Abstract
Acute pancreatitis is a highly dynamic disease process with broad variability in clinical outcomes ranging from self-limited disease to organ failure and mortality. Pancreatic injury can induce a systemic inflammatory response that, if left unmitigated, may lead to poor clinical outcomes. The early prediction of disease severity has been an area of ongoing research over the past few decades. Accurate prediction of disease severity enables physicians to triage patients to the appropriate level of care and guide clinical management early during the disease course. Multiple risk factors (increased age, obesity, alcohol consumption) and laboratory markers (elevated blood urea nitrogen, serum creatinine, hematocrit, C-reactive protein) have been identified as predictors of disease severity. Several clinical scoring systems that incorporate laboratory markers and risk factors have also been developed to help predict clinical outcomes. Additionally, radiographic scoring systems have been evaluated in predicting disease severity. Studies comparing these scoring systems revealed comparable performance characteristics among the different systems.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute Pancreatitis
- Organ Failure
- Blood Urea Nitrogen
- Systemic Inflammatory Response Syndrome
- Pancreatic Necrosis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Acute pancreatitis is currently the leading cause of gastrointestinal-related hospital admissions [1]. Approximately 80 % of patients who develop acute pancreatitis, regardless of etiology, have mild disease. The remaining patients develop severe disease characterized by end organ failure and/or necrosis of the pancreatic parenchyma or peripancreatic fat [2–4]. In mild interstitial disease mortality is about 3 % and reaches 17 % in patients who develop gland necrosis [4]. Organ failure, a consequence of the systemic inflammatory response incited by an insult to the pancreas, is an integral part of the definition of severe disease. Patients who develop multisystem organ failure have significantly increased mortality rates sometimes surpassing 60 % [5–8].
Predicting disease severity in acute pancreatitis has been an area of increasing interest over the past few decades. This has been driven by the fact that acute pancreatitis is a highly variable physiologic process that can lead to a broad range of clinical outcomes. These outcomes range from mild, self-limited disease to a systemic inflammatory process that can progress to organ failure and mortality. Moreover, local complications can develop, including acute fluid collections, gland and peripancreatic necrosis, and portosplenomesenteric venous thrombosis. Infection of necrosed tissue, which can occur later in the disease course, contributes significantly to mortality [4, 7, 9]. Identifying patients at risk for these severe complications is therefore crucial for modifying clinical outcomes. The early recognition of disease severity enables clinicians to tailor medical management and transition patients to the appropriate level of care [4].
Risk Factors
A thorough clinical assessment plays a key role in the overall risk stratification of patients with acute pancreatitis as pre-existing clinical comorbidities serve as risk factors for the development of organ failure and mortality. Obesity is a comorbid condition that has been extensively studied as a risk factor for the development of both local and systemic disease complications [10–12]. Patients with a body mass index (BMI) >=30 have been shown to be at a significantly increased risk for organ failure, pancreatic necrosis, and mortality [10]. These observations have been supported by histological studies demonstrating that patients with a higher BMI, and therefore a higher percentage of intrapancreatic fat, develop more severe disease. Additionally in vitro studies utilizing pancreatic acinar cells have demonstrated that unsaturated fatty acids induce the generation of inflammatory mediators that can ultimately lead to cell death. These findings suggest a role for lipotoxicity in propagating systemic inflammation [13].
Other risk factors that have been evaluated as clinical predictors of disease severity include age, sex, and medical comorbidities. In a large retrospective study, male sex, increased age (>65 years), and the number of chronic medical comorbidities were shown to be significantly associated with early mortality. The medical conditions found to predispose patients to early mortality included malignancy, heart failure, chronic kidney disease, and liver disease [14]. Increased age (>=70 years) was shown to be a significant risk factor for the development of organ failure and mortality in another retrospective study [15]. Moreover, patients who consume more than two alcoholic drinks per day are at an increased risk for developing pancreatic necrosis [16]. Although genetic testing is still not utilized in daily clinical practice, pilot studies have assessed several single nucleotide polymorphisms as risk factors for severe acute pancreatitis. A common polymorphism in the promoter of the monocyte chemotactic protein-1 (MCP-1) gene, namely the MCP-1-2518 G allele, has been shown to increase the risk for organ failure [17].
Clinical risk factors should thus be identified by means of a detailed history taking and physical examination. This provides the initial assessment and preliminary risk stratification in patients presenting with acute pancreatitis. Studies evaluating the ability of clinical assessment alone in predicting severe disease, found clinical judgment to have a high specificity with sensitivities, however, below 50 % [18, 19].
Clinical Scoring Systems
Following the initial clinical assessment, further risk stratification can then be implemented by utilizing clinical scoring systems for the prediction of disease severity. Over the past three decades, a myriad of such clinical scores have been developed and validated in different cohorts of patients with acute pancreatitis. Several of these scoring systems have been utilized to triage patients in clinical practice. Moreover, they have been used extensively in research to identify patients at risk for severe disease. Here we discuss the main clinical scoring systems available to date and review their performance characteristics (Table 5.1).
The first clinical scoring system for the prediction of disease severity in acute pancreatitis was developed by Ranson and colleagues in 1974. See also Chap. 7. This scoring system represented a landmark in the field as prior assessment of patients with acute pancreatitis was based solely on clinical judgment. The Ranson score incorporated objective laboratory and clinical data collected upon initial presentation and within the following 48 h [20, 21]. The 11 prognostic parameters utilized in the Ranson score were selected, based on a statistical analysis, from among 43 variables in a retrospective cohort of 450 patients. When evaluated in a study of 386 patients who presented with an initial attack of acute pancreatitis, a Ranson score of >=3 was found to be associated with a mortality of 15 %. A score of >=6 was associated with 40 % mortality [22]. A meta-analysis evaluating 110 clinical trials that utilized the Ranson score for predicting disease severity showed it to be a moderately accurate predictor with performance characteristics similar to those of clinical judgment [23]. The 48 h needed to complete the score also posed a significant limitation in that this time interval during the early stages of the disease course is critical for optimizing medical intervention and allocating patients to the appropriate level of care [4].
A more rigorous scoring system, the Acute Physiology and Chronic Health Evaluation II (APACHE-II), was subsequently developed in 1989 and has been utilized extensively in assessing disease severity in acute pancreatitis. In addition to encompassing a broad range of clinical data including vital signs, blood studies, and a neurologic assessment, the APACHE-II score also took into account chronic illness [18]. In contrast to the Ranson score, it can be calculated on admission and updated daily during the hospitalization, thus allowing for closer monitoring of the clinical course and response to therapy. The main drawbacks of the APACHE-II score are its complexity and the fact that it is not pancreatitis-specific, as it was designed for patients requiring critical care. Moreover, it is cumbersome to calculate on a daily basis and some of the variables incorporated into the score are not routinely recorded outside of the intensive care unit.
Another pancreatitis-specific score, similar to the Ranson score in that it requires 48 h to be calculated, is the Glasgow score [24]. In well-designed, prospective studies performed approximately 20 years ago, the Ranson, Glasgow, and APACHE II scoring systems were found to have similar accuracies in predicting severity in acute pancreatitis [18, 25, 26]. Following these studies, research on clinical scoring systems subsided for about a decade.
Scoring systems, however, have regained significant attention in recent years with a focus on the development of simple scores that are easy to calculate and apply clinically. The systemic inflammatory response syndrome (SIRS), based on four clinical parameters, has been long established as a physiologic clinical response that is induced by nonspecific insults to the body [27]. The four parameters include: temperature (<36 or >38 °C), heart rate (>90 beats/min), respiratory rate (>20 respirations/min or PaCO2 < 32 mmHg), and white blood cell count (<4,000/mm3, >12,000/mm3 or >10% bands). In recent years SIRS, which precedes the development of organ failure, has been further investigated as a prognostic clinical score in acute pancreatitis. In a prospective study of 121 patients with acute pancreatitis predicted to have a severe course of disease based on an APACHE-II score >=6, early organ dysfunction was found to be significantly associated with mortality. Moreover, the presence of SIRS (score of >=2) on admission, at 24 h, 48 h, and persistent SIRS (SIRS present throughout the initial 48 h), were also significantly associated with mortality [28]. A subsequent large retrospective study reaffirmed persistent SIRS to be strongly associated with mortality [29]. Given the readily available parameters used for calculating the SIRS score, its simplicity, ability to be calculated daily, and strong correlation with poor clinical outcomes, monitoring for the persistence of SIRS has been recommended in recent management guidelines for the prediction of disease severity in acute pancreatitis [30].
In light of this data, studies assessing medical intervention targeted at abrogating systemic inflammation were performed in an attempt to improve clinical outcomes. Early fluid resuscitation, for example, was shown to significantly reduce both SIRS and organ failure in patients with acute pancreatitis. This also led to significantly shorter hospitalizations and a decreased need for intensive care in these patients [31]. In a prospective pilot study, lactated Ringer’s was found to be more effective than normal saline in reducing systemic inflammation [32].
SIRS has also been incorporated into a more recently developed clinical scoring system for predicting overall prognosis in acute pancreatitis. The Bedside Index of Severity in Acute Pancreatitis (BISAP) includes five clinical parameters, one of which is SIRS >= 2. These five parameters are: age >60 years, blood urea nitrogen >25 mg/dL, SIRS >= 2, impaired mental status with a Glasgow Coma Score <15, and presence of pleural effusions [33]. A BISAP score >=3, calculated within 24 h of admission, was shown to be significantly associated with both the development of organ failure and pancreatic necrosis in a large prospective study [34]. In a follow-up prospective study, the BISAP score had a similar accuracy in predicting the development of organ failure, pancreatic necrosis, and mortality when compared to the Ranson score and APACHE-II [35].
Panc 3, another simple clinical scoring system, was developed at about the same time as the BISAP score and included three clinical parameters (hematocrit >44 mg/dL, BMI > 30 kg/m2, and pleural effusions), which had each individually been shown to predict severe disease [36]. The harmless acute pancreatitis score (HAPS) was also recently developed in Germany. This scoring system is unique in that it was designed to identify patients expected to have a mild course of disease. Moreover, it only incorporates three parameters: abdominal tenderness, hematocrit >43 mg/dL for men or >39.6 mg/dL for women and creatinine >2 mg/dL. In a prospective study that had a validation cohort, absence of these parameters identified patients with uncomplicated acute pancreatitis with a specificity of 97 % and a positive predictive value (PPV) of 98 % [37]. Other scoring systems that predict disease severity have also been recently reported including the pancreatitis outcome prediction (POP) score and the new Japanese severity score [38, 39]. The POP score incorporates six objectively weighted clinical variables obtained from patients admitted to the ICU [38]. The new Japanese severity score incorporates nine prognostic variables.
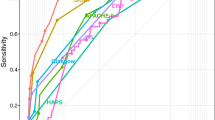
Overall, the studies performed to develop and validate the above mentioned clinical scoring systems are limited by heterogeneity between different populations and varying endpoints among the different studies. Some studies used the original Atlanta criteria for the assessment of disease severity, whereas others evaluated mortality. A recent large dual-center study, conducted to compare all available clinical scoring systems in two prospective cohorts of patients with acute pancreatitis, found all the above described clinical scoring systems to have comparable performance characteristics with only modest overall accuracies among all the scoring systems. Performance characteristics of the various scoring systems from the training cohort of this study are presented in Table 5.2. Furthermore, combining these scoring systems in order of increasing complexity as part of predictive rules in an attempt to improve predictive accuracy yielded no significant improvement in their performance characteristics. This highlighted the limitations of clinical scoring systems in prognosticating disease severity and suggested that these scoring systems have reached their maximal predictive capacity. This may be due to the fact that in the majority of clinical scoring systems clinical parameters are converted from continuous to dichotomous values [40].
Laboratory Markers
Multiple laboratory markers have also been evaluated individually as predictive markers of disease severity including hematocrit, blood urea nitrogen (BUN), creatinine, and C-reactive protein (CRP) levels [4]. Serum hematocrit, which serves as a surrogate marker for intravascular volume, has been evaluated in several studies as a predictor of pancreas necrosis and organ failure [41–43]. Pancreatic necrosis has been attributed to an increase in vascular permeability; a consequence of the systemic inflammatory process that can be induced by pancreatic injury. This increase in vascular permeability leads to a decrease in intravascular volume, an increase in blood viscosity, and thus an impairment in microcirculation within the pancreatic parenchyma resulting in tissue necrosis [3, 4, 44, 45]. In a landmark study performed in 1998 comparing patients with pancreas necrosis to those with mild acute pancreatitis, both a hematocrit >=47 % on admission and failure to decrease the hematocrit within the first 24 h were both found to be significantly associated with the development of necrosis [41]. In a follow-up prospective study by the same group, a serum hematocrit of >=44 % upon admission and failure to decrease the hematocrit level with intravenous hydration within the first 24 were found to be significant predictors of both pancreas necrosis and organ failure [42]. In a subsequent prospective study of patients with a first attack of acute pancreatitis, hemoconcentration at different cut-off values was found to be significantly associated with length of hospitalization and length of ICU stay, but not with the development of organ failure or morality. Performance characteristics of hemoconcentration were comparable to the Ranson and Glasgow scores in this study [43].
BUN serves as another surrogate marker for intravascular volume and catabolic states. As such, the relationship between hemoglobin and BUN, as well as their performance characteristics, were evaluated in an observational study that incorporated retrospectively collected data from 69 hospitals in the U.S. Rising BUN levels within the first 48 h of hospitalization were found to be significantly associated with mortality. This relationship, however, did not hold true for hemoglobin. BUN levels upon admission and changes in BUN over time were found to be independent predictors of mortality with each 5 mg/dL rise in BUN leading to an increase in the odds ratio for mortality of 2.2. When compared to other laboratory parameters (calcium, hemoglobin, creatinine, white blood cell count, and glucose) BUN was found to have the highest accuracy of predicting in-hospital mortality with an area under the curve (AUC) of 0.90 [46]. In patients with pancreas necrosis, elevated BUN correlated with both prolonged ICU stay and mortality [47]. An international multicenter validation study further supported the role of BUN in predicting mortality. A BUN >= 20 mg/dL upon admission was associated with an odds ratio of 4.6 for mortality. When BUN was measured serially during hospitalization, it was also found to be comparable to both creatinine and the APACHE-II score in predicting mortality with an AUC of 0.80. A decline in BUN of >=5 mg/dL with fluid resuscitation led to a significant decrease in mortality [48].
Comparison of admission hematocrit, BUN, and serum creatinine in a prospectively enrolled cohort of 129 patients found all three parameters to be significantly associated with pancreas necrosis. A peak serum creatinine >1.8 mg/dL during the first 48 h of hospitalization was associated with the highest odds ratio (OR) for the development of necrosis (OR = 35) [49]. A follow-up study revealed a lower sensitivity and PPV and comparable specificity and negative predictive value (NPV) for the prediction of pancreas necrosis [50]. The differences in these results have been attributed to differences in the populations between the two studies; the index study population had a higher prevalence of pancreas necrosis that was driven by a referral bias of transferred patients with more severe disease [51].
CRP is a widely available and inexpensive marker of systemic inflammation that has been studied as a predictor of disease severity in acute pancreatitis [52]. In a retrospective study, a CRP level measured at 48 h was found to be a moderately accurate prognostic marker for severe disease. CRP levels predicted the development of organ failure, pancreas necrosis, and inpatient mortality with AUCs ranging from 0.7 to 0.81. Cut-off values used for these endpoints were 190 mg/L, 190 mg/L, and 170 mg/L, respectively [53]. Urine trypsinogen-2, urine trypsinogen activation peptide, and interleukin-6 have also been evaluated for assessing disease severity in acute pancreatitis. These tests, however, have yet to be established in clinical practice [54, 55].
Radiographic Scores
Several radiographic scoring systems utilizing computed tomography (CT) have been proposed over recent years for the assessment of disease severity (Table 5.3). See also Chap. 6. The Balthazar CT score, the first radiographic score developed in 1985, graded severity based on the presence or absence and number of fluid collections on initial non-contrasted CT. Patients found to have fluid collections on CT had a higher morbidity and mortality than those without [56, 57]. Other scoring systems based on non-contrasted CT scan findings include: the pancreatic size index (PSI), mesenteric edema and peritoneal fluid (MOP), extrapancreatic (EP), and extrapancreatic inflammation on CT (EPIC) scores [58–61]. The more recent CT severity index (CTSI) is based upon contrast-enhanced CT and thus incorporates inflammatory changes with the presence or absence of pancreatic necrosis to generate a numeric score [62]. In a large prospective study comparing the performance characteristics of CTSI (obtained within 48 h) to the Ranson, APACHE-II, and BISAP scores, these scores were found to perform comparably. The CTSI score, as expected, had the highest accuracy for predicting pancreatic necrosis [35]. More recently, a study evaluating the accuracy of several radiographic scoring systems, including the CTSI score on the day of admission to the BISAP and APACHE-II scores, found no significant differences in the prediction of disease severity or overall mortality. Based on the comparable performance characteristics found in this study, it was recommended that CT scans not be obtained upon admission for the purpose of assessing disease severity [63].
Conclusion
Despite extensive research over the past few decades, a highly accurate clinical scoring system, laboratory marker, or radiologic score for predicting disease severity in acute pancreatitis has yet to be developed. This likely reflects underlying deficiencies in the scientific and statistical processes used to develop these scores, as well as the complexity and heterogeneity of this disease. Overall, the above approaches can only predict severe disease with moderate accuracy. The authors’ recommendations to clinicians are therefore to assess host risk factors (i.e., age, presence of obesity, alcohol use) and utilize laboratory values and simple scoring systems in the early phase of acute pancreatitis both for risk stratification upon admission and to assess the response to therapy within the first 24–48 h [30]. This is summarized as follows:
-
1.
A BUN level of >=20 mg/dL upon admission, or failure to decrease after 24 h despite adequate resuscitation, places patients at significant risk for mortality.
-
2.
A peak Cr level of >1.8 mg/dL within the first 48 h should raise concern for pancreatic necrosis, even in patients that do not require ICU admission.
-
3.
Presence of systemic inflammatory response syndrome (SIRS score >=2) on admission and persistence of SIRS for 24–48 h despite adequate fluid resuscitation is highly predictive of the development of organ failure.
References
Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–87 e1–3.
Forsmark CE, Baillie J. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007; 132:2022–44.
Whitcomb DC. Clinical practice. Acute pancreatitis. N Engl J Med. 2006;354:2142–50.
Banks PA, Freeman ML. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379–400.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis – 2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–11.
Dellinger EP, Forsmark CE, Layer P, Lévy P, Maraví-Poma E, Petrov MS, et al. Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg. 2012;256:875–80.
Sarr MG. Revision of the Atlanta classification of acute pancreatitis. Pol Arch Med Wewn. 2013; 123(3):118–24 [Epub 25 Jan 2013].
de Beaux AC, Palmer KR, Carter DC. Factors influencing morbidity and mortality in acute pancreatitis: an analysis of 279 cases. Gut. 1995;37:121–6.
Easler J, Muddana V, Furlan A, Dasyam A, Vipperla K, Slivka A, et al. Portosplenomesenteric venous thrombosis in patients with acute pancreatitis is associated with pancreatic necrosis and usually has a benign course. Clin Gastroenterol Hepatol 2014;12(5):854–62.
Papachristou GI, Papachristou DJ, Avula H, Slivka A, Whitcomb DC. Obesity increases the severity of acute pancreatitis: performance of APACHE-O score and correlation with the inflammatory response. Pancreatology. 2006;6:279–85.
Hong S, Qiwen B, Ying J, Wei A, Chaoyang T. Body mass index and the risk and prognosis of acute pancreatitis: a meta-analysis. Eur J Gastroenterol Hepatol. 2011;23:1136–43.
Martinez J, Johnson CD, Sanchez-Paya J, de Madaria E, Robles-Díaz G, Pérez-Mateo M. Obesity is a definitive risk factor of severity and mortality in acute pancreatitis: an updated meta-analysis. Pancreatology. 2006;6:206–9.
Navina S, Acharya C, DeLany JP, Orlichenko LS, Baty CJ, Shiva SS, et al. Lipotoxicity causes multisystem organ failure and exacerbates acute pancreatitis in obesity. Sci Transl Med. 2011;3:107ra110.
Frey C, Zhou H, Harvey D, White RH. Co-morbidity is a strong predictor of early death and multi-organ system failure among patients with acute pancreatitis. J Gastrointest Surg. 2007;11:733–42.
Gardner TB, Vege SS, Chari ST, Pearson RK, Clain JE, Topazian MD, et al. The effect of age on hospital outcomes in severe acute pancreatitis. Pancreatology. 2008;8:265–70.
Papachristou GI, Papachristou DJ, Morinville VD, Slivka A, Whitcomb DC. Chronic alcohol consumption is a major risk factor for pancreatic necrosis in acute pancreatitis. Am J Gastroenterol. 2006;101:2605–10.
Papachristou GI, Sass DA, Avula H, Lamb J, Lokshin A, Barmada MM, et al. Is the monocyte chemotactic protein-1 -2518 G allele a risk factor for severe acute pancreatitis? Clin Gastroenterol Hepatol. 2005;3:475–81.
Larvin M, McMahon MJ. APACHE-II score for assessment and monitoring of acute pancreatitis. Lancet. 1989;2:201–5.
Wilson C, Heath DI, Imrie CW. Prediction of outcome in acute pancreatitis: a comparative study of APACHE II, clinical assessment and multiple factor scoring systems. Br J Surg. 1990;77:1260–4.
Ranson JH, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet. 1974;139:69–81.
Ranson JH, Rifkind KM, Roses DF, Fink SD, Eng K, Localio SA. Objective early identification of severe acute pancreatitis. Am J Gastroenterol. 1974;61:443–51.
Blum T, Maisonneuve P, Lowenfels AB, Lankisch PG. Fatal outcome in acute pancreatitis: its occurrence and early prediction. Pancreatology. 2001;1:237–41.
De Bernardinis M, Violi V, Roncoroni L, Boselli AS, Giunta A, Peracchia A. Discriminant power and information content of Ranson's prognostic signs in acute pancreatitis: a meta-analytic study. Crit Care Med. 1999;27:2272–83.
Blamey SL, Imrie CW, O'Neill J, Gilmour WH, Carter DC. Prognostic factors in acute pancreatitis. Gut. 1984;25:1340–6.
Fan ST, Lai EC, Mok FP, Lo CM, Zheng SS, Wong J. Prediction of the severity of acute pancreatitis. Am J Surg. 1993;166:262–8; discussion 269.
Neoptolemos JP, Kemppainen EA, Mayer JM, Fitzpatrick JM, Raraty MG, Slavin J, et al. Early prediction of severity in acute pancreatitis by urinary trypsinogen activation peptide: a multicentre study. Lancet. 2000;355:1955–60.
Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP. The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA. 1995;273:117–23.
Buter A, Imrie CW, Carter CR, Evans S, McKay CJ. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Br J Surg. 2002;89:298–302.
Mofidi R, Duff MD, Wigmore SJ, Madhavan KK, Garden OJ, Parks RW. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–44.
Working Group IAPAPAAPG. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–15.
Warndorf MG, Kurtzman JT, Bartel MJ, Cox M, Mackenzie T, Robinson S, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:705–9.
Wu BU, Hwang JQ, Gardner TH, Repas K, Delee R, Yu S, et al. Lactated Ringer's solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:710–717 e1.
Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA. The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 2008;57:1698–703.
Singh VK, Wu BU, Bollen TL, Repas K, Maurer R, Johannes RS, et al. A prospective evaluation of the bedside index for severity in acute pancreatitis score in assessing mortality and intermediate markers of severity in acute pancreatitis. Am J Gastroenterol. 2009;104:966–71.
Papachristou GI, Muddana V, Yadav D, O'Connell M, Sanders MK, Slivka A, et al. Comparison of BISAP, Ranson's, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol. 2010;105:435–41 [Quiz 442].
Brown A, James-Stevenson T, Dyson T, Grunkenmeier D. The panc 3 score: a rapid and accurate test for predicting severity on presentation in acute pancreatitis. J Clin Gastroenterol. 2007;41:855–8.
Lankisch PG, Weber-Dany B, Hebel K, Maisonneuve P, Lowenfels AB. The harmless acute pancreatitis score: a clinical algorithm for rapid initial stratification of nonsevere disease. Clin Gastroenterol Hepatol. 2009;7:702–5 [Quiz 607].
Harrison DA, D'Amico G, Singer M. The Pancreatitis Outcome Prediction (POP) Score: a new prognostic index for patients with severe acute pancreatitis. Crit Care Med. 2007;35:1703–8.
Ueda T, Takeyama Y, Yasuda T, Kamei K, Satoi S, Sawa H, et al. Utility of the new Japanese severity score and indications for special therapies in acute pancreatitis. J Gastroenterol. 2009;44:453–9.
Mounzer R, Langmead CJ, Wu BU, Evans AC, Bishehsari F, Muddana V, et al. Comparison of existing clinical scoring systems to predict persistent organ failure in patients with acute pancreatitis. Gastroenterology. 2012;142:1476–82 [Quiz e15-6].
Baillargeon JD, Orav J, Ramagopal V, Tenner SM, Banks PA. Hemoconcentration as an early risk factor for necrotizing pancreatitis. Am J Gastroenterol. 1998;93:2130–4.
Brown A, Orav J, Banks PA. Hemoconcentration is an early marker for organ failure and necrotizing pancreatitis. Pancreas. 2000;20:367–72.
Lankisch PG, Mahlke R, Blum T, Bruns A, Bruns D, Maisonneuve P, et al. Hemoconcentration: an early marker of severe and/or necrotizing pancreatitis? A critical appraisal. Am J Gastroenterol. 2001;96:2081–5.
Knoefel WT, Kollias N, Warshaw AL, Waldner H, Nishioka NS, Rattner DW. Pancreatic microcirculatory changes in experimental pancreatitis of graded severity in the rat. Surgery. 1994;116:904–13.
Klar E, Schratt W, Foitzik T, Buhr H, Herfarth C, Messmer K. Impact of microcirculatory flow pattern changes on the development of acute edematous and necrotizing pancreatitis in rabbit pancreas. Dig Dis Sci. 1994;39:2639–44.
Wu BU, Johannes RS, Sun X, Conwell DL, Banks PA. Early changes in blood urea nitrogen predict mortality in acute pancreatitis. Gastroenterology. 2009;137:129–35.
Faisst M, Wellner UF, Utzolino S, Hopt UT, Keck T. Elevated blood urea nitrogen is an independent risk factor of prolonged intensive care unit stay due to acute necrotizing pancreatitis. J Crit Care. 2010;25:105–11.
Wu BU, Bakker OJ, Papachristou GI, Besselink MG, Repas K, van Santvoort HC, et al. Blood urea nitrogen in the early assessment of acute pancreatitis: an international validation study. Arch Intern Med. 2011;171:669–76.
Muddana V, Whitcomb DC, Khalid A, Slivka A, Papachristou GI. Elevated serum creatinine as a marker of pancreatic necrosis in acute pancreatitis. Am J Gastroenterol. 2009;104:164–70.
Lankisch PG, Weber-Dany B, Maisonneuve P, Lowenfels AB. High serum creatinine in acute pancreatitis: a marker for pancreatic necrosis? Am J Gastroenterol. 2010;105:1196–200.
Papachristou GI, Muddana V, Yadav D, Whitcomb DC. Increased serum creatinine is associated with pancreatic necrosis in acute pancreatitis. Am J Gastroenterol. 2010;105:1451–2.
Larvin M. Assessment of severity and prognosis in acute pancreatitis. Eur J Gastroenterol Hepatol. 1997;9:122–30.
Cardoso FS, Ricardo LB, Oliveira AM, Canena JM, Horta DV, Papoila AL, et al. C-reactive protein prognostic accuracy in acute pancreatitis: timing of measurement and cutoff points. Eur J Gastroenterol Hepatol. 2013;25:784–9.
Papachristou GI, Whitcomb DC. Inflammatory markers of disease severity in acute pancreatitis. Clin Lab Med. 2005;25:17–37.
Huang QL, Qian ZX, Li H. A comparative study of the urinary trypsinogen-2, trypsinogen activation peptide, and the computed tomography severity index as early predictors of the severity of acute pancreatitis. Hepatogastroenterology. 2010;57:1295–9.
Balthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology. 2002;223:603–13.
Balthazar EJ, Ranson JH, Naidich DP, Bailey I, James D. Acute pancreatitis: prognostic value of CT. Radiology. 1985;156:767–72.
London NJ, Neoptolemos JP, Lavelle J, et al. Contrast-enhanced abdominal computed tomography scanning and prediction of severity of acute pancreatitis: a prospective study. Br J Surg. 1989;76:268–72.
King NK, Powell JJ, Redhead D, Siriwardena AK. A simplified method for computed tomographic estimation of prognosis in acute pancreatitis. Scand J Gastroenterol. 2003;38:433–6.
Schroder T, Kivisaari L, Somer K, Standertskjöld-Nordenstam CG, Kivilaakso E, Lempinen M. Significance of extrapancreatic findings in computed tomography (CT) of acute pancreatitis. Eur J Radiol. 1985;5:273–5.
De Waele JJ, Delrue L, Hoste EA, De Vos M, Duyck P, Colardyn FA. Extrapancreatic inflammation on abdominal computed tomography as an early predictor of disease severity in acute pancreatitis: evaluation of a new scoring system. Pancreas. 2007;34:185–90.
Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990;174:331–6.
Bollen TL, Singh VK, Maurer R, Repas K, van Es HW, Banks PA, et al. A comparative evaluation of radiologic and clinical scoring systems in the early prediction of severity in acute pancreatitis. Am J Gastroenterol. 2012;107:612–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Mounzer, R., Papachristou, G.I. (2015). Clinical Predictors. In: Forsmark, C., Gardner, T. (eds) Prediction and Management of Severe Acute Pancreatitis. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0971-1_5
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0971-1_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0970-4
Online ISBN: 978-1-4939-0971-1
eBook Packages: MedicineMedicine (R0)