Abstract
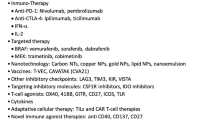
The standard approach for malignant melanoma is represented by surgical excision. In most cases, distant metastases develop. Until few years ago, the main strategies to treat metastatic melanoma were chemotherapy and cytokines with subsequent low efficacy and poor tolerability profile. In the last few years, a new biological therapy has become available for metastatic melanoma. It includes targeted therapy, such as BRAF inhibitors (vemurafenib and dabrafenib) and MEK inhibitors (trametinib), and immunotherapy, such as the monoclonal antibodies anti-CTLA-4 (ipilimumab) and anti-PD-1 (nivolumab and lambrolizumab). The different mechanisms of action of these new drugs imply a variability of outcomes achieved and tolerability profiles. Consequently, the therapeutic options for patients who are diagnosed with metastatic malignant melanoma have been radically changed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Melanoma is the most serious and aggressive form of skin cancer and the sixth most common cancer in North America. The incidence of melanoma has been continuously increasing in the last decades, and faster than any other cancers. It is estimated that 76,100 Americans will be diagnosed with melanoma and 9710 will die from the disease in 2014 [1].
Melanoma is a high-grade, poorly differentiated malignant tumor of melanin pigment-producing cells (melanocytes) with poor prognosis in the metastatic stage, accounting for more than 70 % of the skin cancer related deaths. Melanomas may arise from the mucosal epithelium covering the respiratory, alimentary, and genitourinary tracts (55, 24, and 18 % of cases, respectively), all of which contain melanocytes, as well as from the skin. Mucosal melanomas are rare, account for approximately 1 % of all melanomas and generally carry a worse prognosis than those arising from cutaneous sites. Rare sites of origin include the urinary tract, gall bladder, and small intestine. However, due to the rarity of mucosal melanoma, the understanding of these malignancies and their optimal clinical management remains limited [2]. Instead, there are four major subtypes of invasive cutaneous melanoma: superficial spreading, nodular melanoma, lentigo maligna, and acral lentiginous. For patients with cutaneous melanoma, the prognosis is related to the location and depth of the primary tumor, and the presence or absence of locoregional and distant metastatic disease [3].
Malignant melanoma arises from the neoplastic transformation of epidermal melanocytes resulting from complex interaction between genetic and environmental factors [4, 5]. Sun exposure is widely considered as the critical environmental risk factor for cutaneous malignant melanoma, which originates as a consequence of deleterious interactions between ultraviolet (UV) radiations and the melanocyte genome [6]. In fact, UV radiations may contribute to melanoma development through combined genotoxic and mitogenic effects in melanocytes.
Melanoma is the most dangerous form of skin cancer in the white population, being largely resistant to conventional therapies at advanced stages. The management of patients with advanced melanoma represents a significant challenge considering that, historically, chemotherapy and immunologic therapies have produced only modest results in the treatment of metastatic melanoma. Patients with metastatic melanomas have a median survival rate that typically ranges from 6 to 10 months [7]. Although new lines of targeted therapy and immunotherapy were introduced recently, clinical responses are still either too transient or limited to restricted subsets of patients as it is hard to target the elusive metastatic phenotype. Currently, prevention and early detection represent the only effective strategies to reduce the incidence of this tumor. Despite improvements in early melanoma diagnosis, the 5-year survival rate remains low in advanced disease [8]. Understanding the molecular mechanisms underlying this disease might be the key factor for the development of novel therapeutic strategies.
Molecular Biology of Melanoma
Tumor growth is the result of genetic and/or epigenetic alterations in key genes, regulating processes such as apoptosis, proliferation, cell cycle, survival, senescence, and DNA damage repair. These changes lead to the synthesis of biologically modified proteins by promoting an increase of the tumor progression. At the initial stage, the genetic modifications can be germline and the detection of cancer susceptibility genes plays a key role to identify and monitor patients at risk of developing melanoma. For this reason, the prognosis is closely associated with the early diagnosis.
An increasing understanding of melanocyte biology and melanoma pathogenesis is leading to the development of targeted therapies and the potential for major improvements in the care of patients with advanced melanoma. This section provides an overview of the key genes and associated pathways involved in the acquisition of the malignant melanoma phenotype.
Genetic Risk Factors
The melanomas are genetically and phenotypically heterogeneous tumors harboring various genetic alterations, as revealed by recent clinical, epidemiological, and genetic studies. In 2005, Curtin et al. [9] proposed a molecular classification based on the sites where the melanoma occurs, the genetic alterations and the sun exposure history. BRAF, NRAS, and KIT are three well-known oncogenes involved in melanoma pathogenesis. A high frequency of activating BRAF mutations (80 %) was detected in nevi, indicating that these alterations occur early during melanoma progression, leading to the activation of the cell proliferation followed by induction of senescence [10]. Recent evidence showed that the BRAF V600E mutation was found in the majority of melanomas [11]. Targeting of mutated BRAF kinase has recently been shown to significantly improve overall survival of patients with metastatic melanoma, highlighting the important role of this oncogene in melanoma biology [12]. Mutations in BRAF were significantly more common in melanomas located in areas without chronic sun-induced damage. Melanomas arising in chronically sun-damaged skin, mucosal surfaces, and acral skin were characterized by wild-type BRAF and wild-type NRAS, but exhibited alterations in KIT and, frequently, increased copy number of the genes encoding for cyclin-dependent kinase 4 (CDK4) and cyclin D1 (CCND1), downstream components of the RAS–BRAF pathway [9].
The initial mediator of senescence seems to be p16INK4a, which blocks the CCND1/CDK4 complexes and inhibits cell proliferation. Moreover, although KIT mediates the cell cycle activity, its effect seems to be limited to a subset of melanomas. PTEN phosphatase loss activates the PI3K/AKT signaling pathway by overcoming the BRAFV600E-mediated senescence. Therefore, PTEN loss could evade senescence mediated by p16INK4 loss, promoting melanoma progression via the PI3K/AKT cascade. Indeed, the deregulation of PI3K/AKT pathway is considered a late event in melanoma progression [13]. AKT activation was detected in about 60 % of sporadic melanomas thereafter to gene amplification or to inactivation of PTEN, which negatively regulates the PI3K/AKT pathway [14, 15]. The presence of both PTEN and BRAF mutations has been reported in 17 % of melanomas ([16]; Fig. 16.1).
Also, several studies identified less frequent mutations in other genes, such as PREX2 (phosphatidylinositol-3,4,5-trisphosphatedependent Rac exchange factor 2), encoding for a negative regulator of PTEN [17], PPP6C, encoding for a serine/threonine phosphatase, and RAC1, encoding for a GTPase of the RAS superfamily. Noteworthy, melanomas that were mutated for both BRAF and NRAS exhibited more frequent mutations in PPP6C, while melanomas that were wild-type for both BRAF and NRAS showed more frequent mutations in RAC1 [18, 19]. Furthermore, germline mutations in the genes encoding for CDK4 and CDKN2A (cyclin-dependent kinase inhibitor 2A), involved in regulation of the cell cycle, have been shown to confer a high malignant melanoma risk [20, 21]. In addition, the identification of genetic variants with low/intermediate allele frequency conferring a moderate risk of cancer represents an important scientific approach to discover novel melanoma-predisposing genes [22]. Therefore, frequent germline allelic variants in the Casp8, MTAP, MATP, MC1R (melanocortin 1 receptor) and ASIP genes have been identified as low-risk susceptibility genes or as modifiers of high-risk susceptibility genes [23, 24]. Recently, an increase of the risk of developing melanoma was associated with a germline mutation in the MITF (microphthalmia-associated transcription factor) gene, involved in control of melanocyte homeostasis [25–28]. Functional genomic studies showed that MITF regulates the transcription of several genes involved in DNA replication and repair, though the molecular mechanisms have remained to be elucidated yet [29]. These genes are involved in melanoma progression by conferring metastatic genome stabilization during the metastatic process [30]. Recently, in addition to the commonly mutated genes BRAF, NRAS, PTEN, TP53 and p16, new oncogene candidates such as MAPK1/2, ERBB4, GRIN2A, MMP8 and GRM3 were identified [31–33]. Their particular role in melanoma biology is currently under investigation through in vitro and in vivo experiments, but requires further validation in clinical studies. In the future, these new gene candidates could provide more individualized treatment approaches for metastatic melanoma patients [34].
The RAS/RAF/MEK/ERK Signaling Pathway
In recent years, the most important advance has been the discovery that the mitogen activated protein kinase (MAPK) cascade is the pivotal signaling pathway in melanoma progression and development. In fact, the novel therapeutic approaches rely on the inhibition of some members of this cascade. BRAF and MEK molecular pathways appear to be key players in this field. The RAS/RAF/MEK/ERK cascade is activated by various receptors, including c-KIT, FGF receptor, and c-MET. Dysregulation of signaling can occur at various levels, from alterations at the receptor level to changes in the intracellular signaling cascade, resulting in aberrant cell proliferation and/or apoptosis [35]. The RAS family is made up of small G proteins divided into three different isoforms: NRAS, HRAS, and KRAS. The members consist of a catalytic domain that mediates the guanine nucleotide binding and hydrolysis and of an hypervariable region containing the membrane targeting domain required for its activation. Mutations in NRAS, the most common in melanoma, were detected in 33 % of primary and 26 % of metastatic tumors, and are correlated with sun exposure and nodular lesions [36, 37]. The most frequent NRAS mutations are substitutions of glutamine at position 61 by a lysine or an arginine (Q61K, Q61R) [38]. HRAS point mutations have only been found in benign lesions that does not progress to melanoma [39]. No mutations of KRAS have been described in melanoma.
The family of serine/threonine kinases RAF consists of three isoforms, ARAF, BRAF, and CRAF (RAF-1), activated by the small GTPases RAS. Activating mutations in BRAF are present in approximately 40–60 % of advanced melanomas [40, 41]. In 80–90 % of cases, this activating mutation consists of the substitution of glutamic acid for valine at amino acid 600 (V600E mutation) with most of the remainder consisting of an alternate substitution (lysine for valine) at the V600 locus (V–K) that accounts about 16 % of mutations in melanoma [42–44]. The latter and other less common mutations were found at slightly higher rates in melanomas arising in older patients. Advanced melanomas with a mutation in BRAF appear to have some clinical differences that are associated with a more aggressive clinical course. Patients with BRAF mutations are younger and have greater number of nevi. Current results from melanoma cohorts showed that NRAS and BRAF mutations are almost always mutually exclusive [45–47], indicating that the occurrence of each mutation may be specific to certain subtypes of melanoma [46]. The V600E mutation creates a constitutively active status for BRAF, independent of a previous activation by RAS and upstream extracellular stimulus, determining an increased proliferation and promoting a checkpoint for malignant transformation. However, BRAF requires the cooperation of other determinants to drive melanoma progression. BRAF can regulate various aspects of the cell survival. Activated BRAF promotes IκB degradation, while inhibition of BRAF sensitizes cells to apoptosis[48]. BRAF can also control cell growth by regulating p27kip1 levels [49]. Recently, NRAS/BRAF signaling activation was shown to mediate the epithelial-to-mesenchymal transition (EMT) in advanced melanoma [50].
BRAF together with other two isoforms activates via phosphorylation a second protein known as mitogen-activated protein kinase (MEK), which in turn activates downstream extracellular signal-regulated kinase (ERK). The ERK signaling pathway can regulate various molecules important for tumorigenesis, survival, and senescence. Conversely, the inhibition of RAS, BRAF, or MEK blocks ERK activity and inhibits the growth of melanoma cells both in vitro and in vivo [51]. In wild-type BRAF or NRAS cells, ERK activation is low in comparison to mutant cells and can control proteins involved in extracellular adherence, cell motility, and angiogenesis [52]. In melanoma cells, ERK can inhibit the cell cycle regulator p27kip1 and also alter in vitro invasion capability by regulating the production of matrix metalloproteinase-1 (MMP-1) [53, 54].
Current and Emerging Approaches in Melanoma Treatment
After melanoma diagnosis, the next step is to determine the tumor stage, the extent of its spread and its aggressiveness. Staging is important to plan the most appropriate treatment. Surgical excision is the treatment of choice for early localized cutaneous melanoma and is curative in most cases. Therefore, an appropriate excision is important to lessen the risk of a local recurrence. Although patients with localized disease can be treated successfully with surgical resection in the majority of cases, some individuals develop disseminated disease [55]. The recurrence rates remain high for stage III disease, with relapse-free survival rates of 63, 32, and 11 % for stages IIIA, IIIB, and IIIC, respectively. The prognosis for melanoma patients with distant metastases is poor, and the vast majority of those with stage IV melanoma will die from disease [56].The identification of specific oncogenic-driving mutations and the evolving knowledge of the molecular biology of melanoma have led to notable advances in the treatment of metastatic melanoma. It aims to prolong survival, to block the spread of metastases and to prevent the development of new sites of disease. Approaches that can provide clinically important benefits for appropriately chosen subsets of patients with metastatic melanoma can include surgical excision, immunotherapy, targeted inhibition of the MAP kinase pathway, and radiation therapy to sites of metastases, depending upon the localization and the extent of metastases. Although cytotoxic chemotherapy was widely used prior to the development of targeted therapies, it does not have an established role for patients with metastatic melanoma [57]. Instead, the radiation therapy may be used to reduce tumor mass, to prevent recurrence, and to treat those sites of metastases, such as brain, which are difficult to be treated by surgery [58]. There are three main categories of drug treatment: chemotherapy, targeted therapy, and immunotherapy. This section provides an overview of current and emerging treatment options for melanoma patients (Table 16.1).
Chemotherapy
Conventional chemotherapy is based on the use of alkylating agents such as fotemustine, dacarbazine, and temozolomide which trigger cytotoxic effects able to inhibit or slow the cancer cell growth by blocking cell replication. However, these drugs showed objective response rates of approximately 10–15 %, with no improvement of overall survival [59, 60]. Other cytotoxic agents, including taxanes, have been tested in melanoma with response rates similar to that of dacarbazine. Trials of polychemotherapy and combinations with cytokines, in the 1980s and 1990s, yielded better response rates for multi-agent regimens, but no improvement in overall survival. Therefore, cytotoxic chemotherapy generally is not used as the initial treatment for patients with advanced disease [60]. More recent researches have led to the development of immunotherapy, using an anti-CTLA4 monoclonal antibody, and to targeted therapies (BRAF or MEK inhibition), which prolong progression free and overall survival compared with chemotherapy. Thus, these cytotoxic drugs are actually used for patients harboring non-BRAF mutated melanomas or for patients who developed resistance to previous treatments.
New Targeted Therapies in Melanoma
Targeted therapy is a form of treatment in which drugs (or other substances) are developed with the aim of destroying cancer cells by leaving normal cells intact. These drugs are designed to interfere with the specific molecules that drive the growth and spread of the tumor, and are associated with fewer side effects compared to chemotherapy and radiation therapy.
The recent characterization of the molecular alterations in melanoma led to the development of personalized targeted therapies, which have revolutionized the treatment for advanced melanoma. These treatment options are designed to target tumors according to their molecular diversity and activated intracellular signaling pathways [61]. The BRAF/MEK/ERK signaling pathway has attracted considerable attention as a target for anticancer therapy, due to its high frequency of mutations and its important role in melanoma [57]. Furthermore, less frequent activating KIT mutations were detected in a small portion of patients (15–20 %) with acral lentiginous or mucosal melanomas [62, 63] and with melanoma arising in areas of chronic skin damage [64]. For this reason, there are two main classes of agents used in targeted therapies for melanoma: (1) drugs targeting melanoma cells with alterations in the BRAF/MEK signaling pathway (BRAF and MEK inhibitors) and (2) drugs targeting melanoma cells with alterations in the c-KIT gene. Three agents have showed significant clinical benefit and have been approved for use in patients with BRAF mutations: the BRAF inhibitors, vemurafenib and dabrafenib, and the MEK inhibitor trametinib ([65, 66]; Fig. 16.2).
Other pathways have also been investigated in melanoma to identify new potential targets for therapy.
Some researchers argued that the PI3K–AKT–mTOR pathway could be involved in melanoma genesis. Indeed, AKT3 could be deregulated and PTEN decreased in melanomas, as reported above. Pre-clinical studies showed that rapamycin, an mTOR inhibitor, decreases the proliferation of melanoma cells [67]. These molecular alterations seem to play a role in the resistance to BRAF and MEK inhibitors. However, the use of the mTOR inhibitors, temsirolimus and everolimus, in melanoma patients has not shown a significant activity [68, 69]. These controversial results from pre-clinical and clinical studies may be attributed to a hyper-activation of AKT as a compensatory mechanism.
Tumor angiogenesis has also been involved in melanoma proliferation and progression. Bevacizumab, the anti-VEGF monoclonal antibody, was studied both alone and in combination with chemotherapy or interferon-alpha-2b. Even though some responses were observed, it has not been demonstrated yet whether VEGF-targeted therapy plays a role in improving clinical outcomes [70–74].
BRAF Inhibitors
About half of all melanomas harbor activating mutations in the BRAF gene. As mentioned before, the two most commonly observed BRAF mutations are V600E and V600K, which account for 95 % of these mutations. These changes produce an altered BRAF protein that drives melanoma cells to grow and divide quickly [43]. The presence of a V600 mutation predicts responsiveness to BRAF and MEK inhibitors as they are not likely to act in melanomas harboring the wild-type BRAF gene [75].
The first agent developed to target oncogenic BRAF in melanomas was sorafenib (BAY 43-9006), a multikinase inhibitor that inhibits BRAF (wild-type or V600E), but also PDGFR, VEGFR, and c-KIT [76, 77]. As a monotherapy, sorafenib showed limited clinical activity and proved to be inefficient in the treatment of unresectable or metastatic melanoma. This lack of activity is likely explained by lack of specificity for BRAF [78].
During the last decade, many BRAF inhibitors have been discovered and most of them exhibited potent antitumor activity, especially on tumors that harbor V600E mutations, with little cross-reactivity for wild-type BRAF and CRAF [79]. Some of these compounds have been entered clinical trials and displayed encouraging results. The best validated drugs that appear to have the highest affinity for the catalytic domain of the BRAF kinase, exhibiting unprecedented survival benefits in advanced melanoma, are vemurafenib and dabrafenib. Clinical trials have demonstrated that the first potent and effective drug targeting mutated BRAF in melanoma was vemurafenib [80, 81]. Vemurafenib is a potent inhibitor that selectively binds to mutant BRAF proteins containing V600E amino acid substitutions, preventing constitutive activation of the MAPK pathway, and resulting in antitumor effects of cell proliferation inhibition and apoptosis induction [82, 83]. This drug was approved by the US Food and Drug Administration (FDA) in 2011 for the treatment of BRAFV600E mutant melanomas that cannot be removed by surgery and only for those patients who have tested positive for the BRAF mutation [84]. In phase 1 and 2 clinical trials, vemurafenib showed an objective response rate > 50 % in patients suffering from melanoma. These results were confirmed in a phase 3 clinical trial, which compared vemurafenib to dacarbazine. It showed an improvement of both response rate (RR) and survival outcomes, progression-free survival (PFS) and overall survival (OS) [85]. Based on these results, vemurafenib was approved by FDA in 2011 in those patients with BRAF V600E mutation. The most common side effects are joint pain, fatigue, hair loss, rash, itching, sensitivity to the sun, and nausea. Less common but serious side effects can occur, such as heart rhythm problems, liver function test impairment, severe allergic reactions, and severe skin or eye side effects [86]. Some people may develop new skin cancers called squamous cell carcinomas. These cancers are usually less serious than melanoma and they can be definitively treated by surgery [87].
Despite these excellent results, a subset of BRAFV600E-mutant patients was found initially resistant to vemurafenib (intrinsic resistance) and most of the others developed secondary resistance. Almost all tumors showed reactivation of the MAP kinase pathway or upregulation of parallel signaling pathways with increased ERK phosphorylation at the time of resistance and restored cell survival [88]. The MAPK pathway may also be activated when BRAFV600E splice variants lacking the RAS-binding domain develop. These variants dimerize in the absence of RAS activation by reactivating the pathway [89]. Both PTEN and cyclin D1 are involved in mechanisms of intrinsic resistance. Patients whose tumors exhibit both BRAF mutations and PTEN dysfunction showed a lower response rate than dabrafenib. In addition, cell lines with both cyclin D1 amplification as well as BRAF mutation do not undergo apoptosis when exposed to BRAF inhibitors [90, 91]. Different mechanisms involved in acquired and secondary resistance have been reported [92]. Multiple genetic changes may contribute to this event, and research is currently ongoing to further clarify patterns of resistance to improve the clinical outcome of the patients [93]. Insights into mechanisms of resistance aim to potential drug combinations to overcome this important clinical problem, by promoting the concept of dual inhibition of the MAPK pathway. In this perspective, other BRAF inhibitor agents are developing [94].
Dabrafenib is another new generation BRAF inhibitor showing significant activity in patients with advanced melanoma compared with dacarbazine chemotherapy both in terms of RR and PFS. The difference in OS was not statistically significant. Dabrafenib was approved by the FDA in 2013 for the treatment of patients with advanced melanoma containing the BRAFV600E mutation. This drug is not indicated for the treatment of patients harboring wild-type BRAF, but only for those patients who have tested positive for the BRAF mutation [93]. Dabrafenib belongs to the same class of vemurafenib, working with a similar efficiency, but it seems to be more efficient in melanomas with brain metastasis [95, 96]. Like vemurafenib, dabrafenib decreases phosphorylated ERK and causes cell cycle arrest. In pre-clinical studies, dabrafenib has demonstrated to be almost 20 times more selective at inhibiting BRAF V600E -mutants than wild-type BRAF in several cancer cell lines. In addition, dabrafenib shows inhibitory effects in cell lines containing other activating BRAF mutations, including V600K and V600D [97].
Since dabrafenib and vemurafenib appear to have similar clinical activity, the choice between two agents likely relies on other factors including their toxicity profiles. Common side effects include thickening of the skin (hyperkeratosis), headache, fever, joint pain, non-cancerous skin tumors, hair loss, and hand-foot syndrome (redness, pain, and irritation of the hands and feet). Although it also can cause squamous cell carcinomas of the skin, these may occur less often than with vemurafenib. Some other more serious side effects that can occur with dabrafenib include severe fevers, dehydration, kidney failure, eye problems, and increased blood glycemic levels. However, unlike the vemurafenib, dabrafenibdoes not induce photosensitivity [87].
MEK Inhibitors
As mentioned before, downstream of RAF in the MAPK cascade, there are the MEK and ERK kinases. Since RAF moves from the cytoplasm to the cell membrane during cellular signaling, the new activated complex triggers the signal cascade via consecutive phosphorylations through MEK1 and MEK2. This, in turn, activates ERK 1 and 2 which are able to enter the nucleus and interact with several transcription factors to promote cellular growth and differentiation [98]. Multiple in vitro studies demonstrated that mutated BRAF signaling is mediated via MEK and ERK [99]. Therefore, inhibition of MEK is another option for targeting the MAPK pathway and several studies are currently evaluating the role of MEK inhibitors in patients with BRAF-mutant metastatic melanoma [100]. MEK inhibition is associated with improved response rate, progression-free survival, and overall survival in patients with BRAF-mutated metastatic melanoma.
Pre-clinical studies of the MEK inhibitor, PD0325901, and its precursor, CI-1040, showed direct inhibition of ERK in cell lines and reduced tumor growth in animal models, but they were not brought forward due to their toxicity in early phase trials [101, 102].
Selumetinib was the first allosteric selective MEK inhibitor to be evaluated in a phase II clinical trial in patients with metastatic melanoma. This agent determined a 12 % objective response rate in patients with BRAF mutant tumors, whereas no response was observed in wild-type tumors, enhancing the importance of selecting a specific patient population [103].
Trametinib and MEK162 are potent, highly specific inhibitors of MEK1/MEK2 that provide responses in 20 % of the melanomas harboring a BRAF mutation [104, 105]. MEK162 showed activity in patients with advanced melanoma and a NRAS mutation. MEK inhibition showed efficacy in NRAS-mutated patients, for whom there is no specific targeted therapy [104].
Trametinib was recently approved by the FDA for the treatment of patients with unresectable or metastatic melanoma harboring BRAF V600E or V600K mutations, because in the phase III METRIC trial it achieved a significant improvement of RR, PFS, and OS when compared to dacarbazine or paclitaxel. It is not indicated for the treatment of patients who have received previously a BRAF inhibitor therapy [106]. Common side effects include rash, diarrhea, and swelling. Rare but serious side effects can include heart damage, loss of vision, lung side effects, and skin infections. Combination therapy with a BRAF inhibitor may improve the efficacy and reduce BRAF inhibition-associated side effects, including skin toxicity [107]. There are no clinical trials comparing vemurafenib, dabrafenib, and trametinib with each other, however, data suggest that the BRAF inhibitors, vemurafenib and dabrafenib, are more active than the MEK inhibitor trametinib. The combination of dabrafenib and trametinib appears to have a superior response rate and progression free survival than dabrafenib alone with less skin toxicity, however, comparison of the efficacy of the combination with dabrafenib alone awaits the completion of ongoing phase III trials [108]. Moreover, there are no randomized trials that compare targeted therapy with immunotherapy.
c-KIT Inhibitors
A small portion of melanomas exhibit activating c-KIT mutations that help them develop and grow. These changes are more common in melanomas that arise in certain parts of the body (acral or mucosal melanomas). Some drugs used for the treatment of other cancers, such as imatinib mesylate and nilotinib, are known to target cells with changes in c-KIT. The KIT receptor tyrosine kinase is a transmembrane protein consisting of extracellular and intracellular domains. Most KIT mutations are located in exon 11, which encodes for the juxtamembrane domain, and in exon 13, which encodes for a kinase domain [64]. In the subgroups of patients with melanoma on chronic sun damaged skin, acral lentiginous or mucosal melanoma the incidence of KIT mutations or amplification is up to 25 % [109]. It has been demonstrated in vitro that imatinib mesylate inhibits proliferation and induces apoptosis in melanoma cells with hyperactivation of c-KIT. These biological effects go through the increase of p27KIP and inhibition of the ERK, PI3K/AKT, and STAT signaling pathways [110]. For patients without a BRAF V600 mutation but with a KIT mutation, the use of a KIT inhibitor may provide an important treatment option. Phase II studies using imatinib in unselected groups of patients with advanced melanoma showed no clinical efficacy [111, 112]. However, phase II clinical trials performed on patients with c-KIT mutations showed objective response rates in 33 % of cases [113]. Furthermore, results from a phase II trial showed that imatinib could be effective when tumors harbor KIT mutations, but not if KIT only is amplified [114].
Immunotherapy
Several evidences reported that melanoma is an immunogenic tumor but metastatic melanoma cells have developed mechanisms to escape from immunosurveillance and to survive. Immunological strategies based on the use of drugs with effects on immune system to stop or slow the growth of cancer cells could improve the prognosis of metastatic melanoma [115]. The approaches that have allowed to provide clinically important benefit for patients with disseminated melanoma in appropriately selected patients include immunotherapy with high-dose interleukin-2 (IL-2), immunotherapy with ipilimumab, a monoclonal antibody targeting cytotoxic T-lymphocyte antigen-4 (CTLA-4), and immunotherapy with monoclonal anti-PD-1 antibody.
In 1998, the FDA approved the use of the immune molecule IL-2 as a treatment option for advanced melanoma. IL-2 was first identified as a T cell growth factor in 1976. Subsequently, recombinant IL-2 was shown to have potent, dose-dependent immunomodulatory and antitumor activity in a number of murine tumor models [116]. These observations led to the development of high-dose IL-2 regimens for clinical use. IL-2 is a form of immunotherapy that has allowed to help some people with metastatic melanoma when administered in high doses, leading to complete disappearance of the disease or tumor growth arrest for a prolonged period. However, high dose IL-2 can cause serious side effects, including low blood pressure, irregular heart rhythms, accumulation of fluid in the lungs, fever, and rarely death. For this reason, treatment with high dose IL-2 is generally reserved for younger patients who have good heart and lung function [117].
Conversely, the immune molecule interferon alpha (IFN-α) was used only after surgery as a adjuvant immunotherapy, or in combination with other agents used for treatment of advanced melanoma. However, most of clinical trials based on this immune system activation did not translate into clinically significant objective response rates and any improvement in overall survival [118]. This led to the targeting of T-cell signaling pathways, initially CTLA-4 and more recently programmed death 1 (PD-1) and its ligand PD-L1 (Fig. 16.3).
Immunotherapy Targeting CTLA-4
CTLA-4 is expressed on the surface of activated CD4 + and CD8 + T-cells and binds B7 molecules on antigen-presenting cells (APC), repressing T-cell activation. After T-cell activation, CTLA-4 is recruited to the plasma membrane where it plays an autoregulatory role, attenuating T-cell activation and proliferation, thereby maintaining effective antitumor immunity [119].
Ipilimumab, a novel antibody blocking CTLA-4, is a fully human immunoglobulin that inhibits this negative feedback, potentiating the T-cell-mediated immune response. No drug or combination of drugs showed an impact on overall survival until 2011, when ipilimumab was approved for clinical use by the FDA following the publication of results of a pivotal phase III trial [120]. Major weaknesses of this treatment were the low rate of objective response (10 %), a small percentage of patients achieving long-term disease control, and the serious side effects. It was first compared to the gp100 peptide vaccine with an improvement of OS by 3.6 months. Then it was added to dacarbazine and this combination was compared to dacarbazine alone with a subsequent improvement of OS by 2.1 months. These findings suggest that ipilimumab exerts its function against melanoma regardless a peptide-mediated vaccination. However, the effects of ipilimumab on OS seem to not only be mediated by tumor responses, but also perhaps by prolonged stable diseases, regression after an initial progression and regression of target lesions in the presence of new lesions. Ipilimumab toxicity differs from that of other antibody-based therapies [121]. These are mainly immune-related adverse effects. The most common of them include effects in the gastrointestinal tract, skin and liver. The initial observation of toxic deaths was not reported in the most recent phase III trial with dacarbazine, since the toxicity management protocols were standardized for this drug [122, 123]. Tremelimumab, the other anti-CTLA-4 antibody in clinical development, did not show a statistically significant survival rate in its pivotal trials, although this result may have been affected by the availability of ipilimumab in the United States at the time of that trial [124].
Immunotherapy Targeting PD-1 and PD-L1
The programmed death 1 (PD-1) receptor, expressed at the surface of activated T cells, is a negative regulator of T cells [125]. It was first isolated in 1992 by Ishida and Honjo and initially cloned as a molecule overexpressed in apoptotic cells [126]. Its role as a negative regulator of the immune response was demonstrated and studied in PD-1−/− knockout mice that showed a variety of autoimmune diseases [127]. Unlike CTLA-4, PD-1 receptor ligand (PD-L1) is directly expressed on tumor cells. When PD-L1 binds to its receptor, the T cell ability to target the tumor cell is inhibited. The difference between the CTLA-4/B7 and PD-1/PD-L1 interactions is linked to the phase of T-cell response: the priming phase for the first one and the effector phase for the latter. According to this difference, it was argued that PD-1 blockade could prevent tissue damage. Anti-PD-1 and anti-PD-L1 antibodies directly activate cancer-specific T cells [128]. Nivolumab (also known as BMS-936558) is a fully human anti-PD-1 antibody being explored in lung, melanoma, and renal cancers, demonstrating an approximately 30 % objective response rate in melanoma. Interestingly, tumor PD-L1 expression might provide a basis for selecting patients for the treatment, as none of patients with tumors negative for PD-L1 showed a response. Interstitial pneumonitis is the most serious immune complication of this agent, with deaths resulting from this complication. Immune toxicities were seen with these agents but at a lesser rate and reduced severity compared to other immunomodulating molecules such as ipilimumab [129].
The anti-PD-L1 antibody MDX-1105 (also known as BMS-936559) exhibited objective responses (17 %) in melanoma. Thus far, both the response and toxicity rates were lower than those reported with anti-PD-1 antibodies [130]. Recently, monoclonal anti-PD-1 antibody lambrolizumab (MK-3475) was evaluated in metastatic or unresectable melanomas. Objective response rate was obtained in 38 % of patients and the responses were durable in the majority of patients [131].
Conclusions
Recent advances in the molecular biology field have allowed for the development of treatments able to improve, for the first time, the overall disease-free survival of metastatic melanoma patients. Advances in the use of immunotherapy and targeted therapy have been shown to potentially improve survival and have become the preferred approaches for most patients with metastatic melanoma. However, clinical responses are still either too transient or limited to restricted patient subsets. The complete cure of metastatic melanoma therefore remains a challenge in the clinic. For instance, new molecular targets need to be identified to help the subset of patients who do not harbor BRAF mutations and overcome the limitations of the current therapeutic agents. Moreover, combinations of targeted therapies are required and are being studied to prevent or delay the resistance mechanisms.
In the last few years, the treatment strategy for patients with metastatic malignant melanoma has been changed by the results of clinical trials on BRAF inhibitors and immunomodulators. Therefore, actually oncologists can treat a half of melanoma patients with BRAF inhibitors instead of chemotherapy as they harbor a BRAF activating mutation. For the other ones who are BRAF wild-type, ipilimumab represents the best option, so that the use of chemotherapy is limited to those patients refractory to targeted therapy.
References
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29.
Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998;83(8):1664–78.
Tas F, Keskin S, Karadeniz A, Dagoglu N, Sen F, Kilic L, Yildiz I. Noncutaneous melanoma have distinct features from each other and cutaneous melanoma. Oncology. 2011;81(5–6):353–8.
Greenberg E, Nemlich Y, Markel G. MicroRNAs in cancer: lessons from Melanoma. Curr Pharm Des. 2014;20(33):5246–59.
Oba-Shinjo SM, Correa M, Ricca TI, Molognoni F, Pinhal MA, Neves IA, Marie SK, Sampaio LO, Nader HB, Chammas R, et al. Melanocyte transformation associated with substrate adhesion impediment. Neoplasia. 2006;8(3):231–41.
Jhappan C, Noonan FP, Merlino G. Ultraviolet radiation and cutaneous malignant melanoma. Oncogene. 2003;22(20):3099–12.
Bhatia S, Emdad L, Das SK, Hamed H, Dent P, Sarkar D, Fisher PB. Non-BRAF targeted therapies for melanoma: protein kinase inhibitors in Phase II clinical trials. Expert Opin Investig Drugs. 2014;23(4):489–500.
Caramuta S, Egyhazi S, Rodolfo M, Witten D, Hansson J, Larsson C, Lui WO. MicroRNA expression profiles associated with mutational status and survival in malignant melanoma. J Invest Dermatol. 2010;130(8):2062–70.
Curtin JA, Fridlyand J, Kageshita T, Patel HN, Busam KJ, Kutzner H, Cho KH, Aiba S, Brocker EB, LeBoit PE, et al. Distinct sets of genetic alterations in melanoma. N Engl J Med. 2005;353(20):2135–47.
Pollock PM, Harper UL, Hansen KS, Yudt LM, Stark M, Robbins CM, Moses TY, Hostetter G, Wagner U, Kakareka J, et al. High frequency of BRAF mutations in nevi. Nat Genet. 2003;33(1):19–20.
Yeh I, von Deimling A, Bastian BC. Clonal BRAF mutations in melanocytic nevi and initiating role of BRAF in melanocytic neoplasia. J Natl Cancer Inst. 2013;105(12):917–9.
Kunz M. Oncogenes in melanoma: an update. Eur J Cell Biol. 2014;93(1–2):1–10.
Chudnovsky Y, Adams AE, Robbins PB, Lin Q, Khavari PA. Use of human tissue to assess the oncogenic activity of melanoma-associated mutations. Nat Genet. 2005;37(7):745–9
Stahl JM, Sharma A, Cheung M, Zimmerman M, Cheng JQ, Bosenberg MW, Kester M, Sandirasegarane L, Robertson GP. Deregulated Akt3 activity promotes development of malignant melanoma. Cancer Res. 2004;64(19):7002–10.
Stahl JM, Cheung M, Sharma A, Trivedi NR, Shanmugam S, Robertson GP. Loss of PTEN promotes tumor development in malignant melanoma. Cancer Res. 2003;63(11):2881–90.
Shull AY, Latham-Schwark A, Ramasamy P, Leskoske K, Oroian D, Birtwistle MR, Buckhaults PJ. Novel somatic mutations to PI3K pathway genes in metastatic melanoma. PLoS One. 2012;7(8):e43369.
Berger MF, Hodis E, Heffernan TP, Deribe YL, Lawrence MS, Protopopov A, Ivanova E, Watson IR, Nickerson E, Ghosh P, et al. Melanoma genome sequencing reveals frequent PREX2 mutations. Nature. 2012;485(7399):502–6.
Hodis E, Watson IR, Kryukov GV, Arold ST, Imielinski M, Theurillat JP, Nickerson E, Auclair D, Li L, Place C, et al. A landscape of driver mutations in melanoma. Cell. 2012;150(2):251–63.
Krauthammer M, Kong Y, Ha BH, Evans P, Bacchiocchi A, McCusker JP, Cheng E, Davis MJ, Goh G, Choi M, et al. Exome sequencing identifies recurrent somatic RAC1 mutations in melanoma. Nat Genet. 2012;44(9):1006–14.
Zuo L, Weger J, Yang Q, Goldstein AM, Tucker MA, Walker GJ, Hayward N, Dracopoli NC. Germline mutations in the p16INK4a binding domain of CDK4 in familial melanoma. Nat Genet. 1996;12(1):97–9.
Hussussian CJ, Struewing JP, Goldstein AM, Higgins PA, Ally DS, Sheahan MD, Clark WH Jr, Tucker MA, Dracopoli NC. Germline p16 mutations in familial melanoma. Nat Genet. 1994;8(1):15–21.
Fanale D, Amodeo V, Corsini LR, Rizzo S, Bazan V, Russo A. Breast cancer genome-wide association studies: there is strength in numbers. Oncogene. 2012;31(17):2121–8.
Bressac-de-Paillerets B, Avril MF, Chompret A, Demenais F. Genetic and environmental factors in cutaneous malignant melanoma. Biochimie. 2002;84(1):67–74.
Fargnoli MC, Gandini S, Peris K, Maisonneuve P, Raimondi S. MC1R variants increase melanoma risk in families with CDKN2A mutations: a meta-analysis. Eur J Cancer. 2010;46(8):1413–20.
Yokoyama S, Woods SL, Boyle GM, Aoude LG, MacGregor S, Zismann V, Gartside M, Cust AE, Haq R, Harland M, et al. A novel recurrent mutation in MITF predisposes to familial and sporadic melanoma. Nature. 2011;480(7375):99–103.
Bertolotto C, Lesueur F, Giuliano S, Strub T, de Lichy M, Bille K, Dessen P, d’Hayer B, Mohamdi H, Remenieras A, et al. A SUMOylation-defective MITF germline mutation predisposes to melanoma and renal carcinoma. Nature. 2011;480(7375):94–8.
Sturm RA, Fox C, McClenahan P, Jagirdar K, Ibarrola-Villava M, Banan P, Abbott NC, Ribas G, Gabrielli B, Duffy DL, et al. Phenotypic characterization of nevus and tumor patterns in MITF E318K mutation carrier melanoma patients. J Invest Dermatol. 2014;134(1):141–9.
Ghiorzo P, Pastorino L, Queirolo P, Bruno W, Tibiletti MG, Nasti S, Andreotti V, Paillerets BB, Bianchi Scarra G. Prevalence of the E318K MITF germline mutation in Italian melanoma patients: associations with histological subtypes and family cancer history. Pigment Cell Melanoma Res. 2013;26(2):259–62.
Strub T, Giuliano S, Ye T, Bonet C, Keime C, Kobi D, Le Gras S, Cormont M, Ballotti R, Bertolotto C, et al. Essential role of microphthalmia transcription factor for DNA replication, mitosis and genomic stability in melanoma. Oncogene. 2011;30(20):2319–32.
Kauffmann A, Rosselli F, Lazar V, Winnepenninckx V, Mansuet-Lupo A, Dessen P, van den Oord JJ, Spatz A, Sarasin A. High expression of DNA repair pathways is associated with metastasis in melanoma patients. Oncogene. 2008;27(5):565–73.
Wei X, Walia V, Lin JC, Teer JK, Prickett TD, Gartner J, Davis S, Stemke-Hale K, Davies MA, Gershenwald JE, et al. Exome sequencing identifies GRIN2A as frequently mutated in melanoma. Nat Genet. 2011;43(5):442–6.
Prickett TD, Agrawal NS, Wei X, Yates KE, Lin JC, Wunderlich JR, Cronin JC, Cruz P, Rosenberg SA, Samuels Y. Analysis of the tyrosine kinome in melanoma reveals recurrent mutations in ERBB4. Nat Genet. 2009;41(10):1127–32.
Palavalli LH, Prickett TD, Wunderlich JR, Wei X, Burrell AS, Porter-Gill P, Davis S, Wang C, Cronin JC, Agrawal NS, et al. Analysis of the matrix metalloproteinase family reveals that MMP8 is often mutated in melanoma. Nat Genet. 2009;41(5):518–20.
Bertolotto C. Melanoma: from melanocyte to genetic alterations and clinical options. Scientifica (Cairo). 2013;2013:635203.
Ghosh P, Chin L. Genetics and genomics of melanoma. Expert Rev Dermatol. 2009;4(2):131.
Jafari M, Papp T, Kirchner S, Diener U, Henschler D, Burg G, Schiffmann D. Analysis of ras mutations in human melanocytic lesions: activation of the ras gene seems to be associated with the nodular type of human malignant melanoma. J Cancer Res Clin Oncol. 1995;121(1):23–30
van Elsas A, Zerp SF, van der Flier S, Kruse KM, Aarnoudse C, Hayward NK, Ruiter DJ, Schrier PI. Relevance of ultraviolet-induced N-ras oncogene point mutations in development of primary human cutaneous melanoma. Am J Pathol. 1996;149(3):883–93.
Ellerhorst JA, Greene VR, Ekmekcioglu S, Warneke CL, Johnson MM, Cooke CP, Wang LE, Prieto VG, Gershenwald JE, Wei Q, et al. Clinical correlates of NRAS and BRAF mutations in primary human melanoma. Clin Cancer Res. 2011;17(2):229–35.
Bastian BC, LeBoit PE, Pinkel D. Mutations and copy number increase of HRAS in Spitz nevi with distinctive histopathological features. Am J Pathol. 2000;157(3):967–72.
Wellbrock C, Hurlstone A. BRAF as therapeutic target in melanoma. Biochem Pharmacol. 2010;80(5):561–7.
Long GV, Menzies AM, Nagrial AM, Haydu LE, Hamilton AL, Mann GJ, Hughes TM, Thompson JF, Scolyer RA, Kefford RF. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29(10):1239–46.
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–54.
Madureira P, de Mello RA. BRAF and MEK gene rearrangements in melanoma: implications for targeted therapy. Mol Diagn Ther. 2014;18(3):285–91.
Thomas NE. BRAF somatic mutations in malignant melanoma and melanocytic naevi. Melanoma Res. 2006;16(2):97–103.
Omholt K, Platz A, Kanter L, Ringborg U, Hansson J. NRAS and BRAF mutations arise early during melanoma pathogenesis and are preserved throughout tumor progression. Clin Cancer Res. 2003;9(17):6483–8.
Edlundh-Rose E, Egyhazi S, Omholt K, Mansson-Brahme E, Platz A, Hansson J, Lundeberg J. NRAS and BRAF mutations in melanoma tumours in relation to clinical characteristics: a study based on mutation screening by pyrosequencing. Melanoma Res. 2006;16(6):471–8.
Platz A, Egyhazi S, Ringborg U, Hansson J. Human cutaneous melanoma; a review of NRAS and BRAF mutation frequencies in relation to histogenetic subclass and body site. Mol Oncol. 2008;1(4):395–405.
Liu J, Suresh Kumar KG, Yu D, Molton SA, McMahon M, Herlyn M, Thomas-Tikhonenko A, Fuchs SY. Oncogenic BRAF regulates beta-Trcp expression and NF-kappaB activity in human melanoma cells. Oncogene. 2007;26(13):1954–8.
Bhatt KV, Hu R, Spofford LS, Aplin AE. Mutant B-RAF signaling and cyclin D1 regulate Cks1/S-phase kinase-associated protein 2-mediated degradation of p27Kip1 in human melanoma cells. Oncogene. 2007;26(7):1056–66.
Caramel J, Papadogeorgakis E, Hill L, Browne GJ, Richard G, Wierinckx A, Saldanha G, Osborne J, Hutchinson P, Tse G, et al. A switch in the expression of embryonic EMT-inducers drives the development of malignant melanoma. Cancer Cell. 2013;24(4):466–80.
Sharma A, Tran MA, Liang S, Sharma AK, Amin S, Smith CD, Dong C, Robertson GP. Targeting mitogen-activated protein kinase/extracellular signal-regulated kinase kinase in the mutant (V600E) B-Raf signaling cascade effectively inhibits melanoma lung metastases. Cancer Res. 2006;66(16):8200–9.
Shields JM, Thomas NE, Cregger M, Berger AJ, Leslie M, Torrice C, Hao H, Penland S, Arbiser J, Scott G, et al. Lack of extracellular signal-regulated kinase mitogen-activated protein kinase signaling shows a new type of melanoma. Cancer Res. 2007;67(4):1502–12.
Kortylewski M, Heinrich PC, Kauffmann ME, Bohm M, MacKiewicz A, Behrmann I. Mitogen-activated protein kinases control p27/Kip1 expression and growth of human melanoma cells. Biochem J. 2001;357(Pt 1):297–303.
Huntington JT, Shields JM, Der CJ, Wyatt CA, Benbow U, Slingluff CL Jr, Brinckerhoff CE. Overexpression of collagenase 1 (MMP-1) is mediated by the ERK pathway in invasive melanoma cells: role of BRAF mutation and fibroblast growth factor signaling. J Biol Chem. 2004;279(32):33168–76.
Cole BF, Gelber RD, Kirkwood JM, Goldhirsch A, Barylak E, Borden E. Quality-of-life-adjusted survival analysis of interferon alfa-2b adjuvant treatment of high-risk resected cutaneous melanoma: an Eastern Cooperative Oncology Group Study. J Clin Oncol. 1996;14(10):2666–73.
Romano E, Scordo M, Dusza SW, Coit DG, Chapman PB. Site and timing of first relapse in stage III melanoma patients: implications for follow-up guidelines. J Clin Oncol. 2010;28(18):3042–7.
Rughani MG, Gupta A, Middleton MR. New treatment approaches in melanoma: current research and clinical prospects. Ther Adv Med Oncol. 2013;5(1):73–80.
Rao NG, Yu HH, Trotti A III, Sondak VK. The role of radiation therapy in the management of cutaneous melanoma. Surg Oncol Clin N Am. 2011;20(1):115–31.
Middleton MR, Grob JJ, Aaronson N, Fierlbeck G, Tilgen W, Seiter S, Gore M, Aamdal S, Cebon J, Coates A, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic malignant melanoma. J Clin Oncol. 2000;18(1):158–66.
Tsao H, Atkins MB, Sober AJ. Management of cutaneous melanoma. N Engl J Med. 2004;351(10):998–1012.
Griewank KG, Scolyer RA, Thompson JF, Flaherty KT, Schadendorf D, Murali R. Genetic alterations and personalized medicine in melanoma: progress and future prospects. J Natl Cancer Inst. 2014;106(2):djt435.
Omholt K, Grafstrom E, Kanter-Lewensohn L, Hansson J, Ragnarsson-Olding BK. KIT pathway alterations in mucosal melanomas of the vulva and other sites. Clin Cancer Res. 2011;17(12):3933–42.
Schoenewolf NL, Bull C, Belloni B, Holzmann D, Tonolla S, Lang R, Mihic-Probst D, Andres C, Dummer R. Sinonasal, genital and acrolentiginous melanomas show distinct characteristics of KIT expression and mutations. Eur J Cancer. 2012;48(12):1842–52.
Curtin JA, Busam K, Pinkel D, Bastian BC. Somatic activation of KIT in distinct subtypes of melanoma. J Clin Oncol. 2006;24(26):4340–46.
Kudchadkar RR, Smalley KS, Glass LF, Trimble JS, Sondak VK. Targeted therapy in melanoma. Clin Dermatol. 2013;31(2):200–8.
Ahn A, Eccles MR. Targeted therapy; from advanced melanoma to the adjuvant setting. Front Oncol. 2013;3:205.
Busca R, Bertolotto C, Ortonne JP, Ballotti R. Inhibition of the phosphatidylinositol 3-kinase/p70(S6)-kinase pathway induces B16 melanoma cell differentiation. J Biol Chem. 1996;271(50):31824–30.
Dronca RS, Allred JB, Perez DG, Nevala WK, Lieser EA, Thompson M, Maples WJ, Creagan ET, Pockaj BA, Kaur JS, et al. Phase II study of temozolomide (TMZ) and everolimus (RAD001) therapy for metastatic melanoma: a North Central Cancer Treatment Group Study, N0675. Am J Clin Oncol. 2013;37(4):369–76.
Margolin K, Longmate J, Baratta T, Synold T, Christensen S, Weber J, Gajewski T, Quirt I, Doroshow JH. CCI-779 in metastatic melanoma: a phase II trial of the California Cancer Consortium. Cancer. 2005;104(5):1045–8.
Grignol VP, Olencki T, Relekar K, Taylor C, Kibler A, Kefauver C, Wei L, Walker MJ, Chen HX, Kendra K, et al. A phase 2 trial of bevacizumab and high-dose interferon alpha 2B in metastatic melanoma. J Immunother. 2011;34(6):509–15.
von Moos R, Seifert B, Simcock M, Goldinger SM, , Gillessen S, Ochsenbein A, Michielin O, Cathomas R, Schlappi M, Moch H, et al. First-line temozolomide combined with bevacizumab in metastatic melanoma: a multicentre phase II trial (SAKK 50/07). Ann Oncol. 2012;23(2):531–6.
Perez DG, Suman VJ, Fitch TR, Amatruda T III, Morton RF, Jilani SZ, Constantinou CL, Egner JR, Kottschade LA, Markovic SN. Phase 2 trial of carboplatin, weekly paclitaxel, and biweekly bevacizumab in patients with unresectable stage IV melanoma: a North Central Cancer Treatment Group study, N047A. Cancer. 2009;115(1):119–27.
Kim KB, Sosman JA, Fruehauf JP, Linette GP, Markovic SN, McDermott DF, Weber JS, Nguyen H, Cheverton P, Chen D, et al. BEAM: a randomized phase II study evaluating the activity of bevacizumab in combination with carboplatin plus paclitaxel in patients with previously untreated advanced melanoma. J Clin Oncol. 2012;30(1):34–41.
Kottschade LA, Suman VJ, Perez DG, McWilliams RR, Kaur JS, Amatruda TT III, Geoffroy FJ, Gross HM, Cohen PA, Jaslowski AJ, et al. A randomized phase 2 study of temozolomide and bevacizumab or nab-paclitaxel, carboplatin, and bevacizumab in patients with unresectable stage IV melanoma: a North Central Cancer Treatment Group study, N0775. Cancer. 2013;119(3):586–92.
El-Nassan HB. Recent progress in the identification of BRAF inhibitors as anti-cancer agents. Eur J Med Chem. 2014;72:170–205.
Flaherty KT, Lathia C, Frye RF, Schuchter L, Redlinger M, Rosen M, O’Dwyer PJ. Interaction of sorafenib and cytochrome P450 isoenzymes in patients with advanced melanoma: a phase I/II pharmacokinetic interaction study. Cancer Chemother Pharmacol. 2011;68(5):1111–8.
Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64(19):7099–109.
Wilhelm S, Carter C, Lynch M, Lowinger T, Dumas J, Smith RA, Schwartz B, Simantov R, Kelley S. Discovery and development of sorafenib: a multikinase inhibitor for treating cancer. Nat Rev Drug Discov. 2006;5(10):835–44.
Bollag G, Hirth P, Tsai J, Zhang J, Ibrahim PN, Cho H, Spevak W, Zhang C, Zhang Y, Habets G, et al. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature. 2010;467(7315):596–9.
Flaherty KT, Puzanov I, Kim KB, Ribas A, McArthur GA, Sosman JA, O'Dwyer PJ, Lee RJ, Grippo JF, Nolop K, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010;363(9):809–19.
Dummer R, Goldinger SM, Turtschi CP, Eggmann NB, Michielin O, Mitchell L, Veronese L, Hilfiker PR, Felderer L, Rinderknecht JD. Vemurafenib in patients with BRAF(V600) mutation-positive melanoma with symptomatic brain metastases: final results of an open-label pilot study. Eur J Cancer. 2014;50(3):611–21.
Chapman PB, Hauschild A, Robert C, Haanen JB, Ascierto P, Larkin J, Dummer R, Garbe C, Testori A, Maio M, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507–16.
Yang H, Higgins B, Kolinsky K, Packman K, Go Z, Iyer R, Kolis S, Zhao S, Lee R, Grippo JF, et al. RG7204 (PLX4032), a selective BRAFV600E inhibitor, displays potent antitumor activity in preclinical melanoma models. Cancer Res. 2010;70(13):5518–27.
Sosman JA, Kim KB, Schuchter L, Gonzalez R, Pavlick AC, Weber JS, McArthur GA, Hutson TE, Moschos SJ, Flaherty KT, et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med. 2012;366(8):707–14.
Young K, Minchom A, Larkin J. BRIM-1, -2 and -3 trials: improved survival with vemurafenib in metastatic melanoma patients with a BRAF(V600E) mutation. Future Oncol. 2012;8(5):499–507
Boyd KP, Vincent B, Andea A, Conry RM, Hughey LC. Nonmalignant cutaneous findings associated with vemurafenib use in patients with metastatic melanoma. J Am Acad Dermatol. 2012;67(6):1375–9.
Anforth R, Fernandez-Penas P, Long GV. Cutaneous toxicities of RAF inhibitors. Lancet Oncol. 2013;14(1):e11–8.
Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, Chen Z, Lee MK, Attar N, Sazegar H, et al. 2010 Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 468(7326):973–7.
Poulikakos PI, Persaud Y, Janakiraman M, Kong X, Ng C, Moriceau G, Shi H, Atefi M, Titz B, Gabay MT, et al. RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E). Nature. 2011;480(7377):387–90.
Paraiso KH, Xiang Y, Rebecca VW, Abel EV, Chen YA, Munko AC, Wood E, Fedorenko IV, Sondak VK, Anderson AR, et al. PTEN loss confers BRAF inhibitor resistance to melanoma cells through the suppression of BIM expression. Cancer Res. 2011;71(7):2750–60.
Fedorenko IV, Paraiso KH, Smalley KS. Acquired and intrinsic BRAF inhibitor resistance in BRAF V600E mutant melanoma. Biochem Pharmacol. 2011;82(3):201–9.
Sullivan RJ, Flaherty KT. Resistance to BRAF-targeted therapy in melanoma. Eur J Cancer. 2013;49(6):1297–304.
Hauschild A, Grob JJ, Demidov LV, Jouary T, Gutzmer R, Millward M, Rutkowski P, Blank CU, Miller WH Jr, Kaempgen E, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380(9839):358–65.
Villanueva J, Vultur A, Lee JT, Somasundaram R, Fukunaga-Kalabis M, Cipolla AK, Wubbenhorst B, Xu X, Gimotty PA, Kee D, et al. Acquired resistance to BRAF inhibitors mediated by a RAF kinase switch in melanoma can be overcome by cotargeting MEK and IGF-1R/PI3K. Cancer Cell. 2010;18(6):683–95.
Long GV, Trefzer U, Davies MA, Kefford RF, Ascierto PA, Chapman PB, Puzanov I, Hauschild A, Robert C, Algazi A, et al. Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): a multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(11):1087–95.
Falchook GS, Long GV, Kurzrock R, Kim KB, Arkenau TH, Brown MP, Hamid O, Infante JR, Millward M, Pavlick AC, et al. Dabrafenib in patients with melanoma, untreated brain metastases, and other solid tumours: a phase 1 dose-escalation trial. Lancet. 2012;379(9829):1893–901.
Kainthla R, Kim KB, Falchook GS. Dabrafenib for treatment of BRAF-mutant melanoma. Pharmgenomics Pers Med. 2014;7:21–9.
Russo AE, Torrisi E, Bevelacqua Y, Perrotta R, Libra M, McCubrey JA, Spandidos DA, Stivala F, Malaponte G. Melanoma: molecular pathogenesis and emerging target therapies (Review). Int J Oncol. 2009;34(6):1481–9.
Pratilas CA, Taylor BS, Ye Q, Viale A, Sander C, Solit DB, Rosen N. (V600E)BRAF is associated with disabled feedback inhibition of RAF-MEK signaling and elevated transcriptional output of the pathway. Proc Natl Acad Sci U S A. 2009;106(11):4519–24.
Flaherty KT, Hodi FS, Bastian BC. Mutation-driven drug development in melanoma. Curr Opin Oncol. 2010;22(3):178–83.
Solit DB, Garraway LA, Pratilas CA, Sawai A, Getz G, Basso A, Ye Q, Lobo JM, She Y, Osman I, et al. BRAF mutation predicts sensitivity to MEK inhibition. Nature. 2006;439(7074):358–62.
Lorusso PM, Adjei AA, Varterasian M, Gadgeel S, Reid J, Mitchell DY, Hanson L, DeLuca P, Bruzek L, Piens J, et al. Phase I and pharmacodynamic study of the oral MEK inhibitor CI-1040 in patients with advanced malignancies. J Clin Oncol. 2005;23(23):5281–93.
Kirkwood JM, Bastholt L, Robert C, Sosman J, Larkin J, Hersey P, Middleton M, Cantarini M, Zazulina V, Kemsley K, et al. Phase II, open-label, randomized trial of the MEK1/2 inhibitor selumetinib as monotherapy versus temozolomide in patients with advanced melanoma. Clin Cancer Res. 2012;18(2):555–67.
Ascierto PA, Schadendorf D, Berking C, Agarwala SS, van Herpen CM, Queirolo P, Blank CU, Hauschild A, Beck JT, St-Pierre A, et al. MEK162 for patients with advanced melanoma harbouring NRAS or Val600 BRAF mutations: a non-randomised, open-label phase 2 study. Lancet Oncol. 2013;14(3):249–56.
Flaherty KT, Robert C, Hersey P, Nathan P, Garbe C, Milhem M, Demidov LV, Hassel JC, Rutkowski P, Mohr P, et al. Improved survival with MEK inhibition in BRAF-mutated melanoma. N Engl J Med. 2012;367:107–14.
Grimaldi AM, Simeone E, Ascierto PA. The role of MEK inhibitors in the treatment of metastatic melanoma. Curr Opin Oncol. 2014;26(2):196–203.
Flaherty KT, Infante JR, Daud A, Gonzalez R, Kefford RF, Sosman J, Hamid O, Schuchter L, Cebon J, Ibrahim N, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N Engl J Med. 2012;367(18):1694–703.
Menzies AM, Long GV. Dabrafenib and trametinib, alone and in combination for BRAF-mutant metastatic melanoma. Clin Cancer Res. 2014;20:2035–43.
Carvajal RD, Antonescu CR, Wolchok JD, Chapman PB, Roman RA, Teitcher J, Panageas KS, Busam KJ, Chmielowski B, Lutzky J, et al. KIT as a therapeutic target in metastatic melanoma. JAMA. 2011;305(22):2327–34.
Guo J, Si L, Kong Y, Flaherty KT, Xu X, Zhu Y, Corless CL, Li L, Li H, Sheng X, et al. Phase II, open-label, single-arm trial of imatinib mesylate in patients with metastatic melanoma harboring c-Kit mutation or amplification. J Clin Oncol. 2011;29(21):2904–9.
Wyman K, Atkins MB, Prieto V, Eton O, McDermott DF, Hubbard F, Byrnes C, Sanders K, Sosman JA. Multicenter Phase II trial of high-dose imatinib mesylate in metastatic melanoma: significant toxicity with no clinical efficacy. Cancer. 2006;106(9):2005–11.
Ugurel S, Hildenbrand R, Zimpfer A, La Rosee P, Paschka P, Sucker A, Keikavoussi P, Becker JC, Rittgen W, Hochhaus A, et al. Lack of clinical efficacy of imatinib in metastatic melanoma. Br J Cancer. 2005;92(8):1398–405.
Hodi FS, Friedlander P, Corless CL, Heinrich MC, Mac Rae S, Kruse A, Jagannathan J, Van den Abbeele AD, Velazquez EF, Demetri GD, et al. Major response to imatinib mesylate in KIT-mutated melanoma. J Clin Oncol. 2008;26(12):2046–51.
Hodi FS, Corless CL, Giobbie-Hurder A, Fletcher JA, Zhu M, Marino-Enriquez A, Friedlander P, Gonzalez R, Weber JS, Gajewski TF, et al. Imatinib for melanomas harboring mutationally activated or amplified KIT arising on mucosal, acral, and chronically sun-damaged skin. J Clin Oncol. 2013;31(26):3182–90.
Alexandrescu DT, Ichim TE, Riordan NH, Marincola FM, Di Nardo A, Kabigting FD, Dasanu CA. Immunotherapy for melanoma: current status and perspectives. J Immunother. 2010;33(6):570–90.
Rosenberg SA, Mule JJ, Spiess PJ, Reichert CM, Schwarz SL. Regression of established pulmonary metastases and subcutaneous tumor mediated by the systemic administration of high-dose recombinant interleukin 2. J Exp Med. 1985;161(5):1169–88.
Atkins MB, Lotze MT, Dutcher JP, Fisher RI, Weiss G, Margolin K, Abrams J, Sznol M, Parkinson D, Hawkins M, et al. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: analysis of 270 patients treated between 1985 and 1993. J Clin Oncol. 1999;17(7):2105–16.
Hauschild A. Adjuvant interferon alfa for melanoma: new evidence-based treatment recommendations? Curr Oncol. 2009;16(3):3–6.
Iida T, Ohno H, Nakaseko C, Sakuma M, Takeda-Ezaki M, Arase H, Kominami E, Fujisawa T, Saito T. Regulation of cell surface expression of CTLA-4 by secretion of CTLA-4-containing lysosomes upon activation of CD4 + T cells. J Immunol. 2000;165(9):5062–8.
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23.
Della Vittoria Scarpati G, Fusciello C, Perri F, Sabbatino F, Ferrone S, Carlomagno C, Pepe S. Ipilimumab in the treatment of metastatic melanoma: management of adverse events. Oncol Targets Ther. 2014;7:203–9.
Margolin K, Ernstoff MS, Hamid O, Lawrence D, McDermott D, Puzanov I, Wolchok JD, Clark JI, Sznol M, Logan TF, et al. Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol. 2012;13(5):459–65.
Ascierto PA. Ipilimumab in the treatment of metastatic melanoma: a summary of recent studies. Tumori. 2013;99(6):302e–5
Ascierto PA, Marincola FM, Ribas A. Anti-CTLA4 monoclonal antibodies: the past and the future in clinical application. J Transl Med. 2011;9:196.
Riley JL. PD-1 signaling in primary T cells. Immunol Rev. 2009;229(1):114–25.
Ishida Y, Agata Y, Shibahara K, Honjo T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J. 1992;11(11):3887–95.
Nishimura H, Honjo TÂ. PD-1: an inhibitory immunoreceptor involved in peripheral tolerance. Trends Immunol. 2001;22(5):265–8.
Parry RV, Chemnitz JM, Frauwirth KA, Lanfranco AR, Braunstein I, Kobayashi SV, Linsley PS, Thompson CB, Riley JL. CTLA-4 and PD-1 receptors inhibit T-cell activation by distinct mechanisms. Mol Cell Biol. 2005;25(21):9543–53.
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–54.
Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–65.
Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Fanale, D., Bronte, G., Russo, A. (2015). Targeted Therapies in Melanoma. In: Russo, A., Rosell, R., Rolfo, C. (eds) Targeted Therapies for Solid Tumors. Current Clinical Pathology. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-2047-1_16
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2047-1_16
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-2046-4
Online ISBN: 978-1-4939-2047-1
eBook Packages: MedicineMedicine (R0)