Abstract
Ultrasound is established as a screening method in the patient at high risk for hepatocellular carcinoma. US detection of a nodule in such a patient is frequently followed by contrast-enhanced ultrasound (CEUS) performed with the addition of a microbubble contrast agent. This allows for the evaluation of the mass in a similar manner to that on CT and MR scan where liver mass diagnosis is based on the enhancement characteristics of the mass in the arterial and portal venous phases. CEUS plays an integral role with CT and MR scan in the evaluation of the patient at risk for hepatoma. The classic enhancement characteristics of arterial phase hypervascularity and portal phase washout are shown in the majority of patients. However, well recognized is arterial phase hypovascularity and lack of washout in the portal phase especially in well-differentiated tumors. The real-time nature of CEUS gives it a unique role in the evaluation of small tumors in particular. Its versatility of performance is also invaluable for monitoring RFA and showing response to therapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Key Words
14.1 Introduction
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy. The majority of HCCs occur on a background of liver cirrhosis and it is now well recognized that HCCs commonly develop through a multi-step carcinogenesis from low-grade dysplastic nodule (DN), high-grade DN, well-differentiated HCC to classic advanced HCC ( 1 , 2 ). The change of histologic types of the nodule is believed to be sequential; however, the distinctions between each step are not always clear even on histopathology, which suggests a continuous transition ( 1 ). HCCs may also arise de novo from a relatively normal liver without a background of RN or DN, especially in non-Asian populations ( 3 ). The early diagnosis of HCC is important since the treatment is most effective when the tumor is small.
Detection and characterization of HCC is one of the major roles of imaging diagnosis in high-risk patients. Imaging diagnosis of HCC is primarily based on sequential changes in the intranodular blood supply during the hepatocarcinogenesis; RN show similar blood supply to normal liver, borderline lesions show wide variations of blood supply, and typical HCCs are supplied by abnormal arteries alone ( 4 ). Over the last few decades there has been remarkable progress of imaging techniques for diagnosing HCC. The improvement of gray-scale ultrasound (US) scan enables us to detect subcentimeter lesions in the liver. Recent fast computed tomography (CT) and magnetic resonance (MR) scanners provide multi-phasic contrast-enhanced imaging, which has become an integral part of imaging of HCC. Arterial phase (AP) imaging is extremely important to detect and characterize focal liver lesions in a cirrhotic liver. Worldwide, US scan is most commonly used as a screening test for HCC in high-risk patients ( 5 ). Multi-phasic contrast-enhanced CT and MR scans are usually performed when there is any focal lesion suspected to be HCC on US or there is a strong clinical suspicion of HCC. However, the pattern of the use of imaging tests is variable depending on each institutional preference. Clinical use of microbubble contrast agents has expanded the role of US from that of detection to one-stop characterization of HCC based on the enhancement features at contrast-enhanced US (CEUS) ( 6–13 ). Current low-mechanical index (MI) techniques for CEUS using second-generation microbubble agents have further advantages in characterizing HCC, including real-time demonstration of continuous hemodynamic changes in both the liver and the liver lesion. In our institution, US scan is used as a routine screening/surveillance imaging test for high-risk patients for HCC, and CT/MR scan and/or CEUS is performed to characterize any focal lesions detected on US scan. A large number of CEUS examinations are also performed to characterize small indeterminate focal liver lesions seen on CT or MR scans, producing satisfactory results. We have recently developed a systematic imaging work-up algorithm to evaluate newly detected liver nodules in screening/surveillance imaging examinations based on the American Association for the Study of Liver Diseases (AASLD) guidelines ( 5 ). The algorithm includes performance of CEUS, CT, and MR in all newly detected 10–20 mm nodules and is well received by referring hepatologists.
Although recent progress of imaging techniques improves the sensitivity to detect HCC, it also reveals a large number of pseudolesions and benign tumors that can mimic the appearance of HCC ( 15 ). These lesions can alter the management of the patient, potentially preventing curative surgery. It is, therefore, critical to achieve noninvasive characterization of focal liver lesions with reasonable imaging criteria and adequate additional or follow-up imaging studies. Unfortunately, there are significant overlaps between the imaging findings of benign and malignant liver lesions in cirrhotic livers.
In this chapter, we review the typical US and CEUS imaging features of HCC and other cirrhosis-related nodules. We focus, in particular, on the issue of characterization of small liver lesions in the cirrhotic liver. We also discuss the role of US and CEUS in routine screening/surveillance of HCC in high-risk patients and in monitoring therapeutic responses to local ablation therapy or anti-angiogenic agents.
14.2 Gray-Scale and Doppler Ultrasound
Liver cirrhosis is a diffuse process of alteration of the normal liver architecture into fibrosis with development of regenerating nodules (RN) throughout the liver. RN do not usually stand out on imaging, but may be seen as ill-defined tiny nodules within a diffusely coarse liver parenchyma on US scan.
Dysplastic nodules (DN) demonstrate variable echogenicity patterns, including hyperechoic, isoechoic, and hypoechoic. Hyperechogenicity is related to the fatty metamorphosis that may be seen in DN ( 15 ). The internal architecture of DN is usually homogeneous; however, it is impossible to differentiate DN from small HCC by gray-scale US findings alone.
HCC may grow as solitary or multiple discrete nodules or show as an ill-defined infiltrative mass. It is usually easy to make a diagnosis of HCC when the tumor is large if expansive or advanced infiltrative tumors are shown. Expansive HCCs are well demarcated, nodular, and frequently encapsulated (Fig. 1). On the other hand, infiltrative HCCs have irregular and indistinct margins (Fig. 2) with frequent invasion of the portal veins or hepatic veins ( 2 ). A mixed expansive and infiltrative growth pattern is not uncommon. Expansive HCCs usually have a better prognosis and better response to treatment.
Infiltrative HCC in a 49-year-old man with hepatitis B. (a) US image shows an ill-defined hypoechoic mass (arrows) in the liver. (b) CEUS scan in the arterial phase at 10 s after injection of the contrast material shows diffuse hypervascularity within the mass with an irregular margin. (c) CEUS image at 134 s after injection of the contrast material shows negative enhancement (washout) of the mass relative to the liver. (d) CT image in the arterial phase shows a hyperenhancing mass with an irregular margin. (e) The mass shows washout in the portal venous phase.
HCCs have variable echogenicity on gray-scale ultrasound. Small tumors without fatty metamorphosis are usually hypoechoic, but the echo pattern changes as the size increases. Small HCCs with fatty metamorphosis typically show hyperechogenicity, potentially mimicking the appearance of hemangioma on gray-scale US ( 16 ). With time and increasing size, the masses tend to become more complex and inhomogeneous as a result of necrosis. HCC with expansive growth is usually seen as a discrete nodule with heterogeneous echo texture and frequently has a hypoechoic peripheral halo which corresponds to a fibrous pseudocapsule (Fig. 1) ( 17 ). An uncommon but characteristic appearance of HCC is a nodule-in-nodule pattern which represents a focus of HCC within a DN or areas of different degrees of differentiation of HCC. In contrast, infiltrative HCC appears as an area with heterogeneous echogenicity and can be easily overlooked on an US scan. It is important to carefully evaluate portal or hepatic vein branches within any suspicious heterogeneous area because tumor thrombosis is frequently associated with infiltrative HCC (Fig. 3). Intratumoral fat also occurs in larger HCC. Because it tends to be focal, however, it is unlikely to cause confusion in diagnosis. Rare surface lesions may present with spontaneous rupture and hemoperitoneum.
Infiltrative HCC with right hepatic vein thrombosis in a 42-year-old man with hepatitis B. (a) US image shows an ill-defined slightly hyperechoic area (arrows) in the liver. There is a focal thrombosis (long arrow) in the right hepatic vein. (b) CEUS image in the arterial phase at 9 s shows heterogeneous hypervascularity of the lesion with linear enhancing structures along the course of right hepatic vein thrombosis (arrows). (c) CEUS image at 247 s shows washout of the mass and right hepatic vein thrombus (arrows).
Fibrolamellar carcinoma is a histologic subtype of HCC that is found in younger patients (adolescents and young adults) without coexisting liver disease. The serum α-fetoprotein levels are usually normal. The tumors are usually well differentiated, often encapsulated by fibrous tissue and solitary. The prognosis is generally better for fibrolamellar carcinoma compared with typical HCC. Most patients, however, demonstrate advanced disease at the time of diagnosis ( 18 ). The echogenicity of fibrolamellar carcinoma is variable. Punctuate calcification and a central echogenic scar—features which are distinctly unusual in HCC—are more common in the fibrolamellar subtype.
Color or power Doppler US scan typically shows high-velocity arterial flow within large HCC (Fig. 4). A pattern analysis of the distribution of intratumoral flow might be helpful to suggest the diagnosis of HCC (19–21); however, it is rarely specific and requires a further imaging test for confirmation. Doppler is excellent for detecting neovascularity within tumor thrombi in the portal veins, diagnostic of hepatocellular carcinoma even in the absence of demonstration of the parenchymal lesion (Fig. 5).
14.3 Contrast-Enhanced Ultrasound
14.3.1 Techniques
US contrast agents, which are presently used in radiology, consist of microbubbles of perfluorocarbon gas stabilized by a protein, lipid, or polymer shell. The bubbles are sufficiently small and stable to traverse the pulmonary and cardiac circulations following peripheral venous injection. The bubbles disappear as the gas diffuses through the thin shell, with a typical half-life of a few minutes in blood. In our experience with more than 4,000 injections, patient acceptance has been very high, with no serious adverse events seen at our institutions. A large retrospective study from Europe using a slightly different type of microbubble contrast agent reported 0.0086% incidence of serious adverse events without any fatality among 23,188 examinations ( 22 ). The bubbles are approximately the same size as red blood cells and cannot move through the vascular endothelium into the interstitium, even after an extended period of time; therefore, they are true blood pool agents ( 23 ). Microbubble contrast agents are approved for radiologic use in many countries, including the European Union, Canada, and many Asian countries. Although US contrast material has been approved for clinical use for cardiac diagnosis in the United States for a number of years, its use for radiologic indications is still under investigation at the time of writing this chapter.
A contrast-specific imaging mode, such as pulse inversion technology, is available on all high-end US systems and is essential for the visualization of microbubbles. The use of low-mechanical index (MI) imaging is critical for continuous, real-time evaluation of enhancement. Typically, the contrast agent is injected manually through a three-way stopcock, followed by a 5-mL saline solution flush. Low-MI continuous imaging is performed during the arterial and portal venous phases. Slightly higher MI and larger amounts of microbubbles can be used for deep-seated lesions or lesions within an attenuating liver. The first injection usually includes a stationary field of view to include the lesion of interest and adjacent liver, both observed continuously for 4–5 min. Subsequent injections concentrate on arterial phase vessel morphology and enhancement as well as sweeps of the entire liver in the portal venous phase to look for any further abnormalities. Injections are typically repeated two to five times to obtain images for the same lesion or to evaluate a different lesion. Each injection is separated by 3–5 min. A simultaneous dual-imaging mode, which displays gray-scale imaging and contrast-specific imaging side-by-side, is available on most updated ultrasound scanners. The dual-imaging mode is particularly useful to evaluate small liver nodules. A flash-replenishment technique in conjunction with real-time maximum intensity processing is useful to characterize vascular patterns and morphology of the vessels in the arterial phase ( 24 ).
14.3.2 Differential Diagnosis of Nodules in Liver Cirrhosis
Presently, the evaluation of the blood supply in a hepatocellular nodule is the single most important imaging parameter to characterize nodules in liver cirrhosis, because there are sequential changes in the supplying vessels and hemodynamic state during hepatocarcinogenesis ( 25 ). Clinical use of microbubble contrast agents enables US to characterize HCC based on the enhancement features. Current real-time low-MI imaging techniques with second-generation contrast agents have remarkably improved the capability of CEUS in the characterization of HCC and their differentiation from various nodules related to cirrhosis. It is now feasible to focus on a small indeterminate nodule from wash-in to washout of contrast and CEUS can provide better understanding of complex hemodynamic changes of a nodule and a cirrhotic liver.
Classic HCCs are typically supplied by abnormal arteries alone and show positive enhancement during the hepatic arterial phase and negative enhancement (washout) during the portal venous phase ( 11–13 ). There are irregular dysmorphic arteries within the tumor often visualized in large HCC in the early arterial filling phase (Fig. 6). Detection of arterial hypervascularity is very important to make a diagnosis of HCC as it is one of the most reliable characteristics of nodular HCC. However, there is a small subset of HCC with no arterial hypervascularity, including particularly those that are well differentiated ( 26 ). CEUS is also excellent in the differentiation between tumor thrombosis and benign thrombosis in the portal vein. Tumor thrombi invariably show heterogeneous enhancement and linear, irregular feeding vessels after injection of the microbubbles (Fig. 7) whereas benign thrombi are avascular.
Typical HCC in a 38-year-old man with autoimmune hepatitis. (a) US image shows a large well-defined hypoechoic mass (arrows) in the liver. (b) CEUS scan in the arterial phase at 6 s shows dysmorphic arteries within the mass. (c) CEUS scan at 12 s shows homogeneous enhancement of the mass with small non-enhancing necrotic areas. (d) CEUS image at 69 s shows slight washout of the mass relative to the liver. (e) The mass shows clear washout at 144 s after injection.
HCC with portal vein thrombosis in a 58-year-old man with hepatitis C. (a) US image shows an expanding thrombosis in the right portal vein (arrows). (b) CEUS image in the arterial phase at 6 s shows linear arteries along the thrombosed portal vein branching into the tumor thrombi (arrows). (c) CEUS image at 14 s shows homogeneous enhancement of the mass and tumor thrombi (arrows) in the right portal vein. (d) CEUS image at 86 s shows washout of the mass and right portal vein thrombi (arrows) relative to the liver.
Negative enhancement or ‘washout’ during the venous phase is also an important characteristic of HCC as typical tumors lack portal venous supply. The intensity of enhancement of HCC in the portal venous phase, however, generally decreases more slowly than that in a metastasis. In our study of 115 hypervascular HCC ( 26 ), only 50% showed the expected portal phase washout by 90 s. Extended evaluation over 3 min is important to characterize HCC by demonstrating ‘eventual’ washout (Fig. 8). Further, sustained positive enhancement in the extended portal phase should not be considered diagnostic of a benign lesion, especially in patients at risk for HCC since it may occur in well-differentiated HCC (Fig. 9).
HCC with late washout in an 85-year-old man with hepatitis C. (a) US image shows a hypoechoic mass (arrows) in the liver. (b) CEUS scan in the arterial phase at 8 s shows heterogeneous hypervascularity of the mass (arrows). (c) CEUS image at 133 s shows isoechogenicity of the mass (arrows) relative to the liver. (d) CEUS image at 213 s shows washout of the mass (arrows).
HCC with no washout in a 61-year-old man with hepatitis B. (a) US image shows a hypoechoic nodule (arrows) in the liver. (b) CEUS scan in the arterial phase at 21 s shows homogeneous hypervascularity of the nodule (arrows). (c) CEUS image at 218 s shows persistent hyperechogenicity of the nodule (arrows) relative to the liver.
Most RN are isoechoic to the parenchyma during all phases on CEUS (Fig. 10), although they may show transient hypovascularity in the arterial phase. As DN have more histological atypia, abnormal arteries increase while normal arterial and portal supply decrease. The arterial and portal supplies to DN are variable and inconsistent (Fig. 11) ( 27 ). Moreover, there are significant overlaps of vascular supply between DN and well-differentiated HCC. CEUS, CT, and MR all suffer from similar problems in the imaging of these nodules. CEUS may have advantages from continuous observation in detecting subtle vascular differences of HCC from DN.
Regenerative nodule in a 52-year-old man with hepatitis B. (a) US image shows a hypoechoic nodule (arrows) in the liver. (b–d) The nodule is not visualized on CEUS scans at 22 s (b), 31 s (c), and 113 s (d) after injection of the contrast material because of isoechogenicity of the relative to the liver.
Dysplastic nodule in a 49-year-old woman with hepatitis B. (a) US image shows a hypoechoic nodule (arrows) in the liver. (b) CEUS image in the arterial phase at 10 s shows hypovascularity of the nodule (arrows) relative to the liver. (c) The nodule is not visualized on CEUS scan at 168 s because of isoechogenicity.
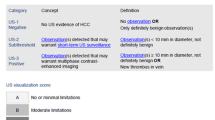
14.3.3 Role of US and CEUS in HCC Surveillance
Surveillance for HCC in high-risk patients is widely practiced particularly in endemic regions such as East Asia. A recent practice guideline for the management of HCC by the American Association for the Study of Liver Diseases (AASLD) recommended that surveillance for HCC should be performed using US at 6–12 month intervals ( 5 ). Traditionally, the diagnostic confirmation of HCC was made by tumor biopsy. However, there is a recent trend to diagnose typical cases of HCC based on imaging and clinical findings without biopsy. For example, the AASLD guideline recommended that the diagnosis of HCC can be made without biopsy in patients with cirrhosis with typical enhancement patterns of HCC on one dynamic contrast-enhanced imaging technique for lesions larger than 2 cm and on two dynamic imaging studies, including multi-phasic contrast-enhanced CT, MR, or CEUS, for lesions between 1 and 2 cm ( 5 ). This guideline defines typical enhancement pattern of HCC as hypervascularity of the lesion in the arterial phase and negative enhancement (washout) of the lesion relative to the hepatic parenchyma in the portal venous or delayed phase.
The University Health Network in Toronto recently developed a systematic imaging work-up protocol for newly detected nodules on surveillance US. Our experience for the initial 2 years shows that surveillance US is able to detect small lesions (<2 cm) in the majority of cases, and a multi-modality imaging approach with contrast-enhanced CT, MR, and CEUS provides an excellent diagnostic ability to characterize typical HCC even if they are smaller than 2 cm. However, there are still considerable numbers of indeterminate lesions in 1–2 cm nodules requiring biopsy. Our experience also shows that about one-fourth of newly detected lesions are hemangiomas and those cases are easily characterized by CEUS at the time of detection, preventing extensive imaging work-up, additional hospital visits, and invasive procedures (Fig. 12). Real-time CEUS is excellent in the characterization of hemangiomas, regardless of the rapidity of the enhancement ( 28 ).
Hemangioma in a 52-year-old woman with hepatitis C. (a) US image shows a slightly hypoechoic nodule (arrows) in the liver. (b–d) CEUS images at 6 s (b), 7 s (c), and 10 s (d) after injection of the contrast material show peripheral nodular enhancement of the nodule (arrows) with subsequent central fill-in. The nodule shows homogeneous hyperechogenicity at 10 s (d).
14.3.4 Post-treatment Monitoring of HCC
Radiofrequency ablation (RFA) has become one of the main treatment modalities for patients with small HCC. Real-time gray-scale US scan is most frequently used for the guidance for RFA procedure; however, there are uncommon cases with poor visibility on US scan. CEUS can be extremely helpful to localize the lesion by demonstrating the arterial phase hypervascularity and washout in the portal venous phase. The use of dual-imaging mode, which displays gray-scale imaging and contrast-specific imaging side-by-side, is critical to visualize the lesion and the needle simultaneously. A routine use of pre-procedure CEUS can reduce the number of incomplete or erroneous RFA significantly.
On the other hand, an accurate assessment of the RFA therapeutic response is crucial because a complete tumor ablation significantly improves patient survival, whereas residual or recurrent HCC may immediately require an additional treatment. CEUS can be applied immediately after RFA procedure so that repeated RFA can be carried out immediately after the procedure in the same treatment session if residual enhancing tumor is found ( 29, 30 ). Contrast-enhanced CT or MR imaging is most commonly used for interval post-RFA monitoring, but CEUS can be used as a useful alternative or a problem-solving method when CT or MR imaging is not conclusive. On CEUS, successful treatment means complete avascularity within the treated HCC. Any intratumoral enhancement indicates residual viable HCC and requires additional RFA procedure (Fig. 13). Benign perfusion abnormalities adjacent to the ablation zone are frequently seen and may persist several months after RFA procedure. It is, therefore, important to define the outer border of the pre-existing tumor and assess any enhancing area within the border. Ill-defined hypervascular areas outside the border usually represent benign perfusion abnormalities and these areas do not show washout in the portal venous phase.
Residual viable tumor after radiofrequency ablation for HCC in a 54-year-old woman with hepatitis B. (a) US image shows a hypoechoic mass (arrows) which has been treated with radiofrequency ablation. (b) CEUS image in the arterial phase at 11 s shows an eccentric intratumoral area of hypervascularity (arrows), representing residual viable tumor. (c) The intratumoral enhancing area (arrows) shows washout at 59 s.
14.4 Conclusion
Recent advances in liver imaging techniques and better understanding of imaging findings have facilitated the detection and characterization of hepatocellular nodules in a cirrhotic liver. It is important to recognize that various types of benign nodules and pseudolesions are identified on all imaging scans performed for the diagnosis of HCC. An accurate differentiation between them is critical for adequate management of patients with cirrhosis. Unfortunately, any of the imaging tests and even percutaneous biopsy is not diagnostic for borderline lesions. Intimate collaboration of hepatologists, pathologists, surgeons, and radiologists with reasonable imaging and clinical criteria estimating the degree of malignancy is imperative.
References
Choi BI, Takayasu K, Han MC. Small hepatocellular carcinomas and associated nodular lesions of the liver: pathology, pathogenesis, and imaging findings. AJR Am J Roentgenol 1993;160:1177–1187.
Kim TK, Jang HJ, Wilson SR. Imaging diagnosis of hepatocellular carcinoma with differentiation from other pathology. Clin Liver Dis 2005;9:253–279.
Freeny PC, Baron RL, Teefey SA. Hepatocellular carcinoma: reduced frequency of typical findings with dynamic contrast-enhanced CT in a non-Asian population. Radiology 1992;182:143–148.
Matsui O. Detection and characterization of hepatocellular carcinoma by imaging. Clin Gastroenterol Hepatol 2005;3:S136–140.
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology 2005;42:1208–1236.
Choi BI, Kim TK, Han JK, Kim AY, Seong CK, Park SJ. Vascularity of hepatocellular carcinoma: assessment with contrast-enhanced second-harmonic versus conventional power Doppler US. Radiology 2000;214:381–386.
Dill-Macky MJ, Burns PN, Khalili K, Wilson SR. Focal hepatic masses: enhancement patterns with SH U 508A and pulse-inversion US. Radiology 2002;222:95–102.
Jang HJ, Kim TK, Wilson SR. Imaging of malignant liver masses: characterization and detection. Ultrasound Q 2006;22:19–29.
Kim TK, Choi BI, Han JK, Hong HS, Park SH, Moon SG. Hepatic tumors: contrast agent-enhancement patterns with pulse-inversion harmonic US. Radiology 2000;216:411–417.
Kim AY, Choi BI, Kim TK, Han JK, Yun EJ, Lee KY, Han MC. Hepatocellular carcinoma: power Doppler US with a contrast agent – preliminary results. Radiology 1998;209:135–140.
Nicolau C, Catala V, Vilana R, Gilabert R, Bianchi L, Sole M, Pages M, et al. Evaluation of hepatocellular carcinoma using SonoVue, a second generation ultrasound contrast agent: correlation with cellular differentiation. Eur Radiol 2004;14:1092–1099.
Quaia E, Calliada F, Bertolotto M, Rossi S, Garioni L, Rosa L, Pozzi-Mucelli R. Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology 2004;232:420–430.
Wilson SR, Burns PN. An algorithm for the diagnosis of focal liver masses using microbubble contrast-enhanced pulse-inversion sonography. AJR Am J Roentgenol 2006;186:1401–1412.
Kim TK, Choi BI, Han JK, Chung JW, Park JH, Han MC. Nontumorous arterioportal shunt mimicking hypervascular tumor in cirrhotic liver: two-phase spiral CT findings. Radiology 1998;208:597–603.
Kim MJ, Lim JH, Lee SJ, Kim SH, Lee WJ, Lim HK, Park JM, et al. Correlation between the echogenicity of dysplastic nodules and their histopathologically determined fat content. J Ultrasound Med 2003;22:327–334.
Caturelli E, Pompili M, Bartolucci F, Siena DA, Sperandeo M, Andriulli A, Bisceglia M. Hemangioma-like lesions in chronic liver disease: diagnostic evaluation in patients. Radiology 2001;220:337–342.
Choi BI, Kim CW, Han MC, Kim CY, Lee HS, Kim ST, Kim YI. Sonographic characteristics of small hepatocellular carcinoma. Gastrointest Radiol 1989;14:255–261.
Stevens WR, Johnson CD, Stephens DH, Nagorney DM. Fibrolamellar hepatocellular carcinoma: stage at presentation and results of aggressive surgical management. AJR Am J Roentgenol 1995;164:1153–1158.
Tanaka S, Kitamura T, Fujita M, Nakanishi K, Okuda S. Color Doppler flow imaging of liver tumors. AJR Am J Roentgenol 1990;154:509–514.
Choi BI, Kim TK, Han JK, Chung JW, Park JH, Han MC. Power versus conventional color Doppler sonography: comparison in the depiction of vasculature in liver tumors. Radiology 1996;200:55–58.
Taylor KJ, Ramos I, Morse SS, Fortune KL, Hammers L, Taylor CR. Focal liver masses: differential diagnosis with pulsed Doppler US. Radiology 1987;164:643–647.
Piscaglia F, Bolondi L. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol 2006;32:1369–1375.
Brannigan M, Burns PN, Wilson SR. Blood flow patterns in focal liver lesions at microbubble-enhanced US. Radiographics 2004;24:921–935.
Wilson SR, Jang HJ, Kim TK, Iijima H, Kamiyama N, Burns PN. Real-time temporal maximum-intensity-projection imaging of hepatic lesions with contrast-enhanced sonography. AJR Am J Roentgenol 2008;190:691–695.
Matsui O, Kadoya M, Kameyama T, Yoshikawa J, Takashima T, Nakanuma Y, Unoura M, et al. Benign and malignant nodules in cirrhotic livers: distinction based on blood supply. Radiology 1991;178:493–497.
Jang HJ, Kim TK, Burns PN, Wilson SR. Enhancement patterns of hepatocellular carcinoma at contrast-enhanced US: comparison with histologic differentiation. Radiology 2007;244:898–906.
Lim JH, Cho JM, Kim EY, Park CK. Dysplastic nodules in liver cirrhosis: evaluation of hemodynamics with CT during arterial portography and CT hepatic arteriography. Radiology 2000;214:869–874.
Kim TK, Jang HJ, Wilson SR. Benign liver masses: imaging with microbubble contrast agents. Ultrasound Q 2006;22:31–39.
Solbiati L, Tonolini M, Cova L. Monitoring RF ablation. Eur Radiol 2004;14 Suppl 8:P34–42.
Dill-Macky MJ, Asch M, Burns P, Wilson S. Radiofrequency ablation of hepatocellular carcinoma: predicting success using contrast-enhanced sonography. AJR Am J Roentgenol 2006;186:S287–295.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Humana Press, a part of Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Kim, T.K., Jang, HJ., Wilson, S.R. (2009). Ultrasound of Hepatocellular Carcinoma: The Important Contribution of Contrast Enhancement. In: Carr, B. (eds) Hepatocellular Carcinoma. Current Clinical Oncology. Humana Press. https://doi.org/10.1007/978-1-60327-376-3_14
Download citation
DOI: https://doi.org/10.1007/978-1-60327-376-3_14
Published:
Publisher Name: Humana Press
Print ISBN: 978-1-60327-373-2
Online ISBN: 978-1-60327-376-3
eBook Packages: MedicineMedicine (R0)