Abstract
Despite the modifications in the past four decades, Gleason grading system has been validated as a fundamental prognostic factor for prostate cancer, both on biopsy and on radical prostatectomy. The modification in 2005 International Society of Urologic Pathology (ISUP) Gleason grading system had an enormous impact on the contemporary practice of prostate cancer. Although 2005 ISUP modified grading system is still imperfect, there is no other marker or grading system that can be as quickly and reproducibly applied in practice, which highlights the role of the pathology in patient management. For a pathologist, the key issue remains the use of consistent grading criteria, which reflect the mainstream grading trends. Further modifications and refinements of the criteria need to be carefully validated and confirmed in large or multi-institutional studies with well-defined outcomes, before additional changes are implemented, preferably based through a broad international consensus. Thus, ISUP modified Gleason system still remains one of the most powerful grading schemes in all of urologic oncology and a gold standard against which other prospective markers are and will be compared with and measured against in future studies. This chapter summarizes the recent developments and modifications of the Gleason grading system and their impact in contemporary clinical practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Historical Background and Context
Nearly half a century ago, in 1966, the pathologist Donald Gleason developed a grading system (Fig. 2.1a, b) for prostatic adenocarcinoma [1], which has been embraced almost universally as an essential component of prostate adenocarcinoma grading and reporting. Over time, the system has been modified by Gleason and his collaborators and by others [1–5]. Despite the modifications in the past four decades, the Gleason grading system has been validated as a fundamental prognostic factor for prostate cancer, both on biopsy and on radical prostatectomy (RP), of patient outcomes, including biochemical failure, local recurrence, and lymph node or distant metastasis . Gleason score (GS) has also been incorporated in clinical tools, such as Partin tables and Kattan nomograms , which are used to predict pathologic stage and outcome following RP or radiotherapy . GS on needle biopsy is also utilized to determine treatment selection, such as active surveillance , RP, brachytherapy, lymph node dissection , and the extent of neurovascular bundle resection.
The Gleason system is based on low-power microscopic assessment (×4 or ×10) of the cancer architecture. The key principle of the grading is based on the use of two most common cancer grades (out of possible 5), primary plus secondary grade , to produce a GS, which theoretically ranges from 2 to 10. When only a single grade is identified, it is doubled to yield a GS. The terms “pattern” and “grade” have also been retained. Typically, pattern is used to describe one or more of the morphologic variations, while grade is used in a more encompassing way, to include all pattern variations within a certain grade.
In clinical practice, the diagnosis of prostate cancer and its management have also evolved over the last few decades, first by introduction of prostate-specific antigen (PSA) testing in the late 1980s, and the extensive use of RP. Prostate cancer incidence has also changed since the introduction of PSA testing, first demonstrating an increase and then a drop; more recently, mortality, primarily in the Western countries, has also decreased [6]. Thus, in current practice, patients are diagnosed earlier, at a younger age, with smaller cancer volumes and lower stage disease [7]. During the last two decades, the practice of thin-needle prostate biopsies (16–18 gauge) has also taken place, first as sextant (six core) biopsies, and then as systematic and extended prostate biopsies, with at least ten tissue cores sampled from different prostate sites (apex, mid, base). The biopsies are also commonly submitted in a site-specific fashion. In contrast, Gleason developed his system on tissue samples from large-bore biopsies (14 gauge) without a site-specific submission, and on transurethral resection of prostate and prostatectomy specimens. In addition, immunohistochemistry was not available in the era when the system was developed, variants of adenocarcinoma and certain morphologic patterns were not recognized, and the significance of the tertiary grade remained uncertain. Around the turn of the century, it also became evident that there are differences in the application of the Gleason system among pathologists (i.e., interobserver variability), particularly in the evolving needle biopsy practice. Pathologists used the Gleason system based on their own understanding, interpretation, or preference. Thus, it was necessary to establish a consensus and to codify the application of the Gleason system to correspond with the clinical practice in the twenty-first century.
International Society of Urologic Pathology 2005 Modification of the Gleason System
In March 2005, a consensus conference was convened by the International Society of Urologic Pathology (ISUP) in San Antonio, TX, USA, in an effort to standardize and unify the use of the Gleason grading system [4]. Specific areas of the original Gleason System reviewed at the 2005 ISUP conference are illustrated in Table 2.1. A “consensus” was defined when two third of the participants were in agreement on certain questions. This effort resulted in the 2005 ISUP modified Gleason system, which, similar to the original Gleason system , outlined the morphologic patterns 1–5 (shown in Table 2.2), which are accompanied by a diagram for the modified Gleason system (shown with the original Gleason system for comparison in Fig. 2.1a, b). The differences between the original Gleason system and the 2005 ISUP modified Gleason system are summarized in Table 2.3 [4, 8]. The 2005 ISUP modified Gleason system reiterated the following points (Table 2.4):
-
a.
GS represents the sum of the primary (most predominant) Gleason grade and the secondary (second most predominant) Gleason grade. However, in needle biopsies, this principle was modified to include any component of higher grade than the second most predominant grade as the secondary grade. Thus, on needle biopsy the GS is derived based on the primary and the highest (worst) grade.
-
b.
The reporting of the grade should be accompanied by using the words “pattern” or “grade,” and it is therefore not acceptable to report only “Gleason 3” because it is unclear whether this represents grade (pattern) or score.
-
c.
GS 1 + 1 = 2 on needle biopsy should rarely, if ever, be reported and should be carefully considered in practice, in any type of specimen. These cancers are extraordinarily rare in needle biopsies, although they can be infrequently seen in transurethral or RP specimens. There is a poor reproducibility even among experts in grading lower-grade tumors. Cancers that are assigned GS 2–4 on needle biopsy correlate poorly with RP GS and these “low” scores may misguide clinicians and misinform patients into considering these tumors as indolent.
-
d.
Individual cells are not part of Gleason pattern 3.
-
e.
Most cribriform glands are diagnosed as Gleason pattern 4. Only rare cribriform glands satisfy the stringent diagnostic criteria required for the diagnosis of cribriform pattern 3: rounded, well-circumscribed glands of the same size as the normal glands.
-
f.
Morphologic variants of acinar adenocarcinoma, such as pseudohyperplastic and foamy adenocarcinoma, should be graded on the basis of the underlying architecture.
-
g.
A secondary pattern of lower-grade cancer, when it occupies less than 5 % of tumor, should be ignored and not reported as part of the GS, both on needle biopsy and RP.
-
h.
High-grade tumor of any quantity, even when occupying less than 5 % of the tumor, should always be included and reported within the GS on needle biopsy.
-
i.
When a tertiary Gleason pattern is present, GS on biopsy should be derived by adding the primary and the highest (worst) pattern, whereas on RP, the tertiary pattern (the least common pattern), should be reported separately if it is of higher grade than the primary and the secondary patterns.
-
j.
When separate tumor nodules with different Gleason patterns are encountered on RP, they should be scored and reported separately.
-
k.
It remains optional to include the actual percentage of Gleason patterns 4 or 5 in a report.
-
l.
For needle biopsies containing different cores with different cancer grades, separate GS should be assigned for individual positive cores, if they are submitted in separate containers or if the cores are in the same container, but have a designated location (for example, if marked by different ink color). An optional, overall GS can be provided at the end of the case for all positive biopsy cores. The overall (global) GS follows the general rule of primary (most predominant) Gleason grade and secondary (second most predominant) Gleason grade [9, 10]. When a container has multiple fragmented cores and it is unclear whether they represent intact cores or multiple cores, an overall score should be provided for all fragments in the container.
Changes and Trends in Practice in Interpreting Gleason Grades 1–5 After the 2005 ISUP Consensus Conference
The 2005 ISUP modified Gleason system was widely promoted and embraced in routine practice after the consensus conference and the subsequent publication, although certain issues remained unresolved. The main trends and changes in the use of individual grades in pathology practice after 2005 were as follows:
Gleason Grade 1
Since the 2005 ISUP consensus conference concluded that Gleason grade 1 tumors should be diagnosed “rarely, if ever,” the use of pattern 1 after 2005 became vanishingly rare. Many uropathology experts maintain that pattern 1 in the original Gleason system likely represented adenosis (atypical adenomatous hyperplasia), a now well-recognized cancer mimicker. At that time, however, immunohistochemistry was not available and thus, adenosis may account for the great majority of cases considered traditionally as Gleason pattern 1. Many of the infrequently published images of Gleason pattern 1 can be critically questioned and accordingly it has been proposed that Gleason pattern 1 is completely abandoned in practice [11].
Gleason Grade 2
Similarly, the appropriateness of using pattern 2 in needle biopsies has also been questioned and pathologists have been advised not to use it in grading cancer on needle biopsies [12]. Cancers assigned GS 2–4 on needle biopsy correlate poorly with GS on RP, which almost always contain higher-grade cancer. Pattern 2 can be seen occasionally in transurethral resection and RP specimens, usually as part of multifocal cancer invariably showing a higher-grade component.
Gleason Grade 3
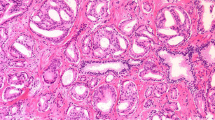
The general focus of the 2005 modifications pertained primarily to the most prevalent patterns 3 and 4. The 2005 ISUP modified Gleason system restricted the definitions of pattern 3 and broadened the spectrum of pattern 4 cancer [8, 13, 14]. As in the original Gleason system, pattern 3 in the 2005 ISUP modified Gleason system includes discrete well-formed individual glands, infiltrating in and among nonneoplastic prostate acini (Fig. 2.2a). Very small, well-formed glands are still considered Gleason pattern 3; however, in contrast to the original Gleason system , “individual cells” are not. The definition of grade 3, however, also stipulates “marked variation in glandular size and shape,” which, unfortunately, was not well depicted in the 2005 diagram. It is still unclear, for example, which variations in glandular shape should be considered Gleason pattern 3 (Fig. 2.2b). Are individual glands showing branching and forming, for example, X, V, T, and Y glandular shapes (not illustrated in the 2005 diagram) still consistent with pattern 3 or do they represent pattern 4? Indeed, many uropathologists would consider these common morphologies to represent pattern 3, but unfortunately this cannot be reconciled using the 2005 ISUP Gleason diagram .
Gleason grade 3 includes discrete infiltrative glands with well-formed lumina (a). Individual glands showing some modifications of size and shape such as branching (not illustrated in the 2005 diagram) are still interpreted as pattern 3, although some may interpret them as pattern 4 (b). Cribriform rounded, well-circumscribed glands of the same size as the normal glands are interpreted as pattern 3 (c). If they are with similar cribriform features but of larger size than a normal gland, they are currently interpreted as pattern 4. Using the original Gleason system, these would have been graded as pattern 3 (d)
More stringent criteria were established by the 2005 ISUP consensus conference concerning cribriform pattern 3 glands. Only rounded, well-circumscribed glands of the same size as the normal glands, with evenly spaced lumina and cellular bridges (Fig. 2.2c) are included as cribriform Gleason pattern 3. In essence, these types of cancers should morphologically resemble cribriform high-grade prostatic intraepithelial neoplasia (HGPIN), but lack basal cells. This definition was in contrast to the original Gleason illustrations of cribriform pattern 3, which included large, cribriform glands with rounded and smooth contours, exceeding the size of the normal glands (Fig. 2.2d). In the current practice, nearly all cribriform glands are being diagnosed as pattern 4 [13].
Gleason Grade 4
The scope of Gleason pattern 4 in the 2005 ISUP modified Gleason system was widened. A consensus was reached that ill-defined glands with poorly formed lumina, a pattern often seen in fused glandular structures, should also be included under Gleason pattern 4. This novel category was not described in the original Gleason system.
Therefore, pattern 4 now includes: (a) fused microacinar glands; (b) ill-defined glands with poorly formed glandular lumina; (c) large, cribriform glands and cribriform glands with an irregular border, and (d) hypernephromatoid glands:
-
a.
Fused glandular morphology implies that discrete glandular units are lost or are unrecognizable (unchanged from the original Gleason system) (Fig. 2.3a).
Fig. 2.3 Gleason grade 4 includes glands that are fused (represented on the right; contrast them with the individual glands on the left) (a), glands with ill-formed lumina (contrast them with a couple of individual glands with well-formed lumina in the upper right) (b), large cribriform glands (c), and hypernephromatoid glands (d)
-
b.
Ill-defined glands with poorly formed glandular lumina, a novel category, is now considered pattern 4 (Fig. 2.3b). The illustrations of this pattern remained sketchy and unclear in the literature, thus creating some confusion and leading to relatively open interpretation of this concept. Distinguishing, for example, between poorly formed glands (pattern 4) and tangentially sectioned glands (pattern 3) seems to be one of the most problematic issues of the current Gleason grading . This essentially requires two-dimensional interpretation of a three-dimensional complex glandular morphology, which can be subjective.
-
c.
Cribriform glands, as previously outlined, are nearly uniformly diagnosed as Gleason pattern 4 in current practice, independently of the glandular contour (Fig. 2.3c). In a recent study, poor reproducibility was reported among urologic pathologists in defining Gleason pattern 3 cribriform glands; in addition, in 73 % of the cases there was a coexistent Gleason pattern 4 tumor [15]. Therefore, a proposal has been made by Epstein to alter the 2005 ISUP diagram and to delete the cribriform 3 morphology [13, 14].
-
d.
Hypernephromatoid, an infrequent glandular morphology of fused glands with clear or pale cytoplasm was retained as pattern 4 (Fig. 2.3d) (unchanged from the original Gleason system).
Gleason Grade 5
Pattern 5 remains almost unchanged from the original Gleason system and indicates absence of glandular differentiation, with neoplastic cells forming solid sheets, cords, or single cells (Fig. 2.4a, b). The presence of cords also includes single file cell formation. Solid nests, i.e., solid structures smaller than a “sheet” may potentially pose some problems, as smaller solid units may be interpreted as glands with ill-defined lumina (pattern 4). Comedocarcinoma with central necrosis surrounded by papillary , cribriform, or solid glands also represents pattern 5 (Fig. 2.4c, d).
Grading Variants of Prostate Adenocarcinoma in Contemporary Practice
Grading of different variants of prostatic adenocarcinoma is shown in Table 2.5 and illustrated in Fig. 2.5a–g) :
Variants of prostatic carcinoma. Pseudohyperplastic carcinoma should be graded as pattern 3 (a). Foamy (or xanthomatous) carcinoma should be graded as pattern 4 if composed of individual glands (b) or pattern 4 if composed of fused or cribriform glands. Ductal adenocarcinoma is graded as pattern 4 (c); if comedonecrosis is present, it is graded as pattern 5. Colloid (mucinous) adenocarcinoma is graded as pattern 3 if individual discrete glands are floating within mucin (d) or pattern 4 if they appear irregular cribriform or fused (as rare glands on the image). Atrophic cancer is graded as pattern 3; note a collagenous micronodule slightly off to the left of the center (e); cystic and microcystic cancers are also graded as pattern 3 (f). PIN-like adenocarcinoma is graded as pattern 3 (g); if there is glandular fusion, it is graded as pattern 4
Pseudohyperplastic Adenocarcinoma
Cancers with pseudohyperplastic features (large individual glands resembling normal glands, but containing cytologically malignant nuclei), should be graded as Gleason grade 3, in large part based on the recognition that they are most often accompanied by more usual Gleason grade 3 adenocarcinoma (Fig. 2.5a) .
Foamy Gland Carcinoma
Although most cases of foamy (or xanthomatous) gland carcinoma would be graded as Gleason grade 3 (Fig. 2.5b), they can also show a higher-grade pattern and should be graded accordingly, usually as Gleason pattern 4.
Ductal Adenocarcinoma
This is graded as Gleason pattern 4, but if comedonecrosis is present, it is graded as Gleason pattern 5 (Fig. 2.5c).
Colloid (mucinous) Carcinoma
According to the 2005 ISUP consensus conference, mucin-containing adenocarcinoma can be graded as Gleason pattern 3, if individual round and discrete glands are floating within mucinous pools, or Gleason pattern 4, if irregular, cribriform or fused glands float within a mucinous background (Fig. 2.5d). In essence, the grade of the tumor should be based on the underlying architectural pattern, while the extracellular mucin should be ignored for grading purposes. Currently, however, there is no consensus on this issue. Both methods are acceptable until additional studies indicate which method is preferable.
Atrophic or Cystic/Microcystic Adenocarcinoma
Both are graded as Gleason pattern 3 (Fig. 2.5e, f). They are often accompanied by usual acinar-type adenocarcinoma. Both atrophic and cystic/microcystic adenocarcinoma variants can be seen in association with PIN-like or pseudohyperplastic carcinoma, which usually represent pattern 3 [16].
PIN-like Adenocarcinoma
This is graded as Gleason pattern 3 if discrete glandular units are present. It can be graded as Gleason pattern 4 if there is evidence of fusion (Fig. 2.5g).
The following types of prostatic carcinoma should not be graded:
-
Small cell (neuroendocrine) carcinoma
-
Squamous or adenosquamous carcinoma
-
Urothelial carcinoma of the prostate
-
Basaloid or adenoid cystic carcinoma
-
Sarcomatoid adenocarcinoma (some would grade as pattern 5)
Grading-Specific Glandular Morphologies in Prostatic Adenocarcinoma
Glomerulations (Glomeruloid Structures)
Glomerulations are glands containing intraluminal, complex or cribriform structures, usually with a single point of attachment to the outer gland (Fig. 2.6a, b). Larger glomeruloid glands are almost uniformly accepted as Gleason pattern 4 by urologic pathologists . The opinions are divided whether all glomeruloid structures should be assigned Gleason pattern 4, or some smaller glomeruloid glands should be graded as Gleason pattern 3. Based on the ISUP consensus, either approach is currently acceptable until this issue is clarified .
Specific glandular morphologies are grades as follows: glomerulations which contain intraluminal cribriform (a) or complex structures (b) should be assigned pattern 4. Note the occasional vacuoles in (a); if vacuoles are present, the cancer should be graded based on the underlying morphology, by subtracting the vacuoles. In the case of collagenous micronodules (mucinous fibroplasia), the underlying glands are graded after subtracting the nodules; if the glands are individual, it is pattern 3 (c); if the background glands are fused, it is pattern 4 (d). Intraductal carcinoma is currently not graded, but a grade is assigned to the background invasive cancer; if single cells are present in the background ( top), it is graded as pattern 5 (e). Signet ring-like as pattern is typically graded as pattern 5 (f)
Collagenous Micronodules (Mucinous Fibroplasia)
Glands containing collagenous micronodules (mucinous fibroplasia) present a grading challenge because glandular architecture is significantly altered. Collagenous micronodules are composed of collagen and scattered fibroblastic cells representing an organization of the intra- and extraluminal mucin associated with the neoplastic glands. Mucinous fibroplasia may also occur in fused or cribriform-appearing glands. In grading collagenous micronodules, it would be currently acceptable to grade the underlying glandular architecture and to subtract the mucinous fibroplasia, analogous to the scenario when grading neoplastic glands associated with mucinous adenocarcinoma (Fig. 2.6c, d).
Intraductal Carcinoma
Typically, intraductal carcinoma is not graded, but a grade is assigned to the background invasive cancer, which is present in the great majority of cases and is usually high grade (pattern 4 or 5) (Fig. 2.6e). Most experts currently do not assign a grade for intraductal carcinoma, but only include a note that intraductal carcinoma is present concomitantly with invasive carcinoma of a certain grade. Sometimes, however, no invasive carcinoma component is identified, particularly in limited needle biopsy specimens. Currently, there is no consensus how and if the isolated intraductal component should be graded. In these situations, it may be prudent to mention the frequent association with high-grade adenocarcinoma and suggest a repeat biopsy to clarify the diagnosis .
Vacuoles
Although vacuoles are usually seen in pattern 4, they may be seen in pattern 5 or even pattern 3 cancer. Cancer should be graded based on the underlying morphology, by subtracting the vacuoles (Fig. 2.6a).
Signet Ring-Like Pattern
Signet ring-like pattern is typically graded as Gleason pattern 5 (Fig. 2.6f). However, sometimes it is difficult to distinguish signet ring-like carcinoma from vacuoles, which can be seen in pattern 4 or even pattern 3. If only isolated or scattered vacuoles are present and there is absence of extensive signet ring formations, the vacuoles should not be graded as pattern 5, but rather the underlying cancer architecture should be evaluated.
Tertiary Gleason Pattern 5
Gleason reported in his original study that more than two tumor patterns occurred only rarely and noted that there were too few cases to permit meaningful analysis of the prognostic significance of a tertiary grade (3). More than two patterns are, however, often present in prostatectomy specimens , and also in needle biopsies. In RP specimens with three grades, it is currently recommended by the 2005 ISUP consensus that the tertiary pattern be reported separately when it is of higher grade than the primary and secondary grades. The incidence of a tertiary pattern varies greatly between series. Some studies consider tertiary pattern only if it is of higher grade than the primary and the secondary grades and if it represents < 5 % of the whole tumor [17]. In other studies, if the tertiary component comprises > 5 % of the tumor, this is considered to be a secondary pattern [18, 19]. One contemporary RP study, performed on a consecutive patient population from a single center, found a prevalence of tertiary Gleason pattern 5 of 22.5 % [20]. In this study, only the tertiary grade > 5 % showed an independent and significant association with adverse pathology, but tertiary pattern ≤ 5 % did not demonstrate an association with adverse outcome [20]. Thus, there are variable approaches for considering the extent of tertiary pattern on RP, which potentially complicates comparisons of different study results. In several RP series, it has been clearly demonstrated that tertiary pattern 5 is a marker of more aggressive disease, which is associated more frequently with PSA recurrence, extraprostatic extension, surgical margin positivity, seminal vesicle infiltration, and lymph node metastasis [17, 19]. In practice, however, some pathologists report the GS, for example, GS 7 (either 3 + 4 or 4 + 3) with tertiary pattern 5, and specify the estimated percentages of primary, secondary, and tertiary grades, usually in a note. Other pathologists, however, maintain that tertiary grade should always represent < 5 % of tumor, and if it exceeds 5 %, they automatically consider it to be a secondary pattern. Despite the recognition of these differences in practice, both approaches should be acceptable, provided it is clearly communicated in reports and in published studies which method was used in assigning the tertiary grade [18, 20, 21]. Currently, in RP reports, many pathologists include a note indicating the association of a tertiary grade 5 with adverse biologic behavior.
Some have recently proposed to account for the presence of tertiary grade 5 in RP specimens by reporting it as follows: GS 6 with tertiary 5 becomes GS 6.5; GS 3 + 4 = 7 with tertiary 5 becomes GS 7.25; Gleason 4 + 3 = 7 becomes GS 7.5; Gleason 4 + 3 = 7 with tertiary 5 becomes GS 8; and GS 8 with tertiary 5 becomes GS 8.5 [18]. While this proposal provides a rationale for stratification of cases which could potentially be used in prognostic nomograms , the practicality of its application remains questionable and awaits further confirmation [18].
Only a few studies have investigated the significance of tertiary Gleason grade on needle biopsy. For needle biopsies, the ISUP 2005 conference recommended that final GS should incorporate the highest (worst) pattern present, even if this was a tertiary one. Thus, GS on biopsy should be derived by adding primary and highest (worst) pattern. This question, however, required validation, with no good data available at the time of the consensus conference. Subsequently, it was demonstrated that in GS 7 cancers, those with tertiary pattern 5 on needle biopsy had a higher risk of PSA recurrence when compared to tumors without tertiary pattern 5 [22]. It has been also shown that tumors with GS 7 and tertiary pattern 5 had an intermediate time to PSA failure between GS 8 and GS 9/10 tumors [23]. In another study on biopsy, Gleason grade 5 was reported overall in 4.1 % of all cancer-positive biopsies: 2.8 % as primary or secondary pattern and 1.3 % as tertiary pattern [24]. Trpkov et al. showed that tertiary pattern 5 on needle biopsy, particularly in nonsurgically treated patients, had a comparable all cause and cancer-specific mortality with secondary pattern 5, but much better outcome than patients with biopsy primary pattern 5 [24]. These findings supported the ISUP recommendation that tertiary pattern 5 found on biopsy is roughly equivalent to secondary pattern 5 and should be factored in the biopsy GS as such.
Grading Minute Foci of Prostate Cancer
Grading should be performed even on minute foci of prostatic carcinoma, which are often diagnostically challenging. Assignment of Gleason grade in this scenario can be problematic and often consists only of one Gleason pattern (Fig. 2.7a, b). If individual glands are present, it is recommended that even small foci of tumor be reported by doubling the pattern and reporting it as a primary and secondary (usually 3 + 3 = 6). The presence of small amounts of tumor in a biopsy does not always correlate with small volume of tumor in the prostatectomy specimens, but this correlation has improved using extended prostate biopsies [12, 25].
Minute foci of prostate adenocarcinoma should be graded. A microfocus composed of 4–5 individual glands represents pattern 3 (a). Immunostains show complete absence of staining for high-molecular-weight keratin in the neoplastic glands, while the basal cells in the adjacent benign glands are positive. Neoplastic glands show diffuse cytoplasmic and luminal staining for racemase in contrast to the negative benign glands (b)
Grading Prostate Cancer After Radiation and Other Treatments
Pathologists should also be familiar with the changes of normal and neoplastic prostate tissue occurring due to various treatments. If uncertain about the diagnosis or whether to grade or not, a pathologist should seek assistance from a uropathologist. Radiation therapy (external beam and brachytherapy, i.e., “seeds”) is a widespread treatment for clinically localized or locally advanced prostate cancer. Cryotherapy (“freezing”) of prostate has also been more widely used during the last decade [26]. A biopsy is typically performed when there is a rising PSA (usually no less than 12 months after radiation or cryotherapy) to distinguish local recurrence from metastatic disease and to determine whether additional treatment is needed. A history of radiation or other therapies is frequently not shared with the pathologist, and it may not be known even to the clinician, so it is essential to be familiar with the changes in benign and malignant glands that occur after various treatments.
Prostate cancers exhibiting marked radiation treatment changes typically display infiltrative, poorly formed glands or single cells with abundantly vacuolated and clear cytoplasm and small shrunken nuclei. Similar cancer morphology may also be seen after cryotherapy. When only cancer with radiation or cryotherapy treatment effect is seen in the specimen, the sign-out may include a statement such as “prostatic adenocarcinoma with extensive radiation/cryo treatment changes” and this cancer should not be Gleason graded . When prostatic adenocarcinoma does not demonstrate significant treatment changes and resembles the usual type adenocarcinoma, it should be graded. In these cases, GS can be assigned, with wording such as “prostatic adenocarcinoma, Gleason pattern 3 + 4 = 7, without significant radiation/cryo treatment changes.” One may add an estimate of the proportion (or %) of the carcinoma exhibiting no treatment changes. Such a diagnosis is important for further clinical management , since patients with negative biopsies and patients whose cancers showed marked therapy changes on biopsy had similar 10-year PSA relapse-free survival outcomes (59 %), and those outcomes were markedly different from patients with positive biopsies without treatment effect (3 %) ( p < 0.001). The 10-year Distant Metastasis-Free Survival rate in patients with negative/marked treatment effect biopsy outcomes was 90 %, while corresponding outcome in patients with positive biopsies without treatment effect was 69 % ( p = 0.0004) [27].
Hormone-treated cancers exhibiting therapy effects also should not be graded because of the possibility of overgrading. One often encounters single and shrunken cells or lack of gland differentiation in this scenario. In summary, it is important to always report GS for cancers that do not exhibit appreciable treatment changes, because cancer in this setting most likely represents either de novo or recurrent disease (or possibly disease that has not been affected or has been missed by the treatment), which is usually associated with worse prognosis .
Concordance of Biopsy and Radical Prostatectomy Gleason Scores
One of the expected consequences of modifying the Gleason grading system has been an improvement in the agreement (concordance) between biopsy GS and RP GS. Before the 2005 Gleason modification, the agreement of the biopsy and RP GS ranged from approximately 30 to 70 % in most studies. After 2005, some studies have indeed documented an improvement between needle biopsy and RP GS. One study showed that overall agreement between needle biopsy and RP specimens increased from 58 to 72 % when the modified Gleason system was applied [28]. Other studies, however, failed to demonstrate significant improvement in the GS agreement between the biopsy and RP [29, 30]. In a study by Uemura et al., the biopsy-RP GS concordance using the original Gleason system and the ISUP modified system was 67 and 70 %, respectively [30]. Similarly, Zareba et al. showed that the biopsy-RP GS agreement did not improve significantly using the modified Gleason system (63.4 and 65.5 %, original vs modified Gleason, respectively). In current practice, RP GS upgrades are reported in 36 % (mean) cases (30 % in our practice) [29, 31]. The incidence of upgrading on biopsy is documented in current practice in fewer studies, and ranges between 5 and 15 % (5 % in our practice) [29].
There are several reasons for biopsy and RP GS discrepancies: sampling error, erroneous pattern interpretation, borderline grades, Gleason grade assignment on biopsy and clinician’s interpretation of the biopsy GS. Extended biopsies (ten cores) are associated with less upgrading on RP than sextant biopsies. Prostate biopsy samples, however, represent only a fraction of a percentage of the whole gland (< 0.05 cc) and the chance to miss a limited higher-grade cancer on biopsy remains high. This typically occurs when a needle biopsy cancer is graded GS 3 + 3 = 6 and a limited pattern 4, which was not sampled in the biopsy becomes apparent in the RP specimen, resulting in RP upgrade of GS 3 + 4 = 7. Tumor multifocality may be another reason for possible discrepancies between biopsy and RP GS. With teaching and growing experience, pathologists also recognize the grading pitfalls and develop better accuracy and reproducibility in their grading. Common pathology errors in grading biopsy specimens include: (a) overcalling Gleason pattern 5 on tangentially sectioned small glands of pattern 3; (b) undercalling cribriform Gleason pattern 4 as pattern 3; and (c) undercalling small foci of Gleason pattern 5 (such as individual cells, cords, or solid nests). There are also common problems in assigning borderline grades between, for example, small glands of pattern 3 and poorly formed glands of pattern 4. Poorly formed glands (pattern 4) may also be interpreted as small foci of individual cells (pattern 5).
Undergrading on biopsy may also result from difficulty in recognizing small foci of glandular fusion. Another reason for apparent discrepancies between biopsy and RP GS is when the single highest (worst) GS in any positive core is considered to be the representative biopsy GS for the entire case. Using this approach in one study, a biopsy GS 8 could be reproduced as RP GS 8 in only 21.5 % cases and corresponded with RP GS < 8 in > 50 % of RP [31]. Similarly, the assignment of biopsy GS based on the primary and the highest (or the worst) grade may account for some discrepancies between the biopsy and RP GS. Although pathologists usually report Gleason grades of each site separately, clinicians often take the highest GS from any site when planning treatment, which may be a possible reason for biopsy-RP GS discrepancies [32].
Currently available prognostic tools, such as nomograms , have limited ability to predict clinically significant upgrading of biopsy GS and are not ready for clinical application. The predictive ability of various models to account for upgrades and downgrades between biopsy and RP GS has also been disappointing, which is also confounded by the differences in biopsy techniques, number of cores sampled, and indications for biopsy. Thus, GS upgrades and downgrades still remain an important issue in clinical practice after 2005.
Inter- and Intraobserver Reproducibility of the Modified Gleason System
The modified Gleason grading system has demonstrated good reproducibility along the entire spectrum of morphologic patterns. The improvement in reproducibility is likely due to the refined definitions of the individual grades and the decreased diagnosis of carcinomas with low GS (Gleason 2–5) on needle biopsy using the modified Gleason system. Exact intraobserver agreement on GS was reported in 43–78 % of cases, and agreement within ± 1 unit was reported in 72–87 % of cases [33, 34]. This is an improvement over Gleason’s own performance, because he was able to exactly reproduce his previous scores approximately half of the times. Highly variable levels of interobserver agreement on GS have also been reported in another study (range of 36–81 % for exact agreement and 69–86 % within ± 1unit) [35].
Interobserver variability and reproducibility in applying the Gleason scoring system are due to various factors, including differences in training (various mentors, different institutions), familiarity with the system, varying personal experience, volume of practice, and inherent subjectivity, as in all grading systems. Problems still persist regarding the inter- and intraobserver variability and the threshold issues (particularly Gleason pattern 3 vs. Gleason pattern 4). These diagnostic variations could potentially have an effect on multi-institutional trials, for example, of active surveillance, because the population of patients at different centers may differ based on the thresholds of Gleason grading. A central, expert review may correct these problems, but even in this setting, the threshold issues may still persist. Providing a review by a specialized uropathologist in problematic cases, either in routine practice in each institution or through a single central review in a study setting may also mitigate the variations in reproducibility. Further improvements in the reproducibility of Gleason grading can be achieved by educational activities focusing on known problematic areas.
Clinical Impact of the ISUP Modified Gleason Grading System in Practice
The impact and consequences in clinical practice have been examined in several studies after the ISUP modified system was introduced in 2005 [14, 28–30, 36–39]. The summary result has been an upward migration of the GS. In clinical practice, Gleason pattern 3, which was previously the most common on biopsy, has become less common than pattern 4. Most of the studies, however, have been performed in retrospective fashion by reviewing previously scored cases [28, 39]. One retrospective study on matched biopsy and RP specimens documented a significant reduction of GS 6 from 48 to 22 % on biopsy and from 32 to only 6 % on RP [28]. This was accompanied by a significant increase in GS 7 from 25 to 68 % on biopsy and from 36 to 83 % on RP. In contrast, in routinely graded biopsy and RP cohorts before and after 2005, which included over 1300 cases, similar trends were observed both on biopsy and on RP [29]. There was a decline of GS 6 on biopsy from 68 to 55 % after 2005, which was reciprocated by an increase in GS 7 biopsies from 30 to 43 % after 2005. In the same fashion, there was a decline of RP GS 6 cancers from 47 to 32 % after 2005, accompanied by a corresponding increase of RP GS 7 cancers from 48 to 60 % after 2005. The most frequent change from biopsy to RP in patients after 2005 was an upgrade from biopsy GS 6 to RP GS 7 (3 + 4) (due to secondary pattern upgrades from pattern 3 to 4). This study also documented a trend towards better complete agreement for GS ≥ 7 [29).
Several changes in the ISUP 200 modified system may account for the upward migration in the Gleason grading . More strict definition of cribriform pattern reduced the morphologic spectrum of cribriform glands interpreted as Gleason pattern 3. Scoring of glands with poorly formed lumina has also been adopted in practice and uniformly interpreted as Gleason pattern 4. Although the morphologic spectrum of ill-defined glands (Gleason pattern 4) may include glands which can be interpreted either as Gleason pattern 3 or Gleason pattern 5, the creation of this category has allowed for routine and mainstream use of this morphologic pattern as Gleason pattern 4. Another reason for the Gleason upward migration after 2005 is the rule of excluding a lower Gleason pattern involving a minimal (< 5 %) proportion of cancer in a setting of extensive high-grade cancer. A sizable proportion of the upgrades on biopsy may be due to the rule to incorporate tertiary Gleason pattern (in practice, pattern 5) as a secondary pattern on biopsy specimens, when it is higher than the secondary pattern. Many pathologists also interpret glands with more or less complex branching (which was not explicitly discussed in the consensus paper) as part of “marked” variation in gland shape criteria, which was included in the text description of Gleason pattern 3. Some pathologists, however, tend to follow more closely the diagram and interpret the irregularities or gland branching as true gland fusion, and grade them as pattern 4, which may also account for some upgrades from pattern 3 to 4 after 2005. Some believe that Gleason pattern 5 is still underdiagnosed, particularly on needle biopsy, which may prompt some pathologists to call pattern 5 on biopsy more frequently [40]. In particular, the single cell pattern of Gleason grade 5, the most common biopsy pattern 5, may be potentially underdiagnosed and under-reported. Tangentially sectioned small-acinar pattern 3 glands may often exhibit a focal single cell pattern, or even glands with poorly formed lumina can sometimes appear as single cells. Thus, it is not unusual that diagnostic difficulties arise in interpreting single cell patterns. One approach in evaluating areas of possible pattern 5, particularly on biopsy, is to consider the background cancer morphology . If the background cancer demonstrates small-acinar pattern 3 or poorly formed glands, pattern 4, it would be prudent not to call these foci as pattern 5, but to interpret them as part of the background cancer morphology.
The significance of the upward shift of the Gleason grading in clinical practice and for patient management and prognosis is still uncertain. One possible consequence may be possible improvement in future patient outcomes for patients after 2005. This phenomenon of improved outcomes due to tumor grade (or stage) reclassification is well recognized and reflects a statistical artifact, known as the Will Rogers phenomenon [41]. This phenomenon occurs when changes are introduced in a classification system and an intermediate-risk group is moved from a low- to a higher-risk group, which improves the outcomes in both groups. Another possible consequence of the upward Gleason migration may be a change in treatment practices after 2005. Because GS is an important factor in treatment selection (i.e., active surveillance vs. RP), the proportion of patients reported as biopsy GS 6 may now be likely reduced, because their biopsy GS are more likely to be reported currently as GS ≥ 7. This may result in exclusion of some patients from active surveillance . Similarly, in some institutions, only patients reported as GS ≤ 6 on biopsy are considered for brachytherapy, and this patient population may now be also potentially reduced [29]. Pathology reviews of biopsies and RPs on specimens read before 2005 may result in GS regrading by using the modified Gleason , which clinicians and patients may not be aware of or familiar with, thus creating confusion. Thus, pathologists should clearly communicate these changes in review and consult reports and explain to clinicians and patients the reasons for GS upgrade.
Correlation of Gleason Score with Clinical Patient Outcomes
A true validation of the modified Gleason system will be demonstrating its correlation with the clinical outcomes. So far, only a few studies addressed clinical outcomes after 2005, mainly because the follow-up in these studies has been relatively short. Two relatively small studies demonstrated that the GS on needle biopsies using the modified system correlated better with progression after RP [30, 39]. Tsivian et al. found that modified GS, when analyzed in prognostic grade groups (< 7 and > 7), predicted biochemical recurrence after RP better than the original GS groups [42]. Berney et al. reported significant upgrading of biopsies, initially graded during 1990–1996 and subsequently regraded and published in 2007 [36]. Whereas the initial grades did not correlate with survival outcomes , the newly recorded grades, largely following the modified Gleason system, did. In the only study favoring the original over the modified Gleason system in predicting disease progression, Delahunt et al. reported that original Gleason system outperformed the modified system in predicting PSA nadir following external beam radiotherapy and hormone therapy [43]. Unfortunately, the use of PSA nadir, a suboptimal endpoint, limited the significance of the study results. Aiming to establish the risk of adverse outcome for patients with a GS 3 + 3 = 6, subsequently upgraded to GS 7 or 8 using the ISUP modified Gleason system, Dong et al. found that 34 % of patients with classical GS 3 + 3 = 6 prostate cancer were upgraded to modified GS 7 or 8, using the ISUP criteria [37]. Compared to patients with modified GS 3 + 3 = 6 and patients with classical GS 3 + 4 = 7, the upgraded patients were at intermediate risk for biochemical progression and metastasis after RP [37]. Another recent study has shown that presence of cribriform glands, now usually graded pattern 4, was more likely to be associated with biochemical failure [44].
After 2005, some studies also examined the clinical significance of specific prostate carcinoma variants and morphologies. While the early studies of mucinous carcinoma from the pre-PSA era showed adverse outcomes, more recent studies reported no deaths from disease and limited biochemical recurrence in patients with mucinous carcinoma treated by RP [45]. This supports the grading approach based on the architectural configuration, which needs confirmation in larger series. Another study examined glomeruloid features in needle biopsies to establish whether there is an association of this pattern with coexistent high-grade carcinoma [46]. In this study, glomerulations were associated with high-grade cancer on the same core, mostly Gleason pattern 4 (80 % of cases) and often appeared to represent a morphologic transition to larger cribriform glands. Only a minority of glomerulations were found to be associated with pattern 3 cancer (16 % of cases). Despite the limitations and the absence of clinical follow-up, this study supported the idea that glomerulations most likely represent an early stage of cribriform pattern 4 cancer and should be graded as such [46].
One of the most compelling testimonials, so far, of the prognostic ability of the ISUP modified grading system came from a large study from Johns Hopkins, which investigated pathologic and short-term outcomes after the Gleason system modifications in 2005 [38]. This study used multivariable models using preoperative and postoperative variables and demonstrated clearly separate prognostic groups based on GS both on biopsy and RP ( ≤ 6; 3 + 4; 4 + 3; 8; 9–10). These prognostic groups were among the strongest predictors of biochemical recurrence-free survival. Based on their results, they proposed adding a descriptive terminology, designated Prognostic Grade Groups (PGG) I–V: PGG I for GS ≤ 6 (well-differentiated or low-grade), PGG II for GS 3 + 4 (moderately differentiated or intermediate low grade), PGG III for GS 4 + 3 = 7 (moderately–poorly differentiated or intermediate grade), PGG IV for GS 8 (poorly differentiated or high intermediate grade), and PGG V for GS 9–10 (undifferentiated or high grade) [38]. Interestingly, in contrast to previous studies, this study failed to show that adding the tertiary pattern enhanced the predictive value in multivariable analysis, which included a preoperative PSA, pathologic stage, margins, and Gleason grade on RP. Although it is currently recommended that tertiary patterns are noted in pathology reports for accurate grading, this study questioned whether the inclusion of tertiary patterns added significant prognostic information, in addition to the routinely reported parameters.
By adopting a system that starts with GS ≤ 6 to represent a prognostic category 1 (PGG1), one would eliminate the current situation when Gleason grading essentially starts with GS 6. After 2005, GS ≤ 6 category represents a more uniform and homogeneous category, reflecting a better patient prognosis . It has been demonstrated that virtually no pure GS 6 cancers are associated with progression after RP, using the ISUP modified Gleason system, whereas in the original Gleason system this occasionally occurred [47]. Of over 14,000 totally embedded RP from multiple institutions, there was not a single case of GS ≤ 6 cancer with nodal metastasis [48]. Clearly defined prognostic groups would also obviate the need to potentially introduce decimal fractions to individual GS to better stratify patients [18, 49]. The proposals to consider these modifications arose from the fact that 2005 Gleason grading system introduced an upward migration, which required better prognostic separation in the current setting.
Future Perspectives
Although the 2005 ISUP modified grading system is still imperfect and somewhat subjective, there is no other marker or grading system that can be as quickly and reproducibly applied in practice, which underscores the pathologist’s role in patient management. For a pathologist, the key issue remains to use consistent criteria for grading and to be attuned to the general and mainstream grading criteria. A consistent and reproducible grading approach will allow adaptation to future grading modifications. It is also desirable to establish a unified grading approach in a group practice with regular intradepartmental consultations or consultations with a uropathologist.
The 2005 ISUP modified Gleason grading has had an enormous impact on the evolving clinical practice of prostate cancer. It has achieved considerable acceptance and has been widely used. Certainly, further modifications and refinements of the criteria need to be carefully validated and confirmed in large or multi-institutional studies with well-defined outcomes, before additional changes are implemented. The ISUP modified Gleason system still remains one of the most powerful grading schemes in all of urologic oncology and a gold standard against which other prospective markers are and will be compared with and measured against in future studies. Although GS is a fundamental prognostic parameter for prostate cancer, additional biomarkers may either complement or replace GS in the future. Each biomarker aiming to replace Gleason, however, needs to be validated first head-to-head with Gleason in retrospective studies, with subsequent validation in independent and prospective data sets and cohorts.
References
Gleason DF. Classification of prostatic carcinomas. Cancer Chemother Rep. 1966;50(3):125–8.
Gleason DF, Mellinger GT. Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol. 1974;111(1):58–64.
Gleason DF. Histologic grading and clinical staging of prostatic carcinoma. In: Teannenbaum M, editor. Urologic pathology: the prostate. the veterans administration cooperative urological research group. Philadelphia: Lea and Febiger; 1977. pp. 171–97.
Epstein JI, Allsbrook WC Jr., Amin MB, Egevad LL. The 2005 international society of urological pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma. Am J Surg Pathol. 2005;29(9):1228–42.
Gleason DF. Histologic grading of prostate cancer: a perspective. Hum Pathol. 1992;23(3):273–9.
Siegel R, Naishadham D, Jemal A. Cancer statistics. CA Cancer J Clin. 2012;62(1):10–29.
Stamey TA, Caldwell M, McNeal JE, Nolley R, Hemenez M, Downs J. The prostate specific antigen era in the United States is over for prostate cancer: what happened in the last 20 years?. J Urol. 2004;172(4 Pt 1):1297–301.
Egevad L, Mazzucchelli R, Montironi R. Implications of the international society of urological pathology modified Gleason grading system. Arch Pathol Lab Med. 2012;136(4):426–34.
Egevad L, Allsbrook WC, Jr., Epstein JI. Current practice of diagnosis and reporting of prostate cancer on needle biopsy among genitourinary pathologists. Hum Pathol. 2006;37(3):292–7.
Srigley JR, Amin MB, Epstein JI, Grignon DJ, Humphrey PA, Renshaw AA, et al. Updated protocol for the examination of specimens from patients with carcinomas of the prostate gland. Arch Pathol Lab Med. 2006;130(7):936–46.
Berney DM. The case for modifying the Gleason grading system. BJU Int. 2007;100(4):725–6.
Epstein JI. Gleason score 2–4 adenocarcinoma of the prostate on needle biopsy: a diagnosis that should not be made. Am J Surg Pathol. 2000;24(4):477–8.
Epstein JI. An update of the Gleason grading system. J Urol. 2010;183(2):433–40.
Lotan TL, Epstein JI. Clinical implications of changing definitions within the Gleason grading system. Nat Rev Urol. 2010;7(3):136–42.
Latour M, Amin MB, Billis A, Egevad L, Grignon DJ, Humphrey PA, et al. Grading of invasive cribriform carcinoma on prostate needle biopsy: an interobserver study among experts in genitourinary pathology. Am J Surg Pathol. 2008;32(10):1532–9.
Yaskiv O, Cao D, Humphrey PA. Microcystic adenocarcinoma of the prostate: a variant of pseudohyperplastic and atrophic patterns. Am J Surg Pathol. 2010;34(4):556–61.
Pan CC, Potter SR, Partin AW, Epstein JI. The prognostic significance of tertiary Gleason patterns of higher grade in radical prostatectomy specimens: a proposal to modify the Gleason grading system. Am J Surg Pathol. 2000;24(4):563–9.
Trock BJ, Guo CC, Gonzalgo ML, Magheli A, Loeb S, Epstein JI. Tertiary Gleason patterns and biochemical recurrence after prostatectomy: proposal for a modified Gleason scoring system. J Urol. 2009;182(4):1364–70.
Mosse CA, Magi-Galluzzi C, Tsuzuki T, Epstein JI. The prognostic significance of tertiary Gleason pattern 5 in radical prostatectomy specimens. Am J Surg Pathol. 2004;28(3):394–8.
Isbarn H, Ahyai SA, Chun FK, Budaus L, Schlomm T, Salomon G, et al. Prevalence of a tertiary Gleason grade and its impact on adverse histopathologic parameters in a contemporary radical prostatectomy series. Eur Urol. 2009;55(2):394–401.
Ikenberg K, Zimmermann AK, Kristiansen G. Re: tertiary Gleason patterns and biochemical recurrence after prostatectomy: proposal for a modified Gleason scoring system. Trock BJ, Guo CC, Gonzalgo ML, Magheli A, Loeb S, Epstein JI. J Urol 2009;182:1364–1370. J Urol. 2010;183(5):2100. Author reply-1.
Patel AA, Chen MH, Renshaw AA, D’Amico AV. PSA failure following definitive treatment of prostate cancer having biopsy Gleason score 7 with tertiary grade 5. JAMA. 2007;298(13):1533–8.
Nanda A, Chen MH, Renshaw AA, D’Amico AV. Gleason Pattern 5 prostate cancer: further stratification of patients with high-risk disease and implications for future randomized trials. Int J Radiat Oncol Biol Phys. 2009;74(5):1419–23.
Trpkov K, Zhang J, Chan M, Eigl BJ, Yilmaz A. Prostate cancer with tertiary Gleason pattern 5 in prostate needle biopsy: clinicopathologic findings and disease progression. Am J Surg Pathol. 2009;33(2):233–40.
Rubin MA, Dunn R, Kambham N, Misick CP, O’Toole KM. Should a Gleason score be assigned to a minute focus of carcinoma on prostate biopsy? Am J Surg Pathol. 2000;24(12):1634–40.
Donnelly BJ, Saliken JC, Brasher PM, Ernst SD, Rewcastle JC, Lau H, et al. A randomized trial of external beam radiotherapy versus cryoablation in patients with localized prostate cancer. Cancer. 2010;116(2):323–30.
Zelefsky MJ, Reuter VE, Fuks Z, Scardino P, Shippy A. Influence of local tumor control on distant metastases and cancer related mortality after external beam radiotherapy for prostate cancer. J Urol. 2008;179(4):1368–73; discussion 73.
Helpap B, Egevad L. The significance of modified Gleason grading of prostatic carcinoma in biopsy and radical prostatectomy specimens. Virchows Arch. 2006;449(6):622–7.
Zareba P, Zhang J, Yilmaz A, Trpkov K. The impact of the 2005 international society of urological pathology (ISUP) consensus on Gleason grading in contemporary practice. Histopathology. 2009;55(4):384–91.
Uemura H, Hoshino K, Sasaki T, Miyoshi Y, Ishiguro H, Inayama Y, et al. Usefulness of the 2005 international society of urologic pathology Gleason grading system in prostate biopsy and radical prostatectomy specimens. BJU Int. 2009;103(9):1190–4.
Epstein JI, Feng Z, Trock BJ, Pierorazio PM. Upgrading and downgrading of prostate cancer from biopsy to radical prostatectomy: incidence and predictive factors using the modified Gleason grading system and factoring in tertiary grades. Eur Urol. 2012;61(5):1019–24.
Rubin MA, Bismar TA, Curtis S, Montie JE. Prostate needle biopsy reporting: how are the surgical members of the Ssociety of urologic oncology using pathology reports to guide treatment of prostate cancer patients? Am J Surg Pathol. 2004;28(7):946–52.
Griffiths DF, Melia J, McWilliam LJ, Ball RY, Grigor K, Harnden P, et al. A study of Gleason score interpretation in different groups of UK pathologists; techniques for improving reproducibility. Histopathology. 2006;48(6):655–62.
Melia J, Moseley R, Ball RY, Griffiths DF, Grigor K, Harnden P, et al. A UK-based investigation of inter-and intra-observer reproducibility of Gleason grading of prostatic biopsies. Histopathology. 2006;48(6):644–54.
Lopez-Beltran A, Mikuz G, Luque RJ, Mazzucchelli R, Montironi R. Current practice of Gleason grading of prostate carcinoma. Virchows Arch. 2006;448(2):111–8.
Berney DM, Fisher G, Kattan MW, Oliver RT, Moller H, Fearn P, et al. Major shifts in the treatment and prognosis of prostate cancer due to changes in pathological diagnosis and grading. BJU Int. 2007;100(6):1240–4.
Dong F, Wang C, Farris B, Wu S, Lee H, Olumi AF, et al. Impact on the clinical outcome of prostate cancer by the 2005 international society of urological pathology modified Gleason grading system. Am J Surg Pathol. 2012:36(6):838–43.
Pierorazio PM, Walsh P, Partin A, Epstein J. Prognostic Gleason grade grouping: data based on the modified Gleason scoring system. BJU Int. 2013;111(5):753–60.
Billis A, Guimaraes MS, Freitas LL, Meirelles L, Magna LA, Ferreira U. The impact of the 2005 international society of urological pathology consensus conference on standard Gleason grading of prostatic carcinoma in needle biopsies. J Urol. 2008;180(2):548–52; discussion 52–3.
Fajardo DA, Miyamoto H, Miller JS, Lee TK, Epstein JI. Identification of Gleason pattern 5 on prostatic needle core biopsy: frequency of underdiagnosis and relation to morphology. Am J Surg Pathol. 2011;35(11):1706–11.
Albertsen PC, Hanley JA, Barrows GH, Penson DF, Kowalczyk PD, Sanders MM, et al. Prostate cancer and the Will Rogers phenomenon. J Natl Cancer Inst. 2005;97(17):1248–53.
Tsivian M, Sun L, Mouraviev V, Madden JF, Mayes JM, Moul JW, et al. Changes in Gleason score grading and their effect in predicting outcome after radical prostatectomy. Urology. 2009;74(5):1090–3.
Delahunt B, Lamb DS, Srigley JR, Murray JD, Wilcox C, Samaratunga H, et al. Gleason scoring: a comparison of classical and modified (international society of urological pathology) criteria using nadir PSA as a clinical end point. Pathology. 2010;42(4):339–43.
Iczkowski KA, Torkko KC, Kotnis GR, Wilson RS, Huang W, Wheeler TM, et al. Digital quantification of five high-grade prostate cancer patterns, including the cribriform pattern, and their association with adverse outcome. Am J Clin Pathol. 2011;136(1):98–107.
Osunkoya AO, Nielsen ME, Epstein JI. Prognosis of mucinous adenocarcinoma of the prostate treated by radical prostatectomy: a study of 47 cases. Am J Surg Pathol. 2008;32(3):468–72.
Lotan TL, Epstein JI. Gleason grading of prostatic adenocarcinoma with glomeruloid features on needle biopsy. Hum Pathol. 2009;40(4):471–7.
Miyamoto H, Hernandez DJ, Epstein JI. A pathological reassessment of organ-confined, Gleason score 6 prostatic adenocarcinomas that progress after radical prostatectomy. Hum Pathol. 2009;40(12):1693–8.
Ross HM, Kryvenko ON, Cowan JE, Simko JP, Wheeler TM, Epstein JI. Do adenocarcinomas of the prostate with Gleason score (GS) < / = 6 have the potential to metastasize to lymph nodes? Am J Surg Pathol. 2012;36(9):1346–52.
Reese AC, Cowan JE, Brajtbord JS, Harris CR, Carroll PR, Cooperberg MR. The quantitative Gleason score improves prostate cancer risk assessment. Cancer. 2012;118(24):6046–54.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Trpkov, K. (2015). Contemporary Gleason Grading System. In: Magi-Galluzzi, C., Przybycin, C. (eds) Genitourinary Pathology. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2044-0_2
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2044-0_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2043-3
Online ISBN: 978-1-4939-2044-0
eBook Packages: MedicineMedicine (R0)