Abstract
Acute pancreatitis is a disease of increasing annual incidence and one that produces significant morbidity and mortality. The ability to predict which patients are at risk for complications is critical in ensuring appropriate management and development of prevention strategies. For this reason, many scores have been developed to predict the severity of acute pancreatitis. Most of the scores incorporate a variety of physiologic, laboratory, and radiological parameters. This chapter will summarize and compare the current prediction models for severe acute pancreatitis as well as measurement of specific routine laboratory tests. The relative advantages and disadvantages of each of these systems will be highlighted. The clinical scoring systems that will be discussed include the Ranson’s score, the Glasgow criteria (also known as the Imrie score), Acute Physiology and Chronic Health Examination (APACHE)-II, Systemic Inflammatory Response Syndrome (SIRS), Pancreatitis Outcome Prediction (POP), Bedside Index for Severity in Acute Pancreatitis (BISAP), the revised Japanese severity score (JSS), and Harmless Acute Pancreatitis Score (HAPS). Particular emphasis will be devoted to the application of these various scoring systems in the routine care of patients with acute pancreatitis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute Pancreatitis
- Positive Predictive Value
- Negative Predictive Value
- Blood Urea Nitrogen
- Systemic Inflammatory Response Syndrome
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Acute pancreatitis is a disease of increasing annual incidence and that produces significant morbidity and mortality. The clinical course is highly variable, as many patients experience self-limited disease that requires only supportive measures. By contrast, others develop severe complications including death. In the United Sates, acute pancreatitis accounts for more than 330,000 hospital admissions per year and patients have an average hospital stay of 4 days [1]. Ten to twenty percent of patients develop persistent organ failure, and among this subgroup, mortality rate reaches 30 % [2]. For this reason, the ability to identify patients at risk for persistent complications such as persistent organ failure early in the disease course is critical in ensuring appropriate management and resource allocation.
Assessment of severity should start immediately with the initial clinical assessment. The objectives of initial clinical assessment are to establish the diagnosis of acute pancreatitis, evaluate potential etiologies, and perform risk stratification. Early risk stratification can help identify patients who are more likely to suffer complications such as organ failure and necrosis or infected necrosis. Patients determined to be at increased risk for morbidity and mortality from acute pancreatitis can then be triaged early to intensive care units and further be selected to undergo specific interventions. For instance, severe cases of pancreatitis may require imaging to evaluate for complications, pancreatic abscess, infected pancreatic necrosis, large pseudocysts, or acute cholangitis that may require interventions such as percutaneous drainage or ERCP.
Clinical scoring systems and laboratory markers function as prognostic indicators for acute pancreatitis; however, they do not measure severity directly. Measures of severity in acute pancreatitis were defined in the 2012 revised Atlanta classification system, which divides the disease into two phases—early and late. Mild acute pancreatitis is defined by the absence of organ failure, local or systemic complications, and resolution of disease within 1 week [3]. Moderate acute pancreatitis is defined by presence of transient organ failure, local complications, or worsening of comorbid diseases. Lastly, severe acute pancreatitis involves persistence of organ failure (signified by shock, respiratory failure, or end organ damage) for greater than 48 h and presence of local complications such as pancreatic or peripancreatic fluid collections, necrosis (sterile or infected), pseudocysts, and walled-off necrosis [3]. Studies using clinical scoring systems initially focused on mortality as the outcome of interest. However, recent data suggest that overall mortality has declined over the past several decades, and this has led to increasing debate over whether death remains the most appropriate outcome to use when predicting the outcome of acute pancreatitis.
Many studies have shown that it is critical to evaluate the patient immediately on presentation and the first 24 h after admission to the hospital for acute pancreatitis. Initial risk stratification should take place immediately and the patient should be reassessed again frequently during the first 24 h. In the retrospective cohort study conducted across 159 intensive care units in the United Kingdom, the median length of stay in the hospital prior to admission to the intensive care unit was 1 day and 22 % of the admissions to the ICU were on same as admission to the hospital [4]. Patients admitted to the ICU with severe pancreatitis have high morbidity and mortality compared to other ICU admissions, and early prediction of the severity can have important implications for management and timely intervention in the event of complications. Therefore, a prediction score that is sensitive and can be applied within the first 24 h of admission would be of great value to clinicians. These patients demand close monitoring for fluid status and nutrition, and improper triage due to underestimating the severity of acute pancreatitis may lead to inappropriate care of these patients and increased morbidity and mortality.
Historical Perspective
The first major advancement for predicting the severity of pancreatitis was the development of the Ranson criteria in 1974. Since then, multiple scoring systems have been developed which incorporate physiologic, laboratory, and radiographic parameters. New studies have also suggested the role of individual laboratory parameters in assessing disease severity such as blood urea nitrogen (BUN) and creatinine. In this chapter, we will summarize the current prediction models for severe acute pancreatitis as well as measurement of specific laboratory tests. We will also highlight the relative advantages and disadvantages of several of these models and markers which have been evaluated in several recent studies. The clinical scoring systems that will be discussed include the Ranson’s score, the Glasgow criteria (also known as the Imrie score), APACHE-II, Systemic Inflammatory Response Syndrome (SIRS), Pancreatitis Outcome Prediction (POP), Bedside Index for Severity in Acute Pancreatitis (BISAP), the revised Japanese severity score (JSS), and Harmless Acute Pancreatitis Score (HAPS). The role of several laboratory markers and level of fluid sequestration in predicting outcomes in acute pancreatitis will also be discussed.
Ranson Score
Ranson’s criteria were first developed in 1974 and are one of the earliest objective scoring systems to predict severity in acute pancreatitis. The criteria consist of five parameters measured at admission and six factors that are assessed during the next 48 h, looking at a total of 11 different components (Table 7.1). If the score is greater than or equal to 3, severe pancreatitis is likely, whereas it is unlikely with a score of less than 3 [5]. Percentage mortality has also been established based on the scoring system. A score of 0–2 has approximately 2 % mortality, a score of 3–4 has 15 % mortality, a score of 5–6 has 40 % mortality, and a score of 7–8 has 100 % mortality [5]. However, recent data suggests that overall mortality from acute pancreatitis has declined over the past several decades, which has led to increasing debate over whether death remains the most appropriate outcome to measure.
Ranson’s criteria continue to be used since it is so well-established; however, there are two main problems with the score. First, it is cumbersome to use in routine clinical practice since there are multiple parameters that are needed that are not routinely calculated as well as the fact that it takes 48 h to complete. Secondly, the inability to calculate the score within the first 24 h misses a very important therapeutic window when risk-stratification should take place. The original study detected the sensitivity of three or more criteria to predict severe disease to be 65 % with a specificity of 99 %, yielding a positive predictive value (PPV) of 95 % and a negative predictive value (NPV) of 86 % [6]. However, a meta-analysis of 12 published series using Ranson’s criteria and encompassing 1,307 patients reported an overall sensitivity for predicting severe acute pancreatitis of 75 %, a specificity of 77 %, a PPV of 49 %, and an NPV of 91 % [6]. Therefore, many patients with a Ranson’s score above 3 will not develop severe pancreatitis, emphasizing a high false-positive rate of Ranson’s criteria [7]. Overall, Ranson criteria have been shown to be a good predictor of severity in acute pancreatitis with sensitivity, specificity, PPV, and NPV ranging from 67 % to 84 %, 76 % to 90 %, 49 % to 70 %, and 89 % to 95 %, respectively [7–10].
APACHE II
Currently, the most widely used index for early risk stratification in acute pancreatitis remains the APACHE II, which was originally developed for critically ill patients in intensive care units (Table 7.2) [11]. The score has 12 components and extra points based upon age and presence of chronic disease. This scoring system has been widely validated for predicting death in acute pancreatitis. The accuracy of this scoring system depends on the chosen cutoff value and time the score is calculated. When calculated at admission, the sensitivity of an APACHE II score of >7 to predict severe acute pancreatitis is 65 %, with a specificity of 76 %, a PPV of 43 %, and a NPV of 89 % [7]. Raising the cutoff to >9 improves the specificity and PPV but reduces the sensitivity [12, 13]. Overall, at 24 h, the sensitivity, specificity, PPV, and NPV of APACHE II range between 65 % and 70.3 %, 71.9 % and 81 %, 20 % and 67 %, and 80 % and 93 %, respectively [8, 14–16]. Many variations of the scoring system have recently been developed but overall, the advantages of using the APACHE II include the ability of the score to be calculated at any point in time during the patient’s hospital stay and the ability to recalculate the score as conditions change.
Body mass index (BMI) score was recently added to APACHE II score, creating the composite score (APACHE-O), which was shown to have greater predictive accuracy [17]. One point was added for a BMI of >25 to 30 and two points were added for a BMI > 30. With a cutoff score of 8, APACHE-O was shown to be a good predictor of severity during the first 24 h of hospitalization with a sensitivity, specificity, PPV, and NPV of 82 %, 86 %, 74 %, and 91 %, respectively [17]. In a prospective study looking at patients with a BMI > 30, the predictive values of APACHE-O and APACHE II were similar with AUC 0.895 and 0.893, respectively [18]. Several additional variables were added to APACHE II to improve its accuracy leading to the development of APACHE III. Both APACHE scoring systems use similar variables; however, they differ in the number of physiologic variables (12 for APACHE II vs. 17 for APACHE III) and the assessment of chronic health status [19].
The advantages of using the APACHE system as a predictive score are that it is widely validated and the score can be calculated at any time during a patient’s hospital stay. In addition, the score can be recalculated as conditions change. There are also several disadvantages to using the APACHE II in a clinical setting. For instance, the score will likely require the use of an online calculator given the incorporation of multiple parameters. Furthermore, many of these parameters are not routinely collected.
Glasgow-Imrie Score
The modified Glasgow score was first developed in the mid-1980s and incorporates seven routinely calculated laboratory tests (white blood cell count, glucose, BUN, PaO2, calcium, albumin, and LDH) as well as the patient’s age (Table 7.3). In the original study, out of 405 episodes of acute pancreatitis, 72 % of patients had severity correctly predicted by the scoring system [20]. The original study included aminotransferase concentrations; however, this was found to not predict severity. Using eight factors, the scoring system was shown to correctly predict severity in 79 % of episodes and has since been widely validated. In a retrospective analysis of 126 cases of pancreatitis, the modified Glasgow score was found to be slightly inferior to Ranson’s score with a sensitivity of 74.5 % and specificity of 71.1 % but had good discriminatory ability with AUC of 0.805 (0.724–0.886) [21]. Those with a score greater than or equal to 3 had statistically significant increase in mortality (P = 0.001) and median length of stay (P = 0.003) [21]. The modified Glasgow score seems simpler to calculate in comparison to Ranson’s criteria and the APACHE II score. However, the score is similar to Ranson’s criteria in that it was designed to be calculated at 48 h after admission.
Bedside Index of Severity in Acute Pancreatitis
Recently, a score known as the BISAP score has been developed for use in the first 24 h of admission (Table 7.4) [22]. The score was derived from a collection of data from 17,992 patients from 212 hospitals during the years of 2000 and 2001. The score was then validated in a population of 18,256 patients from 177 hospitals in 2004–2005. The score includes five factors and one point is assigned for each of the following factors during the first 24 h: BUN > 25 mg/dL, impaired mental status, SIRS (using the same criteria as the SIRS score), age >60 years, or the presence of a pleural effusion. Patients with a score of 0 had a mortality of less than 1 %, whereas patients with a score of 5 had a mortality rate of 22 %. In the validation cohort, the BISAP AUC was 0.82 (95 % CI 0.79–0.84) vs. APACHE II AUC of 0.83 (95 % CI 0.80–0.85); thus, the BISAP score was found to have a similar accuracy to the APACHE II score for predicting death [22]. The accuracy of this score was further validated in several prospective cohort studies [8, 23]. One study aimed to evaluate the ability of the BISAP score to predict mortality and found there to be a significant trend for increasing mortality with increasing BISAP score (P < 0.0001) [23]. Another validation study performed in 57 patients found the sensitivity and specificity of the BISAP score to be 75 % and 97.56 %, respectively [24]. The advantages of this scoring system include the simplicity of calculation and the ability to identify patients at risk of death even in the early phases of acute pancreatitis. The BISAP score, similar to most of the other scoring systems, has not been validated for predicting outcomes such as length of hospital stay, need for ICU care, or need for intervention. Furthermore, it is a static measure and does not incorporate changes over time.
Systemic Inflammatory Response Syndrome
Many studies have tried to determine whether the development of SIRS can be used to determine the severity of acute pancreatitis [25–27]. The SIRS criteria were first developed in the field of sepsis and diagnosis of the syndrome requires two of four criteria (Table 7.5) [28]. The criteria include a temperature of less than 36 °C (96.8 °F) or greater than 38 °C (100.4 °F), a heart rate greater than 90 beats/min, a respiratory rate greater than 20 breaths/min or an arterial partial pressure of carbon dioxide less than 32 mmHg, and a leukocyte count less than 4,000 cells/mm3 or greater than 12,000 cells/mm3 or alternatively the presence of greater than 10 % immature neutrophils (band forms). The presence of the syndrome during the first 24 h of admission has high sensitivity (85 %) for predicting organ failure and death (100 %), but lacks specificity for severe disease (41 %). Specificity was found to increase with duration of the syndrome and those patients with a higher number of criteria on day 1 had an increased risk for severe disease [27].
Harmless Acute Pancreatitis Score
The HAPS was developed in Germany to define and evaluate a simple clinical algorithm to rapidly identify patients with a first attack of acute pancreatitis that do not require intensive care unit level of care (Table 7.6). The score can typically be calculated within 30 min of admission and takes into account three parameters: lack of rebound tenderness or guarding, normal hematocrit, and normal serum creatinine. The prospective study included a cohort of 394 patients, and the score was later validated using a cohort of 452 patients [29]. The score was able to identify a harmless course in 200 of 204 patients (98 %), and in both the initial and validation study, the HAPS score correlated with a non-severe disease course (P < 0.0001). Another study in Sweden looked to evaluate the reproducibility of this scoring system outside of the original study. Five hundred thirty-one patients with acute pancreatitis were included; of the 353 patients who had a HAPS score calculated, 79 were predicted to have a non-severe course [30]. Only 1 of 79 developed severe acute pancreatitis. The validation study found the HAPS score to have high specificity 96.3 % (95 % CI 93.1–100) for predicting a non-severe course of acute pancreatitis and a PPV of 98.7 % (95 % CI 93.1–100) [30]. The score seems to be advantageous in its simplicity, time of administration, and accuracy rate. However, it seems unlikely that providers will accept this score as the sole measure in their clinical practice to triage patients into severe and non-severe cases.
Pancreatitis Outcome Prediction Score
Another study that sought to develop a new and more sensitive outcome prediction score was based on 159 intensive care units in the United Kingdom and included 2,462 patients with severe acute pancreatitis [4]. This retrospective cohort study developed the POP score, which is a composite of demographic, physiologic, and biochemical data collected within the first 24 h of ICU admission (Table 7.7). The score consists of six variables—arterial pH, age, BUN, mean arterial pressure, PaO2/FiO2 ratio, and total serum calcium (listed in order of decreasing impact). These six factors were used to develop this multivariate prognostic score, which ranges from 0 to 40 points. In comparison to other prognostic models, the AUC (95 % confidence interval) of the final score in all admissions was 0.853 (0.838–0.866) compared with 0.670 (0.651–0.688) for the seven available modified Glasgow criteria and 0.804 (0.787–0.820) for the APACHE II score [4]. Though these initial results found the POP score to be statistically superior to other models, calculation of the score seems much more burdensome and further validation studies are needed.
Panc 3 Score
The Panc 3 score was developed for the Emergency Room setting to allow for rapid and accurate prediction of severity on presentation of acute pancreatitis (Table 7.8). The three risk factors used in this score included a serum hematocrit greater than 44 mg/dL, a BMI greater than 30 mg/kg, and a chest X-ray which revealed a pleural effusion [31]. Test-operating characteristics and likelihood ratios were computed for each risk factor using the patients originally sampled in each of the studies (n = 393) and for validation, the study examined the score’s ability to predict severe acute pancreatitis among 238 patients at University of North Carolina at Chapel Hill (UNC) hospitals. Analysis revealed that the Panc 3 score is easy to use and accurate for the prediction of severe acute pancreatitis. In the validation set of data, when all three of these findings were present and the pretest probability of pancreatitis was between 12 and 25 %, the post-test likelihood of severe disease was 99 %. Furthermore, the serum hematocrit was also identified as the strongest predictor of severe disease [31].
Japanese Severity Score
The original Japanese severity scoring system (1999) incorporated 18 prognostic factors, which made the assessment extremely complicated (Table 7.9). Furthermore, the CT grades included in the scoring system were based on plain CT and thus did not accurately reflect the prognosis of acute pancreatitis. For this reason, the scoring system was revised in 2008. In the New Japanese criteria, severity assessment can be made according to both prognostic factors and the contrast-enhanced CT grade. Prognostic factors consist of the following nine items: (1) base excess (BE) ≤3 mEq/L or shock: (systolic blood pressure ≤80 mmHg), (2) PaO2 ≤ 60 mmHg (room air) or requiring respirator management, (3) BUN ≥ 40 mg/dL (or creatinine [Cr] ≥2.0 mg/dL) or oliguria after fluid replacement, (4) lactic dehydrogenase (LDH) ≥2 times of upper limit of normal, (5) platelet count ≤100,000 mm−3, (6) Ca ≤ 7.5 mg/dL, (7) C-reactive protein (CRP) ≥15 mg/dL, (8) number of positive measures in SIRS criteria ≥3, and (9) age ≥70 years [32]. Patients who satisfy three or more of the nine items are assessed as having severe acute pancreatitis. The contrast-enhanced CT grade incorporates the extent of extrapancreatic progression of inflammation and of hypoenhanced area of the pancreas that suggests the presence of ischemia or necrosis. A CT grade of 2 or higher indicates a severe case of pancreatitis [32]. The predictive value of the revised JSS was validated in a large scale study in Japan including 17,901 patients which were able to show a significant increase in the odds ratio for mortality with increasing prognostic factor score. Area under the ROC was 0.798 (95 % confidence interval 0.775–0.821). Thus, the prognostic score factor was found to have good predictive value for in-hospital mortality in acute pancreatitis. The score is pretty well established like many of the other scoring systems, but is quite cumbersome and difficult to calculate quickly at the bedside. Furthermore, many of the prognostic criteria are labs that do not result immediately and the score can thus take up to 48 h to calculate.
Overall Comparison of Clinical Scores
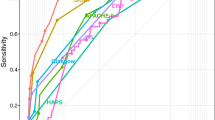
A recent study compared these nine existing clinical scoring systems to predict persistent organ failure in patients with acute pancreatitis. Clinical data were collected from two prospective cohort studies, a training cohort from the Severity of Acute Pancreatitis Study conducted at University of Pittsburg Medical Center, and a validation cohort from Markers of Severity in Acute Pancreatitis study conducted at Brigham and Women’s Hospital. Both centers utilized the same diagnostic criteria for acute pancreatitis and nine clinical scores were calculated at admission and at 48 h [33]. The scores included APACHE-II, BISAP, Glasgow, APS, JSS, Panc 3, POP, Ranson, and SIRS. The primary outcome measure was development of persistent organ failure which was defined as cardiovascular, pulmonary, or renal failure lasting for 48 h or more. A set of 12 predictive rules were developed that combined the various scoring systems in order of increasing complexity. The results showed that patients with organ failure had higher scores across all scoring systems compared to those without organ failure. Also, existing scoring systems showed moderate accuracy. The Glasgow score was found to be the best classifier at admission with AUC of 0.84 in the training cohort and 0.74 in the validation cohort. At 48 h, the best scoring system was JSS, with an AUC of 0.84 in the training cohort and 0.79 in the validation cohort. The study also found that serum levels of creatinine and BUN were similar in their ability to predict organ failure. The 12 predictive rules that combined scoring systems proved to increase accuracy to 0.92 in the training cohort and 0.84 in the validation cohort [33].
Imaging-Based Prediction/Severity Scores
There have also been severity scores based on imaging findings in acute pancreatitis. For example, a CT severity score (the Balthazar score) was developed in 1990 and was based on a combination of CT grade of pancreatitis as well as peri-pancreatic inflammation, phlegmon, and degree of necrosis seen on initial CT [34]. Patients with grade A–E pancreatitis were assigned a score of 0–4 plus an additional 2 points for necrosis up to 30 %, 4 points for necrosis from 30 to 50 %, and 6 points for necrosis greater than 50 %. The study found that there was a 23 % mortality rate and an 82 % complication rate in patients with any degree of necrosis. However, in patients without necrosis, mortality rate was 0 % and complication rate was 6 %. Furthermore, the study found that serious complications occurred in patients with more than 30 % necrosis. Patients with a high CT severity index (score 7–10) had 92 % morbidity and 17 % mortality rate, whereas patients with a low CT severity index (2) had 2 % morbidity and no mortality [34]. A large retrospective study of 268 patients was performed and reported that a CT severity index of >5 strongly correlated with mortality (P = 0.0005), longer hospital stay (P < 0.0001), and need for necrosectomy (P < 0.0001) [7].
Routine Laboratory Tests
Many serum markers have also been identified as possible prognostic indicators for severity in acute pancreatitis, including serum hematocrit, creatinine, and BUN levels (Table 7.10). See also Chap. 4. Laboratory tests allow clinicians to monitor a patient’s initial response to treatment. Several small studies suggested that hemoconcentration, or an elevated hematocrit at admission, was a predictor of pancreatic necrosis [35, 36]. One such study was a prospective cohort study by Brown and colleagues, which found that patients with more severe disease may show hemoconcentration with hematocrit values >44 %. The study also found that failure of this to decrease at 24 h was a good indication of pancreatic necrosis and predictor of organ failure [36]. However, the accuracy of hematocrit to predict pancreatic necrosis was not confirmed in several external validation studies [37–39].
Early changes in serum creatinine levels, specifically within the first 48 h, have also been associated with the development of pancreatic necrosis [40]. However, serial measurement of BUN levels seems to be the most useful laboratory test for determining death. A large retrospective cohort study looked at data from 69 hospitals and examined the relationship between early trends in BUN and hemoglobin [41]. Compared to five other laboratory markers that were examined (hemoglobin, calcium, leukocyte count, creatinine, and serum glucose), BUN had the highest area under the curve for predicting mortality at admission, at 24 h, and at 48 h [41]. The accuracy of measure serial BUN levels has been validated using data from three independent prospective cohort studies [42].
Inflammatory markers such as CRP have also been studied as potential predictors for the outcome of acute pancreatitis. CRP is an acute-phase reactant produced by the hepatocytes and its synthesis is induced by the release of interleukin-1 (IL-1) and 6 (IL-6). Serum CRP peaks on day 3 after the onset of pain and is a useful predictor of severity in acute pancreatitis 48 h after the start of symptoms but not in the early phases [43]. A systematic review showed that the sensitivity of CRP at 48 h for severe pancreatitis was 80 % with a specificity of 76 %, a PPV of 67 %, and a NPV of 86 %, which are comparable to other predictive scores [7]. The advantages of CRP measurement include its low cost and availability; however, its usefulness is limited by the poor predictive value during the initial phases of acute pancreatitis.
Many other serum markers such as procalcitonin, polymorphonuclear elastase, IL-6, and IL-8 have been identified as potentially valuable predictors of severity in acute pancreatitis [43]. Urinary trypsinogen-activation peptide (TAP) has also been shown to accurately predict severity of pancreatitis 24 h after symptom onset [44]. However, the use of these serum markers has been limited by their availability in North America.
The American Gastroenterological Association (AGA) has issued guidelines for assessing the severity of pancreatitis. The recommendations start with the clinician and their ability to assess severity of disease by the presence of organ failure and local complications (pseudocyst, necrosis, or abscess). The AGA recommends the APACHE II score as the preferred predictor of severe disease (using a cutoff of ≥8) [45]. Those with actual or predicted severe disease and those with other severe comorbid conditions should be considered for triage to an intensive care or intermediate medical care unit. In patients with predicted severe disease (i.e., APACHE II score of ≥8) and those with evidence of organ failure within the initial 72 h, rapid-bolus CT should be performed after 72 h of illness to assess the degree of pancreatic necrosis. CT should be used selectively based upon clinical features in patients who do not meet these criteria. The guidelines also suggest that laboratory tests can be used as an adjunct to clinical judgment, multiple factor scoring systems, and CT to guide initial triage decisions. Of all laboratory tests, a serum CRP level of >150 mg/L at 48 h is preferred [45].
Fluid Sequestration
Many early studies seemed to suggest early and aggressive fluid therapy to improve clinical outcome in acute pancreatitis; however, more recent studies have failed to demonstrate improved outcomes and some have suggested potentially worse outcomes. Amount of fluid sequestration has been identified as another factor that may predict outcomes in acute pancreatitis. De-Madaria and colleagues collected data on 403 patients admitted at two different hospitals and the amount of fluid sequestered at 48 h was calculated by subtracting the total amount of fluid administered and lost during the first 48 h of hospitalization [46]. The study was also able to identify factors associated with increased fluid sequestration. Increased fluid sequestration was shown to be associated with pancreatic necrosis, acute fluid collections, persistent organ failure, and increased length of stay.
Conclusion
Diagnosis of pancreatitis has always been clinical and based on elevations in amylase and lipase; however, severity of elevation in pancreatic enzymes does not necessarily correlate with disease severity. Multiple scoring systems have been developed to predict severity in acute pancreatitis, some more cumbersome and accurate than others. As highlighted in the recent study by Mounzer and colleagues [33], the existing clinical scoring systems each performed with moderate accuracy in their ability to predict persistent organ failure. Their method of developing 12 predictive rules to combine these scores further improved the accuracy to predict severe pancreatitis; however, this method too is cumbersome and not easily applicable in clinical practice. Of the risk factors that correlate with severe disease, the ones that are simple and easy to obtain include BMI, age, hematocrit, BUN, and presence of pleural effusions on a chest X-ray. Furthermore, since hemoconcentration itself has been shown to be an accurate predictor of necrosis and organ failure, serial BUN measurements seem to be a valuable routine laboratory marker for following disease progression. It seems that many of the scoring systems will not consistently be accepted into clinical practice since most are quite cumbersome to calculate. Physicians will likely continue to utilize their clinical judgment and individual laboratory markers that are easy to obtain to assess severity in pancreatitis.
References
Fagenholz PJ, Castillo CF, Harris NS, Pelletier AJ, Camargo Jr CA. Increasing United States hospital admissions for acute pancreatitis, 1988-2003. Ann Epidemiol. 2007;17:491–7.
Whitcomb DC. Clinical practice. Acute pancreatitis. N Engl J Med. 2006;354:2142–50.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis—2012; revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–11.
Harrison DA, D’Amico G, Singer M. The Pancreatitis Outcome Prediction (POP) score: a new prognostic index for patients with severe acute pancreatitis. Crit Care Med. 2007;35(7):1703–8. PubMed PMID: 17522578.
Ranson JHC, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC. Surg Gynecol Obstet. 1974;139:69.
De Bernardinis M, Violi V, Roncoroni L, Boselli AS, Giunta A, Peracchia A. Discriminant power and information content of Ranson’s prognostic signs in acute pancreatitis: a meta-analytic study. Crit Care Med. 1999;27(10):2272.
Forsmark CE, Baillie J, AGA Institute Clinical Practice and Economics Committee, AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132(5):2022–44. Review. PubMed PMID: 17484894.
Papachristou GI, Muddana V, Yadav D, O’Connell M, Sanders MK, Slivka A, et al. Comparison of BISAP, Ranson’s, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol. 2010;105:435–41.
Eachempati SR, Hydo LJ, Barie PS. Severity scoring for prognostication in patients with severe acute pancreatitis: comparative analysis of the Ranson score and the APACHE III score. Arch Surg. 2002;137(6):730–6.
Steinberg WM. Predictors of severity of acute pancreatitis. Gastroenterol Clin North Am. 1990;19(4):849–61.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Wilson C, Heath DI, Imrie CW. Prediction of outcome in acute pancreatitis: a comparative study of APACHE II, clinical assessment and multiple factor scoring systems. Br J Surg. 1990;77:1260–4.
Chatzicostas C, Roussomoustakaki M, Vlachonikolis IG, Notas G, Mouzas I, Samonakis D, et al. Comparison of Ranson, APACHE II and APACHE III scoring systems in acute pancreatitis. Pancreas. 2002;25:331–5.
Fan ST, Lai EC, Mok FP, Lo CM, Zheng SS, Wong J. Prediction of the severity of acute pancreatitis. Am J Surg. 1993;166(3):262–8; discussion 9.
Larvin M, McMahon MJ. APACHE-II score for assessment and monitoring of acute pancreatitis. Lancet. 1989;2(8656):201–5.
Mason JM, Babu BI, Bagul A, Siriwardena AK. The performance of organ dysfunction scores for the early prediction and management of severity in acute pancreatitis: an exploratory phase diagnostic study. Pancreas. 2010;39(7):1104–8.
Johnson CD, Toh SK, Campbell MJ. Combination of APACHE-II score and an obesity score (APACHE-O) for the prediction of severe acute pancreatitis. Pancreatology. 2004;4:1.
Papachristou GI, Papachristou DJ, Avula H, Slivka A, Whitcomb DC. Obesity increases the severity of acute pancreatitis: performance of APACHE-O score and correlation with the inflammatory response. Pancreatology. 2006;6(4):279–85.
Williams M, Simms HH. Prognostic usefulness of scoring systems in critically ill patients with severe acute pancreatitis. Crit Care Med. 1999;27:901.
Blamey SL, Imrie CW, O’Neill J, Gilmour WH, Carter DC. Prognostic factors in acute pancreatitis. Gut. 1984;25:1340–6.
Simoes M, Alves P, Esperto H, Canha C, Meira E, Ferreira E. Predicting acute pancreatitis severity: comparison of prognostic scores. Gastroenterol Res. 2011;4(5):216–22.
Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57:1698–703.
Singh VK, Wu BU, Bollen TL, Repas K, Maurer R, Johannes RS, et al. A prospective evaluation of the Bedside Index for Severity in Acute Pancreatitis score in assessing mortality and intermediate markers of severity in acute pancreatitis. Am J Gastroenterol. 2009;104:966–71.
Villacís X, Calle P, Patiño J, Calle G. [Score BISAP validation as a prognostic system in acute pancreatitis]. Rev Gastroenterol Peru. 2011;31(3):230–5. Spanish. PubMed PMID: 22086317.
Buter A, Imrie CW, Carter CR, Evans S, McKay CJ. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Br J Surg. 2002;89:298–302.
Mofidi R, Duff MD, Wigmore SJ, Madhavan KK, Garden OJ, Parks RW. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–44.
Singh VK, Wu BU, Bollen TL, Repas K, Maurer R, Mortele KJ, et al. Early systemic inflammatory response syndrome is associated with severe acute pancreatitis. Clin Gastroenterol Hepatol. 2009;7:1247–51.
Bone RC, Sibbald WJ, Sprung CL. The ACCP-SCCM consensus conference on sepsis and organ failure. Chest. 1992;101:1481–3.
Lankisch PG, Weber-Dany B, Hebel K, Maisonneuve P, Lowenfels AB. The harmless acute pancreatitis score: a clinical algorithm for rapid initial stratification of nonsevere disease. Clin Gastroenterol Hepatol. 2009;7:702.
Oskarsson V, Mehrabi M, Orsini N, Hammarqvist F, Segersvärd R, Andrén-Sandberg A, et al. Validation of the harmless acute pancreatitis score in predicting nonsevere course of acute pancreatitis. Pancreatology. 2011;11(5):464–8. doi:10.1159/000331502. Epub 2011 Sep 29. PubMed PMID:21968430.
Brown A, James-Stevenson T, Dyson T, Grunkenmeier D. The panc 3 score: a rapid and accurate test for predicting severity on presentation in acute pancreatitis. J Clin Gastroenterol. 2007;41(9):855–8. PubMed PMID: 17881932.
Hamada T, Yasunaga H, Nakai Y, Isayama H, Horiguchi H, Fushimi K, Koike K. Japanese severity score for acute pancreatitis well predicts in-hospital mortality: a nationwide survey of 17,901 cases. J Gastroenterol. 2013;48(12):1384–91. doi:10.1007/s00535-013-0765-6. Epub 2013 Feb 19. PubMed PMID: 23420576.
Mounzer R, Langmead CJ, Wu BU, Evans AC, Bishehsari F, Muddana V, et al. Comparison of existing clinical scoring systems to predict persistent organ failure in patients with acute pancreatitis. Gastroenterology. 2012;142(7):1476–82. PubMed PMID: 22425589.
Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990;174:331.
Baillargeon JD, Orav J, Ramagopal V, Tenner SM, Banks PA. Hemoconcentration as an early risk factor for necrotizing pancreatitis. Am J Gastroenterol. 1998;93:2130–4.
Brown A, Orav J, Banks PA. Hemoconcentration is an early marker for organ failure and necrotizing pancreatitis. Pancreas. 2000;20:367–72.
Remes-Troche JM, Duarte-Rojo A, Morales G, Robles-Díaz G. Hemoconcentration is a poor predictor of severity in acute pancreatitis. World J Gastroenterol. 2005;11:7018–23.
Lankisch PG, Mahlke R, Blum T, Bruns A, Bruns D, Maisonneuve P, et al. Hemoconcentration: an early marker of severe and/or necrotizing pancreatitis? A critical appraisal. Am J Gastroenterol. 2001;96:2081–5.
Gardner TB, Olenec CA, Chertoff JD, Mackenzie TA, Robertson DJ. Hemoconcentration and pancreatic necrosis: further defining the relationship. Pancreas. 2006;33:169–73.
Muddana V, Whitcomb DC, Khalid A, Slivka A, Papachristou GI. Elevated serum creatinine as a marker of pancreatic necrosis in acute pancreatitis. Am J Gastroenterol. 2009;104:164–70.
Wu BU, Johannes RS, Sun X, Conwell DL, Banks PA. Early changes in blood urea nitrogen predict mortality in acute pancreatitis. Gastroenterology. 2009;137:129–35.
Wu B, Bakker OJ, Papchristou GI, Repas K, Besselink MG, van Santvoort HC, et al. Prognostic value of blood urea nitrogen (BUN) in the early assessment of acute pancreatitis: an international study [abstract 475p]. Gastroenterology. 2010;138 Suppl 1:S-66.
Papachristou GI, Whitcomb DC. Inflammatory markers of disease severity in acute pancreatitis. Clin Lab Med. 2005;25:17–37.
Neoptolemos JP, Kemppainen EA, Mayer JM, Fitzpatrick JM, Raraty MG, Slavin J, et al. Early prediction of severity in acute pancreatitis by urinary trypsinogen activation peptide: a multicentre study. Lancet. 2000;355:1955–60.
American Gastroenterological Association (AGA) Institute on “Management of Acute Pancreatits” Clinical Practice and Economics Committee, AGA Institute Governing Board. AGA Institute medical position statement on acute pancreatitis. Gastroenterology. 2007;132(5):2019–21. PubMed PMID: 17484893.
De-Madaria E, Banks PA, Moya-Hoyo N, Wu BU, Rey-Riveiro M, Acevedo-Piedra NG, et al. Early factors associated with fluid sequestration and outcomes of acute pancreatitis. Clin Gastroenterol Hepatol. 2013. doi:10.1016/j.cgh.2013.10.017.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Reddy, K.M., Wu, B.U. (2015). Predictive Scoring Systems in Acute Pancreatitis. In: Forsmark, C., Gardner, T. (eds) Prediction and Management of Severe Acute Pancreatitis. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0971-1_7
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0971-1_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0970-4
Online ISBN: 978-1-4939-0971-1
eBook Packages: MedicineMedicine (R0)