Abstract
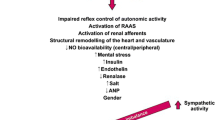
Hypertension is very prevalent among patients with chronic kidney disease (CKD) and it is commonly refractory to treatment. Several mechanisms contribute to hypertension in these patients, including volume expansion and activation of the renin–angiotensin–aldosterone system. This chapter deals with the role of the sympathetic nervous system in hypertension and CKD progression in these patients and with the mechanisms that can contribute to the activation of the sympathetic nervous system, including angiotensin II, increased oxidative stress, and renalase. Finally, this chapter reviews the current role of renal denervation in the management of hypertension in these patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Hypertension is very prevalent among patients with chronic kidney disease (CKD) and it becomes more frequent as patients progress towards end-stage renal disease (ESRD) . Approximately 85 % of patients with ESRD have hypertension, which is in large part responsible for the high incidence of cardiovascular events and deaths in these patients. Hypertension is also a major contributor to the progression of kidney disease.
The pathogenesis of hypertension in patients with kidney diseases is multifactorial and may vary depending on the underlying renal disease. Several factors have been implicated in the pathogenesis of hypertension in CKD. In this chapter, we focus on the evidence that activation of the sympathetic nervous system (SNS) may play a major role in the pathogenesis of hypertension, as well as cardiovascular disease and progression of kidney disease in this patient population.
Evidence for Neurogenic Factors in Hypertension Associated with Kidney Disease
The kidney is not only an elaborate filtering device but also a sensory organ, richly innervated with sensory and afferent nerves. There are two main functional types of renal sensory receptors and afferent nerves: renal baroreceptors , which are activated by changes in renal perfusion and intrarenal pressure; and renal chemoreceptors, which are stimulated by ischemic metabolites or toxins [1, 2]. In rats, these “chemoceptive” receptors are further classified into R1 and R2 based on their resting level of activity and the types of stimuli that elicit a response. The activation of these chemosensitive receptors may, through the renal afferent nerves, establish connections with integrative nuclei of the SNS in the central nervous system [3, 4]. In experimental animals, stimulation of these afferent nerves by either ischemic metabolites such as adenosine, or by urea, evokes reflex increases in efferent sympathetic nerve activity and increased blood pressure (BP) [5].
Our studies on 5/6 nephrectomized (5/6 Nx) rats have provided the most convincing evidence yet for a role of the SNS in the pathogenesis of hypertension associated with 5/6 Nx. The turnover rate [6] and the secretion of norepinephrine (NE) [7] from the posterior hypothalamic (PH) nuclei were greater in 5/6 Nx than in control rats. Bilateral dorsal rhizotomy at the level T-10 to L-3 prevented the increase in BP, the increase in NE turnover in the PH. Evidence also suggest that increased SNS activity may contribute to the progression of kidney disease in rats [8]. These studies led us to postulate that increased renal sensory impulses generating in the affected kidney and then transmitted to the central nervous system activate regions of the brain involved in the noradrenergic control of BP resulting in hypertension.
The notion that kidney injury may lead to activation of the SNS and to hypertension, independently from changes in glomerular filtration rate (GFR), is supported by our studies in the phenol-kidney injury model. In this model, hypertension is caused by injecting 50 μL of 10 % phenol in the lower pole of one kidney. This leads to an immediate elevation of NE secretion from the PH nuclei and a rise in BP that persists at least for 6 weeks after the kidney injury [9]. Renal denervation prevents the rise in NE secretion from the PH nuclei and the rise in BP caused by phenol injection. Serum creatinine did not change after the intrarenal administration of phenol indicating that this model of hypertension does not cause any apparent change in kidney function. These studies have demonstrated that a specific injury to a limited portion of the kidney may cause a permanent elevation of BP in the rat. Hypertension in this model is mediated by neurogenic mechanisms.
The potential importance of this observation is substantial, since clinical experience indicates that not all renal injuries in humans are associated with hypertension. For example, in the absence of renal insufficiency, immunoglobulin A (IgA) nephropathy is more likely to be associated with hypertension than membranous glomerulonephritis or minimal change disease. In addition, it is plausible to expect that not all forms of hypertension associated with kidney disease are due to SNS activation. As a consequence, it is naïve to expect clinical benefits from renal denervation in all forms of hypertension associated with kidney disease.
Both direct and indirect evidence implicates increased SNS activity in the pathogenesis of hypertension in patients with CKD [10–13]. Plasma NE levels are usually increased in hemodialysis patients [14], but these levels, whether measured before or post dialysis, are poorly correlated with levels of BP [15, 16]. Direct recording of neuronal activity from postganglionic sympathetic fibers in the peroneal nerves of ESRD patients have shown a greater rate of sympathetic nerve discharge than in control subjects. Converse et al. [17] observed increased muscle SNS activity (MSNA) and peripheral vascular resistance in hypertensive patients with ESRD. By contrast, patients with bilateral nephrectomy manifested lower MSNA, BP, and peripheral vascular resistance compared to patients with native kidneys. Ligtenberg et al. observed an increase in muscle SNS discharge in CKD, when compared with age- and weight-matched control [18]. Klein et al. [19] observed increased muscle sympathetic nerve activity in hypertensive patients with polycystic kidney disease regardless of kidney function. Activation of renal afferents appears also to be the primary mechanism for calcineurin inhibitors-induced hypertension in rats [20, 21].
Other mechanisms potentially responsible for the increase in sympathetic nerve activity in CKD patients include reduced central dopaminergic tone [22]. Hypertensive patients with CKD have a heightened DOPA and dopamine sulfoconjugating propensity, and dopamine sulfate attenuates the biologic action of free dopamine. The increase in sympathetic activity in CKD could also be due to reduced baroreceptors sensitivity [23], abnormal vagal function [24], increased intracellular calcium concentration [25], and increased plasma β-endorphin and β-lipotropin [26]. Increased neuropeptide Y in response to fluid overload may also participate to hypertension in ESRD [27].
Effects of Angiotensin II and Oxidative Stress on Central SNS Activation
Substantial evidence indicates that angiotensin II (Ang II) enhances sympathetic nerve (SNS) activity centrally and peripherally [28, 29]. Intracerebroventricular infusion of Ang II raises BP, renal sympathetic nervous system activity (RSNA), and NE secretion from the PH nuclei [30]. As a consequence, the anti-hypotensive effects of angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) could be in part related to inhibition of the SNS. ACE inhibitors reduce peripheral sympathetic nerve activity in patients with chronic renal failure (18). Similarly, AT-1 receptor blockers reduced central SNS activity in a model of neurogenic hypertension caused by renal injury [31].
The effects of Ang II on BP are mediated in part by reactive oxygen species (ROS). Infusion of Ang II into rats is associated with increased vascular superoxide production. Ang II stimulates oxidative stress through nicotinamide adenine dinucleotide/nicotinamide adenine dinucleotide phosphate (NADH/NADPH)-oxidase activation, and chronic infusion of Ang II raises the concentration of oxidative markers [21]. Antioxidants, such as tempol and vitamin E, prevent Ang II-induced hypertension in rats .
Limited data are available concerning the effects of Ang II on oxidative stress in the brain and the role this might play in SNS-mediated regulation of cardiovascular function. Zimmerman et al. [32] observed that the effects of intracerebroventricular Ang II on BP and heart rate were abolished by pretreatment with AsSOD in mice. Zanzinger et al. [33] showed that removal of extracellular superoxide or reactive nitrogen species within the rostral ventrolateral medulla by microinjection of SOD reduced SNS activity. We have shown that SOD mimetics administered intracerebroventricularly abrogate the effects of Ang II on BP and SNS activity, supporting the hypothesis that the effects of Ang II on central SNS activation are mediated by increased oxidative stress in brain regions involved in the noradrenergic control of BP [34] .
Effects of Nitric Oxide on SNS Activity
Nitric oxide synthase (NOS) is present in a specific area of the brain involved in the neurogenic control of BP and the cardiovascular system, and it is an important component of transduction pathways that tonically inhibits SNS activity [35, 36].
Vaziri et al. [37] observed downregulation of endothelial and inducible NOS in 5/6 NPX rats, and suggested that this may contribute to BP elevation. Reduced availability of NO in the brain could result in increased SNS activity and in hypertension.
Asymmetric dimethylarginine (ADMA) is an endogenous inhibitor of nitric oxide (NO) synthases that inhibits NO synthesis and may result in endothelial dysfunction, vasoconstriction, and elevation of BP [38]. ADMA blood levels are significantly elevated in CKD and ESRD patients suggesting that ADMA may contribute to hypertension [39, 40], increased SNS activity, atherosclerosis [41], and mortality [42] in these patients .
The Role of Renalase
Renalase is a flavin adenine dinucleotide-dependent amine oxidase highly expressed in the kidney and heart [43]. It metabolizes catecholamines and catecholamine-like substances via a superoxide (O2(–))-dependent mechanism using NADH as a cofactor [44]. Renalase infusion in rats caused a decrease in cardiac contractility, heart rate, and BP and prevented a compensatory increase in peripheral vascular tone . In humans, renalase gene expression is highest in the kidney but is also detectable in the heart, skeletal muscle, and the small intestine. The plasma concentration of renalase is markedly reduced in patients with ESRD as compared with healthy subjects. This raises the possibility that the reduced secretion of renalase in CKD may contribute to increased SNS activity and hypertension [45]. Schlaich et al. measured serum renalase levels in 22 patients with resistant hypertension and observed an inverse relationship between renalase levels and SBP [46].
Some studies have evaluated the relationship between polymorphisms in the renalase (RNLS) gene and BP levels by examining several single nucleotide polymorphisms (SNPs) of RNLS.7 In more than 2000 individuals from the International Collaborative Study of Cardiovascular Disease in Asia (InterASIA in China), Zhao et al. [47] observed that two SNPs (rs2576178 A > G and rs2296545 C > G) were associated with essential hypertension .
In one Chinese population-based study, the G allele of the rs2576178 SNP was associated with hypertension among hemodialysis patients (odds ratio (OR), 1.76; P¼0.008) [48]. In a cohort of 590 Caucasian participants with stable coronary artery disease, the CC genotype (for the rs2296545 SNP) was associated with cardiovascular phenotypes such as cardiac hypertrophy, dysfunction, and ischemia but not with BP [49]. By contrast, the same polymorphisms were genotyped in 5696 participants of the population-based Cardiovascular Cohort of the “Malmö Diet and Cancer” (MDC-CC). Before and after adjustment for major cardiovascular risk factors , the hazard ratio for cardiac and cerebrovascular events was not significantly different in carriers of different genotypes [50] .
Renal Denervation in CKD
In recent years, renal nerve ablation has been utilized with some success in the management of patients with resistant hypertension [51] . However, the frequency and extent of success is still disputed [52].
Given the strong scientific evidence for increased SNS activity particularly in patients with CKD, renal denervation is expected to be useful in this group of patients. However, the evidence so far is quite limited. In one study, the researchers performed renal denervation using radiofrequency waves on 15 patients with resistant hypertension and stage III or IV CKD [53].
The average BP of the patients at the start of the study was 174 ± 22/91 ± 16 mmHg, despite the use of 5.6 ± 1.3 antihypertensive drugs. After the procedure, the average change in office systolic and diastolic BP at 1, 3, 6, and 12 months was − 34/− 14, − 25/− 11, − 32/− 15, and − 33/− 19 mmHg, respectively .
The average nighttime systolic BP had decreased, after 3 months, from 154 ± 16 to 140 ± 22 mmHg (P = 0.03) and was 144 ± 22 mmHg after 6 months. After the procedure, nighttime diastolic BP declined at 3 months (78 ± 11 vs. 70 ± 8 mmHg) and 6 months (78 ± 11 vs. 75 ± 14 mmHg; P = 0.02; Fig. 4.1) .
Office BP values at follow-up. Changes in average office BP (a) and mean decrease in office BP (b) at follow-up. Error bars represent SDs. *P < 0.001 versus baseline (before the procedure). FU follow-up, M month, pre-RDN prerenal denervation. (Reprinted from [53]. With permission from the American Society of Nephrology)
Some concerns of this methodology specifically for CKD patients have to considered. First, in patients with low GFR renal blood flow can be particularly reduced. Since cooling of the catheter tip depends decisively on the blood flow, thermal problems might occur increasing the potential for damage of the renal blood vessels. Second, the procedure requires substantial amounts of contrast media raising the risk of acute kidney injury in these patients. Of interest, Hering et al. observed no deterioration in renal function over the course of the study in CKD patients.
The Simplicity Study III, a randomized controlled study, failed to demonstrate a beneficial effect of renal denervation on BP in a large group of patients with resistant hypertension [54]. Given these unimpressive results, the role of renal denervation in the management of resistant hypertension, particularly in CKD patients, remains to be established. Several issues need to be resolved: first, how to identify patients with increased renal sympathetic nerve activity , who may be more suitable for renal denervation; second, to what extent and with what variability renal denervation is achieved with the Simplicity catheter by various investigators; third, the issue of regeneration of renal nerves after denervation remains unresolved. Until all these issues are satisfactorily resolved, renal denervation should remain an experimental tool in the management of hypertension associated with kidney disease .
References
Recordati G, Moss NG, Genovisi S, Rogenes P. Renal chemoreceptors. J Auton Nerv Syst. 1981;3:237–51.
Katholi RE. Renal nerves and hypertension: an update. Fed Proc. 1985;44:2846–50.
Faber JE, Brody MJ. Afferent renal nerve-dependent hypertension following acute renal artery stenosis in the conscious rat. Circ Res. 1985;57:676–88.
Calaresu FR, Ciriello J. Renal afferent nerves affect discharge rate of medullary and hypothalamic single uits in cat. J Auton Nerv Syst. 1981;3:311–20.
Katholi RE, Whitlow PL, Hageman GR, Woods T. Intrarenal adenosine produces hypertension by activating the sympathetic nervous system via the renal nerves. J Hypertens. 1984;2:349–59.
Bigazzi R, Kogosov E, Campese VM. Altered norepinephrine turnover in the brain of rats with chronic renal failure. J Am Soc Nephrol. 1994;4:1901–7.
Ye S, Ozgur B, Campese VM. Renal afferent impulses, the posterior hypothalamus, and hypertension in rats with chronic renal failure. Kidney Int. 1997;51:722–7.
Campese VM, Kogosov E, Koss M. Renal afferent denervation prevents the progression of renal disease in the renal ablation model of chronic renal failure in the rat. Am J Kidney Dis. 1995;26:861–5.
Ye S, Gumburd M, Campese VM. An acute renal injury may cause a permanent form of neurogenic hypertension. Am J Hypertens. 1998;11:723–8.
Lake CR, Ziegler MG, Coleman MD, Kopin IJ. Plasma levels of norepinephrine and dopamine-beta-hydroxylase in CRF patients treated with dialysis. Cardiovasc Med. 1979;1:1099–111.
Henrich WL, Katz FH, Molinoff PB, Schrier RW. Competitive effects of hypokalemia and, depletion on plasma renin activity, aldosterone and catecholamine concentrations in hemodialysis patients. Kidney Int. 1977;12:279–84.
Lzzo JL, Izzo MS, Sterns RH, Freeman RB. Sympathetic nervous system hyperactivity in maintenance hemodialysis patients. Trans Am Soc Artif Intern Organs. 1982;28:604–7.
Ishii M, Ikeda T, Takagi M. Elevated plasma catecholamines in hypertensives with primary glomerular diseases. Hypertension. 1983;5:545–51.
Cuche JL, Prinseau J, Selz F, Ruget G, Baglin A. Plasma free, sulfo- and glucuro-conjugated catecholamines in uremic patients. Kidney Int. 1986;30:566–72.
Campese VM, Romoff MS, Levitan D, Lane K, Massry SG. Mechanisms of autonomic nervous system dysfunction in uremia. Kidney Int. 1981;20:246–53.
Grekas D, Kalevrosoglou I, Karamouzis M, et al. Effects of sympathetic and plasma renin activity on hemodialysis hypertension. Clin Nephrol. 2001;55:115–20.
Converse RL Jr, Jacobsen TN, Toto RD, et al. Sympathetic overactivity in patients with chronic renal failure. N Engl J Med. 1992;327:1912–8.
Ligtenberg G, Blankestijn PJ, Oey PL, Klein IH, et al. Reduction of sympathetic hyperactivity by enalapril in patients with chronic renal failure. N Engl J Med. 1999;340:1321–8.
Klein IHHT, Ligtenberg G, Oey PL, Koomans HA, Blankestijn PJ. Sympathetic activity is increased in polycystic kidney disease and is associated with hypertension. J Am Soc Nephrol. 2001;12:2427–33.
Moss NG, Powell SL, Falk RJ. Intravenous cyclosporine activates afferent and efferent renal nerves and causes sodium retention in innervated kidneys in rats. Proc Natl Acad Sci U S A. 1985;82:8222–6.
Zhang W, Victor RG. Calcineurin inhibitors cause renal afferent activation in rats: a novel mechanism of cyclosporine-induced hypertension. Am J Hypertens. 2000;13:999–1004.
Kuchel OG, Shigetomi S Dopaminergic abnormalities in hypertension associated with moderate renal insufficiency. Hypertension. 1994;23(Suppl. 1):I240−5.
Pickering TG, Gribbin B, Oliver DO. Baroreflex sensitivity in patients on long-term hemodialysis. Clin Sci. 1972;43:645–7.
Zucchelli P, Catizone L, Degli Esposti E, Fusaroli M, Ligabue A, Zuccala A. Influence of ultrafiltration on plasma renin activity and adrenergic system. Nephron. 1978;21:317–24.
Zimlichman RR, Chaimovitz C, Chaichenco Y, Goligorski M, et al. Vascular hypersensitivity to noradrenaline: a possible mechanism of hypertension in rats with chronic uremia. Clin Sci (Lond). 1984;67:161–6.
Elias AN, Vasiri ND. Plasma catecholamines in chronic renal disease. Int J Artif Org. 1985;8:243–4.
Odar-Cederlof I, Ericsson F, Theodorsson E, Kjellstrand CM. Is neuropeptide Y a contributor to volume-induced hypertension? Am J Kidney Dis. 1998;31:803–8.
Ferrario CM, Gildenberg PL, McCubbin JW. Cardiovascular effects of angiotensin mediated by the central nervous system. Circ Res. 1972;30:257–62.
DiBona GF. Nervous kidney. Interaction between renal sympathetic nerves and the renin-angiotensin system in the control of renal function. Hypertension. 2000;36:1083–8.
Campese VM, Ye S, Zhong H Downregulation of nNOS and interleukin-1β mediates angiotensin II-dependent stimulation of sympathetic nerve activity. Hypertension. 2002;39(Suppl. II):519–24.
Ye S, Zhong H, Duong VN, Campese VM. Losartan reduces central and peripheral sympathetic nerve activity in a rat model of neurogenic hypertension. Hypertension. 2002;39:1101–6.
Zimmerman MC, Lazartigues E, Lang JA, Sinnayah P, Ahmad IM, Spitz DR, Davisson RL. Superoxide mediates the actions of angiotensin II in the central nervous system. Circ Res. 2002;91:1038–54.
Zanzinger J, Czachurski J. Chronic oxidative stress in the RVLM modulates sympathetic control of circulation in pigs. Pflugers Arch. 2000;439:489–94.
Campese VM, Ye S, Zhong H. Oxidative stress mediates angiotensin II-dependent stimulation of sympathetic nerve activity. Hypertension. 2005;46:533–9.
Ye S, Mozayeni P, Gamburd M, Zhong H, Campese VM. Interleukin-1β and neurogenic control of blood pressure in normal rats and rats with chronic renal failure. Am J Physiol Heart Circ Physiol. 2000;279:H2786–96.
Ye S, Nosrati S, Campese VM. Nitric oxide (NO) modulates the neurogenic control of blood pressure in rats with chronic renal failure. J Clin Invest. 1997;99:540–8.
Vaziri ND, Ni Z, Wang XQ, et al. Downregulation of nitric oxide synthase in chronic renal insufficiency: role of excess PTH. Am J Physiol. 1998;274:F642–9.
Schwedhelm E, Boger RH. The role of asymmetric and symmetric dimethylarginines in renal disease. Nat Rev Nephrol. 2011;7:275–85.
Anderstam B, Katzarski K, Bergstrom J. Serum levels of NG NG-dimethyl-Larginine, a potential endogenous nitric oxide inhibitor in dialysis patients. J Am Soc Nephrol. 1997;8:1437–42.
Vallance P, Leone A, Calver A, et al. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet. 1992;339:572–5.
Kielstein JT, Boger RH, Bode-Boger SM, et al. Asymmetric dimethylarginine plasma concentrations differ in patients with end-stage renal disease: relationship to treatment method and atherosclerotic disease. J Am Soc Nephrol. 1999;10:594–600.
Zoccali C, Bode-Boger S, Mallamaci F, et al. Plasma concentration of asymmetrical dimethylarginine and mortality in patients with end-stage renal disease: a prospective study. Lancet. 2001;358:2113–7.
Xu J, Li G, Wang P, Velazquez H, Yao X, Li Y, Wu Y, Peixoto A, Crowley S, Desir GV. Renalase is a novel, soluble monoamine oxidase that regulates cardiac function and blood pressure. J Clin Invest. 2005;115:1275–80.
Desir GV, Wang L, Peixoto AJ. Human renalase: a review of its biology, function, and implications for hypertension. J Am Soc Hypertens. 2012;6(6):417–26.
Malyszko J, Koc-Zorawska E, Malyszko JS, Kozminski P, Zbroch E, Mysliwiec M. Renalase, stroke, and hypertension in hemodialyzed patient. Ren Failure. 2012;34(6):727–31.
Schlaich M, Socratous F, Eikelis N, Chopra R, Lambert G, Hennebry S. Renalase plasma levels are associated with systolic blood pressure in patients with resistant hypertension [abstract]. J Hypertens. 2010;28:e437.
Zhao Q, Fan Z, He J, Chen S, Li H, Zhang P, Wang L, Hu D, Huang J, Qiang B, Gu D. Renalase gene is a novel susceptibility gene for essential hypertension: a two-stage association study in northern Han Chinese population. J Mol Med (Berl). 2007;85:877–85.
Stec A, Semczuk A, Furmaga J, Ksiazek A, Buraczynska M. Polymorphism of the renalase gene in end-stage renal disease patients affected by hypertension. Nephrol Dial Transplant. 2012;27(11):4162–6. doi:10.1093/ndt/gfr293 [published online ahead of print May 26, 2011].
Farzaneh-Far R, Desir GV, Na B, Schiller NB, Whooley MA. A functional polymorphism in renalase (Glu37Asp) is associated with cardiac hypertrophy, dysfunction, and ischemia: data from the heart and soul study. PLoS ONE. 2010;5:e13496.
Fava C, Montagnana M, Danese E, Sjögren M, Almgren P, Engström G, Hedblad B, Guidi GC, Minuz P, Melander O. The renalase Asp37Glu polymorphism is not associated with hypertension and cardiovascular events in an urban-based prospective cohort: the Malmö diet and cancer study. BMC Med Genet. 2012;13:57.
Krum H, Schlaich MP, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009;373:1275–81.
Campese VM. Interventional hypertension: a new hope or a new hype? The need to redefine resistant hypertension. J Hypertens. 2013;31:2118–22.
Hering D, Mahfoud F, Walton AS, Krum H, Lambert GW, et al. Renal denervation in moderate to severe CKD. J Am Soc Nephrol. 2012;23:1250–7. doi:10.1681/ASN.2011111062.
Medtronic announces U.S. renal denervation pivotal trial fails to meet primary efficacy endpoint while meeting primary safety endpoint. Press Release, Minneapolis: medtronic; January 9, 2014 6:00 AM CT.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Campese, V. (2015). Neurogenic Factors in Hypertension Associated With Chronic Kidney Disease. In: Weir, M., Lerma, E. (eds) Chronic Kidney Disease and Hypertension. Clinical Hypertension and Vascular Diseases. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1982-6_4
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1982-6_4
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1981-9
Online ISBN: 978-1-4939-1982-6
eBook Packages: MedicineMedicine (R0)