Abstract
Chronic respiratory diseases primarily affect the lung. Asthma, chronic obstructive pulmonary disease (COPD), bronchiectasis, lung cancer, lung fibrosis, sleep apnoea syndrome, pneumoconiosis and pleural diseases are common respiratory diseases worldwide. They present similar symptoms such as breathlessness on exertion, excess mucous production, chronic cough and wheezing. When these conditions are not adequately treated and/or become chronic may contribute to the development of systemic inflammatory comorbid disorders such as cardiovascular, musculoskeletal, psychiatric and cerebrovascular diseases. These comorbid disorders and pathophysiological mechanisms may vary in their manifestations, despite having similar symptoms. Comorbidities have major impact in patients with chronic respiratory diseases by impairing their quality of life, decreasing exercise capacity and increasing healthcare utilization. Therefore, it is important to screen patients with chronic respiratory diseases for comorbidities and monitor regularly. In addition, those identified with comorbidities should be referred for further assessment and to receive appropriate treatment which may include pharmacological therapy and non-pharmacological therapy (including exercise therapy and cognitive behavioural therapy) using a collaborative care model. Evidence from the available literature suggests that the effects of treating comorbidities in patients with chronic respiratory diseases are beneficial in short term improving quality-of-life patients and their caregivers. However, the long-term impact on clinical outcomes (e.g. healthcare utilization) is uncertain. Thus, well-controlled randomised control trails are needed.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Comorbidities
- COPD
- Hypertension
- Cerebrovascular disease
- Anaemia
- Lung cancer
- Cardiovascular disease
- Collaborative care
- Asthma
- Myocardial infarction
- Musculoskeletal
- Pulmonary hypertension
Introduction
Chronic respiratory diseases primarily affect the lung. Asthma, chronic obstructive pulmonary disease (COPD), bronchiectasis, lung cancer, lung fibrosis, sleep apnoea syndrome, pneumoconiosis and pleural diseases are common respiratory diseases worldwide [1]. They present similar symptoms such as breathlessness on exertion, excess mucous production, chronic cough and wheezing. When these conditions are not adequately treated and/or become chronic may contribute to the development of systemic inflammatory comorbid disorders such as cardiovascular, musculoskeletal, psychiatric and cerebrovascular diseases. These comorbid disorders and pathophysiological mechanisms may vary in their manifestations, despite having similar symptoms. Thus, it is beyond the scope of this chapter to cover all chronic respiratory diseases with their comorbid disorders to explain in detail. COPD was chosen because it is the most common respiratory disease, as an example, to explain and illustrate the impact of the resultant comorbidities and their management. In addition, the chapter briefly comments about comorbidities in Asthma and where appropriate references were made to other chronic respiratory diseases.
COPD is a major cause of morbidity and mortality in old age. In 2004, WHO [2] estimates about 210 million people are living with COPD worldwide. Out of these, 65 million have been physician diagnosed with moderate-to-severe COPD. It is quiet staggering number; only less than one third of the patients have been diagnosed with the disease. The majority of the people are living unaware of such a progressive disabling (debilitating) disease, which may have a major impact on their daily physical functioning, social interaction and their quality of life.
The rationale behind why a large proportion of patients with respiratory impairment remain undiagnosed with the disease is unclear. It is most likely to be a multifactorial including (e.g. lack of spirometer in practice to make accurate diagnosis), lack of public perception awareness the impact of respiratory disease(s), lack of dedicated service and staff manpower to manage patients with respiratory problems especially in developing countries and inadequate funding availability for chronic respiratory diseases research [3] compared with other chronic diseases for example, cardiovascular disease. Furthermore, in terms of disease and societal burden, COPD is projected to be the third leading cause of mortality by 2030 [4]. For example, in the USA, despite medical advancement in producing effective drug therapy for clinical management of COPD, in the past three decades, the death rates from COPD has been exponentially rising almost by twofold, while a significant decline observed in death rates from heart disease and stroke in the same period [5].
The recent Canadian population-based study from the administrative data (approximately 13 million people) [6] investigated the lifetime risk of developing of COPD. They found that the incidence of COPD was rising with increasing age. Men are at a higher lifetime risk of developing COPD compared to women. Those who live in rural areas and lower socio-economic status are at elevated risk of developing COPD compared to their counterparts of urban community-dwellers and higher socio-economic status, respectively. The lifetime incidence rate of physician-diagnosed COPD at the age of 50 was 2.6% (1000 person-years by age) and at the age of 80 years was 27.6% [6]. The exponential rise in the incidence of COPD with increasing age is quiet alarming and challenging. It is possible that older people are less likely to appreciate the subjective reduction in the perception of bronco-constriction and low expectation in physical functioning because of their age [7].
A population-based study in Italy (over 7 million people) [8] showed that the prevalence of COPD in adults aged 45 years and older was 3.6%. Of these, 126,283 COPD patients, the prevalence of COPD was related with increasing age. The prevalence of COPD was 1.9% in the age group 45–64 years, 4.8% in 65–74 years, 6.8% in 75–84 years and 5.6% in over 85 years. There was a significant gender difference in the prevalence of COPD, more common in males compared to women (4.1% in males and 3.1 in females). Historically and epidemiological evidences showed that men were high tobacco consumers (taking into account average pack-years) compared to women. This partly may have contributed to a high prevalence of COPD and deaths rate in men. In contrast to this, the recent mortality data, from the USA indicated that the number of women dying from COPD was surpassing that of men dying from COPD [9]. Why this might be a disease that requires further exploration? In 2012, Perera et al. [10] published a study that examined in the US the national inpatient survey of burden of acute exacerbations of COPD and the impact of comorbidities on inpatient costs and mortality. Their findings showed that women had more comorbidities compared to men. The total costs of managing COPD patients (n = 1,254,703 hospitalization) with acute exacerbations was US$11.9 billion. The inpatient mortality during admission was 4.3% (n = 53,748). A number of comorbidities (acute myocardial infarction; congestive heart failure; cerebrovascular disease; lung cancer; cardiac arrhythmias; pulmonary circulation disorders; and weight loss) may have contributed for both inpatient mortality and for incremental costs. In light of these findings, this chapter intends to update and synthesize the impact of comorbidities especially cardiovascular disease, depression and anxiety and lung cancer in patients with COPD. It will also explore the impact of other comorbidities on quality of life and healthcare utilization. Finally, it will provide succinct summary of clinical tips in how to manage these comorbid disorders.
Comorbidity implies to a disease coexisting with the main diagnosis of the patient, for example, the occurrence of depressive symptoms after the initial diagnosis of COPD. Comorbidities contribute to a substantial burden in increased disability and mortality in COPD patients in old age [5, 8, 9]. The causes of comorbidities in COPD patients are multifactorial and their manifestations are less clearly understood. There are several potential mechanisms for COPD patients to develop comorbidities compared with the general healthy population. COPD primarily affects the lung, and the irreversible and progressive nature of respiratory impairment and chronic inflammation of the disease are often associated with systemic manifestations outside the lung. The ongoing chronic inflammation of the airways in the lung especially those continued smoking with COPD and alterations in repair and in immune mechanisms tends to affect other organs and cardiovascular system in the body. Barnes and Celli [11] describe this phenomenon as the ‘spillover’ of the local airway inflammation through ‘inflammatory mediators into circulation may result to develop systemic manifestations of the disease, e.g. skeletal muscle wasting and cachexia’. Systemic inflammation (interleukin-6, interleukin-B and tumour necrosis factor) in turn may lead to worsen health status of patients with comorbid diseases, e.g. cardiovascular diseases.
A recent meta-analysis by Gan et al. [12] identified that reduced lung function was associated with raised levels of systematic inflammatory markers such as C-reactive protein (CRP), fibrinogen, leucocytes and tumour necrosis factor-alpha (TNF-alpha) in COPD patients compared with healthy controls. In addition, others have demonstrated [13] that lung function decline and systemic inflammation exhibited by the presence of elevated fibrinogen levels may contribute to frequent acute exacerbations in patients with COPD. Thus, further work is needed to explore the role of inflammatory markers in the pathogenesis of acute exacerbations in order to improve the clinical management of patients with COPD.
Comorbidities from Population-Based Studies
A recent Danish Nationwide population study of 7.4 million people [14] examined the prevalence of COPD and related comorbidities. Out of these, 313,958 people were suffering with COPD. The five common comorbidities in COPD patients were: 57,129 (18%) myocardial infarction, 32,577 (10.3%) diabetes, 24,408 (3.5%) lung cancer, 11,172 (3.5%) depression and 9608 (3%) with hip fracture. In addition, findings from the epidemiological cross-sectional study in Italy [7] revealed that the three common comorbidities with high prevalence were cardiovascular disease 80,840 (64%), diabetes 17,091 (12.4%) and depression 10,292 (8%). Furthermore in 2009, a nationwide telephone survey in the USA, in randomly selected of (n = 1003) COPD patients [15] the most commonly reported comorbidities were hypertension (58%), hypercholestromeia (52%), depression (37%), cataracts (31%) and osteoporosis (28%). Furthermore, a recent US retrospective observational study of 183,681 patients with COPD from a large administrative claims data set [16] identified that the four common comorbidities were cardiovascular disease (34.8%), diabetes (22.8%), asthma (14.7%) and anaemia (14.2%). Over 52% of the COPD patients had one or more comorbidities that significantly affect their daily activities and quality of life.
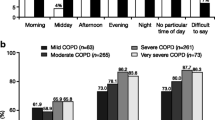
The variation in the spectrum of phenotype of comorbidities in patients diagnosed with COPD, population surveys are most likely because of heterogeneity of the sample, and the various methodologies adopted to collect data in different countries. The impact of comorbidities in COPD patients are multidimensional including increased risk of high levels of anxiety, decreased in physical functioning due to disuse muscle weaknesses and reduced in social interaction and dependency on caregivers in daily activities. All these factors may contribute to significant impairment in COPD patients’ physical activities and their quality of life as ‘disease burden’ increases illustrated in Table 9.1. Therefore, there is great uncertainty and challenges for the healthcare professionals in how best to treat elderly COPD patients with multiple comorbid chronic diseases including the potential drug side effects and toxicity.
Asthma and Comorbidities
Asthma is a common airway inflammatory disorder characterized by variable airway obstruction and hyperresponsiveness. It affects over 300 million people worldwide [1]. Uncontrolled asthma is a major cause of hospital admission and increased psychological morbidity in all ages. Boulet and Boulay [17] in a recent review identified that the most common comorbidities in patients with Asthma include rhinitis, sinusitis, gastroesophageal reflux disease, obesity, obstructive sleep apnoea, hormonal disorders and psychopathologies. These respiratory disorders share similar pathophysiological mechanism with asthma may influence asthma control, its phenotype and treatment.
Chronic asthma may coexist or develop to COPD especially in smoking asthmatic patients. Studies have shown that asthmatic patients who smoke may have early COPD, as indicated by more severe airway obstruction and lower carbon monoxide diffusion capacity [17, 18]. A recent systematic review [18] reported about 15–20% of COPD patients may have the asthma-COPD overlap syndrome (ACOS). ACOS is defined as with symptoms increased variability of airflow in association with an incompletely reversible airflow obstruction. Furthermore, patients with ACOS have more frequent exacerbations, more wheezing and dyspnoea, but similar cough and sputum production compared with COPD [18].
Recent clinical guidelines advocate [19] the identification and treatment of comorbidities should be an integral part of the chronic asthma management. Therefore, a comprehensive disease-management approach that is individually tailored which include education, weight loss management (diet and exercise), cognitive behavioural therapy and smoking cessation program are worthy of consideration for asthmatic patients with comorbid disorders.
Healthcare Utilization and COPD
In 2007, in the USA, the overall cost of COPD, pneumonia and asthma was approximately $85 billion. Out of these, $66 billion was for in direct healthcare expenditures (hospital and professional services, medication, medical equipment), and $19 billion was for in indirect mortality costs [20]. Of these expenditures, the large proportion of the healthcare budget was spent on patients with COPD. In 2002, Mannino et al. [9] reported that COPD was responsible for 8 million physician office and hospital outpatient visits, 1.5 million emergency department visits, 726,000 hospitalizations and 119,000 deaths. In five-year surveillance population-based study in Denmark, Blide et al. [21] examined the healthcare utilization in patients with COPD compared with the general population. The findings showed that COPD patients were (12 times per year) more likely to consult general practitioners for their health problems than patients without COPD. The total cost of managing COPD was over 256 million euro (approximately US$332 million). Further detailed analysis revealed that only one third of the cost was accounted for the primary diagnosis of COPD. Two-thirds of the COPD-related costs were mainly due to admissions for other diseases such as comorbid cardiovascular diseases, other respiratory diseases (e.g. pneumonia) and cancer. Thus, signify COPD patients with comorbid diseases are most likely to be high healthcare users compared without comorbidities. In a separate study [22] in the USA, COPD patients were more likely to utilize healthcare services and had excess total healthcare costs about $20,500 higher (p < 0.0001) than the comparison cohort of non-COPD patients. Comorbidities in COPD patients were high, accounting for 46% of the observed excess cost. Of these, ‘the impact on total healthcare costs was greatest for anaemia ($10,762 more, on average, than a patient with COPD without anaemia)’ [16].
Undiagnosed and/or in-adequately treated comorbidities in COPD patients will have detrimental effect on patients’ health status and substantial care burden to caregivers. COPD patients with several comorbidities are most likely to consult their general practitioners more frequently compared with one or two comorbidities [14, 19, 21]. COPD patients with multiple comorbidities are most likely to experience frequent episodes of acute exacerbations, with longer days of hospitalization and use more intensive care or high-dependency units compared without comorbidities [19, 20].
Cardiovascular Diseases in COPD
Cardiovascular diseases (CVD) and COPD are projected to be the second and fifths leading causes of mortality worldwide by 2030 [23]. In addition, COPD patients with comorbid CVD are most likely to live with increased burden of physical disability and impaired quality of life. The direct and indirect economic costs to the healthcare providers and the society are most likely to be enormous. In 2008, a retrospective cohort study in the USA by Dalal et al. [24] examined the total healthcare costs of COPD patients with CVD aged ≥40 years from the administrative data (n = 6000). They showed that the annual average direct medical costs per patient for COPD patients with comorbid CVD was $22,775 compared without CVD was $8036 (p < 0.001) and total costs were $27,032 versus $11,506 (p < 0.001), respectively. Furthermore, COPD patients with comorbid CVD twice most likely to be hospitalized and 47% more likely to have emergency room visits in a previous year compared with COPD patients alone. This provides some evidence that the healthcare professionals should treat CVD aggressively in order to reduce the burden in COPD patients, improve their quality of life and reduce healthcare cost.
Association of CVD with Systemic Inflammation and Vascular Damage
Both CVD and COPD share similar risk factors for developing the disease such as cigarette smoking and environmental air pollutions. However, the mechanism by which COPD patients develop CVD is unclear. Atherosclerosis is the main cause of CVD. Therefore, the early detection of atherosclerosis is crucial to identify patients with high risk in developing CVD and in planning appropriate intervention. Vascular function can be assessed non-invasively by measuring endothelial function and arterial stiffness, using pulse wave analysis derived measures (pulse wave velocity and augmentation index).
A recent study by MacLay et al. [25] with a relative small sample size (n = 18 COPD patients, n = 17 healthy controls) examined the vascular dysfunction of the participants with a lifetime exposure of smoking, controlling for the cardiovascular risk factors. They found that COPD patients have greater stiffness mean (SD) [pulse wave velocity, 11 (2) vs. 9 (2) m/s; p = 0.003; augmentation index, 27 (10) vs. 21 (6)%; p = 0.02] compared with health controls, independent of cigarette smoking exposure. In a larger prospective study (n = 102 COPD and n = 103 healthy controls), Mills and et al. [26] examined whether the occurrence of arterial stiffness and blood pressure in patients with COPD was higher than with age in a smoking matched healthy controls. Increased arterial stiffness and high blood pressure were exhibited in COPD patients compared with the healthy controls. In addition, serum C-reactive protein concentrations were threefold higher in COPD patients compared with healthy controls mean (SD), (6.1 (0.9) vs. 2.3 (0.4) mg/l; p = 0.001). Systemic inflammation and vascular dysfunction are the potential risk factors through which for COPD patients to develop cardiovascular disease. However, the exact mechanistic link is unclear, because of the study designs and relative small sample size to determine the causal association between COPD and vascular dysfunction. Larger randomised control trials are required.
Curkendall et al. [27] in a three-year follow-up study (n = 11,493) examined the incidence of cardiovascular events in patients with COPD. Their findings indicate that COPD patients with CVD experienced threefold to fourfold of increase in the rate of fatal cardiovascular events compared without COPD. In addition, COPD patients with comorbid CVD had twice the risk of premature mortality 2.07 (CI: 1.82–2.36) and all cause of mortality 2.82 (CI: 2.61–3.05) in comparison without CVD. In a separate study by Sidney et al., in a longitudinal study, [28] examined the relationship between COPD, incidence of CVD, hospitalization and mortality of patients with COPD (n = 45,966), with a similar number of the control group in four-year follow-up. They found that COPD was a risk factor for elevated cardiovascular-related mortality and hospitalization. Younger COPD patients (aged < 65 years) and female patients were at high risk of developing CVD. Therefore, CVD risk should be monitored and treated with particular care in younger adults with COPD. Hackett et al. [29] examined between the gene environment interactions, smoking and inflammatory markers (IL-6, interferon-y, interleukin-1b,) and COPD. Findings from this study showed that a polymorphism in the gene encoding IL-6 interacts with smoking history to influence the rate of lung function decline in patients with COPD as well as their risk of cardiovascular disease. A recent systematic review by Clarenbach et al. [30] postulated that systematic inflammation, oxidative stress, hypoxia, sympathetic activation and physical inactivity might be potential mechanisms in COPD leading to vascular dysfunction and cardiovascular disease as Shown in Fig. 9.1.
Postulated mechanisms of vascular damage in chronic obstructive pulmonary disease. From Clarenbach et al. [30], with permission of Taylor & Francis Ltd, www.tandfonline.com
Periodical evaluation of these clinical markers may play an important role to improve prognosis and reduce premature mortality in this patient group.
Myocardial Infarction
A recent UK primary care-based survey [31] by Schneider and colleagues investigated the prevalence of comorbidities in COPD patients (n = 35,700) identified that patients with COPD have a higher risk of developing myocardial infarction (40%), cardiac arrhythmia (19%), stroke (13%) and deep vein thrombosis (35%) compared with COPD-free counterparts. In a similar setting, Feary et al. [32] examined factors that are associated with COPD from computerized database primary care records of 1,204,100 million people in the UK. Physician-diagnosed COPD was associated with increased risks of CVD (odds ration 4.98, 95% CI 4.85–5.81; p < 0.001), stroke (odds ratio 3.34, 95% CI 3.21–3.48; p < 0.001) and diabetes mellitus (odds ration 2.04, 95% CI 1.97–2.12; p < 0.001). Further analysis was performed adjusting for the confounding factors sex and smoking status and stratifying for age. Their findings indicate that the greatest increase in the rate of ‘acute arteriovascular events was found in the youngest age groups, the hazard ratio for acute MI was 10.34 (95% CI 3.28–32.60; p < 0.001) and for stroke the hazard ratio was 3.44 (95% CI 0.85–13.84; p < 0.001) compared with the oldest age group’. They have highlighted the importance of an integrated collaborative treatment approach to deal with the excess comorbidities. McAllister et al. [33] in a prospective study (n = 242) COPD patients aged 40 years and above admitted with acute exacerbations with a smoking history of 10 pack-years were examined at discharge to determine the potential risk factors to develop MI. Their findings showed that 1 in 12 of patients met the diagnosis criteria for MI. None of the patients was receiving appropriate care for comorbid MI. This indicates undiagnosed MI was relatively common in patients with COPD. Future research has to focus on early detection and treatment strategies to reduce the risk of MI in COPD patients.
Pulmonary Arterial Hypertension
Pulmonary arterial hypertension (PAH) is common in patients with severe advanced COPD, but the prevalence in mild-to-moderate COPD is unknown. Thabut et al. [34] explored the prevalence of PAH in severe COPD patients (n = 251) who had a lung volume reduction surgery or lung transplantation surgery. Over fifty per cent of the COPD patients were identified with hypertension with mean pulmonary artery pressure (PAPm) > 25 mm Hg, but in patients with moderate (PAPm, 35–45 mm Hg) or severe (PAPm > 45 mm Hg) in 9.8% and in 3.7% of COPD patients, respectively. The severity of pulmonary hypertension was associated with the severity of lung function impairment and with hypoxia. The exact mechanism in how pulmonary hypertension manifest in COPD patients is unclear. It is most likely to be multifactorial. Variables that increase pulmonary vascular resistance may also increase the ‘pulmonary wedge pressure of left ventricular dysfunction or severe airway obstruction with wide intrathroacic pressure swings, and destruction of lung parenchyma leading to loss of part of the pulmonary vascular bed may play a role’ [35]. Given this proposition in patients with mild-to-moderate COPD, the pulmonary arteries may exhibit an enlarged intima, because of the proliferation of poorly differentiated smooth muscle cells and deposition of elastic and collagen fibres, with reduction in the lumen and arteriolar muscularization [36]. However, the contribution of hypoxic vasoconstriction to the ventilation-perfusion ratio balances to be greater in mild COPD but is less active in moderate-to-severe COPD. All these changes may contribute to the dysfunction of the vascular structure and function in COPD patients, for detailed review see [35]. The exact role of systemic inflammation in PAH patients is unknown. Peinado et al. [36] have shown that (current cigarette smoking was associated with elevated CD8+ T-lymphocytes and neutrophils) inflammatory process in the pathogenesis of pulmonary vascular abnormalities in the early stage of COPD. Furthermore, vascular abnormalities impair gas exchange and may result in pulmonary hypertension, which is one of the principal factors associated with reduced survival in COPD patients [35, 36].
The management of COPD patients with PAH requires a systematic and coherent treatment approach. Minai et al. provide [35] the most helpful strategy in the management of PAH in COPD patients: (1) confirm the diagnosis using Doppler echocardiography; (2) optimize COPD management; (3) rule out other comorbidities; (4) assess and treat hypoxemia; and (5) enrol the patient to pulmonary rehabilitation programme.
Table 9.2 provides variable related to develop cardiovascular diseases the majority are modifiable risk factors, which fall under the umbrella lifestyle issues. Thus, coordinated, integrated and innovative public healthcare programme is most likely to be beneficial for patients with COPD. Therefore, the focus should be to change attitudes and maximize lifestyle-related interventions for self-management. Those COPD patients with high-risk CVD profiles should be referred to experts in the field for proper assessment and treatment and periodically monitored by their general practitioners. It is advisable for patients to be encouraged in a self-management programme to stop cigarette smoking, to be involved in a regular physical exercise programme, e.g. regular walking exercise 2–3 times per week for the duration of 30 min. It is beyond the scope of this chapter to discuss the whole medical management for patients with cardiovascular diseases. Therefore, readers are encouraged to read the detail guidance provided by the WHO and the National Institute for Clinical Excellence guidelines for cardiovascular diseases [37, 38].
Depression in COPD
Depression is common in patients with COPD. A recent systematic review in our department [39] identified the prevalence clinically significant depression was between 8 and 80%. This is comparable to patients with chronic heart failure with clinically importance of depression range between 10 and 60%. The recent update of the National Institute Clinical Excellence for the management of COPD highlighted the importance of early screening and treating depression effectively to remission [40]. Untreated and under-recognized depressive symptoms in patients with COPD were associated with poor adherence with medical treatment [41], early dropout from pulmonary rehabilitation [42], frequent consultations with the general practitioners and frequent episodes of emergency care and hospital admission, and all these factors may contribute to premature mortality [39–41].
Risk Factors Associated with Depression in COPD
There are a number of risk factors that are associated with elevated depression in patients with COPD including increase in physical disability, low socio-economic status, social isolation, reduced lung function and low body mass index [39, 40]. In addition, an increase in physical disability was a predictive factor for the subsequent onset of depression in the preceding year. Depression in COPD patients often interferes with self-care management, adherence to medical treatment, persistence in active smoking and loss of interest in pleasurable activities, in turn all these factors may lead to a gradual decline in health status and social interaction [39–42]. However, there is limited understanding in terms of the pathways to trigger depression in patients with COPD. The interaction between COPD and developing depressive symptoms in older patients is dynamic in nature, but the exact mechanism it manifests is not fully understood. It is likely to be a multifactorial.
The pathway in which COPD patients develop depression is not clear. It is most likely as the result of complex interaction between physiological, physical and psychosocial factors. There is a possibility of a bidirectional two-way relationship. Smoking cigarette is the main cause of developing COPD. It is possible that COPD patients with depression are most likely to continue smoking because of loss of interest or motivation to quit due to the low mood. Therefore, there is a link between smoking cigarettes and depression but the particular mechanism is not clear. It does not follow a single pathway. Future studies may explore the bidirectional relationship in a longitudinal study, and the aetiology of depression in elderly patients with COPD, e.g. the relationship with cardiovascular diseases and degenerative changes in the brain.
Minor depressive symptoms that do not meet the criteria for major depression are common in patients with COPD [43] and point of prevalence estimated at 25%. They are associated with increased physical disability and impaired quality of life in patients with COPD and part of continuum with major depression [44, 45]. Depression has been associated with increased healthcare utilization [45], episodes for frequent hospital readmission and longer days of hospital stay [46] and premature mortality [47]. Katz et al. [48] in a longitudinal study identified increased physical disability was a strong predictive factor for the new onset of depression.
A recent review [49] showed that pulmonary rehabilitation in a short term may be useful in reducing anxiety and depressive symptoms in patients with COPD. However, the long-term efficacy is unknown. A few studies [50, 51] have shown that cognitive behavioural therapy (CBT) helps to reduce depressive symptoms in patients with COPD. It is quiet promising and novel treatment approach to incorporate CBT as part of routine clinical practice. Currently, CBT is quiet scarce for the wider healthcare provision. Innovative approach such as web-based CBT is worthy of consideration.
The use of antidepressant drug therapy for COPD patients with depression is inconclusive [52]. It is partly to do patients refusals to receive antidepressant drug therapy. It is possible that patients do not see the relevance of treatment seeing the gloomy picture of their condition or the impact of depression in their life. Some of the perceived barriers reported by the COPD patients include: Stigma attached to depression, afraid of side effects, Fed up, angry, denial and not bothered, fear of being addicted to antidepressant medication, belief that having depression is a weakness and frustrated with taking too many drugs [43, 52].
Therefore, it is important to teach and educate patients about the perceived barriers of treatment of depression in COPD patients. The collaborative care model using a case manager has been shown to be beneficial to improve treatment adherence and improve depression treatment [53]. Therefore, further work is required to determine the cost efficacy of this kind of treatment approach.
Anxiety
The prevalence of potentially clinical anxiety symptoms ranges between 6 and 74% in patients with COPD [39]. This figure is similar to patients with chronic heart failure with anxiety symptoms, which was between 11 and 45%. Anxiety has been shown to be associated with poor health outcomes including decreased in exercise tolerance, with greater risk of self-related functional limitations, frequent episodes of hospital readmission and impaired quality of life [54, 55].
Anxiety disorders in patients with COPD are heterogeneous than depression, including diverse diagnoses such as generalized anxiety disorder, social phobia, phobic anxiety, obsessive-compulsive disorder and post-traumatic disorder [56]. There is very little or no epidemiological data available to determine the accurate prevalence of these disorders in patients with COPD. In addition, the management of anxiety in patients with COPD is often suboptimal. Kim et al. [57] reported that only a quarter of people with COPD and moderate-severe anxiety were receiving appropriate treatment. Two studies have shown that CBT was effective in reducing anxiety symptoms in patients with COPD [50, 51]. Kunik et al. [50] demonstrated that there was no difference in the efficacy between educational programme and CBT in 12-month follow-up programme in reducing anxiety symptoms in patients with COPD. Therefore, larger randomized controlled trials are needed to examine the cost efficacy of CBT in patients with COPD.
Lung Cancer in COPD
Lung cancer is an overwhelming additional life-limiting disease with profound impact on COPD patients’ survival, impairing their quality of life, compromising their coping strategies and increases caregivers’ anxiety and burden.
The prevalence of lung cancer in patients with COPD estimated between 40 and 70% dependent on diagnostic criteria, age, gender and duration of smoking exposure [58, 59]. Wasswa-Kintu et al. have shown that COPD patients are four times likely at a risk of developing lung cancer [60] compared with smokers with normal lung function. After controlling for the disease severity, a recent meta-analysis reported that an established diagnosis of COPD plus radiologic evidence of emphysema gave 2.64 times relative risk of lung cancer compared with non-COPD patients [61]. Furthermore, Young et al. [59] have demonstrated the prevalence of COPD in newly diagnosed lung cancer cases was sixfold greater than in matched smokers. In a separate study by de Tores et al. [62], the incidence of lung cancer in patients with COPD was (incidence density of 16.7 cases per 1000 person-years) higher compared to 4.2 cases per 1000 person-years in Towards a Revolution in COPD Health [63]. In this study, the most frequent type of histological subtype was squamous cell cancer (44%). Others have reported [62] that COPD increases the risk of the squamous cell histological subtype by more than four times, while chronic bronchitis relates to adenocarcinoma.
The risk factors to develop lung cancer are multifactorial. A recent editorial [64] from our department reported that COPD patients with the following characteristics are prone (susceptible) to develop lung cancer:
-
Older people with COPD
-
Low body mass index
-
Active smoking status
-
Diffusion capacity for carbon monoxide <80% predicted
-
Global Initiative for chronic obstructive lung disease stages (I and II)
-
Severe COPD
-
Emphysema
-
Chronic airway inflammation
-
Inhaled corticosteroids
-
Occupational exposure to diesel motor exhaust
-
Occupational exposure to organic dust.
The disease manifestations are multifactorial. The pathological processes are incompletely understood. It is most likely as the result of complex interaction of physiological (lung function impairment), environmental pollutions (fumes and dusts), social habits (active smoking) and chronic inflammation, which predispose COPD patients to lung cancer [63, 64]. In addition, the potential mechanisms for the increased risk lung cancer in COPD are unclear. Chronic inflammation, which is common in COPD, is most likely to play an important role in the pathogenesis of lung cancer. Given this proposition, patients with COPD are most likely to experience a multiple episodes of respiratory infection with two or three times the rate of hospital admission per annum [40]. Papi et al. [65] have postulated that repeated chest infections tend to affect the function of the mucociliary clearance system, compromising its ability to remove carcinogens and other damaging substances present in cigarette smoke. This may contribute for the development of airways obstruction in the distal airways that may lead to emphysema. Furthermore, persistent exposure of the bronchial epithelium to active cigarette smoking precipitates irritation of the lumen, which allows carcinogens for increased access to the epithelium (increase permeability) and produces low-grade inflammation over a period of time and these carcinogens may promote pathologic changes leading to squamous cell neoplasia [65].
In 2011, a comprehensive review by Raviv et al. [66] examined the surgical options for patients with COPD with comorbid lung cancer. The review showed that surgical intervention (e.g. tumour resection, lobectomy and combining lung volume reduction surgery) with curative intent may have better survival outcomes compared with non-surgical intervention. However, COPD patients with lung cancer often do not fulfil the inclusion criteria for surgery because of the severity of lung function impairment and poor exercise tolerance. Therefore, further work is required to determine the efficacy of various options of surgical procedures in randomized controlled clinical trials. Current availability of palliative care for patients with severe COPD is very scant. Those COPD patients identified with lung cancer should receive a holistic and integrated palliative care treatment to improve their quality of life and reduce healthcare cost.
Osteoporosis in COPD
Osteoporosis is one of the systemic features of COPD. It is a systemic skeletal disease characterized by low bone mineral density (BMD) and micro architectural changes in bone tissue that increases the susceptibility to fractures [67].
Anaemia in COPD
A recent systematic review [68] identified the prevalence of comorbid anaemia in patients with COPD ranges from 7.5 to 34% depending upon the populations selected and diagnostic tools employed to determine the level of haemoglobin. Comorbid anaemia in patients with COPD was associated with greater healthcare resource utilization, impaired quality of life, older age and male gender. Furthermore, anaemia in patients with COPD is an independent prognostic predictor of premature mortality and a greater likelihood of hospitalization.
Although the precise cause of anaemia in COPD patients is unknown, there appears to be a relationship with certain proinflammatory markers suggesting that at least a component of the observed anaemia in that often attribute to inflammation i.e. the anaemia of chronic inflammation) [69]. Moreover, the cause of anaemia in patients with COPD is most likely that observed in other chronic inflammatory diseases including nutritional deficits, stress ulcer (especially those on steroids) carboxyhemoglobin effects of cigarette smoking. Compromised oxygen delivery may also impact cardiac and renal function [68].
To date very little work has been done to treat comorbid anaemia in randomized control trial setting in patients with COPD. Therefore, robust and prospective studies are needed in well-characterized COPD patients to determine the true prevalence, consequence of concomitant anaemia and efficacy of intervention. Furthermore, research design should include longitudinal assessment to both lung function and haemoglobin level to account for any changes during exacerbation-free periods in patients with COPD and to establish the influence of anaemia on the natural history of COPD.
Cognitive Impairment
Cognitive impairments such as problems with working memory, executive functioning, visuospatial and attention are common in patients with COPD. Untreated cognitive impairments may compromise an individual's ability to manage his/her own personal care, dependency on caregivers, non-adherence to medical treatment or rehabilitation, increase disability and healthcare utilization [70]. The latest systematic review and meta-regression analysis in our department [71] in patients with COPD showed one in four patients had MCI. None of the studies reported the efficacy of intervention to treat MCI. Future work should focus on ways of detection, managing and treatment of MCI in this patient group.
Clinical Implications of Comorbidities
Comorbid conditions may influence the diagnosis and assessment of the severity, self-management and control of patients with chronic respiratory diseases.
Evidence from the available literature suggest that the effect of treating comorbidities in patients with chronic respiratory diseases and long-term clinical outcomes are uncertain. Thus, well-controlled randomized control trials are needed.
All the projections indicate that COPD and asthma are growing problems worldwide and the incidence are most likely to rise in the next few decades before they level off. They may warrant public awareness campaign of their burden and screening healthy populations’ especially current smokers for early detection and treatment of COPD and asthma.
Comorbidities are common in COPD and asthma patients. Current medical approach is not sufficient to alleviate social and economic burden of the disease. Therefore, a comprehensive medical and psychosocial approach using a collaborative care model might help to reduce the impact of the disease to patients, caregivers and society.
COPD is a potential risk factor for developing cardiovascular disease. However, the mechanisms it develops less clear. The potential postulated mechanism is most likely because of complex interaction of systemic inflammation, hypoxia, sympathetic activation, oxidative stress and physical inactivity.
Depression and anxiety are common in patients with COPD and asthma. They are often under-recognized and under-treated. Therefore, healthcare professionals should play an active role to identify these psychiatric disorders using screening tools during routine consultations.
Current evidence suggests that simply offering antidepressant drug therapy for COPD patients with depression is not an effective method to treat this patient group. Collaborative care model which involve patients in self-management programme is worthy of consideration.
The role of systemic inflammatory markers in the pathogenesis of depression and cardiovascular disease in patients with COPD are worthy of exploration.
COPD is a risk factor for developing lung cancer. It is important to assess high-risk COPD patients periodically for lung cancer in order to provide appropriate early curative intent intervention.
Conclusion
The impact of comorbidities on COPD and asthma patients’ quality of life and healthcare utilization is most likely to be enormous in the next few years. Therefore, it is important to screen patients for comorbidities and monitor regularly for potential side effects after a change in health status or a significant lifetime event (e.g. after loss of a job or loss of the loved ones). Those identified with clinically depression should be treated promptly with appropriate pharmacological (antidepressant drug therapy) and non-pharmacological therapy (including exercise therapy and cognitive behavioural therapy).
The findings of this review highlight factors that contribute to cardiovascular diseases, lung cancer and major depressive episodes in patients with COPD are multifactorial. The majority of COPD patients are most likely from the disadvantaged lower socio-economic status, who are prone to high psychosocial morbidity, e.g. elevated active smoking, overweight status and low physical inactivity. Therefore, the time has come for close collaboration between secondary/tertiary healthcare providers and primary healthcare and social care services to mobilize resources and devise innovative long-term public health initiatives, for example, smoking cessation and obesity in order management to reduce the burden of lung cancer, cardiovascular diseases and depression to the wider society.
References
WHO. Chronic respiratory diseases. Accessed on 31 July 2015. http://www.who.int/gard/publications/chronic_respiratory_diseases.pdf.
WHO. Chronic obstructive pulmonary disease. Fact sheet No. 315. November 2011. Accessed 15 Feb 2012. http://www.who.int/mediacentre/factsheets/fs315/en/index.html.
Gillum LA, Gouveia C, Dorsey ER, Pletcher M, Mathers CD, McCulloch CE, Johnston SC. NIH disease funding levels and burden of disease. PLoS ONE. 2011;6(2):e16837.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine. 2006;3:e442.
Jemal A, Ward E, Hao Y, Thun M. Trends in the leading cause of death in the United States, 1970–2002. JAMA. 2005;294:1255–9.
Gershon AS, Warner L, Cascagnette P, Victor JC, To T. Lifetime risk of developing chronic obstructive pulmonary disease: a longitudinal population study. Lancet. 2011;378:991–6.
Marks GB, Yates DH, Sist M, Ceyhan B, DeCampos M, Scott DM, Barnes PJ. Respiratory sensation during bronchial challenge testing with methacholine, sodium metabisulphite and adenosine monophosphate. Thorax. 1996;51:793–8.
Anechino C, Rossi E, Fanizza C, De Rosa M, Tognoni G, Romero M, for working group “ARNO project”. Prevalence of chronic obstructive pulmonary disease and pattern of comorbidities in a general population. Int J COPD 2007;2(4):567–74.
Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance–United States, 1971–2000. Respir Care. 2002;47(10):1184–99.
Perera PN, Armstrong EP, Sherrill DL, Skrepnek GH. Acute exacerbations of COPD in the United States: inpatient burden and predictors of costs and mortality. COPD. 2012;9(2):131–41.
Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33:1165–85.
Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59(7):574–80.
Groenewegen KH, Postma DS, Hop WC, Wielders PL, Schlösser NJ, Wouters EF, COSMIC Study Group. Increased systemic inflammation is a risk factor for COPD exacerbations. Chest. 2008;133(2):350–7.
Sode BF, Dahl M, Norddestgaard BG. Myocardial infarction and other co-morbidities in patients with chronic obstructive pulmonary disease: a Danish nationwide study of 7.4 million individuals. Eur Heart J. 2011;32:2365–75.
Barr RG, Celli BR, Mannino DM, Petty T, Rennard SI, Sciurba FC, Stoller JK, Thomashow BM, Turino GM. Comorbidities, patient knowledge, and disease management in a national sample of patients with COPD. Am J Med. 2009;122:348–55.
Mannino DM, Higuchi K, Yu TC, Zhou H, Li Y, Tian H, Suh K. Economic burden of COPD in the presence of comorbidities. Chest. 2015;148(1):138–50.
Boulet L-P, Boulay M-E. Asthma-related comorbidities. Expert Rev Respir Med. 2011;5(3):377–93.
Barrecheguren M, Esquinas C, Miravitlles M. The asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): opportunities and challenges. Curr Opin Pulm Med. 2015;21(1):74–9.
Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, Hanania NA, ACCP Workshop Panel on Anxiety and Depression in COPD. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest 2008;134(4 Suppl):43S–56S.
National Heart Lung Blood Institute Factbook FY 2010. Bethesda, MD: National Institutes of Health/National Heart, Lung and Blood Institute, 2010. http://www.nhlbi.nih.gov/about/factbook/FactBook_2010.pdf.
Bilde L, Rud Svenning A, Dollerup J, Baekke Borgeskov H, Lange P. The cost of treating patients with COPD in Denmark—a population study of COPD patients compared with non-COPD controls. Respir Med. 2007;101(3):539–46.
Menzin J, Boulanger L, Marton J, Guadagno L, Dastani H, Dirani R, Phillips A, Shah H. The economic burden of chronic obstructive pulmonary disease (COPD) in a U.S. medicare population. Respir Med. 2008;102(9):1248–56.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442.
Dalal AA, Shah M, Lunacsek O, Hanania NA. Clinical and economic burden of patients diagnosed with COPD with comorbid cardiovascular disease. Respir Med. 2011;105(10):1516–22.
Maclay JD, McAllister DA, Mills NL, Paterson FP, Ludlam CA, Drost EM, Newby DE, Macnee W. Vascular dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180(6):513–20.
Mills NL, Miller JJ, Anand A, Robinson SD, Frazer GA, Anderson D, Breen L, Wilkinson IB, McEniery CM, Donaldson K, Newby DE, Macnee W. Increased arterial stiffness in patients with chronic obstructive pulmonary disease: a mechanism for increased cardiovascular risk. Thorax. 2008;63(4):306–11.
Curkendall SM, DeLuise C, Jones JK, et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann Epidemiol. 2006;16(1):63–70.
Sidney S, Sorel M, Quesenberry CP. COPD and incident cardiovascular disease hospitalization and mortality: Kaiser Permnante medical care program. Chest. 2005;128:2068–75.
Hackett TL, Stefanowicz D, Aminuddin F, Sin DD, Connett JE, Anthonisen NR, Paré PD, Sandford AJ. Effect of gene environment on lung function and cardiovascular disease in COPD. Intern J Chron Obst Pulmon Dis. 2011;6:277–87.
Clarenbach CF, Thurnheer R, Kohler M. Vascular dysfunction in chronic obstructive pulmonary disease: current evidence and perspectives. Expert Rev Respir Med. 2012;6(1):37–43.
Schneider C, Bothner U, Jick SS, Meier CR. Chronic obstructive pulmonary disease and the risk of cardiovascular diseases. Eur J Epidemiol. 2010;25(4):253–60.
Feary JR, Rodrigues LC, Smith CJ, Hubbard RB, Gibson JE. Prevalence of major comorbidities in subjects with COPD and incidence of myocardial infarction and stroke: a comprehensive analysis using data from primary care. Thorax. 2010;65(11):956–62.
McAllister DA, Maclay JD, Mills NL, Leitch A, Reid P, Carruthers R, O’Connor J, McAlpine L, Chalmers G, Newby DE, Clark E, Macfarlane PW, Macnee W. Diagnosis of myocardial infarction following hospitalisation for exacerbation of COPD. Eur Respir J 2012;9 (Epub ahead of print).
Thabut G, Dauriat G, Stern JB, Logeart D, Lévy A, Marrash-Chahla R, Mal H. Pulmonary hemodynamics in advanced COPD candidates for lung volume reduction surgery or lung transplantation. Chest. 2005;127(5):1531–6.
Minai OA, Chaouat A, Adnot S. Pulmonary hypertension in COPD: epidemiology, significance, and management: pulmonary vascular disease: the global perspective. Chest. 2010;137(6 Suppl):39S–51S.
Peinado VI, Pizarro S, Barberà JA. Pulmonary vascular involvement in COPD. Chest. 2008;134(4):808–14.
World Health Organization. Prevention of cardiovascular disease. Guidelines for assessment and management of cardiovascular risk. 2007, Geneva. http://whqlibdoc.who.int/publications/2007/9789241547178_eng.pdf.
National Institute for Health and Clinical Excellence. Prevention of cardiovascular disease at population level. 2010, London. http://www.nice.org.uk/nicemedia/live/13024/49273/49273.pdf.
Yohannes AM, Willgoss T, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance and management principles. Int J Geriatr Psychiatry. 2010;25(12):1209–21.
National Collaborating Centre for Chronic Conditions. Chronic obstructive pulmonary disease: national clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. London: NICE; 2010.
Yohannes AM. Management of anxiety and depression in patients with COPD. Expert Rev Resp Med. 2008;2:337–47.
Garrod R, Marshall J, Barley E, Jones PW. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J. 2006;27(4):788–94.
Yohannes AM, Baldwin RC, Connolly MJ. Prevalence of sub-threshold depression in elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry. 2003;18:412–6.
Kessler RC, Zhao S, Blazer DG, Swartz MJ. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord. 1997;45(1–2):19–30.
Ng TP, Niti M, Tan W-C, Cao Z, Ong K-C, Eng P. Depressive symptoms and chronic obstructive pulmonary disease. Effect on mortality, hospital readmission, symptom burden, functional status and quality of life. Arch Intern Med. 2007;167:60–7.
Coultas DB, Edwards DW, Barnett B, Wludyka P. Predictors of depressive symptoms in patients with COPD and health impact. J Chron Obstr Pulm Dis. 2007;4:23–8.
Yohannes AM, Baldwin RC, Connolly MJ. Predictors of 1-year mortality in patients discharged from hospital following acute exacerbation of chronic obstructive pulmonary disease. Age Ageing. 2005;34:491–6.
Katz PP, Julian LJ, Omachi TA, Gregorich SE, Eisner MD, Yelin EH, Blanc PD. The impact of disability on depression among individuals with COPD. Chest. 2010;137(4):838–45.
Coventry PA. Does pulmonary rehabilitation reduce anxiety and depression in chronic obstructive pulmonary disease? Curr Opin Pulm Med. 2009;15(2):143–9.
Kunik ME, Veazey C, Cully JA, Souchek J, Graham DP, Hopko D, Carter R, Sharafkhaneh A, Goepfert EJ, Wray N, Stanley MA. COPD education and cognitive behavioural therapy group treatment for clinically significant symptoms of depression and anxiety in COPD patients: a randomized controlled trial. Psychol Med. 2007;37:1–12.
Hynninen MJ, Bjerke N, Pallesen S, Bakke PS, Nordhus IH. A randomized controlled trial of cognitive behavioral therapy for anxiety and depression in COPD. Respir Med. 2010;104(7):986–94.
Yohannes AM, Connolly MJ. Do antidepressants work in patients with chronic obstructive pulmonary disease with comorbid depression? Expert Rev Respir Med. 2011;5(6):727–9.
Sirey JA, Raue PJ, Alexopoulos GS. An intervention to improve depression care in older adults with COPD. Int J Geriatr Psychiatry. 2007;22:154–9.
Eisner MD, Blanc PD, Yelin EH, Katz PP, Sanchez G, Iribarren C, Omachi TA. Influence of anxiety on health outcomes in COPD. Thorax. 2010;65(3):229–34.
Yohannes AM, Baldwin RC, Connolly MJ. Depression and anxiety in elderly out-patients with chronic obstructive pulmonary disease: prevalence and validation of BASDEC screening questionnaire. Int J Geriatr Psychiatry. 2000;15:1090–6.
Brenes GA. Anxiety and chronic obstructive pulmonary disease: prevalence, impact and treatment. Psychosom Med. 2003;65:963–70.
Kim HF, Kunik ME, Molinari VA, Hillman SL, Lalani S, Orengo CA, Petersen NJ, Nahas Z, Goodnight-White S. Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics. 2000;41(6):465–71.
Loganathan RS, Stover DE, Shi W, et al. Prevalence of COPD in women compared to men around the time of diagnosis of primary lung cancer. Chest. 2006;129:1305–12.
Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J. 2009;34:380–6.
Wasswa-Kintu S, Gan WQ, Man SF, Pare PD, Sin DD. Relationship between reduced forced expiratory volume in one second and the risk of lung cancer: a systematic review and meta-analysis. Thorax. 2005;60:570–5.
Brenner DR, McLaughlin JR, Hung RJ. Previous lung diseases and lung cancer risk: a systematic review and meta-analysis. PloS One 2011;6:e17479.
de Torres JP, Marin JM, Casanova C, Cote C, Carrizo S, Cordoba-Lanus E, Baz-Davila R, Zulueta J, Aguirre-Jaime A, Saetta M, Cosio MG, Celli BR. Lung cancer in patients with chronic obstructive pulmonary disease. Incidence and predicting factors. Am J Respir Crit Care Med. 2011;184:913–9.
McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA, TORCH Clinical Endpoint Committee. Ascertainment of cause-specific mortality in COPD: operations of the TORCH clinical endpoint committee. Thorax. 2007;62:411–5.
Yohannes AM. Lung cancer in COPD patients is a double blow. Expert Rev Respir Med. 2012;6:6–9.
Papi A, Casoni G, Caramori G, Guzzinati I, Boschetto P, Ravenna F, Calia N, Petruzzeli S, Corbetta L, Cavallesco G, Forini E, Saetta M, Ciaccia A, Fabbri LM. COPD increases the risk of squamous histological subtype in smokers who develop non-small cell lung cancer carcinoma. Thorax. 2004;59:679–81.
Raviv S, Hawkins KA, DeCamp MM Jr, Kalhan R. Lung cancer in chronic obstructive pulmonary disease: enhancing surgical options and outcomes. Am J Respir Crit Care Med. 2011;183(9):1138–46.
WHO Scientific Group on the Prevention and Management of Osteoporosis. Prevention and management of osteoporosis: report of a WHO scientific group [WHO technical report series; 921], http://whqlibdocwhoint/trs/WHO_TRS_921pdf; 2007.
Yohannes AM, Ershler WB. Anemia in chronic obstructive pulmonary disease: a systematic review of the prevalence, quality of life and mortality. Respir Care. 2011;56(5):644–52.
Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005;352(10):1011–23.
Yohannes AM. Cognitive impairment and risk of disability in patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11(9):1445–56.
Yohannes AM, Chen W, Moga AM, Leroi I, Connolly MJ. Cognitive impairment in chronic obstructive pulmonary disease and chronic heart failure: a systematic review and meta-analysis of observational studies. ERJ. 2016;48(60):874.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media LLC
About this chapter
Cite this chapter
Yohannes, A.M. (2017). The Impact of Comorbidities in Patients with Chronic Respiratory Diseases. In: Sharafkhaneh, A., Yohannes, A., Hanania, N., Kunik, M. (eds) Depression and Anxiety in Patients with Chronic Respiratory Diseases. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-7009-4_9
Download citation
DOI: https://doi.org/10.1007/978-1-4939-7009-4_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-7007-0
Online ISBN: 978-1-4939-7009-4
eBook Packages: MedicineMedicine (R0)