lifetime risk assessment as a basis for recommendations of intervention to treat elevated cholesterol and other lipid abnormalities.
Risk Assessment by Atherosclerosis Imaging
Framingham risk scoring is highly dependent on age as a risk factor. Since atherosclerosis increases progressively with age, age essentially becomes a surrogate for atherosclerosis burden. The relation between age and plaque burden may hold for populations but not necessarily for individuals. Therefore, some investigators have postulated that a better way to estimate risk would be to replace age with a more direct measure of atherosclerosis.
One method for determining subclinical atherosclerosis burden is by measuring coronary artery calcium (CAC) [89]. CAC measurements are strongly correlated with coronary artery plaque burden [90–94]. Some years ago, Grundy [95] proposed using CAC to replace chronological age as a risk factor when using Framingham risk scoring. This approach has been validated in more recent studies [96]. One utility of this adjustment is to identify persons who are at low risk and who are unlikely to benefit from cholesterol-lowering drugs. Although some persons lacking in CAC can still have coronary plaques, these individuals are relatively rare and do not negate the value of CAC testing in individuals. This method of risk assessment appears to be particularly attractive for older persons. If it is used, many fewer older people will require statin therapy than is selected by the ACC/AHA algorithm.
Since the ACC/AHA algorithm includes stroke as well as CHD, imaging of the carotid arteries may also be helpful in the selection of patients for statin therapy. This is best done by measurement of carotid intimal medial thickness (IMT) with sonography [97]. If the patient is found to have an increased IMT, prevention of stroke through use of statins is reasonable.
Role of Emerging Risk Factors in Risk Assessment
A variety of other factors have been found to associate with increased risk for ASCVD [1, 98]. These include various lipid factors (e.g., low HDL, small LDL particles, and lipoprotein [a]), pro-inflammatory factors (e.g., C-reactive protein [CRP]), prothrombotic factors (e.g., PAI-1), insulin resistance , and hyperglycemia. A low HDL strongly correlates with ASCVD risk, but whether it is a cause of atherosclerotic disease has not been determined. Further, a low HDL is confounded by non-HDL-C levels; nonetheless, HDL-C is incorporated into most risk algorithms because of the strong association with ASCVD risk. A high CRP appears to reflect a pro-inflammatory state; it has been included in one CHD risk algorithm [99, 100]. Small LDL particles are confounded by a high non-HDL-C, but whether they are more atherogenic than normal-sized LDL is uncertain. Diabetes is accompanied by increased ASCVD risk; but whether this is due to hyperglycemia per se is uncertain. Diabetes and insulin resistance are components of the metabolic syndrome, which likewise highly correlates cardiovascular risk [101–102]. Finally, a strong family history of premature ASCVD associates with risk. Thus, the presence of all of these emerging risk factors is strongly suggestive of higher risk, although they have not been incorporated into either Framingham or ACC/AHA algorithms. Patients who exhibit one or more of these risk factors can be considered to be at higher risk, but clinical judgment is required whether to modify therapy beyond that advocated using standard algorithms. In the cardiovascular field, opinion is divided on this point.
LDL-C Goals in Primary Prevention
If guidelines are going to employ LDL-C goals, it may be useful to classify LDL-C levels according to relative risk reduction (Table 18.1). These ranges are potential goals for therapy.
In 2002, ATP III set a goal of < 130 mg/dL for individuals with a moderate-to-moderately high risk [1]. Since that time, there has been growing evidence for further risk reduction by reducing LDL-C levels below 130 mg/dL [103]. The ATP III update [2] indicated that when drug therapy is employed, it is reasonable to set an LDL-C goal of < 100 mg/dL (e.g., 75–99 mg/dL). The Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) trial [103] showed that still lower LDL-C levels reduce ASCVD risk even more. In strictly scientific terms, therefore, it can be said for LDL-C that “the lower, the better” for risk reduction. But to achieve very low LDL-C levels (50–74 mg/dL), high-intensity statins are required for many people. On practical grounds, therefore, clinical judgment is needed to determine whether an effort should be made to achieve a very low LDL-C level. Recent Canadian guidelines [24] favored obtaining a very low LDL-C for primary prevention when statins are employed. Certainly, for high-risk patients, (e.g., those with diabetes and cigarette smokers) attaining very low levels is reasonable. But for those at lower risk, reducing LDL-C to < 100 mg/dL (75–99 mg/dL) should be sufficient. According to current epidemiologic data [55], once LDL-C levels reach 100 mg/dL, additional lowering appears to be accompanied by diminishing returns for risk reduction. From RCTs, it is uncertain whether the decline in risk accompanied a decline in LDL-C is linear or curvilinear (log-linear).
Statin Therapy Without LDL-Cholesterol Goals in Primary Prevention
Since most clinical trials have employed statin therapy, it can be expected that statins will receive highest priority in any guidelines for cholesterol-lowering drugs. As mentioned before, ACC/AHA guidelines hold that statin therapy should be based exclusively on risk estimates regardless of LDL-C levels and without any defined LDL-C goals of therapy. If this approach is to be recommended for primary prevention, a nontrivial question is whether to use moderate-intensity or high-intensity statins. ACC/AHA [4] appears to favor high-intensity statins where possible, although they seemingly accept moderate-intensity statins for primary prevention. The latter include simvastatin 20 mg, pravastatin 40 mg, lovastatin 40 mg, atorvastatin 10 mg, and rosuvastatin 5 mg. Some investigators favor starting with moderate-intensity drugs and triturating the drug upwards as tolerated and according to the degree of LDL lowering.
Since publication of ACC/AHA guidelines, concern has been raised about elimination of LDL-C goals from recommendations [104–107]. Several advantages to use of goals have been claimed: (a) monitoring adherence to drug therapy, (b) monitoring LDL-C response to therapy, (c) allowing adjustment of drug dosage to achieve the goal of therapy, and (d) ensuring maximal LDL-C reduction in higher-risk patients.
When to Start Drug Therapy in Primary Prevention
Most investigators would agree that statin therapy is indicated for persons with 10-year risk for CHD of ≥ 20 % (ASCVD > 27 %). Likewise, in accord with ATP III, cost-effective statin therapy can be recommended for persons whose 10-year risk for CHD is ≥ 10 % (ASCVD > 15 %). Whether to recommend statins for a CHD-risk threshold of 5 % (e.g., ASCVD risk 7–10 %) is more open to question. This question cannot be separated from the age group of the patient. For convenience, it may be useful to separate subjects and at 20-year periods: 60–79 years, 40–59 years, and 20–39 years. Older persons have the highest risk for ASCVD; but reliability for risk assessment is lowest in this age group. Measurement of subclinical atherosclerosis can be particularly useful for deciding when to initiate statin therapy. If the ACC/AHA algorithm is employed, it may be preferable to set a 10-year risk threshold for ASCVD of ≥ 15 %. This corresponds to adding a major risk factor (e.g., hypertension, cigarette smoking, or diabetes) to an optimal or near-optimal baseline risk. In middle age, the ACC/AHA algorithm appears to be adequate. Likewise, a risk threshold for statin therapy of 7.5 % appears appropriate. Finally, for young adults, emphasis should be on lifestyle therapy. Combining a non-atherogenic diet with weight control and exercise and avoidance of cigarette smoking in most cases should be sufficient to retard development of atherosclerosis . However, if major risk factors including high LDL-C have taken hold at a young age, it seems appropriate to intervene with drug therapy if necessary to reverse the risk factor.
Non-Statin Drugs in Primary Prevention
Let us next ask whether statins are the only acceptable drugs for primary prevention. Other agents are approved for LDL lowering: bile acid sequestrants , nicotinic acid, ezetimibe, and fibrates. LDL lowering with bile acid sequestrants have been shown to safely reduce risk in hypercholesterolemic subjects without established ASCVD [108–110]; but it has not been adequately tested for primary prevention. Ezetimibe has not been studied for primary prevention, although theoretically should lower risk if used for a long period. Fibrates have been reported for lower risk in primary prevention [111], but they are not strong LDL-lowering drugs. Thus, statins are obviously first-line therapy for primary prevention; ezetimibe and bile acid sequestrants have potential, but are not adequately tested for efficacy to satisfy most investigators. However, they might be used as add-on drugs to statins in patients with hypercholesterolemia in whom low LDL levels are not attained by statins alone. The potential value of combining another LDL-lowering drug with a statin has been shown by the IMPROVE-IT trial.
If a 15 % reduction in LDL-C starting in young adulthood with mildly elevated LDL-C can reduce risk by 50 % over a lifetime, it might be worthwhile to consider using a bile acid sequestrant, to age 60; thereafter, a moderate dose of statin could be introduced to achieve further reduce risk for the remainder of life. Such a strategy could be based on currently available information, although it has not been tested with RCTs.
Lifestyle Intervention for Primary Prevention
The goal for lifestyle intervention in primary prevention is to reduce all of the risk factors for ASCVD. Highest on the list is elimination of tobacco use. Cigarette smoking is the most important lifestyle factor responsible for ASCVD. Other lifestyle factors have been discussed in detail previously [1]. To achieve maximal LDL lowering, saturated fatty acids should be reduced < 7 % of total calories, or at least to < 10 %. Intake of trans fatty acids should be lowered to < 1 % of total calories and dietary cholesterol to < 200 mg/day. For greater LDL lowering, plant sterols/stanols (2 g/day) can be used as a dietary adjunct. The preferable total fat intake is about 30 % of total calories, with most fatty acids being unsaturated. Total caloric intake should be adjusted to achieve a desirable body weight. Finally, many investigators believe that the diet should be enriched in fruits, vegetables, and fibers. Sodium intake should be < 2 gm/day, and foods high in potassium should be encouraged. A common recommendation is for a diet containing fish rich in omega-3 fatty acids .
Population studies show that favorable life habits can greatly reduce the population volume of ASCVD. This combined with judicious use of agents that will moderately reduce LDL-C levels should magnify the reduction of atherosclerosis burden in the population. Finally, use of statins later in life can take advantage of their ability to markedly lower lifetime risk for ASCVD.
References
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation. and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106:3143–421.
Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, et al. National Heart, Lung, and Blood Institute; American College of Cardiology Foundation; American Heart Association. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227–39. (Review. Erratum. Circulation. 2004 Aug;110(6):763).
Cohen JC, Boerwinkle E, Mosley TH Jr, Hobbs HH. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N Engl J Med. 2006;354(12):1264–72.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934.
Rossouw JE, Lewis B, Rifkind BM. The value of lowering cholesterol after myocardial infarction. N Engl J Med. 1990;323(16):1112–9.
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383–89.
Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335(14):1001–09.
Post Coronary Artery Bypass Graft Trial Investigators. The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. N Engl J Med. 1997;336(3):153–62.
Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339(19):1349–57.
Serruys PW, de Feyter P, Macaya C, Kokott N, Puel J, Vrolix M, et al. Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002;287(24):3215–22.
Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebo-controlled trial. The Lancet. 2002;360(9326):7–22.
Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. The Lancet. 2002;360(9346):1623–30.
Holdaas H, Fellstrom B, Jardine AG, Holme I, Nyberg G, Fauchald P, et al. Effect of fluvastatin on cardiac outcomes in renal transplant recipients: a multicentre, ranomised, placebo-controlled trial. The Lancet. 2003;361(9374):2024–31.
Athyros VG, Papageorgiou AA, Mercouris BR, Athyrou VV, Symeonidis AN, et al. Treatment with atorvastatin to the National Cholesterol Educational Program goal versus ‘usual’ care in secondary coronary heart disease prevention. Curr Med Res Opin. 2002;18(4):220–28.
Cannon CP, Braunwald E, McCabe CH, et al. Comparison of intensive and moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–504.
Nissen SE, Tuzcu EM, Schoenhagen P, Brown BG, Ganz P, Vogen RA, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004;291(9):1071–80.
LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352(14):1425–35.
SEARCH investigators. Study of the effectiveness of additional reductions in cholesterol and homocysteine. http://www.ctsu.ox.ac.uk/projects/search.shtml. Accessed: 18. Sept. 2005.
Pedersen TR, Faergeman O, Holme I, Olsson AG, Tikkanen MJ. Effect of greater LDL-C reductions on prognosis: the Incremental Decrease in Endpoints through Aggressive Lipid Lowering (IDEAL) trial. Atherosclerosis. 1999;144:38.
Schwartz GG, Olsson AG, Ezekowitz MD, Ganz P, Oliver MF, Waters D, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study—a randomized controlled trial. JAMA. 2001;285(13):1711–18.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. The Lancet. 2003;361(9374):2005–16.
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. World Heart Federation and the Preventive Cardiovascular Nurses Association. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124(22):2458–73. (Epub 2011 Nov 3).
Catapano AL, Reiner Z, De Backer G, Graham I, Taskinen MR, Wiklund O, et al. European Society of Cardiology (ESC); European Atherosclerosis Society (EAS). ESC/EAS guidelines for the management of dyslipidaemias the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis. 2011;217(1):3–46.
Anderson TJ, Grégoire J, Hegele RA, Couture P, Mancini GB, McPherson R, et al. 2012 update of the Canadian cardiovascular society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2013;29(2):151–67.
Boekholdt SM, Arsenault BJ, Mora S, Pedersen TR, LaRosa JC, Nestel PJ, et al. Association of LDL cholesterol, non–HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins. JAMA. 2012;307(12):1302–9.
Boekholdt SM, Hovingh GK, Mora S, Arsenault BJ, Amarenco P, Pedersen TR, et al. Very low levels of atherogenic lipoproteins and risk of cardiovascular events; a meta-analysis of statin trials. In press JACC 2014.
Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61(4):427–36.
Barter PJ, Ballantyne CM, Carmena R, Castro Cabezas M, Chapman MJ, Couture P, et al. Apo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: report of the thirty-person/ten-country panel. J Intern Med. 2006;259(3):247–58.
Sniderman AD, Islam S, Yusuf S, McQueen MJ. Discordance analysis of apolipoprotein B and non-high density lipoprotein cholesterol as markers of cardiovascular risk in the INTERHEART study. Atherosclerosis. 2012;225(2):444–9.
Mora S, Glynn RJ, Boekholdt S, Nordestgaard BG, Kastelein JP, Ridker PM. On-treatment non–high-density lipoprotein cholesterol, apolipoprotein B, triglycerides, and lipid ratios in relation to residual vascular risk after treatment with potent statin therapy: JUPITER (Justification for the use of statins in prevention: an intervention trial evaluating rosuvastatin). J Am Coll Cardiol. 2012;59(17):1521–8.
Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, et al. American Diabetes Association; American College of Cardiology Foundation. Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care. 2008;31(15):811–22.
Kastelein JJ, van der Steeg WA, Holme I, Gaffney M, Cater NB, Barter P, et al. TNT Study Group; IDEAL Study Group. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation. 2008;117(23):3002–9.
Clarenbach JJ, Grundy SM, Palacio N, Vega GL. Relationship of apolipoprotein B levels to the number of risk factors for metabolic syndrome. J Investig Med. 2007;55(5):237–47.
Grundy SM, Vega GL, Tomassini JE, Tershakovec AM. Comparisons of apolipoprotein B levels estimated by immunoassay, nuclear magnetic resonance, vertical auto profile, and non-high-density lipoprotein cholesterol in subjects with hypertriglyceridemia (SAFARI Trial). Am J Cardiol. 2011;108(1):40–6.
Harper CR, Jacobson TA. Using apolipoprotein B to manage dyslipidemic patients: time for a change? Mayo Clin Proc. 2010;85(5):440–5.
Ray KK, Cannon CP, Cairns R, Morrow DA, Ridker PM, Braunwald E. Prognostic utility of apoB/AI, total cholesterol/HDL, non-HDL cholesterol, or hs-CRP as predictors of clinical risk in patients receiving statin therapy after acutecoronary syndromes: results from PROVE IT-TIMI 22. Arterioscler Thromb Vasc Biol. 2009;29(3):424–30.
Lipid Research Clinics Program. The lipid research clinics coronary primary prevention trial results. I. Reduction in incidence of coronary heart disease. JAMA. 1984;251:351–64.
Bays HE, Moore PB, Drehobl MA, Rosenblatt S, Toth PD, Dujovne CA, et al. Ezetimibe Study Group. Effectiveness and tolerability of ezetimibe in patients with primary hypercholesterolemia: pooled analysis of two phase II studies. ClinTher. 2001;23(8):1209–30. (Erratum in: ClinTher 2001 Sep;23(9):1601).
Hunninghake D, Insull W Jr, Toth P, Davidson D, Donovan JM, Burke SK. Coadministration of colesevelam hydrochloride with atorvastatin lowers LDL cholesterol additively. Atherosclerosis. 2001;158(2):407–16.
Leiter LA, Bays H, Conard S, Bird S, Rubino J, Hanson ME, et al. Efficacy and safety of ezetimibe added on to atorvastatin (40 mg) compared with uptitration of atorvastatin (to 80 mg) in hypercholesterolemic patients at high risk of coronary heart disease. Am J Cardiol. 2008;102(11):1495–501. (Epub 2008 Oct 23).
Califf RM, Lokhnygina Y, Cannon CP, Stepanavage ME, McCabe CH, Musliner TA, et al. An update on the IMProved reduction of outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) design. Am Heart J. 2010;159(5):705–9. (Epub 2010 Mar 15).
Canner PL, Berge KG, Wenger NK, Stamler J, Friedman L, Prineas RJ, et al. Fifteen year mortality in coronary drug project patients: long-term benefit with niacin. J Am Coll Cardiol. 1986;8(6):1245–55.
Canner PL, Furberg CD, Terrin ML, McGovern ME, et al. Benefits of niacin by glycemic status in patients with healed myocardial infarction (from the Coronary Drug Project). Am J Cardiol. 2005;95(2):254–7.
Brown BG, Zhao XQ. Nicotinic acid, alone and in combinations, for reduction of cardiovascular risk. Am J Cardiol. 2008;101(8A):58B–62B.
Taylor AJ, Lee HJ, Sullenberger LE. The effect of 24 months of combination statin and extended-release niacin on carotid intima-media thickness: ARBITER 3. Curr Med Res Opin. 2006;22(11):2243–50.
AIM-HIGH Investigators, Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255–67.
Cuchel M, Bloedon LT, Szapary PO, Kolansky DM, Wolfe ML, Sarkis A, et al. Inhibition of microsomal triglyceride transfer protein in familial hypercholesterolemia. N Engl J Med. 2007;356(2):148–56.
Stein EA, Dufour R, Gagne C, Gaudet D, East C, Donovan JM, et al. Apolipoprotein B synthesis inhibition with mipomersen in heterozygous familial hypercholesterolemia: results of a randomized, double-blind, placebo-controlled trial to assess efficacy and safety as add-on therapy in patients with coronary artery disease. Circulation. 2012;126(19):2283–92. (Epub 2012 Oct 11).
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, et al. ILLUMINATE Investigators. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357(21):2109–22. (Epub 2007 Nov 5.)
Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. dal-OUTCOMES Investigators. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–99. (Epub 2012 Nov 5).
Cannon CP, Shah S, Dansky HM, Davidson M, Brinton EA, Gotto AM, et al. Determining the Efficacy and Tolerability Investigators. Safety of anacetrapib in patients with or at high risk for coronary heart disease. N Engl J Med 2010;363(25):2406–15. (Epub 2010 Nov 17).
Horton JD, Cohen JC, Hobbs HH. PCSK9: a convertase that coordinates LDL catabolism. J Lipid Res. 2009;50 Suppl:S172–7. Epub 2008 Nov 19.
Lo Surdo PB, Pandit S, et al. Mechanistic implications for LDL receptor degradation from the PCSK9/ LDLR structure at neutral pH. EMBO Rep. 2011;12(12):1300–5.
Cohen JC. Emerging LDL therapies: using human genetics to discover new therapeutic targets for plasma lipids. J Clin Lipidol. 2013;7(3 Suppl):S1–5. (Epub 2013 Mar 26).
Benn M, Nordestgaard BG, Grande P, Schnohr P, Tybjaerg-Hansen A. PCSK9 R46L, low-density lipoprotein cholesterol levels, and risk of ischemic heart disease: 3 independent studies and meta-analyses. J Am Coll Cardiol. 2010;55(25):2833–42. Review.
Stein EA, Gipe D, Bergeron J, Gaudet D, Weiss R, Dufour R, et al. Effect of a monoclonal antibody to PCSK9, REGN727/SAR236553, to reduce low-density lipoprotein cholesterol in patients with heterozygous familial hypercholesterolaemia on stable statin dose with or without ezetimibe therapy: a phase 2 randomised controlled trial. Lancet. 2012;380(9836):29–36. (Epub 2012 May 26).
Roth EM, McKenney JM, Hanotin C, Asset G, Stein EA. Atorvastatin with or without an antibody to PCSK9 in primary hypercholesterolemia. N Engl J Med. 2012;367(20):1891–900. (Epub 2012 Oct 31).
Grundy SM, Vega GL. Fibric acids: effects on lipids and lipoprotein metabolism. Am J Med. 1987;83(5B):9–20.
Jun M, Foote C, Lv J, Neal B, Patel A, Nicholls SJ, et al. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. The Lancet. 2010;375(9729):1875–84.
Lee M, Saver JL, Towfighi A, Chow J, Ovbiagete B. Efficacy of fibrates for cardiovascular risk reduction in persons with atherogenic dyslipidemia: a meta-analysis. Atherosclerosis. 2011;217(2):492–8.
Guo J, Meng F, Ma N, Li C, Ding Z, Wang H, et al. Meta-analysis of safety of the coadministration of statin with fenofibrate in patients with combined hyperlipidemia. Am J Cardiol. 2012;110(9):1296–301. (Epub 2012 Jul 27).
D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM. General cardiovascular risk profile for use in primary care. The Framingham heart study. Circulation. 2008;117(6):743–53.
Tattersall MC, Karmali KN, Gangnon RE, Keevil JG. The population effects of the global cardiovascular risk model in United States adults: findings from the National Health and Nutrition Surveys, 2005–2006. J Clin Lipidol. 2011;5(3):166–72. (Epub 2011 Mar 2).
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB Sr, Gibbons R, et al. 2013 ACC/AHA Guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2013 [Epub ahead of print).
Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. The Lancet. 2013;382(9907):1762–5.
Eichler K, Puhan MA, Steurer J, Bachmann LM. Prediction of first coronary events with the Framingham score: a systematic review. Am Heart J. 2007;153(5):722–31.
Marrugat J, D’Agostino R, Sullivan L, Elosua R, Wilson P, Ordovas J, et al. An adaptation of the Framingham coronary heart disease risk function to European Mediterranean areas. J Epidemiol Community Health. 2003;57(8):634–8.
Marques-Vidal P, Rodondi N, Bochud M, Pecoud A, Hayoz D, Paccaud F, et al. Predictive accuracy of original and recalibrated Framingham risk score in the Swiss population. Int J Cardiol. 2009;133(4):346–53.
Brindle P, Emberson J, Lampe F, Walker M, Whincup P, Fahey T, et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ. 2003;327(7426):1267.
Menotti A, Puddu PE, Lanti M. Comparison of the Framingham risk function-based coronary chart with risk function from an Italian population study. Eur Heart J. 2000;21(5):365–70.
Laurier D, Nguyen PC, Cazelles B, Segond P. Estimation of CHD risk in a French working population using a modified Framingham model. The PCV-METRA Group. J Clin Epidemiol. 1994;471(12):1353–64.
Hense HW, Schulte H, Lowel H, Assman G, Keil U. Framingham risk function overestimates risk of coronary heart disease in men and women from Germany—results from the MONICA Augsburg and the PROCAM cohorts. Eur Heart J. 2003;24(10):937–45.
Lloyd-Jones DM, Wilson PW, Larson MG, Beiser A, Leip EP, D’Agostino RB, et al. Framingham risk score and prediction of lifetime risk for coronary heart disease. Am J Cardiol. 2004;94(1):20–4.
Pencina MJ, D’Agostino RB, Beiser AS, Cobain MR, Vasan RS. Estimating lifetime risk of developing high serum total cholesterol: adjustment for baseline prevalence and single-occasion measurements. Am J Epidemiol. 2007;165(4):464–72. (Epub 2006 Nov 20).
Pencina MJ, D’Agostino RB Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2009;119(24):3078–84. Epub 2009.
Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321–9.
Hippisley-Cox J, Coupland C, Robson J, Brindle P. Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using Q Research database. BMJ. 2010;341:c6624.
Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. The Lancet. 1999;353(16):89–92.
Lloyd-Jones DM, Wilson PW, Larson MG, Leip E, Beiser A, D’Agostino RB, et al. Lifetime risk of coronary heart disease by cholesterol levels at selected ages. Arch Intern Med. 2003;163(16):1966–72.
Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113(6):791–8. (Epub 2006 Feb 6).
Lloyd-Jones DM, Dyer AR, Wang R, Daviglus ML, Greenland P. Risk factor burden in middle age and lifetime risks for cardiovascular and non-cardiovascular death (Chicago Heart Association Detection Project in Industry). Am J Cardiol. 2007;99(4):535–40.
Marma AK, Berry JD, Ning H, Persell SD, Lloyd-Jones DM. Distribution of10-year and lifetime predicted risks for cardiovascular disease in US adults: findings from the National Health and Nutrition Examination Survey 2003–2006. Circ Cardiovasc Qual Outcomes. 2010;3(1):8–14.
Allen N, Berry JD, Ning H, Van Horn L, Dyer A, Lloyd-Jones DM. Impact of blood pressure and blood pressure change during middle age on the remaining lifetime risk for cardiovascular disease: the cardiovascular lifetime risk pooling project. Circulation. 2012;125(1):37–44.
Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308(17):1795–801.
Karmali KN, Lloyd-Jones DM. Adding a life-course perspective to cardiovascular-risk communication. Nat Rev Cardiol. 2013;10(2):111–5. (Epub 2013 Jan 8).
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, Brindle P. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336(7659):1475–82. (Epub 2008 Jun 23).
Collins GS, Altman DG. Predicting the 10 year risk of cardiovascular disease in the United Kingdom: independent and external validation of an updated version of QRISK2. BMJ. 2012;344:e4181.
Expert Dyslipidemia Panel of the International Atherosclerosis Society Panel members. An international atherosclerosis society position paper: global recommendations for the management of dyslipidemia–full report. J Clin Lipidol. 2014;8(1):29–60.
Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/ AHA Writing Committee to Update the 2000 expert consensus document on electron beam computed tomography); society of atherosclerosis imaging and prevention; society of cardiovascular computer tomography. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography). Circulation. 2007;115(3):402–26. (Epub 2007 Jan 12).
Rumberger JA, Schwartz RS, Simons DB, Sheedy PF III, Edwards WD, Fitzpatrick LA. Relation of coronary calcium determined by electron beam computed tomography and lumen narrowing determined by autopsy. Am J Cardiol. 1994;73(16):1169–73.
Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92(8):2157–62.
Budoff MJ, Georgiou D, Brody A, Agatston AS, Kennedy J, Wolfkiel C, et al. Ultrafast computed tomography as a diagnostic modality in the detection of coronary artery disease: a multicenter study. Circulation. 1996;93(5):898–904.
Guerci AD, Spadaro LA, Popma JJ, Goodman KJ, Brundage BH, Budoff M, et al. Relation of coronary calcium score by electron beam computed tomography to arteriographic findings in asymptomatic and symptomatic adults. Am J Cardiol. 1997;79(2):128–33.
Schmermund A, Baumgart D, Gorge G, Gronemeyer D, Seibel R, Bailey KR, Rumberger JA, Paar D, Erbel R. Measuring the effect of risk factors on coronary atherosclerosis: coronary calcium score versus angiographic disease severity. J Am Coll Cardiol. 1998;31(6):1267–73.
Grundy SM. Age as a risk factor: you are as old as your arteries. Am J Cardiol. 1999;83(10):1455–7.
McClelland RL, Nasir K, Budoff M, Blumenthal RS, Kronmal RA. Arterial age as a function of coronary artery calcium (from the Multi-Ethnic Study of Atherosclerosis [MESA]). Am J Cardiol. 2009;103(1):59–63.
O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular health study collaborative research group. N Engl J Med. 1999;340(1):14–22.
Lowe GD, Danesh J. The need for risk factor assessment in atherothrombotic vascular disease. Semin Vasc Med. 2002;2(3):231–2.
Ridker PM, Paynter NP, Rifai N, Gaziano JM, Cook NR. C-reactive protein and parental history improve global cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation. 2008;118(22):2243–51.
Cook NR, Paynter NP, Eaton CB, Manson JE, Martin LW, Robinson JG, et al. Comparison of the Framingham and Reynolds Risk scores for global cardiovascular risk prediction in the multiethnic Women’s Health Initiative. Circulation. 2012;125(14):1748–56.
Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49(4):403–14.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–207.
Ginsberg HN. The 2013 ACC/AHA guidelines on the treatment of blood cholesterol. Questions, questions, questions. Circ Res. 2014;114(5):761–4.
Anderson TJ, Grégoire J, Hegele RA, Couture P, Mancini GB, McPherson R, et al. Are the ACC/AHA Guidelines on the treatment of blood cholesterol a game changer? A perspective from the canadian cardiovascular society dyslipidemia panel. Can J Cardiol. 2014;30(4):37–80.
Raymond C, Cho L, Rocco M, Hazen SL. New cholesterol guidelines: worth the wait? Cleve Clin J Med. 2014;81(1):11–9.
Breslow JL. Perspective on the 2013 American Heart Association/American College of Cardiology Guideline for the use of statins in primary prevention of low-risk individuals. Circ Res. 2014;114(5):758–60.
The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart disease. JAMA. 1984;251(13):351–64.
The Lipid Research Clinics Coronary Primary Prevention Trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984;251(3):365–74.
Canner PL, Berge KG, Wenger NK, Stamler J, Friedman L, Prineas RJ, et al. Fifteen year mortality in Coronary drug project patients: long-term benefit with niacin. J Am Coll Cardiol. 1986;8(6):1245–55.
Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, Huttunen JK, Kaitaniemi P, Koskinen P, Manninen V, et al. Helsinki heart study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987;317(20):1237–45.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Humana Press
About this chapter
Cite this chapter
Grundy, S. (2015). Perspectives on Cholesterol Guidelines. In: Garg, A. (eds) Dyslipidemias. Contemporary Endocrinology. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-60761-424-1_18
Download citation
DOI: https://doi.org/10.1007/978-1-60761-424-1_18
Published:
Publisher Name: Humana Press, Totowa, NJ
Print ISBN: 978-1-60761-423-4
Online ISBN: 978-1-60761-424-1
eBook Packages: MedicineMedicine (R0)