Abstract
Before the era of pulmonary arterial hypertension (PAH)-specific therapies, clinicians treating patients with pulmonary hypertension (PH) employed nonspecific, time-honored treatments in an effort to help these unfortunate patients. While the role of these therapies has not been rigorously studied they are still commonly used as adjuncts to PAH-specific therapies. This chapter outlines the logic and rationale behind the use of digoxin therapy, anticoagulation, oxygen therapy, diuretic therapy, and high-dose calcium channel blocker therapy and reviews the limited data supporting the use of these therapies in patients with PAH.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pulmonary hypertension
- Digoxin
- Anticoagulation
- Oxygen therapy
- Diuretic therapy
- Vasodilator responsiveness
- Vasoreactivity testing
- Calcium channel blockers
Introduction
Until the development of pulmonary arterial hypertension (PAH)-specific therapy two decades ago, clinicians relied on nonspecific therapies such as oxygen, diuretics, digoxin, and anticoagulation therapy to relieve symptoms in patients with this dreaded disorder. While these therapeutic approaches did not prove to impact meaningfully on survival [1], most experts feel that these adjunctive therapies have beneficial effects for pulmonary hypertension (PH) patients [2–4] despite the lack of robust, randomized, placebo-controlled data to support these interventions. Their use has been based largely on concepts originating from physiologic observations and experience with these treatments in other cardiac and pulmonary disease states that share symptoms and similar clinical features [4]. While it is unlikely that large, prospective, clinical trials of these standard adjunctive therapies will ever be conducted, their use in conjunction with PAH-specific therapies is well established in the day-to-day clinical management of these patients. This chapter discusses current recommendations regarding these therapies as well as the current role of high-dose calcium channel blocker (CCB) therapy in a subset of PAH patients.
Digoxin Therapy
The use of cardiac glycosides dates back to Sir William Withering’s 1785 description of the use of foxglove in the management of “dropsy” and other diseases [5]. Once a mainstay in the treatment of heart failure and atrial fibrillation, their use has lessened over the years as newer therapies such as vasodilators, angiotensin-converting enzyme (ACE) inhibitors, and newer inotropic agents emerged [6]. Nonetheless, these generally inexpensive and well-tolerated agents still have a role in the management of heart failure [6, 7].
Cardiac glycosides such as digoxin exert a number of potentially beneficial cardiac effects. Digoxin binds to the membrane-bound α subunit of the sodium-potassium ATPase, promoting sodium-calcium exchange which in turn increases the intracellular calcium concentration available to contractile proteins [6–8], with resultant positive inotropic effects. In dogs this positive inotropic effect is obtained with little oxygen wasting making it a metabolically efficient drug [9]. Digitalis preparations have no effect on cardiac output in normal control subjects [6, 10, 11] but significantly improve left ventricular ejection fraction in those with systolic heart failure [12–15]. Aside from their positive inotropic effects digitalis preparations have salutary effects on the neurohormonal activation known to be important in systolic heart failure [16–20].
Numerous double-blinded studies examining the effect of digoxin have demonstrated improvement in clinical status [13, 17, 21–24]. Digoxin reduced the incidence of hospitalizations and the number of emergency room visits for heart failure in the Captopril-Digoxin Multicenter Trial of 300 patients with mild to moderate heart failure [13] and increased the exercise time while reducing both plasma norepinephrine concentrations and renin activity at 6 months of therapy in the Dutch Ibopamine Multicenter Trial [17]. In studies examining the effects of withdrawing digoxin therapy, patients who remained on digoxin maintained their exercise ability whereas those randomized to placebo but continuing on ACE inhibitors and diuretics [21] or diuretics alone [23] had a deterioration in their exercise capacity. In the study by Packer et al. patients withdrawn from digoxin had a sixfold increase in worsening of heart failure as reflected in heart failure-related hospitalizations, emergency care visits for heart failure, or the need for concomitant heart failure therapy [21]. In the largest trial of digoxin therapy to date, 7,788 patients were randomized to 0.25 mg of digoxin daily or placebo in the setting of background ACE inhibitor and diuretic therapy [25]. Although this study showed no difference in all-cause mortality between the placebo and digoxin groups, there was a 25 % reduction in the number of hospitalizations for worsening heart failure in the digoxin-treated group and total hospitalizations were reduced 65 % in the digoxin-treated group [25].
The abundance of data supporting digoxin use for patients with left heart failure resulted in extrapolation to patients with PAH and right heart failure (RHF). Rich et al. studied the effects of a single dose of digoxin in 17 consecutive patients with severe PAH and right heart failure and normal left ventricular function [26]. After 2 h, cardiac output increased from 3.49 + 1.2 L/min to 3.81 L/min + 1.2 L (p = 0.028) suggesting modest inotropic effect. Neurohormonal samples in this study also revealed a significant fall in norepinephrine levels (680 + 89 to 580 + 85 pg/ml; p = 0.013) and significant and unexpected increases in atrial natriuretic peptide (311 + 44 to 421 + 9 pg/ml; p = 0.010) following digoxin administration. Plasma renin activity decreased but not significantly so (0.085 + 1.2 to 0.59 + 1.21 ng/ml/h; p = 0.07). It is of interest in this study that as pulmonary vascular resistance decreased with nitroprusside administration no effect of digoxin on pulmonary artery pressure was noted [26]. Others have suggested a role for digoxin in those with chronic obstructive pulmonary disease (COPD) and associated PAH [World Health Organization (WHO) Class III PAH]. Recent animal data suggests that digoxin may inhibit hypoxia-inducible factor-1 (HIF-1) transcriptional activity in the chronic hypoxia murine model of PH [27]. Mice injected daily with digoxin had attenuated right ventricular (RV) hypertrophy, pulmonary vascular remodeling, and RV pressure compared to saline-treated mice exposed to the same degree of chronic hypoxia [27]. Furthermore, when digoxin was given after PH was already established in these mice, RV pressures and pulmonary artery smooth muscle cell (PASMC) intracellular calcium increases were attenuated as well [27]. Furthermore, early work on digitalis glycosides did demonstrate inotropic effects on the right ventricle [28]. This work has provided theoretical grounds for the use of digoxin in patients with COPD-associated PH. In a study of 15 patients with COPD and RHF, Mathur et al. showed that after 8 weeks of digoxin therapy RV ejection fraction (RVEF) as measured by radionuclide angiography improved in the 4 patients that had reduced left ventricular ejection fractions (LVEF) at the study outset but did not change in the remaining 11 patients who had normal LVEF to begin with [29].
Based on this limited human data, use of digoxin in patients with PAH is controversial. If its use is elected, prescribers should be highly mindful of the potential for toxicity [4, 30, 31]. Since many patients will be on concomitant diuretic therapy, monitoring of serum potassium and magnesium is mandatory [4, 6, 7] as hypokalemia and hypomagnesemia increase automaticity and promote sodium pump inhibition by digoxin with resulting arrhythmogenic effects [6, 33]. Digoxin is renally cleared and should be used with caution in those with impaired renal function and a reduced starting dose is more appropriate in these patients [4, 34]. A recent study of digoxin levels revealed that an increased mortality rate existed for those patients with higher serum digoxin levels with optimum outcomes seen in serum digoxin levels of 0.5–0.8 ng/ml [32]. Mortality risk also seems increased in those with active myocardial ischemia [6, 25, 31] and digoxin should not be used in this setting. The prescriber must also be aware of interactions with agents such as macrolides, cyclosporine, amiodarone, itraconazole, and many other drugs which can increase digoxin levels increasing the potential for toxicity [4, 34, 35].
Anticoagulation
Many factors increase the tendency for patients with PAH to form clot in the pulmonary vascular bed. Many PAH patients lead a more sedentary existence increasing the risk of venous thrombosis. Venous engorgement and stasis also occur due to elevated right atrial (RA) pressures. Advancing disease results in poor flow through the pulmonary circulation as a result of declining cardiac output [4]. Structural remodeling leads to altered interactions between circulating platelets and the pulmonary arterial endothelium [36, 37] with potential for in situ clot formation [36, 38–40]. In addition a number of human studies have revealed idiopathic PAH (IPAH) to be a prothrombotic state [41–57] (see Table 12.1). Interestingly this prothrombotic state does not appear to be the result of inherited thrombophilias [58–60] but rather a dysregulation of the normal balance between thrombin formation and the prevention of clot formation at least in part due to endothelial cell dysfunction [36, 37, 42, 43, 46, 49, 56, 57, 59, 61, 70], in part due to platelet activation [37, 41, 42, 48, 46, 49, 52–54, 57], and in part due to proteins related to coagulation and fibrinolysis [42, 43, 55, 58, 59]. Some of these abnormalities appear reversible with the use of PAH-specific therapies [62–65]. While these observations are supportive of a role for thrombotic arteriopathy in patients with PAH, it is unclear from the current literature if this is a cause or consequence of IPAH or associated forms of PAH (APAH) [57, 61]. Irrespective, thrombotic arteriopathy may alter the disease course and prognosis in IPAH and APAH.
To date, three retrospective [66–68] and one non-blinded, non-placebo-controlled prospective study [69] have suggested a survival advantage to those patients with IPAH treated with anticoagulation in the form of warfarin. In the single-center retrospective study by Fuster et al., the course of 120 IPAH patients pulmonary hypertension was examined. In a multivariate analysis of a number of variables only pulmonary arterial oxygen saturation and use of anticoagulant therapy emerged as prognosticators of survival [66]. In the 56 patients with autopsy lung specimens, 18 had plexogenic arteriopathy and in 32 the major histologic feature was chronic thrombus. To further investigate the role of anticoagulation 78 additional patients treated with anticoagulation were compared to 37 receiving no anticoagulation. This analysis showed a more favorable survivorship in the warfarin-treated group [66]. Of note, from a study design standpoint the numbers were too small to reach statistical significance. Additionally, the criteria used to decide when not to anticoagulate were not clear leaving the potential for selection bias.
In the study by Frank et al., 173 patients with PAH (104 who took aminorex and 69 with PH of unexplained etiology) were retrospectively reviewed [67]. Fifty-six of the 104 aminorex induced PAH and 24 of the 69 patients with IPAH received warfarin therapy. Patients with aminorex APAH fared better than those with IPAH (7.5 years vs. 3.9 years; p = <0.001) and the best survival times occurred in those aminorex APAH who were anticoagulated (8.3 years vs. 6.1 years). In addition, those receiving anticoagulation therapy early after onset of symptoms had a better prognosis (10.9 year survival) than those commencing anticoagulation therapy 2 years or longer after symptomatic presentation [67]. Of note, no differences in survival were seen in the first 5 years of follow-up but some survival advantage was seen in the IPAH group in the subsequent 5 years that did not reach statistical significance.
In a more contemporary retrospective study during an era of PAH-specific therapy, Kawut et al. reviewed patients with PAH that was idiopathic, familial, or associated with anorexigen use [68]. The primary combined end point was death or lung transplantation. Eighty-four patients with newly diagnosed PAH were included. Interestingly, their analysis demonstrated that warfarin use was associated with increased survival in their cohort while the use of other PAH-specific medications were not [68]. Once again, the criteria for deciding who not to anticoagulate was not defined raising concern for potential selection bias.
In the only single-center, prospective trial of warfarin therapy in IPAH, no control group existed and the authors used a historical control group from the National Institute of Health Primary Pulmonary Hypertension Registry. Sixty-four patients were assessed for response to high-dose CCB therapy [69]. Twenty-six % (n = 17) responded (defined as a > 20 % decrease in mean pulmonary artery pressure or a 20 % or more decrease in pulmonary vascular resistance) and were maintained on high-dose CCB for 5 years. Warfarin therapy was given to 55 % of all patients as concurrent therapy. Warfarin therapy was associated with increased survival in the group as a whole, and particularly in patients who were nonresponders to high-dose CCB. The decision to put patients on warfarin therapy was based on the finding of nonuniform perfusion on a ventilation-perfusion (V/Q) scan [69].
Based on the biological rationale offered earlier and on the results of these four studies the current expert recommendation is to treat IPAH patients with warfarin anticoagulation in the absence of contraindications [2, 3] and to consider warfarin therapy in APAH patients with more advanced disease such as those on continuous intravenous therapy, in the absence of contraindications [3]. Since little data exist in the APAH subgroup the presumption that anticoagulation will have beneficial effects on survival remains speculative. The recommended anticoagulation dose of warfarin is that which achieves an international normalized ratio (INR) of 1.5–2.5 [3, 7] though some experts in Europe recommend achieving INRs between 2.0 and 3.0 [4]. A decision to anticoagulate APAH subgroups must be weighed against the risk for potential bleeding complications [71–73] especially in those with systemic sclerosis (SSc) APAH where a high risk of gastrointestinal bleeding can be expected [73]. Indeed, a recent retrospective study of 275 patients with SSc-APAH and 155 patients with IPAH used Bayesian propensity scores to adjust for baseline differences between patients exposed and not exposed to warfarin. In a matched cohort of SSc-APAH (n = 98; 49 treated with warfarin) the median hazard ratio was 1.06 while in a matched cohort of IPAH patients [n = 66; 33 treated with warfarin] the median hazard ratio was 1.07. This analysis suggested that there was a 70 % probability that warfarin provided no significant benefit or was harmful [74]. The authors concluded that SSc-APAH should not receive warfarin therapy. Likewise in portopulmonary APAH, experts advise that anticoagulation should probably be avoided due to the risk of bleeding [2]. In addition, consideration of the other medications being used may influence the decision to anticoagulate as concerning drug-drug interactions can occur [75]. The finding of an increased incidence of subarachnoid hemorrhage in the imatinib-treated patients who were also receiving warfarin in the IMPRES study underscores the need for careful consideration of context in the use of anticoagulation [76]. Anticoagulation is an irrefutable part of the treatment of chronic thromboembolic PAH [77].
While warfarin therapy is the recommended form of anticoagulation, it is not clear that other forms of anticoagulation should not be considered. In fact, numerous animal studies have suggested that heparin may have some advantages in PAH. In a murine model of PH induced by chronic hypoxia, high-dose heparin therapy partially but significantly reduced RV systolic pressures and remodeling of distal small pulmonary arteries [78]. A similar finding has been reported in a guinea pig chronic hypoxia model where PH and total pulmonary resistance were partially reversed with the continuous infusion of heparin [79]. When heparin and warfarin treatment were compared in the same guinea pig model, only heparin showed partial reversal of PH once established [80]. The mechanism for this effect of heparin is unclear but inhibition of platelet-derived growth factor (PDGF) [78] and inhibition of smooth muscle growth in the pulmonary artery perhaps by alterations in the regulation of cyclin-dependent kinase [81] and/or the guanine nucleotide exchange factor −H1/Rho A/Rho kinase/p27 pathway [82] have been suggested. Heparin has not been studied in humans with PAH. Other forms of anticoagulation have not been studied adequately in PAH though a double-blind, placebo-controlled, crossover study of 19 IPAH patients (9 on intravenous (IV) epoprostenol) assessed the effect of aspirin and clopidogrel [83]. The authors noted a reduction in measures of platelet aggregability and aspirin was noted to reduce thromboxane metabolite production without affecting prostaglandin I2 metabolite synthesis [83]. Recently, the direct factor Xa inhibitor rivaroxaban was compared with warfarin and enoxaparin in a monocrotaline rat model of PAH [84]. Rivaroxaban reduced systolic and end-diastolic RV pressure increases and RV hypertrophy while warfarin reduced RV pressure increases only. Enoxaparin had no effect on either RV pressure or RV hypertrophy [83]. Neither of these agents have been studied in humans with PAH.
Oxygen Therapy
The role of oxygen therapy has not been specifically studied in PAH, but recommendations for its use [2, 3] have been extrapolated from data in hypoxemic patients with COPD. It is well known that hypoxemia is a strong stimulus for pulmonary vasoconstriction, possibly through a reactive oxygen species and induced superoxide dismutase pathway [85], and that this occurs as an attempt to match lung perfusion with ventilation. Two landmark trials established the benefit of oxygen therapy in hypoxemic patients with COPD [86, 87], with both studies showing long-term improvements in survival in patients treated with 15 h/day or more of oxygen therapy. Interestingly, oxygen therapy does not correct or even near-correct PH in patients with COPD though it does improve it and the noted improved survival in COPD patients treated with oxygen is not felt to be due to the modest reduction in pulmonary artery pressure (PAP) [88]. In fact, in the Nocturnal Oxygen Therapy in Hypoxemic Chronic Obstructive Lung Disease Trial (NOTT), it was patients with low baseline pulmonary vascular resistance (PVR) that had improved mortality on continuous oxygen supplementation, whereas patients with high PVR did not experience a survival benefit [86]. Those with the largest drop in PVR at right-heart catheterization at 6 months in fact had the greatest mortality again suggesting that alteration of the PH per se did not confer the survival benefit [4, 86].
Many patients with PAH have hypoxemia at rest or intermittently with exercise and sleep, and it is important for practitioners to know that as many as 60 % of PAH patients who do not desaturate with exercise in the office evaluations will do so during sleep even in the absence of sleep apnea [89]. Intermittent worsening of oxygen saturation during exercise is often seen as a consequence of increased right-to-left shunting through a patent foramen ovale. Currently, it is recommended that patients with PAH whose partial pressure of arterial oxygen is consistently less than or equal to 55 mmHg or whose oxyhemoglobin saturation is less than or equal to 88 % at rest, during sleep, or with ambulation receive oxygen therapy [2–4]. In addition, patients with evidence of chronic hypoxemia such as polycythemia (hematocrit >55), signs of cor pulmonale, or suggestion of right heart failure on an electrocardiogram or echocardiography should receive oxygen therapy if the oxyhemoglobin saturation is less than or equal to 89 % or if the PaO2 is less than 60 mmHg [4, 90]. In addition, all patients with a diffusion of carbon monoxide impairment of moderate-to-severe nature warrant testing of oxyhemoglobin desaturation [91, 92]. These recommendations are based solely on expert opinion in patients with IPAH or APAH as no direct evidence exists to support these recommendations (with the exception of COPD-APAH).
The role of oxygen therapy in congenital heart disease (CHD) APAH is controversial. Nocturnal administration of oxygen in children with CHD-APAH has been shown to slow the rate of progression of polycythemia and to improve symptoms [93, 94]. Whether or not oxygen therapy improves survival is not clear. One small study of 15 patients with CHD-APAH studied oxygen supplementation (15 or more h/day) over 5 years. Nine patients received oxygen therapy and six did not. A mortality benefit was seen with 9/9 alive in the oxygen therapy group and 1/6 alive in the untreated group at the 5-year time point [93]. However, a recent well-designed, prospective, randomized, controlled study of 23 adult patients with CHD-APAH and Eisenmenger’s syndrome showed no survival benefit with nocturnal oxygen administration [94]. In addition, no improvement in 6-min walk distances, hematocrit levels, or quality of life were seen in the oxygen-treated group [94].
Patients with obstructive sleep apnea (OSA) will generally have mild-to-moderate PH [95–98] in anywhere from 17 to 53 % of the time [96, 97]. Moderate-to-severe PH should not be attributed to sleep-disordered breathing in these patients and other causes such as pulmonary venous hypertension from obesity cardiomyopathy or concurrent COPD should be looked for. In OSA-related PH continuous positive airway pressure (CPAP) combined with oxygen therapy (when needed) will result in a more pronounced decrease in mean PAP and PVR than that seen in patients treated with oxygen alone. Full resolution of PH in this setting is not expected with even the most compliant of CPAP use [99–101]. Patients with the obesity hypoventilation syndrome, however, can develop severe PAH and RHF and treatment requires noninvasive positive pressure ventilation or bilevel positive pressure ventilation which can reverse hypercapnea and signs of RHF within months [102–104]. In patients who cannot tolerate such therapy tracheostomy with chronic outpatient mechanical ventilation at night should be offered [4] and has the potential to be life saving [105, 106].
Oxygen therapy carries with it a number of logistic and social stigma issues that need to be addressed with its recipients. The inconvenience of ambulatory systems, limitations of time that portable systems allow, danger of falls over long cords and tubing, and stigma some patients feel when seen in public may all negatively impact on the patients’ self-concept and the perception that others have of them. These issues need to be discussed frankly with patients before oxygen therapy is prescribed.
Diuretics
Diuretics are a mainstay in the management of left heart failure [107], and while never systematically studied are universally accepted in the management of peripheral edema in RHF [2–4]. The short-term effects of diuretics in patients with RHF from PH are usually obvious, and their effect on symptoms likewise usually transparent [4]. In fact, the benefit of diuretics is so intuitively obvious that a randomized, double-blinded, controlled, prospective trial is not likely to occur.
Theoretic basis for their use in RHF includes improvement in RV-LV interdependency with reduced paradoxical septal bowing which causes attendant encroachment on LV stroke volume [108] and impairment of LV diastolic function [109, 110]. Aldosterone antagonism has been shown to reduce both morbidity and mortality in patients with severe left heart failure with New York Heart Association class III or IV functional status [111]. In this study a low dose of spironolactone was added to ACE inhibitor therapy and furosemide diuretic therapy. An impressive 35 % decrease in need for subsequent hospitalization was observed and the 2-year mortality was 35 % for the spironolactone group compared to 46 % in controls [111]. No such trial of the effects of aldosterone antagonists has been performed in patients with PAH and RHF. Extreme caution should be used with these agents in patients with RHF who have concurrent renal failure and/or diabetes [4], and in patients using ACE inhibitors or nonsteroidal anti-inflammatory agents [106]. Careful modification of potassium supplements and follow-up of electrolytes are critical when aldosterone antagonists are prescribed.
Amiloride, a potassium-sparing diuretic, has been shown to reduce PASMC proliferation and significantly reduces PAP and total pulmonary resistance compared to controls in a hypoxia-induced rat model of PH [112]. The clinical relevance of this observation to PAH patients is speculative as no clinical studies with these agents in PAH exist.
The use of diuretics in patients with PAH requires careful monitoring. Maintenance of potassium concentration above 4.0 mmol/L is important, especially in patients on digoxin therapy to avoid arrhythmias. Rapid, large-volume diuresis should be avoided except when frank cardiogenic pulmonary edema and/or worsening hypoxemia is present as the very preload-dependent RV may react to underfilling with hypotension [4]. Orthostatic dizziness should be addressed with dose adjustments accordingly to avoid hypotension, but underdosing in the setting of low blood pressure that these patients often have can result in overall clinical worsening, worsening hepatic congestion, or bowel wall edema with symptoms of early satiety [4, 68]. Optimal volume status represents a narrow window requiring frequent evaluations by the practitioner. Patients with RHF often require salt and fluid restriction, leg elevation when not ambulating, and compressive stockings to control their edema in conjunction with judicious diuretic use [4].
Calcium Channel Blockers
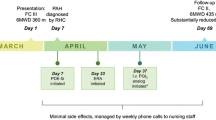
Vasoconstriction is a component of the elevated PVR seen in patients with PAH. In an earlier era, this was felt to be the major component to the aberrant vascular bed in these patients and as such numerous attempts at reversing vasoconstriction with medications originally designed for systemic hypertension ensued [112–115]. As our understanding of the pathogenesis of PAH evolved it became clearer that vasoconstriction was only a part of the story and that dysregulated endothelial cell function with attendant PASMC proliferation, vascular inflammation [36, 116, 117], and in situ thrombosis [38–40, 66] all play pivotal roles in elevating the PVR. As such it is now recognized that only a minority of IPAH patients have primary aberrant vasoconstriction as their phenotype [69, 118, 119] and that when present this corresponds to a truly different genetic subgroup that do not have bone morphogenic receptor protein gene mutations [120]. In fact, by earlier definitions of a positive pulmonary vasodilator response (defined as a drop in mPAP or PVR by >20 %) 26 % of a cohort of IPAH patients demonstrated this phenomena and seemed to do remarkably well during a 5-year follow-up period when treated with high-dose CCB [69]. More recent retrospective evaluation of vasoresponders meeting this earlier criteria revealed that a significant portion of them did not have sustained responses to high-dose CCB [119] resulting in a more stringent definition of a “vasoresponder” [119]. Using these new criteria of a positive pulmonary vasodilator response (drop in mPAP by 10 mmHg or more to an absolute value of 40 or less with no change or an improvement in cardiac output) only 6.8 % of IPAH patients were deemed vasoresponders who might do well with high-dose CCB therapy [119]. These criteria are now the recommended American College of Chest Physicians (ACCP) criteria for diagnosing a positive pulmonary vasodilator response in IPAH patients during right-heart catheterization testing that would predict sustained benefit from high-dose CCB therapy. An acute pulmonary vasodilator response occurs even less often in patients with APAH [121, 122]. The role of acute vasoreactivity testing in APAH and the role of high-dose CCB in these patients are not known, though the report of the French experience by Montani et al. would suggest that they do not have a role in HIV-APAH, connective-tissue disease APAH, or CHD-APAH [122]. There may be a role for high-dose CCB in anorexigen-APAH who meet the ACCP criteria for acute vasoresponders [122]. Pragmatically, acute vasoreactivity testing is still routinely done in many forms of APAH if only to appease insurance companies and third-party payers that cheaper CCB therapy is not appropriate in these patients.
The choice of agent used for acute vasodilator testing has also evolved over time. Use of titrated administration of CCB agents [69] should no longer be used in the current era as these agents are longer acting than current alternatives and they may precipitate systemic hypotension and worsening hypoxemia [4]. Inhaled nitric oxide (iNO), intravenous (IV) prostacyclin, or IV adenosine are all acceptable agents for acute testing [2, 123]. Few head-to-head comparisons of these agents exist but in a recent study comparing IV adenosine to iNO in acute pulmonary vasoreactivity testing, 6 of 39 (15 %) with IPAH were found to be responders by the current ACCP criteria to iNO while none of these patients demonstrated a vasodilator response to adenosine, perhaps due to side effect limitations in reaching the maximal adenosine dose [124]. Regardless of the agent selected, caution must be used in certain situations. Vasodilator testing should not be done in patients with severely depressed cardiac function (e.g., cardiac index < 2.0) as undesirable drops in systemic blood pressure may occur [4]. It should be done with extreme caution in patients with pulmonary artery wedge pressures (PAWP) > 15 mmHg and in the event of sudden worsening of the oxyhemoglobin saturation the trial should be aborted and intravenous morphine, nitroglycerin, and diuretics administered if needed. Reports of acute pulmonary edema development during acute vasodilator testing exist [125–128] and death from such pulmonary edema has occurred in the context of occult pulmonary venoocclusive disease [129]. In patients with elevated PAWP, the use of nitroprusside as an acute vasodilator has been advocated [130]. It should be emphasized that failure to respond acutely to vasodilator testing does not exclude improvement with long-term use of prostacyclin or other PAH-specific therapies [128, 131–133].
Only when patients meet the ACCP criteria for vasoresponsiveness should high-dose CCB therapy be prescribed. This can occur in an inpatient setting with a PA catheter in place or slowly by oral titration as an outpatient [4]. In general, nifedipine should be used in those with heart rates <100 while many advocate diltiazem for those with heart rates >100 [4, 69, 119, 134]. Amlodipine is also an acceptable agent in vasoreactive patients [4]. Close follow-up is essential as nearly half of the patients meeting acute vasodilator criteria will not have durable response and may require other PAH-specific therapies [119]. Empiric use of CCB is never indicated and may be fatal [4]. The studies of high-dose CCB properly applied in the proper subgroup suggest excellent survivals compared with nonresponders [69, 119]. A small observational study of seven patients initially shown to be nonresponders appeared to develop a vasodilator response several months after treatment with epoprostenol [134]. The clinical significance of this and its implication for CCB use in this subgroup of patients are unknown.
Summary
In an era of PAH-specific therapies, adjunctive use of digoxin, anticoagulation, oxygen, and diuretics is still advised in IPAH patients on the basis of retrospective, uncontrolled studies or on assumptions from data in other similar disease states [2, 3]. Their use in APAH remains speculative but common. In the absence of better randomized, controlled studies a low threshold should exist for discontinuation should side effects or tolerability issues emerge. Acute vasoreactivity testing defines a small subset of IPAH patients in whom high-dose CCB monotherapy can be effective. These patients generally have a better prognosis and greater survival times but still require close monitoring for durability of response as many will ultimately require addition of other PAH-specific therapies.
Abbreviations
- ACCP:
-
American College of Chest Physicians
- ACE:
-
Angiotensin-converting enzyme
- APAH:
-
Associated pulmonary arterial hypertension
- CCB:
-
Calcium channel blocker
- CHD:
-
Congenital heart disease
- CO:
-
Cardiac output
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- HIF-1:
-
Hypoxia-inducible factor-1
- iNO:
-
Inhaled nitric oxide
- INR:
-
International normalized ratio
- IPAH:
-
Idiopathic pulmonary arterial hypertension
- LA:
-
Left atrium
- LAP:
-
Left atrial pressure
- LV:
-
Left ventricle
- LVEF:
-
Left ventricular ejection fractions
- mPAP:
-
Mean pulmonary artery pressure
- OSA:
-
Obstructive sleep apnea
- PA:
-
Pulmonary artery
- PAH:
-
Pulmonary arterial hypertension
- PASMC:
-
Pulmonary artery smooth muscle cells
- PAWP:
-
Pulmonary artery wedge pressure
- PH:
-
Pulmonary hypertension
- PVR:
-
Pulmonary vascular resistance
- RA:
-
Right atrial
- RHF:
-
Right heart failure (RHF)
- RV:
-
Right ventricle
- RVEF:
-
Right ventricular ejection fraction
- SSc:
-
Systemic sclerosis
- WHO:
-
World Health Organization
References
D’Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991;115:343–9.
Badesch DB, Abman SH, Ahearn GS, Barst RJ, McCrory DC, Simonneau G, et al. Medical therapy for pulmonary hypertension. ACCP evidence-based clinical practice guidelines. Chest. 2004;126:S35–62.
ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension. J Am Coll Cardiol. 2009;53:1573–619.
Alam S, Palevsky HI. Standard therapies for pulmonary arterial hypertension. Clin Chest Med. 2007;28:91–115.
Withering W. An account of the foxglove and some of its medical uses, with practical remarks on dropsy, and other diseases. In: Willis FA, Keys TE, editors. Classics of cardiology, vol. 1. New York: Henry Schuman, Dover Publications; 1941. p. 231–52.
Eichhorn EJ, Gheorghiade M. Digoxin. Prog Cardiovasc Dis. 2002;44:251–66.
Dec GW. Digoxin remains useful in the management of chronic heart failure. Med Clin N Am. 2003;87:317–37.
Little WC, Rassi A, Freeman GL. Comparison of effects of dobuatmine and ouabaing on left ventricular contraction and relaxation in closed-chest dogs. J Clin Invest. 1987;80:613–20.
Li PC, Hos CS, Swaminathan R. The chronic effects of long-term digoxin administration on Na+/K+-ATPase activity in rat tissues. Int J Cardiol. 1993;40:95–100.
Hasenfuss G, Mulieri LA, Allen PD, Just H, Alpert NR. Influence of isoproterenol and ouabain on excitation-contraction coupling, cross-bridge function, and energetics in failing human myocardium. Circulation. 1996;94:S3155–60.
Braunwald E. Effects of digitalis on the normal and the failing heart. J Am Coll Cardiol. 1985;5:S51A–9.
Mason DT, Braunwald E. Studies on digitalis. IX. Effects of oubain on the nonfailing human heart. J Clin Invest. 1963;42:1105–11.
The Captopril-Digoxin Multicenter Research Group. Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. JAMA. 1988;259:539–44.
Gheorghiade M, Hall V, Lakier JB, Goldstein S. Comparative hemodynamic and neurohormonal effects of intravenous captopril and digoxin and their combinations in patients with severe heart failure. J Am Coll Cardiol. 1989;13:134–42.
Davies RF, Beanland DS, Nadeau C, Phanefu D, Morris A, Parker JO, et al. Enalapril versus digoxin in patients with congestive heart failure: a multicenter study. Canadian enalapril versus digoxin study group. J Am Coll Cardiol. 1991;18:1602–9.
Gheorghiade M, Ferguson D. Digoxin. A neurohormonal modulator in heart failure? Circulation. 1991;84:2181–6.
Van Veldhusien DJ, Man int’Veld AJ, Dunselman PHJM, Lok DJA, Dohmen HJM, Poortersmans JC, et al. Double-blind placebo-controlled study of Ibopamine and digoxin in patients with mild to moderate heart failure: results of the Dutch ibopamine multicenter trial (DIMT). J Am Coll Cardiol. 1993;22:1564–73.
Krum H, Bigger JT, Goldsmith RL, Packer M. Effect of long-term digoxin therapy on autonomic function in patients with chronic heart failure. J Am Coll Cardiol. 1995;25:289–94.
Newton GE, Tong JH, Schofield AM, Baines AD, Floras JS, Parker JD. Digoxin reduces cardiac sympathetic activity in severe congestive heart failure. J Am Coll Cardiol. 1996;28:155–61.
Ferguson DW, Berg WJ, Sanders JS, Roach PJ, Kempf JS, Kienzle MG. Sympathoinhibitory responses to digitalis glycosides in heart failure patients. Direct evidence from sympathetic neural recordings. Circulation. 1989;80:65–77.
Packer M, Gheorghiade M, Young JB, Costantini PJ, Adams KF, Cody RJ, et al. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin –converting-enzyme inhibitors. N Engl J Med. 1993;329:1–7.
DiBianco R, Shabetai R, Kostuk W, Moran J, Schlant RC, Wright R. A comparison of oral milrionoe, digoxin, and their combination in the treatment of patients with chronic heart failure. N Engl J Med. 1989;320:677–83.
Uretsky BF, Young JB, Shahidi FE, Yellen LG, Harrison MC, Jolly MK. Randomized study assessing the effect of digoxin withdrawal in patients with mild to moderate chronic congestive heart failure: results of the PROVED trial. J Am Coll Cardiol. 1993;22:955–62.
Gheorghiade M, Zarowitz BJ. Review of randomized trials of digoxin therapy in patients with chronic heart failure. Am J Cardiol. 1992;69:S48G–63.
The Digitalis Investigation Group. The effect of digoxin on mortality in patients with heart failure. N Engl J Med. 1997;336:525–33.
Rich S, Seidlitz M, Dodin E, Osimani D, Judd D, Genthner D, et al. Chest. 1998;114:787–92.
Abud EM, Undem C, Punjab A, Zaiman AL, Myers AC, Semenza GL, et al. Digoxin inhibits development of hypoxic pulmonary hypertension in mice. PNAS. 2012;109:1239–44.
Cattell M, Gold H. The influence of digitalis glycosides on the force of contraction of mammalian cardiac muscle. J Pharmacol Exp Ther. 1938;62:116–25.
Mathur PN, Powles P, Pugsley SO, McEwan MP, Campell EJM. Effect of digoxin on right ventricular function in severe chronic airflow obstruction. Ann Intern Med. 1981;95:283–8.
Marik PE, Fromm L. A case series of hospitalized patients with elevated digoxin levels. Am J Med. 1998;105:110–5.
Leor J, Goldbout U, Rabinowitz B, Reicher-Ross H, Boyko V, Kaplinsky E, et al. Digoxin and increased mortality among patients recovering from acute myocardial infarction: importance of digoxin dose. Cardiovasc Drugs Ther. 1995;9:723–9.
Rathore SS, Curtis JP, Wang Y, Bristow MR, Krumholz HM. Association of serum digoxin concentration and outcomes in patients with heart failure. JAMA. 2003;289:871–8.
Smith TW, Antman EM, Friedman PL, Blatt CM, Marsh JD. Digitalis glycosides: mechanisms and manifestations of toxicity. Prog Cardiovasc Dis. 1984;27(1):21–56.
Jelliffe RW, Brooker G. A nomogram for digoxin therapy. Am J Med. 1974;57:63–8.
Juurlink DN, Mamdani M, Kopp A, Laupacis A, Redelmeir DA. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 2003;289:1652–8.
Humbert M, Morrell NW, Archer SL, Stenmark KR, MacLean MR, Lang IM, et al. Cellular and molecular pathobiology of pulmonary arterial hypertension. J Am Coll Cardiol. 2004;43:S13–24.
Johnson SR, Granton JT, Mehta S. Thrombotic arteriopathy and anticoagulation in pulmonary hypertension. Chest. 2006;130:545–52.
Wagenvoort CA. Lung biopsy specimens in the evaluation of pulmonary vascular disease. Chest. 1980;77:614–25.
Bjornsson J, Edwards WD. Primary pulmonary hypertension: a histopathological study of 80 cases. Mayo Clin Proc. 1985;60:16–25.
Pietra GG, Edwards WD, Kay JM, Rich S, Kernis J, Schloo B, et al. Histopathology of primary pulmonary hypertension. A qualitative and quantitative study of pulmonary vessels from 58 patients in the National Heart, Lung, and Blood Institute Primary Pulmonary Hypertension Registry. Circulation. 1989;80:1198–206.
Christman BW, McPherson CD, Newman JH, King GA, Bernard BR, Groves BM, et al. An imbalance between the excretion of thromboxane and prostacyclin metabolites in pulmonary hypertension. N Engl J Med. 1992;327:70–5.
Welsh CH, Hassell KL, Badesch DB, Kressin DC, Marlar RA. Coagulation and fibrinolytic profiles in patients with severe pulmonary hypertension. Chest. 1996;110:710–7.
Collados MR, Sandoval J, Lopez S, Masso FA, Paez A, Borbolla JR, Monatano LF. Characterization of von Willebrand factor in primary pulmonary hypertension. Heart Vessels. 1999;14:246–52.
Lopes AA, Maeda NY. Circulating von Willebrand factor antigen as a predictor of short-term prognosis in pulmonary hypertension. Chest. 1998;114:1276–82.
Lopes AA, Maeda NY, Aiello VD, Bydlowski SP. Abnormal multimeric and oligomeric composition is associated with enhanced endothelial expression of von Willebrand factor in pulmonary hypertension. Chest. 1993;104:1455–60.
Geggel RL, Carvalho AC, Hoyer LW, Reid LM. von Willebrand factor abnormalities in primary pulmonary hypertension. Am Rev Respir Dis. 1987;135:294–9.
Huber K, Beckman R, Frank H, Kneussl M, Mlczoch J, Binder BR. Am J Respir Crit Care Med. 1994;150:929–33.
Lopes AA, Maeda NY, Almeida A, Jaeger R, Ebaid M, Charmone DF. Circulating platelet aggregates indicative of in vivo platelet activation in pulmonary hypertension. Angiology. 1993;44:701–6.
Cacoub P, Karmochkine M, Dorent R, Nataf P, Piette JC, Godeau P, et al. Plasma levels of thrombomodulin in pulmonary hypertension. Am J Med. 1996;101:160–4.
Eisenberg PR, Lucore C, Kaufman L, Sobel BE, Jaffe AS, Rich S. Circulation. 1990;82:841–7.
Can MM, Tanboga IH, Demircan HC, Ozkan A, Koca F, Keles N, et al. Enhanced hemostatic indices in patients with pulmonary arterial hypertension: an observational study. Thromb Res. 2010;126:280–2.
Herve P, Droute L, Dosquet C, Launa JM, Rain B, Simonneau G, et al. Primary pulmonary hypertension in a patient with a familial platelet storage pool disease: role of serotonin. Am J Med. 1990;89:117–20.
Herve P, Launau JM, Scrobohaci M, Brenot F, Simonneau G, Petipretz P, et al. Increased plasma serotonin in primary pulmonary hypertension. Am J Med. 1995;99:249–54.
Kerveur A, Callebert J, Humbert M, Herve P, Simonneau J, Launay JM, Drouet L. High plasma serotonin levels in primary pulmonary hypertension. Effect of long-term epoprostenol(prostacyclin) therapy. Arterioscler Thromb Vasc Biol. 2000;20:2233–9.
Langleben D, Moroz LA, McGregor M, Lisbona R. Decreased half-life of fibrinogen in primary pulmonary hypertension. Thromb Res. 1985;40:577–80.
Giaid A, Saleh D. Reduced expression of endothelial nitric oxide synthase in the lungs of patients with pulmonary hypertension. N Engl J Med. 1995;333:214–21.
Archer SL, Djaballah K, Humbert M, Weir EK, Fartoukh M, Dallava-santucci J, et al. Am J Respir Crit Care Med. 1998;158:1061–7.
Wolf M, Boyer-Neumann C, Parent F, Eschwege V, Jaillet H, Meyer D, et al. Thrombotic risk factors in pulmonary hypertension. Eur Respir J. 2000;15:395–9.
Hoeper MM, Sosada M, Fabel H. Plasma coagulation profiles in patients with severe primary pulmonary hypertension. Eur Respir J. 1998;12:1446–9.
Lang IM, Klepeko W, Pabinger I. No increased prevalence of factor V Leiden mutation in chronic major vessel thromboembolic pulmonary hypertension (CTEPH). Thromb Haemost. 1996;76:476–7.
Chaouat A, Weitzenblum E, Higenbottom T. The role of thrombosis in severe pulmonary hypertension. Eur Respir J. 1996;9:356–63.
Girgis RE, Champion HC, Diette GB, Johns RA, Permutt S, Sylvester JT. Am J Respir Crit Care Med. 2005;172:352–7.
Veyradier A, Nishikubo T, Humbert M, Wolf M, Sitbon O, Simonneau G, et al. Improvement of von Willebrand factor proteolysis after prostacyclin infusion in severe pulmonary arterial hypertension. Circulation. 2000;102:2460–2.
Sakamaki F, Kyotani S, Nagaya N, Sato N, Oya H, Satoh T, et al. Increased plasma p-selectin and decreased thrombomodulin in pulmonary arterial hypertension were improved by continuous prostacyclin therapy. Circulation. 2000;102:2720–5.
Boyer-Neumann C, Brenot F, Wolf M, Peynaud-Debayle E, Duroux P, Meyer D, et al. Continuous infusion of prostacyclin decreases plasma levels of tPA and PAI-1 in pulmonary hypertension. Thromb Haemost. 1995;73:735–6.
Fuster V, Steele PM, Edwards WD, Gersh BJ, McGoon M, Frye RL. Primary pulmonary hypertension: natural history and importance of thrombosis. Circulation. 1984;70:580–7.
Frank H, Mlczoch J, Huber K, Schuster E, Gurtner P, Kneusl M. Chest. 1997;112:714–21.
Kawut SM, Horn EM, Berekashvili KK, Garofano RP, Goldsmith RL, Widliz AC, et al. New predictors of outcomes in idiopathic pulmonary arterial hypertension. Am J Cardiol. 2005;95:199–203.
Rich S, Kaufman E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med. 1992;327:76–81.
Hrachovinova JP, Ambroz D, Maresova J, Polacek P, Simkova I, Linhart A, et al. Effect of warfarin anticoagulation on thrombin generation in patients with idiopathic pulmonary arterial hypertension. Bratisi Lek Listy. 2010;111:595–8.
Levine MN, Raskob G, Beyth RJ, Keron C, Schulman S. Hermorrhagic complications of anticoagulant treatment: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004;126:S287–310.
Optiz CF, Mueller EA, Pittrow D. Bleeding events in pulmonary arterial hypertension. Eur J Clin Invest. 2009;39:68–73.
Duchini A, Sessoms SL. Gastrointestinal hemorrhage in patients with systemic sclerosis and CREST syndrome. Am J Gastroenterol. 1998;1998(93):1453–6.
Johnson SR, Granton JT, Tomlinson GA, Grosbein HA, Le T, Lee P, et al. Warfarin in systemic sclerosis-associated and idiopathic pulmonary arterial hypertension. A Bayesian approach to evaluation treatment for uncommon disease. J Rheumatol. 2012;39:276–85.
Spangler ML, Saxean S. Warfarin and bosentan interactions in a patient with pulmonary hypertension secondary to bilateral pulmonary emboli. Clin Ther. 2010;32:53–6.
Hoeper MM, Barst RJ, Bourge RC, Feldman J, Frost AE, Galié N, Gómez-Sánchez MA, Grimminger F, Grünig E, Hassoun PM, Morrell NW, Peacock AJ, Satoh T, Simonneau G, Tapson VF, Torres F, Lawrence D, Quinn DA, Ghofrani HA. Imatinib mesylate as add-on therapy for pulmonary arterial hypertension: results of the randomized IMPRES study. Circulation. 2013;127(10):1128–38.
Poli D, Miniati M. The incidence of recurrent venous thromboembolism and chronic thromboembolic hypertension following a first episode of pulmonary embolism. Curr Opin Pulm Med. 2011;17:392–7.
Hales CA, Kradin RL, Brandstetter RD, Zhu YJ. Impairment of hypoxic pulmonary artery remodeling by heparin in mice. Am Rev Respir Dis. 1983;128:747–51.
Hassoun PM, Thompson BT, Hales CA. Partial reversal of hypoxic pulmonary hypertension by heparin. Am Rev Respir Dis. 1992;145:193–6.
Hassoun PM, Thompson BT, Steigman D, Hales CA. Effect of heparin and warfarin on chronic hypoxic pulmonary hypertension and vascular remodeling in the guinea pig. Am Rev Respir Dis. 1989;139:763–8.
Yu L, Quinn DA, Garg HG, Hales CA. Gene expression of cyclin-dependent kinase inhibitors and effect of heparin on their expression in mice with hypoxia-induced pulmonary hypertension. Biochem Biophys Res Commun. 2006;345:1565–72.
Yu L, Quinn DA, Garg HG, Hale CA. Heparin inhibits pulmonary artery smooth muscle cell proliferation through guanine nucleotide exchange factor-H1/RhoA/Rho kinase/p27. Am J Respir Crit Care Med. 2011;44:524–30.
Robbins IM, Kawut SM, Yung D, Reilly MP, Loyd W, Cunningham G, et al. A study of aspirin and clopidogrel in idiopathic pulmonary hypertension. Eur Respir J. 2006;27:578–84.
Delbeck M, Nickel KF, Perzborn E, Ellinghaus P, Strassburger J, Kast R, et al. A role for coagulation factor Xa in experimental pulmonary hypertension. Cardiovasc Res. 2011;92:159–68.
Weissman N, Tadic A, Hanze J, Rose F, Winterhalder S, Nollen M, et al. Hypoxic vasoconstriction in intact lungs: a role for NADPH oxidase-derived H2O2? Am J Physiol Lung Cell Mol Physiol. 2000;279:L683–90.
Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease. Ann Intern Med. 1980;93:391–8.
Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema: report of the Medical Research Council Working Party. Lancet 1981;1:681-6.
Timms RM, Khaja FU, Williams GW, Nocturnal Oxygen Therapy Trial Group. Hemodynamic response to oxygen therapy in chronic obstructive pulmonary disease. Ann Intern Med. 1985;102:29–36.
Minai O, Pandya C, Golish JA, Avecillas JF, McCarthy K, Marlow S, et al. Predictors of nocturnal oxygen desaturation in pulmonary artery hypertension. Chest. 2007;131:109–17.
Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO workshop report. In: Global initiative for chronic obstructive pulmonary lung disease. Bethesda, MD: National Heart, Lung and Blood Institute; 2005 Available at http://www.goldcopd.com/Guidelineitem.asp?11=2&12=1&intID=989. Accessed October 7, 2012.
Owens GR, Rogers RM, Pennock B, Levin D. The diffusing capacity as a predictor of arterial oxygen desaturation during exercise in patients with chronic obstructive pulmonary disease. N Engl J Med. 1984;310:1218–21.
Kelley MA, Panettieri RA, Krupinski AV. Resting single-breath diffusion capacity as aw screening test for exercise-induced hypoxemia. Am J Med. 1986;80:807–12.
Bowyer JJ, Bust CM, Denison DM, Shinebourne EA. Effect of long term oxygen treatment at home in children with pulmonary vascular disease. Br Heart J. 1986;55:385–90.
Widlitz A, Barst RJ. Pulmonary artery hypertension in children. Eur Respir J. 2003;21:155–76.
Sandoval J, Aguirre JS, Pulido T, Martinez-guerra L, Santos E, Avlarado P, et al. Nocturnal oxygen therapy in patients with the Eisenmenger syndrome. Am J Respir Crit Care Med. 2001;164:1682–7.
Koo KW, Sax DS, Snider G. Arterial blood gases and pH during sleep in chronic obstructive pulmonary disease. Am J Med. 1975;58:663–70.
Atwood CW, McCrory D, Garcia JG, Abman SH, Ahearn GS. Pulmonary artery hypertension and sleep-disordered breathing: ACCP evidence-based clinical practice guidelines. Chest. 2004;126:S72–7.
Podszus T, Bauer W, Mayer J, Penzel T, Peter JH, von Wichert P. Sleep apnea and pulmonary hypertension. Klin Wochenschr. 1986;64:131–4.
Alchanatis M, Tourkhhoriti G, Kakaouros S, Kosmas E, Podaras S, Jordanoglou JB. Daytime pulmonary hypertension in patients with obstructive sleep apnea. The effect of continuous positive airway pressure on pulmonary hemodynamics. Respiration. 2001;68:566–72.
Sakjov D, Saunders NA, Bune AJ, McEvoy RD. Continuous positive airway pressure treatment improves pulmonary hemodynamics in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2002;165:152–8.
Arias M, Garcia-Rio F, Alonso-Fernandes A, Martinez I, Viallamor J. Pulmonary hypertension in obstructive sleep apnoea: effects of continuous positive airway pressure: a randomized, controlled cross-over study. Eur Heart J. 2006;27:106–13.
Littleton SW, Mokhlesi B. The Pickwickian syndrome – obesity hypoventilation syndrome. Clin Chest Med. 2009;30:467–78.
Kessler R, Chaouat A, Schinkewitch P, Faller M, Casel S, Krieger J, et al. The obesity-hypoventilation syndrome revisited. A prospective study of 34 consecutive cases. Chest. 2001;120:369–76.
Masa JF, Celli BR, Riesco JA, Hernandez M, Sanches de Cos J, Disdier C. The obesity hypoventilation syndrome can be treated with mechanical ventilation. Chest. 2001;119:1102–7.
Nowbar S, Burkart KM, Gonzales R, Fedorowicz A, Gozansky WS, Gaudio JC, et al. Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. Am J Med. 2004;116:1–7.
Budweiser S, Riedi SG, Jorres RA, Heinemann F, Pfeifer M. Mortality and prognostic factors in patients with obesity-hypoventilation syndrome undergoing noninvasive ventilation. J Intern Med. 2007;261:375–83.
ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult. A report of the American College of Cardiology/American Heart Association Task Force for Practice Guidelines (Writing Committee to update the 2001 Guidelines for the Evaluation and Management of Heart Failure) ACC-www.acc.org; AHA-www.americanheart.org 2005; e1-e82.
Gan CTJ, Lankhaar JWS, Marcus T, Westerhof N, Marques KM, Bronzwaer JGF, et al. Impaired left ventricular filling due to right-to-left ventricular interaction in patients with pulmonary arterial hypertension. Am J Physiol Heart Circ Physiol. 2006;290:H1528–33.
Dittrich HC, Chow LC, Nicod PH. Early improvement in left ventricular diastolic function after relief of chronic right ventricular pressure overload. Circulation. 1989;80:823–30.
Krayenbuehl HP, Turina J, Hess O. Left ventricular function in chronic pulmonary hypertension. Am J Cardiol. 1978;41:1150–8.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe left heart failure. N Engl J Med. 1999;341:709–17.
Quinn DA, Du HK, Thompson BT, Hales CA. Amiloride analogs inhibit chronic hypoxic pulmonary hypertension. Am J Respir Crit Care Med. 1998;157:1263–8.
Rubin LJ, Peter RH. Oral hydralazine therapy for primary pulmonary hypertension. N Engl J Med. 1980;302:69–73.
Carmerini F, Alberti E, Klugmann S, Salvi A. Primary pulmonary hypertension: effects of nifedipine. Br Heart J. 1980;44:352–6.
Packer M, Greenberg B, Massie B, Dash H. Deleterious effects of hydralazine in patients with pulmonary hypertension. N Engl J Med. 1982;306:1326–31.
McLaughlini VV, McGoon MD. Pulmonary arterial hypertension. Circulation. 2006;114(13):1417–31.
Newman JH, Phillips JA, Loyd JE. Narrative review: the enigma of pulmonary arterial hypertension: new insights from genetic studies. Ann Intern Med. 2008;148:278–83.
Rich S, Kaufmann E. High dose titration of calcium channel blocking agents for primary pulmonary hypertension: guidelines for short-term testing. J Am Coll Cardiol. 1991;18:1323–7.
Sitbon O, Humbert M, Jais X, Ioos V, Hamid AM, Provencher S, et al. Long-term response to calcium channel blockers in idiopathic pulmonary hypertension. Circulation. 2005;111:3105–11.
Elliot CG, Glissmeyer EW, Gavlena GT, Carlquist J, McKinney JT, McGoon MD, et al. Relationship of BMPR2 mutations to vasoreactivity in pulmonary arterial hypertension. Circulation. 2006;113:2509–15.
Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al. Pulmonary arterial hypertension in France. Results from a national registry. Am J Respir Crit Care Med. 2006;173:1023–30.
Montani D, Savale L, Natali D, Jais X, Herve P, Garcia G, et al. Long-term response to calcium-channel blockers in non-idiopathic pulmonary arterial hypertension. Eur Heart J. 2010;31:1898–907.
Guidelines of diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J. 2004;25:2243–78.
Oliveira EC, Ribeiro ALP, Amaral CFS. Adenosine for vasoreactivity testing in pulmonary hypertension: a head-to-head comparison with inhaled nitric oxide. Respir Med. 2010;104:606–11.
Preston IR, Klinger JR, Houtchens J, Nelson D, Mehta S, Hill NS. Pulmonary edema caused by inhaled nitric oxide therapy in two patients with pulmonary hypertension associated with CREST syndrome. Chest. 2002;121:656–9.
Farber HW, Graven KK, Kokolski G, Korn JH. Pulmonary edema during acute infusion of epoprostenol in a patient with pulmonary hypertension and limited scleroderma. J Rheumatol. 1999;26:1195–6.
Strange C, Bolster M, Mazur J, Taylor M, Gossage JR, Silver R. Chest. Hemodynamic effects of epoprostenol in patients with systemic sclerosis and pulmonary hypertension. 2000;118:1077–82.
Rubin LJ, Mendoza J, Hood M, McGoon M, Barst R, Williams WB, et al. Treatment of primary pulmonary hypertension with continuous intravenous prostacyclin (epoprostenol). Results of a randomized trial. Ann Intern Med. 1990;112:485–91.
Palmer SM, Robinson LJ, Wang A, Gossage JR, Bashore T, Tapson VF. Massive pulmonary edema and death after prostacyclin infusion in a patient with pulmonary veno-occlusive disease. Chest. 1998;113:237–40.
Zakliczynski M, Zebik T, Maruszewski M, Swierad M, Zembala M. Usefulness of pulmonary hypertension reversibility test with sodium nitroprusside in stratification of early death risk after orthotopic heart transplantation. Transplant Proc. 2005;37:1346–8.
Barst RJ, Rubin LJ, McGoon MD, Caldwell EJ, Long WA, Levy PS. Survival in primary pulmonary hypertension with long-term continuous intravenous prostacyclin. Ann Intern Med. 1994;121:409–15.
Barst RJ, Rubin LJ, Long WA, McGoon MD, Rich S, Badesch DB, et al. A comparison of continous intravenous epoprostenol(prostacylin) with conventional therapy for primary pulmonary hypertension. N Engl J Med. 1996;334:296–301.
Rich S, Brundage BH. High-dose calcium channel-blocking therapy for primary pulmonary hypertension: evidence for long-term reduction in pulmonary arterial pressure and regression of right ventricular hypertrophy. Circulation. 1987;76(1):135–41.
Ziesche R, Petkov V, Wittman K, Kopatschka J, Striebellehner L, Schenk P, et al. Treatment with epoprostenol reverts nitric oxide non-responsiveness in patients with primary pulmonary hypertension. Heart. 2000;83:406–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Trow, T.K. (2015). Adjunct Therapy and Calcium Channel Blockers. In: Klinger, J., Frantz, R. (eds) Diagnosis and Management of Pulmonary Hypertension. Respiratory Medicine, vol 12. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-2636-7_12
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2636-7_12
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-2635-0
Online ISBN: 978-1-4939-2636-7
eBook Packages: MedicineMedicine (R0)