Abstract
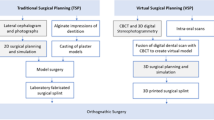
Orthognathic surgery has become a sophisticated operative procedure for the correction of dentofacial deformities. Recent advances in virtual surgical planning (VSP) allow surgeons’ improved computer-assisted digital preoperative case preparation compared to traditional plaster cast analysis and model surgery with lateral cephalometric prediction tracings. VSP allows surgeons to directly visualize osteotomy cuts, actual positioning of segments, visualization of occlusion, and 3D soft tissue predictions. Precise measurements of segment movements and bone excision for osteotomies allows highly accurate presurgical planning that is superior to traditional model surgery. Rapid printing of surgical splints and cutting guides has proven to be more accurate than handmade splints based on plaster models. Optical scans of the patient’s dentition or dental tests can be merged with the CT data. Orthognathic surgery for single or double jaw can be planned with virtual intermediate and final splints visualized and then printed for clinical use. Genioplasty can also be planned using VSP with cutting and positioning guides. Studies have shown that VSP saves considerable time and cost to patients, surgeons, hospitals, and insurance companies. Distraction osteogenesis can also be planned using VSP with the creation of cutting and hardware positioning guides. VSP is utilized for the combined planning of total TMJ alloplastic replacement in coordination with orthognathic surgery. In this way separate service providers can integrate custom implant fabrication with osteotomy planning. VSP permits a team approach and improved communication through web-based treatment planning sessions. VSP aids patient education through the 3D images developed through treatment planning with visualization of the surgical plan and prediction.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Orthognathic surgery is a fascinating and powerful treatment modality to provide correction for patients with dentofacial deformities. These complex surgical procedures require accurate diagnosis, appropriate treatment planning, and precise surgical execution.
The first mandibular osteotomies were first performed in the mid-1800s by Simon P. Hullihan [1] who operated the first subapical osteotomy. There was an evolution to the vertical ramus osteotomies in the 1930s by Lane and others and the bilateral sagittal split osteotomies performed in the 1950s and 1960s by Trauner, Obwegeser, and DalPont [1]. The maxillary LeFort classification dates to the early 1900s with progressive advances in surgical technique by Bell and others over time leading to the LeFort I down fracture in the 1970s [1].
Orthognathic surgery has developed over time into a routine procedure, allowing it to be performed on a regular basis, and has become a safe and effective surgical procedure for skeletal facial deformities.
Traditionally, the diagnostic methods for orthognathic surgery have included detailed pre-orthodontic and preoperative clinical examination, plain radiographic analysis, and dental casts. The diagnostic workup is performed with articulator-mounted dental models, standard facial photography, panoramic dental radiograph, and traced posterior-anterior (PA) and lateral cephalometric radiographs followed by analysis techniques using various established norms. The surgical plan is then determined based on the analyzed data and the use of “model surgery.” Model surgery includes the cutting , repositioning, and fixation of stone models mounted on a semi-adjustable articulator. Surgical splints are then hand fabricated in this process and used intraoperatively to guide the positioning of the maxilla and/or mandible. When combined with well-executed surgical technique, traditional orthognathic planning has proven to be safe, and a reasonably accurate method for the correction of dentofacial deformities.
Virtual Surgical Planning
The use of traditional model surgery for orthognathic surgery has harbored many inaccuracies related to surgical planning. These inaccuracies stem from the attempt to transfer from dental models the exact spatial relationship of the three-dimensional maxillomandibular complex to the semi-adjustable articulator. Diagnosing and accurately transferring the exact anterior-posterior and transverse positions of the maxilla, occlusal plane angle, and any existing cant of maxilla (the yaw, pitch, and roll) are not only cumbersome but also somewhat inaccurate [2]. The inaccuracy is inherent as part of human error, device error, and unavoidable volumetric expansion of materials such as plaster, wax, and glue. The standard articulator is designed to represent the average “normal” cranio-maxillofacial relationship and bilateral temporomandibular joint functional anatomy. This is problematic for patients with dentofacial deformit ies who often present with anatomical relationships that may significantly deviate from the norms. Furthermore, two-dimensional radiography can fail to adequately reveal complex anatomic variations and asymmetries of the facial skeleton. Identification of landmarks on cephalometric radiographs, especially for overlapping structures in an asymmetric patient can be inconsistent. Two-dimensional imaging provides insufficient information about condylar abnormalities, bone thickness in areas of interest, and exact spatial position of important structures. In addition, image distortion and magnification errors may be sources of error [3]. Precision of the surgical outcome in orthognathic surgery requires a detailed appreciation of patient’s true anatomy and accurate planning. Limitations of 2D imaging, facebow transfer, and cast model surgery can lead to imprecise and inadequate diagnostic data gathering, inaccurate treatment planning, and suboptimal results, (especially in complex cases), even in the hands of the most experienced surgeons [4, 5]. Lastly, the large number of hours spent by the practitioner on the preoperative workup can be a discouraging factor.
Virtual surgical planning (VSP) for orthognathic surgery is a form of computer-assisted surgery that has developed from the various fields such as neurosurgery, orthopedic surgery, sinus surgery, dental implantology, and prosthodontics [6,7,8]. VSP has been made possible by the general advances in imaging technology, especially with the advent of 3D CT scanning in the 1970s and the subsequent improvements upon the resolution and accuracy of the software algorithms to generate 3D representations of soft and hard tissues. Computer-assisted surgery may involve preoperative planning in the form of manufactured stereolithographic models or by virtual surgical planning. In addition, computer-assisted surgery can include intraoperative navigation for complex reconstructive and corrective cranio-maxillofacial surgery [9, 10].
Virtual surgical planning (VSP) plays a role in both diagnostic as well as planning phases of orthognathic surgery. It uses digital imaging technology in the form of 3D computed tomography (CT) or cone beam computed tomography (CBCT) and 3D laser surface scanning of dental cast models (or directly from the patient’s dentition) merged to capture the patients’ exact anatomy. When combined with the traditional clinical examination and cephalometric analysis, one can arrive at a comprehensive diagnostic picture of the patient. The various maxillary and mandibular osteotomy techniques are performed to virtually simulate the surgical movements which upon completion computer-aided design/computer-aided manufacturing (CAD/CAM) technology is then utilized to design and fabricate surgical cutting and positioning guides.
The Virtual Surgical Planning (VSP) Process
A thorough discussion is held with the patient, assessing in detail pertinent subjective goals, chief complaints and expectations, history of dental and orthodontic treatment, as well as medical, surgical, and family history. A complete review of systems is performed with particular emphasis on sleep, speech, breathing, mastication, swallowing, orofacial pain, and oral habits. In our center, the clinical examination begins with complete dentofacial data gathering including TMJ examination, nasal and oral airway, dental, occlusal, and facial measurements and relationships, and soft tissue assessment. High-quality clinical photographs are obtained in natural head position in repose and with full animation in lateral, frontal, and 3/4 views, as well as intraoral views. A photograph is taken with a wooden tongue depressor placed against the maxillary canines and held by the patient to capture any obvious cant of the maxilla. Full-face CBCT of the patient in standing position is obtained. We prefer the CBCT imaging with the patient in an upright position to avoid the effect of gravity on the soft tissues, as well as for its reduced radiation dose compared to standard CT. Although panoramic and lateral cephalometric 2D radiographs can be generated from the CBCT, we obtain standard panoramic and plain lateral and posterior-anterior cephalometric views. The cephalometric radiographs are easily calibrated, traced, and analyzed by digital tracing and analysis software, which serves as a baseline or reference for comparison to postoperative imaging. A minimum of two sets of maxillary and mandibular alginate impressions are taken and poured with orthodontic stone or die stone. A bite registration and facebow registration are no longer obtained, as they are unnecessary.
The occlusion of trimmed dental cast-models is evaluated to assess the need for segmentation of the maxilla and/or occlusal adjustment. Segmentation of the maxilla can correct limited (<7 mm) transverse maxillary deficiencies or unleveled arches in comparison to the mandibular arch. When indicated, one maxillary cast can be segmented in two or more pieces and set in the desired position using rigid sticky wax or glue. The standard desired position of the maxillary cast is Class I occlusion in maximum intercuspation, unless otherwise indicated. The second maxillary cast is only needed to serve as reference for any occlusal adjustments or in case of unforeseen damage to the first cast during segmentation.
Once the desired occlusion is achieved with the dental casts, they are mounted on a Galetti articulator (Fig. 6.1) in the desired occlusal relationship. A thin layer of Vaseline is applied on all the teeth, and a bite registration is obtained using polyvinyl siloxane (PVS) bite registration material. The bite registration record is removed after setting, and the occlusion is checked again to ensure it is the desired final occlusion. The casts are unmounted from the articulator and placed into occlusion with the bite registration record secured in between, along with the uncut maxillary cast and they are shipped to the company for optical scanning and data merge with the CT data. An online meeting is then scheduled for the actual virtual surgical planning (VSP). Time can be saved by informing the technician of what type of maxillary and mandibular osteotomies are to be performed, thus allowing for virtual preparation prior to the planning session. The CT data is uploaded to the company website with Digital Imaging and Communications in Medicine (DICOM) format (Table 6.1).
Prior to the online meeting, the DICOM data is reconstructed in 3D, providing accurate skeletal and soft tissue rendering. The dental casts are scanned with surface to surface registration superimposed on the 3D reconstruction to provide high-resolution dental anatomy. The reason for scanning and registration of the dental casts is due to limitations of today’s CT technology to accurately capture the complex dental anatomy which is obscured by streak artifacts created by metallic brackets, wires, and dental restorations.
During the online planning meeting, desired osteotomies and skeletal movements are virtually created. Our preferred approach is maxilla-first surgery, where by the maxilla is moved to the desired position based on the previously gathered clinical data (patient expectations, clinical measurements, facial and cephalometric analysis). Attention is paid to dental and facial midlines, presence of cants, and need for differential impactions (the roll, yaw, and pitch). The maxilla can be pivoted against any desired point of rotation with immediate visualization of the amount of interosseous gaps, overlaps, and degree of movement to the tenth of millimeters or angular degrees.
Although surgical guides can be fabricated for segmentation of the maxilla, we usually do not find them necessary. However, in cases of TMJ implant reconstruction, inverted-L mandibular osteotomies and interosseous bone grafting, or genioplasty for correction of an asymmetric chin, we find that cutting and positioning guides can be very helpful. The intermediate and final splints are generated with the use of CAD/CAM technology . They can be separate or as in the sandwich technique. If large skeletal movements are planned (such as in maxillomandibular advancement for the treatment of severe obstructive sleep apnea), a thick intermediate splint can be helpful as it facilitates the intraoperative intermaxillary fixation. The stability of a multi-piece maxilla can be improved by designing lingual lips that fit against the lingual surface of maxillary posterior teeth. A palatal strap with desired amount of clearance from palatal mucosa may be added for further strength.
Preparing for Orthognathic Surgery
Orthognathic surgery has many facets that need to be looked at carefully and performed correctly to achieve a good outcome. Each one of these facets must be addressed individually and then brought together as a whole to produce the desired result. So there are multiple steps that we review as surgeons when we approach a patient that presents for orthognathic surgery. What should our thought process be and how we then translate that information to the patient’s understanding and surgical success. It should include the following:
-
Patient presentation
-
Patient workup
-
Diagnosis
-
Communication with the orthodontic team
-
Surgical planning
-
Surgery
-
Postoperative care
-
Final records
Patient Presentation
When patients present for a surgical consultation, they may or may not have a good idea what a proposed surgery may involve or entail. It is our responsibility as surgeons to inform the patient of the diagnosis in detail and in language the patient can understand. Once we feel confident that the patient understands the diagnosis, we must then offer all possible treatment options available. Some solutions may not include a surgical procedure to correct the patients presenting diagnosis; however, more often than not, when a patient presents with a maxillary/mandibular skeletal deformity , the proposed solution will be somewhere in the surgical realm. The surgeon’s consultation then will have to include the preoperative course, the operative procedure, risks and benefits, complications, long-term prognosis, and postoperative care. The importance of informing the patient and achieving realistic expectations requires good communiction which cannot be overemphasized.
The consultation must stress; that orthognathic surgery is a team effort; thus, working closely with the orthodontist is of utmost importance, whether it be surgery first or orthodontics first. The conversation should continue in an open dialog format leading the discussion in a logical manner informing the patient of the initial workup including facial measurements, intraoral exam, photos, X-rays, maxillary/mandibular arch impressions, and a bite registration. An analysis is then performed with the information that is gathered to render a diagnosis, which will then move toward the development of a surgical plan. The surgical plan is devised and executed leading to the postoperative phase of treatment with finalization of orthodontics and long-term stability. We should stress to the patient that part of our armamentarium is the utilization of virtual surgical planning, which includes 3D renderings of the patient’s anatomy and the proposed bony movements. These images can also be instrumental in patient education and understanding the actual surgical procedure prior to having the operative procedure performed. The patient should be informed that 3D predicted images are highly accurate but may not be an exact representation of the final outcome.
Patient Workup
The workup should be done in a meticulous systematic fashion . If it is done in a haphazard way, it is possible to make crucial mistakes that can lead to an altered diagnosis or errors related to the surgical procedure. Thus, obtaining accurate records is essential to the success of orthognathic surgery. The records obtained will be used as a representation of the patient as we move forward in the process of developing a diagnosis and ultimately the surgical plan. A cephalometric analysis of the X-rays is performed, and the models are articulated with the bite registration obtained. The photographs are another key element essential to the process. Intraoral photographs help us ensure that our mounted models are articulated correctly, and they give us information regarding the patients smile line, and the resting lip line which helps in the diagnosis of anterior vertical discrepancy. It provides a reference for the evaluation of the patient’s facial midline and dental midlines, as well as a reference for any facial asymmetries. The actual facial and intraoral measurements obtained during the physical exam are utilized to ensure that all of the aforementioned data is correct. We can now incorporate the many different data sources we have obtained and integrate them into a final diagnosis.
Diagnosis
We must always remember that the diagnosis of a facial skeletal deformity is ultimately a clinical decision. One cannot utilize cephalograms or CT scans to provide a diagnosis without correlating the actual physical findings.
When developing the diagnosis, we must think of all the skeletal discrepancies in three dimensions, the vertical, horizontal, and anterior posterior planes. This is the only way to obtain the correct diagnosis and develop a good surgical plan, thus allowing us to address all aspects of the skeletal deformity requiring correction.
It is also important to note that prior to utilizing our VSP software, we need to have the correct preliminary diagnosis and have formulated a surgical plan. In other words we should already know the basic maxillary/mandibular surgical technique to be performed and the movements planned for the surgical correction that we formulated from our diagnosis. The surgical plan is then inputted into the 3D virtual planning environment software to show what the result of our surgery will produce in three dimensions: the exact bony movements and their measurements.
VSP has become an essential tool as an adjunct to our cognitive ability to develop a diagnosis and derive a surgical plan that will produce the best result . There may also be considerations for facial implants, and bone grafting as it relates to contour deformities of dentofacial deformities and craniofacial disorders.
Communication with the Orthodontic Team
The team approach in orthognathic surgery is paramount to obtaining the best possible outcome for the patient. Open communication with the orthodontic team regarding the following key points will allow the patient, the surgeon, and orthodontist to have a clear view of the surgical process and plan:
-
Initial diagnosis
-
Removal of third molars and other teeth agreed upon by the orthodontist and the surgeon
-
Beginning of orthodontic treatment
-
Developing a surgical/orthodontic plan
-
Time required for orthodontic movement prior to surgery
-
Placement of final rectangular wire and surgical hooks
-
Final models
-
CBCT within 6 months
-
Virtual surgical planning (VSP)
-
Surgery
-
Postoperative care
-
Postoperative orthodontics and long term retention
When the practitioners maintain sufficient dialog and a high level of communication, the patient’s overall treatment will lead to a satisfactory outcome and a satisfied patient.
Virtual Surgical Planning
Once we have finalized the diagnosis and surgical plan, it is possible to proceed with the VSP and observe the bony movements in three dimensions. The VSP is usually performed 2–3 weeks before surgery after the final rectangular wire has been placed by the orthodontist. Stone models are obtained and placed in corrected occlusion with wax or polyether bite. If necessary models are sectioned and segments fixated with sticky wax or glue and then sent directly to the company to optically scan and merge into the VSP software. A sterolithographic model (if desired) can be obtained from the CBCT DICOM data which is uploaded by fileshare to the company. Once the company has both the dental models and CBCT DICOM data, an online meeting time can be scheduled to perform the virtual surgery and prepare to make surgical guides and splints.
As the movements are done virtually in a three-dimensional environment, one can readily see the relationship of the bony segments as they are moved into the planned position with measurements and provides an accurate view of the jaw position and possible bone interferences. For maxillary osteotomies , this allows simulation of advancement, impaction, differential movement, segmentation, cant correction, interferences, the amount of bone to removed, and overlap of segments. The mandibular osteotomies have the same advantage post movement; whether an intraoral vertical ramus osteotomy (IVRO) , bilateral mandibular ramus sagittal split osteotomies (BSSO) , or anterior horizontal mandibular osteotomy (AHMO) . One can determine areas of premature contact, areas of adequate contact, and areas without contact. This information is invaluable to the surgeon regarding the surgical plan. If the preplanned movements are not appropriate for good bone approximation and healing, it would be an indication to modify the surgical approach or alter the plan to obtain a stable result.
When evaluating the final position of the upper and lower jaw in three dimensions, it becomes clear whether to make rotational movements and/or yaw changes that will improve the final outcome. Prior to VSP there was little to no control over these types of movements. With the help of VSP, we can make these additional movements, thus helping us in the operating room and to improve our outcomes.
For single jaw surgery, whether in the mandible or the maxilla, only a final splint needs to be fabricated, while for two jaw surgery, an intermediate and final splint is needed. Genioplasty positional splints also can be fabricated. Specifications for the splints can include the depth of indentation of the dentition, the width of the buccal flange, and optional wiring holes . VSP can also provide soft tissue changes in 2D and 3D images.
Surgery
When entering the operating room as surgeons, we like to have an accurate plan that can be executed swiftly with precision, with the confidence that we can achieve our surgical goals with patient safety and the best possible outcomes. With the use of VSP, we are able to have great confidence in our plan and decisions. All surgery still depends on knowledge of surgical anatomy and impeccable decision making while in the operating room. Thus, we always need to rely on our education, and surgical judgement and experience to be successful. Knowing where to make incisions and accurate osteotomies determines good surgical and functional results. As time progresses and technology becomes more integrated into medicine and surgery, we may continue to grow in confidence and rely on more accurate surgical adjuncts. Greater core knowledge of the patient’s 3D skeletal anatomy reduces complications during surgical procedures. VSP thus saves considerable time during the surgical planning when compared to traditional model surgery, which has shown to be highly accurate, and surgery more efficient with the decision making planned well in advance. This reduces planning and operating time, which is better for surgeons and patients, and can be a cost savings for the delivery setting whether in the hospital, ambulatory surgery center, or private office.
Postoperative Care
The first 6 weeks post orthognathic surgery is an important time for patient care and a successful outcome of the surgery. The patient should be evaluated weekly for occlusal stability and/or stability of maxillary/mandibular fixation if jaws are wired shut. Monitoring nutritional status, wound care, and maxillary pedicle perfusion are essential aspects of postoperative care. The use of guiding elastics can be an important modality during the healing phase.
Postoperative radiographs on the first day may include panoramic, lateral cephalometric, PA cephalometric, or a 3D cone beam to evaluate:
-
Soft tissue profile changes
-
Position of the bony segments
-
Condylar position in the fossa
-
Hardware placement
-
Possible injury to the roots of teeth
-
Oral pharyngeal airway changes
-
Compare movements to preoperative VSP
-
Proper splint position and fit
If maxillomandibular fixation is utilized or splint removal is required, follow-up radiographs can also be performed 4–6 weeks postoperatively to evaluate the stability of the movements.
Orthodontic evaluation can begin as early as 1 week postoperatively depending on the team’s preferences. However, postsurgical orthodontic forces are usually not applied for 6–7 weeks. Frequency of surgical follow-up during the 3–6 months, postoperative orthodontic treatment is also team dependent. Upon de-bonding, patients are given retainers; removable or fixed for long term orthodontic retention .
Final Records
Approximately 1 year following orthognathic surgery, the patient will return for final records which should include CBCT, panoramic radiograph, lateral cephalometric radiograph, models, and photos. These are utilized to compare the movements to the preoperative plan, the immediate postoperative results and to evaluate stability of the result, for healing of the segments and relapse. The final record taking session also completes the patient record from the initial consultation to the probable discharge of the patient from surgical care. The session will usually include:
-
Physical exam
-
Facial appearance
-
Anterior posterior view
-
Lateral view
-
Three-fourths view
-
-
Mandibular mobility and jaw opening
-
TMJ
-
Clicking, popping, or crepitation
-
Muscles of mastication tenderness
-
TMJ tenderness
-
Headaches
-
-
Cranial nerve
-
V2
-
V3
-
-
Occlusion
-
Dental injuries (endodontic and periodontic)
-
-
Photos
-
Facial views
-
Intra oral
-
-
Radiographs
-
Plain films
-
Lateral ceph
-
PA ceph
-
Panoramic
-
Periapical
-
-
3D cone beam
-
Pros and Cons of Virtual Surgical Planning
Pros
-
Accuracy
-
Bone movements
-
Measurements of movements
-
Osteotomy design
-
-
3D view of the bony segments
-
Overlap
-
Bony gaps
-
Interferences
-
Asymmetries
-
Midlines
-
Rotation
-
Bodily shifts
-
-
Maxillary impaction
-
Rotation Point
-
ANS
-
Incisal edge
-
-
Bodily/differential movements
-
-
-
Fabrication
-
Intermediate occlusal splints
-
Final occlusal splints
-
Cutting guides
-
Positional jigs
-
Simulated graft wedges
-
Size
-
Shape
-
-
-
Time
-
Decreased
-
Less model surgery
-
No splint fabrication
-
Decreased radiographic analysis and prediction tracing
-
Improved presurgical understanding of patients bony anatomy
-
OR time
-
-
Cons
-
Cost
-
Increased
-
CT scan
-
Shipping
-
Models
-
Bite
-
CT CD
-
Splints
-
Guides
-
Plans
-
-
-
-
Teaching
-
Less model surgery
-
No splint fabrication
-
Improved 3D visualization
-
Research tool
-
-
Back up
-
No ability to fabricate a backup splint unless stone or 3D printed models are available .
-
3D Virtual Surgical Planning
Maxillary and Mandibular Movements
VSP is performed in a virtual 3D environment utilizing the patient’s CT scan data merged with optical scan data of the dental occlusion. To begin the process of VSP a 3D image of the preoperative facial skeleton is observed (Fig. 6.2). This image can be rotated and viewed from all sides. Based on a prediction tracing of a lateral cephalometric radiograph, desired positions for single or double jaw osteotomy segments can be planned. Commonly the maxilla is operated first at the Lefort I level and repositioned based on the intact mandible (Figs. 1.6a–n and 6.3). For double jaw osteotomies. once the position of the maxilla is established, whether as a single piece or in a segmental osteotomy, the mandible undergoes virtual vertical or sagittal split osteotomies and is set in position in the correct dental occlusion (Fig. 6.4). If genioplasty is to be performed, an anterior horizontal mandibular osteotomy is virtually performed and the inferior segment positioned (Fig. 6.5). The software provides precise measurements of the osteotomy cuts and movements (Figs. 6.6a, b and 6.7). Lateral cephalometric reference angle measurements can be incorporated into the planning (Fig. 6.8). For a double jaw case, the intermediate splint is virtually created as an STL file for CAD/CAM fabrication, usually via 3D printing (Fig. 6.9). STL files for CAD/CAM fabrication of the final splint is then virtually created for single or double jaw osteotomies (Fig. 6.10). Wire holes for the final splint can be digitally created. Cutting guides for all osteotomies can be also be created. As examples, a Genioplasty cutting guide (Fig. 6.11), and a positioning guide for Genioplasty (Fig. 6.12) are seen.
VSP planned LeFort I maxillary movement for Class III skeletal malocclusion with mandibular prognathism and deviation to the right. For a single jaw osteotomy of the maxilla, from this set final position of the maxilla a final splint can be fabricated. For a double jaw, planning would continue with the mandibular osteotomies. (a) Frontal view 3D (b) Inferior view 3D (c) Right lateral 3D (d) Left lateral 3D. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP planned mandibular movement with a right sagittal split ramus and left vertical ramus osteotomies as it relates to the new LeFort I maxillary position for Class III skeletal malocclusion with mandibular prognathism and deviation to the right. (a) Frontal view 3D (b) inferior view 3D (c) right lateral 3D (d) left lateral 3D. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP planned genioplasty as it relates to the LeFort I and mandibular movement with a right sagittal split ramus and left vertical ramus osteotomies for Class III skeletal malocclusion with mandibular prognathism and deviation to the right. (a) Frontal view 3D (b) inferior view 3D (c) right lateral 3D (d) left lateral 3D. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP planned mandibular movement measurements with mandibular canal marking with a right sagittal split ramus, left vertical ramus, and genioplasty osteotomies as it relates to the new maxillary position for Class III skeletal malocclusion with mandibular prognathism and deviation to the right frontal view. (a) frontal view 3D (b) right lateral view 3D (c) left lateral 3D view (d) sagittal 2D view. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP lateral cephalometric reference angle measurements preoperative and planned movements for a LeFort I, right sagittal split ramus, left vertical ramus, and genioplasty osteotomies as it relates to the new maxillary position for Class III skeletal malocclusion with mandibular prognathism and deviation to the right frontal view. (a) Right lateral preoperative view 3D (b) right lateral planned 3D view. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP virtual intermediate splint fabrication for planned mandibular movement measurements with a right sagittal split ramus, left vertical ramus, and genioplasty osteotomies as it relates to the new maxillary position for Class III skeletal malocclusion with mandibular prognathism and deviation to the right frontal view. (a) Frontal view 3D (b) left lateral view 3D (c) intermediate splint superior view (d) intermediate splint inferior view. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP virtual final splint fabrication for planned mandibular movement measurements with a right sagittal split ramus, left vertical ramus, and genioplasty osteotomies as it relates to the new maxillary position for Class III skeletal malocclusion with mandibular prognathism and deviation to the right frontal view. (a) Frontal view 3D (b) left lateral view 3D (c) final splint superior view (d) final splint inferior view. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP cutting guide for genioplasty as it relates to the LeFort I and mandibular movement with a right sagittal split ramus and left vertical ramus osteotomies for Class III skeletal malocclusion with mandibular prognathism and deviation to the right. (a) Frontal view 3D (b) right lateral view 3D (c) cutting guide 3D frontal view (d) left lateral 3D view. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
VSP positioning guide for genioplasty as it relates to the LeFort I and mandibular movement with a right sagittal split ramus and left vertical ramus osteotomies for Class III skeletal malocclusion with mandibular prognathism and deviation to the right. Drill holes in guide allow fixation of the inferior genioplasty segment for rigid fixation. (a) Frontal view 3D (b) right lateral view 3D (c) positioning guide frontal 3D view (d) left lateral 3D view. (Proplan, DuPuy Synthes Craniomaxillofacial, Paoli, PA, USA)
Surgical Cases Planned with Digital Technology
Case 1 Figures 6.13–6.71
Twenty-eight year-old female presented with Class III skeletal malocclusion with mandibular prognathism and deviation to the right and bilateral midfacial and malar hypoplasia, following presurgical orthodontics.
Surgical plan was for LeFort I osteotomy, bilateral mandibular vertical ramus osteotomies, genioplasty, and bilateral malar implants. VSP (Proplan, DePuy Synthes Craniomaxillofacial, Paoli, PA, USA) was utilized to plan and fabricate custom intermediate and final splints. Bilateral Medpor zygomatic implant (Stryker, Kalamazoo, MI, USA) with DePuy Synthes screw fixation (DePuy Synthes Craniomaxillofacial, Paoli, PA, USA) was performed. Satisfactory postsurgical facial esthetic and occlusal result are demonstrated. (Surgery: Alex M. Greenberg, DDS, New York, NY, Orthodontics: Dr. Ronald Schwalb, New York, NY, USA).
Case 2 Figures 6.72–6.122
A 20 year-old female with possible diagnosis of Churg–Strauss syndrome presented with severe bilateral mandibular condylar resorption and mandibular retrognathia and retrogenia with Class II skeletal malocclusion . The plan was for LeFort I osteotomy, bilateral mandibular total joint prostheses, and genioplasty. An integrated planning process with VSP (Medical Modelling, Golden, CO, USA) to plan the surgery and fabricate custom intermediate and final splints, and the custom fabrication of the bilateral total TMJ prostheses (TMJ Concepts, Ventura, CA, USA) was utilized. Surgery was performed with a satisfactory facial esthetic, and occlusal result was achieved. A postoperative high level of occlusal stability is seen at 4 weeks and 1 year. (Surgery: Alex M Greenberg, DDS, Michael Perrino, DDS, MD, Assistant Professor, Oral and Maxillofacial Surgery, Columbia University College of Dental Medicine, Maher Jandali Rifai, DMD, MD, Chief Resident, Oral and Maxillofacial Surgery, Columbia University College of Dental Medicine, New York, NY, USA, Orthodontics: Dr. Shirley Lew, Private Practice, Brooklyn, NY, USA).
Patient-Specific Surgical Guides and Bone Plates
Patient-specific surgical guides for osteotomies and custom prebent bone plates can now be virtually planned and 3D printed from Titanium Grade 2 using laser melting process (Figs. 6.123, 6.124, 6.125, and 6.126).
Virtual orthognathic bimaxillary surgical planning of patient-specific custom surgical guide for LeFort I osteotomy and predrilling holes for custom bone plate (Proplan and Trumatch, DePuy Synthes Craniomaxillofacial, Paoli, PA, USA). (Case courtesy of Prof. Dr. Dr. Alexander Schramm and PD Dr. Dr. Frank Wilde, Oral and Plastic Maxillofacial Surgery, University Hospital Ulm and Military Hospital Ulm, Ulm, Germany)
Virtual orthognathic bimaxillary surgical planning of patient-specific custom bone plate for LeFort I osteotomy (Proplan and Trumatch, DePuy Synthes Craniomaxillofacial, Paoli, PA, USA). (Case courtesy of Prof. Dr. Dr. Alexander Schramm and PD Dr. Dr. Frank Wilde, Oral and Plastic Maxillofacial Surgery, University Hospital Ulm and Military Hospital Ulm, Ulm, Germany)
Intraoperative view of patient-specific custom surgical guide fabricated from 3D printed Titanium Grade 2 using laser melting process for LeFort I osteotomy and predrilling holes for custom prebent bone plate (Proplan and Trumatch, DePuy Synthes Craniomaxillofacial, Paoli, PA, USA). (Case courtesy of Prof. Dr. Dr. Alexander Schramm and PD Dr. Dr. Frank Wilde, Oral and Plastic Maxillofacial Surgery, University Hospital Ulm and Military Hospital Ulm, Ulm, Germany)
Intraoperative view of patient-specific custom surgical guide for osteotomies and predrilling holes for custom bone plate from 3D printed Titanium Grade 2 using laser melting process (Proplan and Trumatch, DePuy Synthes Craniomaxillofacial, Paoli, PA, USA). (Case courtesy of Prof. Dr. Dr. Alexander Schramm and PD Dr. Dr. Frank Wilde, Oral and Plastic Maxillofacial Surgery, University Hospital Ulm and Military Hospital Ulm, Ulm, Germany)
Conclusion
As a result of advances in digital technologies such as VSP and rapid printing , orthognathic surgery has gone through an important evolution. Advances in surgical techniques, equipment, diagnostic tools, and planning software have changed how the surgery is currently being performed.
VSP is another adjunct to improve our surgical outcomes, save time and costs, and ultimately improve patient care. It has given us an accurate way to measure bone movements, supply rapid printed occlusal splints/surgical guides, and a 3D view of surgery that we have learned to trust. New 3D printed Titanium Grade 2 surgical guides for precision osteotomies and patient-specific bone plates are important developments.
As with all scientific advancements surgeons must always use good judgment and knowledge when incorporating new technologies into our treatment of patients.
References
Greenberg AM, Prein J, editors. Craniomaxillofacial Reconstructive and Corrective Bone Surgery: Principles of Internal Fixation Using the AO/ASIF Technique. New York: Springer Verlag; 2002. p. 581–622
Ellis E III, Tharanon W, Gambrell K. Accuracy of face-bow transfer effect on surgical prediction and postsurgical result. J Oral Maxillofac Surg. 1998;50:562.
Gribel B, Gribel M, Frazao D, McNamara J Jr, Manzi F. Accuracy and reliability of craniometric measurements on lateral cephalometry and 3D measurements on CBCT scans. Angle Orthod. 2011;81:26–35.
Bell R. Computer planning and intraoperative navigation in orthognathic surgery. J Oral Maxillofac Surg. 2011;69:592–605.
Barbenel J, Paul P, Khambay B, Walker F, Moos K, Ayoub A. Errors in orthognathic surgery planning: the effect of inaccurate study model orientation. Int J Oral Maxillofac Surg. 2010;39:1103–8.
Schramm A, Gellrich NC, Schmelzeisen R. Navigational surgery of the facial skeleton. Berlin: Springer; 2007.
Vannier M, Marsh J, Warren J. Three dimensional CT reconstruction images for craniofacial surgical planning and evaluation. Radiology. 1984;150:179.
Altobelli D, Kikinis R, Mulliken F, et al. Computer-assisted three-dimensional planning in craniofacial surgery. Plast Reconstr Surg. 1993;92:576.
Hohlweg-Majert B, Schon R, Schmelzeisen R, et al. Navigational maxillofacial surgery using virtual models. World J Surg. 2005;29:1530.
Luebbers H, Messmer P, Obwegeser J, et al. Comparison of different registration methods for surgical navigation in craniomaxillofacial surgery. J Craniomaxillofac Surg. 2008;36:109.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Science+Business Media, LLC, part of Springer Nature
About this chapter
Cite this chapter
Carrao, V., Tofigh, M., Greenberg, A.M. (2018). Virtual Surgical Planning for Orthognathic Surgery. In: Greenberg, A. (eds) Digital Technologies in Craniomaxillofacial Surgery. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1532-3_6
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1532-3_6
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1531-6
Online ISBN: 978-1-4939-1532-3
eBook Packages: MedicineMedicine (R0)