Abstract
Chronic kidney disease (CKD) is a very prevalent disease which encounters a huge all-cause and cardiovascular mortality. Several risk factors were assessed during time in an attempt to decrease the mortality of renal patients; left ventricular hypertrophy, anemia, mineral metabolism disturbance, inflammation, endothelial dysfunction are among them. However, in 2013 we still have an enormous mortality rate. In this context, we tried to define newer risk factors which could be used for improving the enormous morbidity and mortality risk. The best-characterized CKD model patient has hypertension (HTN) and often resistant HTN, high prevalence of arrhythmias, and sudden cardiac death infraclinic overhydration, obesity, and frequently apnea sleep syndrome.
In this chapter, we have tried to summarize the most important data, currently available on obesity, metabolic syndrome, and obstructive sleep apnea (OSA), focusing especially on the impact of these diseases in the outcome of CKD patients. Several therapeutic strategies are presented, being kept only those which can improve the quality of life and the survival of our patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Chronic kidney disease (CKD) patient’s exhibit elevated rates of deaths compared to the general population [1], with almost similar increase in proportion of cardiovascular (CV) and non-CV deaths [1]; however, the CV mortality risk in patients starting dialysis is much higher compared to the general population (unstandardized CV risk—15-fold higher/age-standardized CV risk—almost 9-fold higher than in matched individuals from the general population) [1]. This huge mortality risk is not determined by the same classical, traditional risk factors; indeed, classical atherosclerotic disease is not the most important and common cause of death in a modern dialysis population. Analysis traditional CV risk factor (like hypertension (HTN), diabetes, or lipids) interventions in CKD has been disappointing. Over the past decade, numerous nontraditional risk factors have been investigated: left ventricular hypertrophy, anemia, mineral metabolism disturbance (phosphate, calcium, vascular calcification or FGF-23), inflammation, electrolyte shifts during hemodialysis (HD) or abnormalities in myocardial ultrastructure and function, including endothelial dysfunction, interstitial fibrosis, impaired coronary flow reserve, and diminished ischemia tolerance, but the results were equally disappointing [2]. In 2013, we still have an enormous mortality rate.
In this context, a new approach would be interesting to be considered. We summarize what is so special about CKD patients and then discuss how these particularities can be used for improving the enormous morbidity and mortality risk.
A “typical” CKD patient has:
-
a.
HTN—gradually increasing with the severity of CKD (35.8 % in CKD stage 1, 48.1 % in CKD stage 2, 59.9 % in CKD stage 3, and 84.1 % in CKD stage 4–5)
-
b.
Resistant HTN
-
c.
High prevalence of nondipping HTN even in patients with early impairment of GFR
-
d.
Overhydration, subclinical in almost 25 % of the cases, secondary volume-dependent HTN, left ventricular hypertrophy and death
-
e.
Autonomous dysfunction associated with impaired heart rate variability, resting tachycardia, exercise intolerance, abnormal blood pressure regulation and orthostatic hypotension
-
f.
High prevalence of arrhythmias and sudden cardiac death
-
g.
High prevalence of sleep apnea syndrome
Coming back to the issue, the best-characterized CKD model patient has HTN, infraclinic overhydration, obesity, and frequently apnea sleep syndrome.
Obesity and Metabolic Syndrome in CKD
Obesity is an extremely important problem in 2014, with an increasing trend in prevalence; in 2008, more than 1.4 billion adults of age 20 years and older were overweight, and the number is still growing [3]. In CKD patients, obesity is common [4] . The appropriate methodology used for correct classification of obesity is still debated [5]; although body mass index (BMI) is used by almost all nutritional guidelines, it provides an inadequate estimation of true fat mass, especially in patients with gross imbalances of fluid balance, such as kidney disease patients. The waist to hip ratio (WHR) and skinfold thickness seem to be better methods for a correct estimation of obesity [5].
The consensus definition for metabolic syndrome (MetS) encloses central obesity, elevated BP, dyslipidemia (low levels of high-density lipoprotein (HDL) cholesterol and elevated serum triglycerides), and elevated fasting glucose (impaired fasting glucose or type 2 diabetes) .
Obesity/MetS and CKD Stage 3–5
In predialysis CKD population, MetS is highly prevalent (60–65 %) [6], most probably secondary to a higher prevalence of the individual risk factors for metabolic syndrome in these patients .
MetS was independently associated with proteinuria and CKD progression in numerous observational studies. However, this evidence is still controversial. In the secondary analysis of the African American Study of Kidney Disease and Hypertension Trial [7], MetS was associated with a 31 % of increased risk of CKD progression to end-stage renal disease (ESRD) , but this risk was no longer significant when adjusted for baseline proteinuria. In another recent study, Lee et al. [8] found that the influence of MetS on CKD progression was major only in nondiabetic early stage (1–3) CKD subjects, and became nonsignificant in late-stage CKD and in diabetic (early or late) CKD patients. More recently, Navaethan et al. found in a large and retrospective observational study including 25,868 patients with stage 3–4 CKD an independent association between MetS and ESRD [9]; the subgroup analysis showed that the association between MetS and ESRD was attenuated and no longer statistically significant with adjustment for proteinuria. In this context, in a recent editorial comment, Lea J. suggests that proteinuria could play a central role in the potential impact of MetS on CKD progression [9].
The individual components of MetS were also associated with CKD progression. High-grade obesity is a well-recognized risk factor; this association appears to be stronger in females; the effect could be a direct one, obesity causing glomerular hyperfiltration, activation of the renin–angiotensin system, insulin resistance, and direct lipotoxicity or indirectly, obesity leading to comorbidities, such as type 2 diabetes, HTN, and atherosclerosis, which in turn may accelerate progression of CKD [10]. Even in dialysis patients, obesity was associated with the loss of the residual renal function.
The relationship between obesity and survival is a subject of controversy. In a large study [9], MetS was not linked with an increased risk of death in CKD stage 3–5 patients (individual components, such as low HDL cholesterol level and impaired glucose metabolism, were related with an increased risk for death, whereas obesity and HTN were related with a lower risk for death). No significant association between survival and BMI was shown in modification of diet in renal disease (MDRD) study [11]. Often, the different methods used for obesity assessment might have generated these different results. Elsayed et al. analyzed 1669 participants with CKD from two cohorts and found no significant connection between overweight or obesity and cardiac events compared with an ideal BMI (20–24.9 kg/m2). However, using WHR, they reported a 36 % greater relative risk of cardiac events in the group with the highest WHR (≥ 1.02 and ≥ 0.96 in men and women, respectively) [12].
Obesity/MetS and Dialysis
The prevalence of MetS in HD which varies between 60 and 80 % [13] is increasing with age and is more frequent in women. In peritoneal dialysis, the prevalence is even higher; these patients have an increased risk of metabolic disturbances (hyperglycemia, dyslipidemia, or weight gain), leading to oxidative stress, systemic inflammation, and endothelial dysfunction and finally, to increase risk of CV events and death. Moreover, the definition of MetS is not appropriate: The plasma glucose is complicated to standardize because of the inherent continuous absorption of glucose from dialysate; the measurement of waist circumference is also difficult—as it can fluctuate in relation to the intraperitoneal dialysate volume or residual volume after dialysate drainage [14] . Recently, dual-energy X-ray absorptiometry, bioelectric impedance analysis, or abdominal fat computed tomography has been used in clinical studies involving PD patients.
Surprisingly, MetS was associated with a better nutritional status, but not with CVD or all-cause mortality in dialysis patients. The role of obesity, a central part of the MetS represents a complicated dilemma. Numerous studies [15, 16], with a short median period of follow-up (2 years) revealed substantial and significant advantage in overall and CV survival in the group of patients with BMI of 25 kg/m2 or greater, including the highest BMI category (≥ 37 kg/m2) compared to patients with BMI less than 22 kg/m2. However, several studies with an extended follow-up (5–10 years), a baseline BMI of 30 kg/m2 or greater was associated with an increased risk of mortality compared to patients with ideal BMI [17, 18].
In the same line, truncal fat mass and abdominal obesity were associated with inflammation (IL-6 and CRP). Truncal fat mass is associated with an adipokine imbalance; an increase of leptin, resistin, tumor necrosis factor-α (TNF-α), and IL-6; and a decrease of adiponectin, and thereby, it may contribute to endothelial dysfunction, inflammation, oxidative stress, vascular calcification, and CV events.
Obstructive Sleep Apnea
Disturbed sleep patterns can be a disease-generating condition. Obstructive sleep apnea (OSA) is one of these conditions, being a high-priority health problem because it disrupts sleep and reduces quality of life. It is caused by a cessation of airflow caused by occlusion of the oropharyngeal tract. The main clinical features include sleepiness, fatigue, or poor concentration, signs of disturbed sleep, such as snoring, restlessness, and last but not least hypopnea or even long periods apnea terminated by loud snorts or snoring. The physical exam can be normal, although obesity, elevated blood pressure, a narrow airway, and a large neck circumference are common.
Definite risk factors for OSA include obesity, craniofacial abnormalities, and upper airway soft tissue abnormalities. Potential risk factors include heredity, smoking, and nasal congestion.
The diagnosis is mainly based upon the presence of the mentioned symptoms as well as the frequency of respiratory events during sleep. Polysomnography is the gold standard method for the diagnosis of OSA, which is defined as an intermittent interruption of airflow at the level of nose and mouth during sleep. Episodes of apnea are considered clinically relevant if they persist for longer than 10 s, but in some cases they may last as long as 2 min .
OSA is associated with obesity, HTN, especially resistant HTN, congestive heart failure, diabetes, mild pulmonary HTN; patients with severe OSA being at risk for high CV complications and death. Additionally, some patients with OSA may present proteinuria, associated with focal segmental glomerulosclerosis, hypercapnia, or nocturnal cardiac arrhythmias including bradycardia or atrial fibrillation triggered by persistent hypoxemia.
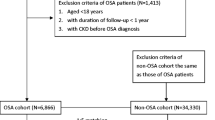
The presence of OSA may be even more relevant in nephrology because some of the factors involved in the pathogenesis of renal disease like HTN, diabetes, and obesity are the same that cause, or are associated with, OSA in the general population. However, so far, only a few studies assesed the presence of OSA in CKD patients with a minor degree of renal dysfunction, OSA being mainly suggested from questionnaires related to specific symptoms (daytime somnolence or snoring) and not assessed by polysomnographic examinations .
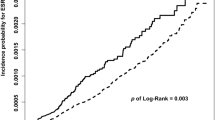
Several epidemiologic studies provided evidence that obesity is strongly associated with CKD, closing the triangle between OSA, obesity, and CKD [19, 20]. It appears that OSA is one of the most important triggers of sympathetic activity induced by the decreased arterial oxygenation which in turn raises blood pressure, particularly during nighttime. The high sympathetic activity engenders three intermediate mechanisms: chronic HTN, left ventricular hypertrophy, and arrhythmias, particularly atrial fibrillation, which eventually leads to CV complications and death. Another mechanism in the pathogenesis of renal damage in OSA patients is impairment of renal hemodynamics as measured by an increased renal resistance index (RRI) [21]. This can be of great importance since changes of renal blood flow may identify OSA patients at high risk for declining renal function. Furthermore, renal perfusion assessed by RRI is improved with an effective treatment of OSA [22] .
OSA is significantly more common in ESRD patients and it has been related with markers of CV disease and poorer survival. Unlike the general population, the usual risk factors for OSA (such as obesity, craniofacial abnormalities, nasal congestion, and smoking) do not usually apply to dialysis patients. Potential mechanisms implicated with higher prevalence of OSA in ESRD patients include the desensitizing effects of uremia or metabolic acidosis on higher respiratory control centers. These assumptions came from observational studies that showed improvement of OSA after correction of biochemical abnormalities, by increasing ultrafiltration or after kidney transplantation. The high prevalence of OSA in ESRD patients can also be the result of fluid overload and more precisely by the increased amount of fluid displaced from the legs into the neck overnight, which can eventually compress the upper airway [23].
In conclusion, OSA seems to be a more frequent disorder even in minor renal dysfunction than previously thought. Given the high risk associated with OSA and CKD, clinical trials would be warranted in the attempt to reduce the burden of morbidity and mortality linked to respiratory disorders in renal diseases [19] .
Competing Risk: OSA–MetS–Obesity: A Possible Link?
The relation between MetS, obesity, and OSA is complex. Obesity is one of the most important risk factors for OSA. Even mild to moderate obesity has been associated with increased sleep apnea prevalence . In a community of moderately overweight men, OSA had a prevalence of approximately 40 % [24], which increased to 90 % in patients with severe obesity (BMI > 40 kg/m2). Changes in body weight determine an increasing risk for OSA; two important studies, the Wisconsin Sleep Cohort Study and the Sleep Heart Health Study, showed that more than 10 kg weight gain over a 5-year period determines a fivefold increased risk in men and 2.5-fold increase in the severity of OSA [25–27]. Additionally, weight loss is associated with a parallel decrease in apnea frequency. Being the only modifiable risk factor of OSA, numerous studies, using both surgically and medically methods for losing weight investigated and founded that weight loss can improve obesity-related OSA [28, 29].
The mechanisms of this relationship are still uncertain, and may include: (1) fat deposition on airway anatomy; (2) changes in the central mechanisms regulating airway tone or ventilatory control stability. The particularly strong association seems to be between visceral fat deposition and OSA; recent studies described neck circumference as a positive predictor of OSA, associated with the severity of OSA independently of visceral obesity [30].
Inversely, OSA may predispose to obesity. It has been assumed that OSA induces neurohormonal changes: a stress reaction activating the hypothalamic–pituitary–adrenal axis leading to release of cortisol and other hormones may trigger mechanisms generating insulin resistance and preferential abdominal fat accumulation [31]. Moreover, hypoxia may generate inflammation in obesity. Adipose tissue contains numerous pro-inflammatory adipocytokines which may support endothelial dysfunction, insulin resistance, and lipid peroxidation.
Even more complex, a link between OSA and MetS, independent of obesity can be described [32]. Many of the individual components of MetS are associated with OSA. The possible mechanisms underlying OSA–MetS–obesity relationship may include the determinant role of intermittent hypoxia and sleep fragmentation who may determine: (1) the release of reactive oxygen species and oxidative stress; (2) inflammation and impaired insulin action in peripheral tissues, associated with insulin resistance, dyslipidaemia, and HTN; (3) release of adipocyte-generated hormones, like adiponectin, leptin, or adipocyte-fatty acid-binding protein. Prospective longitudinal cohort studies and interventional trials are needed to establish a definite direction of the relationship between OSA and MS or its components.
OSA–MetS–Autonomic Dysfunction–HTN
HTN is frequently found in patients with MetS (BP in the high–normal or frankly HTN range was found in more than 80 % of individuals with MetS) [33]. One of the most incriminate mechanisms is autonomic dysfunction.
Several experimental and human studies reported autonomic dysfunction as one of the mechanism for HTN in patients with MetS; it is associated with increased heart rate and cardiac output, increased peripheral vascular resistance, increased tubular sodium reabsorption in the kidney, and consequent elevation of systemic blood pressure. At the same time, abdominal visceral fat is associated with sympathetic neural activation in humans. Experimental studies suggest a regional sympathetic activation in various types of human obesity, in the absence of other comorbidities; obesity can be associated with an increase in sympathetic activity in the kidney [34, 35]. In addition, the insulin resistance typically found in MetS increases plasma leptin levels, and leptin has been reported to elevate sympathetic nervous activity, suggesting that leptin-dependent sympathetic nervous activation may contribute to an obesity-associated HTN.
Treatment
Noninvasive Positive Pressure Ventilation
Noninvasive positive pressure ventilation has been reported to be effective for improving OSA in resistant hypertensive patients, in randomized clinical trials [19, 36, 37] but, despite advances in technology and easiness of application, this technique is either not accepted or refused by many patients. In such cases, pharmacological treatment of sympathetic overactivity remains the sole treatment available to counteract the high risk of this condition.
Intensification of Ultrafiltration
In dialyzed patients, as noted above, fluid overload plays an important role in the pathogenesis of OSA. Many trials have assessed this issue, intensive dialysis or even better nocturnal dialysis having good results in improving OSA in patients with severe sleep-disordered breathing [19, 38, 39]. Additionally, ultrafiltration guided by bioimpedance or ultrasound lung comets may provide a practical method for reaching true patient euvolemia. Renal transplantation is in theory the ideal way for correcting OSA, since it eliminates all uremic toxicity. In a case-control study [40], the prevalence of OSA was almost identical in renal transplant patients as compared to age-, sex-, and BMI-matched healthy subjects, supporting the hypothesis that renal transplantation reverses OSA.
Bariatric Surgery
As noted above, obesity is a risk factor for developing CKD that may be improved with bariatric surgical weight reduction. Bariatric surgical procedures affect weight loss through two fundamental mechanisms: malabsorption and restriction. The main indications are patients who failed previous nonsurgical weight loss methods with BMI > 40 or > 35 in the setting of other comorbidities like diabetes or sleep apnea .
The goal of surgery is to reduce the morbidity and mortality associated with obesity, and to improve metabolic and organ function all along with reduction of hospitalization periods, medication costs, and improving quality of life [41, 42].
Among the positive effects of bariatric surgery we note:
-
A reduction of 50 % in incidence of diabetic nephropathy 5 years following bariatric surgery
-
An improvement in microalbuminuria in the early postoperative period
-
Hyperlipidemia improved in 70 % or more of patients
-
HTN resolved in 62 % and resolved or improved in 79 % of patients
-
Obstructive sleep apnea resolved or improved in 84 %
Although there have been dramatic improvements in the safety of bariatric procedures in the past decade, bariatric surgery is not without serious risks, including significant perioperative complications and mortality. The presence and severity of CKD is associated with a higher risk of complications among patients undergoing bariatric surgery [44].
Physical Exercise
A healthy lifestyle facilitated by participation in a regular exercise regimen may prevent or retard conditions commonly associated with CKD, including HTN, hyperlipidemia, and diabetes [45].
Although proteinuria is augmented immediately after exercise, the effect of long-term exercise on proteinuria at rest is less clear. Data from a recent systematic review showed that intentional weight loss after physical exercise is associated with decreased proteinuria and microalbuminuria. Exercise was defined as moderate to intense physical activity with at least 1.8 metabolic equivalents for a minimum duration of 15 min/day for at least 2 days/week for a minimum of 1 month [46].
Physical exercise was suggested as a useful approach to diminish impaired oxidative defense mechanisms, which is very important in the setting of CKD. In a recent study on rats, physical training prevented superoxide production, and decreased the oxidative damage in the CKD group. Furthermore, physical training before induction of a renal lesion is capable of improving oxidative damage parameters and oxidant production, without altering renal function and the antioxidant defense system [47].
Hypolipemiant Treatment
Abnormalities in lipid metabolism occur in patients with all stages of CKD and may contribute to the higher risk of CV disease in this population.
Studies in predialysis are inconclusive as they fail to draw firm conclusions. Some studies in patients with CKD show a positive relation between higher cholesterol levels and mortality risk, while other studies have found that low serum cholesterol is associated with increased mortality. This may reflect the profound adverse effect of malnutrition and chronic inflammation upon mortality, resulting in the so-called reverse epidemiology.
In CKD stage 1–3 patients with dyslipidemia, the available data suggest that statin therapy is associated with a relative reduction in the risk of major CV events. Beyond CKD stage 3, the benefits from statin treatment are less clear, more randomized studies with predefined CV end points being needed to make the correct decisions.
In dialysis patients, the statin therapy is not recommended currently. This approach is supported by three large randomized, controlled studies: 4D, SHARP, and AURORA. In those studies, the statins failed to demonstrate a significant effect of statins in CV or all-cause mortality [48–50].
References
de Jager DJ, et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA. 2009;302(16):1782–9.
Tonelli M, et al. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol. 2006;17(7):2034–47.
Stenvinkel P, et al. Obesity and nephrology: results of a knowledge and practice pattern survey. Nephrol Dial Transplant. 2013;28(Suppl 4):iv99–104.
Kramer H. Obesity and chronic kidney disease. Contrib Nephrol. 2006;151:1–18.
Zoccali C, et al. Assessment of obesity in chronic kidney disease: what is the best measure? Curr Opin Nephrol Hypertens. 2012;21(6):641–6.
Singh AK, Kari JA. Metabolic syndrome and chronic kidney disease. Curr Opin Nephrol Hypertens. 2013;22(2):198–203.
Lea J, et al. Metabolic syndrome, proteinuria, and the risk of progressive CKD in hypertensive African Americans. Am J Kidney Dis. 2008;51(5):732–40.
Lee CC, et al. Metabolic syndrome loses its predictive power in late-stage chronic kidney disease progression-a paradoxical phenomenon. Clin Nephrol. 2011;75(2):141–9.
Navaneethan SD, et al. Metabolic syndrome, ESRD, and death in CKD. Clin J Am Soc Nephrol. 2013;8(6):945–52.
Wahba IM, Mak RH. Obesity and obesity-initiated metabolic syndrome: mechanistic links to chronic kidney disease. Clin J Am Soc Nephrol. 2007;2(3):550–62.
Kimmel PL, et al. Anthropometric measures, cytokines and survival in haemodialysis patients. Nephrol Dial Transplant. 2003;18(2):326–32.
Elsayed EF, et al. Waist-to-hip ratio and body mass index as risk factors for cardiovascular events in CKD. Am J Kidney Dis. 2008;52(1):49–57.
Ucar E, et al. Frequency of metabolic syndrome among hemodialysis patients according to NCEP-ATP III and IDF definitions. Ren Fail. 2009;31(3):221–8.
Park SH, Lindholm B. Definition of metabolic syndrome in peritoneal dialysis. Perit Dial Int. 2009;29(Suppl 2):S137–44.
Snyder JJ, et al. Body size and outcomes on peritoneal dialysis in the United States. Kidney Int. 2003;64(5):1838–44.
Johansen KL, et al. Association of body size with outcomes among patients beginning dialysis. Am J Clin Nutr. 2004;80(2):324–32.
McDonald SP, Collins JF, Johnson DW. Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand patient populations. J Am Soc Nephrol. 2003;14(11):2894–901.
Hoogeveen EK, et al. Obesity and mortality risk among younger dialysis patients. Clin J Am Soc Nephrol. 2012;7(2):280–8.
Mallamaci F, Tripepi G. Comment accompanying: obstructive sleep apnoea: a stand-alone risk factor for chronic kidney disease by Chou Yu-Ting. Nephrol Dial Transplant. 2011;26(7):2072–4.
Abrass CK. Overview: obesity: what does it have to do with kidney disease? J Am Soc Nephrol. 2004;15(11):2768–72.
Buchner NJ, et al. The renal resistance index is increased in mild-to-moderate obstructive sleep apnoea and is reduced under continuous positive airway pressure. Nephrol Dial Transplant. 2011;26(3):914–20.
Chou YT, et al. Obstructive sleep apnea: a stand-alone risk factor for chronic kidney disease. Nephrol Dial Transplant. 2011;26(7):2244–50.
Elias RM, et al. Relationship of pharyngeal water content and jugular volume with severity of obstructive sleep apnea in renal failure. Nephrol Dial Transplant. 2013;28(4):937–44.
Schwartz AR, et al. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc. 2008;5(2):185–92.
Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol. (1985);99(4):1592–9.
Young T, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the sleep heart health study. Arch Intern Med. 2002;162(8):893–900.
Newman AB, et al. Progression and regression of sleep-disordered breathing with changes in weight: the sleep heart health study. Arch Intern Med. 2005;165(20):2408–13.
Johansson K, et al. Effect of a very low energy diet on moderate and severe obstructive sleep apnoea in obese men: a randomised controlled trial. BMJ. 2009;339:b4609.
Lam B, et al. Randomised study of three non-surgical treatments in mild to moderate obstructive sleep apnoea. Thorax. 2007;62(4):354–9.
Kawaguchi Y, et al. Different impacts of neck circumference and visceral obesity on the severity of obstructive sleep apnea syndrome. Obesity (Silver Spring). 2011;19(2):276–82.
Rosmond R, Bjorntorp P. The interactions between hypothalamic-pituitary-adrenal axis activity, testosterone, insulin-like growth factor I and abdominal obesity with metabolism and blood pressure in men. Int J Obes Relat Metab Disord. 1998;22(12):1184–96.
Lam JC, Mak JC, Ip MS. Obesity, obstructive sleep apnoea and metabolic syndrome. Respirology. 2012;17(2):223–36.
Mancia G, et al. Metabolic syndrome in the Pressioni Arteriose Monitorate E Loro Associazioni (PAMELA) study: daily life blood pressure, cardiac damage, and prognosis. Hypertension. 2007;49(1):40–7.
Smith MM, Minson CT. Obesity and adipokines: effects on sympathetic overactivity. J Physiol. 2012;590(Pt 8):1787–801.
Wolk R, Shamsuzzaman AS, Somers VK. Obesity, sleep apnea, and hypertension. Hypertension. 2003;42(6):1067–74.
Lozano L, et al. Continuous positive airway pressure treatment in sleep apnea patients with resistant hypertension: a randomized, controlled trial. J Hypertens. 2010;28(10):2161–8.
Duran-Cantolla J, et al. Continuous positive airway pressure as treatment for systemic hypertension in people with obstructive sleep apnoea: randomised controlled trial. BMJ. 2010;341:c5991.
Tang SC, et al. Improvement in sleep apnea during nocturnal peritoneal dialysis is associated with reduced airway congestion and better uremic clearance. Clin J Am Soc Nephrol. 2009;4(2):410–8.
Bradley TD, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353(19):2025–33.
Mallamaci F, et al. Sleep disordered breathing in renal transplant patients. Am J Transplant. 2009;9(6):1373–81.
Christou NV, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240(3):416–23; discussion 423–4.
Abu-Abeid S, Keidar A, Szold A. Resolution of chronic medical conditions after laparoscopic adjustable silicone gastric banding for the treatment of morbid obesity in the elderly. Surg Endosc. 2001;15(2):132–4.
Sjostrom L, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Flum DR, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445–54.
Chen PY, et al. Effects of an exercise program on blood biochemical values and exercise stage of chronic kidney disease patients. J Nurs Res. 2010;18(2):98–107.
Afshinnia F, et al. Weight loss and proteinuria: systematic review of clinical trials and comparative cohorts. Nephrol Dial Transplant. 2010;25(4):1173–83.
Coelho BL, et al. Physical exercise prevents the exacerbation of oxidative stress parameters in chronic kidney disease. J Ren Nutr. 2010;20(3):169–75.
Wanner C, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353(3):238–48.
Fellstrom BC, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360(14):1395–407.
Baigent C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (study of heart and renal protection): a randomised placebo-controlled trial. Lancet. 2011;377(9784):2181–92.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Apetrii, M., Voroneanu, L., Covic, A. (2015). Obesity/OSA/Metabolic Syndrome in Patients with CKD and Hypertension: The Missing Link?. In: Weir, M., Lerma, E. (eds) Chronic Kidney Disease and Hypertension. Clinical Hypertension and Vascular Diseases. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1982-6_18
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1982-6_18
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1981-9
Online ISBN: 978-1-4939-1982-6
eBook Packages: MedicineMedicine (R0)