Abstract
Drug-induced acute kidney injury (AKI) is a relatively common problem. Prescribed medications, over-the-counter drugs/substances, and diagnostic agents may alter kidney function. As the kidney filters, secretes, reabsorbs, biotransforms, and excretes many drugs, it is not surprising that acute kidney injury is an adverse effect. Drugs and their metabolites can lead to injury within all compartments of the kidney including the vasculature, glomerulus, tubules, and interstitium. Common forms of drug-induced AKI affecting the various renal compartments include thrombotic microangiopathy, membranous and minimal change/focal segmental glomerulosclerosis, acute tubular injury/necrosis, osmotic nephropathy, crystalline-induced AKI, and acute interstitial nephritis. Recognizing AKI syndromes that are associated with various agents can lead to early identification of potentially harmful drugs and therapeutic agents, reducing exposure in at-risk patients. Once identified, the medication or agent can be withheld or dose-reduced, thereby significantly impacting and potentially reducing the duration and severity of kidney injury.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute kidney injury
- Chronic kidney disease
- Prerenal
- Intrinsic renal
- Postrenal
- Acute tubular necrosis
- Acute interstitial nephritis
- Crystalline nephropathy
1 Introduction
Therapeutic and diagnostic agents have long been noted to alter kidney function. The kidney is a common site of drug toxicity since many drugs are filtered, secreted, reabsorbed, biotransformed, and excreted by the kidney. The resulting enhanced and prolonged renal exposure to various drugs and drug metabolites can lead to injury within all compartments of the kidney: the interstitium, tubules, glomeruli, and renal blood vessels. Recognizing acute kidney injury (AKI) syndromes that are associated with various agents can lead to early identification in the treatment course of potentially harmful drugs and therapeutic agents. Once identified, the medication or agent can be withheld or dose-reduced, thereby significantly impacting and potentially reducing the duration and severity of kidney injury. This chapter focuses on diagnosis and recognition of patterns of AKI associated with certain drugs. While not all encompassing, it highlights major drugs.
2 Epidemiology of Drug-Induced Kidney Injury
The incidence and prevalence of drug-induced acute kidney injury (DI-AKI) are problematic and difficult to determine for several reasons. While therapeutic agents have been implicated in up to 60% of all hospital-acquired acute kidney injury (AKI) [1], the incidence is actually quite variable. In-hospital administration of medications has contributed to approximately 17–27% of all AKI, based on various studies [2,3,4,5,6]. The wide variability of estimating AKI prevalence in these studies is multifactorial. First, the prevalence variability of AKI may be related to the definition of AKI employed in certain studies. Second, most studies capture data on ICU patients yet miss the data on non-ICU patients, and very few studies examine AKI in non-hospitalized patients. Third, the inclusion of diagnostic agents, such as radiocontrast, can significantly alter the percentages of drug-induced versus other causes of AKI in hospitalized patients. Fourth, the effect of therapeutic agents on patients with chronic kidney disease (CKD) is often overlooked or actively excluded. Despite the variability, drug-induced AKI does have a high incidence and prevalence and is associated with an increased morbidity and mortality.
3 Risk Factors for Drug-Induced Kidney Injury
Risk factors for drug-induced AKI can be divided into risks specific to the drug or diagnostic agent, factors specific to the kidney’s drug handling, or characteristics specific to the patient (Table 9.1) Distinguishing these various risks is critical to assess whether any modifiable factors exist that can facilitate the use of measures that prevent or alleviate injury. While medications or therapeutic agents themselves are directly toxic or injurious to the kidney, development of AKI is significantly influenced by the presence of concurrent patient risk factors for nephrotoxicity.
3.1 Renal Risk Factors
The kidney itself is more prone to injury based on several factors. First, the kidney has significant exposure to potentially nephrotoxic medications and therapeutic agents by virtue of its high blood flow rate, which averages approximately 20–25% of cardiac output. As a result, therapeutic and diagnostic agents are delivered at a high rate to the kidney, allowing for greater exposure of potentially toxic substance to the kidney, thereby contributing to the burden of kidney injury [7].
On a cellular level, certain areas of the kidney are more prone to injury. Renal tubular epithelial cells (RTECs) that exist deep in the renal medullary regions are highly metabolically active, resulting in increased oxygen consumption. This demand creates a relatively hypoxic environment that makes cells exquisitely sensitive to toxic injury. As a result, these RTECs, through localized hypoxia, have a decreased ability to adequately respond to nephrotoxic substances that are encountered. In addition to this inherent hypoxic property of the cellular environment, the medullary region also has a significant concentrating ability, which can lead to the accumulation of drugs or drug metabolites at high concentrations. Ultimately, this concentrating effect on drug levels may promote toxic renal injury [7].
The unique transport properties of proximal RTECs make this region more prone to injury. These cells have extensive apical and basolateral cellular uptake mechanisms. Apical uptake of compounds occurs through endocytosis and other uptake mechanisms [8,9,10]. Upon uptake via the megalin/cubilin receptor, compounds enter lysosomes, accumulate and form myeloid bodies and/or rupture, and spill toxic substances into the cytoplasm. This results in the accumulation and concentration of potentially nephrotoxic substances within cells that can result in signaling pathways and cascades that ultimately lead to cell injury and death. Basolateral delivery also leads to proximal tubular exposure of compounds. Delivery occurs via peritubular capillaries, with uptake occurring through transporters called human organic anion/cation transporters (HOAT/HOCT) [9, 11]. This movement of potentially toxic substances into the intracellular space, and subsequent shuttling and apical excretion, increases the exposure of the proximal tubular cells to these substances, thereby contributing to AKI.
On a biochemical level, the kidney has several enzymes responsible for the biotransformation of drugs. These include CYP450 and flavin-containing monooxygenases. The breakdown of compounds in the kidney results in the generation of potentially nephrotoxic metabolites and reactive oxygen species that can promote injury (apoptosis and/or necrosis). Reactive oxygen species generation leads to oxidative stress and the generation of free radicals. Through nucleic acid oxidation and alkylation causing DNA breaks, direct protein damage, and lipid peroxidation, kidney injury can occur [7].
3.2 Patient Risk Factors
Various patient-specific factors also contribute to drug-induced kidney injury. Certain factors are not modifiable including age and sex. Both older age (>65 years old) and female sex increase the risk of drug-induced AKI. This effect is generally multifactorial. First, reductions in total body water are common in the elderly due to decreased lean body mass, leading to a decrease in total body water that affects drug distribution and plasma concentrations of water-soluble drugs. Second, lower muscle mass may impair the ability to detect abnormal GFRs masked by apparently normal serum creatinine concentrations. GFR estimating equations that are based on age attempt to ameliorate this concern, but oftentimes serum creatinine concentration, and not estimated GFR is assessed when clinicians are dosing drugs. Lastly, the elderly also tend to be more prone to increased renal arteriolar vasoconstriction secondary to angiotensin II or endothelin excess. This renal effect may expose the patient to increased drug concentrations [12,13,14].
Additional risk factors for drug-related injury unique to patients include the presence of acute or chronic kidney disease. Underlying kidney injury, either current AKI or CKD, makes a patient more susceptible to drug nephrotoxicity. Acutely injured kidneys may have ischemia preconditioned tubules that generate a more pronounced renal oxidative injury response to toxins. In both AKI and CKD, there may be an increased exposure of a decreased number of functioning nephrons to toxins, which will exacerbate pre-existing kidney dysfunction. Employing GFR estimating equations during AKI may also result in an overestimation of the GFR, especially with rapidly declining renal function. This can potentially lead to mis-dosing of medications leading to the accumulation of toxic doses of medications or metabolites [7]. More severe and prolonged AKI often develops, which risks development of CKD.
Apart from underlying kidney disease, other systemic diseases that are known to impair renal perfusion can increase susceptibility to drug injury. These include edematous states such as acute and chronic heart failure, nephrotic syndrome, and cirrhosis, which create a state of effective circulating volume depletion and renal underperfusion. This effectively volume-depleted state will lead to the activation of neurohormonal cascades that reduce renal perfusion. Patients with nephrotic syndrome and cirrhosis, and to a minor degree in malnourished heart failure patients, will develop hypoalbuminemia. As a result of reduced protein binding of drugs, low serum albumin can lead to increased free drug concentrations, thereby increasing exposure of certain potentially toxic drugs to the kidney [13, 14].
Certain host genetic differences can explain the heterogenous response that patients have to drug-induced kidney injury. For example, differences in innate host immune response genes can predispose certain patients to allergic drug reactions with acute interstitial nephritis (AIN) developing. In addition, the kidney has CYP450 enzymes, and polymorphisms in these genes may lead to altered metabolism with the potential for increased nephrotoxicity [15, 16]. Also, specific polymorphisms in transport channels may lead to altered metabolism with associated drug nephrotoxicity.
4 Diagnosis of Drug-Induced Acute Kidney Injury
Diagnosis of DI-AKI is similar to that of other forms of AKI and utilizes a combination of clinical, laboratory, and imaging findings (Table 9.2). Kidney injury may lead to various physical exam abnormalities. If allergic in nature, drug-induced injury may lead to a fever or rash; however these findings are relatively uncommon. The rash can present as a morbilliform, maculopapular, toxic epidermal necrolysis or a purpuric rash depending on the underlying renal lesion [17]. In addition to these findings, the patient may experience flank pain if there is swelling in the renal parenchyma and stretching of the renal capsule.
Laboratory evaluations can provide insight into the type of kidney injury. Elevations in blood urea nitrogen (BUN) and serum creatinine concentrations are often the first clinical manifestation of drug-induced kidney injury. As shown in animal (and some human) studies, novel serum and urinary biomarkers of kidney injury may provide an earlier diagnosis of acute kidney injury but are currently not available in the USA. Serum potassium and phosphorous are usually elevated in AKI; however hypophosphatemia and hypokalemia can also be important findings in the setting of certain forms of drug-induced tubular injury. Low serum phosphorus and potassium, in the correct context, can indicate adequate or modestly reduced GFR, yet impaired tubular reabsorption, suggesting proximal RTEC dysfunction. This injury pattern is often seen in a Fanconi syndrome , which occurs with several drugs.
A complete blood count can also provide clues into the type of kidney injury. Increased serum eosinophils may be seen with allergic or hypersensitivity-related renal disorders, both of which are common forms of drug-induced kidney injury. The combination of anemia and thrombocytopenia is very suggestive of a microangiopathic hemolytic anemic disease, such as drug-induced thrombotic microangiopathy, which is associated with AKI.
When evaluating drug-induced kidney injury, a thorough examination of the urine, through both automated laboratory analysis and direct sediment analysis, is critical in classifying the various types of renal injury and predicting the severity of injury. Automated urinalysis provides information that is complimentary to clinical labs and the urine sediment findings. Normoglycemic glucosuria suggests decreased proximal tubular glucose reabsorption, indicative of tubular dysfunction. Positive leukocyte esterase indicates the presence of leukocytes in the urine suggesting infection when accompanied by bacteria or yeast in the urine or, in the absence of microorganisms, inflammation along the genitourinary tract. Urinary eosinophils have been used in the past to suggest the possibility of AIN. However, the sensitivity and specificity of this test are quite low, and therefore, it is not recommended in the diagnostic workup [18].
Protein present on automated urinalysis indicates urinary albumin and not other proteins. Protein positive on a urinalysis is qualitative and should prompt protein quantification by the direct measurement of urinary albumin and total protein. Kidney injury that is predominantly glomerular in nature will generally have a large amount of albuminuria relative to total urinary protein. In contrast, low urinary albumin levels relative to total protein suggest either the presence of excess filtered non-albumin serum proteins or tubular dysfunction with tubular proteinuria [19, 20].
Urine sediment examination is an extremely useful diagnostic tool. The presence of RTECs, white blood cells (WBCs), or red blood cells (RBCs) can be suggestive of kidney injury. While RTECs may exist in low numbers in a patient without kidney injury, an abundance of RTECs often indicates underlying tubular injury. The presence of isomorphic RBCs can suggest an injury anywhere along the genitourinary tract, from the kidney to the urethra. However, dysmorphic RBCs is highly specific for glomerular injury, although they can be seen with certain inflammatory tubular disorders. The presence of urinary WBCs suggests inflammation anywhere along the genitourinary tract. The presence of bacteria or yeast alongside WBCs should raise the suspicion for an infection, whereas sterile pyuria raises suspicion for a renal inflammatory process [21].
Apart from cells, the urinary sediment is also useful in the identification of casts (cellular and noncellular) and crystals. Casts are composed of Tamm Horsfall protein, or uromodulin, a protein secreted by loop of Henle renal tubular cells. Hyaline casts are made of this protein and form in the setting of sluggish urinary flow rates. Cellular casts , whether RBC, WBC, RTEC, or a mix of these cells, is indicative of intrinsic kidney injury [22]. Muddy brown granular casts are also indicative of kidney injury and generally reflect ischemic or nephrotoxic acute tubular injury. Crystals may also be present in the urinary sediment [23]. Crystal-induced kidney disease will be discussed in detail in subsequent sections.
Imaging may be a useful tool in the diagnosis of acute and chronic kidney disease. Ultrasound demonstrates kidney size and echogenicity, which may indicate the possibility of chronic kidney disease or congenital or acquired unilateral kidney. Ultrasound is also helpful in evaluating for obstruction, manifested by hydronephrosis and/or hydroureter. Gallium scintigraphy and FDG-PET scans have also been used to diagnose AKI due to kidney inflammation such as AIN but are insensitive and non-specific findings [17].
Kidney biopsy is the gold standard in the diagnosis of drug-induced kidney injury. With examination of renal histology, the vasculature, glomeruli, tubules, and interstitium should be evaluated for injury patterns that can differentiate between the different etiologies of drug-induced kidney injury. Examples include drug-induced thrombotic microangiopathy and vasculitis as indicative of drug-associated vascular injury and immune-complex deposition and podocytopathies from a large number of drugs causing glomerular injury. Numerous medications promote acute tubular injury and necrosis through direct toxic effects, ischemic injury, osmotic effects, and crystal deposition within tubular lumens. An inflammatory infiltrate within the renal interstitium along with tubulitis and sometimes granulomas are histologic manifestations of drug-induced acute interstitial nephritis observed on kidney biopsy.
5 Drug-Induced Acute Kidney Injury
Many drugs can affect kidney function. The following sections describe drug-induced kidney injury patterns based on the underlying location in the kidney. Common drugs or drug classes are included, with more in-depth listings of drugs included in associated tables.
5.1 Prerenal (Hemodynamic) Acute Kidney Injury
Glomerular filtration is modulated by a number of local and systemic hormones which include the prostaglandins (PG), angiotensin, endothelin, catecholamines, and atrial natriuretic peptide, to name a few. Afferent vasodilation and efferent vasoconstriction allow maintenance of glomerular filtration, especially when renal perfusion is compromised by hypotension and true or effective volume depletion. Perturbations of these vascular forces can lead to prerenal physiology or hemodynamic reductions in GFR. Several drugs may reduce GFR by altering afferent or efferent vascular tone (Fig. 9.1).
Glomerular filtration is determined in part by afferent arteriolar and efferent arteriolar vascular tone. In states of reduced blood flow and low blood pressure, the afferent arteriole is dilated, and the efferent arteriole is constricted. The medications noted in the figure disturb this response and reduce GFR
5.1.1 Afferent Vasoconstriction
Nonsteroidal anti-inflammatory drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly employed as analgesics, antipyretics, and anti-inflammatory medications. NSAIDs are implicated in many forms of drug-related injury including hemodynamic AKI from dysregulation of glomerular blood flow [24, 25]. NSAIDs inhibit cyclooxygenase (COX) enzymes, which convert arachidonic acid (AA) to various PGs. Inhibition of the COX enzymes leads to a decrease in prostaglandin synthesis, thereby severely curtailing prostaglandin function to modulate afferent arteriolar tone. As PGs potentiate afferent arteriolar dilatation, inhibition of their synthesis through NSAID use can lead afferent vasoconstriction, thereby impairing renal blood flow leading to a decreased GFR and hemodynamic AKI. Normally the effects of prostaglandins on arteriolar tone are minimal; however in severe acute volume depletion, in effective volume depletion (cirrhosis, heart failure, nephrotic syndrome), or in CKD, patients are prostaglandin dependent for maintenance of GFR. In these settings, PG inhibition can tip the afferent arteriole to vasoconstriction, thus leading to decreased GFR. COX enzymes can exist as either a COX-1 or COX-2 subtypes, both of which are important to maintain GFR and inhibition of either can hemodynamic AKI [26,27,28].
Calcineurin inhibitors
Cyclosporine and tacrolimus belong to a class of medications known as the calcineurin inhibitors (CNI) . These medications function by binding cytoplasmic proteins (cyclophilins and FK-binding protein, respectively), which leads to the inhibition of calcineurin, which in turn prevents the transcription of certain immune cytokines. These medications are widely used as immunosuppressants for solid organ transplantation and a variety of autoimmune disorders. One side effect of these drugs, especially at higher doses with supratherapeutic levels, is afferent and efferent arteriolar vasoconstriction caused primarily by endothelial dysfunction. This leads to the decreased production of vasodilators, such as PGs and nitric oxide, and the release of vasoconstrictors, such as thromboxane A2 and endothelin, which reduce renal perfusion and GFR [29, 30]. As with the NSAIDs, true or effective volume depletion and CKD predispose to reductions in GFR and AKI. In addition, the use of these agents in the setting of graft ischemia can prolong primary graft dysfunction and failure. In addition to CNI dose reduction, discontinuation of certain drugs (NSAIDs, ACE/ARBs), calcium channel blocker therapy, and administration of intravenous volume can mitigate the effects of CNI nephrotoxicity.
Angiotensin converting enzyme inhibition/angiotensin receptor blockade
Activation of the angiotensin type I receptor (AT-I) of the efferent arteriole causes arteriolar vasoconstriction that leads to an increase in intraglomerular capillary pressure and thereby maintains GFR in the setting of mild to moderate renal underperfusion. In normal states, angiotensin antagonism by angiotensin converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARBs) has little effect on renal hemodynamics. However, ACEI or ARBS are administered in settings of reduced RBF, as with severe renal artery stenosis, states of true or effective volume depletion, with CKD, or NSAID or CNI therapy, intraglomerular capillary pressure decreases and GFR declines [31, 32]. A decline in GFR that stabilizes is typically beneficial in patients with proteinuric CKD. However, in severe RAS and volume-depleted states, AKI with rising serum creatinine develops and warrants investigation with temporary drug discontinuation (and correction of the underlying disease state) .
5.2 Intrinsic Kidney Disease
5.2.1 Vascular Disease
Several medications have been implicated in drug-induced AKI as a result of vascular injury. As the kidney is extremely vascular organ, local and systemic disease causing renal vascular injury is often associated with AKI. Below are three forms of vascular injury that have been associated with drug-induced AKI.
Cholesterol embolization is a syndrome that can be induced by anticoagulant and thrombolytic therapy. While this complication more often occurs following arteriography and certain vascular procedures, the diagnosis is sometimes difficult to differentiate from radiocontrast-induced AKI. Upon administration of the thrombolytic agents, which dissolve thrombus covering atherosclerotic plaques, cholesterol fragments embolize to vessels in various end organs including the kidneys. Most often the skin, as manifested by acute distal cyanosis in the form of infarcted digits or livedo reticularis, or the kidney, as manifested by AKI and acute hypertension, is involved. Recognition of the syndrome can be tricky as AKI usually manifests upward to 1–2 weeks, and it mimics other syndromes including vasculitis [33, 34]. Therapy is supportive although cases of steroid therapy responsiveness have been reported. Outcomes are quite poor, with one study showing greater than 25% of patients requiring chronic hemodialysis and a large percentage of patients developing nondialysis-dependent CKD.
Drug-induced thrombotic microangiopathy (TMA) has also been reported with numerous medications (Fig. 9.2). TMA following drug administration can either be caused by drug-related induction of antibody production (targeting ADAMTS-13, inhibitory complement factors, or platelets) or direct toxicity of the drug leading to vascular injury and platelet-rich thrombus formation in small blood vessels. A list of drugs implicated in both forms of TMA is listed in Table 9.3. Anticancer agents such as the anti-angiogenesis drugs, gemcitabine, and mitomycin C are associated with TMA. Proteinuria and hypertension are the most common renal effects of the ADs; however AKI often signal severe TMA. This class of drugs is now the most common cause of drug-induced TMA. Systemic evidence of TMA is absent in 50% of patients, and a renal limited form of TMA must be entertained in patients with AKI. Although relatively rare, a cumulative TMA incidence of 0.31% has been noted in patients exposed to gemcitabine. Gemcitabine use has been noted to have both immune-mediated and direct toxicity leading to its nephrotoxicity profile [35, 36]. Interferon when used in high dose and for prolonged periods is associated with TMA, especially in patients with chronic myelogenous leukemia. The antiplatelet agents (ticlopidine, clopidogrel, and prasugrel) are all associated with TMA, while quinine exposure through prescription, beverages, and health food stores is associated with TMA via formation of quinine-dependent IgG antibodies to platelets .
Thrombotic microangiopathy (TMA) is seen in the glomerulus of a patient treated with gemcitabine. As seen in this image, the glomeruli containing multiple intracapillary fibrin thrombi, mesangiolysis, and numerous red blood cell fragments within the injured subendothelial and mesangial areas of the glomerular tuft. These findings characterize TMA
Kidney-specific ANCA-associated vasculitis (AAV) has been associated with certain drugs, including hydralazine, minocycline, phenytoin, penicillamine, allopurinol, sulfasalazine, antitumor necrosis factor agents, and propylthiouracil (PTU) (Table 9.4). Cocaine cut with levamisole is another cause of AAV. ANCA-associated vasculitides refer to a disease that results in the production of anti-neutrophil cytoplasmic antibodies (ANCA) that can either have a cytoplasmic (C-ANCA) or perinuclear (P-ANCA) pattern . The C-ANCA pattern is almost exclusively caused by antibodies directed against proteinase 3 (PRC), while P-ANCA is usually due to antibodies directed against myeloperoxidase (MPO) but also can be seen with antibodies against lactoferrin and human leukocyte esterase (HLE) [37, 38]. Presence of these antibodies leads to small vessel injury and when present in the kidney is manifested as a necrotizing glomerulonephritis (Fig. 9.3). Induction of vasculitis is quite rare in these medications. PTU is the drug that is most commonly associated with an AAV. PTU-associated ANCA conversion has been reported in 20–64% of patients, with only a very small fraction of patients (4–6%) having clinical evidence of vasculitis. Although vasculitis is not common, it should be recognized early, as consequences can be fatal if the medication is not withheld and immunosuppressive therapy not administered.
5.2.2 Glomerular Disease
Several forms of drug-induced glomerular disease (Table 9.5) have been reported, and these agents target all glomerular cell types (podocyte, endothelial cell, and mesangial cell). Classic lesions include minimal change disease (MCD) , membranous nephropathy (MGN), and focal and segmental glomerulosclerosis (FSGS) . These are secondary forms of glomerulopathy which, while relatively uncommon, must be recognized to facilitate drug discontinuation and therapy to limit kidney injury. In these cases, drug-induced glomerular disease presents similarly to idiopathic or primary forms of glomerular diseases, although the effects, often proteinuria, may not be as severe. In general, one can demonstrate a temporal association between offending agent exposure and development of the glomerulopathy.
Drug-induced podocyte (glomerular epithelial cell) injury leading to either MCD or FSGS is well described. As with the idiopathic or primary counterparts, patients will usually have nephrotic-range proteinuria and peripheral edema; however, it can be less severe. Drugs that have been implicated in MCD include interferon, pamidronate, lithium, and NSAIDs. Another podocytopathy associated with glomerular scarring is FSGS. Drugs implicated in causing FSGS (Fig. 9.4) include interferon, pamidronate, sirolimus, lithium, and anabolic steroids. These patients tend to have more severe AKI and may not fully recover kidney function following discontinuation. As with other forms of drug-induced injury, care is largely supportive with removal of the offending agent and sometimes a course of steroids [39].
Membranous nephropathy (Fig. 9.5) is a form of glomerular disease characterized by nephrotic syndrome and varying severities of AKI. Biopsy, unlike the two previously mentioned nephropathies, will demonstrate with thick capillary loops on light microscopy, granular immunofluorescence (IF) pattern, and glomerular subepithelial membrane immune complexes on electron microscopy. In contrast to primary MGN, immunofluorescence is often negative for anti-PLAR2 antibodies with absent IgG4 subtype staining on IF [40]. MGN is described with penicillamine/bucillamine and gold salts, three antiquated agents that were used to treat rheumatoid arthritis. Now, however, MGN is reported, albeit rarely, with NSAIDs and selective COX inhibitors, the antitumor necrosis factor agent adalimumab, captopril, and certain organic mercurials contained in skin-lightening creams. As NSAIDs are widely used, recognition that MGN can occur is important for clinicians, although it is less common than MCD. Drug discontinuation may reverse the lesion, but immunosuppressive therapy may also be employed.
(a) Membranous glomerulonephritis is seen on light microscopy in a patient treated with a nonsteroidal anti-inflammatory drug. The capillary loops are thickened and appear rigid. (b) On electron microscopy, electron dense deposits are seen in the subepithelial space. These findings are diagnostic for membranous glomerulonephritis
Drug-induced lupus (DIL) is relatively uncommon, occurring more commonly in older patients (Table 9.4). Major organ involvement is rare but has been reported with glomerular involvement associated with hydralazine, sulfasalazine, penicillamine, and anti-TNF-a therapy [41]. Serologies in drug-induced lupus nephritis are slightly different than idiopathic lupus, with antihistone antibodies more prevalent, yet anti-dsDNA antibodies still present in hydralazine-induced lupus nephritis. Complement levels are variably reduced, and other abnormalities may be reported, such as the presence of p-ANCA antibodies. Treatment of drug-induced lupus nephritis includes removing the offending agent, with manifestations of disease resolving within days to weeks of this intervention. Major organ involvement including AKI can require the use of immunosuppressive agents .
5.2.3 Acute Interstitial Nephritis
Drugs are the most predominant cause of acute interstitial nephritis (AIN) , ahead of autoimmune disorders and infections. In developed countries, studies have shown upward of 70% of AIN attributed to medications, especially hospital-acquired AIN. AIN typically presents as a steady, not abrupt, rise in serum creatinine approximately 2 weeks after introduction of a medications. This is not always the case, as repeat exposure may lead to a more abrupt rise in serum creatinine. Along this line, drugs such as the NSAIDs and proton-pump inhibitors may present with a gradual and prolonged rise in serum creatinine. Except for methicillin, AIN rarely presents with a systemic hypersensitivity reaction, with triad of fever, skin rash, and eosinophilia <5–10% and clearly much less common than kidney involvement. In contrast, AKI, as evidenced by a rise in serum creatinine, sterile pyuria with the presence of leukocyturia and white blood cell casts, and low-grade proteinuria are more commonly present [17].
AIN is an allergic response that is mediated predominantly by T cells in concert with plasma cells, eosinophils, neutrophils, and mast cells. The end result is an inflammatory cell-rich interstitial infiltrate accompanied by tubulitis and sometimes granuloma (Fig. 9.6). Certain factors can play a role in the development of AIN, including drugs acting as haptens, molecular mimicry, and an individual’s underlying immune response genes. However at times, although rarely, a humoral response may lead to the inflammatory response, whereby portion of the drug, which acts as a hapten, binds to the tubular basement membrane and evokes an antibody response with formation of tubulointerstitial immune complexes [17].
All drugs are suspect when AIN has been diagnosed, but certain medications, perhaps based on usage patterns, are more common. When discovered, the first and foremost therapy is to remove the offending agent. If AKI is severe enough, time of recognition is recent, minimal interstitial fibrosis is present on histology, and the resulting AIN is from a more acute rather than chronic exposure, a course of steroids may be warranted with the hopes of preserving kidney function. Table 9.6 lists drugs that are commonly associated with AIN. Three classes of medications that have been commonly implicated in acute interstitial nephritis are discussed.
Antimicrobials have a high potential to cause AIN [42]. Beta-lactams (penicillin derivatives and cephalosporins) are more common inducers of AIN than other antibiotics. Methicillin frequently caused AIN with an associated hypersensitivity syndrome and for this reason is no longer routinely used. Other beta-lactams remain a common cause of AIN along with the sulfonamides. As with methicillin , these drugs more tend to cause more hypersensitivity reactions, with fever, rash, and eosinophilia than other drugs. Fluoroquinolones have also been implicated in AIN, with ciprofloxacin being more common than the others. Several antiviral agents can also cause AIN and must be considered when AKI develops. Discontinuation of the culprit drug is the mainstay of therapy. However, it may be difficult identifying the causative agent when several are employed. In addition, it may also be difficult to discontinue the antibiotic that is being used for a documented infection unless other good options are available. Avoidance of the particular antibiotic and possibly similar antibiotics of the same class is advised. Steroid therapy may also be warranted in cases of severe AKI, especially when AIN is documented within 2–3 weeks of drug initiation and histology has limited interstitial fibrosis. This can be tricky when patient has severe underlying infection although steroids have been employed in sepsis and septic shock. Discussion with the infectious disease consultant is often warranted.
NSAIDs are another important cause of AIN [43]. Clinical presentation tends to be more subacute or chronic and usually falls well outside the classical range of the medication initiation within 1–2 weeks. Hypersensitivity symptoms and signs are extremely rare with these drugs. Unlike other forms of AIN, NSAIDs may be accompanied by nephrotic-range proteinuria due to associated MCD. The interstitial infiltrate typically shows a mononuclear infiltrate with few or no eosinophils. NSAID-induced AIN may develop due to inhibition of COX enzyme, which leads to leukotriene overproduction through the activity of lipoxygenases on arachidonic acid. These pro-inflammatory cytokines can be responsible for the interstitial inflammatory lesion observed with NSAID therapy. All NSAIDs, including topical preparations and the selective COX-2 inhibitor celecoxib, can cause AIN [44].
Proton-pump inhibitors (PPIs) , which are a mainstay of therapy for acid-related gastrointestinal (GI) disease, are a well-described cause of AIN [45,46,47]. AIN was first described with omeprazole and subsequently with several other PPIs. Unlike other forms of drug-induced AIN, PPIs develop the lesion at a mean time of approximately 11 weeks. Like NSAIDs, patients often do not develop a typical hypersensitivity reaction. Early recognition of PPI-induced AIN and drug discontinuation is generally associated with a good prognosis. Importantly, AIN with the PPIs is a class affect, and switching to H2 antagonists is required for further treatment of acid-related GI disorders. While kidney function usually recovers, many patients may develop CKD.
5.2.4 Acute Tubular Injury/Necrosis
One of the most common renal lesions associated with drug therapy is acute tubular injury/necrosis (ATI/ATN), which often develops from direct tubular toxicity [48]. As mentioned, most patients have underlying risk factors for drug-induced tubular injury (Fig. 9.7). Tubular injury usually occurs in a dose-dependent fashion with increased exposure producing progressively worse injury moving from subclinical damage to advanced stage 3 AKI from severe ATN. The proximal tubule is particularly prone to injury as it is the site of drug reabsorption through multiple pathways. Medications may injure cells through promoting mitochondrial dysfunction, disrupting lysosomal or cell membranes, enhancing cellular entry of calcium and other ions, and directly promoting the formation of free radicals. Indirect tubular injury by drugs can occur through induction of rhabdomyolysis with associated myoglobinuria and direct tubular pigment toxicity, as seen with the statin drugs. Table 9.7 lists various drugs associated with acute tubular injury/necrosis. Selected drugs or drug classes that have been commonly associated with acute tubular injury/necrosis are reviewed.
Aminoglycosides are bactericidal agents that have been employed for many years to treat gram-negative infections. Kidney injury with select aminoglycosides has been reported as high as 25% [49]. Aminoglycosides are freely filtered and due to cationic charge are attracted by apical phospholipids and reabsorbed in proximal tubules via megalin/cubilin receptor binding. Toxicity is associated with cationic charge with neomycin (most cationic) demonstrating a high degree of nephrotoxicity, followed by gentamicin, tobramycin, amikacin, and streptomycin. Tubular injury usually occurs 5–7 days after administration, with nephrotoxicity being dose dependent. Risks for AKI include volume depletion, underlying AKI or CKD, and patient age. AKI is generally nonoliguric and may be associated with electrolyte and acid-base disturbances due to aminoglycoside-related Fanconi or Bartter-like syndromes. Prevention or reductions in AKI are based on volume repletion and careful calculation of loading and maintenance doses based on eGFR. While monitoring peak and trough serum aminoglycoside levels can reduce risk of nephrotoxicity, single daily versus multiple doses per day reduced tubular injury and maintains drug efficacy. Dialysis is sometimes required for severe ATI/ATN. Dialysis does effectively remove aminoglycosides .
Several osmotically active agents that are excreted by the kidney can cause AKI from tubular injury [50]. These agents, which include intravenous sucrose (a carrier in some forms of intravenous immunoglobulin), radiocontrast dye, hydroxyethylstarch, mannitol, and intravenous cyclodextrin, are filtered macromolecules that are not metabolized by the kidney due to a lack of enzymes. These substances undergo proximal tubular uptake via pinocytosis, are internalized, and taken up by lysosomes. Lysosomes are packed with these substances and due to inefficient removal cause severe cell swelling. Cellular swelling leads to disturbed cell function and tubular luminal occlusion, a process termed osmotic nephrosis or nephropathy. Risks for AKI include volume depletion, excessive drug concentrations, and underlying AKI or CKD. Patients may develop oliguric AKI and may require dialysis until renal recovery occurs within 5–7 days. Several large trials demonstrate increased AKI and dialysis requirement in critical care patients treated with hydroxyethyl starch [51, 52]. Treatment is largely supportive with avoidance of further nephrotoxin exposure and dialysis when indicated, which may also reduce drug levels and facilitate renal recovery.
Cisplatin is a member of the platinum-based chemotherapeutic agents utilized to effectively treat various malignancies. Tumor killing results from the ability of cisplatin to bind to and crosslink DNA, thereby leading to tumor cell apoptosis. AKI has long been recognized as a complication of cisplatin and is due primarily to direct tubular toxicity with some contribution from glomerular and vascular injury [11, 53]. Drug uptake into proximal tubular cells occurs primarily via OCT2. Once inside of cells, it can cause injury and apoptosis via inflammation, oxidative stress, and activation of cell death pathways (caspase, cyclin-dependent kinases, etc.). Chloride at the cis position of the molecule is thought to promote much of the injury. Risks for toxicity include volume depletion and underlying CKD. Forced diuresis with normal saline and 3% saline may reduce tubular injury. Intravenous magnesium, amifostine, and other agents may also reduce AKI. Other platin agents such as carboplatin and oxaliplatin are less nephrotoxic in part due to absent OCT2 transport and replacement of chloride at the cis position with carboxylate and cyclobutane. Therapy is mainly supportive and dialysis initiated for the usual indication, but it will not remove the drug. Other anticancer agents associated with various degrees of tubular injury include ifosfamide, pemetrexed, zoledronate, pentostatin, imatinib, and the BRAF inhibitors among others.
Tenofovir is a reverse transcriptase inhibitor that is used as part of combination anti-retroviral therapy (cART) in patients with HIV infection. The drug is structurally similar to naturally occurring oligonucleotides and the known nephrotoxins adefovir and cidofovir. This structure, along with its pathway of excretion through proximal tubular cells via OAT1, promotes cellular injury. While initial clinical trials suggested renal safety, subsequent case reports/series, systematic reviews, VHA database study, and more recent phase 3 trials have shown clear-cut AKI and proximal tubulopathy (Fanconi syndrome ) associated with tenofovir [54, 55]. Animal studies and patient biopsies demonstrate ATI/ATN with associated mitochondrial disturbance/disruption [55]. Risks for tenofovir-associated kidney injury include underlying CKD, coadministration of medications that increase tenofovir levels, and endogenous apical efflux transport mutations (MRP2 gene) [56]. AKI typically resolves with drug discontinuation, and patients may rarely require dialysis. Up to 50% of patient may be left with some level of CKD [55].
5.2.5 Crystalline Nephropathy
Certain drugs and/or their metabolites can precipitate within tubular lumens to form crystals (Fig. 9.8). This process usually occurs in distal tubular lumens leading to both a tubular obstruction and an interstitial cellular activation and inflammation [57]. Crystals generally form due to inherent insoluble properties, sluggish urine flow rates, urine pH effects on drug solubility, and underlying kidney disease. Risks that can therefore lead to intratubular crystal formation include true or effective volume depletion as seen in cirrhosis, CHF, renal salt wasting or chronic diarrhea, underlying AKI or CKD, and excessive drug dosing. Table 9.8 lists drugs that have been reported to cause crystalline nephropathy. A couple of illustrative examples are discussed.
Acyclovir is an antiviral agent that is used to treat herpes simplex virus infection and when employed intravenously can cause crystalluria and AKI. Rapid high-dose acyclovir bolus employed for viral meningoencephalitis leads to high concentrations of drug within tubular lumens. In fact, upward of 90% of the drug is eliminated through the kidney. Due to high urinary concentrations and the relative insolubility of acyclovir, drug crystals precipitate within the tubular lumens. As a result, AKI has been described in between 12 and 48% of patients receiving high-dose intravenous acyclovir , a number that increases with concomitant volume depletion and underlying CKD [58, 59]. Acyclovir crystals can be identified on urine sediment exam where they are usually needle shaped and positively birefringent with polarization. Prevention or reduction of AKI can be achieved with appropriate drug dosing adjusted to GFR, volume repletion prior to drug administration, and slower infusion of drug (versus bolus). When AKI occurs and is associated with neurotoxicity, dialysis can effectively remove the drug. Most patients recover kidney function with supportive therapy.
Orlistat , an inhibitor of gastric and pancreatic lipase, is approved as a prescription and an over-the-counter medication for weight loss. It functions by promoting fat malabsorption, which can promote enteric hyperoxaluria. Fat within the bowel lumen saponifies calcium, which allows unbound oxalate to be absorbed and increase serum oxalate levels. The resulting hyperoxaluria promotes calcium oxalate precipitation with tubular lumens. This results in acute/subacute oxalate nephropathy and AKI, which stems from both tubulointerstitial inflammation and luminal obstruction. Several case reports of AKI in the setting of orlistat therapy have demonstrated biopsy-proven calcium oxalate nephropathy [60, 61]. All patients in these cases had underlying diabetes mellitus and CKD. A population-based study of 953 patients also documented increased AKI in patient-administered orlistat. CKD, hypertension, and CHF were AKI risks for those taking orlistat. Drug avoidance in patients with known CKD and careful monitoring in high-risk patients prone to volume depletion can help reduce the risk. Using lower doses may also decrease AKI risk as well. In general, AKI recovers with drug discontinuation and supportive care.
Methotrexate is dihydrofolate reductase inhibitor that is used in high intravenous doses to treat certain malignancies. The drug and its metabolite (7-OH methotrexate) are filtered and secreted by the tubules into the urine. Nephrotoxicity develops predominantly in patients treated with doses ranging from 1 to 12 grams/m2, and AKI incidence ranges from 1.8 to 12% depending on the population studied [58, 62]. Methotrexate crystal precipitation within tubular lumens is associated with kidney injury (plus interstitial inflammation), although direct tubular injury from oxidative stress associated with reduced adenosine deaminase activity may contribute. The poor solubility of methotrexate/7-OH methotrexate in acidic urine as well as reduced urine flow rates enhances crystal precipitation. Prevention of or reduction in AKI involves urinary alkalinization (pH > 7.1) and induction of high urinary flow rates. Treatment of AKI revolves around leucovorin rescue and in some instances the use of high-flux hemodialysis or carboxypeptidase G2 administration (to convert the drug to a harmless metabolite) [63].
Atazanavir is a protease inhibitor that is used as a once daily medication to treat HIV. IT has a rather favorable side effect profile. However, case reports of atazanavir crystal nephropathy have been reported. Early reports have shown stones with birefringent atazanavir crystals [64, 65]. About 7% of the medication is excreted non-metabolized in the urine [66]. It is poorly soluble and more likely to precipitate in alkaline urine. A large retrospective study has demonstrated nephrolithiasis in approximately 1% of patients on atazanavir with a median time of onset of 23 months [67].
5.3 Postrenal AKI
AKI can also present as the result of post-kidney obstruction promoted by a medication [48]. Obstruction occurring downstream of the kidney can be the result of injury or obstruction to the ureters, bladder, prostate, or urethra. This can either be the result of direct injury to these organs, luminal or outflow obstruction, or extrinsic compression of these organs impeding urinary flow. Ultrasonography reveals dilatation of the pelvis and calyces of the kidneys (Fig. 9.9).
Medications that increase the risk of nephrolithiasis should be suspected in patients who present with stone-related obstruction. Approximately 1–2% of kidney stones are caused by drugs with lithogenic potential [48]. Either the drug or its metabolite may form all or part of the stone, or the drug or metabolite may impair calcium oxalate or purine metabolism, thereby leading to the formation of these stones [68]. Coadministration of medications that alter drug metabolism can also enhance stone formation. Lastly, chronic drug use or high medication dose can increase the risk of stone formation. Patient-specific factors increase the risk of nephrolithiasis including either a personal or family history of lithogenesis, abnormal urine pH, current or frequent genitourinary tract infections, low urine volume, acute or chronic states of volume depletion, and underlying AKI or CKD. Table 9.9 lists drugs commonly associated with nephrolithiasis .
Aside from the formation of kidney stones, medications that cause retroperitoneal fibrosis (RPF) can also lead to ureteral encasement thereby creating a significant urinary obstruction and AKI. Ergot derivatives, beta-blockers, and dopaminergic agents have all been reported as causing RPF. Finally agents that promote urinary retention, including anticholinergics, antihistamines, anesthetic agents, opiates, ecstasy, and alcohol, can also lead to AKI from impaired bladder emptying .
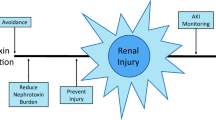
5.4 Summary
All parts of the kidney are vulnerable to effects of medication. Certain patient- and kidney-specific factors are not modifiable and may make some patients more susceptible to injury. Medications themselves or metabolites can have varied nephrotoxic potential. Injury can take the form of hemodynamic, tubular, interstitial, or glomerular injury. Recognizing signs of kidney injury early and identifying potential medications that can cause injury can help to decrease the burden and impact of medication-induced acute kidney injury.
References
Schetz M, Dasta J, Goldstein S, Golper T. Drug-induced acute kidney injury. Curr Opin Crit Care. 2005;11:555–65.
Choudhury D, Ahmed Z. Drug-induced nephrotoxicity. Med Clin North Am. 1997;81:705–17.
Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324:377–84.
Mehta RL, Pascual MT, Soroko S, et al. Spectrum of acute renal failure in the intensive care unit: the PICARD experience. Kidney Int. 2004;66:1613–21.
Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–6.
Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–8.
Perazella MA. Renal vulnerability to drug toxicity. Clin J Am Soc Nephrol. 2009;4:1275–83.
Fanos V, Cataldi L. Renal transport of antibiotics and nephrotoxicity: a review. J Chemother. 2001;13:461–72.
Enomoto A, Endou H. Roles of organic anion transporters (OATs) and a urate transporter (URAT1) in the pathophysiology of human disease. Clin Exp Nephrol. 2005;9:195–205.
Nagai J, Takano M. Molecular aspects of renal handling of aminoglycosides and strategies for preventing the nephrotoxicity. Drug Metab Pharmacokinet. 2004;19:159–70.
Ciarimboli G, Ludwig T, Lang D, et al. Cisplatin nephrotoxicity is critically mediated via the human organic cation transporter 2. Am J Pathol. 2005;167:1477–84.
Jerkic M, Vojvodic S, Lopez-Novoa JM. The mechanism of increased renal susceptibility to toxic substances in the elderly. Part I. The role of increased vasoconstriction. Int Urol Nephrol. 2001;32:539–47.
Singh NP, Ganguli A, Prakash A. Drug-induced kidney diseases. J Assoc Physicians India. 2003;51:970–9.
Guo X, Nzerue C. How to prevent, recognize, and treat drug-induced nephrotoxicity. Cleveland Clin J Med. 2002;69:289–90, 293–284, 296–287 passim.
Ciarimboli G, Koepsell H, Iordanova M, et al. Individual PKC-phosphorylation sites in organic cation transporter 1 determine substrate selectivity and transport regulation. J Am Soc Nephrol. 2005;16:1562–70.
Harty L, Johnson K, Power A. Race and ethnicity in the era of emerging pharmacogenomics. J Clin Pharmacol. 2006;46:405–7.
Perazella MA. Diagnosing drug-induced AIN in the hospitalized patient: a challenge for the clinician. Clin Nephrol. 2014;81:381–8.
Muriithi AK, Nasr SH, Leung N. Utility of urine eosinophils in the diagnosis of acute interstitial nephritis. Clin J Am Soc Nephrol. 2013;8:1857–62.
Smith ER, Cai MM, McMahon LP, Wright DA, Holt SG. The value of simultaneous measurements of urinary albumin and total protein in proteinuric patients. Nephrol Dial Transplant. 2012;27:1534–41.
Samarawickrama A, Cai M, Smith ER, et al. Simultaneous measurement of urinary albumin and total protein may facilitate decision-making in HIV-infected patients with proteinuria. HIV Med. 2012;13:526–32.
Fogazzi GB, Verdesca S, Garigali G. Urinalysis: core curriculum 2008. Am J Kidney Dis. 2008;51:1052–67.
Perazella MA. The urine sediment as a biomarker of kidney disease. Am J Kidney Dis. 2015;66:748.
Fogazzi GB. Crystalluria: a neglected aspect of urinary sediment analysis. Nephrol Dial Transplant. 1996;11:379–87.
Clive DM, Stoff JS. Renal syndromes associated with nonsteroidal antiinflammatory drugs. N Engl J Med. 1984;310:563–72.
Schlondorff D. Renal complications of nonsteroidal anti-inflammatory drugs. Kidney Int. 1993;44:643–53.
Perazella MA. COX-2 selective inhibitors: analysis of the renal effects. Expert Opin Drug Saf. 2002;1:53–64.
Perazella MA, Tray K. Selective cyclooxygenase-2 inhibitors: a pattern of nephrotoxicity similar to traditional nonsteroidal anti-inflammatory drugs. Am J Med. 2001;111:64–7.
Eras J, Perazella MA. NSAIDs and the kidney revisited: are selective cyclooxygenase-2 inhibitors safe? Am J Med Sci. 2001;321:181–90.
Nankivell BJ, Borrows RJ, Fung CL, O’Connell PJ, Chapman JR, Allen RD. Calcineurin inhibitor nephrotoxicity: longitudinal assessment by protocol histology. Transplantation. 2004;78:557–65.
Fellstrom B. Cyclosporine nephrotoxicity. Transplant Proc. 2004;36:220S–3S.
Navar LG, Harrison-Bernard LM, Imig JD, Wang CT, Cervenka L, Mitchell KD. Intrarenal angiotensin II generation and renal effects of AT1 receptor blockade. J Am Soc Nephrol. 1999;10(Suppl 12):S266–72.
Brewster UC, Perazella MA. The renin-angiotensin-aldosterone system and the kidney: effects on kidney disease. Am J Med. 2004;116:263–72.
Lee KG, Loh HL, Tan CS. Spontaneous cholesterol crystal embolism—a rare cause of renal failure. Ann Acad Med Singapore. 2012;41:176–7.
Hitti WA, Wali RK, Weinman EJ, Drachenberg C, Briglia A. Cholesterol embolization syndrome induced by thrombolytic therapy. Am J Cardiovasc Drugs. 2008;8:27–34.
Walter RB, Joerger M, Pestalozzi BC. Gemcitabine-associated hemolytic-uremic syndrome. Am J Kidney Dis. 2002;40:E16.
Fung MC, Storniolo AM, Nguyen B, Arning M, Brookfield W, Vigil J. A review of hemolytic uremic syndrome in patients treated with gemcitabine therapy. Cancer. 1999;85:2023–32.
Harper L, Savage CO. Pathogenesis of ANCA-associated systemic vasculitis. J Pathol. 2000;190:349–59.
Gao Y, Zhao MH. Review article: drug-induced anti-neutrophil cytoplasmic antibody-associated vasculitis. Nephrology. 2009;14:33–41.
Markowitz GS, Bomback AS, Perazella MA. Drug-induced glomerular disease: direct cellular injury. Clin J Am Soc Nephrol. 2015;10:1291–9.
Hofstra JM, Debiec H, Short CD, et al. Antiphospholipase A2 receptor antibody titer and subclass in idiopathic membranous nephropathy. J Am Soc Nephrol. 2012;23:1735–43.
Hogan JJ, Markowitz GS, Radhakrishnan J. Drug-induced glomerular disease: immune-mediated injury. Clin J Am Soc Nephrol. 2015;10:1300–10.
Perazella MA, Markowitz GS. Drug-induced acute interstitial nephritis. Nat Rev Nephrol. 2010;6:461–70.
Pirani CL, Valeri A, D’Agati V, Appel GB. Renal toxicity of nonsteroidal anti-inflammatory drugs. Contrib Nephrol. 1987;55:159–75.
Alper AB Jr, Meleg-Smith S, Krane NK. Nephrotic syndrome and interstitial nephritis associated with celecoxib. Am J Kidney dis. 2002;40:1086–90.
Brewster UC, Perazella MA. Proton pump inhibitors and the kidney: critical review. Clin Nephrol. 2007;68:65–72.
Brewster UC, Perazella MA. Acute kidney injury following proton pump inhibitor therapy. Kidney Int. 2007;71:589–93.
Geevasinga N, Coleman PL, Webster AC, Roger SD. Proton pump inhibitors and acute interstitial nephritis. Clin Gastroenterol Hepatol. 2006;4:597–604.
Perazella MA. Drug-induced nephropathy: an update. Expert Opin Drug Saf. 2005;4:689–706.
Lopez-Novoa JM, Quiros Y, Vicente L, Morales AI, Lopez-Hernandez FJ. New insights into the mechanism of aminoglycoside nephrotoxicity: an integrative point of view. Kidney Int. 2011;79:33–45.
Dickenmann M, Oettl T, Mihatsch MJ. Osmotic nephrosis: acute kidney injury with accumulation of proximal tubular lysosomes due to administration of exogenous solutes. Am J Kidney Dis. 2008;51:491–503.
Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124–34.
Myburgh JA, Finfer S, Bellomo R, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–11.
Miller RP, Tadagavadi RK, Ramesh G, Reeves WB. Mechanisms of cisplatin nephrotoxicity. Toxins. 2010;2:2490–518.
Zaidan M, Lescure FX, Brocheriou I, et al. Tubulointerstitial nephropathies in HIV-infected patients over the past 15 years: a clinico-pathological study. Clin J Am Soc Nephrol. 2013;8:930–8.
Herlitz LC, Mohan S, Stokes MB, Radhakrishnan J, D’Agati VD, Markowitz GS. Tenofovir nephrotoxicity: acute tubular necrosis with distinctive clinical, pathological, and mitochondrial abnormalities. Kidney Int. 2010;78:1171–7.
Perazella MA. Tenofovir-induced kidney disease: an acquired renal tubular mitochondriopathy. Kidney Int. 2010;78:1060–3.
Luciano RL, Perazella MA. Crystalline-induced kidney disease: a case for urine microscopy. Clin Kidney J. 2015;8:131–6.
Yarlagadda SG, Perazella MA. Drug-induced crystal nephropathy: an update. Expert Opin Drug Saf. 2008;7:147–58.
Fleischer R, Johnson M. Acyclovir nephrotoxicity: a case report highlighting the importance of prevention, detection, and treatment of acyclovir-induced nephropathy. Case Rep Med. 2010;2010:1.
Chaudhari D, Crisostomo C, Ganote C, Youngberg G. Acute oxalate nephropathy associated with orlistat: a case report with a review of the literature. Case Rep Nephrol. 2013;2013:124604.
Singh A, Sarkar SR, Gaber LW, Perazella MA. Acute oxalate nephropathy associated with orlistat, a gastrointestinal lipase inhibitor. Am J Kidney Dis. 2007;49:153–7.
Perazella MA, Moeckel GW. Nephrotoxicity from chemotherapeutic agents: clinical manifestations, pathobiology, and prevention/therapy. Semin Nephrol. 2010;30:570–81.
Widemann BC, Balis FM, Kim A, et al. Glucarpidase, leucovorin, and thymidine for high-dose methotrexate-induced renal dysfunction: clinical and pharmacologic factors affecting outcome. J Clin Oncol. 2010;28:3979–86.
Chang HR, Pella PM. Atazanavir urolithiasis. N Engl J Med. 2006;355:2158–9.
Pacanowski J, Poirier JM, Petit I, Meynard JL, Girard PM. Atazanavir urinary stones in an HIV-infected patient. AIDS. 2006;20:2131.
Jao J, Wyatt CM. Antiretroviral medications: adverse effects on the kidney. Adv Chronic Kidney Dis. 2010;17:72–82.
Couzigou C, Daudon M, Meynard JL, et al. Urolithiasis in HIV-positive patients treated with atazanavir. Clin Infect Dis. 2007;45:e105–8.
Daudon M, Jungers P. Drug-induced renal calculi: epidemiology, prevention and management. Drugs. 2004;64:245–75.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Science+Business Media, LLC, part of Springer Nature
About this chapter
Cite this chapter
Luciano, R.L., Perazella, M.A. (2018). Drug-Induced Acute Kidney Injury. In: Waikar, S., Murray, P., Singh, A. (eds) Core Concepts in Acute Kidney Injury. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-8628-6_9
Download citation
DOI: https://doi.org/10.1007/978-1-4939-8628-6_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-8626-2
Online ISBN: 978-1-4939-8628-6
eBook Packages: MedicineMedicine (R0)