Abstract
When prosthetic information is supplied to the auditory nerve or auditory brainstem the pattern of nerve activity to the brain is highly unnatural compared to the normal acoustic pattern of activation. How does the brain respond to and incorporate this unnatural pattern of activity? The answer depends on the place of stimulation (cochlea, brainstem, midbrain, cortex), the residual health of the stimulated neurons (intact or damaged), the age of the individual when they receive the stimulation (young or older), and their prior experience with sound before their hearing loss (congenital vs. acquired loss). This chapter discusses the history of perception when sensory function is restored, in both hearing and vision. Early philosophers thought that perceptual pattern perception was “pre-ordained” and so once sensory input was restored the person should have immediate function. In the 1700s European philosophers argued that perception was determined by experience so that once sensory function was restored people would have to learn to hear or see from the beginning. We now know that this is correct from the experience with hearing and vision restoration. In this chapter we discuss the implications of cochlear implants (CIs) and auditory brainstem implants (ABIs) for our understanding of the interaction between sensory systems and the brain. CIs provide a degraded but tonotopically organized representation of sound information to the brain, while ABIs provide a degraded and tonotopically scrambled pattern of information to the brain. We discuss CI and ABI outcomes in adults and children, in both congenitally or postlingually deafened adults and children. The contrasts and similarities in outcomes across these different patient populations and devices provide an opportunity to refine our understanding of the relative roles of sensory periphery and the brain in sensory function.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Auditory brainstem implant
- ABI
- Critical period
- Speech production
- Speech recognition
- Cognitive development
Introduction
In the early 1700s philosophers were debating whether the senses were innate or learned. William Molyneux, an Irish philosopher, posed a question that has become known as “Molyneux’s problem .” Essentially, this thought experiment asked whether a person, born blind, but familiar with object shape from touch, could identify an object by sight alone if they had their vision restored. Molyneux and his friend, English philosopher John Locke, both argued that the blind person would not be able to tell a ball from a cube using sight alone. They both believed that the brain did not have an intrinsic template for sensory information—that it had to be learned. They further assumed that even if this shape information was learned from touch it would not transfer to vision without visual experience. Since that time, there have been cases where people, congenitally blind from cataracts, regain sight from surgery to remove or replace the lens of the eye. In most cases they could technically see, but could not recognize objects because their brains had not been trained on visual input. Even after many months of experience most such people functioned as if they were still blind (Gregory and Wallace 1963). More recent data shows some limited ability to learn basic visual pattern recognition skills in adulthood after congenital blindness (Kalia et al. 2014).
It appears that at least two factors influence the development of the brain’s ability to process sensory information: receiving information during the critical period of brain development in childhood, and the quality of the sensory information. The brain is a complex and dynamic organ—some aspects of brain development are highly choreographed by biological stages of plasticity. We now know that complex sensory development must occur quite early—before about 5 years of age, or the window of plasticity closes (e.g., Ruben and Rapin 1980). If no sensory experience is obtained prior to age 5, then later restoration of that sense is difficult if not impossible. Other aspects of brain plasticity remain after age 5, but the level of organization needed to process a complete new sensory modality appears to be not available after 5 years of age.
In our lab at the House Ear Institute (Shannon 2015) we had direct experience with a man in his early 40s who had been profoundly deaf since birth from Usher’s syndrome. He was working as an electrical engineer but was losing his sight from retinitis pigmentosa. Although he had never heard sound he was confident that he could learn to recognize sounds because of his training as an engineer—he knew mathematically what a sine wave was and what an auditory filter was. He understood the physics of speech sounds and their spectrograms. He felt that with this knowledge he could learn to differentiate and recognize sounds from a cochlear implant. Following cochlear implantation, CI researcher Qian-Jie Fu developed a computerized training program for him to practice simple auditory distinctions: loud vs. soft, high vs. low pitch, one sound vs. two sounds, etc. (This software is available for free at http://www.emilyshannonfufoundation.org/esff_software.html.) Another training program simply presented spoken words that identified everyday objects: ear, nose, eye, fingers, etc. He worked diligently at this task but never made much progress. The sound from the implant always evoked an emotional feeling that included some degree of sadness, probably because his unused auditory cortex had been repurposed to accommodate emotional information. Electric stimulation of the auditory system was now triggering emotions instead of, or in addition to, sound sensations. Although he knew the sounds mathematically he was not able to learn even simple patterns acoustically. After 2 years of dedicated work and practice he gave up. This outcome is consistent with the Molyneux’s conjecture and with the prior experience with congenital blindness.
What is the relationship between brain development and sensory information? What are the critical periods for sensory brain development? How much sensory information is necessary for brain development? The answers to these questions are now better understood thanks to restoration of hearing with cochlear implants (CIs) and auditory brainstem implants (ABIs) in children. This chapter briefly reviews the findings on CIs and ABIs and discusses the results in the context of neuroscience and brain development.
Cochlear Implants
In Molyneux’s time it was rare for a person born with a sensory deficit—blindness or deafness—to recover the sense, so there was no way to resolve his conjecture. However, the thought experiments of these early philosophers can now be tested in scientific detail with the advent of cochlear implants and auditory brainstem implants for the congenitally deaf. Early in the application of CIs it was apparent that providing CIs to congenitally deaf adults was of little value. Just like cataract surgeries in the congenitally blind, these CIs resulted in only rudimentary auditory capability for adults, even after many years of experience.
However modern cochlear implants can restore good functional hearing to children born deaf. The results are now completely clear, as this volume attests, that cochlear implants provide sufficient auditory information for children to develop functional hearing. Most children can identify sounds, recognize speech, and produce speech well enough to interact in a mostly normal fashion with the hearing world. However, we also know that congenitally deaf children don’t typically achieve these results if implanted after the age of 8. The plasticity of the brain in adapting to new sensory information appears to diminish after the age of 5 years (Niparko et al. 2010). Although cochlear implant outcomes are best when the child is younger, some neural plasticity remains so that older children can still benefit from a CI, but on average their outcome is not expected to be as good as children implanted early. Some evidence suggests that if a brain region is not used by its natural sense, it becomes “colonized” by some other function (Lee et al. 2001; Shepherd et al. 1997). Once hearing is restored by a cochlear implant it is difficult to dislodge the “interloper” after age 5 years. Of course, children who have even limited early auditory experience can use the CI information more effectively because their brains have received some input from the auditory system and their brain will have developed some abilities to interpret auditory information.
Lee et al. (2001; Giraud and Lee 2007) showed PET images of congenitally deaf children implanted with CIs at different ages. The area of auditory cortex that responded to the CI diminished as the duration of deafness increased. It appeared that the auditory cortex in these children now responded to sign language or other things and not as strongly to acoustic sound. The auditory performance of these children was proportional to the area of the cortex that responded to acoustic sound. Children who had a long period of deafness showed poor speech recognition with the cochlear implant and strong responses in auditory cortex to sign language. Children with a short period of deafness showed a larger area of the cortex that responded to sound and had excellent speech recognition with the CI.
Children implanted at early ages have shown dramatic hearing abilities with cochlear implants (Govaerts et al. 2002; Rubinstein 2002; Manrique et al. 2004; Robbins et al. 2004; Svirsky et al. 2000, 2004; Dettman et al. 2007; Niparko et al. 2010, Colletti et al. 2014). Measures of speech recognition have shown an almost normal trajectory of speech recognition development as long as the CI was provided prior to 3 years of age. Recent research has shown improved performance with even earlier implantation, so that cochlear implantation prior to 12 months of age is now the norm. There is now evidence that implantation prior to 12 months of age provides improved long-term auditory performance compared to those implanted after 12 months (Colletti et al. 2011; Waltzman and Roland 2005).
The brain develops remarkable pattern recognition abilities, and this development begins even prior to birth. In a normally hearing child, hearing begins at least 1 month prior to normal term birth. At birth newborns can already distinguish their mother’s heartbeat and voice from others (Smith et al. 2007; Kisilevsky et al. 2003, Kisilevsky and Hains 2011) and can recognize music that was played in utero (Lecanuet et al. 2000). This shows that the brain’s auditory pattern recognition is already in action prior to birth. And so children with congenital deafness have a disadvantage already at birth because their brain’s processing of auditory sensation was not “jump-started” in utero.
Even if prosthetic stimulation is available during the time of critical brain plasticity, the quality of the sensory information will have a large effect on the ability of the brain to use it. If the quality of sensory information is poor, then even the developing adaptive brain may not have sufficient information to work with. The pattern of neural activity provided by normal acoustic stimulation and the pattern produced by electric stimulation are highly different, with the acoustic pattern being much richer in cues than the electric. Psychophysical studies in persons with CIs have shown almost normal perceptual abilities in timing, e.g., gap detection, forward masking, and modulation detection (e.g., Shannon 1990). But CI listeners have reduced abilities in the perception of intensity (Zeng and Shannon 1994) and frequency resolution (Nelson et al. 2008). But not all of those cues are equally important for speech—some cues can be dropped with little consequence for speech perception while other cues are essential. So which aspects of the pattern of sensory information are more important for sensory development and which are less important? Fu and Shannon (1998) showed that distortions in amplitude mapping only have a small effect on speech recognition, while Shannon et al. (2004) showed that the number of spectral channels necessary for recognition depends on the difficulty of the listening situation. We know that the information provided by a cochlear implant is sufficient for understanding speech. Congenitally deaf children implanted with a CI are mostly able to understand speech and develop spoken language. In spite of the many differences between the patterns of acoustic and electric activity, the brain is able to make optimal use of the information. Congenitally deaf children with CIs reach the same level of performance as adults with CIs who had prior normal-hearing experience. Even though the implant activation has highly abnormal timing and a smeared representation of tonotopic place, the brain is able to extract the information fully from the signal. This observation suggests that the limiting factor in modern cochlear implants is in the signal processing. The same high level of performance is achieved by both adults who have heard prior to deafness and by children who are learning to hear with only the signal provided by the CI. It is now clear that the most serious limitation of CI signal processing is the limited number of spectral channels. Even though modern CIs contain up to 20 electrodes, the electrical field interactions and neural interactions limit the effective number of spectral channels to 8–10 (Friesen et al. 2001). If we can improve the tonotopic specificity we should be able to improve the speech recognition abilities of patients with CIs.
Auditory Brainstem Implants
The auditory brainstem implant was developed for patients without an intact auditory nerve, making them unable to benefit from a CI. The ABI is similar to a CI except that the electrode is placed on the cochlear nucleus in the brainstem instead of in the cochlea. The cochlear nucleus is the first auditory relay station beyond the cochlea in the pathway of auditory information to the brain. An ABI provides a case of more extreme distortion of the sensory pattern of information than a CI. The ABI electrodes rest on the surface of the cochlear nucleus, a complex structure with three main divisions (anteroventral: AVCN, posteroventral: PVCN, and dorsal: DCN). Each of these divisions has unique cell types and physiological response properties. Each division has at least one tonotopic axis. The ABI electrode is 8 mm in length, so that it likely stimulates both PVCN and DCN. However, the tonotopic axes in these divisions are not well represented on the surface. So the surface electrode ABI probably stimulates a mix of cell types, mostly low-pitch tonotopic regions, and at least two major functional divisions. Previous experience with adults shows that the pitch map of electrodes is complex and non-monotonic (Otto et al. 2002). We know little about the temporal pattern of neural activity evoked by ABI firing. Based on what is known from stimulation of the auditory nerve by a CI we can assume that the ABI produces extreme, nonnatural phase locking to electric pulses.
Even though it was known that CIs could provide sufficient information for speech recognition in adults and children, little attention was paid to auditory brainstem implants because ABI results in adults were poor compared to CIs (Otto et al. 2002). However, Colletti et al. (2004) showed excellent open-set speech recognition in adults with ABIs. In the USA, most recipients of an ABI were individuals with neurofibromatosis type 2 (NF2). In contrast, ABI recipients implanted by Colletti in Italy lost their auditory nerve from trauma or severe ossification (Colletti et al. 2004). The fact that the ABI could support open-set speech recognition in non-NF2 patients showed that the poor ABI results in NF2 patients were not due to the device or to electrode placement; rather, it suggested that the poor performance was related to the damage to the auditory pathway as a result of NF2.
In a CI the electrodes typically change systematically in pitch sensation from one end of the array to the other. The pitch representation may be shifted relative to normal if the electrode is placed too shallowly in the cochlea, but CI patients usually adjust in a few months to this shifted pitch representation. In contrast, the ABI electrode is placed on the surface of the cochlear nucleus in the brainstem. The ABI electrodes do not produce a monotonic change in pitch because the cochlear nucleus has multiple tonotopic maps and these are not accessible from the surface of the nucleus (Moore and Osen 1979; Moore et al. 1994). In the first few months of ABI use, adults find the sound quality strange and unhelpful. They typically require 3–6 months of experience to make sense of the sounds. Among adult ABI users who were deafened due to NF2, only a few out of hundreds were able to obtain open-set speech understanding (Otto et al. 2002). Among adult ABI user who did not have NF2, about 30 % were able to understand speech with an ABI well enough to have a conversation on the telephone (Colletti and Shannon 2005; Behr et al. 2007; Matthies et al. 2013, 2014). A few in this latter group achieved speech recognition levels comparable to the best CI outcomes: 100 % recognition of simple sentences presented in quiet, and 50 % recognition of speech presented in noise at signal-to-noise ratios of 3–4 dB. These high-performing ABI-implanted adults were able to successfully map this scrambled tonotopic information onto the speech pattern recognition that already existed in their brain. Such cases are interesting for neuroscience, because it shows that an adult brain, trained in speech pattern recognition with acoustic sound, can map that pattern recognition onto a new pattern generated through electrical stimulation that has little in common with the original pattern—different temporal properties (phase locking, etc.) and tonotopic organization that is highly scrambled compared to the acoustic representation. In this case the brain can “morph” the new pattern into the previously established speech recognition system in the brain.
Recent outcomes show that even some people with NF2 can achieve speech recognition with an ABI. Two surgeons (Behr et al. 2007; Matthies et al. 2013, 2014) have shown that about 30 % of their NF2 ABI patients were able to understand speech well enough to converse on the telephone. These surgeons use a different surgical approach that may cause less neural and vascular damage to the cochlear nucleus region. The fact that they are able to show improved speech recognition suggests that even subtle damage to the cochlear nucleus can have large effects on ABI performance.
ABI in Children
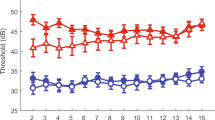
Colletti et al. (2014) also implanted the ABI in children with no auditory nerve. This was controversial because at that time most outcomes with the ABI were poor compared with CIs. Many people thought that it was not ethical to incur the risks of ABI surgery for a limited outcome, especially in children. However, Colletti had seen excellent CI-like outcomes in non-NF2 adults (Colletti and Shannon 2005) and so implanted the ABI in non-NF2 children. Colletti et al. (2010) demonstrated that the complication rate of ABI surgery in children implanted at his medical center was similar to that seen in a CI, so the surgical risk did not appear to be unreasonable. He selected children with congenital anomalies who had no auditory nerve based upon magnetic resonance imaging (MRI) or those who had failed to show any progress with a cochlear implant. Some of these children had severe ossification following meningitis and some had temporal bone fractures that severed the auditory nerve. After a few months, he started to see CI-like outcomes in some of the children. Figure 15.1 shows the outcomes over 7 years from 64 children implanted in Verona with ABIs (data from Table 1 of Colletti et al. 2014). The results show median scores over time on the CAP, a categorical evaluation of auditory performance (Archbold et al. 1995). On the CAP a category of 0 indicates no detection of sound, 4 represents identification of words from a closed set of alternatives, and 7 indicates the ability to converse on the telephone with a familiar person. Results in Fig. 15.1 are divided into groups that differ in the age at the time of ABI surgery and the numbers in the figure show the number of children at each time point. Note that the group that received the ABI before 4 years of age (N = 39) had better performance, with the median score reaching high closed-set (CAP level 4) performance. These are children with diverse etiologies, but all had no auditory nerve visible by MRI, mostly from genetic problems and a few from disease or trauma. Lower median CAP scores were observed in the children who received the ABI after age 4 (N = 25). These children showed an increase in CAP level but the median level only reached a level of 2, which represents only being able to make simple discriminations between sounds. Overall, of the 64 children, 11 (17 %) reached CAP level 7, which means that they are able to converse on the telephone with a family member, and 20 children (31 %) were able to achieve open-set speech understanding (CAP scores of 5–7). Twenty-two of the 64 children had previously received a CI and showed no response. These results show that the scrambled spatiotemporal pattern of activity from the ABI is sufficient for the brain to learn to hear even with no prior experience. This result shows the potential for the ABI to restore a significant amount of hearing function to children who cannot benefit from a CI. Good speech recognition is now being obtained in other centers with ABIs in children (Sennaroglu et al. 2009, 2011; Eisenberg et al. 2008, 2012). The implication of this observation for neuroscience is addressed in the next section.
Auditory performance as measured by the CAP test as a function of time after ABI surgery. The two groups or results show scores over time for children implanted before or after 4 years of age. Note that the number of children represented by each data point decreases over time: the numbers in the legend show the N for each successive point for the two groups
The Role of Ear and Brain
Now let us return to Molyneux’s problem. If a person does not receive any sensory input from birth and then that sensory input is restored as an adult, the person will not be able to use it very well, if at all. There are two issues to consider: At what age is the sensory information provided, and what is the quality of the restored sensory information? Cases of visual cataracts and cases of cochlear implants both show that sensory information provided as an adult to a person with congenital absence of that input is not effective. We assume that this is due to the plasticity of the brain not being as fully available in adulthood as in infancy. Learning complex pattern recognition from sensory input apparently requires a high level of brain plasticity, which is not available to adults. Outcomes from CIs and ABIs in children show better outcomes the earlier the device is implanted. This result suggests that the necessary neural plasticity is most available right after birth.
A newborn brain must learn about the universe from its sensory experience. Studies have shown how babies learn to distinguish subtle differences in sensory patterns by computing the probabilities from their sensory experience (Saffran 2002, 2003; Saffran et al. 1996; Jusczyk and Aslin 1995). Babies can be presented with sequences of nonsense sounds of only 2 min in duration and they will remember phonetic aspects of the sequences even 1 week later. When the babies’ response to sounds has a desired effect on the mother’s behavior, the distinction is quickly learned. But even in the case of normal hearing it takes many years to learn the complex patterns of speech. Hart and Risley (1995) estimated that children are exposed to more than 30 million words of direct interaction with their mother before the age of 5 years. This observation has given rise to the 30 Million Word project in Chicago to train parents on the importance of early word and language exposure in their children (Leffel and Suskind 2013). The learning of sensory probabilities is also well studied in vision, showing that people learn the detailed probabilities of the visual world over many millions of experiences (D’Antona et al. 2013). This kind of intensive experience has been popularized as the “10,000-h” rule, suggesting that mastery of any complex task takes 10,000 h of dedicated practice. Early development of sensory systems may require millions of repetitions to achieve mastery of complex pattern recognition.
So even if the sensory information is intact it can take thousands of hours and millions of repetitions to gain “fluency.” What happens when the sensory information is degraded and distorted, as in the case of CI and ABI auditory input? If the sensory experience is dramatically reduced in quality, then the level of sensory development will be limited by this poor signal. Is it possible to learn patterns of sensory information that are dramatically different from the normal pattern? The pattern of CI stimulation is different from the pattern of acoustic stimulation—the activation by CI electrodes is compressed and probably shifted along the cochlea compared to the normal acoustic pattern. In the ABI neural activation patterns are much more scrambled in tonotopic order than with a CI. Will children still be able to learn the probabilities, the regularities in the sensory patterns when they are so distorted?
First let us consider cochlear implants. The CI activates neurons with electric currents. Research has shown that there are large differences in the spatial and temporal patterns of neural responses to electric stimulation compared to acoustic stimulation. How well will the brain be able to use such a neural pattern for hearing? Early single-channel CI devices presented an analog version of the speech wave form directly to a single intracochlear electrode—almost like just removing the wire from your stereo speaker and connecting it to a wire in the cochlea. Such stimulation did not use multiple electrodes to access the normal tonotopic distribution of information in the cochlea. However, even with this signal some children were able to achieve limited open-set speech understanding—a level of performance that was unexpected and still not fully understood (Berliner et al. 1989).
In multichannel CIs the signal is split into different frequency bands and each band is presented to a different electrode, to take advantage of the normal tonotopic distribution of information in the cochlea. But even if we present many “channels” or electrodes of electric stimulation we know that not all of those channels are used effectively. Studies have shown that CI patients only receive 8–10 channels of effective information even if we present 16–22 channels of input (Friesen et al. 2001). The loss of information occurs because of interference between electrodes, either electrically or at the neural level. In a CI the information is also presented to a limited region of the cochlea, and is probably shifted in tonotopic space from the normal acoustic locations due to insertion in the basal cochlear region. Congenitally deaf children never learned the “normal” tonotopic map, so their developing brains simply take the pattern of implant stimulation as the “new normal.” Speech recognition results show that most children with a CI can rapidly adapt to the degraded and distorted pattern of sensory information and achieve a high level of speech recognition and production. They are mostly able to reach the same level of speech recognition as adult CI users who have had normal acoustic hearing prior to deafness. This suggests that the brain is able to use the full information in this implant signal, in spite of the distortion compared to the normal acoustic pattern.
But not all children achieve this level of speech recognition. About 10 % of children implanted with a CI show minimal auditory capabilities even over a long period of time (Niparko et al. 2010). These children may have deficiencies in their residual auditory nerve or central processing limitations that limit their performance (Govaerts et al. 2003; Casselman et al. 2008; Carner et al. 2009; Buchman et al. 2011; Young et al. 2012). In these cases speech recognition is not limited by the signal processing of the device but by the status of their auditory nerve. Some of these children may be candidates for an ABI. Colletti’s results (Colletti et al. 2014) indicate that ABI outcomes are poorer in children with multiple disabilities compared to children without additional disabilities. Clinical trials are now under way in several centers to refine the selection criterion for children to receive an ABI.
In spite of the ABI distortions in time and spatial activation patterns, some children are achieving high levels of open-set speech recognition with the ABI (Colletti et al. 2014; Sennaroglu et al. 2009, 2011). This result demonstrates the flexibility of the developing brain when presented with degraded and tonotopically scrambled auditory information. The fact that some children can achieve high-level CI-like performance shows that even in the ABI case the brain is capable of getting the maximum information out of the implant signal. One unsolved problem with ABIs is why the rate of children obtaining good speech recognition is lower than for CIs. It is possible that the genetic problems that cause the loss of their VIII nerve also affect development of the cochlear nucleus and other central auditory nuclei. It is also possible that some children have more complex central problems in development that limit their ability to use the information provided by an ABI.
Cognitive Development
One understudied aspect of auditory implants is the effect of prosthetic sensory experience on cognitive development. Work with deaf children and with CIs has shown reductions in executive function, including visual working memory (Pisoni 2000; Pisoni and Cleary 2004; Khan et al. 2005; Edwards et al. 2006; Shin et al. 2007; Le Maner-Idrissi et al. 2008; Fagan and Pisoni 2009; Kronenberger et al. 2014). At first glance this is a puzzling finding. Why would a sensory deficit in hearing affect visual memory? One possible answer comes from the consideration of how memory depends on the senses. It has long been known that people with synesthesia have exceptional memories (Rothen et al. 2012). Synesthesia is a rare phenomenon where activation of one sense, e.g., vision, is accompanied by linked sensations in another sense, like hearing or taste. For example, some persons with synesthesia always see a specific color associated with a number, or sense a specific color to be associated with a particular pitch; all eights may also be perceived as blue, or middle C is always accompanied by the sensation of green. It is thought that the extra sensory experience provides the brain with an extra dimension of information about objects and events. This extra dimension of sensory experience provides more cues for the storage and retrieval of memories. It is possible that the deficit in memory (and other cognitive deficits) in deaf children is due to the loss of dimensionality of sensory experience (Fagan and Pisoni 2009). If only two sensory dimensions (e.g., vision and smell) provide cues to a memory event, the memory may be weaker than if three sensory dimensions (e.g., add hearing) contribute to the memory. The early development of executive function may also be delayed by the reduced dimensionality of sensory experience. So having one less sensory dimension (deafness) may degrade memory and cognitive development.
If CIs and ABIs restore the auditory dimension do they also restore deficits in memory and executive function? Is the restoration of memory proportional to the restoration of sensory function? We do not yet have answers to these questions, but research is under way to quantify such possible effects. One study (Colletti and Zoccante 2008) in nine children with an ABI showed that even the sensory information provided by an ABI provided significant improvements in selective visual-spatial attention and fluid reasoning (i.e., reasoning or the ability to solve problems in novel situations). It appears that adding another dimension of sensory experience, even a limited dimension, can provide sufficient additional information to improve cognitive development.
Issues for the Future
There is still much research to be done to fully understand the role of prosthetic hearing on speech, language, and cognitive development. It is clear that it is of critical importance to provide the best sensory information at as early an age as possible. Brain development is moving fast in the years 0–3 and every month lost is a lost opportunity. If a child with an implant is not making progress we need to determine if this is due to a poor adjustment of the processor, a partial failure of the device, or a problem with their neurons due to the etiology of hearing loss. Once this is determined we can improve the adjustment, replace the device, or, in the case of the CI implanted child, contemplate moving to the ABI. But whatever solution is correct, the brain plasticity clock is ticking. Figure 15.2 presents a schematic of the normal fitting cycle for a CI or ABI in a child. Initially the child cannot provide feedback on the qualities of the hearing sensation because they have no experience with sound. The initial maps are often fit based on the levels of evoked auditory brainstem electrophysiological responses (ABR) and avoiding any non-auditory side effects (NASE), especially for the ABI. Trained pediatric audiologists can manage the child’s attentional state and observe behavioral responses. Once an initial map setting is achieved, the child must adapt to it. This adaptation may take several weeks or even months before any assessment can be made of the efficacy of the fitting. This is an area where better methods and tools are needed. The sooner we can determine if a device setting is inadequate the sooner we can adjust the map in an attempt to fix the inadequacy. This cycle can’t occur too quickly because it takes some time for the child to adapt to the changes before we can reasonably assess their use of acoustic cues. However, this fitting cycle should occur early in the process so that the final map can take advantage of the plasticity of the brain.
Schematic representation of the fitting cycle for an ABI. Initial test measures indicate the ability of the child to detect and discriminate sounds with the new map, but additional tests are made after a period of adjustment where the child learns to use the new information provided. The cycle must be short to achieve an optimal mapping as soon as possible to take advantage of brain plasticity, but long enough to allow the child to accommodate to the new information
New brain imaging methods may hold promise in this process. Cortical potentials and optical imaging may be able to show new patterns of cortical activity before any behavioral manifestations (Friesen et al. 2009; Aslin 2012, Martinez et al. 2013). We assume that a strong physiological response at the auditory cortex is a sign that the information from the implant is activating the brain in the desired fashion. Even if the individual child has not yet learned how to use this information, normal developmental plasticity gives us some confidence that the information will be used if it is present. Behavioral techniques, such as the rate of babbling development, may offer a metric for assessing early auditory progress (Oller and Eilers 1988; Kishon-Rabin et al. 2005; Schauwers et al. 2008; Ertmer and Goffman 2011). At the present time these tools are not fully developed to allow this kind of assessment, but there is hope that, individually and in combination, they will be useful in the near future.
Conclusion
New outcomes with ABIs in children show the power of brain plasticity. A complex, novel, and distorted pattern of neural activity presented by the prosthesis to the brainstem is capable of providing high levels of open-set speech recognition in some pediatric recipients. This observation is not only greatly satisfying to clinicians, but also important for neuroscience. Children without an auditory nerve cannot receive hearing from a CI. But some of these children can receive CI-like hearing from an ABI. Questions remain about the best etiology for the ABI and why some children show only sound awareness and simple discrimination with the ABI. More research is necessary to further develop the ABI device, fitting, and evaluation. But the results now show that an ABI can provide useful hearing to children who cannot benefit from a CI.
References
Archbold SM, Lutman E, Marshall D. Categories of auditory performance. Ann Otol Rhinol Laryngol. 1995;104 Suppl 166:312–4.
Aslin RN. Questioning the questions that have been asked about the infant brain using near-infrared spectroscopy. Cogn Neuropsychol. 2012;29(1–2):7–33.
Behr R, Müller J, Shehata-Dieler W, Schlake HP, Helms J, Roosen KK, et al. The high rate CIS auditory brainstem implant for restoration of hearing in NF-2 patients. Skull Base. 2007;17:91–107.
Berliner KI, Tonokawa LL, Dye LM, House WF. Open-set speech recognition in children with a single-channel cochlear implant. Ear Hear. 1989;10(4):237–42.
Buchman CA, Teagle HF, Roush PA, Park LR, Hatch D, Woodard J, Zdanski C, Adunka OF. Cochlear implantation in children with labyrinthine anomalies and cochlear nerve deficiency: implications for auditory brainstem implantation. Laryngoscope. 2011;121(9):1979–88.
Carner M, Colletti V, Shannon R, Cerini R, Barillari M, Colletti L. Imaging in 28 children with cochlear nerve aplasia. Acta Otolaryngol. 2009;129(4):458–61.
Casselman J, Mermuys K, Delanote J, Ghekiere J, Coenegrachts K. MRI of the cranial nerves--more than meets the eye: technical considerations and advanced anatomy. Neuroimaging Clin N Am. 2008;18(2):197–231.
Colletti V, Shannon RV. Open set speech perception with auditory brainstem implant? Laryngoscope. 2005;115:1974–8.
Colletti L, Zoccante L. Nonverbal cognitive abilities and auditory performance in children fitted with auditory brainstem implants: preliminary report. Laryngoscope. 2008;118:1443–8.
Colletti V, Carner M, Miorelli V, Colletti L, Guida M, Fiorino F. Auditory brainstem implant in posttraumatic cochlear nerve avulsion. Audiol Neurootol. 2004;9(4):247–55.
Colletti V, Shannon RV, Carner M, et al. Complications in auditory brainstem implant surgery in adults and children. Otol Neurotol. 2010;31:558–64.
Colletti L, Mandalà M, Zoccante L, Shannon RV, Colletti V. Infants versus older children fitted with cochlear implants: performance over 10 years. Int J Pediatr Otorhinolaryngol. 2011;75(4):504–9.
Colletti L, Shannon RV, Colletti V. The development of auditory perception in children after auditory brainstem implantation. Audiol Neurotol. 2014;19(6):386–94.
D’Antona AD, Perry JS, Geisler WS. Humans make efficient use of natural image statistics when performing spatial interpolation. J Vis. 2013;13(14).
Dettman L, Pinder D, Briggs R, Dowell R, Leigh J. Communication development in children who receive the cochlear implant younger than 12 months: risks versus benefits. Ear Hear. 2007;28:11S–8.
Edwards L, Khan S, Langdon D. Exploration of the cognitive and behavioural consequences of paediatric cochlear implantation. Cochlear Implants Int. 2006;7:61–76.
Eisenberg LS, Johnson KC, Martinez AS, DesJardin JL, Stika CL, Dzubak D, Mahalak ML, Rector EP. Comprehensive evaluation of a child with an auditory brainstem implant. Otol Neurotol. 2008;29(2):251–7.
Eisenberg LS, Johnson KC, Martinez AS, Visser-Dumont L, Ganguly DH, Still JF. Studies in pediatric hearing loss at the House Research Institute. J Am Acad Audiol. 2012;23(6):412–21.
Ertmer DJ, Goffman L. Speech production accuracy and variability in young cochlear implant recipients: comparisons with typically developing age-peers. J Speech Lang Hear Res. 2011;54(1):177–89.
Fagan MK, Pisoni DB. Perspectives on multisensory experience and cognitive development in infants with cochlear implants. Scand J Psychol. 2009;50:62–457.
Friesen LM, Shannon RV, Baskent D, Wang X. Speech recognition in noise as a function of the number of spectral channels: comparison of acoustic hearing and cochlear implants. J Acoust Soc Am. 2001;110(2):1150–63.
Friesen LM, Tremblay KL, Rohila N, Wright RA, Shannon RV, Başkent D, Rubinstein JT. Evoked cortical activity and speech recognition as a function of the number of simulated cochlear implant channels. Clin Neurophysiol. 2009;120(4):776–82.
Fu Q-J, Shannon RV. Effects of amplitude nonlinearity on phoneme recognition by cochlear implant users and normal-hearing listeners. J Acoust Soc Am. 1998;104(5):2570–7.
Giraud AL, Lee HJ. Predicting cochlear implant outcome from brain organisation in the deaf. Restor Neurol Neurosci. 2007;25(3-4):381–90.
Govaerts PJ, De Beukelaer C, Daemers K, De Ceulaer D, Yperman M, Somers T, et al. Outcome of cochlear implantation at different ages from 0 to 6 years. Otol Neurotol. 2002;23:885–90.
Govaerts PJ, Casselman J, Daemers K, De Beukelaer C, Yperman M, De Ceulaer G. Cochlear implants in aplasia and hypoplasia of the cochleovestibular nerve. Otol Neurotol. 2003;24(6):887–91.
Gregory RL, Wallace JG. Recovery from early blindness, Experimental psychology society monograph 2. Cambridge: Heifer; 1963.
Hart B, Risley TR. Meaningful differences in the everyday experience of young American children. Baltimore: Peter Bloom Publishing; 1995.
Jusczyk PW, Aslin RN. Infants’ detection of sound patterns of words in fluent speech. Cogn Psychol. 1995;29:1–23.
Kalia A, Lesmes LA, Dorr M, Gandhi T, Chatterjee G, Ganesh S, Bex PJ, Sinha P. Development of pattern vision following early and extended blindness. Proc Natl Acad Sci. 2014;111(5):2035–9.
Khan S, Edwards L, Langdon D. The cognition and behaviour of children with cochlear implants, children with hearing aids and their hearing peers: a comparison. Audiol Neurootol. 2005;10:26–117.
Kishon-Rabin L, Taitelbaum-Swead R, Ezrati-Vinacour R, et al. Prelexical vocalization in normal hearing and hearing- impaired infants before and after cochlear implantation and its relation to early auditory skills. Ear Hear. 2005;26:17S–29.
Kisilevsky BS, Hains SM. Onset and maturation of fetal heart rate response to the mother’s voice over late gestation. Dev Sci. 2011;14(2):214–23.
Kisilevsky BS, Hains SM, Lee K, Xie X, Huang H, Ye HH, Zhang K, Wang Z. Effects of experience on fetal voice recognition. Psychol Sci. 2003;14(3):220–4.
Kronenberger WG, Beer J, Castellanos I, Pisoni DB, Miyamoto RT. Neurocognitive risk in children with cochlear implants. JAMA Otolaryngol Head Neck Surg. 2014;140(7):608–15. PMID: 24854882.
Le Maner-Idrissi G, Barbu S, Bescond G, Godey B. Some aspects of cognitive and social development in children with cochlear implant. Dev Med Child Neurol. 2008;50(10):796–7.
Lecanuet JP, Graniere-Deferre C, Jacquet AY, DeCasper AJ. Fetal discrimination of low-pitched musical notes. Dev Psychobiol. 2000;36:29.
Lee DS, Lee JS, Oh SH, Kim SK, Kim JW, Chung JK, Lee MC, Kim CS. Cross-modal plasticity and cochlear implants. Nature. 2001;409(6817):149–50.
Leffel K, Suskind D. Parent-directed approaches to enrich the early language environments of children living in poverty. Semin Speech Lang. 2013;34(4):267–78.
Manrique M, Cevera-Paz FJ, Huarte A, Molina M. Advantages of cochlear implantation in prelingual deaf children before 2 years of age when compared to later implantation. Laryngoscope. 2004;114:1462–9.
Martinez AS, Eisenberg LS, Boothroyd A. The acoustic change complex in young children with hearing loss: a preliminary study. Semin Hear. 2013;34:278–87.
Matthies C, Brill S, Kaga K, Morita A, Kumakawa K, Skarzynski H, Claassen A, Hui Y, Chiong C, Müller J, Behr R. Auditory brainstem implantation improves speech recognition in neurofibromatosis type II patients. ORL J Otorhinolaryngol Relat Spec. 2013;75(5):282–95.
Matthies C, Brill S, Varallyay C, Solymosi L, Gelbrich G, Roosen K, Ernestus RI, Helms J, Hagen R, Mlynski R, Shehata-Dieler W, Müller J. Auditory brainstem implants in neurofibromatosis Type 2: is open speech perception feasible? J Neurosurg. 2014;120(2):546–58.
Moore JK, Osen KK. The cochlear nuclei in man. Am J Anat. 1979;154(3):393–418.
Moore JK, Niparko JK, Miller MR, Linthicum FH. Effect of profound hearing loss on a central auditory nucleus. Am J Otol. 1994;15(5):588–95.
Nelson DA, Donaldson GS, Kreft H. Forward-masked spatial tuning curves in cochlear implant users. J Acoust Soc Am. 2008;123(3):1522–43.
Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL, Fink NE, et al. Spoken language development in children following cochlear implantation. JAMA. 2010;303(15):1498–506.
Oller DK, Eilers RE. The role of audition in infant babbling. Child Dev. 1988;59:441–9.
Otto SR, Brackmann DE, Hitselberger WE, Shannon RV, Kuchta J. Multichannel auditory brainstem implant: update on performance in 61 patients. J Neurosurg. 2002;96(6):1063–71.
Pisoni D. Cognitive factors and cochlear implants: some thoughts on perception, learning, and memory in speech perception. Ear Hear. 2000;21(1):70–8.
Pisoni DB, Cleary M. Learning, memory and cognitive processes in deaf children following cochlear implantation. In: Popper ANR, Fay R, Zeng FG, editors. Springer handbook of auditory research: auditory prosthesis SHAR, vol. X. New York: Springer; 2004. p. 377–426.
Robbins A, Koch DB, Osberger MJ, Zimmerman-Phillips S, Kishon-Rabin L. Effect of age at cochlear implantation on auditory skill development in infants and toddlers. Arch Otolaryngol Head Neck Surg. 2004;130(5):570–4.
Rothen N, Meier B, Ward J. Enhanced memory ability: insights from synaesthesia. Neurosci Biobehav Rev. 2012;36(8):1952–63.
Ruben RJ, Rapin I. Plasticity of the developing auditory system. Ann Otol Rhinol Laryngol. 1980;89:11–303.
Rubinstein JT. Paediatric cochlear implantation: prosthetic hearing and language development. Lancet. 2002;360:483–5.
Saffran JR. Constraints on statistical language learning. J Mem Lang. 2002;47:172–96.
Saffran JR. Statistical language learning: mechanisms and constraints. Curr Dir Psychol Sci. 2003;12:110–4.
Saffran JR, Aslin RN, Newport EL. Statistical learning by 8-month-old infants. Science. 1996;274:1926–8. PubMed: 8943209.
Schauwers K, Gillis S, Govaerts PJ. The characteristics of prelexical babbling after cochlear implantation between 5 and 20 months of age. Ear Hear. 2008;29(4):627–37.
Sennaroglu L, Ziyal I, Atas A, Sennaroglu G, Yucel E, Sevinc S, Ekin MC, Sarac S, Atay G, Ozgen B, Ozcan OE, Belgin E, Colletti V, Turan E. Preliminary results of auditory brainstem implantation in prelingually deaf children with inner ear malformations including severe stenosis of the cochlear aperture and aplasia of the cochlear nerve. Otol Neurotol. 2009;30(6):708–15.
Sennaroglu L, Colletti V, Manrique M, Laszig R, Offeciers E, Saeed S, Ramsden R, Sarac S, Freeman S, Andersen HR, Zarowski A, Ziyal I, Sollmann WP, Kaminsky J, Bejarano B, Atas A, Sennaroglu G, Yucel E, Sevinc S, Colletti L, Huarte A, Henderson L, Wesarg T, Konradsson K. Auditory brainstem implantation in children and non-neurofibromatosis type 2 patients: a consensus statement. Otol Neurotol. 2011;32(2):187–91.
Shannon RV. Forward masking in patients with cochlear implants. J Acoust Soc Am. 1990;88:741–4.
Shannon RV. Auditory implant research at the House Ear Institute 1989-2013. Hear Res. 2015;322:57–66.
Shannon RV, Fu Q-J, Galvin J. The number of spectral channels required for speech recognition depends on the difficulty of the listening situation. Acta Otolaryngol Suppl. 2004;552:50–4.
Shepherd RK, Hartmann R, Heid S, Hardie N, Klinke R. The central auditory system and auditory deprivation: experience with cochlear implants in the congenitally deaf. Acta Otolaryngol Suppl. 1997;532:28–33.
Shin MS, Kim SK, Kim SS, Park MH, Kim CS, Oh SH. Comparison of cognitive function in deaf children between before and after cochlear implant. Ear Hear. 2007;28(2 Suppl):22S–8.
Smith LS, Dmochowski PA, Muir DW, Kisilevsky BS. Estimated cardiac vagal tone predicts fetal responses to mother’s and stranger’s voices. Dev Psychobiol. 2007;49(5):543–7.
Svirsky MA, Robbins AM, Kirk KI, Pisoni DB, Miyamoto RT. Language development in profoundly deaf children with cochlear implants. Psychol Sci. 2000;11:153–8.
Svirsky MA, Teoh SW, Neuberger H. Development of language and speech perception in congenitally, profoundly deaf children as a function of age at cochlear implantation. Audiol Neurotol. 2004;9:224–33.
Waltzman S, Roland JT. Cochlear implantation in children younger than 12 months. Pediatrics. 2005;116:487–93.
Young NM, Kim FM, Ryan ME, Tournis E, Yaras S. Pediatric cochlear implantation of children with eighth nerve deficiency. Int J Pediatr Otorhinolaryngol. 2012;76(10):1442–8.
Zeng F-G, Shannon RV. Loudness coding mechanisms inferred from electric stimulation of the human auditory system. Science. 1994;264:564–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media LLC
About this chapter
Cite this chapter
Shannon, R., Colletti, L., Colletti, V. (2016). The Neuroscience of the Pediatric Auditory Brainstem Implant. In: Young, N., Iler Kirk, K. (eds) Pediatric Cochlear Implantation. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2788-3_15
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2788-3_15
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2787-6
Online ISBN: 978-1-4939-2788-3
eBook Packages: MedicineMedicine (R0)