Abstract
Cardiovascular disease remains the leading cause of mortality in the developed world and results in a heavy economic burden on society. It is largely preventable if modifiable risk factors are successfully addressed. In order for preventive efforts to be successful, a concerted approach to care by the clinician, the patient, and their families and larger societal initiatives for both education and creation of the needed infrastructure for a healthier lifestyle are necessary. A good clinician plays a crucial role, as a diagnostician, advisor, and supporter for his/her patient. A multipronged approach at prevention is needed and focuses on the following aspects: supporting increased physical activity especially in sedentary patients; strongly advising tobacco cessation in smokers; encouraging weight loss in overweight and obese patients; discussing a balanced and healthy approach to diet; as well as identifying and treating known cardiovascular disease risk factors of hypertension, hyperlipidemia, metabolic syndrome, and diabetes. It is important for the clinician to be comfortable with both non-pharmacological (lifestyle modification, dietary, etc.) and pharmacological approaches to address most of these critical factors in primary and secondary prevention. Successful prevention efforts have been clearly shown to decrease mortality as well as cardiovascular events and are a critical part of every clinician’s responsibility in prolonging and improving the lives of his/her patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Prevention
- Cardiovascular disease
- Tobacco use
- Hypertension
- Hyperlipidemia
- Physical activity
- Sedentary lifestyle
- Nutrition
- Obesity
7.1 Introduction
Cardiovascular disease (CVD) which encompasses coronary heart disease, stroke, and peripheral artery disease remains the leading cause of mortality in the developed world, notwithstanding significant advances in the prevention and acute management of these syndrome s [1]. Despite a remarkable decline in mortality due to therapeutic and preventive measures, CVD still accounts for 33.6 % of all deaths in the USA and is the cause of 1 death every 36 s in the USA alone. Notably, males continue to experience far higher mortality rates at earlier ages than their female counterparts.
The economic burden of CVD was estimated at $444 billion in 2010, with the treatment of these diseases accounting for $1 of every $6 spent on healthcare in the USA. CVD remains the leading cause of hospitalization in the USA.
Most known risk factors for developing CVD are modifiable by preventive measures. These risk factors include cigarette smoking, sedentary lifestyle, dyslipidemia, hypertension, diabetes, metabolic syndrome, abdominal obesity, lack of regular exercise, and poor diet. According to the CDC, an estimated 68 million adults have hypertension (with only one half having their blood pressure controlled adequately) and 71 million have hyperlipidemia (with only one third having adequate treatment for this condition).
Simply stated, prevention saves lives. This chapter will address primary prevention strategies in males, divided by the major known contributors to CVD.
7.2 Major Components of Primary Prevention
7.2.1 Physical Activity
Sedentary persons have almost double the risk for CAD death as that of active persons. Even moderate physical activity provides a reduction in risk. Numerous studies have shown a strong graded response between levels of physical activities and decreased CV events. In addition, regular exercise is associated with improvement in the BP (mean reduction by 5 mmHg in those with hypertension), improves HDL, reduces triglyceride levels, and increases LDL particle size (without an effect on lowering LDL levels). Interestingly, these favorable effects are independent of weight loss associated with exercise and have a somewhat linear relationship with the intensity of exercise. Only 22 % of US adults engage in 30 min (or more) of exercise five times weekly. The American Heart Association recommends that adults perform at least 30 min of moderate intensity physical activity on most (and preferably all) days of the week. The rate of death decreased by 50 % by men 60 years and older whose status changed from unfit to fit over an 18-year follow-up period.
The mechanisms by which exercise exerts its beneficial effects are several and include improvement in CV risk factors (namely, hypertension, hyperlipidemia, and potential weight loss), as well as improve insulin sensitivity in diabetic patients. In fact, moderate intensity exercise has been associated with a reduced incidence of diabetes.
7.2.2 Tobacco
Despite the decline in the number of smokers in the Unites States in the past decade, nearly 20 % of adult Americans remain current smokers (with an increased rate of use in some populations including adolescents and young adults). There are more men than women who continue to smoke (21.5 % vs. 17.3 %), notwithstanding the recent rise in the rates of tobacco use among women [2].
Tobacco use is the single most important modifiable cardiovascular disease risk factor . In fact, cigarette use remains the leading cause of death in the USA, accounting for >400,000 deaths annually from CV and non-CV causes. There is a two- to threefold increase in the rates for coronary heart disease among those who consume >20 cigarettes daily. It is also important to remember that even passive exposure to tobacco or very low levels of consumption (<4 cigarettes daily) are also associated with increased rate of coronary artery disease. It has been clearly shown that continuation of smoking increases the risk for recurrent MI and need for repeat revascularization after the initial episode. Complete cessation is advocated and has been shown to reduce the risk of recurrent MI to levels equal to that of a nonsmoker within 3 years [3]. If complete cessation is not achievable, even a reduction of consumption by an increment of 5 cigarettes is associated with an 18 % decrease in mortality for each increment in patients who quit after MI [4].
Smoking leads to increased atherosclerosis and subsequent CVD. This occurs via several pathways which include acute unfavorable effects on blood pressure, myocardial oxygen supply, and sympathetic tone and longer-term vasomotor and endothelial dysfunction, increased inflammatory response, adverse lipid profile, platelet dysfunction, and a pro-coagulation state.
The importance of smoking cessation in any preventive clinic can hardly be overstated. The “5As” model for treating tobacco dependence has been shown to be effective and consists of the following components: ask, advise, assess, assist, and arrange. Patients should be asked about tobacco use at every encounter, and then every patient should be advised to quit (if current smoker) or provided with positive reinforcement (if past smoker). After identification, a physician should assess their readiness to quit. A commonly used model includes the following stages: pre-contemplation (no change intended), contemplation (intention to quit in the next 6 months), preparation (intend to quit within 1 month), action (discontinued smoking within the past 6 months), and maintenance (quit greater than 6 months prior). After assessment, the physician should assist the patient in quitting through counseling, providing resources (such as access to a support line), and pharmacotherapy. Although 70 % of all smokers state their intention to stop smoking, only ~4 % will be successful in doing so unaided, hence the importance of this step in successful smoking cessation. Counseling (as brief as 3 min or less during an office visit) has been shown to increase cessation rates by 30 %. The importance of community education regarding the dangers of smoking (severely lacking in developing countries and still important in developed countries) and physician-based primary prevention in the office remain paramount. Pharmacotherapy approaches are broadly divided into nicotine replacement therapies (via patch, gum, or nasal spray), and non-nicotine therapy (which includes sustained release bupropion, varenicline, clonidine, or nortriptyline) can also significantly increase abstinence rates. Interestingly, social influences can have a tremendous effect, with a ~2/3 increase in the chances of abstinence among smokers whose spouse also quits smoking and ~1/3 among those with a friend or coworker quitting smoking.
7.2.3 Hypertension
Hypertension is defined as a systolic blood pressure (BP ) of 140 mmHg or greater and/or a diastolic blood pressures of 90 mmHg or greater among those not taking antihypertensive medications. Patients with a systolic BP of 120–140 mmHg and/or diastolic BP of 80–90 mmHg are classified as prehypertensive. It is thought to be present in ~ 30 % of the US population and is increasingly prevalent with advanced age. Strikingly, a normotensive 55-year-old person might have a 90 % lifetime risk of developing hypertension as suggested by the Framingham Heart Study. In the National Health and Nutrition Examination Survey , only 68 % of participants were aware of their hypertension, and less than half of those aware of having hypertension had their BP adequately controlled. Although there remains a great deal of discussion regarding the relative importance of systolic vs. diastolic BP, ambulatory vs. office-based measurements, diurnal variations in blood pressures, etc., greater emphasis has been placed on systolic blood pressure as a predictor of cardiovascular risk.
Primary (also called essential or idiopathic ) hypertension accounts for 90 % of all cases of hypertension, while secondary hypertension (due to a variety of mostly treatable conditions) accounts for the rest. It is a complex disease with several environmental and genetic determinants. There is long-established graded relationship between blood pressure and cardiovascular risk, which holds even for those in the prehypertensive range . Beginning at 115/75 mmHg, each increase in 20/10 mmHg doubles the risk of cardiovascular disease. Importantly, the gradual rise of blood pressure over most patients’ lifetime is not benign, and treatment of hypertension even in the elderly population has been shown to be beneficial.
Sodium reduction (e.g., DASH diet), weight loss, and exercise and discontinuation of tobacco and alcohol use are non-pharmacological approaches to reduce BP that could be successful in compliant patients. Nonetheless, the long-term effects of solely non-pharmacological approaches have generally been disappointing. The initiation of relatively simple mono or combination pharmacotherapies has been shown to be effective in treating hypertension and has a significant reduction in cardiovascular complications. The selection of the specific class of antihypertensive should be based on demographic factors and presence of concomitant comorbidities. For example, alpha-blockers should be considered for patients with benign prostatic hypertrophy, while ACE-inhibitors should be considered for those with diabetic nephropathy.
7.2.4 Hyperlipidemia
There is an estimate of more than 33 million Americans with elevated cholesterol levels [5]. Observational studies have repeatedly showed a strong graded relation between total cholesterol and LDL levels with cardiovascular events.
All patients with elevated total cholesterol or LDL should receive counseling on appropriate lifestyle modifications which include aerobic exercise, weight loss (for overweight patients), and a healthy diet.
Statins (HMG-CoA reductase inhibitors ) represent the mainstay of pharmacologic therapy for patients with hyperlipidemia. Other lipid-lowering therapies (fibrates, niacin) have not shown convincing reductions in CV events despite their effect on improving lipid profiles. Newer therapies (such as PCSK-9 inhibitors) have shown great promise in early trials, but much more additional data is needed prior to widespread clinical use. Patients with known cardiovascular disease, CAD risk equivalents, or combination of multiple CV risk factors clearly benefit from initiation of statin therapy. For the remaining of the patients, the decision to initiate statin therapy depends on their baseline risk for CVD events and the potential for absolute risk reduction with addition of statin therapies. Several risk calculators are available and include the Framingham risk score, the recently issued AHA/ACC CV risk calculator in order to guide the clinician in appropriate risk stratification.
Recent guidelines have focused on identifying populations who would benefit from initiation of moderate vs. high-potency statins and have downplayed the importance of achieving specific LDL targets (except when checking for compliance with statin use). Examples of low-to-moderate statin doses include pravastatin 40 mg, lovastatin 20–40 mg, simvastatin 40 mg, and atorvastatin 10–20 mg, while high intensity statin doses include atorvastatin 40–80 mg and rosuvastatin 10–20 mg. Dose of statin should not be intensified for any LDL target . Statin intolerance (most commonly due to myalgia) is unfortunately not uncommon. While this could be resolved in some instances (by dose modification or switching statins), statins might have to be discontinued all together if the benefit of primary prevention does not outweigh the adverse effects. Patients should also undergo monitoring for the serious side effects of transaminitis (periodic monitoring of LFTs is recommended, frequency remains debated) and myopathy (clinicians should check CK for symptomatic patients only).
7.2.5 Diabetes and Metabolic Syndrome
Diabetes mellitus is the seventh leading cause of death in the USA. The prevalence of type 2 diabetes (which accounts for 90 % of cases) has unfortunately been on the rise, following the increase in rates of obesity in the USA and worldwide. The number of diabetics worldwide has increased from 35 million in 1985 to 171 million in 2000. Two million people are newly diagnosed with diabetes each year in the USA alone. The prevalence of diabetes is higher in men compared to women.
Simply stated, diabetes is a metabolic disorder characterized by inadequate insulin secretion necessary to maintain normal plasma glucose levels. Type II diabetes is characterized by increased insulin resistance, requiring ever-increasing levels of insulin production in order to maintain glycemic control. The definition of diabetes (according to the American Diabetes Association in 2011) is a fasting plasma glucose ≥126 mg/dl, a random plasma glucose ≥200 mg/dl (with hyperglycemic symptoms), 2-h plasma glucose ≥200 mg/dl, or a hemoglobin A1C ≥6.5 %.
It is important to note that CAD accounts for 75 % of deaths among diabetics, while CAD accounts for 30 % in nondiabetics. The 10-year risk of coronary heart disease (MI or death) is almost equal to those with a prior history of MI; therefore, DM is recognized as a CHD risk equivalent. Diabetic complications are generally divided into 2 categories: microvascular and macrovascular complications. Notably, hyperglycemia has a linear causal relationship with microvascular complications (such as retinopathy and nephropathy). Tight glucose control has been convincingly shown to lower diabetic retinopathy and nephropathy trials in two large trials: the Diabetes Control and Complications Trial and the UK Prospective Diabetes Study , both completed in the 1990s. On the other hand, insulin resistance promotes atherosclerosis even before frank diabetes occurs. In fact, patients with prediabetes have threefold increase in rate of myocardial infarctions, almost as high patients diagnosed with diabetes. There has been a relative paucity of data supporting intensive glucose control strategies for prevention of macrovascular complications (such as MI) when compared to prevention of microvascular complications. The current recommended target in a hemoglobin A1C is ≤7 % and unfortunately has been shown to reach in only 31 % of participants in the NHANES registry .
Diabetes is a preventable disease and can be prevented or delayed by specific interventions such as 5–10 % weight loss, moderate exercise, avoiding tobacco use, and pharmacotherapy when indicated (metformin).
The term “metabolic syndrome ” has slightly differing definitions according to different organizations. The joint AHA/IDF criteria for the diagnosis of metabolic syndrome consist of the following: (1) waist circumference in excess of population-/country-specific dimensions, (2) triglycerides ≥ 150 mg/dl (or drug treatment for hypertriglyceridemia), (3) HDL < 40 mg/dL in males (or drug treatment for low HDL), (4) systolic BP ≥ 130 mmHg and/or diastolic BP ≥ 85 mmHg (or drug treatment for hypertension), and (5) fasting glucose ≥ 100 mg/dL (or drug treatment for hyperglycemia). There has been some recent controversy on whether the sum of parts (metabolic syndrome) offers any additional risk prediction when compared to the sum of its parts (individual criteria). Controversies notwithstanding the identification of metabolic syndrome should focus the attention of the clinician on patients who are at a clearly higher risk of cardiovascular events.
7.2.6 Diet
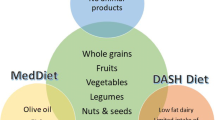
The importance of a healthy eating pattern was emphasized in the 2006 American Heart Association Diet and Lifestyle recommendations for CVD risk reduction. General recommendations consist of (1) balanced calorie intake with physical activity to achieve a healthy weight; (2) consumption of fruits and vegetables; (3) choosing high-fiber, whole grain options; (4) at least twice weekly consumption of fish; (5) minimization of intake of beverages and foods with added sugars; (6) choosing/preparing foods with little or no added salt; and (7) moderate alcohol use if consumed. Specific recommendations include limiting intake of saturated fat to <7 %, trans fat to <1 %, total fat to 25–35 % of total energy intake daily, and cholesterol to <300 mg daily. Some specific dietary patterns, such as the Mediterranean diet, have been the subject of large observational studies and have been associated with beneficial long-term effects on known CV risk factors . Although randomized trials have generally been disappointing, a Mediterranean diet might be associated with decreased cardiovascular events compared to a control group (who only received advice on low fat diet), with an observed absolute reduction in risk of ~ 3 CV deaths per 1000 person/year [6].
The issue of alcohol use has received significant attention recently. Moderate consumption of alcohol is defined as 2 drinks or less per day for men (1 or less for women). Men who have a moderate intake do not need to be counseled to discontinue, while those who do not consume alcohol do not need to start.
7.2.7 Obesity
Rate of obesity remains on the rise, and recent statistics show that a majority of Americans (66 %) are overweight (defined as BMI > 25 kg/m2), while 32 % are obese (defined as BMI > 30 kg/m2). The percentage of obese Americans has more than doubled in the past decade alone. This is a critical issue, especially in light of the steep rise in rates of obesity among adolescents. Numerous studies have shown that obesity has a linear relationship with the CV risk factors of hypertension, hyperlipidemia, and diabetes. Even after adjusting for known CV risk factors, higher BMI is clearly associated with cardiovascular mortality. Interestingly, obesity is associated with increased vascular events regardless of levels of physical activity. The waist-to-hip ratio, which is a marker of abdominal adiposity, has been shown to be an accurate predictor of coronary artery disease. Moreover, central obesity is a component of the diagnosis of metabolic syndrome, discussed separately in this chapter.
The main approach of therapy remains achieving a desirable balance between calorie restriction and exercise, along with general lifestyle improvement. Every patient presenting at a preventive clinic should receive advice and encouragement for lifestyle changes of proven benefit. Medications could be used for temporary management, but the effects of long-term use are uncertain. Surgical therapy is available in extreme cases and is associated with generally positive outcomes.
7.3 Conclusions
Primary prevention focusing on modification of known risk factors saves lives and is essential in our daily practice. These modifiable risk factors include cigarette smoking, sedentary lifestyle, dyslipidemia, hypertension, diabetes, metabolic syndrome, abdominal obesity, lack of regular exercise, and poor diet. Preventive interventions include both therapeutic lifestyle changes and adjunctive drug therapies when indicated, with additive beneficial effects achieved with the targeting of all relevant risk factors.
References
Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors--United States, 2005-2013. MMWR Surveill Summ. 2014;63 Suppl 4:3–27.
Gfroerer J, Dube SR, King BA, Garrett BE, Babb S, McAfee T. Vital signs: current cigarette smoking among adults aged ≥ 18 years with mental illness – United States, 2009-2011. MMWR Morb Mortal Wkly Rep. 2013;62:81–7.
Rea TD, Heckbert SR, Kaplan RC, Smith NL, Lemaitre RN, Psaty BM. Smoking status and risk for recurrent coronary events after myocardial infarction. Ann Intern Med. 2002;137:494–500.
Gerber Y, Rosen LJ, Goldbourt U, Benyamini Y, Drory Y, Myoca ISGFA. Smoking status and long-term survival after first acute myocardial infarction a population-based cohort study. J Am Coll Cardiol. 2009;54:2382–7.
Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–209.
Estruch R, Ros E, Salas-Salvado J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–90.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Lahoud, R., Franco, I. (2016). Cardiovascular Prevention in Men. In: Potts, J. (eds) Men's Health. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3237-5_7
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3237-5_7
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3236-8
Online ISBN: 978-1-4939-3237-5
eBook Packages: MedicineMedicine (R0)