Abstract
Individuals with autism spectrum disorders (ASD) spend the majority of their lives as adults, and psychosocial interventions show promise for improving outcomes in this population. This research conducted a systematic review of all peer-review studies evaluating psychosocial interventions for adults with ASD. A total of 1,217 studies were reviewed, only 13 met inclusion criteria. The majority of studies were single case studies or non-randomized controlled trials, and most focused on applied behavior analysis or social cognition training. Effects of psychosocial treatment in adults with ASD were largely positive ranging from d = 0.14 to 3.59, although the quantity and quality of studies is limited. These findings suggest that there is substantial need for the rigorous development and evaluation of psychosocial treatments for adults with ASD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Autism Spectrum Disorder
- Autism Spectrum Disorder
- Psychosocial Intervention
- Applied Behavior Analysis
- Single Case Study
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Autism spectrum disorders (ASD) are chronic congenital neurological conditions which are characterized by abnormal or impaired development in social interaction and communication and a restricted repertoire of activity and interests (American Psychiatric Association, 2000). Currently, it is estimated that ASD affect approximately 1 in 88 children (Centers for Disease Control and Prevention, 2012), 70 % of whom are less than 14 years old (Gerhardt & Lainer, 2011), which indicates that the number of adults with ASD will be increasing dramatically in the coming years. However, relatively little work has investigated the best and most effective ways to treat adults with ASD in the community.
Since autism was first described by Kanner (1943), extensive research has documented its presentation, etiology, and treatment. Individuals diagnosed with an ASD typically experience difficulty in three main areas: (1) communication; (2) social interaction; and (3) flexibility of thinking and behavior (Wing & Gould, 1979). In order to address these difficulties, families often seek services for pre-school and school-aged children both inside and outside of the United States special education system (Thomas, Morrissey, & McLaurin, 2007). However, federal regulation mandates that individuals are no longer able to receive special education services after age 21 under the Individuals with Disabilities Education Act (Shattuck, Wagner, Narendorf, Sterzing, & Hensley, 2011). Given that approximately 70 % of people with ASD are currently less than 14 years old (Gerhardt & Lainer, 2011), the number of adults with ASD, and consequently the number of people who do not qualify for special education services, will increase dramatically in coming years. This is particularly concerning given that a recent study reported that the lifetime per capita societal cost of autism is $3.2 million (Ganz, 2007). More importantly, the areas of lifelong condition management that contribute most to the per capita cost of ASD are adult care and lost productivity, two aspects of living with an ASD which relate specifically to the approximately $1.9 million per capita spent after affected individuals age out of the United States special education system. Despite these findings, relatively little is known about effective interventions for adults with autism that might serve to facilitate positive outcomes for this group.
Historically, the prognosis for individuals diagnosed with ASD in childhood has been poor: Levy and Perry (2011) found across studies that prior to 1990, only 25 % of such individuals were classified as having “good” or “fair” outcomes based on an operationalized definition of a “good” or “fair” outcome for an adult with ASD as having achieved some form of formal education, maintaining employment, living independently, and sustaining social relationships. Currently, the state of affairs is not greatly improved. According to Seltzer, Shattuck, Abbeduto, and Greenberg (2004), very few adults with ASD live independently, get married, go to college, work in competitive jobs, or develop large social networks, and most individuals with ASD remain dependent on their families or on professional service providers. Levy and Perry (2011) found across studies that an average of 50–60 % of adults with ASD leave school without educational or vocational credentials, 76 % are unable to find work, and 90–95 % are unable to establish long-term romantic relationships or meaningful friendships. Beyond this, adults with ASD often suffer from comorbid psychiatric conditions, such as depressive and anxiety disorders, at potentially higher rates than both the general population and individuals with other developmental disabilities (Bradley, Summers, Wood, & Bryson, 2004; Brereton, Tonge, & Einfeld, 2006). This body of literature indicates that only a minority of diagnosed individuals are able to transition successfully to adulthood in the traditional sense, while an even smaller minority of the same individuals would be considered successful among those not affected by ASD.
Because many of the problems associated with ASD in childhood persist into and often intensify in adulthood, psychosocial interventions that target communication, social interaction, and flexibility of thinking and behavior, similar to those reported in reviews of the child ASD literature (Matson, Benavidez, Compton, Paclawskyj, & Baglio, 1996; Odom, Boyd, Hall, & Hume, 2010), may prove efficacious in the treatment of adults with ASD. Certainly, companies that cater to families and to agencies that serve adults with autism market a plethora of costly intervention programs and self-help books that promise to help this group of people in any number of ways. However, empirical evidence supporting their effectiveness is often unavailable.
The investigation of psychosocial interventions for adults with ASD is a relatively new area of research. However, work in this area is moving in a promising direction. For example, researchers in England have recently developed a psychosocial intervention protocol which utilizes a computer-based program to target impairments in social cognition (Golan & Baron-Cohen, 2006), while researchers in Spain have developed a protocol to reduce stress and more broadly improve quality of life (García-Villamisar & Dattilo, 2010). In addition to psychosocial interventions, researchers have also examined the efficacy of pharmacological treatment on adults with ASD, and while only five double-blind, randomized controlled trials (RCTs), have been conducted with modest sample sizes (M = 30), they have provided some evidence for the efficacy of risperidone, fluvoxamine, and haloperidol in the treatment of adults with ASD (Broadstock, Doughty, & Eggleston, 2007). Despite a limited but growing evidence base, a recent study reported that the percentage of adolescents and adults with ASD who were taking at least one psychotropic medication increased from 70 to 81 % over a four and a half year period (Esbensen, Greenberg, Seltzer, & Aman, 2009).
While evidence is accumulating regarding the benefits of psychosocial interventions for adults with ASD, there have been no systematic reviews or meta-analyses conducted to summarize the cumulative evidence base for these approaches. Therefore, we conducted a systematic review to examine the evidence base of psychosocial interventions for adults with ASD in order to determine common themes in treatment approaches and evaluate the evidence of their efficacy.
Method
Literature Search
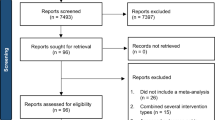
An extensive literature search was conducted in order to locate published studies documenting interventions for adults with ASD. In order to conduct this literature search, keyword searches were performed over a 4-month period of abstracts available in the PsycINFO, Medline, and Web of Knowledge databases published between January 1950 to September 2011, using the search terms “autism,” “Asperger’s,” or “pervasive developmental disorder” combined with “adult” or “adolescent” combined with “intervention,” “treatment,” or “therapy.” Additionally, abstracts of articles published online ahead of print between July 2011 and September 2011 were searched to identify recent pre-publication studies in five journals: The Journal of Autism and Developmental Disabilities, Autism, Research on Autism Spectrum Disorders, Research in Developmental Disabilities, and The Journal of Intellectual Disability Research. These searches revealed 1,217 published reports. Additionally, references of relevant studies were examined for additional studies to be included in this research.
Abstracts retrieved from database searches were then reviewed, and studies were included for further consideration if they reported a psychosocial intervention for adults with ASD. From these abstract searches, studies were then examined and included in this review if they (1) were conducted using a single case study, non-controlled trial, non-randomized controlled trial, or RCT design that reported pre-test and post-test data, (2) reported quantitative findings, (3) included participants ages 18 and older, and (4) included participants with ASD. In total, 13 studies assessing psychosocial interventions for adults with ASD were found. Of the 1,204 studies that did not meet inclusion criteria for this review, only two reported findings from psychosocial intervention studies for adults with ASD. Of these two studies, one was excluded because the sample of participants also included children as young as 9 years old (Herbrecht et al., 2009) and the other was excluded because it did not report quantitative findings (McClannahan, MacDuff, & Krantz, 2002). Overall, the largest category of excluded studies were those that described or classified the symptoms and challenges faced by individuals with ASD (k = 574). There were also a substantial number of studies that sought to expand upon knowledge of the genetics and neurobiology of ASD (k = 184). Other categories of excluded studies included non-empirical studies, including book reviews (k = 138), followed by empirical studies of adults only (k = 97), measurement studies (k = 80), studies of psychosocial interventions for children and adolescents (k = 73), review articles (k = 41), pharmacological studies (k = 35), prevalence studies (k = 23), studies of the effect of autism on families (k = 22), studies of services available for people with ASD (k = 16), studies of adult outcomes for children diagnosed with ASD (k = 8), and unrelated studies (k = 10).
Study Coding Procedures
After assembling the studies included in this review, theoretically and/or methodically relevant characteristics and variables were recorded. These included the demographic characteristics and IQ of participants. For studies which examined other populations, only demographic and IQ information for the ASD sample was obtained. Finally, the design of each study (i.e., single case study, non-randomized controlled trial, non-controlled trial, or RCT) was recorded.
Study Analysis
After coding the different characteristics of each study, the main outcomes were recorded. In order to ascertain the relative effectiveness of the psychosocial interventions described in the studies, Cohen’s d was calculated using mean change divided by pooled standard deviation. For longitudinal controlled studies, aggregate Cohen’s d of differential efficacy for the experimental versus control group for the study was calculated using within group standardized change for each group and subtracting the effect sizes of the control group from the treatment group. For uncontrolled pre–post studies, Cohen’s d was calculated using within-group standardized change for the treatment group. For studies for which only Z scores were reported, Cohen’s d was computed by converting Z to r and r to d (Hedges & Olkin, 1984). Cohen’s d was not reported for single case studies. In all cases, Cohen’s d was computed using methods which align with best practice (Littell, Corcoran, & Pillai, 2008; Rosenthal, 1984).
Results
A total of 13 studies were identified which evaluated psychosocial interventions and met inclusion criteria. A list of studies and their characteristics are detailed in Table 16.1. The included studies were diverse in their methodologies and represented numerous categories of interventions. A total of five were single case studies, four were RCTs, three were non-randomized controlled trials, and one was an uncontrolled pre–post trial. Six studies evaluated the efficacy of social cognition training, five studies evaluated the efficacy of applied behavior analysis (ABA) techniques, and two studies evaluated the efficacy of other types of community-based interventions. We considered numerous ways to organize the presentation of these studies, including around outcome. In the end, we viewed organization around the type of intervention studied as most appropriate, given that some investigations examined outcomes that were not clearly connected to their intervention targets (e.g., examining the cognitive effects of a supported employment program). While such studies are quite valuable, organizing them around the outcomes they report could give readers the false impression that such interventions are specifically designed to target those outcomes, which is not always the case. Consequently, we decided that organizing the review around the nature of the intervention (as opposed to its effects) was the most accurate way to represent this treatment literature.
Social Cognition Training
Unlike what is indicated in systematic reviews of the child ASD literature (Matson et al., 1996; Odom et al., 2010), more included studies focused on social cognition training than on ABA techniques (Baker et al., 2005; Bölte et al. 2002; Faja et al., 2012; Gantman, Kapp, Orenski, & Laugeson, 2012; Golan & Baron-Cohen, 2006; McDonald & Hemmes, 2003; Moore, 2009; Rehfeldt & Chambers, 2003; Shabani & Fisher, 2006; Trepagnier et al., 2011; Turner-Brown et al., 2008). The six social cognition training studies (Bölte et al. 2002; Faja et al., 2012; Gantman et al., 2012; Golan & Baron-Cohen, 2006; Trepagnier et al., 2011; Turner-Brown et al., 2008) sought to improve participants’ ability to grasp social cues and, as a consequence, improve social functioning. Notably, four out of six of the studies in this category utilized computer-based training, indicating a trend toward the utilization of computer software for this specific type intervention (Bölte et al. 2002; Faja et al., 2012; Golan & Baron-Cohen, 2006; Trepagnier et al., 2011). Additionally, three out of six studies concentrated on improving Theory of Mind (Bölte et al. 2002; Golan & Baron-Cohen, 2006; Turner-Brown et al., 2008). With one exception (Trepagnier et al., 2011), which found only a trend toward improvement in social cognition, all social cognition training interventions saw significant improvement in participants’ scores on included measures. The overall effect size (d) for the social cognition training studies ranged broadly from 0.14 to 3.59 for improving domains of social cognition, communication, and social skills.
Three of the six social cognition training studies utilized interventions based on the theory of mind theory of autism (Baron-Cohen, Leslie, & Frith, 1985). Bölte and colleagues (2002) designed a computer program to test and train participants in the capacity to detect seven facially expressed emotions (happiness, sadness, anger, disgust, fear, surprise, neutral) using either a picture of the whole face or a picture of the eyes. The authors found that participants in this intervention performed better on Baron-Cohen’s Reading the Mind in Eyes (Baron-Cohen, Wheelwright, Hill, Raste, & Plumb, 2001) and Reading the Mind in Face (Baron-Cohen et al., 1996) tasks. Golan and Baron-Cohen (2006) designed and tested a computer-based training program designed to teach people with ASD how to correctly recognize facial emotions. They found significant improvement on measures of face and voice recognition. Finally, Turner-Brown et al. (2008) used a group-based cognitive behavioral intervention that was comprised of three phases (emotion training, figuring out situations, and integration) and designed to improve social-cognitive functioning. The authors found that participants who received the intervention showed significant improvement in theory of mind skills and trend-level improvement in social communication skills. Notably, two of these interventions (Bölte et al. 2002; Golan & Baron-Cohen, 2006) utilized a computer-based protocol to improve theory of mind.
The final three social cognition training studies did not explicitly target theory of mind, but instead used other interventions designed to improve functioning in these areas. Faja and colleagues (2012) reported the results of a study in which participants were randomized to a computerized training program involving either faces or houses and the ability to recognize either faces or houses was tested by asking participants to categorize pictures of faces or houses based on set criteria, such as gender (for faces) or house shape (for houses). The authors found that both participants trained in face recognition and participants trained in house recognition showed improvement on measures of memory of faces and houses. Gantman and colleagues (2012) tested the effectiveness of a caregiver-assisted social skills training intervention (PEERS for Young Adults). The authors found that participants reported significantly less loneliness and improved social skills knowledge while their caregivers reported significant improvements in participants’ overall social skills, social responsiveness, empathy, and frequency of get-togethers. Finally, Trepagnier et al. (2011) reported on the development of a computer-based conversation simulation program designed to teach conversational skills to adolescents and adults with ASD. While the authors found that participants generally liked the intervention, the authors did not report any significant level of improvement on psychometric or behavioral measures.
Applied Behavior Analysis
This review identified a total of five studies that utilized ABA techniques. All of the included ABA studies were single case studies. All ABA studies sought to reduce the instances of an undesirable behavior or increase the instances of a desirable behavior. All ABA studies reported positive benefits of treatment, although the maintenance of this benefit varied between studies. Effect size was not reported for the ABA studies, as findings were based on a single subject.
Three studies utilized ABA principles to reduce the instance of undesirable behaviors such as coprophagia (Baker et al., 2005), repeated inappropriate gestures (Moore, 2009), or verbal perseverations (Rehfeldt & Chambers, 2003). Baker et al. (2005) reported on an intervention in which highly spiced, flavorful foods were provided with meals and snacks to reduce coprophagia. The authors found that this intervention variably reduced the frequency of coprophagia for the first 6 months following intervention and completely eliminated coprophagia thereafter. Moore (2009) evaluated a self-management treatment package in which a participant administered positive reinforcement (Diet Cola) as a reward if he was able to achieve an increasing interval without exhibiting stereotypic behaviors (e.g., finger tapping, mouth grabbing, genital touching). The author found that this intervention helped to increase the latency to stereotypic behaviors over time. Finally, Rehfeldt and Chambers (2003) used a reversal (BABAB) design to examine the effects of intervening with mild reprimands (e.g., “you shouldn’t talk about sirens so much at work”) and reciprocal statements (e.g., “you sure don’t like those sirens, do you?”) when the participant perseverated verbally. The authors found that this intervention was effective in decreasing the number of verbal perseverations.
Two studies used ABA principles to increase the instances of desirable behaviors such as social interaction (McDonald & Hemmes, 2003) and compliance with medical procedures (Shabani & Fisher, 2006). McDonald and Hemmes (2003) reported on an intervention in which token reinforcers were used to increase the instance of verbal initiating with adult staff in a classroom setting. The authors found that spontaneous initiating increased over the course of the intervention. Shabani and Fisher (2006) evaluated an intervention for a person diagnosed with both autism and diabetes that was designed to make glucose monitoring possible. This intervention used stimulus fading, which consisted of gradually increased exposure to a needle, combined with differential reinforcement to increase the percentage of successful blood glucose monitoring trials. The authors found that the percentage of successful blood glucose monitoring trials improved over the course of the intervention.
Community-Based Interventions
Two studies examined community-based intervention programs. These programs included a supported employment program (García-Villamisar & Hughes, 2007) and a leisure program (García-Villamisar & Dattilo, 2010). García-Villamisar and Hughes (2007) examined the effects of a classic, community-based supported employment program on measures of cognitive functioning. They found that participants enrolled in the supported employment program exhibited better executive functioning on cognitive measures than a comparison group of unemployed participants. García-Villamisar and Dattilo (2010) examined the effects of a leisure program (a group recreation program where participants had access to games, crafts, group activities, community events, and socialization) on quality of life and stress. The authors found that participants in the leisure program reported significant decreases in stress and significant increases in quality of life. Effect sizes for these two studies were 0.45 for improving cognitive functioning and 0.83 for improving adaptive behavior, respectively.
Discussion
Current estimates indicate that approximately 1 in every 88 children has ASD (Centers for Disease Control and Prevention, 2012) and that approximately 70 % of identified individuals with ASD are under age 14 (Gerhardt & Lainer, 2011). This cohort of children is rapidly approaching adulthood and will need effective treatment and services once they age out of entitlement services provided within and through the United States special education system. Studies have indicated that individuals with ASD have challenges and difficulties as they transition to adulthood (Howlin, Goode, Hutton, & Rutter, 2004), which are not being sufficiently met by the available treatments and services for adults with ASD (Shattuck et al., 2011). Therefore, it is important for the autism research community to be familiar with the current evidence base for psychosocial interventions for adults with these conditions in order to inform future research and treatment.
We conducted a systematic review to examine the evidence base of psychosocial intervention studies for adults with ASD. Of the 1,217 studies retrieved from a comprehensive literature search, only 13 studies met inclusion criteria (i.e., reported quantitative findings, included participants ages 18 and older, and included participants with ASD). The studies represented three main types of interventions (social cognition training, ABA, and a small heterogeneous group of community-based programs) and a range of methodological approaches. Of these 13 studies reviewed, four were randomized-controlled trials, while five were single case studies. As a whole, the studies identified had modest sample sizes, with the greatest including 71 participants and over three-quarters of studies having less than 20 participants. These characteristics identify methodological limitations in the current evidence base of psychosocial treatment for ASD, yet despite these limitations, all studies in this review reported favorable outcomes and benefits to participants.
The studies detailed in this review addressed many of the core deficits of ASD (i.e., communication, social interaction, and flexibility of thinking and behavior) with considerable success. Beyond this, the included studies often used creative techniques to help adults with ASD address these deficits. For instance, three intervention protocols taught skills to address deficits in communication and social interaction via computer-based training (Bölte et al. 2002; Golan & Baron-Cohen, 2006; Trepagnier et al., 2011), an intervention technique that has been found to be enjoyable for and agreeable to adults with ASD (Trepagnier et al., 2011). However, it must be noted that while such computer-based approaches seem to represent an increasing trend, no evidence currently exists indicating they are more effective than non-computer-based interventions. While all included studies were effective, the social cognition training studies appear to show the most promise as they included the most rigorous methodologies while maintaining adequate power and effect sizes. This indicates a particularly promising direction for future research on psychosocial interventions for adults with ASD, especially those that employ more comprehensive interventions designed to target core information professing deficits and facilitate the generalization of social-cognitive abilities such as perspective-taking and social context appraisal to unrehearsed social situations.
Despite evidence of the benefits of psychosocial interventions for adults with ASD, there are significant limitations to the current evidence base. While we conducted an extensive search of the literature available on psychosocial interventions for adults with ASD since 1950, only 13 studies were found. Due to the small number of studies, we were unable to conduct a meta-analysis of the adult ASD literature. As a consequence, clear estimates of effect size for different types of psychosocial interventions are not available. Effect sizes should also be interpreted with caution, especially for studies with small sample sizes, which comprised the majority of studies. The incongruent nature of outcome measures used in some of the included studies also indicate that the reader should take caution before generalizing the results of included studies. For instance, García-Villamisar & Hughes (2007) used cognitive functioning outcomes, such as the Stockings of Cambridge and Big Circle/Little Circle tasks, to measure the effectiveness of a supported employment program but did not report outcome data on the number of adults with ASD who were employed as a result of the program. Similarly, Golan & Baron-Cohen (2006) reported significant improvement on the Cambridge Mindreading (CAM) Face-Voice Battery, which tests recall of specific questions, photographs, and voice recordings which are specifically taught in the Mind Reading intervention program but did not report significant improvement on other measures for which participants had not been specifically trained. Clearly, there is a potential benefit of effectively treating adults with ASD, but there is a need for continued investigation in this area.
This review of the evidence base for psychosocial interventions in adults with ASD is informative in guiding future studies. The new research conducted on psychosocial interventions for adults should use more rigorous and adequately powered methodology and carefully select outcome measures which are congruent with the intervention type and research questions. Because the social cognition training protocols appear to show the most promise, there is a significant need to test novel social cognition training approaches which use creative intervention techniques in rigorous intervention studies with larger sample sizes. This will undoubtedly build upon the work that has been conducted in this area to date. While many of the studies described in this review use protocols that could be easily adapted to community-based settings, it is important to note that none of the studies detailed in this review apply lab-tested psychosocial intervention programs to samples within the community. In the future, when research has identified efficacious intervention studies through careful testing, these evidence-based interventions need to be disseminated to the community and adapted to community-based settings in order to test their effectiveness in the day-to-day treatment of adults with ASD. As such, it will be important for interventionists to develop treatments that can not only be tested in academic research settings, but easily disseminated to the community-based programs that serve the majority of adults with these conditions.
While the number of studies which comprise the evidence base of psychosocial interventions for adults with ASD is small, all of the studies included in this review report a positive benefit to study participants. This indicates that psychosocial interventions for adults with ASD will likely be beneficial for this population. However, because this field is in its infancy, researchers have the opportunity to make a significant contribution to the way that adults with ASD are treated by creating and conducting innovative and methodologically rigorous intervention studies which help adults with autism adjust to and thrive in the world in which they live.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
Baker, D., Valenzuela, S., & Wieseler, N. (2005). Naturalistic inquiry and treatment of coprophagia in one individual. Journal of Developmental and Physical Disabilities, 17(4), 361–367.
Baron-Cohen, S., Leslie, A. M., & Frith, U. (1985). Does the autistic child have a “theory of mind”? Cognition, 21, 37–46.
Baron-Cohen, S., Riviere, A., Fukushima, M., French, D., Hadwin, J., Cross, P., et al. (1996). Reading the mind in the face: A cross-cultural and developmental study. Visual Cognition, 3(1), 39–59.
Baron-Cohen, S., Wheelwright, S., Hill, J., Raste, Y., & Plumb, I. (2001). The “Reading the Mind in the Eyes” test revised version: A study with normal adults, and adults with Asperger syndrome or high-functioning autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 42(2), 241–251.
Bölte, S., Feineis-Matthews, S., Leber, S., Dierks, T., Hubl, D., & Poustka, F. (2002). The development and evaluation of a computer-based program to test and to teach the recognition of facial affect. International Journal of Circumpolar Health, 61(Suppl 2), 61–68.
Bradley, E., Summers, J., Wood, H., & Bryson, S. (2004). Comparing rates of psychiatric and behavior disorders in adolescents and young adults with severe intellectual disability with and without autism. Journal of Autism and Developmental Disorders, 34(2), 151–161.
Brereton, A. V., Tonge, B. J., & Einfeld, S. L. (2006). Psychopathology in children and adolescents with autism compared to young people with intellectual disability. Journal of Autism and Developmental Disorders, 36(7), 863–870.
Broadstock, M., Doughty, C., & Eggleston, M. (2007). Systematic review of the effectiveness of pharmacological treatments for adolescents and adults with autism spectrum disorder. Autism, 11(4), 335–348.
Centers for Disease Control and Prevention. (2012). Prevalence of autism spectrum disorders—Autism and developmental disabilities monitoring network, 14 Sites, United States 2008. MMWR Surveillance Summaries, 61(3), 1–19.
Esbensen, A. J., Greenberg, J. S., Seltzer, M. M., & Aman, M. G. (2009). A longitudinal investigation of psychotropic and non-psychotropic medication use among adolescents and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(9), 1339–1349.
Faja, S., Webb, S. J., Jones, E., Merkle, K., Kamara, D., Bavaro, J., et al. (2012). The effects of face expertise training on the behavioral performance and brain activity of adults with high functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(2), 278–293.
Gantman, A., Kapp, S. K., Orenski, K., & Laugeson, E. A. (2012). Social skills training for young adults with high-functioning autism spectrum disorders: A randomized controlled pilot study. Journal of Autism and Developmental Disorders, 42(6), 1094–1103.
Ganz, M. L. (2007). The lifetime distribution of the incremental societal costs of autism. Archives of Pediatric & Adolescent Medicine, 161(4), 343–349.
García-Villamisar, D., & Dattilo, J. (2010). Effects of a leisure programme on quality of life and stress of individuals with ASD. Journal of Intellectual Disability Research, 54(7), 611–619.
García-Villamisar, D., & Hughes, C. (2007). Supported employment improves cognitive performance in adults with autism. Journal of Intellectual Disability Research, 51(2), 142–150.
Gerhardt, P., & Lainer, I. (2011). Addressing the needs of adolescents and adults with autism: A crisis on the horizon. Journal of Contemporary Psychotherapy, 41(1), 37–45.
Golan, O., & Baron-Cohen, S. (2006). Systemizing empathy: Teaching adults with Asperger syndrome or high-functioning autism to recognize complex emotions using interactive multimedia. Development and Psychopathology, 18(02), 591–617.
Hedges, L. V., & Olkin, I. (1984). Nonparametric estimators of effect size in meta-analysis. Psychological Bulletin, 96(3), 573–580.
Herbrecht, E., Poustka, F., Birnkammer, S., Duketis, E., Schlitt, S., Schmötzer, G., et al. (2009). Pilot evaluation of the Frankfurt Social Skills Training for children and adolescents with autism spectrum disorder. European Child & Adolescent Psychiatry, 18(6), 327–335.
Howlin, P., Goode, S., Hutton, J., & Rutter, M. (2004). Adult outcome for children with autism. Journal of Child Psychology and Psychiatry, 45(2), 212–229.
Kanner, L. (1943). Autistic disturbances of affective contact. Nervous Child, 2(3), 217–250.
Levy, A., & Perry, A. (2011). Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders, 5(4), 1271–1282.
Littell, J. A., Corcoran, J., & Pillai, V. (2008). Systematic reviews and meta-analysis. New York: Oxford University Press.
Matson, J. L., Benavidez, D. A., Compton, L. S., Paclawskyj, T., & Baglio, C. (1996). Behavioral treatment of autistic persons: A review of research from 1980 to the present. Research in Developmental Disabilities, 17(6), 433–465.
McClannahan, L. E., MacDuff, G. S., & Krantz, P. J. (2002). Behavior analysis and intervention for adults with autism. Behavior Modification, 26(1), 9–26.
McDonald, M. E., & Hemmes, N. S. (2003). Increases in social initiation toward an adolescent with autism: Reciprocity effects. Research in Developmental Disabilities, 24, 453–465.
Moore, T. R. (2009). A brief report on the effects of a self-management treatment package on streotypic behavior. Research in Autism Spectrum Disorders, 3, 695–701.
Odom, S. L., Boyd, B. A., Hall, L. J., & Hume, K. (2010). Evaluation of comprehensive treatment models for individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(4), 425–436.
Rehfeldt, R. A., & Chambers, M. R. (2003). Functional analysis and treatment of verbal perseverations displayed by an adult with autism. Journal of Applied Behavior Analysis, 36(2), 259–261.
Rosenthal, R. (1984). Meta-analytic procedures for social research. Beverly Hills, CA: Sage.
Seltzer, M. M., Shattuck, P. T., Abbeduto, L., & Greenberg, J. S. (2004). Trajectory of development in adolescents and adults with autism. Mental Retardation and Developmental Disabilities Research Reviews, 10(4), 234–247.
Shabani, D. B., & Fisher, W. W. (2006). Stimulus fading and differential reinforcement for the treatment of needle phobia in a youth with autism. Journal of Applied Behavior Analysis, 39(4), 449–452.
Shattuck, P. T., Wagner, M., Narendorf, S., Sterzing, P., & Hensley, M. (2011). Post-high school service use among young adults with an autism spectrum disorder. Archives of Pediatric & Adolescent Medicine, 165(2), 141–146.
Thomas, K. C., Morrissey, J. P., & McLaurin, C. (2007). Use of autism-related services by families and children. Journal of Autism and Developmental Disorders, 37(5), 818–829.
Trepagnier, C. Y., Olsen, D. E., Boteler, L., & Bell, C. A. (2011). Virtual conversation partner for adults with autism. Cyberpsychology, Behavior and Social Networking, 14(1–2), 21–27.
Turner-Brown, L., Perry, T., Dichter, G., Bodfish, J., & Penn, D. (2008). Brief report: Feasibility of social cognition and interaction training for adults with high functioning autism. Journal of Autism and Developmental Disorders, 38(9), 1777–1784.
Wing, L., & Gould, J. (1979). Severe impairments of social interaction and associated abnormalities in children: Epidemiology and classification. Journal of Autism and Developmental Disorders, 9(1), 11–29.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Bishop-Fitzpatrick, L., Minshew, N.J., Eack, S.M. (2014). A Systematic Review of Psychosocial Interventions for Adults with Autism Spectrum Disorders. In: Volkmar, F., Reichow, B., McPartland, J. (eds) Adolescents and Adults with Autism Spectrum Disorders. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0506-5_16
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0506-5_16
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0505-8
Online ISBN: 978-1-4939-0506-5
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)