Abstract
Recent advances about multiple-organ failure have highlighted several aspects of its diagnosis and management. However, broad areas remain undiscovered. The classic differentiation into two hits has been challenged with the discovery of mixed gene responses and prolonged clinical outcomes, leading to a new proposed concept, the persistent inflammation-immunosuppression catabolism syndrome (PICS). The incidence ranges between 15 and 40 % and associated mortality is six- to eightfold higher than patients without organ dysfunction. Current scoring systems are valid but are not useful for prognosis, as all of them lack specificity and sensibility for selected populations. Single organ dysfunction criteria has been revisited and revised: Berlin ARDS criteria, AKIN classification, and gastrointestinal failure. Physiopathology research has specially focused on gene involvement, neural regulation, and mitochondrial damage as future targets for innovative therapies. A search for early biomarkers is underway with limited results, and traditional nutritional support guidelines have been challenged.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute Lung Injury
- Acute Respiratory Distress Syndrome
- Migration Inhibitory Factor
- Sequential Organ Failure Assessment
- Disseminate Intravascular Coagulation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The presence or development of dysfunction and failure of organs and systems negatively impacts the outcome among severely ill surgical patients. This unfavorable course is the clinical manifestation of an imbalance between an excessive pro-inflammatory action, the systemic inflammatory response syndrome (SIRS), and an excess in the mechanisms of anti-inflammatory regulation, the compensatory anti-inflammatory response syndrome (CARS), leading to an immunoparetic state.
Multiple-organ dysfunction syndrome or multiple-organ failure syndrome (MODS/MOF) becomes a very interesting clinical entity because it raises many questions, a lot of them without definitive answers. In this chapter, we will demonstrate the state of the art of this entity regarding its epidemiology, different physiopathology hypothesis, scoring, clinical manifestations current approach, and treatment with special attention to metabolic and nutritional management.
The Concept of MODS/MOF
Even though concept of MODS/MOF seems easy to understand and identify, current reality is not so conclusive. Despite the fact that this entity is easily and well known, the origin has been subjected to different theories and presumed mechanisms. In a recent review from Baue identifies more than two dozen types of organ failure. The common framework used to detect MODS/MOF is based on the presence of symptoms, abnormal biochemical and/or hematologic tests, and the perturbations in mean arterial pressure and hourly urine output. Recent Surviving Sepsis Campaign guidelines describes organ failure as a state where organ function is acutely altered, such that homeostasis cannot be maintained without pharmacologic or mechanical interventions; and in its last review [1] describes the criteria to consider organ dysfunction or failure (Table 13.1). However, a conceptual dilemma remains: first, whether organ failure is a consequence of microcirculatory disturbances leading to an imbalance in organ metabolism and oxygen utilization, with severe damage, even death, in cellular structures, as it was initially described [2]; or secondly, if organ failure is due to an adaptive mechanism that allows cells protect organ function by diminishing their metabolism, and allowing a presumable recovery [3] (Fig. 13.1).
This dualism regarding the origin or primus movens in the development of MODS/MOF may be partially the result of the chronology and the clinical profile of this entity. Moore et al. [4] were the first authors to refer a biphasic course in the presentation of MOF among trauma patients. They described an early-onset MOF on days 0–3 after the initial trauma, and a late-onset MOF appearing on day 4. Moreover, others authors supported the hypothesis that affected organs in early MOF were lung, heart, and kidney, while on late MOF, liver, nervous system or gastrointestinal tract (GIT) were involved. This resulted in the concept of two-hit theory of MOF, considering GIT as an engine of the second “hit” resulting in the successive failure of organs [5]; according to other authors, the motor would be a nosocomial infection [6]. This theory is now under revision due to observations of different host responses after injury and the universal application of resuscitation protocols to prevent the potential failure of organs and systems.
Another issue to consider is the role of MODS concept as a precursor to MOF, allowing the clinician to apply therapies that would minimize organ damage and potentially restore function. Different prognosis scores around MODS concept have been created, as we will develop later in this review.
Epidemiology and Outcome
Controversy exists around the epidemiology of MOF. Its incidence ranges between 15 and 61 %. Reasons for this variation include differences in patient populations, scoring systems [7], and the clinical period where observations were made. Early observations demonstrated a very high incidence [8], but the latest studies exhibit a trend to a better outlook. Trauma patients have the lowest incidence of MOF ranging from 15 [9] to 25 % [10], in contrast to burn patients where the incidence can reach 40 % [11]. A recent observational, multicenter study performed in 79 ICUs in Spain, and in Latin America, on 7,615 trauma, medical, surgical, and cardiac critically ill patients over a 2-month period noted an incidence of 17.6 % [12].
MOF associated mortality among trauma patients is six- to eightfold higher than in trauma patients without MOF [9, 13]. Morbidity closely parallels mortality as patients with MODS/MOF have more days of mechanical ventilation, longer ICU and hospital lengths of stay and a higher number of nosocomial infections. Mortality is closely related to the number of organs systems that fail, hence a patient with four or more affected organs has a predicted mortality of 100 % [14, 15].
Patients who survive MODS/MOF exhibit greater mortality over time, even after been discharged. In a cohort study of 545 medical-surgical ICU patients with MODS followed for 1 year, global mortality was 52.9 %, 29.5 % in ICU, and 14.8 % at the hospital. Variables associated with delayed mortality include decreased functional condition and the need for readmission at the hospital [16]. In a recent multicenter Scottish study on 872 patients from ten ICUs, authors described a 5-year mortality of 58.2 %, 34.4 % of which were within 28 days. They concluded that cardiovascular, respiratory, and liver failure during their stay were potent independent factors associated with this adverse prognosis [17]. This data supports previous reports demonstrating that patients who suffered MOF had 3.9 times greater odds for assistance in daily activities than those without MOF.
Scoring Systems
As there is no concise definition for MOF different MOF scores systems have been developed to stratify grades of organ dysfunction, and to predict outcome.
The four commonly accepted and applied scoring systems are: the Denver postinjury multiple-organ failure score; the Marshall score, the logistic organ dysfunction system (LODS) score (more commonly utilized in Europe) [18], and the sequential organ failure assessment (SOFA) score [19]. Differences exist among them regarding number of organs and systems to be checked and the grades of severity and limits for each step in each organ system (Table 13.2). The Denver score considers four organs and four grades; meanwhile LODS, Marshall, and SOFA scores accept six organs or systems and five grades. The definition of grade varies among the former three, moreover the weight of each dysfunction is different. A parameter very useful in these scores is the value delta, which means the maximum difference between the initial value and the highest score obtained during the patient’s stay; thus it is common to use delta SOFA or delta MODS.
The Marshall score was validated on surgical ICU patients, and has been found to be a predictive of mortality using both raw score and a delta MODS [8]. These findings were confirmed in a prospective observational cohort study on 1,200 mechanically ventilated patients performed in Canada [20]. The SOFA score has been validated in medical-surgical ICU patients and multiple patient populations (sepsis, cardiovascular, trauma, peritonitis, burns) [21, 22]. Although not designed for prognosis, a SOFA greater than 15 has been correlated with a mortality rate of 100 % according to a multicenter prospective study in 1,449 ICU patients. Furthermore, among the patients who remained in ICU more than 1 week, an increase of the SOFA score was associated with worse outcome [23]. In another multicenter prospective observational study on 1,340 ICU patients with MODS, those with SOFA score 10 or higher for 5 or more and an age greater than 60, had a mortality rate of 100 %.
The LODS score has been developed through a multiple logistic regression on 13,152 ICU patients in 12 countries [18]. The LODS allows the determination of the degree of organ dysfunction, as well as the prediction of mortality. In one French multicenter prospective study on 1,685 ICU patients comparing daily LODS vs. SOFA scores during the first 7 days of stay, both scores displayed good accuracy for both prognosis and the prediction of mortality.
Sauaia et al. [24], in a validation of the Denver and Marshall scores, concluded that both were useful tools but that the Denver score showed a greater specificity for mortality and ventilator free days (higher than 70 %). However, the sensitivity and specificity for days of mechanical ventilation and ICU length of stay in the intensive care unit were under 70 %.
Peres-Bota et al. [25] compared LODS and SOFA scores, and concluded that both were accurate predictors of outcome; nevertheless, patients in shock or with cardiovascular dysfunction, the SOFA score was a better predictor. This difference has also been found in patients with severe traumatic brain injury. In a prospective cohort study, the SOFA scoring system better discriminates both mortality and neurologic outcome [26].
Since MODS/MOF scores have been developed using different modalities (literature reviews, panel of experts, logistic regression), and on varied patient populations (trauma, surgery, mixed ICU, medical), it seems evident that their strength is their stratification of organ dysfunction in general, but their weakness there is a loss of accuracy in specific populations [27]. This is the reason for the development of disease-specific scoring systems.
Disease-specific scoring systems include the Glasgow Coma Scale (GCS) for evaluation of central nervous system dysfunction; risk injury failure end stage renal disease (RIFLE) [28] and acute kidney injury network (AKIN) [29] classification of renal involvement; Child-Pugh score for liver failure [30, 31]; and lung injury score (LIS) for patients with acute respiratory distress syndrome (ARDS) [32].
At this point it should be clear that organ dysfunction scores are not designed for outcome prediction. The Acute Physiology and Chronic Health Evaluation (APACHE) scale, the simplified acute physiology score (SAPS), or mortality probability model (MPM) are better able to predict outcome.
Pathophysiology
General Mechanisms
Dysfunction and/or failure of organs and systems are following multiple different types of injury. Despite this, a detailed and definite knowledge about the pathophysiology remains incomplete, even in the bimodal model proposed by Moore.
However, general mechanisms that uncouple in the presence of MODS/MOF after any of these entities are quite well known. The inciting event could either be septic or non-septic; nevertheless, both trigger a common inflammatory response through activator molecules, coming from microorganisms or their products, damaged tissues, denatured proteins from dying cells, or even foreign bodies. Those activators, known as PAMP (pathogen-associated molecular patterns), accomplish their activity either directly or through the activation of cytokines and other inflammatory mediators, generating biologic and metabolic effects resulting in the clinical syndrome of MOF.
PAMPs may be divided into microbial origin and non-microbial origins. The best known microbiologic PAMPs are lipopolysaccharide (LPS), lipoteichoic acid, peptidoglycan, phenol-soluble modulin. Non-microbiologic PAMPs include allergens, toxic compounds, and lipoproteins.
Immunologic identification of damaged tissues is mediated by intracellular proteins or by other mediators coming from damaged cells called alarmins. For some authors alarmins and PAMPs together are called damage-associated molecular patterns (DAMP), although for some others DAMP are synonymous with alarmins. Characteristics of alarmins include release from necrotic cells (not apoptotic), or release from living immune cells by means of endoplasmic reticulum or Golgi apparatus. The ability to recruit and activate of other immune cells where receptors are expressed and the capacity to restore lost hemostasis to injured tissues are also characteristics of DAMPs.
DAMPs such as alarmins are recognized by immune cells receptors identified as pattern-recognition receptors (PRR) resulting in activation of innate immunity and a generalized inflammatory response. Many receptors have been described, including triggering receptor expressed on myeloid cells (TREM 1), receptor of advanced glycation end products (RAGE), macrophage scavenger receptor (MSR), K+ channels, CD11/CD18 receptors, CD55, CXCR4 chemokine receptor, CD180, heat shock protein 70/90 Receptor (Hsp70/Hsp90), but the best known are TOLL-like receptors (TLR) and nucleotide-binding oligomerization domain (NOD)-like receptors (NLR), formerly named NOD. PRRs trigger changes in transcription factors; the best known of which is NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells), the control of transcription of nuclear DNA, and resulting in altered regulation of genes responsible for both innate and adaptive immune responses.
Activation of host response to injury is independent of the type of stimulus. Adaptive immunity occurs concurrently, once B-cell receptors are activated. Activation and ultimate cellular recruitment are performed by cytokines and some of the alarmins. Cytokine production tends to be brief and time-limited in response to a stimulus. Cytokines can be divided in two big groups, pro-inflammatory (e.g., TNF-a, IL-1b, IL-6, IL-12, IL-17, INF-c) and anti-inflammatory (e.g., IL-1ra, IL-4, IL-6, IL-10, IP10, IL-13, TGF-b, sTNFR p55, p75, sIL-6R), though some of them (e.g., IL-6) can share both characteristics according the inflammatory milieu. In addition to the large constellation of cytokines involved in the inflammatory response, different alarmins have been recognized as active clinical agents [33], including S100 proteins, calcium pyrophosphate dihydrate (CPPD); spliceosome-associated protein 130 (SAP130), uric acid and monosodium urate crystals, DNA, mitochondrial DNA, RNA, ATP, hyaluronan, biglycan, heparin sulfate, formylpeptides, and cholesterol crystals. Among alarmins, it is also worth highlighting heat shock proteins (HSP), high mobility group box 1 (HMGB1), and macrophage migration inhibitory factor (MIF).
Some members of the HSP family, HSP60 and HSP70, can be detected in serum. As signal molecules, they have a global pro-inflammatory activity, but may also attenuate ischemia-reperfusion injury (oxidative injury) and protect endothelial cells from neutrophil mediated necrosis.
HMGB1 is a nuclear protein that binds DNA and modulates transcription and chromatin remodeling, and facilitates the binding of transcription factors and nucleosomes. It is produced by injured, dying, or stressed cells, as well as by macrophages and other immune cells. It is involved in the stabilization of nucleosomes and the facilitation of gene transcription through the modulation of the activity of steroid hormone receptors. MHBGN1 also induces maturation of dendritic cells and has activity as chemokine, since its effects are also exerted in the endothelium. It binds to TLR4, increasing the release of pro-inflammatory mediators, and interacts with RAGE receptors. It mediates fever and anorexia, and is considered a late mediator of sepsis (8–32 h). High concentrations have been associated with clinical deterioration. HMGB1 can also be considered a trigger in the stimuli which activate innate immunity [34]. In experimental studies, blocking HMGB1 with polyclonal antibodies protects from lethal entodoxinemia and from acute lung injury (ALI). HMBG1 blocking agents may be considered as a therapeutic target.
MIF protein is constitutively expressed in large quantities by epithelial cells of the lung and kidney, immune cells (macrophages, eosinophils), and endocrine cells (pituitary), and is released by following exposure to inflammatory cytokines or bacterial products. It modulates the immune response through TLR4, allowing quick response of macrophages [35]. In situations of severe sepsis and septic shock, high levels of MIF have been detected, activating a pro-inflammatory response and increasing the secretion of cytokines by the upregulation TLR4 expression. MIF represents a putative biomarker and potential molecular target in ALI [36] and is detectable in the alveolar airspaces of patients with sepsis-induced ARDS [37].
MODS/MOF presentation is also related to imbalance in humoral responses. Complement system is clearly involved in this process [38]. Complement may be activated in three different pathways: the classic, mannose-binding lectin, and alternative pathways. All converge at the crossroads C3 to continue the cascade activation. The process releases large amounts of anaphylatoxin C5a. This is a central molecule in the inflammatory response, and exerts its effects through interactions with the C5AR and C5a-like receptor 2 (C5L2) receptors, which are upregulated during sepsis. The synergistic action of C5a and its receptors contributes, at an early state, to the inflammatory activity that turns into expression of tissue factor, and triggers the release of MIF and HMGB1. On the other hand, it facilitates an immunosuppression reaction through an induction of neutrophil dysfunction, and apoptosis of thymocytes and medullary adrenal cells. In animal model of sepsis, the blockade of C5a improved outcome and prevented MOF [39]. In a baboon model of sepsis, the use of the C5a inhibitor compstatin decreased the coagulopathic response by down-regulating tissue factor and PAI-1, reduced fibrinogen, fibrin-degradation products, and APTT, and preserved the endothelial anticoagulant properties [40]. Those findings might have implications on future complement-blocking approach in the clinical treatment of MODS/MOF.
Neural Regulation
The active participation of autonomic nervous system (ANS) in the control of inflammatory response opens new fields and perspectives for the understanding of MODS/MOF physiopathology. Stimulation of the adrenergic system leads to an amplification in pro-inflammatory behavior, particularly during the first steps of injury and organ dysfunction, whereas the activation of cholinergic system prompts an anti-inflammatory trend. Catecholamines released in adrenal glands and in neurons of the sympathetic system act through α and β-adrenergic receptors expressed on different types of cells. In the other hand, anti-inflammatory effects of cholinergic pathway are mediated through α7 nicotinic acetylcholine (ACh) receptors (α7nAChRs) [41]. Vagal nerve stimulation releases acetylcholine that inhibits pro-inflammatory molecules such as HMGB1 and TNF. Activation of the α-7 receptors with nicotine in an animal model of sepsis has shown an improvement of inflammation and an increase on survival [42].
Microvascular Milieu
The molecular storm triggered by host response to injury occurs in the microvascular environment. Normal endothelium performs two essential roles. It regulates blood vessel tone and it actively participates in leucocytes recruitment, directing them to sites where the cellular damage and inflammation occur. This process is mediated through the expression of adhesion molecules (ICAM, VCAM, ELAM) that are able to bind to leucocyte integrins CD11/CD18 and initiate leukocyte diapedesis and migration through endothelial wall. This process results in high levels of nitric oxide (NO) by monocytes inducible NO synthase (iNOS), which converts l-arginine to l-citrulline. NO acts as free radical and is a modulator of the vascular tone, causing vasodilatation, increased vascular permeability and organ dysfunction. Free radical formation is a result of inhibition of mitochondrial function, leading to a decrease in TPA synthesis and an increase of reactive oxygen species (ROS), generating peroxynitrite. Action of ROS on cells contributes to important changes in release of lipid substrates such as series 2 prostaglandins (PG2) and series 4 leukotrienes (LT4) with additional pro-inflammatory and pro-aggregate activities.
Alterations in the coagulation and fibrinolytic cascades also occur at the level of the endothelium. Pro-coagulant activity is upregulated, mediated by thromboxan A2, plasminogen activator inhibitor (PAI), platelet activating factor (PAF), and von Willebrand factor. There is also an associated downregulation of anticoagulant activity factors, including thrombomodulin, protein C receptor, and tissue plasminogen activator (t-PA).
Metabolic changes at the level of the endothelium, combined with hypoxia leads to intravascular platelet aggregations and microvascular thrombosis, manifesting clinically as fever, chills, tachycardia, tachypnea, agitation, and a subsequently organ dysfunction if homeostasis cannot be restored [43]. The association between organ failure and endothelial cell damage has been established by Shapiro et al. [44] in septic patients, who measured levels of vascular endothelial growth factor (VEGF), a stimulator of permeability, and its receptor sFLT. They concluded that sFLT levels correlated with measured initial SOFA and SOFA at 24 h; VEGF and sFLT levels also correlated with inflammatory cascade activation. A second study by the same investigators, performed in patients with sepsis further supports the strong role of the microcirculation in the genesis to MODS/MOF. They measured a broad panel of endothelial activation markers including sVCAM-1, sICAM-1, sE-selectin, PAI, VEGF and sFLT-1, and found an association between endothelial activation and subsequent organ dysfunction and mortality. sFLT-1 was the marker with the strongest association with SOFA score [45]. Animal models also demonstrate a relationship between high levels of angiopoietin-2 (Angpt-2), an endothelial protein released upon inflammatory stimulation, and SOFA measurements [46]. Sakr et al. [47] measured microcirculatory perfusion on 46 patients with septic shock and noted that decreased microcirculatory flow was associated with the development of multiorgan failure and death. With the same methods, Trzeciak et al. [48] stated that an increase of microcirculatory flow during resuscitation was associated with reduced organ failure.
Consequently, derangement of microcirculation seems to play a very important role, as the first hit in the presence of multiple-organ failure, while late multiple-organ dysfunction may be associated with mitochondrial failure [49].
Mitochondrial Role
Mitochondrial function has emerged as one of the cornerstones of MODS/MOF genesis. Release of pro-inflammatory cytokines and other mediators, together the release of great amounts of NO and ROS, and a maldistribution of macrovascular and microvascular blood flow, affects the mitochondrial function and energy production. If the inciting stimulus continues, mitochondrial energy is severely compromised, a situation which may be reversed by regeneration of new mitochondria as the patient enters in a recovery state [50].
The classic interpretation of decreased mitochondrial function is that cells die and organs fail due to a lack of energy, but an alternative hypothesis has been postulated by Singer [51], based in the observation that cell necrosis is not a key feature of the response to sepsis. Singer proposed that the decline in mitochondrial function is a protective response, with cells entering a hibernation-like state, and MODS/MOF would be a manifestation of the “physiologic shutdown.” This process could be reversed with the generation of new functional mitochondria and a recovery of energy, subsequent metabolic restoration, and clinical improvement. This regeneration, called biogenesis, seems to be triggered by NO production and mitochondrial DNA oxidative damage [52]. In the other hand, if sepsis persists, hibernation stops being playing an adaptive and potentially protective role, and shifts to a pathologic and harmful situation.
Others have supported this hypothesis. Haden et al. [53], in a murine model of peritonitis, found during recovery an increase in the mitochondrial biogenesis with restoration of oxidative metabolism. Brealey et al. [54], in a study based on skeletal muscle biopsies on 28 septic ICU patients, reported an association between NO overproduction, antioxidant depletion, mitochondrial dysfunction, and decreased ATP concentrations related to organ failure and outcome.
Carré et al. [55] studied biogenesis responses in muscle biopsies on 16 critically ill patients with MOF, at their admission to ICU, vs. 10 patients submitted to elective hip surgery as control group. Their study showed that muscle mitochondrial capacity was decreased soon after ICU admission, especially among non-survivors. However in the group of ICU survivors, early mitochondrial biogenesis and antioxidant defense responses were found. These authors conclude that an over-exuberant response to sepsis could increase susceptibility to mitochondrial damage, cellular energetic dysfunction, and would prevent the recovery of normal function.
However, criticism has arisen due to the heterogeneity of the body of evidence. Diversion among the methodology of different studies on mitochondrial dysfunction has prompted criticism of the proposed theories and interpretation of the conclusions. As has been pointed out by Jeger et al. [56], a consensus definition for “mitochondrial dysfunction” seems to be missing. Even in human studies, only the musculoskeletal and circulatory systems have been studied, although MOF affects numerous other organ systems. Answers to these questions need new tools for mitochondrial function assessment such as dynamic and biological tests providing new and complementary information.
Genomics
Recent genomic studies have contributed to a new understanding to physiopathology and timing of MOF. The generally accepted biphasic “two hit” model, fueled by gastrointestinal tract dysfunction (GITD), by nosocomial infection, or by new surgery, must be revisited due to new insights related to the expression of pro and anti-inflammatory genes.
Xiao et al. [57] studied a cohort of 167 adult severe blunt trauma patients who presented in shock requiring transfusion and evaluated the leukocyte transcriptome at several time points over 28 days. The authors found the expression of more than 80 % of leucocyte transcriptome was significantly altered in a way described as “genomic storm,” changes that occurred rapidly (4–12 h) and continued for days and weeks. The “genomic storm” included both inflammatory and anti-inflammatory gene upregulation and was independent of inciting stimulus (trauma, burns, low dose of endotoxin). Moreover, the gene profile showed similar behavior despite patient outcome (complicated and uncomplicated recovery). These authors propose a new paradigm for the inflammatory response where changes in the expression of systemic inflammatory genes, and anti-inflammatory and adaptive genes, occur early and concurrently, not sequentially. Interestingly, complicated recovery is not related to a different leucocyte transcriptome pattern, but with a prolongation in this gene expression profile [58]. This paradigm reappraises the classical diagram of two curves explaining SIRS, CARS, MOF and outcome, and substitutes it by a new model. Partially based in this concept, Gentile et al. [59] have coined a new clinical entity they called “persistent inflammation-immunosuppression catabolism syndrome” (PICS), encompassing those ICU patients who remain with manageable organ dysfunctions but usually do not meet established criteria for late MOF (Fig. 13.2). Poor nutritional status, poor wound healing, immunosuppression, and recurrent infections characterize their clinical course.
Clinical Presentation
Lung
The lung is one of the most frequently affected organs in the course of MODS/MOF. Pulmonary dysfunction has been well studied since the study of Asbaugh et al. in 1967 [60]. Its incidence has reached approximately 190,000 cases per year in the United States [61], and mortality in the more severe forms is 40–60 %. Its clinical presentation was formerly classified by the American-European Consensus Conference Committee [62] as ALI if PaO2/FiO2 < 300, and ARDS if PaO2/FiO2 < 200. Nevertheless, this definition has been very recently changed. However these definitions have been revised by the European Society of Intensive Care Medicine, the American Thoracic Society, and the Society of Critical Care Medicine [32] in order to improve case recognition and better match treatment options to severity, in both research trials and clinical practice [63]. In the new classification ALI concept disappears and ARDS is classified as: mild (200 < PaO2/FiO2 ≤ 300 with positive end expiratory pressure (PEEP) or continuous positive airway pressure (CPAP) ≥ 5 cm H2O); moderate (100 < PaO2/FiO2 ≤ 200 with PEEP ≥5 cm H2O); and severe (PaO2/FiO2 ≤ 100 with PEEP ≥5 cm H2O).
The inflammatory response and resultant increase in lung vascular permeability promote an alveolar invasion of activated neutrophils, red blood cells, and fibrin-rich fluid, resulting in damage to alveolar epithelium and a denuded alveolar basement membrane with loss of type I cells [64]. This drives the formation of hyaline membranes, inactivation of surfactant, and finally collapse of the alveoli [65].
Clinically, ARDS is manifested as a rapid onset of respiratory failure due to arterial hypoxemia that is refractory to treatment with supplemental oxygen. Radiological findings include bilateral infiltrates described as patchy or asymmetric, with or without including pleural effusions, consolidation, and atelectasis. If ARDS progresses, an increased alveolar dead space and a decrease in pulmonary compliance result.
Kidney
The kidney is a commonly affected organ in MODS/MOF. The prevalence of acute kidney injury/failure is approximately 60 % in patients with MODS/MOF [28], with associated mortality rates between 26 and 64 % [66].
A previous definition for acute renal failure (ARF) was developed following RIFLE criteria [67]. Recently, a newer definition of AKI has been coined [68], and finally, a new consensus from the kidney disease: improving global outcomes (K-DIGO) group [69] has been issued to address the entire spectrum of ARF. Diagnostic criteria for AKI are a reduction (within 48 h) in kidney function currently defined as an absolute increase in serum creatinine of greater than or equal to 0.3 mg/dL (≥26.4 μmol/L), an increase in serum creatinine of greater than 50 % (1.5-fold from baseline), or documented oliguria of less than 0.5 mL/kg/h for more than 6 h. The Consensus Conference has also proposed a three grade staging system based on quantitative changes in serum creatinine and urine output (based on RIFLE criteria).
The pathophysiology of AKI is uncertain and factors such as hypovolemia, inflammatory response, neuronal mechanisms, coagulopathies, renal arterial vasoconstriction have been implicated. Sepsis, major surgery (especially open heart surgery), and acute decompensated heart failure are also common triggers of acute kidney injury [70].
As AKI is often a result of renal hypoperfusion, rapid resuscitation is best first step in the treatment of AKI. Ideally, one or more biomarkers would exist to aid in the early identification of AKI Biomarkers under study include urinary neutrophil gelatinase-associated lipocalin (uNGAL), urinary hepatocyte growth factor (uHGF), urinary cystatin C (uCystatin C), kidney injury molecule-1 (KIM-1), N-acetyl-β-d-glucosaminidase (NAG), monocyte chemotactic peptide (MCP-1), Il-18, liver-type fatty acid-binding protein (L-FABP), and netrin-1. According to early results, these markers can identify patients with a renal dysfunction prior to the development of a high creatinine level [71] and they may increase the possibility for recovery [72]. Moreover, it has been suggested that they could reflect different etiologies of AKI. Cystatin C can predict changes in glomerular filtration rate, whereas neutrophil gelatinase-associated lipocalin is related to tubular stress or injury [73]. At present, it is necessary to better understand these biomarkers before adopting them in current clinical practice [73].
Cardiovascular System
The cardiovascular system can be affected via myocardial dysfunction, refractory peripheral vasodilatation, or a combination of the two.
Septic injury often results in cardiovascular derangement, and neural mechanisms may be implicated as cardiac autonomic dysfunction, clinically displayed as rhythm disturbances. Cardiac myocytes may be also directly damaged by PAMP such as endotoxin [74] and by NO and its substrate peroxynitrite which induce mitochondrial impairment and a diminished cardiac contractility. This septic cardiomyopathy is characterized by a global cardiac enlargement with biventricular contractility impairment, and a striking reduction in left ventricular (LV) ejection fraction and stroke work index [75]. A good biomarker for diagnosis and for assess the degree of ventricular dysfunction are troponins.
Vascular dysfunction is characterized by microvascular and endothelial impairment, decreased vasoconstrictor tone and a vascular hyporesponsiveness to vasopressor agents [76] resulting in resistant hypotension. Involved mechanisms seem to be the same as in cardiac dysfunction, with a preponderant role for NO and its metabolites. However, adrenal insufficiency, anomalous catecholamine signaling, damaged potassium channels, even hyperglycemia are factors that could be also implicated [77].
Nervous System
Neurological dysfunction in MODS/MOF is represented by two different entities, residing each one in different zones in the nervous system. Disturbances in mental status, confusion, delirium, even coma are very frequent in severe sepsis and septic shock [78]. Sepsis-associated encephalopathy (SAE) occurs in up to 87 % of septic patients, and is of unknown pathophysiology. Putative etiologies include aromatic amino acids and cytokines crossing blood–brain barrier, oxidative stress, or decrease of cerebral blood flow. Electroencephalogram is a sensitive test for the diagnosis of SAE when the patient is sedated and mechanically ventilated, while biomarkers such as S100B protein could be also useful but need more study prior to widespread clinical use. SAE is potentially reversible, but its presence is a poor prognostic indicator [79].
The other great complication in neural dysfunction axonal polyneuropathy named critical illness polyneuropathy (CIP), resulting in generalized weakness and difficulty weaning from mechanical ventilation. As in the case of SAE, its origin and pathophysiology remain unknown, although hyperosmolality, parenteral nutrition, non-depolarizing neuromuscular blockers, and neurologic failure are associated with its development. CIP is significantly associated with an increase in the mortality [80], duration of mechanical ventilation and in the lengths of intensive care unit and hospital stays [81].
Gastrointestinal Tract
The gastrointestinal tract (GIT) is a commonly affected organ in MODS/MOF, caused variably by compromised blood flow, structure damage, inappropriate cell function, alteration of metabolic activity, and impairment of the gastrointestinal barrier itself [82]. The effects of MODS/MOF on intestinal absorption are not fully understood.
Intestinal absorption of amino acids is regulated by three mechanisms: quantity of intraluminal substrate, capacity of the transport systems, and ability of the enterocyte to metabolize the substrates. This absorption is impaired as demonstrated by Gardiner & Barbull [83] in a model of septic rats, where a decrease in the intraluminal concentration of amino acids (arginine, leucine, and proline) occurred. Intestinal transport of amino acids has been studied in septic patients by analyzing the vesicles on the edge of the intestinal lining [84], and the release of glutamine, alanine, and leucine were considerably decreased with respect to the control group. The transport of substrates through intestinal wall is also inhibited as a result of the decrease of mesenteric blood flow and subsequently, owing to an increase of anaerobic metabolism, there may be decreased stores of ATP and reduced active transport of intraluminal substrates.
Both mechanisms reduce the ability of the intestinal lumen to absorb nutrients, and this event can limit the availability of intracellular substrates for the maintenance of metabolic functions and the enterocyte barrier [85]. Consequently, the reduced intestinal absorption in MODS/MOF may limit the use of enteral feeding. If we also consider the fact that malnutrition is common in these patients and that there is often a gastrointestinal paresis or dysfunction, it is clear that nutritional requirements often cannot be met and it is necessary to resort to total or supplementary parenteral feeding [86], even though this type of mixed feeding has been criticized by some researchers [87].
A very interesting controversy is to consider gastrointestinal failure (GIF) as a motor for development of secondary MOF since GIT lumen is loaded with a great number of bacteria and an increase of permeability would allow a massive translocation of bacterial products. This hypothesis, raised by Marshall et al. [5], considered gut as an “undrained abscess” and bacterial translocation is supported by different experimental studies [88]. Although inflammatory GIT damage, bacterial translocation, and development of subsequent failure of other organs become a frequent clinically found association, causality has not been proven. It is possible that the increase of the GIT permeability and translocation are epiphenomenons that occur alongside to other organ dysfunctions and not its motor. In a recent study, aiming to develop a GIF score for 28-day mortality prediction of ventilated patients [89], authors concluded GIF is often secondary and not the primary cause of other organ failure.
This conclusion leads to another important issue in GIF, the need of a definition and the development of a specific score for stratifying and, if possible, predicting this organ dysfunction. The search for accurate markers has not yielded satisfactory results, although plasma citrulline, an amino acid mainly synthesized from glutamine by enterocytes, has been studied as possible marker for small bowel function [90]. Their clinical utility in diagnosis and management of GI dysfunction (GITD) remains to be verified. Currently, two types of GITD are seen in MOF, intra-abdominal hypertension (IAH) [91] defined by a sustained increase in intra-abdominal pressure equal to or above 12 mmHg as measured by bladder pressures; and the presence enteral feeding (EF) intolerance. Malbrain and De Laet [92] coined the term Acute Intestinal Distress Syndrome based on IAH measurements. Reintam et al. [93] elaborated a GIF score based upon the occurrence of feeding intolerance and IAH, ranging from level 0 (normal gastrointestinal function) to level 4 (abdominal compartment syndrome) based on a prospective, single-center, study on 264 mechanically ventilated. They concluded that mean GIF score during the first 3 days had a prognostic value for ICU mortality. Nevertheless, since feeding intolerance is a subjective measurement, an expert panel published of the results of a Conference Report defining terminology, definitions, and management of GI function in ICU setting [94]. In this consensus of the ESICM Working Group on Abdominal Problems, acute gastrointestinal injury (AGI) has been scored with four grades of severity: grade I = increased risk of developing GI dysfunction or failure (a self-limiting condition); AGI grade II = GI dysfunction (a condition that requires interventions); AGI grade III = GI failure (GI function cannot be restored with interventions); and AGI grade IV = dramatically manifesting GI failure (a condition that is immediately life-threatening). They also defined Primary AGI as associated with primary disease or direct injury to organs of the GI system, and Secondary AGI when developed as the consequence of a host response in critical illness without primary pathology in the GI system. Feeding Intolerance syndrome (FI) defined as a failure to tolerate at least 20 kcal/kg BW/day via enteral route within 72 h of feeding attempt or if enteral feeding had to be stopped for whatever clinical reason. Finally definitions for GI symptoms, and their respective managements, have been delineated: vomiting, gastric residual volume, GI bleeding, diarrhea, lower GIT paralysis, abnormal bowel sounds, and bowel dilatation.
An attempt to test the hypothesis that symptoms of GI dysfunction could be used as predictors separately and/or as part of SOFA was unsuccessful [69] as a valid GI dysfunction score does not improve its accuracy.
Liver
Liver dysfunction in MODS is less frequent than pulmonary, cardiovascular, or renal dysfunction. This is in some way surprising because crucial metabolic and immunological pathways occur in the liver. Moreover, it produces and releases high amounts of inflammatory substrates such as cytokines, bioactive lipids, and acute phase proteins [95].
Early dysfunction occurs within hours after injury and, produced by hepatosplanchnic hypoperfusion, resulting in acute increases in transaminases, lactate dehydrogenase, and bilirubin, and is often reversible with adequate resuscitation. Late dysfunction is caused by inflammatory molecules and/or sterile DAMP, and characterized by structural and functional injury [96]. The liver is an organ with large populations of Kupffer cells and natural killer (NK) cells that are able to induce a high rate of expression of endothelial adhesion molecules [97]. It is remarkable that late hepatic failure has increased production of inflammatory cytokines in the hepatosplanchnic area, despite increased hepatic blood flow [98]. Dysfunction in the GI tract is also a putative mechanism of liver dysfunction. Contributing agents for this gut-liver axis [99] would be intestinally induced cytokines.
Hematological System
Imbalance in the pro-coagulant and anti-fibrinolytic states may lead to the development of disseminated intravascular coagulation (DIC), resulting in increased mortality due to microvascular thrombosis and resultant end-organ ischemia. Fortunately, DIC is much less frequent than isolated thrombopenia or abnormal clotting times, but its diagnosis may be influenced by the different scores used by clinicians (JMHW DIC [100], ISTH overt DIC (ISTH DIC) [101], and JAAM DIC [102]). The three scoring systems have been evaluated [103] in a prospective study on 413 patients with different underlying diseases of DIC, and results displayed a high sensitivity with JAAM score, and high specificity ISTH overt-DIC diagnostic criteria. The three DIC scores may prognosticate poor patient outcome depending on the studied population [104].
Metabolic Disturbances
Metabolic disturbances in MODS/MOF are highly dependent on timing, the inflammatory status, and organs affected. The ebb and flow proposed by Cuthbertson [105] may not be relevant to the early resuscitation of patients. Metabolic derangements are characterized by the hypermetabolic response defined by Cerra [106] composed of hyperglycemia, increased protein catabolism, hyperlactacidemia, increased lipolysis, and hypertriglyceridemia. Hyperglycemia requires careful management and has gained significant attention due to its recognized association with increased mortality and morbidity [107]. Hypoglycemia, associated with hepatic failure, is a poor prognostic indicator.
Protein catabolism is fueled by the needs for gluconeogenesis, substrates for wound repair, acute phase reactants production, and substrates for enterocytes and immune cells. Urinary urea nitrogen excretion is greatly augmented in the first days of injury, especially in burns and trauma where catabolic daily losses higher than 25 g. are not uncommon.
Increased pro-inflammatory cytokines, mainly TNF, block some enzymes such as lipoprotein-lipase and contribute to a decrease of free fatty acids and a hypertriglyceridemia in a direct proportion to the severity of injury.
Resting energy expenditure (REE) is strikingly elevated at the initial phases of MODS/MOF [108], but as dysfunction progress, REE requirements decline [109]. In the same manner, albumin and hepatic protein synthesis are downregulated. These observations determine nutritional support, as we shall detail below.
Treatment
General Management
Treatment of MODS/MOF is based on three arms: prevention of its appearance, adequate resuscitation to avoid progression if present, and selective organ support.
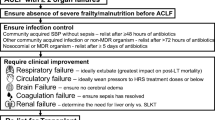
For prevention, an adequate fluid and oxygen support optimize oxygen delivery to tissues are mandatory. At the same time, any potential or real source of injury has to be addressed in a rapid fashion. According to Surviving Sepsis Campaign2 intervention has to be undertaken within the first 12 h after the diagnosis, if feasible, including, necrotizing soft tissue infection debridement, any emergency surgical procedure, burn wound excision, removal of suspected intravascular access devices, etc. If severe sepsis is present, appropriate empiric antibiotic treatment needs to be administered within the first hour of the recognition. Moreover, selective decontamination of the digestive tract (SDD) reduces the number of patients with multiple-organ dysfunction syndrome [110], although this treatment is controversial and no consistent improvement in mortality has been demonstrated. Blood transfusions should be avoided and a restrictive transfusion policy established [111]; even among critically ill non-bleeding patients with moderate anemia, red blood cell transfusion has no demonstrable benefits [112]. Glucose control is imperative since hyperglycemia has been associated to MODS/MOF through a mechanism of mitochondrial damage [113].
Once organ dysfunction is present, adequate resuscitation to preserve microcirculation and cellular metabolism is necessary. Careful hemodynamic monitoring, judicious use of vasopressors and fluids, and an approach minimizing the initial metabolic derailment are cornerstones in the management in this phase. The use of algorithms and criteria for early identification in organ disorder may be useful [114].
There have been several recent criticisms about routine interventions in the setting of MOD/MOF. A meta-analysis of Marik & Cavallazzi [115] has categorically disqualified the use of central venous pressure (CVP) as a guide for fluid therapy. The European Medicines Agency’s (EMA’s) Pharmacovigilance Risk Assessment Committee concluded that solutions containing hydroxyethyl starch (HES) are associated to a greater risk of kidney injury requiring dialysis and had a greater risk of mortality and recommended suspension of marketing authorizations for these solutions [116]. Norepinephrine is preferred over dopamine as the first-choice vasopressor, based on evidence that dopamine in septic shock is associated with an increased risk development of arrhythmias and death compared to norepinephrine [117]. β-2 agonist treatment in patients with ARDS should be limited to the treatment of important reversible airway obstruction but not in routine therapy; a multicentre, placebo-controlled, parallel-group, randomized trial on ARDS patients treated with intravenous salbutamol vs. a control group (BALTI-2 study), was stopped after the second interim analysis because an increased 28-day mortality. These results were concordant with previous where aerosolized albuterol in ALI was used [118].
Individual organ support is important and is restricted to pulmonary, cardiovascular, and renal support. Hematological failure can be restored with blood product administration. Recent recommendations about mechanical ventilation of ARDS have been issued regarding recommended tidal volume, plateau pressure, PEEP, recruitment manoeuvres, and patient positioning [2]. Renal replacements therapy can be instituted either by continuous renal replacement therapies or by conventional hemodialysis but the first issue is preferred in hemodynamically unstable patients [2]. Extracorporeal Membrane Oxygenation (ECMO) is only suggested for children with refractory respiratory failure of septic origin but it is not recommended for adults. Intra-aortic balloon pump (IABP) counterpulsation and left ventricular assist devices (LVAD) have rare indications in cardiac support for patients with secondary MODS/MOF and are reserved for primary and isolated refractory cardiac failure.
Nutritional and Tailored Substrates Support
Metabolic and nutritional support of these patients is one most complex challenge in the field of critical care. Strategies must take in account at least two considerations, the current inflammatory state and how many organs and at what extent are at failure or dysfunction. These considerations discourage the use of so-called “nutrients soup” formulations commercially labeled for injury or sepsis or MODS/MOF, and they justify the rationale for tailored substrates support.
The clinician’s approach nutritional repletion needs to consider if patient is in a pro-inflammatory state or in an immunoparetic period. At the first situation, substrates and formulations that are associated with a decrease of the inflammation have to be used; in the other hand, if patient is under CARS, immunostimulating formulas are appropriated (Table 13.3) as substrates can act as pharmaconutrients instead of simple nutrients [119]. For example, arginine may be appropriate early in the course of inflammation, inappropriate at the peak of systemic inflammation, and again appropriate in the recovery phase [120].
There is however a lack of studies on this topic of isolated substrates, as the great majority has been performed with commercially mixed formulations, and to extrapolate those results for the behavior of one particular substrate is difficult. Other challenges include directing nutritional support to address single vs. multiple-organ systems in failure.
Finally, and as an added problem for this issue, the presence of hyperglycemia requires careful control and may sometimes impact caloric support.
Arginine
Data regarding arginine repletion is conflicting. Some authors proposed that arginine should be avoided in infected critically ill patients, based on a meta-analysis [121] which concluded in infected critically ill patients immunonutrition may be harmful. The theory was based on the hypothesis of an overproduction of NO through arginine negatively impacts outcome. Other studies have demonstrated that plasma concentrations of arginine are clearly decreased in patients with sepsis in the absence of trauma or surgery [122].
Glutamine
Glutamine has long been well regarded in the nutritional support of injury, not only because it is an essential amino acid, but because its use has been associated with good outcomes in critical illness. Low plasma glutamine concentration is an independent predictor of poor. Wernerman et al. [123] in a multicenter, controlled, randomized, double-blind placebo-controlled study of intravenous glutamine administration tested the hypothesis that this support could improve SOFA scores and mortality. This study demonstrated lower mortality in the treatment arm, without significance when they were studied by intention to treat. Glutamine administration did not alter serial SOFA scores.
In another randomized, controlled, and double-blind study, glutamine supplementation did not reduce appearance of new infections, 6 months mortality, length of stay, SOFA score, nor the use of antibiotics [124].
However, a recent study demonstrated that glutamine repletion was associated with a reduced rate of infectious complications and a better glycemic control than the control group. However, there were no changes in SOFA, ICU and hospital length of stay, or mortality [125].
A recent multicenter, randomized, 2-by-2 factorial trial was performed on multiple-organ failure patients receiving mechanical ventilation who received nutrition supplemented with glutamine, antioxidants, both, or placebo (REDOXS) [126]. The primary outcome was 28-day mortality. Results were striking in that there was a trend toward increased mortality at 28 days among patients in the study group vs. control group (32.4 % vs. 27.2 %; adjusted odds ratio, 1.28; 95 % confidence interval [CI], 1.00–1.64; P = 0.05). Hospital morbidity and mortality at 6 months were significantly higher among those who received glutamine. They did not find any effect of glutamine on rates of organ failure or infectious complications. This study has aroused great controversy among scientific community. Criticism is mainly directed at the potential toxicity of the amount in glutamine support (60 % of total dietary protein), and in a presumed bias in allocation of patients according to the number of failing organs at baseline. According to REDOXS study, recommendations about glutamine support are maintained in EN in burn and trauma patients but a caution in patients with shock and MOF, given the possibility of increasing mortality.
Lipids
Omega-6 polyunsaturated fatty acids (ω-6 PUFA) are essential and required in the inflammatory response. In a recent study on patients with sepsis compared to healthy controls, arachidonic acid (AA) concentrations were more reduced among septic patients [127]. Gene expression studies confirmed a reduction of the induction of the expression of messenger RNA of cyclo-oxygenase 2 (COX-2). Likewise, authors concluded that reduction in the release of AA, and its metabolites, 11-HETE, PGE2, and TXB2 was associated with worse outcome.
Monounsaturated fatty acids (ω-9MUFA) and oleic acid metabolites are generally considered as less active than ω-6 PUFA in the setting of injury and organ failure. In a study of 100 critically ill mostly surgical patients receiving PN, and were randomly assigned to receive emulsions of soybean oil (ω-6) or olive oil-based fat emulsion (ω-9), did not demonstrate significant effects on mortality, length of stay, rates of infectious and noninfectious complications, glycemic control, oxidative stress markers, immune function and inflammatory markers [128].
These results confirm a previous, observational and prospective study [129], on a smaller number of critically ill patients receiving to PN, without differences between the control group (soybean oil) and the study group (olive oil-based fat emulsion), with regard to infection rate, variations on the protein levels of acute phase, clinical variables (stay, mortality), and leukocytosis. In fact, the study group had a trend toward greater leukocytes, challenging the assumptions that ω-9 have either a presumed anti-inflammatory or neutral effect.
Polyunsaturated fatty acids (ω-3 PUFA) have been studied in patients in MOF with ALI or ARDS. In a recent multicenter, controlled and randomized phase II trial patients received either enteral fish oil (9.75 g Eicosapentaenoic acid + 6.75 g Docosahexaenoic acid) or saline in EN. Outcome measures were the quantification of interleukin-8 levels in bronchoalveolar lavage. Authors concluded that fish oil did not reduce biomarkers of pulmonary or systemic inflammation in patients with ALI.
Rice et al. performed a randomized, double-blind, and multicenter placebo-controlled OMEGA study on patients with respiratory failure [130], to determine if the supplementation of the diet with ω-3 PUFA, γ-linolenic acid, and antioxidants would increase mechanical ventilation-free days. The study was stopped for futility and the authors concluded that supplementation did not improve the clinical outcomes of patients with ALI and may be harmful.
Another randomized, multicenter study examined the effects of an enteral diet enriched with Eicosapentaenoic acid, γ-linolenic acid, and antioxidants on the incidence of organ dysfunction and nosocomial infections in patients with respiratory, against a control group with standard enteral nutrition [131]. Results showed that there were not differences in PO2/FiO2 ratio, mechanical ventilation days or nosocomial infection rate.
Future Options
After more than a decade searching a magic bullet to block the inflammatory process has generated plenty of conflicting results, research is being directed to new approaches and new targets.
Inhibition of C5a in MODS/MOF of septic origin is promising, with preliminary results in rheumatoid diseases [132]. Mesenchymal stem cells may have an application due to the large number of studies supporting an immunosuppressive function of these cells [133] through production of activated molecules that enhance repair [134, 135].
Regulation of neural pathways is other promising strategy. ACE-inhibitors [ACEI] are known to ameliorate depressed autonomic function (heart rate variability [HRV]) and improve endothelial function; in an retrospective study on 178 MODS patients, ACEI treatment was associated with lower short- and longer-term mortality compared with patients without ACEI [136].
On the side of mitochondrial therapies, different therapies have been proposed targeting membrane stabilization, mitochondrial ROS scavenger, mitochondrial antioxidants, substrate and/or cofactor provision, with promising results in different [137] experimental studies.
The horizon for MODS/MOF therapy could be altered by advances in gene therapy [138], tissue regeneration and molecular reprogramming, in the term health engineering proposed by Cobb [139], where a joint approach of critical care, systems sciences, molecular engineering, computational biology, and applied mathematics would work for improving prognosis issues.
Conclusion
The appearance of MODS/MOF in the outcome of surgical patients is always a concern for clinician. Its presence is clearly associated with a worse prognosis and a heavy burden for hospital costs, although frequency and mortality are fortunately decreasing. MODS/MOF has been always contemplated to be initiated by an inflammatory response, but a different approach considering it as an adaptive mechanism mediated by mitochondrial switch off against the initial injury is gaining ground. Both may be present in the timeline of the process, and it could explain, together with the recent advances in genomic response, the revisited concept of late MOF and a new consideration for PICS. All the scoring systems lack sensitivity and specificity and are poor tools for prognosis. Several studies have produced an important advance in the knowledge of pro and anti-inflammatory pathways and their modulation. Potential therapeutic implications have been demonstrated, such as neural regulation or mitochondrial role, and new attempts have been made to evaluate the behavior of the microcirculation and tissue perfusion. In the clinical setting, a renewed interest in the validation of diagnosis criteria is taking place with new definition for ARDS, GIT failure, and AKI; and a searching for biomarkers that may detect dysfunction at early phase is underway. Regarding to treatment, search for a magic bullet has been abandoned and the efforts are directed to prevention and resuscitation. Several therapeutic postulates have been challenged, affecting not only resuscitative fluids but also metabolic and nutritional support. Fortunately, new targets for future therapies are emerging, as is the case for gene modulation, mesenchymal stem cells application, or different lines on mitochondrial therapies.
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal S, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228.
Eiseman B, Beart R, Norton L. Multiple organ failure. Surg Gynecol Obstet. 1977;144:323–6.
Singer M, De Santis V, Vitale D, Jeffcoate W. Multiorgan failure is an adaptive, endocrine-mediated, metabolic response to overwhelming systemic inflammation. Lancet. 2004;364(9433): 545–8.
Moore FA, Sauaia A, Moore EE, Haenel JB, Burch JM, Lezotte DC. Postinjury multiple organ failure: a bimodal phenomenon. J Trauma. 1996;40:501–10.
Marshall JC, Christou NV, Meakins JL. The gastrointestinal tract. The “undrained abscess” of multiple organ failure. Ann Surg. 1993;218(2):111–9.
Minei JP, Cuschieri J, Sperry J, Moore EE, West MA, Harbrecht BG, et al. The changing pattern and implications of multiple organ failure after blunt injury with hemorrhagic shock. Crit Care Med. 2012;40(4):1129–35.
Brattstrom O, Granath F, Rossi P, Oldner A. Early predictors of morbidity and mortality in trauma patients treated in the intensive care unit. Acta Anaesthesiol Scand. 2010;54:1007–17.
Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, et al. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38(2):185–93.
Dewar DC, Tarrant SM, King KL, Balogh ZJ. Changes in the epidemiology and prediction of multiple-organ failure after injury. J Trauma Acute Care Surg. 2013;74(3):774–9.
Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A. A 12-year prospective study of postinjury multiple organ failure: has anything changed? Arch Surg. 2005;140(5):432–8.
Kallinen O, Maisniemi K, Böhling T, Tukiainen E, Koljonen V. Multiple organ failure as a cause of death in patients with severe burns. J Burn Care Res. 2012;33(2):206–11.
Cabré L, Mancebo J, Solsona JF, Saura P, Gich I, Blanch L, et al. Multicenter study of the multiple organ dysfunction syndrome in intensive care units: the usefulness of Sequential Organ Failure Assessment scores in decision making. Intensive Care Med. 2005;31:927–33.
Ulvik A, Kvale R, Wentzel-Larsen T, Flaatten H. Multiple organ failure after trauma affects even long-term survival and functional status. Crit Care. 2007;11(5):1–8.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. Prognosis in acute organ-system failure. Ann Surg. 1985;202(6):685–93.
Zimmerman JE, Knaus WA, Sun X, Wagner DP. Severity stratification and outcome prediction for multisystem organ failure and dysfunction. World J Surg. 1996;20(4):401–5.
Hortigüela-Martín VA, Sanchez-Casado M, Rodríguez-Villar S, Quintana-Díaz M, Marco-Schulke C, Gómez-Tello V, et al. Post-Intensive Care Unit mortality and related prognostic factors in a cohort of critically ill patients with multi-organ dysfunction. Med Clin. 2013;140(11):479–86.
Lone NI, Walsh TS. Impact of intensive care unit organ failures on mortality during the five years after a critical illness. Am J Respir Crit Care Med. 2012;186(7):640–7.
Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C, Artigas A, Teres D. ICU Scoring Group. The logistic organ dysfunction system: a new way to assess organ dysfunction in the intensive care unit. JAMA. 1996;276:802–10.
Vincent JL, Moreno R, Takala J, Willatts S, de Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–10.
Cook R, Cook D, Tilley J, Lee KA, Marshall J. Multiple organ dysfunction: baseline and serial component scores. Crit Care Med. 2001;29(11): 2046–50.
Giannoni C, Chelazzi C, Villa G, Raffaele De Gaudio A. Organ dysfunction scores in ICU. Trends Anaesth Crit Care. 2013;3(3):89–96.
Lorente JA, Vallejo A, Galeiras R, Tómicic V, Zamora J, Cerdá E, et al. Organ dysfunction as estimated by the sequential organ failure assessment score is related to outcome in critically ill burn patients. Shock. 2009;31(2):125–31.
Vincent JL, De Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Crit Care Med. 1998;26(11): 1793–800.
Sauaia A, Moore EE, Johnson JL, Ciesla DJ, Biffl WL, Banerjee A. Validation of postinjury multiple organ failure scores. Shock. 2009;31(5):438–47.
Peres-Bota D, Melot C, Ferreira FL, Ba VN, Vincent JL. The multiple organ dysfunction score (MODS) versus the sequential organ failure assessment (SOFA) score in outcome prediction. Intensive Care Med. 2002;28(11):1619–24.
Zygun D, Berthiaume L, Laupland K, Kortbeek J, Doig C. SOFA is superior to MOD score for the determination of non-neurologic organ dysfunction in patients with severe traumatic brain injury: a cohort study. Crit Care. 2006;10(4):R115.
Vincent JL, Moreno R. Scoring systems in the critically ill. Crit Care. 2010;14:207–15.
Hoste EAJ, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10(3):1–10.
Molitoris BA, Levin A, Warnock DG, Joannidis M, Mehta RL, Kellum JA, et al. Improving outcomes of acute kidney injury: report of an initiative. Nat Clin Pract Nephrol. 2007;3(8):439–42.
Child CG. Surgery and portal hypertension. In: Child CG, editor. The liver and portal hypertension. Philadelphia, PA: WB Saunders; 1964. p. 50–72.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–9.
ARDS Definition Task Force. Acute respiratory distress syndrome. JAMA. 2012;307(23):2526–33.
Chen GY, Nuñez G. Sterile inflammation: sensing and reacting to damage. Nat Rev Immunol. 2010;10(12):826–37.
Andersson U, Tracey KJ. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol. 2011;29:139–62.
Calandra T, Roger T. Macrophage migration inhibitory factor: a regulator of innate immunity. Nat Rev Immunol. 2003;3(10):791–800.
Gao L, Flores C, Fan-Ma S, Miller EJ, Moitra J, Moreno L, et al. Macrophage migration inhibitory factor in acute lung injury: expression, biomarker, and associations. Transl Res. 2007;150(1):18–29.
Donnelly SC, Bucala R, Metz CN, Grant IS, Robertson CR, Haslett C. Macrophage migration inhibitory factor and acute lung injury. Chest. 1999;116 Suppl 1:111S.
Rittirsch D, Redl H, Huber-Lang M. Role of complement in multiorgan failure. Clin Dev Immunol. 2012;2012:962927.
Rittirsch D, Flierl MA, Nadeau BA, Day DE, Huber-Lang M, Mackay CR, et al. Functional roles for C5a receptors in sepsis. Nat Med. 2008;14(5):551–7.
Silasi-Mansat R, Zhu H, Popescu NI, Peer G, Sfyroera G, Magotti P, et al. Complement inhibition decreases the procoagulant response and confers organ protection in a baboon model of Escherichia coli sepsis. Blood. 2010;116(6):1002–10.
Rosas-Ballina M, Tracey KJ. The neurology of the immune system: neural reflexes regulate immunity. Neuron. 2009;64(1):28–32.
Tracey KJ. Reflex control of immunity. Nature. 2002;420:853–9.
Doerschug KC, Delsing AS, Schmidt GA, Haynes WG. Impairments in microvascular reactivity are related to organ failure in human sepsis. Am J Physiol Heart Circ Physiol. 2007;293(2):H1065–71.
Shapiro NI, Yano K, Okada H, Fischer C, Howell M, Spokes KC, et al. A prospective, observational study of soluble FLT-1 and vascular endothelial growth factor in sepsis. Shock. 2008;29(4):452–7.
Shapiro NI, Schuetz P, Yano K, Sorasaki M, Parikh SM, Jones AE, et al. The association of endothelial cell signaling, severity of illness, and organ dysfunction in sepsis. Crit Care. 2010;14(5):R182.
David S, Mukherjee A, Ghosh CC, Yano M, Khankin EV, Wenger JB, et al. Angiopoietin-2 may contribute to multiple organ dysfunction and death in sepsis. Crit Care Med. 2012;40(11):3034–41.
Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL. Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med. 2001;32(9):1825–31.
Trzeciak S, McCoy JV, Dellinger RP, Arnold RC, Rizzuto M, Abate NL, et al. Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Med. 2008;34(12):2210–7.
Trzeciak S, Cinel I, Dellinger RP, Shapiro NI, Arnold RC, Parrillo JE, et al. Resuscitating the microcirculation in sepsis: the central role of nitric oxide, emerging concepts for novel therapies, and challenges for clinical trials. Acad Emerg Med. 2008;15(5):399–413.
Singer M. Mitochondrial function in sepsis: acute phase versus multiple organ failure. Crit Care Med. 2007;35(9):S441–8.
Singer M. Mechanisms of sepsis-induced organ dysfunction and recovery update in intensive care and emergency medicine. Crit Care Emerg Med. 2007;44:299–310.
Harrois A, Huet O, Duranteau J. Alterations of mitochondrial function in sepsis and critical illness. Curr Opin Anaesthesiol. 2009;22(2):143–9.
Haden DW, Suliman HB, Carraway MS, Welty-Wolf KE, Al AS, Shitara H, et al. Mitochondrial biogenesis restores oxidative metabolism during Staphylococcus aureus sepsis. Am J Respir Crit Care Med. 2007;176:768–77.
Brealey D, Brand M, Hargreaves I, Heales S, Land J, Smolenski R, et al. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet. 2002;360:219–23.
Carré JE, Orban JC, Re L, Felsmann K, Iffert W, Bauer M, et al. Survival in critical illness is associated with early activation of mitochondrial biogenesis. Am J Resp Crit Care Med. 2010;182(6):745–51.
Jeger V, Djafarzadeh S, Jakob SM, Takala J. Mitochondrial function in sepsis. Eur J Clin Invest. 2013;43(5):532–42.
Xiao W, Mindrinos MN, Seok J, Cuschieri J, Cuenca AG, Gao H, et al. A genomic storm in critically injured humans. J Exp Med. 2011;208(13):2581–90.
Leavy O. Inflammation: trauma kicks up a storm. Nat Rev Immunol. 2011;12(1):3.
Gentile LF, Cuenca AG, Efron PA, Ang D, Bihorac A, McKinley BA, et al. Persistent inflammation and immunosuppression: a common syndrome and new horizon for surgical intensive care. J Trauma Acute Care Surg. 2012;72(6):1491–501.
Ashbaugh D, Boyd BD, Petty T, Levine B. Acute respiratory distress in adults. Lancet. 1967; 290(7511):319–23.
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Nef M, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–93.
Abraham E, Matthay MA, Dinarello CA, Vincent JL, Cohen J, Opal SM, et al. Consensus conference definitions for sepsis, septic shock, acute lung injury, and acute respiratory distress syndrome: time for a reevaluation. Crit Care Med. 2000;28(1):232–5.
Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38(10):1573–82.
Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342:1334–49.
Tsushima K, King LS, Aggarwal NR, De Gorordo A, D’Alessio FR, Kubo K. Acute lung injury review. Intern Med. 2009;48:621–30.
Bagshaw SM, Lapinsky S, Dial S, Arabi Y, Dodek P, Wood G, et al. Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med. 2009;35:871–81.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, The Acute Dialysis Quality Initiative Workgroup. Acute renal failure definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the Acute Dialysis Quality Initiative Group. Crit Care. 2004;8:R204–12.
Mehta RL, Kellum JA, Shah SV, The Acute Kidney Injury Network. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
The Kidney Disease Improving Global Outcomes (KDIGO) Working Group. Definition and classification of acute kidney injury. Kidney Int. 2012; Suppl 2:19–36.
Bellomo R, Kellum JA, Ronco C. Acute kidney injury. Lancet. 2012;380:756–66.
Haase M, Bellomo R, Devarajan P, Schlattmann P, Haase-Fielitz A. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;54:1012–24.
Srisawat N, Wen X, Lee M, Kong L, Elder M, Carter M, et al. Urinary biomarkers and renal recovery in critically ill patients with renal support. Clin J Am Soc Nephrol. 2011;6(8):1815–23.
Obermüller N, Geiger H, Weipert C, Urbschat A. Current developments in early diagnosis of acute kidney injury. Int Urol Nephrol. 2014;46(1):1–7. doi:10.1007/s11255-013-0448-5 [Epub ahead of print].
Werdan K, Schmidt H, Ebelt H, Zorn-Pauly K, Koidl B, Hoke RS, et al. Impaired regulation of cardiac function in sepsis, SIRS, and MODS. Can J Physiol Pharmacol. 2009;87(4):266–74.
Hunter JD, Doddi M. Sepsis and the heart. Br J Anaesth. 2010;104(1):3–11.
Matsuda N, Hattori Y. Vascular biology in sepsis: pathophysiological and therapeutic significance of vascular dysfunction. J Smooth Muscle Res. 2007; 43(4):117–37.
Levy B, Collin S, Sennoun N, Ducrocq N, Kimmoun A, Asfar P, et al. Vascular hyporesponsiveness to vasopressors in septic shock: from bench to bedside. In: Pinsky MR, Brochard L, Mancebo J, Antonelli M, editors. Applied physiology in intensive care medicine 2. Berlin: Springer; 2012. p. 251–61.
Lamar CD, Hurley RA, Taber KH. Sepsis-associated encephalopathy: review of the neuropsychiatric manifestations and cognitive outcome. J Neuropsychiatry Clin Neurosci. 2011;23:237–41.
Chelazzi C, Consales G, De Gaudio AR. Sepsis associated encephalopathy. Curr Anaesth Crit Care. 2008;19(1):15–21.
Garnacho-Montero J, Madrazo-Osuna J, García-Garmendia JL, Ortiz-Leyba C, Jiménez-Jiménez FJ, Barrero-Almodóvar A, et al. Critical illness polyneuropathy: risk factors and clinical consequences. A cohort study in septic patients. Intensive Care Med. 2001;27(8):1288–96.
Garnacho-Montero J, Amaya-Villar R, García-Garmendía JL, Madrazo-Osuna J, Ortiz-Leyba C. Effect of critical illness polyneuropathy on the withdrawal from mechanical ventilation and the length of stay in septic patients. Crit Care Med. 2005;33(2):349–54.
Ortiz-Leyba C, Ortiz-Moyano C, Jiménez-Jiménez FJ, Garnacho-Montero J, García-Garmendia JL. Nutritional support in severe sepsis. Clin Pulm Med. 2003;10(1):26–33.
Gardiner K, Barbull A. Intestinal amino acid absorption during sepsis. JPEN. 1993;17:277–83.
Salloun RM, Copeland EM, Souba WW. Brush border transport of glutamine and other substrates during sepsis and endotoxemia. Ann Surg. 1991; 213:401–10.
Groeneveld ABJ. Gastrointestinal exocrine failure in critical illness. In: Rombeau JL, Takala J, editors. Gut dysfunction in critical illness, Update in intensive care and emergency medicine, vol. 26. Berlin: Springer; 1996. p. 297–306.
Heidegger CP, Berge MM, Graf S, Zingg W, Darmon P, Costanza MC, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet. 2013;381(9864):385–93.
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011;365(6):506–17.
Louis K, Netea MG, Carrer DP, Kotsaki A, Mylona V, Pistiki A, et al. Bacterial translocation in an experimental model of multiple organ dysfunctions. J Surg Res. 2013;183(2):686–94.
Reintam A, Poeze M, Malbrain ML, Björck M, Oudemans-van Straaten HM, Starkopf J, Gastro-Intestinal Failure Trial Group. Gastrointestinal symptoms during the first week of intensive care are associated with poor outcome: a prospective multicentre study. Intensive Care Med. 2013;39(5):899–909.
Piton G, Manzon C, Cypriani B, Carbonnel F, Capellier G. Acute intestinal failure in critically ill patients: is plasma citrulline the right marker? Intensive Care Med. 2011;37(6):911–7.
Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, et al. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. I. Definitions. Intensive Care Med. 2006; 32(11): 1722–32.
Malbrain ML, De Laet I. AIDS is coming to your ICU: be prepared for acute bowel injury and acute intestinal distress syndrome. Intensive Care Med. 2008;34(9):1565–9.
Reintam A, Parm P, Kitus R, Starkopf J, Kern H. Gastrointestinal failure score in critically ill patients: a prospective observational study. Crit Care. 2008;12:R90.
Reintam A, Malbrain ML, Starkopf J, Fruhwald S, Jakob SM, De Waele J, et al. Gastrointestinal function in intensive care patients: terminology, definitions and management. Recommendations of the ESICM Working Group on Abdominal Problems. Intensive Care Med. 2012;38(3):384–94.
Dhainaut JF, Marin N, Mignon A, Vinsonneau C. Hepatic response to sepsis: interaction between coagulation and inflammatory processes. Crit Care Med. 2001;29:S42–7.
Spapen H. Liver perfusion in sepsis, septic shock, and multiorgan failure. Anat Rec. 2008;291:714–20.
Olanders K, Sun Z, Borjesson A, Dib M, Andersson E, Lasson Å, et al. The effect of intestinal ischemia and reperfusion injury on ICAM-1 expression, endothelial barrier function, neutrophil tissue influx, and protease inhibitor levels in rats. Shock. 2002;18(1):86–92.
Poeze M, Ramsay G, Buurman WA, Greve JWM, Dentener M, Takala J. Increased hepatosplanchnic inflammation precedes the development of organ dysfunction after elective high-risk surgery. Shock. 2002;17:451–8.
Soeters PB, Luyer MS, Willem J, Greve M, Buurman WA. The significance of bowel permeability. Curr Opin Clin Nutr Metab Care. 2007;10:632–8.
Kobayashi N, Maekawa T, Takada M, Tanaka H, Gonmori H. Criteria for diagnosis of DIC based on the analysis of clinical and laboratory findings in 345 DIC patients collected by the Research Committee on DIC in Japan. Bibl Haematol. 1987;49:848–52.
Taylor Jr FB, Toh CH, Hoots WK, Wada H, Levi M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation: on behalf of the Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Thromb Haemost. 2001;86: 1327–30.
Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, et al. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006;34:625–31.
Takemitsu T, Wada H, Hatada T, Ohmori Y, Ishikura K, Takeda T, et al. Prospective evaluation of three different diagnostic criteria for disseminated intravascular coagulation. Thromb Haemost. 2011;105: 40–4.
Iskander KN, Osuchowski MF, Stearns-Kurosawa DJ, Kurosawa S, Stepien D, Valentine C, et al. Sepsis: multiple abnormalities, heterogeneous responses, and evolving understanding. Physiol Rev. 2013;93(3):1247–88.
Cuthbertson DP. Post-shock metabolic response. Lancet. 1942;239(6189):433–7.
Cerra FB. Hypermetabolism, organ failure, and metabolic support. Surgery. 1987;101:1–14.
Van Den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–67.
Frankenfield DC, Oniert LA, Badellino MM, Wiles CE, Bagley SM, Goodarzi S, et al. Correlation between measured energy expenditure and clinically obtained variables in trauma and sepsis patients. JPEN. 1994;18(5):398–403.
Dickerson RN. Optimal caloric intake for critically ill patients: first, do no harm. Nutr Clin Pract. 2011;26(1):48–54.
Silvestri L, van Saene HK, Zandstra DF, Marshall JC, Gregori D, Gullo A. Impact of selective decontamination of the digestive tract on multiple organ dysfunction syndrome: systematic review of randomized controlled trials. Crit Care Med. 2010; 38(5):1370–6.
Leal-Noval SR, Muñoz M, Asuero M, Contreras E, García-Erce JA, Llau JV, et al. Spanish Consensus Statement on alternatives to allogeneic blood transfusion: the 2013 update of the “Seville Document”. Blood Transfus. 2013;11(4):1–25.
Leal-Noval SR, Muñoz-Gómez M, Jiménez-Sánchez M, Cayuela A, Leal-Romero M, Puppo-Moreno A, et al. Red blood cell transfusion in non-bleeding critically ill patients with moderate anemia: is there a benefit? Intensive Care Med. 2013;39(3):445–53.
Gunst J, Derese I, Aertgeerts A, Ververs EJ, Wauters A, Van den Berghe G, et al. Insufficient autophagy contributes to mitochondrial dysfunction, organ failure, and adverse outcome in an animal model of critical illness. Crit Care Med. 2013;41(1):182–94.
Levitt JE, Calfee CS, Goldstein BA, Vojnik R, Matthay MA. Early acute lung injury: criteria for identifying lung injury prior to the need for positive pressure ventilation. Crit Care Med. 2013;41(8): 1929–37.
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41(7):1774–81.
European Medicines Agency. Recommendation to suspend marketing authorisations for hydroxyethyl-starch solutions to be re-examined. 12 July 2013. EMA/349341/2013.
De Backer D, Aldecoa C, Hassane H, Vincent JL. Dopamine versus norepinephrine in the treatment of septic shock: a meta-analysis. Crit Care Med. 2012;40(3):725–30.
Home AJRCCM, Home AJRCMB, By Subject CME. Randomized, placebo-controlled clinical trial of an aerosolized β 2-agonist for treatment of acute lung injury. Am J Resp Crit Care Med. 2011;184(5): 561–8.
Jones NE, Heyland DK. Pharmaconutrition: a new emerging paradigm. Curr Opin Gastroenterol. 2008;24(2):215–22.
Ortiz-Leyba C, Montejo-González JC, Vaquerizo-Alonso C, Metabolism and Nutrition Working Group of the Spanish Society of Intensive Care Medicine and Coronary Units. Guidelines for specialized nutritional and metabolic support in the critically-ill patient: update. Consensus SEMICYUC-SENPE: septic patient. Nutr Hosp. 2011;26 Suppl 2:67–71.
Heyland DK, Novak F, Drover JW, Jain M, Suchner U. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. JAMA. 2001;286:944–53.
Davis J, Anstey N. Is plasma arginine concentration decreased in patients with sepsis? A systematic review and meta-analysis. Crit Care Med. 2011; 39(2):380–5.
Wernerman J, Kirketeig T, Andersson B, et al. Scandinavian glutamine trial: a pragmatic multi-centre randomised clinical trial of intensive care unit patients. Acta Anaesthesiol Scand. 2011;55:812–8.
Andrews PJ, Avenell A, Noble DW, Campbell MK, Croal BL, Simpson WG, et al. Randomised trial of glutamine, selenium, or both, to supplement parenteral nutrition for critically ill patients. BMJ. 2011;342:d1542.
Grau T, Bonet A, Miñambres E, Piñeiro L, Irles JA, Robles A, et al.; for the Metabolism, Nutrition Working Group, SEMICYUC, Spain. The effect of l-alanyl-l-glutamine dipeptide supplemented total parenteral nutrition on infectious morbidity and insulin sensitivity in critically ill patients. Crit Care Med. 2011;39(6):1263–8.
Heyland D, Muscedere J, Wischmeyer PE, Cook D, Jones G, Albert M, et al. A randomized trial of glutamine and antioxidants in critically ill patients. N Engl J Med. 2013;368:1489–97.
Bruegel M, Ludwig U, Kleinhempel A. Sepsis-associated changes of the arachidonic acid metabolism and their diagnostic potential in septic patients. Crit Care Med. 2012;40(5):1478–86.
Umpierrez GE, Spiegelman R, Zhao V, Smiley DD, Pinzon I, Griffith DP, et al. A double-blind, randomized clinical trial comparing soybean oil–based versus olive oil–based lipid emulsions in adult medical–surgical intensive care unit patients requiring parenteral nutrition. Crit Care Med. 2012; 40:1792.
Mateu-de Antonio J, Grau S, Luque S, Marín-Casino M, Albert I, Ribes E. Comparative effects of olive oil-based and soyabean oil-based emulsions on infection rate and leucocyte count in critically ill patients receiving parenteral nutrition. Br J Nutr. 2008;99(4):846–54.
Rice TW, Wheeler AP, Thompson BT, de Boisblanc BP, Steingrub J, Rock P, NIH NHLBI Acute Respiratory Distress Syndrome Network of Investigators. Enteral omega-3 fatty acid, γ-linolenic acid, and antioxidant supplementation in acute lung injury. JAMA. 2011;306(14):1574–81.
Grau-Carmona T, Morán-García V, García-de-Lorenzo A, Heras-de-la-Calle G, Quesada-Bellver B, López-Martínez J, et al. Effect of an enteral diet enriched with eicosapentaenoic acid, gamma-linolenic acid and anti-oxidants on the outcome of mechanically ventilated, critically ill, septic patients. Clin Nutr. 2011;30(5):578–84.
Wagner E, Frank MM. Therapeutic potential of complement modulation. Nat Rev Drug Discov. 2010;9:43–56.
Ghannam S, Bouffi C, Djouad F, Jorgensen C, Noël D. Immunosuppression by mesenchymal stem cells: mechanisms and clinical applications. Stem Cell Res Ther. 2010;1:2.
Groeneveld KM, Leenen LP, Koenderman L, Kesecioglu J. Immunotherapy after trauma: timing is essential. Curr Opin Anaesthesiol. 2011;24(2): 219–23.
Gotts JE, Matthay MA. Mesenchymal stem cells and acute lung injury. Crit Care Clin. 2011;27(3):719–33.
Schmidt H, Hoyer D, Rauchhaus M, Prondzinsky R, Hennen R, Schlitt A, et al. ACE-inhibitor therapy and survival among patients with multiorgan dysfunction syndrome (MODS) of cardiac and non-cardiac origin. Int J Cardiol. 2010;140(3):296–303.
Dare AJ, Phillips AR, Hickey AJ, Mittal A, Loveday B, Thompson N, Windsor JA. A systematic review of experimental treatments for mitochondrial dysfunction in sepsis and multiple organ dysfunction syndrome. Free Radic Biol Med. 2009;47(11):1517–25.
Teoh H, Quan A, Creighton AK, Bang KA, Singh KK, Shukla PC, et al. BRCA1 gene therapy reduces systemic inflammatory response and multiple organ failure and improves survival in experimental sepsis. Gene Ther. 2012;20(1):51–61.
Cobb JP. MORE for multiple organ dysfunction syndrome: Multiple Organ REanimation, REgeneration, and Reprogramming. Crit Care Med. 2010;38(11): 2242–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Ortiz-Leyba, C. (2014). Considerations in Organ Failure. In: Davis, K., Rosenbaum, S. (eds) Surgical Metabolism. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1121-9_13
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1121-9_13
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1120-2
Online ISBN: 978-1-4939-1121-9
eBook Packages: MedicineMedicine (R0)